- 1Institute for Urology and Reproductive Health, Sechenov University, Moscow, Russia
- 2Division of Urology, Department of Oncology, School of Medicine, San Luigi Hospital, University of Turin, Orbassano, Italy
- 3International School “Medicine of the Future”, Sechenov University, Moscow, Russia
- 4Laniado Hospital, Netanya, Israel
- 5Urology Department, University of Modena and Reggio Emilia, Modena, Italy
- 6Department of Uro-Nephrology, Virgen del RocíoUniversity Hospital, Seville, Seville Biomedicine Institute, IBiS/Virgen del Rocío University Hospital/Consejo Superior de Investigaciones Científicas/Seville University, Seville, Spain
- 7Department of Urology, University Medical Center Mannheim, Heidelberg University, Mannheim, Germany
- 8Department of Urology, Ludwig-Maximilians-University, Munich, Germany
- 9Department of Urology, Clinico San Carlos University Hospital, Madrid, Spain
- 10Institute of Urology and Catherine & Joseph Aresty Department of Urology, Keck School of Medicine, University of Southern California, Los Angeles, CA, United States
- 11Artificial Intelligence Center at University of Southern California (USC) Urology, Institute of Urology, University of Southern California, Los Angeles, CA, United States
- 12Department of Urology, Medical University of Vienna, Vienna, Austria
Introduction: The Thulium fiber laser (TFL) is a new device that in contrast to the other solid-state YAG-based lasers takes a different approach to pulse formation allowing for two different modes: in the QCW (quasi-continuous wave) function, TFL is convenient for soft tissue surgery and in the SP (Superpulsed) mode it is highly effective in lithotripsy. Thus, unlike the other thulium lasers (Tm : YAG), TFL can be used in a wide range of surgical procedures.
Materials and Methods: We conducted a systematic search in 3 databases: Medline, Scopus and Cochrane library. All original articles (both preclinical and clinical) on TFL application in soft tissue surgery were included in data analysis.
Results: In terms of its cutting properties, QCW TFL is not inferior to the other thulium lasers, and in fact allows for decreased carbonization (due to lower heat production) compared to continuous lasers (e.g. Tm : YAG). It has been used successfully in endoscopic enucleation of the prostate (EEP) and in en bloc resection of bladder tumors (ERBT). The efficacy and safety of this laser is comparable to TURP and simple prostatectomy, but the recovery period is shorter and the learning curve is slightly superior to other endoscopic procedures. There are no significant differences between TFL and Ho : YAG in terms of efficacy and safety during EEP. Unfortunately, there are no clinical studies that analyse the efficacy and safety of SP TFL in EEP or ERBT.
Conclusion: TFL is a safe and effective tool for BPH surgery. In terms of parameters, it is in no way inferior to Tm : YAG or Ho : YAG during EEP. However, TFL surpasses these lasers in terms of usability and serviceability. These advantages are likely to render it more popular over time.
Introduction
Lasers are now unquestionably an integral part of endoscopic surgery. Laser based techniques have become the standard modalities of choice in BPH surgery, NMIBC treatment and of course in lithotripsy procedures (1–5). This spectrum of capabilities is linked to the specific properties of the laser such as wavelength, pulse power and pulse duration (6). Whilst some types of lasers are better applied to soft tissue surgery others lend themselves more to lithotripsy. The most significant determining factor for a laser’s efficiency is its wavelength. The laser affects only molecules whose absorption spectrum is as close as possible to the wavelength of the laser. They are called chromophores. Water and hemoglobin molecules are the most prevalent chromophores in the human body; their peak of absorption happens at 1910 nm and 532 nm respectively (7). Chromophores absorb the laser energy which leads to the heating of tissues containing those chromophores (8). If the laser wavelength is close to the chromophore absorption peak (high absorption coefficient), the majority of energy affects directly the chromophore without resulting in energy dispersion in the surrounding tissues. This means that collateral damage can be minimized by using lasers with a high absorption coefficient (9).
Since the late 1990s, the Holmium : YAG laser (Ho : YAG) has become the most frequently used device in endoscopy. Thanks to its wavelength, Ho : YAG is highly absorbed by water which leads to vaporization without deep coagulative necrosis with the depth of tissue penetration being 0.4-0.7 mm (10). The main feature of this laser is its high peak power (2-10 kW) and its ability to rapidly increase its power. This titanic outburst of power creates a large stream of vapor bubbles which can be a factor in soft tissue surgery, when it is not only the laser radiation which cuts the tissue, but the stream of vapor.
Thulium based lasers stepped into the limelight with the introduction of the solid-state Tm : YAG laser. This laser is a continuous, water-targeted laser with a wavelength of 2010 nm. Its theoretical penetration depth is approximately 0.2 mm, and its firing regimen is different to that of the Ho : YAG. Tm : YAG is a continuous wave device and is therefore characterized by effective hemostasis, and so we would expect it to become a suitable tool for soft tissue cutting (10). It can be used for prostate vaporization, vaporesection, vapoenucleation and for mostly mechanical enucleation (11–13). Also, it has turned out to be a highly effective, safe and convenient tool for en bloc resection of NMIBC (14, 15). In summary, one could say that this laser is a good option for the cutting of soft tissues but you could say that its advantage is also its limitation – being a continuous wave device it is not effective for lithotripsy.
TFL construction substantially differs from Tm : YAG. Firstly, the YAG laser medium was replaced with thulium doped silica fiber (16, 17). Thulium was chosen because the wavelength it creates is the closest to the water absorption peak (TFL – 1940 nm, water – 1910). For this reason, its theoretical penetration depth is only 0.15 mm (in comparison, for the Tm : YAG it is 0.2 mm, Ho : YAG – 0.4-0.7 mm) (10). This feature may decrease the risk of complications and minimize collateral damage (18). Secondly, the silica fiber instead of YAG-crystal decreases the energy consumption and heat production. It allows instead to create an air-cooling system (instead of water-cooling in Ho : YAG), so the device is smaller and lighter compared with other lasers (19). Also, the decreased energy consumption comes about from using the standard 220V wall plugs without any proprietary connectors or any custom voltage. Thirdly, in TFL a Q-switcher system was applied to convert the super pulsed (SP) mode to quasi-continuous (QCW) for better soft tissue cutting. Due to those properties, the modifications of TFL combining in itself both (QCW) and (SP) modes exist today (20).
The thulium fiber laser (TFL) was created to combine the advantages of thulium-based effective cutting with holmium-like lithotripsy. The development of this device was followed by a series of preclinical tests, carefully studying each feature of the laser. This meant that the efficiency of the laser could be tested on a preclinical basis, and that the findings could be translated into surgical practice. In this paper, we will show how the preclinical results of TFL were tested in the clinic, and how our understanding of the device’s physics and build will affect the outcomes.
Materials and methods
We performed a systematic literature search using two databases (Medline (PubMed), Scopus and Cochrane library) where the majority of the TFLs preclinical and clinical trials results are comprehensively described. We used the following search query: “(TFL OR “Thulium fiber laser” NOT tensor) AND ((Soft tissu*) OR Cutting OR ThuFLEP OR EEP OR enucleation OR BPH OR “en bloc” OR resection)”. Such an approach was chosen because a precise search would definitely ensure that we do not miss any data related to the use of the Thulium fiber laser in BPH treatment.
The inclusion criteria were as follows: all types of studies (both prospective and retrospective) containing their own data on TFLs preclinical and clinical trial results. We included only articles in English. Any other literature without original data or sufficient information were excluded. These might include different types of reviews, comments, single cases, editorial material, books as well as conference abstracts.
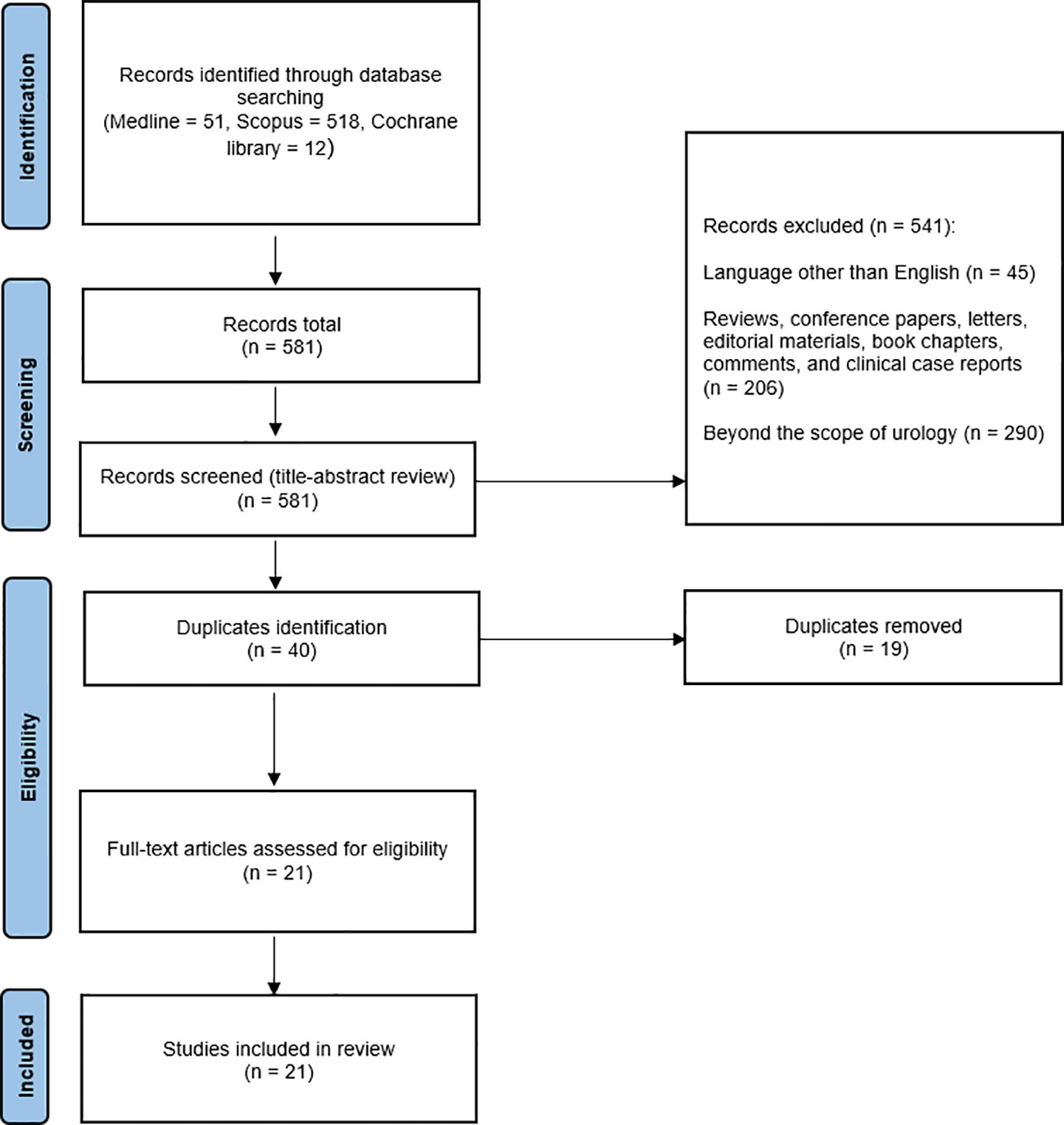
Firstly, AA and CA performed a title review. No additional filters or limitations to the search were used. Only articles in English were included. Secondly, MT and AO independently performed abstract reviews according to the same criteria. Once the title and abstract were reviewed, AA and CA manually removed any duplicates. Different types of reviews, editorial material, books, comments and clinical case reports were excluded. In addition, all articles that deal with the use of TFL for lithotripsy were excluded. Also, MT, CA and AA excluded all studies which went beyond the scope of urologic surgery. As a last step, MT, AO and AA independently performed a full-text review. In the event of any disagreement, each party made their case and tried to resolve it. If they could not come to an agreement, DE made the final decision. All in all, 21 articles were included in our review – 9 preclinical and 12 clinical (Figure 1).
Thulium fiber laser for soft tissues
Thulium fiber laser for soft tissues: preclinical trials
The first in-vitro trial on TFL was conducted by Fried et al. (21, 22) showing the TFL potential in tissue cutting with a prostate (canine model) vaporization rate of 0.83+/-0.11 g/minute and with the hope that it would lead to an effective hemostasis. To assess the impact of the different TFL modes on soft tissue and to compare it with the other lasers, Taratkin et al. conducted a preclinical study using a non-frozen porcine kidney (23). The Ho : YAG incision had a conical ablation zone with a deep tissue rupture at the apex of the cone. The margins also were ruptured and shallow with a thin coagulation area without any carbonization. The QCW TFL mode made a coniform ablation zone approximately 1.5 times larger than Ho : YAG, with a rounded apex with a moderate carbonization. The Superpulsed (SP) mode of TFL produced an incision shape that was similar to Ho : YAG with minimal carbonization (23).
This finding was supported in another trial, assessing the impact of the fiber diameter (200 vs 600 μm) in different laser modes. No significant differences were observed irrespective of the fiber diameter except for the width of the coagulation zone for QCW TFL (smaller for 600 μm). QCW TFL made a coagulation zone 3 – 5 times larger than the SP TFL. The QCW laser mode cuts the tissues faster, its incision was 1.5-2 times deeper, and the vaporization volume was 2-5 times higher, and yet it leads to increased tissue carbonization. The SP TFL incision showed no carbonization, but its hemostasis may be considered insufficient due to lower coagulation depth. These results suggest that QCW TFL may be a good option for soft tissue cutting with adequate hemostasis (24).
Another preclinical study aimed to compare the distance-dependent impact of different lasers on soft tissue. Only Ho : YAG made an incision of a distance ≥ 2 mm (25). The deepest incision performed in the contact mode (fiber-tissue distance = 0 mm) was made by QCW TFL (70-90% higher than other lasers); at the fiber-tissue distance at 1 mm all of those lasers showed the similar results. The coagulation depth demonstrated similar patterns – QCW TFL coagulation was 70-90% deeper than that for other lasers at the distance <2 mm; no coagulation was noticed at the distance >3 mm. So, the authors recognized QCW TFL as the most effective for tissue cutting and cauterizing in contact mode. SP TFL has a similar pattern to Ho : YAG. However, the authors consider SP TFL to be the safer device as it showed no tissue damage at 2 mm (Ho : YAG show tissue rupture at >3 mm) (25). Doizi et al. (26) also compared the incision and coagulation depth of Ho : YAG and TFL. The results were in line with those of Taratkin et al.
Yilmaz et al. (27) in their study tried to simulate the prostate enucleation process using a model of porcine belly. The researchers compared the speed of anterior abdominal wall fascial layers with separation, coagulation performance of lasers and the ease with which the surgeon could operate. The high-power Ho : YAG (4.5 J, 22.3 Hz, 100 W, 0.15 ms) performed the fastest layer separation (31.5 cm2 per minute). The other lasers produced more modest results: pulsed-Tm : YAG - 15 cm2 at 3 J, 25 Hz, 75 W, and 0.86 ms pulse duration; TFL – 12 cm2 at setting 4 J, 10 Hz, 40 W, and 8 ms; low-power Ho : YAG – 6 cm2 at 3.5 J, 10 Hz, 35 W and a pulse duration of 0.45 ms. At the same laser settings (3 J, 10 Hz), TFL demonstrated its higher efficacy - 5.25 cm2 of layer separation compared to the other lasers: HP-Ho : YAG - 4.5 cm2, p-Tm : YAG - 3 cm2, LP-Ho : YAG 2 cm2. P-Tm : YAG demonstrated the highest coagulation performance – a total score of 4.3 followed by TFL (3.5), LP-Ho : YAG (3.0) and HP-Ho : YAG (2.5), which was the least satisfactory in terms of coagulation properties. HP-Ho : YAG was rated subjectively as the most satisfactory laser in terms of surgeons’ usability (Likert scale 4.06, NASA-TLX 4.38) due to its high enucleation speed and efficacy. TFL took the penultimate place with its Likert scale reading of 3.38 and NASA-TLX 3.92. LP-Ho : YAG was considered the least effective (Likert scale 3.25, NASA-TLX 4.09).
Comparing the impact on the soft tissues of TFL and Hybrid laser (combination of a Thulium fiber and Blue diode laser), Becker et al. obtained the following results (28): the Hybrid laser demonstrated the best vaporization and coagulation properties (50% more than TFL and 2-3 times more than Ho : YAG) with a coagulation zone smaller (by 10%) compared to the QCW TFL. The Hybrid laser’s carbonisation was significantly lower than those for TFL (28). Those properties for both TFL and Hybrid laser were observed by Arkhipova et al. in their study (29).
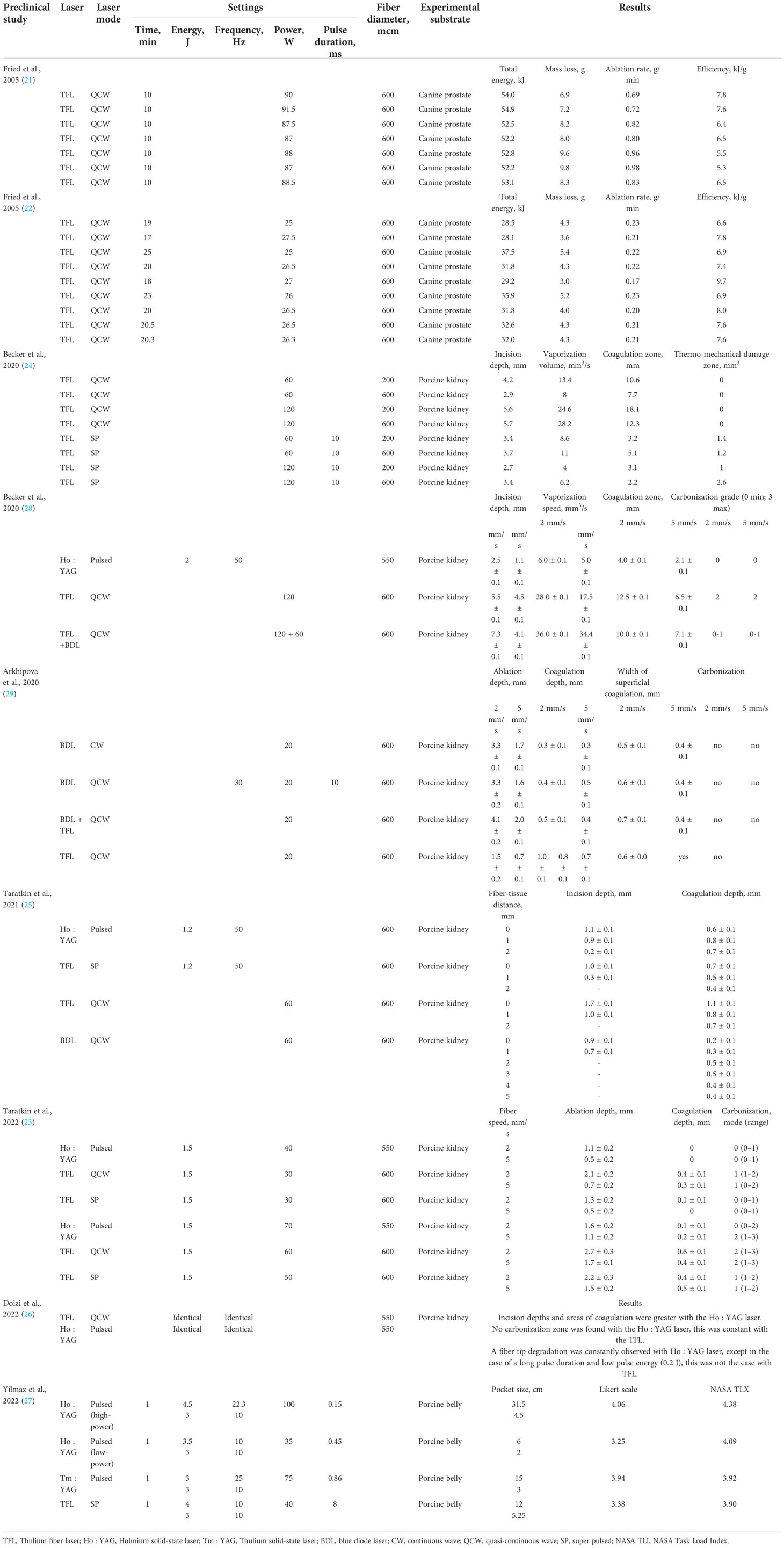
All data on the preclinical studies is collected in Table 1.
Thulium fiber laser for soft tissues: clinical trials
The above-mentioned preclinical studies demonstrated that TFL lends itself to soft tissue surgery for it is efficient at both cutting and coagulation. As a next step, these findings should be backed up with evidence from clinical trials.
A pioneered clinical study for thulium fiber laser enucleation of the prostate (ThuFLEP) was presented by Enikeev et al. on 2018 (30). ThuFLEP’s efficacy (in voiding parameters improvement) and safety (in complication rate) turned out to be in no way inferior to TURP which remains the standard benchmark when it comes to these kind of comparisons. Also, ThuFLEP led to a pronounced prostate-specific antigen (PSA) decrease which implies that there was a more complete removal of the prostate tissue (30).
Compared to a simple prostatectomy in large volume BPH (> 80 cc), ThuFLEP proved to be as equally effective: the mean operative time, resection speed and resected tissue weight were comparable in both procedures (31). After simple prostatectomy, the patients stayed in hospital longer (9.0 days vs 3.3 days, p<0.001). At the 6-month follow-up, the stress urinary incontinence rate was 1,1% after ThuFLEP and 2.5% after simple prostatectomy (31). QCW TFL was successfully applied to different enucleation techniques like en bloc and two-lobe (32). Another study using this laser showed that routine stenting after ureteral orifice damage should not be considered mandatory, largely thanks to its short laser penetration depth (33).
A large retrospective study comparing ThuFLEP, HoLEP and MEP (monopolar enucleation of the prostate) reported no significant differences between those procedures regarding the complications rate at intraoperative, early postoperative period, as well as 6 months after surgery (34). As for the learning curve for these 3 endoscopic enucleation techniques, ThuFLEP was slightly superior (without significant difference [p>0.05]) to HoLEP and MEP in terms of the overall enucleation rate – 1.0 g/min vs. 0.8 g/min and 0.7 g/min, respectively. Also, similar enucleation rates at the initial stages of training (first 20 surgeries) were observed, but after that period laser endoscopic enucleation techniques favored MEP (p<0.001) (35).
Erectile function 6 months post-op after ThuFLEP compared to TURP differed significantly (p < 0.001) (36) favored ThuFLEP: a mean increase of IIEF-5 score in ThuFLEP 0.72 ± 1.6 vs mean decrease in TURP 0.24 ± 2.2. EF after TURP impaired in 34% of patients (18% in patients after ThuFLEP) and it improved in 21% of them (26% after ThuFLEP) (36).. The safety profile for ThuFLEP also was also acceptable with an overall complication rate of 9.7%, Clavien-Dindo grade III complications only in 1.9% of cases (37).
Also, Enikeev et al. compared the severity of irritative symptoms after HoLEP and ThuFLEP (38). No differences in functional outcomes (IPSS, Qmax), rate of SUI or irritative symptoms were found. Both surgeries were comparable in terms of duration and postoperative complication rates (38).
Elmansy et al. (39) compared TFL with Ho : YAG modified with Moses technology in patients with BPH undergoing transurethral enucleation of the prostate. The key differences were in median enucleation, hemostasis, and morcellation times which were longer in TFL group (p < 0.001). Otherwise, there were no significant differences – so, safety and efficacy profile with comparable postoperative outcomes were similar for those lasers (39).
The study of Maltagliati et al. (40) is of great interest because it compared ThuFLEP with Thulium solid-state laser enucleation of the prostate (ThuLEP). The authors reported only one difference between these procedures – the duration of ThuLEP was shorter than the duration of ThuFLEP (63.69 ± 41.44 vs 79.66 ± 48.70 minutes, respectively, p=0.045). Hemoglobin drop (0.47 g/dL after ThuFLEP and 0.45 g/dL after ThuLEP, p=0.32), catheterization time (1.9 vs 2.1 days, p=0.37), hospital stay (2.2 vs 2.6 days, p=0.22), irrigation volume (29.4 vs 32.8 L, p=0.43) and functional parameters (Qmax, IPSS, PVR, and QoL) at 3 months after surgery were comparable between both groups.
BPH surgery aside, TFL proved itself to be a suitable device for en bloc resection of bladder tumor (ERBT), predominantly NMIBC, within a prospective clinical trial (41). It was shown that patients after TFL ERBT had a better relapse-free rate than TURBT at both 3 (97.2% and 84.5%, p = 0.011) and 6 months (91.5% and 67.2%, p < 0.001). Also, TFL ERBT demonstrated a lower complication rate (like obturator nerve reflex, perforation) and better specimen quality compared to conventional TURBT (showing better detrusor rate on pathology). The only reported disadvantage for TFL ERBT was the prolonged surgery duration time (39.0 ( ± 16.5) vs 34.0 ( ± 8.8) min for TURBT) (41).
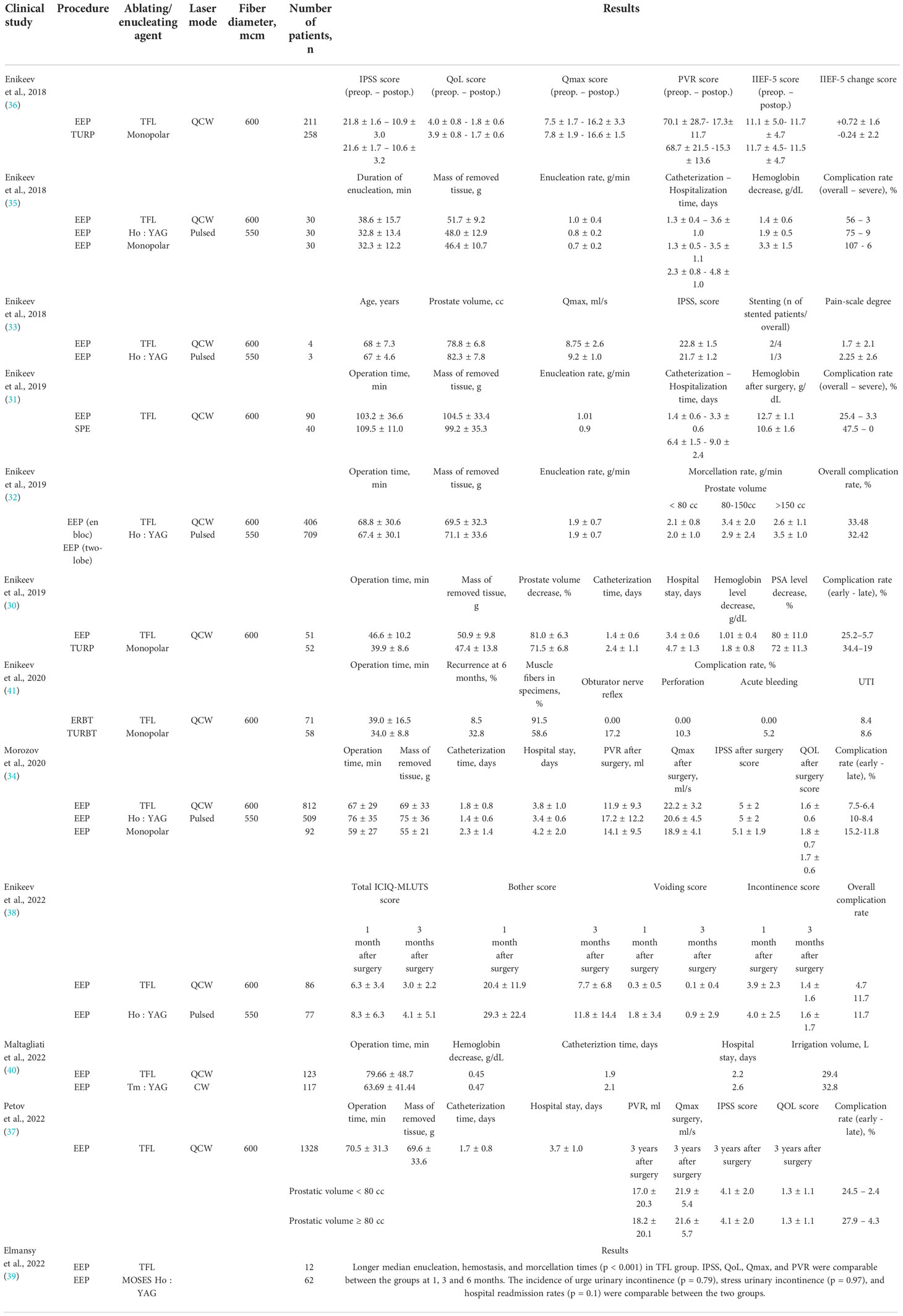
All data on the clinical studies is collected in Table 2.
Discussion
The thulium fiber laser is a novel device which can be applied for both soft tissue cutting and lithotripsy. This laser has 2 modes to complete these tasks – quasi-continuous (QCW) and super pulsed (SP), respectively. QCW is close in properties to Tm : YAG laser, so it can be applied only in soft tissue surgery – for surgical treatment of BPH or NMIBC. It also may be used for UTUC resection/vaporization but there are currently no studies regarding TFL application. SP TFL mode is close in its properties to Ho : YAG laser, so it may be used in both soft tissue and stone surgery.
There are 3 major differences between SP TFL and Ho : YAG. Firstly, SP TFL has a potentially higher frequency (up to 25 – 40 times – 2000 Hz for SP TFL and 50-80 Hz for Ho : YAG) (42). Secondly, its peak power is lower (SP TFL – 500 W, Ho : YAG – 2-10 kW). Thirdly, its pulse duration is longer (TFL: 500 ms; Ho : YAG: 350 at same Energy-Frequency settings) (43). The last difference is determined by different pulse profile – SP TFL has a Gaussian profile while Ho : YAG has a rapidly approaching power peak. In stone surgery those features are associated with lower stone retropulsion and faster soft stone dusting in favor of SP TFL. At the same laser setting, SP TFL and Ho : YAG do not differ in their soft tissue cutting properties – in in vitro studies they were almost the same in terms of ablation depth, coagulation depth and carbonization mode (23, 25). As for clinical practice in BPH surgery, SP TFL may be associated with longer operation time, decreased hemoglobin drop and reduced urinary incontinence rate due to sphincter damage compared to Ho : YAG. Those features may be associated with reduced peak power and increased laser frequency. Unfortunately, we have no data of SP TFL and Ho : YAG clinical comparison in different laser settings.
As for QCW TFL, it has established itself as a effective and safe device for EEP which is not inferior in these terms to Tm : YAG and Ho : YAG. QCW TFL may be safer than Tm : YAG in terms of carbonization – the quasi-continuous mode decreases the thermal damage to tissue reducing carbonization and simplifying the intraoperative navigation (16, 17). Unfortunately, there is no one preclinical comparison of those lasers yet. In a clinical comparison, TFL and Tm : YAG showed themselves to be similar in terms of safety and functional outcomes (40). TFL was associated with longer operation time, which may be caused with decreased vaporization speed. Thus, TFL may have a reduced tissue heating profile compared to Tm : YAG, so insignificant differences in hemoglobin drop and in catheterization or hospitalization time may be signs of its better safety profile. If our assumption is correct, carbonization may also be lower when using TFL. In comparing TFL and pulsed Tm : YAG (27), no significant differences were found. That can be explained by the change of laser pulse generation. Classic Tm : YAG is a continuous wave laser, so it influences the tissue continuously and the tissue heating occurs constantly over time. TFL is a quasi-continuous wave laser – prolonged periods of tissue heating alternate with transient periods of tissue relaxation. So, when Tm : YAG functions as a pulsed laser, the effect on the tissue is directly comparable to those for TFL. This explains the lack of significant differences between these lasers.
In comparison with Ho : YAG, TFL proved to be comparable in terms of efficacy and safety. At the same time, using TFL for EEP was associated with longer operation time, insignificant decrease of complication rate and hemoglobin drop and better functional outcomes. The prolonged operation time may be associated with lower laser tissue penetration depth, absence of explosive vaporization effect and complicated intraoperative navigation due to carbonization. A hemoglobin drop may be associated with better QCW TFL hemostatic properties due to deeper coagulation and the lack of an explosive vaporization effect. The reduced complication rate and the better functional outcomes may be associated with minimized sphincter traumatization due to lower tissue penetration depth and the lack of an explosive vaporization effect. So, TFL may be considered as an effective and safe tool for EEP on a par with Ho : YAG.
As for the difference in learning curves, residents may reach the plateau faster using TFL because of its physical properties. At first, the fact that there was no explosive vaporization makes it easier to dissect along the capsule – that effect would accelerate the operation time but slow down the learning curve. The resident is led to believe that he can do EEP easily, and so he slows down to perfect oneself. This assumption is also supported by the fact that surgeons leave more adenomatous tissue when using Ho : YAG then TFL (35). We assume that gradual and more slow cutting during ThuFLEP may lead to a more predictable dissection. So the resident studying ThuFLEP, begins to identify the prostate capsule and to get into subcapsular layer earlier then resident using other EEP procedures. However, there is no evidence to support these assumptions.
So far we have only discussed the properties of TFL and did not comment on its usability and serviceability. The thulium fiber laser setups are smaller than those for Ho : YAG, so they require less space in the operating theatre. Also TFL laser setups are lighter than those for Ho : YAG which makes it easier to use in theatre. Besides, the TFL setup requires a standard 220V or 110V electrical socket without any conversion. All these features are very useful and convenient for hospital administration because they make less demands on placement in small operation rooms. As for the surgeon’s comfort, Moore et al. determined that TFL produces less noise than Ho : YAG (44). This makes it more pleasant to use TFL and means that surgeons and nurses can easily talk to one another during the procedure (44).
As it stands, TFL is something that urological residents who are just setting out to learn EEP should familiarize themselves with – they are likely to quickly reach an EEP learning curve plateau using TFL compared to other cutting agents. TFL may also be interesting for experienced surgeons who are accustomed to performing EEP or ERBT using thulium solid-state laser (Tm : YAG). TFL could also be used within hospital administration because this laser makes fewer demands on placement in small operation theatres and incorporates two tools – an effective laser for soft tissue cutting and a useful device for stone ablation.
Limitations
Our study has a few limitations. At first, we have not added any data regarding clinical studies laser settings because no relevant data in the original studies were to be found. So, the only data that we had was information about which laser mode was used – SP or QCW. Secondly, we have not found any preclinical studies that compare the effects of TFL with continuous-wave Tm : YAG. Therefore, we cannot compare the vaporization speed and the carbonization mode for those lasers. Yet, we have described in detail the physics of the lasers so that the reader may form easily his or her impression based on the theoretical background. We hope that this makes up for the lack of experimental data.
Conclusions
TFL is a safe and effective tool for BPH surgery. In terms of parameters, it is in no way inferior to Tm : YAG or Ho : YAG during EEP. However, TFL surpasses these lasers in terms of usability and serviceability. These advantages are likely to render it more popular over time.
Author contributions
MT Project development, Systematic search, Data analysis, Manuscript writing EC Project development, Data analysis, Manuscript editing AA Data analysis, Systematic search, Manuscript writing, Tabulation СA Data analysis, Systematic search, Manuscript editing BB Project development, Data analysis, Manuscript editing AM Data analysis, Systematic search, Manuscript writing SP Data analysis, Manuscript editing IB Data analysis, Manuscript editing K-FK Data analysis, Manuscript editing SR Data analysis, Manuscript editing JR Data analysis, Manuscript editing GC Data analysis, Manuscript editing DE Project development, Systematic search, Manuscript editing All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fruro.2022.1017069/full#supplementary-material
References
1. Panthier F, Doizi S, Corrales M, Traxer O. Pulsed lasers and endocorporeal laser lithotripsy. Progres Urol (2021) 31(8–9):451–7. doi: 10.1016/j.purol.2020.11.008
2. Rapisarda S, Russo GI, Osman NI, Chapple CR, Morgia G, Tubaro A, et al. The use of laser as a therapeutic modality as compared to TURP for the small prostate ≤40 mL: a collaborative review. Minerva Urol Nefrol (2019) 71(6):569–75. doi: 10.23736/S0393-2249.19.03350-2
3. Reale G, Marchioni M, Altieri V, Greco F, de Nunzio C, Destefanis P, et al. Operative profile, safety and functional outcomes after GreenLight laser prostate surgery: results from a 12 months follow-up multicenter Italian cohort analyses. Minerva Urol Nefrol (2020) 72(5):622–8. doi: 10.23736/S0393-2249.20.03597-3
4. Bozzini G, Gastaldi C, Besana U, Calori A, Casellato S, Parma P, et al. Thulium-laser retrograde intra renal ablation of upper urinary tract transitional cell carcinoma: an ESUT study. Minerva Urol Nephrol (2021) 73(1):114–21. doi: 10.23736/S2724-6051.20.03689-9
5. Fuschi A, Salhi Y, Velotti G, Capone L, Martoccia A, Suraci PP, et al. Holmium laser enucleation of prostate versus minimally invasive simple prostatectomy for large volume (≥120 mL) prostate glands: a prospective multicenter randomized study. Minerva Urol Nephrol (2021) 73(5):638–48. doi: 10.23736/S2724-6051.20.04043-6
6. Ventimiglia E, Villa L, Doizi S, Briganti A, Proietti S, Giusti G, et al. Laser lithotripsy: The importance of peak power and pulse modulation. Eur Urol Focus (2021) 7(1):22–5. doi: 10.1016/j.euf.2021.01.012
7. Pierre SA, Albala DM. The future of lasers in urology. World J Urol (2007) 25(3):275–83. doi: 10.1007/s00345-007-0185-4
8. Niemz MH. Laser-tissue interactions: fundamentals and applications. Berlin; New York: Springer. (2004) 305
9. Floratos DL, de la Rosette JJMCH. Lasers in urology. BJU Int (1999) 84(2):204–11. doi: 10.1046/j.1464-410x.1999.00163.x
10. Enikeev D, Shariat SF, Taratkin M, Glybochko P. The changing role of lasers in urologic surgery. Curr Opin Urol (2020) 30(1):24–9. doi: 10.1097/MOU.0000000000000695
11. Dołowy Ł, Krajewski W, Dembowski J, Zdrojowy R, Kołodziej A. The role of lasers in modern urology. Cent Eur J Urol (2015) 68(2):175–82. .doi: 10.5173/ceju.2015.537
12. Gross AJ, Orywal AK, Becker B, Netsch C. Five-year outcomes of thulium vapoenucleation of the prostate for symptomatic benign prostatic obstruction. World J Urol (2017) 35(10):1585–93. doi: 10.1007/s00345-017-2034-4
13. Netsch C, Becker B, Tiburtius C, Moritz C, Becci AV, Herrmann TRW, et al. A prospective, randomized trial comparing thulium vapoenucleation with holmium laser enucleation of the prostate for the treatment of symptomatic benign prostatic obstruction: perioperative safety and efficacy. World J Urol (2017) 35(12):1913–21. doi: 10.1007/s00345-017-2071-z
14. Migliari R, Buffardi A, Ghabin H. Thulium laser endoscopic en bloc enucleation of nonmuscle-invasive bladder cancer. J Endourol (2015) 29(11):1258–62. doi: 10.1089/end.2015.0336
15. Liu Z, Long G, Zhang Y, Sun G, Ouyang W, Wang S, et al. Thulium laser resection of bladder tumors vs. conventional transurethral resection of bladder tumors for intermediate and high risk non-Muscle-Invasive bladder cancer followed by intravesical BCG immunotherapy. Front Surg (2021) 8. doi: 10.3389/fsurg.2021.759487
16. Enikeev D, Taratkin M, Azilgareeva C, Glybochko P. Knowing the inside of a laser. Archivos Espanoles Urol (2020) 73(8):665–74.
17. Taratkin M, Azilgareeva C, Cacciamani GE, Enikeev D. Thulium fiber laser in urology: physics made simple. Curr Opin Urol (2022) 32(2):166–72. doi: 10.1097/MOU.0000000000000967
18. Kronenberg P, Traxer O. The laser of the future: reality and expectations about the new thulium fiber laser-a systematic review. Transl Androl Urol (2019) 8(Suppl 4):S398–417. doi: 10.21037/tau.2019.08.01
19. Pal D, das Chowdhury S, Dhar A, Saraf S, Maiti K, DK P, et al. Ex vivo testing of air-cooled CW/modulated 30 W thulium fiber laser for lithotripsy. Appl Opt (2019) 58(25):6720. doi: 10.1364/AO.58.006720
20. Taratkin M, Laukhtina E, Singla N, Tarasov A, Alekseeva T, Enikeev M, et al. How lasers ablate stones: In vitro study of laser lithotripsy (Ho:YAG and Tm-fiber lasers) in different environments. J Endourol (2021) 35(6):931–6. doi: 10.1089/end.2019.0441
21. Fried NM. High-power laser vaporization of the canine prostate using a 110 W thulium fiber laser at 1.91 microm. Lasers Surg Med (2005) 36(1):52–6. doi: 10.1002/lsm.20126
22. Fried NM, Murray KE. High-power thulium fiber laser ablation of urinary tissues at 1.94 microm. J Endourol (2005) 19(1):25–31. doi: 10.1089/end.2005.19.25
23. Taratkin M, Kovalenko A, Laukhtina E, Paramonova N, Spivak L, Wachtendorf LJ, et al. Ex vivo study of Ho:YAG and thulium fiber lasers for soft tissue surgery: which laser for which case? Lasers Med Sci (2022) 37(1):149–54. doi: 10.1007/s10103-020-03189-7
24. Becker B, Enikeev D, Glybochko P, Rapoport L, Taratkin M, Gross AJ, et al. Effect of optical fiber diameter and laser emission mode (cw vs pulse) on tissue damage profile using 1.94 µm tm:fiber lasers in a porcine kidney model. World J Urol (2020) 38(6):1563–8. doi: 10.1007/s00345-019-02944-y
25. Taratkin M, Netsch C, Enikeev D, Gross AJ, Herrmann TRW, Korolev D, et al. The impact of the laser fiber-tissue distance on histological parameters in a porcine kidney model. World J Urol (2021) 39(5):1607–12. doi: 10.1007/s00345-020-03326-5
26. Doizi S, Germain T, Panthier F, Compérat E, Traxer O, Berthe L. Comparison of Holmium:YAG and thulium fiber lasers on soft tissue: An ex vivo study. J Endourol (2022) 36(2):251–8. doi: 10.1089/end.2021.0263
27. Yilmaz M, Esser J, Kraft L, Petzold R, Sigle A, Gratzke C, et al. Experimental ex-vivo performance study comparing a novel, pulsed thulium solid-state laser, chopped thulium fibre laser, low and high-power holmium:YAG laser for endoscopic enucleation of the prostate. World J Urol (2022) 40(2):601–6. doi: 10.1007/s00345-021-03825-z
28. Becker B, Enikeev D, Netsch C, Gross AJ, Laukhtina E, Glybochko P, et al. Comparative analysis of vaporization and coagulation properties of a hybrid laser (Combination of a thulium and blue diode laser) vs thulium and Ho:YAG lasers: Potential applications in endoscopic enucleation of the prostate. J Endourol (2020) 34(8):862–7. doi: 10.1089/end.2020.0009
29. Arkhipova V, Enikeev M, Laukhtina E, Kurkov A, Andreeva V, Yaroslavsky I, et al. Ex vivo and animal study of the blue diode laser, Tm fiber laser, and their combination for laparoscopic partial nephrectomy. Lasers Surg Med (2020) 52(5):437–48. doi: 10.1002/lsm.23158
30. Enikeev D, Netsch C, Rapoport L, Gazimiev M, Laukhtina E, Snurnitsyna O, et al. Novel thulium fiber laser for endoscopic enucleation of the prostate: A prospective comparison with conventional transurethral resection of the prostate. Int J Urol (2019) 26(12):1138–43. doi: 10.1111/iju.14115
31. Enikeev D, Okhunov Z, Rapoport L, Taratkin M, Enikeev M, Snurnitsyna O, et al. Novel thulium fiber laser for enucleation of prostate: A retrospective comparison with open simple prostatectomy. J Endourol (2019) 33(1):16–21. doi: 10.1089/end.2018.0791
32. Enikeev D, Taratkin M, Laukhtina E, Alekseeva T, Snurnitsyna O, Potoldykova N, et al. En bloc and two-lobe techniques for laser endoscopic enucleation of the prostate: retrospective comparative analysis of peri- and postoperative outcomes. Int Urol Nephrol (2019) 51(11):1969–74. doi: 10.1007/s11255-019-02259-2
33. Enikeev D, Glybochko P, Rapoport L, Snurnitsyna O, Potoldykova N, Novoselova T, et al. Need for upper urinary tract stenting in cases of ureteral orifice injury during laser enucleation of the prostate. Int Urol Nephrol (2018) 50(12):2173–7. doi: 10.1007/s11255-018-2007-6
34. Morozov A, Taratkin M, Kozlov V, Tarasov A, Bezrukov E, Enikeev M, et al. Retrospective assessment of endoscopic enucleation of prostate complications: A single-center experience of more than 1400 patients. J Endourol (2020) 34(2):192–7. doi: 10.1089/end.2019.0630
35. Enikeev D, Glybochko P, Rapoport L, Gahan J, Gazimiev M, Spivak L, et al. A randomized trial comparing the learning curve of 3 endoscopic enucleation techniques (HoLEP, ThuFLEP, and MEP) for BPH using mentoring approach-initial results. Urology (2018) 121:51–7. doi: 10.1016/j.urology.2018.06.045
36. Enikeev D, Glybochko P, Rapoport L, Okhunov Z, O’Leary M, Potoldykova N, et al. Impact of endoscopic enucleation of the prostate with thulium fiber laser on the erectile function. BMC Urol (2018) 18(1):87. doi: 10.1186/s12894-018-0400-1
37. Petov V, Babaevskaya D, Taratkin MS, Chuvalov L, Lusuardi L, Misrai V, et al. Thulium fiber laser enucleation of the prostate (ThuFLEP). prospective study of mid- and long-term outcomes in 1328 patients. J Endourol (2022) 36(9):1231–6. doi: 10.1089/end.2022.0029
38. Enikeev D, Taratkin M, Babaevskaya D, Morozov A, Petov V, Sukhanov R, et al. Randomized prospective trial of the severity of irritative symptoms after HoLEP vs ThuFLEP. World J Urol (2022) 40(8):2047–53. doi: 10.1007/s00345-022-04046-8
39. Elmansy H, Hodhod A, Elshafei A, Noureldin YA, Mehrnoush V, Zakaria AS, et al. Comparative analysis of MOSES TM technology versus novel thulium fiber laser (TFL) for transurethral enucleation of the prostate: A single-institutional study. Archivio Italiano di Urol Androl (2022) 94(2):180–5. doi: 10.4081/aiua.2022.2.180
40. Maltagliati M, Berti L, Micali S, Besana U, Buizza C, Rocco B, et al. MP04-16 Thulium yag vs thulium fiber laser enucleation of the prostate (thulep vs tflep): a multi-institution trial to compare intra and early postoperative outcomes. J Urol (2022) 207(Supplement 5):e64. doi: 10.1097/JU.0000000000002521.16
41. Enikeev D, Taratkin M, Margulis V, Sorokin N, Severgina L, Paramonova N, et al. Safety and short-term oncological outcomes of thulium fiber laser en bloc resection of non-Muscle-Invasive bladder cancer: A prospective non-randomized phase II trial. Bladder Cancer (2020) 6(2):201–10. doi: 10.3233/BLC-200275
42. Andreeva V, Vinarov A, Yaroslavsky I, Kovalenko A, Vybornov A, Rapoport L, et al. Preclinical comparison of superpulse thulium fiber laser and a holmium:YAG laser for lithotripsy. World J Urol (2020) 38:497–503. doi: 10.1007/s00345-019-02785-9
43. Ventimiglia E, Doizi S, Kovalenko A, Andreeva V, Traxer O. Effect of temporal pulse shape on urinary stone phantom retropulsion rate and ablation efficiency using holmium:YAG and super-pulse thulium fibre lasers. BJU Int (2020) 126(1):159–67. doi: 10.1111/bju.15079
Keywords: thulium fiber laser (TFL), Ho : YAG (Holmium), lithotripsy, enucleation (EEP), vaporization, lasers, BPH, urolithiasis
Citation: Taratkin M, Checcucci E, Androsov A, Azilgareeva C, Brill B, Morozov A, Puliatti S, Belenchon IR, Kowalewski K-F, Rodler S, Rivas JG, Cacciamani GE and Enikeev D (2022) Thulium fiber laser in BPH surgery: Bench to bedside - a systematic review on behalf of YAU Urotechnology Working Group. Front. Urol. 2:1017069. doi: 10.3389/fruro.2022.1017069
Received: 11 August 2022; Accepted: 28 October 2022;
Published: 24 November 2022.
Edited by:
Jake Patterson, Sheffield Teaching Hospitals NHS Foundation Trust, United KingdomReviewed by:
Vineet Gauhar, National University Hospital, SingaporeBhaskar K. Somani, University of Southampton, United Kingdom
Copyright © 2022 Taratkin, Checcucci, Androsov, Azilgareeva, Brill, Morozov, Puliatti, Belenchon, Kowalewski, Rodler, Rivas, Cacciamani and Enikeev. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dmitry Enikeev, dvenikeev@gmail.com
 Mark Taratkin
Mark Taratkin Enrico Checcucci
Enrico Checcucci Alexander Androsov3
Alexander Androsov3 Andrey Morozov
Andrey Morozov Stefano Puliatti
Stefano Puliatti Ines Rivero Belenchon
Ines Rivero Belenchon Juan Gomez Rivas
Juan Gomez Rivas Giovanni E. Cacciamani
Giovanni E. Cacciamani Dmitry Enikeev
Dmitry Enikeev