- 1Qurtuba University of Science and Information Technology, Peshawar, Pakistan
- 2Abbottabad University of Science and Technology, Abbottabad, Pakistan
- 3Institute of Management Sciences (IMSciences), Peshawar, Pakistan
- 4Department of Industrial Engineering, College of Engineering, King Saud University, Riyadh, Saudi Arabia
- 5Department of Computer Science, Kohat University of Science and Technology, Kohat, Pakistan
- 6School of Information Technology, Deakin University, Burwood, VIC, Australia
A Corrigendum on
An enhanced pattern detection and segmentation of brain tumors in MRI images using deep learning technique
by Kiran, L., Zeb, A., Rehman, Q. N. U., Rahman, T., Shehzad Khan, M., Ahmad, S., Irfan, M., Naeem, M., Huda, S., and Mahmoud, H. (2024). Front. Comput. Neurosci. 18:1418280. doi: 10.3389/fncom.2024.1418280
In the published article, in the Section 3. Materials and methods, 3.1 Dataset of brain MRI images, 10 references and citations were erroneously omitted from the subheadings “CNS Lymphoma,” “Glioblastoma,” “Meningioma,” “Metastases,” “Astrocytoma,” “Pituitary Adenoma,” “Ependymomas,” “Medulloblastomas,” “Oligodendrogliomas,” and “Hemangioblastomas”. The corrected paragraphs with citations included, and a corrected Reference list, appears below:
“CNS Lymphoma: Primary central nervous system Lymphoma is a type of brain tumor that can be primary and secondary; in this type of tumor, cells emerge in the lymphoma and/or the spinal cord region (RMH Neuropathology, 2013).
Glioblastoma: This type of tumor is considered dangerous because it grows fast and spreads quickly inside the brain. Initially, glioblastoma attacks adjacent brain tissues (Gaillard, 2018).
Meningioma: This brain tumor starts inside the brain tissues called meninges that protect the brain and spinal cord. Most meningiomas are not dangerous but can reach up to Grade III tumor levels (Di Muzio, 2023).
Metastases: These types of tumors spread from other parts of the body, such as the lungs, breasts, and kidneys, to the rest of the body. Once they spread to the brain, they can create one or more tumors inside the brain (Brusic, 2021).
Astrocytoma: These tumors can be cancerous or non-cancerous. Some grow very slowly, while others can be aggressive. They appear first in cells called astrocytes (Gaillard, 2021).
Cystic Pituitary Adenoma and Meningioma: They are generally slow-growing types and fall in the benign category of brain tumors, which are mostly considered Grade 1 or Grade II tumors. Most patients with this type of tumor are diagnosed after several years before observing any signs. It develops from pituitary tissues and grows inside the pituitary gland of the brain (Gaillard, 2016).
Ependymomas: This type of brain tumor develops inside the brain or spinal cord area. It can reach Grade 3 from Grade 1. It initially begins in ependymal cells that help to maintain and improve brain streams (Schubert, 2011).
CNS Embryonal Tumor NOS: It is the most common type of brain tumor found in children <3 years of age. By nature, this type of tumor is malignant, and it exists in the area of the cerebellum as a solid mass (Jones, 2021).
Oligodendrogliomas: They emerge around the brain and cortex, the brighter white portion of the brain. They are most commonly considered the middle-aged adult's tumor (Gaillard, 2010).
Hemangioblastomas: They are benign brain tumors that mostly rise around the brain, spinal cord, and behind the eye tissues (retina). They normally occur in young and middle-aged people. (Balachandran, 2010).
In the published article, in Section 3. Materials and methods, 3.1 Dataset of brain MRI images, the title of the paragraphs “Pituitary Adenoma” and “Medulloblastomas” were incorrectly mistyped. The correct titles of the paragraphs should have been “Cystic Pituitary Adenoma and Meningioma” and “CNS Embryonal Tumor NOS” respectively.
In the published article, there was an error in Figure 1 as published, where “Pituitary Adenoma” and “Medulloblastomas” were mislabeled. This should have been “Cystic Pituitary Adenoma and Meningioma” and “CNS Embryonal Tumor NOS” respectively.
The corrected Figure 1 and its caption appear below:
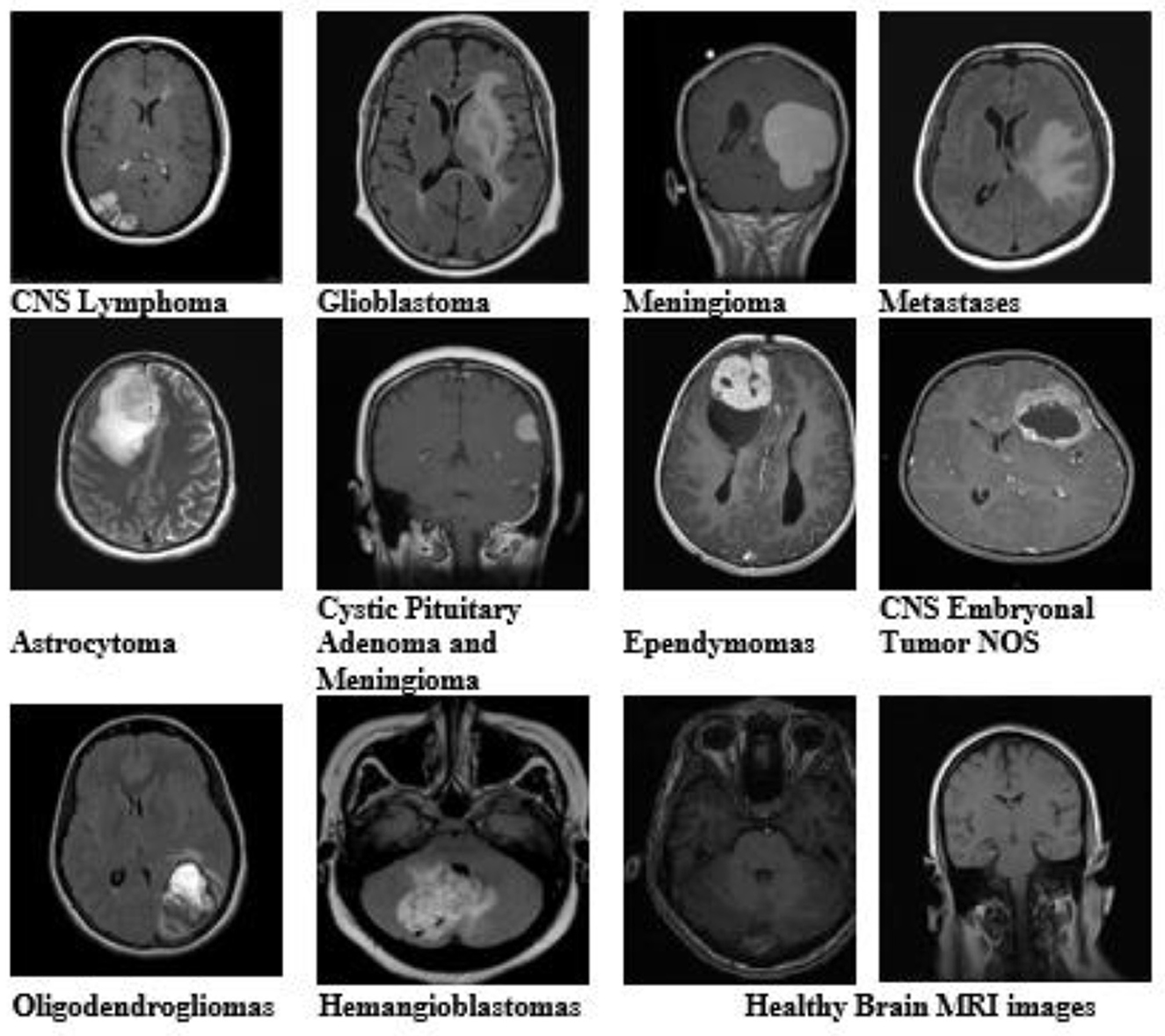
Figure 1. Brain MRI images of all tumor types and healthy brain MRI images from the dataset with different variants and modalities.
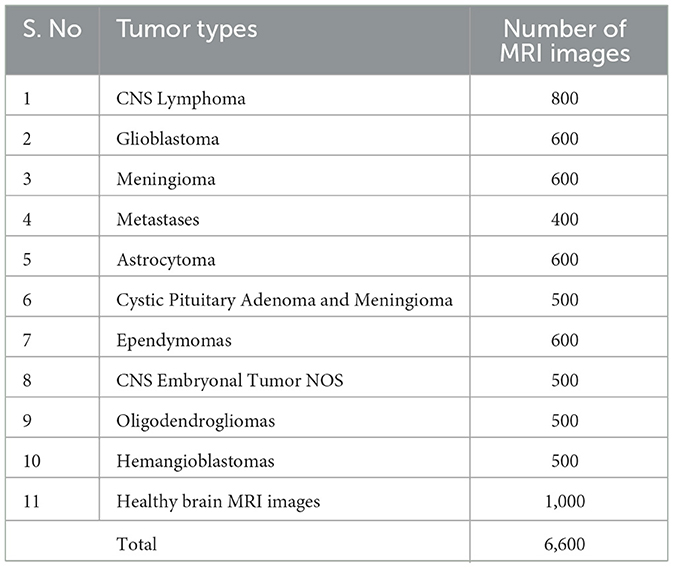
In the published article, there was an error in Table 1 as published, where in the column “Tumor Type” “Pituitary Adenoma” and “Medulloblastomas” were mislabeled. These should have been “Cystic Pituitary Adenoma and Meningioma” and “CNS Embryonal Tumor NOS” respectively.
The corrected Table 1 and its caption appear below:
The authors apologize for these errors and state that they do not change the scientific conclusions of the article in any way. The original article has been updated.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Balachandran, G. (2010). Cerebellar hemangioblastoma. Case study. Radiopaedia.org (accessed July 22, 2023) doi: 10.53347/rID-10779
Brusic, A. (2021). Brain metastases - breast cancer. Case study. Radiopaedia.org (accessed July 22, 2023) doi: 10.53347/rID-88568
Di Muzio, B. (2023). Meningioma. Case study. Radiopaedia.org (accessed July 22, 2023) doi: 10.53347/rID-54380
Gaillard, F. (2010). Glioblastoma NOS - hemorrhagic. Case study. Radiopaedia.org (accessed July 22, 2023) doi: 10.53347/rID-9969
Gaillard, F. (2016). Cystic pituitary adenoma and meningioma. Case study. Radiopaedia.org (accessed July 22, 2023) doi: 10.53347/rID-49382
Gaillard, F. (2018). Glioblastoma. Case study. Radiopaedia.org (accessed July 22, 2023) doi: 10.53347/rID-63888
Gaillard, F. (2021), Astrocytoma. Case study. Radiopaedia.org (accessed July 22, 2023) doi: 10.53347/rID-85660
Jones, J. (2021). CNS Embryonal tumor NOS. Case study. Radiopaedia.org (accessed July 22, 2023) doi: 10.53347/rID-90346
RMH Neuropathology (2013). CNS lymphoma and demyelination. Case study. Radiopaedia.org (accessed July 22, 2023). doi: 10.53347/rID-25592
Keywords: brain tumor, deep learning, pattern detection, neuroscience, segmentation technique, convolution neural network, binary convolution neural network, magnetic resonance images
Citation: Kiran L, Zeb A, Rehman QNU, Rahman T, Shehzad Khan M, Ahmad S, Irfan M, Naeem M, Huda S and Mahmoud H (2025) Corrigendum: An enhanced pattern detection and segmentation of brain tumors in MRI images using deep learning technique. Front. Comput. Neurosci. 19:1570979. doi: 10.3389/fncom.2025.1570979
Received: 04 February 2025; Accepted: 13 February 2025;
Published: 03 June 2025.
Edited and reviewed by: Najib Ben Aoun, Al Baha University, Saudi Arabia
Copyright © 2025 Kiran, Zeb, Rehman, Rahman, Shehzad Khan, Ahmad, Irfan, Naeem, Huda and Mahmoud. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Asim Zeb, YXNpbXplYjFAZ21haWwuY29t
 Lubna Kiran
Lubna Kiran Asim Zeb
Asim Zeb Qazi Nida Ur Rehman
Qazi Nida Ur Rehman Taj Rahman1
Taj Rahman1