- 1Jiujiang City Key Laboratory of Cell Therapy, Department of Oncology, The First Hospital of Jiujiang City, Jiujiang, China
- 2Department of Thoracic Surgery, The First Affiliated Hospital of Xinxiang Medical University, Xinxiang, China
- 3Jiujiang City Key Laboratory of Cell Therapy, Department of Cardiovascular Medicine, The First Hospital of Jiujiang City, Jiujiang, China
- 4Department of Pathology, General Hospital of Central Theater Command of the Chinese People’s Liberation Army, Wuhan, China
- 5Department of Neurosurgery, First Affiliated Hospital of Gannan Medical University, Ganzhou, China
Background: Pulmonary sarcomatoid carcinoma (PSC) is rare among lung malignancies, but it has a high degree of malignancy, and the average survival time for clinically diagnosed patients with PSC is less than 1 year. There are few reports of multiple solid spherical metastases in the lungs of patients with PSC.
Case presentation: This case presents an 80-year-old male with a history of Alzheimer’s disease who was hospitalized due to a frequent dry cough. A 16-slice computed tomography examination of the chest revealed multiple solid, egg-sized lesions with smooth borders in both lungs. Because this type of medical imaging data is very rare in clinical practice, the patient’s diagnosis was initially confusing. Given that the patient had no history of fever and no special abnormalities in the results of laboratory tests, the multidisciplinary team (MDT) suggested that lung metastases or lung malignancies with intrapulmonary metastasis should be considered. A magnetic resonance imaging (MRI) examination of the head was performed and revealed brain metastatic lesion. Finally, a puncture biopsy of the lung lesion was performed under ultrasound guidance. The case results confirmed PSC.
Conclusion: This case presents a very rare medical imaging dataset of solid lesions with multiple egg-sized having smooth borders in both lungs. This special medical imaging data highlights the variability of PSC imaging and the complexity of accurate diagnosis, aiming to improve the understanding of PSC.
Introduction
Multiple solid lesions in both lungs can present a diagnostic challenge due to their rarity and the broad differential diagnoses they encompass (1–3). These lesions may represent a variety of pathologies, including metastatic disease, multiple primary lung cancers, infectious processes, or benign conditions. For example, tuberculosis and non-tuberculous infectious lesions can appear as solid lung nodules or masses. Understanding the underlying cause is crucial for determining the appropriate management and prognosis. Currently, the presence of multiple solid lesions in both lungs necessitate a thorough diagnostic workup, including imaging studies and possibly histopathological examination, to identify the underlying cause and guide appropriate treatment strategies. Previous reports have shown multiple metastases in the lungs of patients with pulmonary sarcomatoid carcinoma (PSC) (4). However, there are no published reports on PSC that include a medical imaging dataset of solid lesions with multiple egg-sized nodules having smooth borders in both lungs. This case presents an 80-year-old male with this very rare medical imaging dataset.
Case report
An 80-year-old male was hospitalized with an irritating dry cough that had persisted for 2 weeks. This cough was unaffected by temperature and pungent odors. The patient was generally in good health except for Alzheimer’s disease. His Alzheimer’s disease mainly manifested as forgetfulness, dementia, and lethargy, but he believed that he could take care of himself. Consequently, he refused medication for Alzheimer’s. The patient and his companion denied that he had asthma, chronic obstructive pulmonary disease, or gastroesophageal reflux disease. He did not exhibit any signs of distress or chest discomfort and was able to climb four flights of stairs without requiring rest. He recently denied having a fever, obvious night sweats, low-grade fever, skin-related abnormalities, diarrhea, or edema in his lower extremities. Meanwhile, he also stated that he had no sputum production, chest tightness, dyspnea, night sweats, cyanosis, or clubbing of the fingers. The patient is currently eating normally, and his food intake has not changed significantly in the past 10 years. However, he has lost about 3 kg in the last 3 months. The patient has been smoking for more than 60 years and has not quit, with a daily average of 20 cigarettes. He has 5 years of prior work experience with asbestos exposure. According to the patient’s companion, the chest X-ray examination conducted after the end of that work did not show significant abnormalities. The patient has no history of pet ownership or unclean sexual contact. His professional occupation was not related to any special exposure or radiation exposure, and he reported no alcohol consumption, illicit drug use, or recent travel.
His physical examination found no obvious bilateral swelling of the supraclavicular lymph nodes, slightly weak bilateral lung breath sounds, scattered wet rales, and pleural friction rubs. He underwent a chest and abdomen computed tomography examination, which revealed multiple solid, egg-sized lesions with smooth borders in both lungs (Figures 1A,B). His laboratory results (complete blood cell count, liver panel, kidney panel, tumor marker) were within normal limits, and his lung function tests were also within normal limits.
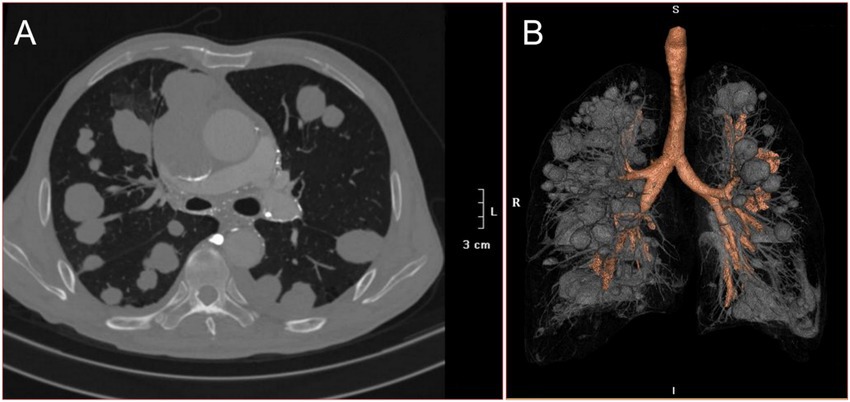
Figure 1. 16-slice computerized tomography images of the chest with the patient at admission. (A) Horizontal planes. (B) Three dimensional reconstruction.
Because this type of medical imaging data is very rare in clinical practice, the patient’s diagnosis was initially confusing. One potential cause of multiple solid lesions in the lungs is synchronous multiple primary non-small cell lung cancer (SMPNSCLC). Another possible cause of multiple solid lesions in the lungs is intrapulmonary metastases, such as those from osteosarcoma. In addition to metastatic and primary lung cancers, infectious diseases can also present as multiple solid lesions in the lungs. For example, tuberculosis and invasive candidiasis can manifest as multiple pulmonary lesions.
Given that the patient had no history of fever and no special abnormalities in the results of laboratory tests, the multidisciplinary team (MDT) suggested that lung metastases or lung malignancies with intrapulmonary metastasis should be considered. A magnetic resonance imaging (MRI) examination of the head was performed and revealed brain metastatic lesion (Figures 2A,B). Unfortunately, due to financial constraints, the patient did not undergo the PET-CT examination. At the same time, he underwent gastroscopy and colonoscopy because of concerns about weight loss, but no tumor was found. Finally, a puncture biopsy of the lung lesion was performed under ultrasound guidance, and the histologic results confirmed PSC with giant-cell carcinoma (Figures 3A–C), PD-L1 (=1%, Clone: 22C3, Dako, Agilent Technologies, Inc.).
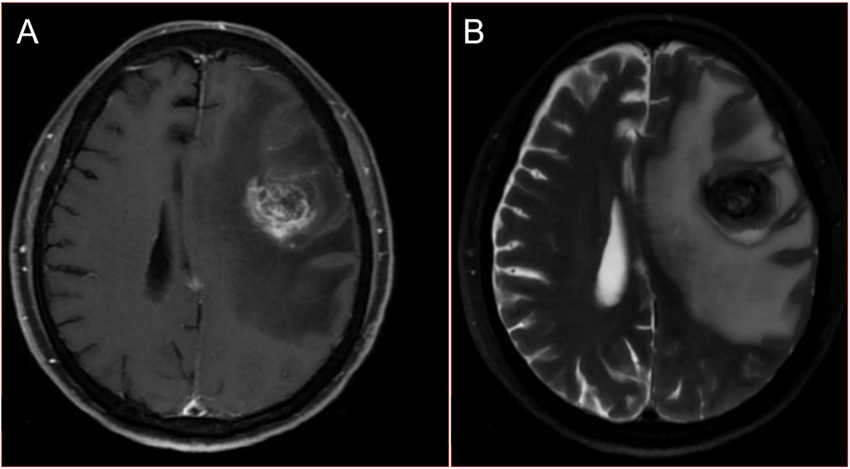
Figure 2. Magnetic resonance images of the head with the patient at admission. (A) Contrast enhanced T1WI. (B) T2WI.
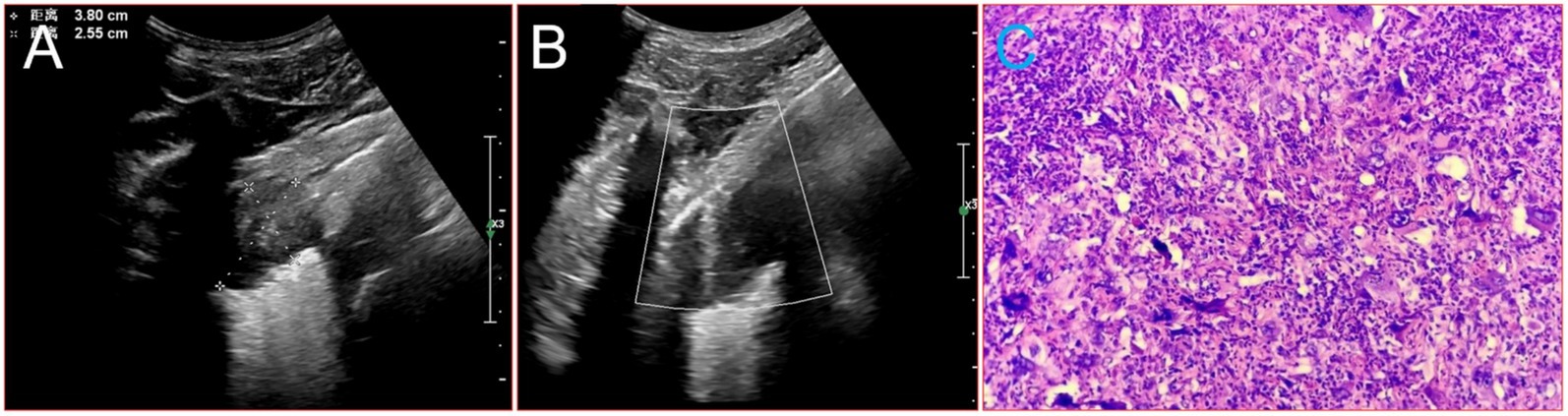
Figure 3. Image about puncture biopsy of the lung lesion under ultrasound guidance, and the histologic results. (A) Ultrasound images of the lesion in the patient’s lower lobe of the left lung. (B) The process of puncture biopsy of the lung lesion under ultrasound guidance. (C) HE × 20.
The actionability of genomic alterations and the level of evidence were determined based on the OncoKB dataset. Drug approval status in mainland China revealed no mutated genes such as EGFR (Exons 18/19/20/21/T790), FGFR2, FGFR3, ROS1, PIK3CA (Exons 10/12, coding exons 9/20), KRAS (Codons 12/13/61/146), TP53, RET, ALK, NRAS (Codons 12/13/61), and KIT (Exons 9/11). Genetic testing was conducted in a CLIA-certified lab using hybridization capture-based next-generation sequencing panels. Gene targets included those from MyGene, BGI-Shenzhen (Headquarters: Shenzhen, 518083, China). The genomic alterations assessed included single nucleotide variations, insertions and deletions, copy number variations, and gene rearrangements in selected genes. The MyGene panels covered common lung cancer-related genes, with a minimum coverage across samples of ≥1,000×.
He received a diagnosis of stage IVb PSC, cT4N3M1, with a negative EGFR status (as per the ninth edition TNM classification, the presence of numerous lesions in the same lung lobe is classified as T4, while the presence of nodules in the opposite lung lobe and multiple metastases in distant organs is categorized as M1. Additionally, the presence of bilateral hilar and mediastinal lymphadenopathy is classified as N3). He received recombinant human endostatin (Endostar, days 1–14: 7.5 mg/m2 every day) combined with pemetrexed (250 mg/m2 on day 1) and cisplatin (15 mg/m2, daily from days 1 to 3). During this treatment, the patient experienced some common side effects, such as nausea, fatigue, infections, vomiting, decreased appetite, decreased red blood cell count, decreased platelet count, and decreases in the components of white blood cells, which were successfully alleviated with conventional methods. After two cycles of chemotherapy, there was no significant improvement in his symptoms. Reexamination of the head MRI showed that the metastatic tumor had become smaller (Figures 4A,B), but the chest X-ray showed no significant improvement in the lung lesions. Then he encountered a new wave of the COVID-19 pandemic. When he was taken to the hospital after being infected, his face was blue, and he had severe breathing difficulties. A blood oxygen saturation test showed that his peripheral blood oxygen saturation was only 72%. The doctor recommended ventilator treatment with endotracheal intubation, but the patient’s family refused to allow it, citing the patient’s prior wishes. Unfortunately, he died that day. His family refused further autopsy.
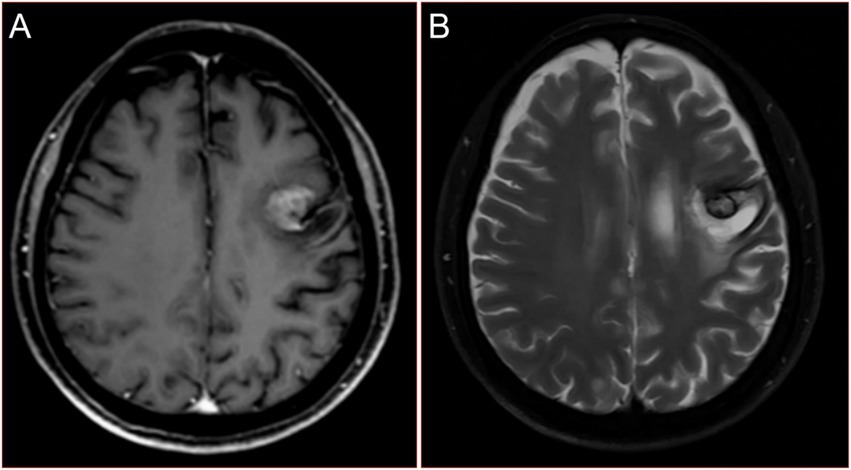
Figure 4. Reexamination magnetic resonance images of the head after chemotherapy of reexamination of the patient. (A) Contrast enhanced T1WI. (B) T2WI.
Discussion
PSC is indeed a rare and aggressive subtype of non-small cell lung cancer (NSCLC) that poses significant challenges in imaging diagnosis due to its rarity and the overlap of its morphological features (5, 6). Imaging diagnosis of lung lesion(s) diseases, including artificial intelligence assistance, is difficult to obtain satisfactory accuracy (7). Multiple lesions in lung includes lumpy lesions, nodular lesions and miliary lesions.
Lumpy lesions characterized by several or uncountable discrete pulmonary mass lesions, most were solid lesions, usually larger than 3 cm in diameter, and with or without cavity formation. It can often be associated with metastatic diseases, such as gastrointestinal stromal tumors (GISTs), which are known to metastasize to the lungs, albeit infrequently (8). Other include sarcomatous lung metastasis and malignant melanoma lung metastasis (9, 10), etc. In a few cases, synchronous multiple primary lung cancers, infectious or inflammatory processes can also exhibit this form (11–13).
Nodular lesions are another common form of pulmonary abnormality characterized by uncountable discrete pulmonary nodules lesions usually, most were ground-glass opacity lesions, the diameter varies from 0.5 cm to 3 cm, and accompanied or accompanied by a burr sign. It can be indicative of a range of conditions, from benign to malignant. In this context, two particular diseases deserve attention, primary pulmonary lymphoma and pulmonary cryptococcosis (14, 15). Primary pulmonary lymphoma, which can coexist with other benign lesions such as hamartomas (14). This rare occurrence can mimic invasive pulmonary mycosis, making accurate diagnosis challenging (15). Additionally, benign metastasizing leiomyoma (BML) and pulmonary metastasis can present as multiple nodules in the lungs also (16, 17).
Miliary lesions, characterized by uncountable discrete pulmonary micronodules, generally tiny and uniform in size (≤5 mm) and diffusely distributed throughout the lungs, can represent a wide variety of pathologies, including but not limited to tuberculosis (TB), sarcoidosis, histoplasmosis, coccidioidomycosis, silicosis, malignancies (thyroid, renal, prostate, and breast cancer), etc. In endemic areas, TB is a major cause of miliary nodules (18–21). As the presence of multiple lesions in lung patterns on radiological images is not specific, the final diagnosis cannot be established without a tissue biopsy.
This type of carcinoma is characterized by its poor prognosis and resistance to conventional treatments, making it a subject of ongoing research and clinical interest (22–25). Due to its rarity and aggressive nature, the treatment options for PSC are limited and often result in suboptimal outcomes. However, recent advancements in targeted therapies and immunotherapies have shown promise in improving the prognosis for patients with PSC. Studies have shown that PSC often expresses high levels of PD-L1, making it a potential candidate for treatment with PD-1/PD-L1 inhibitors (26–28). In addition to immunotherapy, targeted therapies have also been explored for PSC. The presence of MET exon 14 skipping mutations in some PSC patients provides an opportunity for targeted treatment (28). Furthermore, the identification of novel genetic alterations, such as the PHF20-NTRK1 fusion, in PSC patients opens up possibilities for targeted treatment with NTRK1 inhibitors, which could potentially improve outcomes for patients with these specific genetic profiles (29). Despite these advancements, the overall prognosis for PSC remains poor, and there is a need for further research to develop more effective treatment strategies (30). The combination of immunotherapy with other treatment modalities, such as radiotherapy, has shown potential in enhancing treatment efficacy and warrants further investigation (31).
In conclusion, there are no published reports on PSC with multiple synchronous lung and brain metastases, this case presents a very rare medical imaging dataset of solid lesions with multiple egg-sized having smooth borders in both lungs. This special medical imaging data highlights the variability of PSC imaging and the complexity of accurate diagnosis, aiming to stimulate discussion of the disease, and to gain more attention for targeted diagnosis and treatment.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
Q-LL: Data curation, Formal analysis, Writing – original draft. KC: Investigation, Methodology, Resources, Validation, Writing – original draft. J-DC: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YZ: Formal analysis, Investigation, Methodology, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. B-MG: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Li, J, Yang, X, Xia, T, Guan, Y, and Zhong, N. Stage I synchronous multiple primary non-small cell lung cancer: CT findings and the effect of TNM staging with the 7th and 8th editions on prognosis. J Thorac Dis. (2017) 9:5335–44. doi: 10.21037/jtd.2017.12.101
2. Liu, J, Mao, G, Li, Y, Tao, L, Wang, W, Peng, X, et al. Targeted deep sequencing helps distinguish independent primary tumors from intrapulmonary metastasis for lung cancer diagnosis. J Cancer Res Clin Oncol. (2020) 146:2359–67. doi: 10.1007/s00432-020-03227-5
3. Zhu, J, Xu, Y, Huang, WC, Ji, T, Ai, GP, and Gao, YH. Case Report: Recombinant human endostatin plus chemotherapy for epidermal growth factor receptor-negative miliary lung adenocarcinoma. Front Oncol. (2022) 12:922076. doi: 10.3389/fonc.2022.922076
4. Gu, L, Xu, Y, Chen, Z, Pan, Y, and Lu, S. Clinical analysis of 95 cases of pulmonary sarcomatoid carcinoma. Biomed Pharmacother. (2015) 76:134–40. doi: 10.1016/j.biopha.2015.10.009
5. Wang, L, Zhang, J, Chen, X, Liang, M, Li, S, Zhou, W, et al. Pulmonary sarcomatoid carcinoma mimicking pleural mesothelioma: a case report. Medicine. (2021) 100:e27813. doi: 10.1097/MD.0000000000027813
6. Wu, XY, Ding, F, Li, K, Huang, WC, Zhang, Y, and Zhu, J. Analysis of the causes of solitary pulmonary nodule misdiagnosed as lung cancer by using artificial intelligence: a retrospective study at a single center. Diagnostics. (2022) 12:2218. doi: 10.3390/diagnostics12092218
7. Marchiori, E, Zanetti, G, Barreto, MM, de Andrade, FT, and Rodrigues, RS. Atypical distribution of small nodules on high resolution CT studies: patterns and differentials. Respir Med. (2011) 105:1263–7. doi: 10.1016/j.rmed.2011.02.010
8. Nannini, M, Biasco, G, Di Scioscio, V, Di Battista, M, Zompatori, M, Catena, F, et al. Clinical, radiological and biological features of lung metastases in gastrointestinal stromal tumors (case reports). Oncol Rep. (2011) 25:113–20.
9. Choi, YJ, Jung, MH, Park, YK, Lee, BY, and Huh, CY. Uterine müllerian adenosarcoma with sarcomatous overgrowth and lung metastasis in a 25-year-old woman. Eur J Gynaecol Oncol. (2011) 32:91–4.
10. Smyth, EC, Hsu, M, Panageas, KS, and Chapman, PB. Histology and outcomes of newly detected lung lesions in melanoma patients. Ann Oncol. (2012) 23:577–82. doi: 10.1093/annonc/mdr364
11. Qu, R, Tu, D, Ping, W, Cai, Y, Zhang, N, and Fu, X. Surgical outcomes of one-stage resection for synchronous multiple primary lung adenocarcinomas with no less than three lesions. J Cardiothorac Surg. (2021) 16:265. doi: 10.1186/s13019-021-01647-z
12. Zhu, J, Huang, WC, Huang, B, Zhu, Y, Jiang, XJ, Zou, JN, et al. Clinical characteristics and prognosis of COVID-19 patients with initial presentation of lung lesions confined to a single pulmonary lobe. Am J Transl Res. (2020) 12:7501–9.
13. Wu, J, Wu, X, Zeng, W, Guo, D, Fang, Z, Chen, L, et al. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Investig Radiol. (2020) 55:257–61. doi: 10.1097/RLI.0000000000000670
14. Chen, Y, Li, LQ, Ge, YL, Xie, BX, Li, WQ, Jing, Q, et al. A rare case of benign hamartoma and malignant primary pulmonary lymphoma coexisting in a patient mimicking invasive pulmonary mycosis: a case report and literature review. Clin Lab. (2021) 67. doi: 10.7754/Clin.Lab.2020.200646
15. Wang, D, Wu, C, Gao, J, Zhao, S, Ma, X, Wei, B, et al. Comparative study of primary pulmonary cryptococcosis with multiple nodules or masses by CT and pathology. Exp Ther Med. (2018) 16:4437–44. doi: 10.3892/etm.2018.6745
16. Lee, SR, Choi, YI, Lee, SJ, Shim, SS, Lee, JH, Kim, YK, et al. Multiple cavitating pulmonary nodules: rare manifestation of benign metastatic leiomyoma. J Thorac Dis. (2017) 9:E1–5. doi: 10.21037/jtd.2016.11.112
17. Imokawa, S, Uehara, M, Uto, T, Sagisaka, S, Sato, J, Yasuda, K, et al. Pulmonary metastasis from urothelial carcinoma showing progressive multiple cystic lesions. Am J Respir Crit Care Med. (2013) 188:1267–8. doi: 10.1164/rccm.201305-0887LE
18. Andreu, J, Mauleón, S, Pallisa, E, Majó, J, Martinez-Rodriguez, M, and Cáceres, J. Miliary lung disease revisited. Curr Probl Diagn Radiol. (2002) 31:189–97. doi: 10.1067/mdr.2002.127634
19. Zhang, Y, Chen, Y, Li, K, Jiang, W, and Zhang, BC. Artificial intelligence system application in miliary lung metastasis: experience from a rare case. Risk Manag Healthc Policy. (2021) 14:2825–9. doi: 10.2147/RMHP.S315152
20. Matsuura, S, Mochizuka, Y, Oishi, K, Miyashita, K, Naoi, H, Mochizuki, E, et al. Sarcoidosis with pancreatic mass, endobronchial nodules, and miliary opacities in the lung. Intern Med. (2017) 56:3083–7. doi: 10.2169/internalmedicine.8916-17
21. Ani, AMMA, Darweesh, A, Almashhadani, MAA, Babiker, I, and Abdelrahman, A. Lung adenocarcinoma presenting as miliary lung metastasis on imaging. Radiol Case Rep. (2024) 19:4702–7. doi: 10.1016/j.radcr.2024.07.024
22. Chen, P, Yu, M, Zhang, JL, Chen, WY, Zhu, L, Song, Y, et al. Significant benefits of pembrolizumab in treating refractory advanced pulmonary sarcomatoid carcinoma: a case report. World J Clin Cases. (2020) 8:2876–84. doi: 10.12998/wjcc.v8.i13.2876
23. Su, C, Wang, Y, Zhu, X, and Zhang, J. Recurrence of pulmonary sarcomatoid carcinoma presenting as haemothorax: a case report. J Int Med Res. (2023) 51:3000605231213533. doi: 10.1177/03000605231213533
24. Devkota, A, Paudel, A, Sapkota, S, Pandit, S, and Baniya, A. Case report: pulmonary sarcomatoid carcinoma in a female patient from Nepal. F1000Res. (2021) 10:723. doi: 10.12688/f1000research.55187.1
25. Gao, C, Zou, Q, and Liu, H. Pulmonary sarcomatoid carcinoma with epiglottis and ileum metastasis detected by 18F-FDG PET/CT. Clin Nucl Med. (2022) 47:231–3. doi: 10.1097/RLU.0000000000003936
26. Roesel, C, Kambartel, K, Kopeika, U, Berzins, A, Voshaar, T, and Krbek, T. Lazarus-type tumour response to therapy with nivolumab for sarcomatoid carcinomas of the lung. Curr Oncol. (2019) 26:270–e273. doi: 10.3747/co.26.4377
27. Wu, S, Wu, S, Liao, X, Zhou, C, Qiu, F, Wang, C, et al. Pembrolizumab combined with anlotinib improves therapeutic efficacy in pulmonary sarcomatoid carcinoma with TMB-H and PD-L1 expression: a case report and literature review. Front Immunol. (2023) 14:1274937. doi: 10.3389/fimmu.2023.1274937
28. Yu, Y, Zhang, Q, Zhang, J, and Lu, S. Prevalence of MET exon 14 skipping mutation in pulmonary sarcomatoid carcinoma patients without common targetable mutations: a single-institute study. J Cancer Res Ther. (2019) 15:909–13. doi: 10.4103/jcrt.JCRT_591_18
29. Ge, J, Yao, B, Huang, J, Wu, X, Bao, H, Ou, Q, et al. Molecular genetic characterization reveals linear tumor evolution in a pulmonary sarcomatoid carcinomas patient with a novel PHF20-NTRK1 fusion: a case report. BMC Cancer. (2019) 19:592. doi: 10.1186/s12885-019-5780-4
30. Jiao, Y, Liu, M, Luo, N, Guo, H, and Li, J. Successful treatment of advanced pulmonary sarcomatoid carcinoma with the PD-1 inhibitor toripalimab: a case report. Oral Oncol. (2021) 112:104992. doi: 10.1016/j.oraloncology.2020.104992
31. Manzotti, G, Torricelli, F, Benedetta, D, Lococo, F, Sancisi, V, Rossi, G, et al. An epithelial-to-mesenchymal transcriptional switch triggers evolution of pulmonary sarcomatoid carcinoma (PSC) and identifies dasatinib as new therapeutic option. Clin Cancer Res. (2019) 25:2348–60. doi: 10.1158/1078-0432.CCR-18-2364
Keywords: multiple masses, sarcomatoid carcinoma, metastases, lung cancer, differential diagnosis
Citation: Liu Q-L, Cao K, Cao J-D, Zhang Y and Guo B-M (2025) Case Report: Cracking the case: unique presentation of pulmonary sarcomatoid carcinoma with spherical lung metastases. Front. Med. 12:1567046. doi: 10.3389/fmed.2025.1567046
Edited by:
Carmelo Caldarella, Fondazione Policlinico Universitario A. Gemelli IRCCS, ItalyReviewed by:
Apurva Patel, Gujarat Cancer & Research Institute, IndiaMehmet Ali Bedirhan, Yedikule Teaching Hospital, Türkiye
Copyright © 2025 Liu, Cao, Cao, Zhang and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu Zhang, eXVjaHUyMDIzMDBAMTYzLmNvbQ==; Bang-Ming Guo, Z3lnYm0yOUAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Qiu-Lian Liu1†
Qiu-Lian Liu1† Bang-Ming Guo
Bang-Ming Guo