- 1Charité-Universitätsmedizin Berlin, Department of Psychiatry and Psychotherapy, CCM, Mind and Brain Research, Berlin, Germany
- 2Independent Researcher, Maastricht, Netherlands
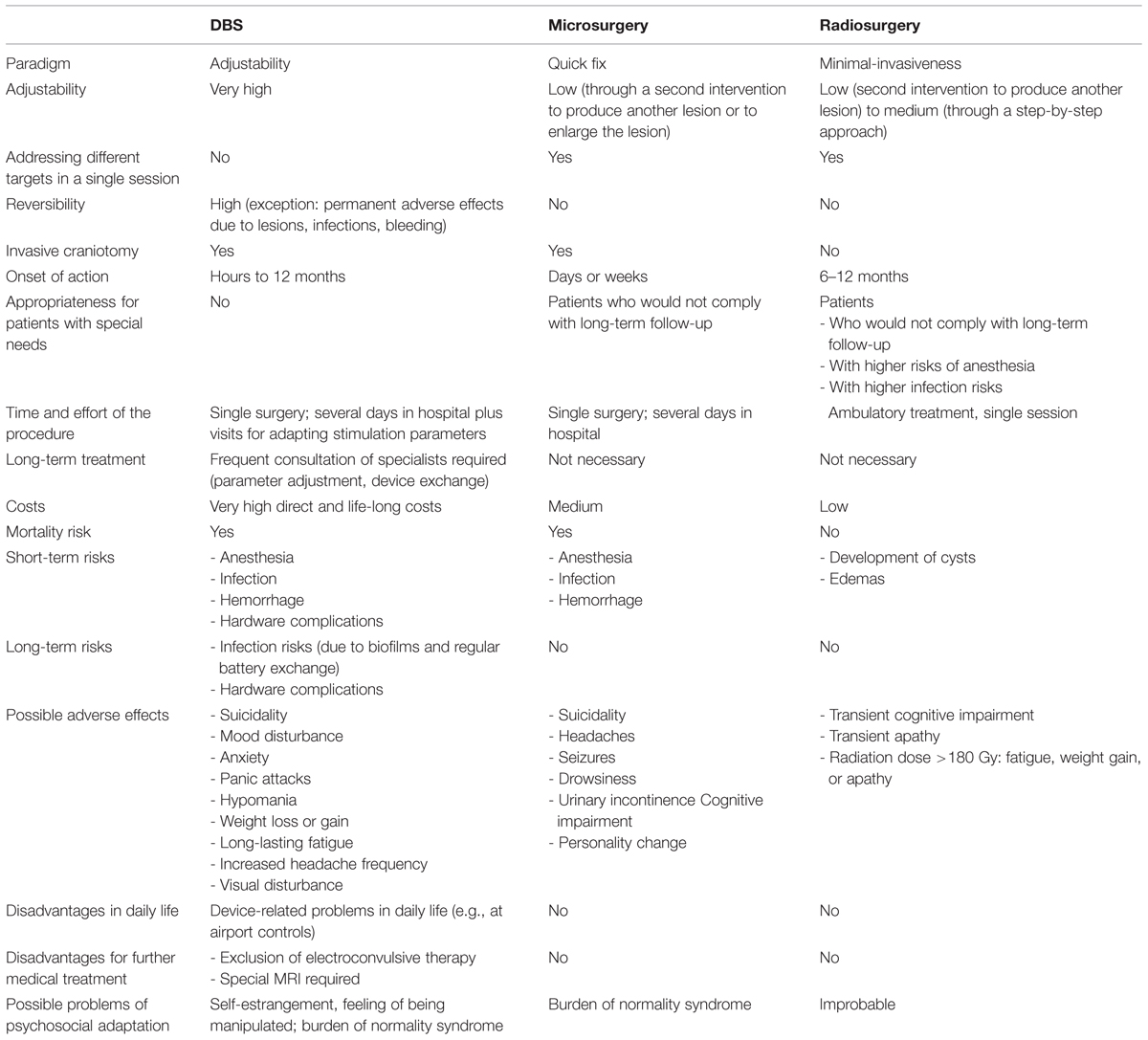
In the wake of deep brain stimulation (DBS) development, ablative neurosurgical procedures are seeing a comeback, although they had been discredited and nearly completely abandoned in the 1970s because of their unethical practice. Modern stereotactic ablative procedures as thermal or radiofrequency ablation, and particularly radiosurgery (e.g., Gamma Knife) are much safer than the historical procedures, so that a re-evaluation of this technique is required. The different approaches of modern psychiatric neurosurgery refer to different paradigms: microsurgical ablative procedures is based on the paradigm ‘quick fix,’ radiosurgery on the paradigm ‘minimal-invasiveness,’ and DBS on the paradigm ‘adjustability.’ From a mere medical perspective, none of the procedures is absolutely superior; rather, they have different profiles of advantages and disadvantages. Therefore, individual factors are crucial in decision-making, particularly the patients’ social situation, individual preferences, and individual attitudes. The different approaches are not only rivals, but also enriching mutually. DBS is preferable for exploring new targets, which may become candidates for ablative microsurgery or radiosurgery.
Introduction
Since 2000, there is a renaissance of neurosurgical treatments of psychiatric disorders. Many researchers and clinicians hope that modern neurosurgical approaches will be established as treatment options for a growing number of therapy-refractory psychiatric disorders. About 90% of functional neurosurgeons feel optimistic about the future of psychiatric neurosurgery (Lipsman et al., 2011; Mendelsohn et al., 2013).
Modern psychiatric neurosurgery includes DBS and ablative neurosurgical procedures (thermal or radiofrequency ablation, and radiosurgery). DBS and thermal or radiofrequency ablation procedures require a craniotomy. Radiosurgery (Gamma Knife Radiosurgery) is performed without craniotomy, mostly as an ambulant treatment. In future, high intensity focused ultrasound might become another option. The worldwide first four patients have been treated with this technique in South Korea (Na et al., 2015).
Many authors consider DBS as the most modern and superior technology, particularly because of its adjustability and high degree of reversibility. However, in the wake of DBS development, ablative neurosurgical procedures are seeing a comeback, although they had been discredited and nearly completely abandoned in the 1970s because of their frequent serious complications and their unethical practice. Since modern stereotactic ablative procedures, particularly radiosurgery are much safer and more efficient than their historical antecessors, a re-evaluation of this technique is required.
Until now, ethical discussion about non-DBS psychiatric neurosurgery is scarce, whereas psychiatric DBS is intensively discussed ethically. This blind spot in neuroethics is astonishing for several reasons: First, the fraction of ablative procedures in psychiatric neurosurgery is big: in North America, 50% of psychiatric neurosurgeons use lesioning exclusively or combined with DBS (Lipsman et al., 2011); outside of North America even 54.9% (Mendelsohn et al., 2013). Second, two expert panels have affirmed stereotactic ablative procedures as important alternatives for appropriately selected patients (Parkinsonism: Bronstein et al., 2011; psychiatric disorders: Nuttin et al., 2014). Third, a clear superiority of any procedure in all relevant aspects cannot be established. Forth, which approach is optimal, depends significantly on patients’ individual medical and non-medical properties. Fifth, the much higher costs of DBS, particularly for long-term treatment, exclude this option for the majority of patients world-wide.
Therefore, a comprehensive ethical analysis of the pros and cons of the different approaches is necessary, based on clinical facts, not on ideological prejudices. Particularly, it is not justified to characterize modern lesioning procedures as successors of historical psychosurgery, while presenting DBS as something quite different. In fact, both psychiatric DBS and modern ablative psychiatric neurosurgery are significantly improved successors of the historical psychosurgery.
Different Paradigms
The different approaches of modern psychiatric neurosurgery refer to different paradigms: microsurgical ablative procedures is based on the paradigm ‘quick fix,’ radiosurgery on the paradigm ‘minimal-invasiveness,’ and DBS on the paradigm ‘adjustability.’
The purpose of ablative microsurgical procedures is to disconnect limbic system circuits related to different psychiatric disorders in order to enhance brain function and reduce psychiatric symptoms (Martinez-Alvarez, 2015).
Radiosurgery is usually considered as an ablative treatment. However, recent neurophysiological, radiological, and histological studies challenge this view. Radiosurgical protocols for neurological or psychiatric disorders might have differential effects on various neuronal populations and remodel the glial environment, leading to a modulation of function while preserving basic processing. Thus, modern functional radiosurgery might be based on neuromodulatory effects (Régis, 2013).
DBS has been considered as a method to produce reversible lesions. Indeed, high-frequency DBS has a similar effect as lesions, i.e., inhibition of targets that are hyperactive in psychiatric disorders. However, its mechanism of action is unclear, and several hypotheses have been put forward to explain the blocking effect of stimulation (Lévèque, 2014). Its main advantage is that the stimulation effect can be adjusted by adapting the stimulation parameters.
Efficacy
A direct comparison of the efficacy of the different approaches is not yet possible, particularly because of the heterogeneity of the studies, the small patient numbers, and the fact that most studies are neither placebo-controlled nor double-blind. The rapid development of the methods aggravates their comparison: In psychiatric DBS, many targets (mostly overlapping for different diagnoses) are tested with different stimulation parameters. In radiosurgery, the radiation doses used decreased significantly. Randomized controlled trials would be optimal to directly compare the efficacy of the different approaches. However, this scientific standard cannot be met for practical and ethical reasons. Nevertheless, studies that directly compare different approaches with matched patients would also provide a valid efficacy comparison. In any case, this would be much better than the current practice of publishing reviews. The problem with most reviews is that they summarize only data published in medical journals in English language. However, this practice does not represent the clinical reality but presents a distorted picture. Therefore, we expect a severe publication bias (Schläpfer and Fins, 2010), leading to a systematic over-evaluation of the benefits.
The publication bias is no minor problem in psychiatric neurosurgery, but a fundamental problem, which corrupts the evaluation of risks and benefits of the different procedures. For example, we have performed a systematic literature search on psychiatric neurosurgery for treating anorexia nervosa, which yielded only 27 cases (Müller et al., forthcoming). However, from presentations on conferences we learned that a multiple of the patients reported in journals have been treated with ablative neurosurgery. Websites of private clinics in Europe as well as in Asia offer ablative surgery for a broad spectrum of psychiatric disorders as part of clinical routine. These treatments are not part of clinical studies and usually not published. Recently, a book of Sun and De Salles (2015) has been published which presents original data from several studies with ablative neurosurgery for different psychiatric disorders which had not been published in medical journals.
That being said, we summarize available data on the efficacy of the different approaches, whereby we refer to the most recent reviews as well as to the above mentioned book of Sun and De Salles.
Deep Brain Stimulation
For OCD, data from 25 papers comprising 109 patients and five targets (NAcc, VC/VS, ITP, nucleus subthalamicus, and internal capsule) have been published (Kohl et al., 2014). The responder rates ranged from 45.5 to 100%.
For depression, data from 22 papers comprising 188 patients and six targets (NAcc, VC/VS, SCC, lateral habenula, ITP, and slMFB) have been published (Morishita et al., 2014). The responder rates ranged from 29 to 92%. However, two multicenter, randomized, controlled, prospective studies evaluating the efficacy of VC/VS, and SCC DBS were recently discontinued because of inefficacy based on futility analyses (Morishita et al., 2014). The failure of two high quality studies in spite of the universally positive results of reported open-label trials could be attributable to the typical overestimation of efficacy associated with open label trials that arises from the failure to control for placebo, and biases due to lack of blinding and randomization (Morishita et al., 2014).
For anorexia nervosa, six papers comprising 18 patients and three targets (NAcc, subcallosal cingulum, and VC/VS) have been published (Müller et al., forthcoming). Remission (normalized body mass index) occurred in 61% of patients, and in 88.9%, psychiatric comorbidities improved, too. However, Sun et al. (2015) have recently published less favorable results: only 20% (3/15) of their patients treated with NAcc DBS showed improvements in symptoms. The other 80% underwent a second surgery (anterior capsulotomy), which improved eating behavior and psychiatric symptoms in all patients (Sun et al., 2015).
Generally, the current knowledge does not allow for identifying a superior target (Kohl et al., 2014; Morishita et al., 2014; Müller et al., forthcoming).
Microsurgical Ablative Procedures
For treatment-refractory depression, 40–60% of patients responded to bilateral capsulotomy or cingulotomy performed with thermal coagulation or radiosurgery (Eljamel, 2015).
For OCD, response rates between 36 and 89% have been published (Martinez-Alvarez, 2015). Martinez-Alvarez (2015) reports own data of 100 OCD patients of whom 71% responded.
For anorexia nervosa, three papers with nine patients report a remission rate of 100%, with regard to both weight normalization and psychiatric comorbidities. Different targets were used (dorsomedial thalamus, anterior capsula, NAcc; Müller et al., forthcoming). Sun et al. (2015) report 150 patients treated with capsulotomy, of whom 85% experienced an improvement in symptoms.
Radiosurgical Ablative Procedures
For OCD patients, a response rate of 70% has been reported in the literature (Martinez-Alvarez, 2015). Martinez-Alvarez (2015) reported a response rate of 100% in five own patients.
Adverse Effects
Deep Brain Stimulation
Following DBS, surgery-related, device-related, and stimulation-related side-effects have been reported. Serious adverse events during surgery were reported: seizures, intracerebral hemorrhages (in one case causing a temporary hemiparesis), a panic attack, and a cardiac air embolus (Kohl et al., 2014; Morishita et al., 2014; Müller et al., forthcoming). In anorexia nervosa patients, a high rate of severe complications have been reported: further weight loss, pancreatitis, hypophosphataemia, hypokalaemia, a refeeding delirium, an epileptic seizure during electrode programming, QT prolongation, and worsening of mood (Müller et al., forthcoming).
In several cases, superficial wound infections, inflammation, or allergic reactions occurred (Kohl et al., 2014). Device-related adverse effects comprised breaks in stimulating leads or extension wires requiring replacement, dysesthesia in the subclavicular region, and feelings of the leads or stimulators (Kohl et al., 2014).
Stimulation-induced adverse effects comprised mood disturbances, suicidality, anxiety, panic attacks, fatigue, and hypomania, partly induced either by a change of stimulation parameters, or by battery depletion. These effects were either adjustable by parameter adaption or device exchange (Kohl et al., 2014; Morishita et al., 2014; Müller et al., forthcoming). Some DBS patients report feelings of self-estrangement (Gilbert, 2013). A great problem is the high number of suicides and suicide attempts after DBS that have been reported in eight papers (Kohl et al., 2014; Morishita et al., 2014). Further side effects include vertigo, weight loss or gain, long-lasting fatigue, an increased headache frequency, and visual disturbance (Kohl et al., 2014).
Microsurgical Ablative Procedures
Adverse side effects of microsurgical ablative surgery for major depression comprised epilepsy (up to 10%), incontinence, weight gain, transient confusion, transient mania, and transient incontinence. Further side effects reported by only one or two studies are personality change (7 and 10%), lethargy, hemiplegia (0.3%), and suicide (1 and 9%) (Eljamel, 2015). Following microsurgical ablative surgery for treating OCD, a similar spectrum of adverse effects has been published. Most side effects were transient, and included headaches, urinary incontinence, impaired cognitive function, and confusion. Tardive epileptic seizures occurred in 2–9% of patients (Martinez-Alvarez, 2015). In case of anorexia nervosa, the journal papers reported only transient adverse effects: bradycardia, mild disorientation, moderate somnolence, loss of concentration, apathy, emotional emptiness and mild loss of decorum, headaches, and centric fever (Müller et al., forthcoming). However, Sun et al. (2015) report intracranial hematomas in 1.9% of the patients (4/216); one patient died thereof (0.5%).
Radiosurgical Ablative Procedures
Side-effects such as fatigue, weight gain, or apathy occurred in several patients who had received doses of more than 180 Gy. In newer studies with lower radiation doses, adverse effects did not occur (Lévèque, 2014).
Recommendations
From a mere medical perspective, none of the procedures is absolutely superior; rather, they have different profiles of advantages and disadvantages (see Table 1). The main advantages of DBS are its adaptability and high degree of reversibility; of microsurgical ablative procedures the rapid onset of action; and of radiosurgery its noninvasiveness and low rate of adverse effects. Furthermore, it differs individually what counts as an advantage or disadvantage: For example, the delayed onset of action of radiosurgery makes it disadvantageous for patients who need a rapid symptom reduction. However, the gradual development of effects might be advantageous since it alleviates the psychological adjustment (Lindquist et al., 1991). This may be protective against feelings of being manipulated, self-estrangement and the burden of normality syndrome.
We support further research in this area generally, but think that therapeutic adventurism cannot be justified. The current research practice in psychiatric neurosurgery does not fulfill the highest ethical and scientific standards. We plead for ethical reasons for better safeguards in research and clinical practice. Since psychiatric neurosurgery has both the goal and the potential to change core features of the patients’ personalities, these interventions require a solid scientific fundament. Particularly, we recommend the following:
-
Case registries should become obligatory for all clinical studies in order to avoid a publication bias and its negative consequences, namely faulty evaluations of therapies, flawed therapy recommendations, unpromising treatment attempts and unneeded clinical studies (Morishita et al., 2014). Individual treatment attempts should not be performed.
-
A multi-center, randomized, controlled study should be performed that directly compares DBS, microsurgical ablative procedures and radiosurgery for different psychiatric disorders.
-
Since multiple circuits seem to be involved in psychiatric disorders, targets of DBS or ablative procedures, respectively, should be selected specifically with regard to the prominent symptoms instead of using the institution-specific target for all patients.
-
Since no single procedure is absolutely superior, patients should be informed comprehensively about the different treatment options and their respective benefit-risk-profiles. Individual factors have to be crucial in decision making, particularly the patients’ social situation, individual preferences, and individual attitudes (e.g., whether they could tolerate implanted devices; whether they are more afraid of the irreversibility of an ablative procedure or of the medical risks of brain surgery).
We are convinced that the different approaches are not only rivals, but also enriching mutually. DBS is preferable for exploring new targets, which may become candidates for ablative microsurgery or radiosurgery.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgment
The research of Sabine Müller has been supported by the German Research Foundation (DFG), Germany (MU 3321/1-1).
Abbreviations
ALIC, anterior limb of the internal capsule; DBS, deep brain stimulation; ITP, inferior thalamic peduncule; MRI, magnetic resonance imaging; NAcc, nucleus accumbens; OCD, obsessive-compulsive disorder; SCC, subgenual cingulate cortex; slMFB, superolateral medial forebrain bundle; VC/VS, ventral capsula/ventral striatum.
References
Bronstein, J. M., Tagliati, M., Alterman, R. L., Lozano, A. M., Volkmann, J., Stefani, A., et al. (2011). Deep brain stimulation for Parkinson disease: an expert consensus and review of key issues. Arch. Neurol. 68, 165–171. doi: 10.1001/archneurol.2010.260
Eljamel, S. (2015). “Ablative surgery for depression,” in Neurosurgical Treatments for Psychiatric Disorders, eds B. Sun and A. De Salles (Dordrecht: Springer), 87–94. doi: 10.1007/978-94-017-9576-0_8
Gilbert, F. (2013). Deep brain stimulation for treatment resistant depression: postoperative feeling of self-estrangement, suicide attempt and impulsive-aggressive behaviours. Neuroethics 6, 473–481. doi: 10.1007/s12152-013-9178-8
Kohl, S., Schönherr, D. M., Juigjes, J., Denys, D., Mueller, U. J., Lenartz, D., et al. (2014). Deep brain stimulation for treatment-refractory obsessive compulsive disorder: a systematic review. BMC Psychiatry 14:214. doi: 10.1186/s12888-014-0214-y
PubMed Abstract | Full Text | CrossRef Full Text | Google Scholar
Lévèque, M. (2014). Psychosurgery. New Techniques for Brain Disorders. Dordrecht: Springer. doi: 10.1007/978-3-319-01144-8
Lindquist, C., Kihlström, L., and Hellstrand, E. (1991). Functional neurosurgery–a future for the Gamma Knife? Stereotact. Funct. Neurosurg. 57, 72–81. doi: 10.1159/000099557
Lipsman, N., Mendelsohn, D., Taira, T., and Bernstein, M. (2011). The contemporary practice of psychiatric surgery: results from a global survey of North American functional neurosurgeons. Stereotact. Funct. Neurosurg. 89, 103–110. doi: 10.1159/000323545
PubMed Abstract | Full Text | CrossRef Full Text | Google Scholar
Martinez-Alvarez, R. (2015). “Ablative surgery for obsessive-compulsive disorders,” in Neurosurgical Treatments for Psychiatric Disorders, eds B. Sun and A. De Salles (Dordrecht: Springer), 105–112. doi: 10.1007/978-94-017-9576-0_10
Mendelsohn, D., Lipsman, N., Lozano, A. M., Taira, T., and Bernstein, M. (2013). The contemporary practice of psychiatric surgery: results from a global survey of functional neurosurgeons. Stereotact. Funct. Neurosurg. 91, 306–313. doi: 10.1159/000348323
PubMed Abstract | Full Text | CrossRef Full Text | Google Scholar
Morishita, T., Fayad, S. M., Higuchi, M., Nestor, K. A., and Foote, K. D. (2014). Deep brain stimulation for treatment-resistant depression: systematic review of clinical outcomes. Neurotherapeutics 11, 475–484. doi: 10.1007/s13311-014-0282-1
PubMed Abstract | Full Text | CrossRef Full Text | Google Scholar
Müller, S., Riedmüller, R., Walter, H., and Christen, M. (forthcoming). An ethical evaluation of stereotactic neurosurgery for anorexia nervosa. AJOB Neurosci.
Na, Y. C., Jung, H. H., and Chang, J. W. (2015). “Focused ultrasound for the treatment of obsessive-compulsive disorder,” in Neurosurgical Treatments for Psychiatric Disorders, eds B. Sun and A. De Salles (Dordrecht: Springer), 125–141.
Nuttin, B., Wu, H., Mayberg, H., Hariz, M., Gabriëls, L., Galert, T., et al. (2014). Consensus on guidelines for stereotactic neurosurgery for psychiatric disorders. J. Neurol. Neurosurg. Psychiatr. 85, 1003–1008. doi: 10.1136/jnnp-2013-306580
PubMed Abstract | Full Text | CrossRef Full Text | Google Scholar
Régis, J. (2013). “Radiosurgery as a modulation therapy!,” in Gamma Knife Neurosurgery in the Management of Intracranial Disorders, Vol. 116, Acta Neurochirurgica Supplement, eds M. F. Chernov, M. Hayashi, J. C. Ganz, and K. Takakura (Vienna: Springer), 121–126.
Schläpfer, T. E., and Fins, J. J. (2010). Deep brain stimulation and the neuroethics of responsible publishing: when one is not enough. JAMA 303, 775–776. doi: 10.1001/jama.2010.140
PubMed Abstract | Full Text | CrossRef Full Text | Google Scholar
Sun, B., and De Salles, A. (2015). Neurosurgical Treatments for Psychiatric Disorders. Dordrecht: Springer. doi: 10.1007/978-94-017-9576-0
Keywords: psychiatric neurosurgery, radiosurgery, gamma knife, DBS, ablative neurosurgery, cingulotomy, capsulotomy, neuroethics
Citation: Müller S, Riedmüller R and van Oosterhout A (2015) Rivaling paradigms in psychiatric neurosurgery: adjustability versus quick fix versus minimal-invasiveness. Front. Integr. Neurosci. 9:27. doi: 10.3389/fnint.2015.00027
Received: 20 January 2015; Accepted: 17 March 2015;
Published online: 02 April 2015.
Edited by:
Elizabeth B. Torres, Rutgers University, USAReviewed by:
Eduardo Fernandez, Miguel Hernández University of Elche, SpainDawei Li, Duke University, USA
Copyright © 2015 Müller, Riedmüller and van Oosterhout. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sabine Müller, Charité-Universitätsmedizin Berlin, Department of Psychiatry and Psychotherapy, CCM, Mind and Brain Research, Charitéplatz 1, 10117 Berlin, GermanybXVlbGxlci5zYWJpbmVAY2hhcml0ZS5kZQ==
 Sabine Müller
Sabine Müller Rita Riedmüller
Rita Riedmüller Ansel van Oosterhout
Ansel van Oosterhout