- 1Department of Ophthalmology, University of Nigeria Teaching Hospital, Ituku-Ozalla, Enugu, Nigeria
- 2Department of Optometry, Faculty of Medicine and Health Sciences, Abia University Uturu, Okigwe, Abia, Nigeria
- 3Department of Optometry, Faculty of Medicine and Health Sciences, Imo State University, Owerri, Nigeria
- 4Department of Community Medicine, Federal Medical Centre Umuahia, Umuahia, Abia, Nigeria
- 5Department of Psychiatry, University of Nigeria Teaching Hospital, Ituku-Ozalla, Enugu, Nigeria
Background/Aim: To examine how music can impact preoperative and intraoperative anxiety via assessment of physiological markers such as pupil size, blood pressure, pulse rate, and respiratory rate.
Methods: This is a randomized interventional study of individuals aged 50 years and above who were scheduled for and undergoing cataract surgery under regional anesthesia, with music (test group) randomly matched with similar individuals undergoing the same procedure but without music (control group). The surgeries were performed in the operating theater of the Department of Ophthalmology, University of Nigeria Teaching Hospital (UNTH), Ituku-Ozalla, Enugu. Using a systematic random sampling method, a total of 98 patients were grouped into two. Both groups completed the State–Trait Anxiety Inventory (STAI) questionnaire at baseline, immediately upon entrance into the preoperative room and 5 min after intervention. Relevant study indices (blood pressure, pulse, respiratory rate, and pupil diameter) were measured and recorded, and these served as baseline parameters. The STAI questionnaire was then administered. Results were analyzed using the SPSS version 20 and analysis of variance was used to compare means of variables measured at baseline, preoperative before intervention, and preoperative after intervention. Categorical variables were compared using the Chi-square test. Student’s t-test was used to analyze the continuous variables.
Results: Our analysis, using the multiple linear regression, showed that music has an effect on preoperative anxiety and intraoperative anxiety by positively affecting the blood pressure, pulse rate, respiratory rate, and pupil diameter (P ≤ 0.001).
Conclusion: Music reduces preoperative and intraoperative anxiety evidenced by its effect on the physiological biomarkers.
Introduction
Globally, it is well-established that preoperative and intraoperative anxiety can have profound effects on both patients and surgical outcomes (1). According to a systematic and meta-analysis study by Abate et al. (2020), the pooled prevalence of preoperative anxiety is estimated at 48% (2). Several related epidemiological research in low- and middle-income countries found that the prevalence of preoperative anxiety varies (3–5), with Nigeria ranging from 51% to 90% (6, 7).
Anxiety is commonly characterized by restlessness, fatigue, diminished concentration, and heightened muscular tension (8). According to Liu, “Preoperative anxiety is often described as an uncomfortable, tense, and unpleasant mood before surgery, an emotional response to a potential challenge or threat to reality.” (9) The preoperative period is the period that spans from the moment the patient is informed about the procedure to be done, through the preoperative room until patient is placed on the operating table, while intraoperative period spans from the moment the patient is placed on the operating table to the moment patient is wheeled to the recovery room (Terri Goodman, 2012) (10). Preoperative anxiety is the most common form associated with a number of postoperative complications, such as delayed healing of wounds, prolonged stay in the hospital, and decreased pain threshold (11, 12).
Physiological markers such as pupil size, blood pressure, and respiratory rate are affected by anxiety. Anxiety has also been noted to have ocular manifestations such as change in intraocular pressure and pupil diameter (13, 14). Many studies have been conducted to establish the relationship between psychophysiological stress and increased intraocular pressure (14). Anxiety has been documented to activate the sympathetic nervous system, which is mediated by the hypothalamic-pituitary-adrenal axis (15). Through this pathway, there is increased circulating hormones such as cortisol, which leads to indirectly increasing the intraocular pressure by its direct effect in increasing the blood pressure (15). In anxiety states, there could be as much as 2-3-mmHg rise in intraocular pressure in normal eyes and this could be more in high-risk eyes such as patients being managed for glaucoma (15). During surgery, this increased intraocular pressure as a consequence of anxiety, combined with fluctuating pupil diameter may lead to complications intraoperatively such as iris prolapse and vitreous loss (15, 16).
Pupil diameter has also been known to be affected by stress or anxiety state (13). During small incision cataract surgery, from the onset of surgery to the placement of the intraocular lens, proper pupillary dilation is necessary and if this is not achieved, there could be iris trauma, damage to the lens zonules, posterior capsular rent with vitreous loss, and lens matter retention due to difficult lens washout (16, 17). Also immediately following intraocular lens placement, pupillary constriction is beneficial and if there is improper dilation due to anxiety, this could lead to improper placement of the lens causing iris damage intraoperatively and other complications (17). Therefore, allaying anxiety, which may lead to these intraoperative and postoperative complications is important (13).
Pharmacological products such as the benzodiazepines, either singly or in combined form for more efficacy such as the lytic cocktails comprising mainly of pethidine, chlorpromazine, and promethazine (18) have been used to reduce anxiety. These sedatives exhibit some adverse effects ranging from extrapyramidal side effects such as hallucinations to systemic hepatotoxicity, so their use have been limited (18). Music, a non-pharmacological alternative intervention and relatively cost-effective can be employed preoperatively to alleviate anxiety (19). Minichiello (2019) revealed that listening to certain types of music, particularly new-age music and classical music, can increase feelings associated with relaxation, such as peacefulness and a sense of ease (20).
In Nigeria, where preoperative anxiety and intraoperative anxiety have been documented as a prevalent concern during cataract surgery (6, 7), there is a significant gap in the understanding of how music can alleviate anxiety. While prior research has predominantly focused on the effects of pharmacological agents, there is a pressing need to explore alternative approaches. This study endeavors to address this critical knowledge gap by examining how music can impact preoperative and intraoperative anxiety via assessment of physiological markers such as pupil size, blood pressure, pulse rate, and respiratory rate. The findings of this study will provide valuable insights that can inform clinical practice and enhance the wellbeing of patients undergoing cataract surgery in Nigeria.
Materials and methods
Study design and setting
This study was conducted at the Department of Ophthalmology of the University of Nigeria Teaching Hospital (UNTH), Ituku-Ozalla, located 21 km from the Enugu metropolis. This was a randomized interventional study of individuals aged 50 years and above who were scheduled for and undergoing cataract surgery, with music and regional anesthesia, matched with individuals 50 years and above scheduled for and undergoing cataract surgery without music but also with regional anesthesia in the operating theater of the Department of Ophthalmology, UNTH, Ituku-Ozalla Enugu. Participants were excluded from this study if they had other types of cataracts other than age-related cataract, younger than 50 years of age, had major ocular morbidity, diagnosed with uncorrected hearing problems, and declined to participate. Patients whose age were equal to or greater than 50 years, scheduled for cataract surgery under regional anesthesia at UNTH Ituku-Ozalla, and consented to participate were enrolled in the study. A total of 98 participants were selected using a systematic random sampling method. Study participants were assigned into two groups (i.e., Group A, those that underwent surgery with music, and Group B, those that underwent surgery without music).
Sampling technique
Patients that visited the hospital for uncomplicated cataract surgery were recruited in outpatient clinics after comprehensive clinical assessments to ensure they met the study’s eligibility criteria. Approximately 15 patients were enrolled each week and provided with detailed information about the study, the surgical procedure, and the music intervention, after which written informed consent was obtained. Enrolled individuals were randomized into two groups using a systematic sampling method, with the researcher remaining blinded to the group assignments and the randomization done by a research assistant. The patients were divided into two groups based on odd and even numbers, with odd-numbered patients (Group A) receiving surgery with music and even-numbered patients (Group B) undergoing surgery without music, while maintaining sterility with assigned earphones, and their data were meticulously recorded. This randomization was done by the research assistant, and the researcher was blinded to the groups.
Sample size determination
The minimum sample size (n) for this study was determined using the formula for comparison between two groups/proportions. Sample size calculation was based on prevalence and the results of similar studies among preoperative anxiety studies in cataract patient (21).
Zα = the standard normal variate at 95% confidence interval if p<0.05, which equals 1.96.
Zβ = power of the study at 80% from the Z-table, which equals 0.842.
P1 = the proportion of patients who used preoperative and intraoperative music – 0.6454.23.
P2 = the proportion of patients who did not use preoperative and intraoperative music – 0.3546.23.
(P1−P2)2 = the difference in independent proportions, which equals (0.6454−0.3546)2 = 0.0846.
The minimum sample size was adjusted based on the probability of a non-response rate of 10% with the formula:
where n = minimum sample size, which equals 42 and r = 10% or 0.1.
Thus, the sample size for the two groups = 47 × 2 = 94, so n = 94.
Increasing n by 10% to leave room for errors, which involves any factor that would make any participant not show up or have his/her surgery suddenly cancelled = 94+ (10% of 94).
= 94 + 10
n = 104
Study instrument and procedure
A pretest was carried out on six patients aged 50 years and above and scheduled for uncomplicated cataract surgery at the Enugu State University Teaching Hospital Parklane, Enugu, which is approximately a 2-h drive from the UNTH study center. State–Trait Anxiety Inventory (STAI) questionnaire was administered on the patients, and different measurements were taken at different times. This was used to determine the adequacy of the materials and methods. A pilot study was subsequently carried out on 10 patients aged 50 years and above and scheduled for uncomplicated cataract surgery at the Enugu State University Teaching Hospital Parklane, Enugu, with the help of study assistants. This was aimed at determining the feasibility of the study. Patients used in the pilot study were not included in the index study.
For group A: baseline
This was the routine for the test group and the control group. In the clinic, an anterior and posterior segment examination was done with the aid of a slit lamp and 90D lens, respectively, to be certain that the patient met the inclusion criteria. Rinne’s and Weber’s tests were done to ascertain patients with uncorrected hearing problems. Study participants were informed about the study´s components and objectives, and written informed consent was obtained upon recruitment in the clinic. The patients were admitted a day before the surgery, and after approximately a 30-min rest on the bed, baseline parameters were taken including blood pressure, pulse, respiratory rate, and pupil diameter, serving as objective parameters for the indirect assessment of anxiety. Blood pressure measurement was done with each patient lying down, sitting, and standing to rule out positional change in blood pressure. The pupil diameter was checked on the contralateral eye to avoid interfering with the eye to be operated on. The pupil diameter was assessed using a transparent meter rule, and the patient was given a target to look at vertically upwards while in a supine position. The STAI questionnaire was then administered. This was the subjective parameter for anxiety assessment. The patients were allowed to choose their preferred music before being transferred to the preoperative room.
Preoperative
In the preoperative room, the objective indices were checked and recorded again in the same manner. The STAI questionnaire was subsequently administered to the patients again. Patients were given earphones and helped to put them in place. Their preferred music was turned on and the volume was adjusted to the patient’s satisfaction. After 5 min of listening to music, the blood pressure, pulse rate, and respiratory rate were checked again and recorded. The pupil diameter was measured again on the contralateral eye and recorded, after which peribulbar anesthesia was given. The STAI questionnaire was again administered on the patients intraoperatively. Each patient was wheeled into the theater with the instrument used in measuring blood pressure and pulse still attached to the patient and the earphone still in situ, with the music still playing. The surgeon was blinded as to the group each patient belonged to. The music played for the whole duration of the surgery. At the end of surgery, as soon as the drapes were removed, the pupil diameter was measured on the contralateral eye. The music was then discontinued and each patient was wheeled out of the theater.
For group B
The patients in this group were processed exactly the same way and in the same order as the patients in Group A for the baseline, preoperative, and intraoperative stages. However, music was not played though the earphones were attached as with the patients in Group A.
Data analysis
Data collected from the study were initially entered into a Microsoft Excel spreadsheet, underwent cleaning and coding, and were later imported into SPSS version 20 for analysis. Analysis included the use of tables, charts, Chi-square tests for categorical variables, Student’s t-test for continuous variables to compare pre- and post-intervention means in both groups, and ANOVA for comparing means involving more than two variables, with a significance level set at a P-value of less than 0.05.
Ethical considerations
Ethical approval for this study was sought and obtained from the Health Research and Ethics Committee of UNTH, Ituku-Ozalla. Permission was sought from the consultants operating in the theater where the study was carried out and also from the Head of the Department of Ophthalmology. A written informed consent was obtained from the study participants. Participants were informed of their right to decline or withdraw from the study at any point without any consequences. Data collected for this research were stored in password-protected computers and the names of the participants were made anonymous.
Results
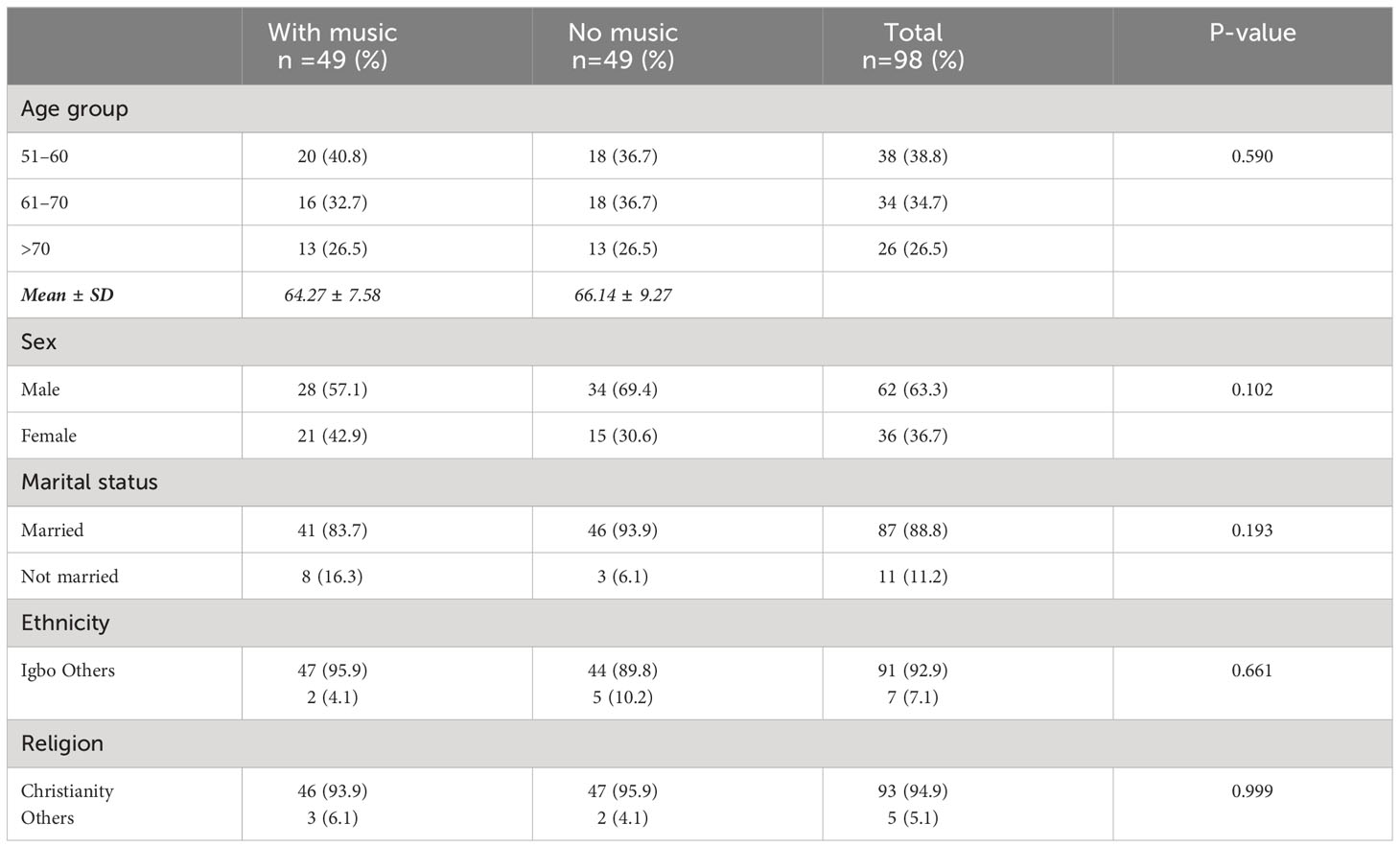
Table 1 shows the sociodemographic characteristics of the participants in terms of age, sex distribution, marital status, ethnicity, and religion. There was no statistically significant difference between the two groups with P-values as indicated.
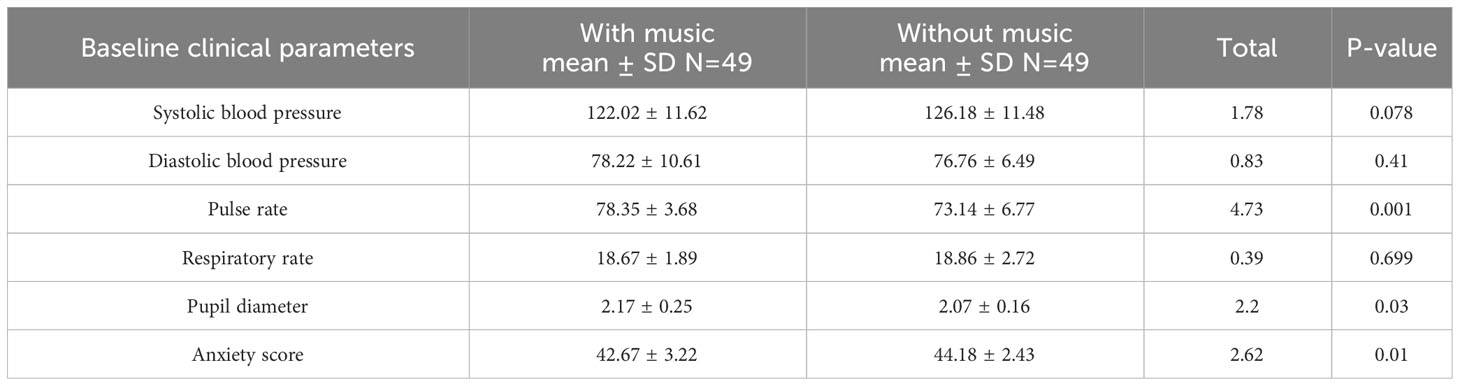
Table 2 gives the baseline clinical parameters of the participants. Both groups were comparable with respect to systolic and diastolic blood pressure. Therefore, these parameters were further analyzed using multiple linear regression.
Table 3 provides the comparison of blood pressure (systolic/diastolic), pulse rate, and respiratory rate within the groups, before and after intervention. For the music group, the systolic and diastolic pressures decreased by 14.88 mmHg (95% CI =12.06–17.69) and 6.37 (95% CI =4.80–7.94). However, the systolic and diastolic blood pressure increased by 5.06 mmHg (95% CI = 2.86–7.27) and 2.65 (95 CI = 0.98–4.33) in the no-music group.
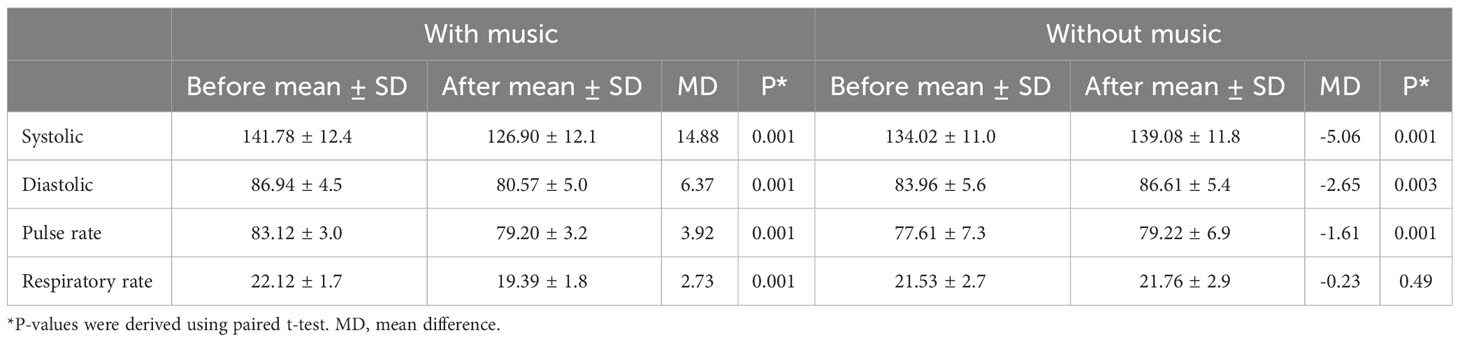
Table 3 Intragroup comparison of mean systolic, diastolic blood pressure, pulse rate, and respiratory rate before and after music was played for the music and no-music groups.
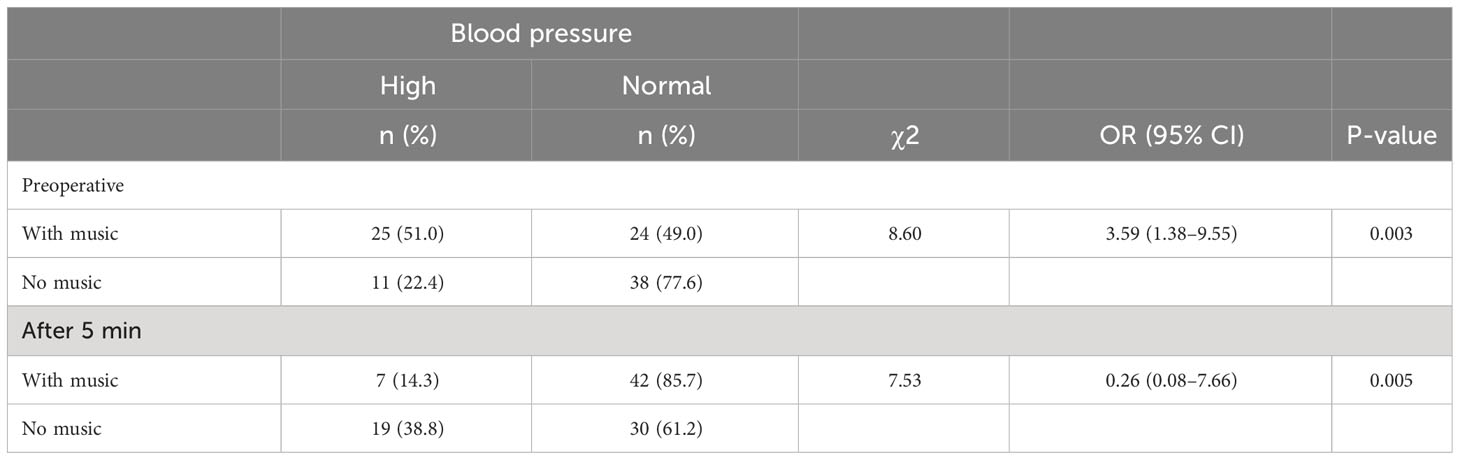
Table 4 shows the intergroup comparison of prevalence of blood pressure before and after music intervention. The blood pressure was significantly higher (51% vs. 22.4%) in the music group prior to the music intervention and the odds of having abnormal blood pressure was 3.59 times (95% CI: 1.38–9.55, p = 0.003) greater in the music group. However, following the music intervention, the blood pressure in the music group became significantly lower (14% vs. 38%) and the odds of having high blood pressure was lower 0.26 (95% CI: 0.08–7.66, p= 0.005). Conversely, the blood pressure rather increased in the group with no music intervention (22.4% →38%), p = 0.010.
Table 5 provides the intergroup comparison of mean systolic blood pressure, diastolic blood pressure, pulse rate, and respiratory rate between the music group and the no-music group. Apart from respiratory rate, the other parameters were significantly lower in the no-music group compared to the music group in the preoperative period. However, after the music intervention, the mean values for all the clinical measurements became significantly higher in the no-music group. Furthermore, in the no-music group, there was a linear increase for the vital signs across the different times of measurement. These observed linear trends of incremental rise with time were statistically significant for systolic blood pressure, diastolic blood pressure, pulse rate, and respiratory rate, using one way ANOVA for the repeated measure test for trend.
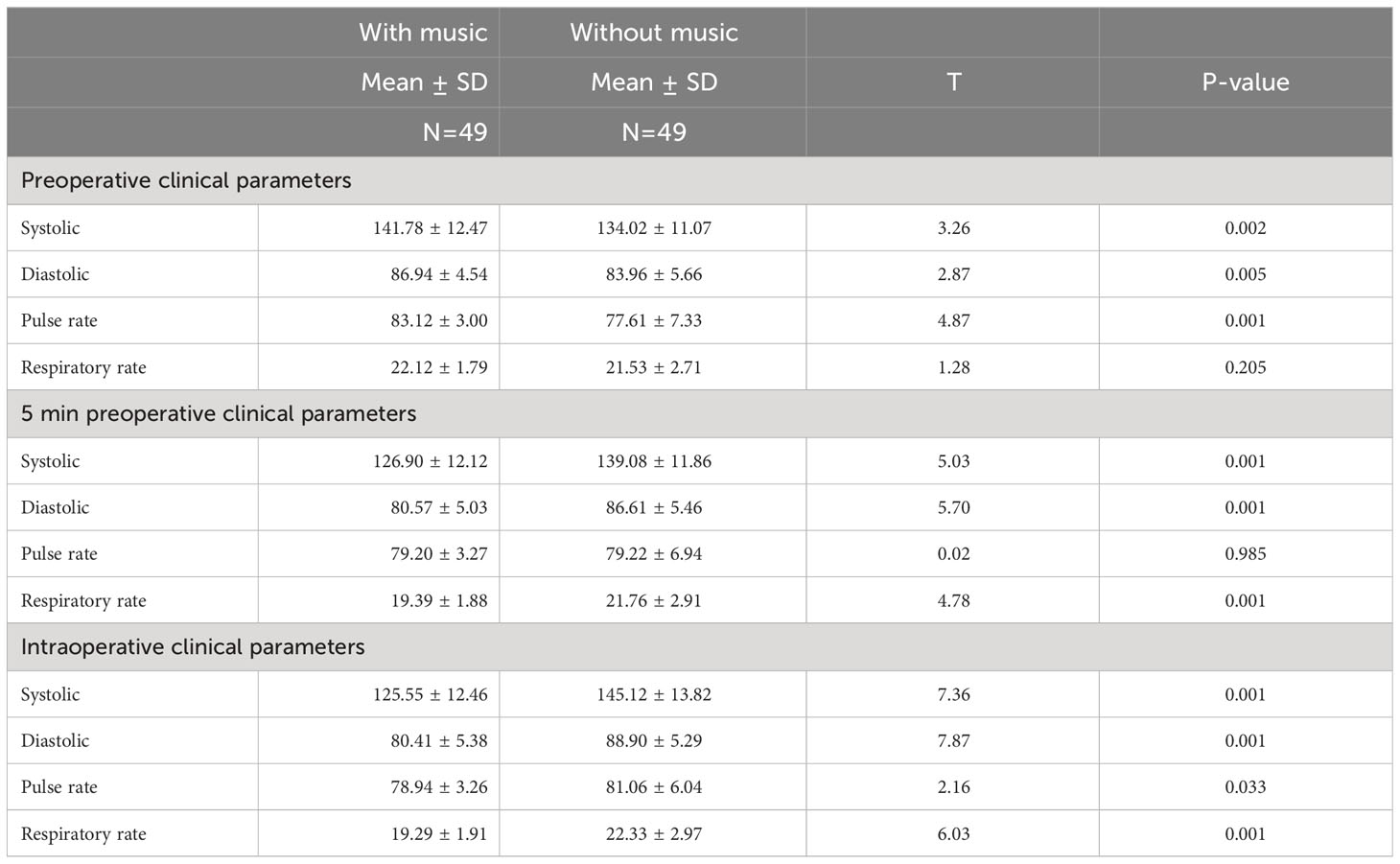
Table 5 Comparison of mean systolic, diastolic blood pressure, pulse rate, and respiratory rate between the music group and the no-music group.
Multiple linear regression was fitted to determine the independent effect of music on systolic blood pressure while adjusting for the effect of differences in pre-intervention (before music). After adjusting for the differences in pre-intervention systolic blood pressure, music still had a significant effect on post- intervention systolic blood pressure (p = 0.001). The model indicates that a participant in the music group, after listening to music, on average, had systolic blood pressure 17.91 mmHg (95% CI: 14.8–21.4) lower compared to participants in the no-music group who had the same pre-intervention anxiety score (see the Supplementary Table 6A).
Similarly, the Supplementary Tables 6B–D, after adjusting for the differences in pre-intervention diastolic blood pressure, pre-intervention pulse rate, and pre-intervention respiratory rate, the music group had average post-intervention diastolic blood pressure, post-intervention pulse rate, and post-intervention respiratory rate 7.28 mmHg (95% CI = −9.29, −5.26), 4.63 (95% CI: −5.86, −3.41), and 2.76 (95% CI = −3.54–1.99) lower, respectively, compared to the no-music group (see the Supplementary Table 6A). Multiple logistic regression was done to determine the effect of music on the likelihood of having high blood pressure. After adjusting for the differences in pre-intervention blood pressure values, the odds of having high blood pressure were significantly greater in the no-music group, with OR = 5.16, 95% CI = 1.22–21.85, p =0.026 (see the Supplementary Table 6B).
Supplementary Table 7 provides the comparative mean pupil diameter of the group with music and without music at different times during the study. The mean pupil diameter was significantly lower in the no-music group compared to the music group at baseline and the preoperative period. However, after the music intervention, the mean pupil diameter became significantly lower for the music group compared to the no-music group. Furthermore, in the no-music group, there was a significant linear increase in the mean pupil diameter across the different times of measurement.
Discussion
The present study examined the effect of music on the level of preoperative and intraoperative anxiety in patients scheduled to undergo cataract surgery. Anxiety levels, measured using the STAI questionnaire and physiological indices (blood pressure, pulse, respiratory rate, and pupil diameter) were assessed at baseline, before, during, and after the surgery and were compared between two groups of participants, one with music intervention and the other without.
With regard to the effect on blood pressure, respiratory rate, and pulse rate, the participants that received music intervention had significantly lower values of their systolic and diastolic blood pressure and respiratory rate compared to the control group. The pulse rate of the music intervention group though lower was not significantly different from that of the control group. Camara et al. (22) and Merakou et al. (23) found that playing live classical music significantly lowered the blood pressure, respiratory rate, and pulse rate of pre-surgical patients compared to pre-exposure values (22, 24). This finding is similar to the findings by Labrague and McEnroe-Petitte (25). The result of their study involving women undergoing gynecological surgery showed that music intervention led to a significantly lower systolic and diastolic blood pressure and pulse rate. A meta-analysis of studies on music interventions for preoperative anxiety by Bradt et al. (26) also reported that music significantly reduced heart rate and diastolic blood pressure with an insignificant effect on respiratory rates (26). Another study conducted among patients undergoing abdominal surgery concluded that there was no significant difference between the anxiety level and physiological responses in two groups of patients before intervention. The findings indicate a statistically significant difference in the level of anxiety and mean blood pressure in the intervention group (p<0.05). Also, the heart and respiratory rates in the two groups of patients revealed no significant difference (27).
In our study, there was significant reduction in pupil diameter in the patients who received music intervention while those who were not exposed to music had sustained dilatation. Research has shown that pupil diameter is increased as a result of anxiety arising from anticipated distress and pain due to increased sympathetic outflow (28, 29). The reduction in pupil diameter in this study and related study (28) is therefore an indirect assessment of anxiety. It has been shown that this reduction may have been caused by a reduction in neuronal activity in the amygdala and locus coeruleus, hence the reduced pupil diameter (29). This shows that there is a likely relationship between music and pupil sizes. Also, there is a relationship between pupil size and anxiety state, which can all be influenced by music.
This study has some limitations that need to be acknowledged. Patients often struggled to comply because of survey fatigue from repeated questioning, while some had difficulty hearing the interviewer due to music-playing earphones. Conducting interviews during surgery proved distracting for both the patients and surgeons. As a result, many studies opt for the STAI questionnaire to assess anxiety before or after surgery, rather than during the procedure. Notably, the two patient groups were not age- and sex-matched, potentially introducing confounding variables. Preoperative and intraoperative anxiety present challenges in patients scheduled for and undergoing cataract surgery. There is also an effect of music on preoperative and intraoperative anxiety in patients undergoing cataract surgery at UNTH Enugu. These indirect effects can be evidenced by indirect effects of music on blood pressure, pulse rate, respiratory rate, and pupil diameter. Music has been shown by this study to be a valuable non-pharmacological agent that could be used to allay preoperative and intraoperative anxiety in such patients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethical approval for this study was obtained from the Health Research and Ethics Committee of University of Nigeria Teaching Hospital, Ituku Ozalla (NHREC/05/01/2008B-FWA0002458-1RB0002323). Written informed consent was obtained from all the study participants. Participants were told of their right to decline or withdraw from the study at any point, without any consequences. Data collected for this research were stored in password-protected computers, and participant names were anonymized. Participants gave informed consent to participate in the study before taking part. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CE: Conceptualization, Investigation, Writing – original draft, Writing – review & editing, Formal Analysis. OA: Data curation, Software, Validation, Writing – review & editing. CD: Conceptualization, Data curation, Methodology, Resources, Validation, Writing – review & editing. FO: Conceptualization, Investigation, Methodology, Resources, Validation, Writing – review & editing. NZN: Formal Analysis, Investigation, Methodology, Validation, Writing – review & editing. NN: Conceptualization, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. CO: Conceptualization, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – review & editing. CAO: Conceptualization, Resources, Software, Validation, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We acknowledge the Department of Ophthalmology, University of Nigeria Teaching Hospital, Ituku- Ozalla, Enugu State for their support throughout the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fopht.2023.1340752/full#supplementary-material
References
1. Kassahun WT, Mehdorn M, Wagner TC, Babel J, Danker H, Gockel I. The effect of preoperative patient-reported anxiety on morbidity and mortality outcomes in patients undergoing major general surgery. Sci Rep (2022) 12(1):6312. doi: 10.1038/s41598-022-10302-z
2. Abate SM, Chekol YA, Basu B. Global prevalence and determinants of preoperative anxiety among surgical patients: A systematic review and meta-analysis. Int J Surg Open (2020) 25:6–16. doi: 10.1016/j.ijso.2020.05.010
3. Bansal T, Joon A. A comparative study to assess preoperative anxiety in obstetric patients undergoing elective or emergency caesarean section. Anaesthesia Pain Intensive Care (2019) 21(1):25–30.
4. Jafar MF, Khan FA. Frequency of preoperative anxiety in Pakistani surgical patients. J Pakistan Med Assoc (2009) 59(6):359.
5. Zeb A, Hammad AM, Baig R, Rahman S. Pre-operative anxiety in patients at tertiary care hospital, Peshawar. Pakistan. J Clin Trials Res (2019) 2:76–80. doi: 10.36346/sarjnhc.2019.v01i01.004
6. Ebirim LA, Tobin M. Factors responsible for pre-operative anxiety in elective surgical patients at a university teaching hospital: a pilot study. Internet J Anesthesiology (2010) 29(2):1–6.
7. Akinsulore A, Owojuyigbe AM, Faponle AF, Fatoye FO. Assessment of preoperative and postoperative anxiety among elective major surgery patients in a tertiary hospital in Nigeria. Middle East J Anesthesiol. (2015) 23(2):235–40.
8. Sigdel S. Perioperative anxiety: A short review. Glob Anesth Perioper Med (2015) 1(4):107–8. doi: 10.15761/GAPM.1000126
9. Liu JD. Preoperative anxiety’s incidence and related factors in surgical patients. Natl Libr Med (2017) 71(9):35–78. doi: 10.3390/ijerph191912162
10. Terri Goodman CS. Introduction to perioperative nursing. Sixth Edit. Jones & Bartlett learning – Essentials of preoperative anxiety (2012) p. 1–12.
11. Mulugeta H, Ayana M, Sintayehu M, Dessie G, Zewdu T. Preoperative anxiety and associated factors among adult surgical patients in Debre Markos and Felege Hiwot referral hospitals, Northwest Ethiopia. BMC Anesthesiol. (2018) 18(1):1–9. doi: 10.1186/s12871-018-0619-0
12. Coker A, Balogun M, Balogun B, Adekoya BJ. Assessment of pre and postoperative psychiatric comorbidity among patients scheduled for elective cataract surgery in Lagos, Nigeria. Res J Heal Sci (2016) 4(3):232. doi: 10.4314/rejhs.v4i3.6
13. Folk J. Pupils anxiety symptoms: dilated or contracted (2019). Available at: https://www.anxietycentre.com/anxiety-symptoms/pupils-anxiety-symptoms.shtml.
14. Méndez-Ulrich JL, Sanz A, Feliu-Soler A, Álvarez M, Borràs X. Could white coat ocular hypertension affect to the accuracy of the diagnosis of glaucoma? Relationships between anxiety and intraocular pressure in a simulated clinical setting. Appl Psychophysiol Biofeedback. (2018) 43(1):49–56. doi: 10.1007/s10484-017-9385-x
15. Gillmann KH. Acute emotional stress as a trigger for intraocular pressure elevation in Glaucoma. BMC Ophthalmol (2019) 19(69):61. doi: 10.1186/s12886-019-1075-4
16. Malyugin B. Cataract surgery in small pupils. Indian J Ophthalmol (2017) 65(12):1323–8. doi: 10.4103/ijo.IJO_800_17
17. Gonzalez-Salinas R, Guarnieri A, Guirao Navarro MC, Saenz-de-Viteri M. Patient considerations in cataract surgery - the role of combined therapy using phenylephrine and ketorolac. Patient Prefer Adherence. (2016) 10:1795–801. doi: 10.2147/PPA.S90468
18. Stallard H. Anaesthesia and akinesia for eye operations. In: Roper-Hall M, editor. EyeSurgery, fifth. Wright, Bristol (1973). p. 77.
19. Graff V, Cai L, Badiola EN. Music versus midazolam during preoperative nerve block placements: a prospective randomized controlled study. Reg Anesth Pain Med (2019) 10(2):20–34. doi: 10.1136/rapm-2018-100251
21. Wiwatwongwana D, Vichitvejpaisal P, Thaikruea L, Klaphajone J, Tantong A, Wiwatwongwana A, et al. The effect of music with and without binaural beat audio on operative anxiety in patients undergoing cataract surgery: A randomized controlled trial. Eye (2016) 30(11):1407–14. doi: 10.1038/eye.2016.160
22. Camara JG, Ruszkowski JM, Worak SR. The effect of live classical piano music on the vital signs of patients undergoing ophthalmic surgery. MedGenMed Medscape Gen Med (2008) 10(6):149.
23. Merakou K, Varouxi G, Barbouni A, Antoniadou E, Karageorgos G, Theodoridis D, et al. Blood pressure and heart rate alterations through music in patients undergoing cataractSurgery in Greece. Ophthalmol Eye Dis (2015) 7(8):57. doi: 10.4137/OED.S20960
24. Heise L, Greene ME, Opper N, Stavropoulou M, Harper C, Nascimento M, et al. Gender inequality and restrictive gender norms: framing the challenges to health. Lancet (2019) 393(10189):2440–54. doi: 10.1016/S0140-6736(19)30652-X
25. Labrague LJ, McEnroe-Petitte DM. Influence of music on preoperative anxiety and physiologic parameters in women undergoing gynecologic surgery. Clin Nurs Res (2016) 25(2):157–73. doi: 10.1177/1054773814544168
26. Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. Cochrane Database Syst Rev (2013) 2013(6):CD006908. doi: 10.1002/14651858.CD006908
27. Barnason S, Zimmerman L, Nieveen J. The effects of music interventions on anxiety in the patient after coronary artery bypass grafting. Heart Lung. (1995) 24(2):124–32. doi: 10.1016/s0147-9563(05)80007-x
28. Lee D, Henderson A, Shum D. The effect of music on preprocedure anxiety in Hong Kong Chinese day patients. J Clin Nurs. (2004) 13(3):297–303. doi: 10.1046/j.1365-2702.2003.00888
Keywords: music, vitals, Nigeria, state trait anxiety questionnaire (STAI), cataract
Citation: Ezepue CO, Anyatonwu OP, Duru CC, Odini F, Nwachukwu NZ, Onoh C, Nwachukwu N and Oguonu CA (2024) Effects of music on the preoperative and intraoperative anxiety through the assessment of pupil size and vital signs (blood pressure, respiratory, and pulse rates) among cataract surgery patients at UNTH-Enugu. Front. Ophthalmol. 3:1340752. doi: 10.3389/fopht.2023.1340752
Received: 18 November 2023; Accepted: 14 December 2023;
Published: 15 January 2024.
Edited by:
Barbara Pierscionek, Anglia Ruskin University, United KingdomReviewed by:
Ovidiu Samoila, University of Medicine and Pharmacy Iuliu Hatieganu, RomaniaAbhishek Mahesh Appaji, BMS College of Engineering, India
Copyright © 2024 Ezepue, Anyatonwu, Duru, Odini, Nwachukwu, Onoh, Nwachukwu and Oguonu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Obinna Princewill Anyatonwu, obynoprincewill@yahoo.com
 Chukwubuike Obiora Ezepue1
Chukwubuike Obiora Ezepue1 Obinna Princewill Anyatonwu
Obinna Princewill Anyatonwu Christian Chukwuka Duru
Christian Chukwuka Duru