- 1Department of Respiratory and Critical Care Medicine, People’s Hospital of Yangjiang, Yangjiang, China
- 2National Center for Respiratory Medicine, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China
- 3Department of Allergy and Clinical Immunology, First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China
Background: Body mass index (BMI) is known to affect the outcomes of spirometry indices. However, its association with spirometry indices in COPD and asthma is less studied. We aimed to explore the impact of BMI on these patients.
Methods: Patients with COPD or asthma who completed bronchodilator tests (BDTs) between 2017 and 2021 were reviewed. Spirometry indices were compared among patients with COPD or asthma that were subclassified as underweight (BMI< 18.5 kg/m2), normal weight (≥18.5 to < 25), overweight (≥ 25 to < 30), and obesity (≥ 30). Results.
Results: Analysis was conducted on 3891 COPD patients (age:66.5 ± 7.8 years) and 1208 asthma patients (age:59.7 ± 7.5 years). COPD patients classified as underweight demonstrated significantly lower values of pre-and post FEV1 (L, %), pre-and post FVC (L, %), and pre- and post-FEV1/FVC (all p < 0.05). In contrast, COPD patients who were overweight or obese exhibited higher values for pre-and post FEV1 (L, %), and pre and post FEV1/FVC (all p < 0.05). Within the cohort of asthma patients, those underweight had lower pre-and post FEV1 (L, %), pre and post FVC (L, %), pre and post FEV1/FVC %. Obese asthma patients displayed higher pre and post FEV1/FVC (all p < 0.05).
Conclusion: Significant BMI category differences in spirometry indices can be seen in patients with COPD or asthma. Both underweight and obesity could affect the diagnosis and severity of these diseases. Recognizing these effects is essential to better management and diagnosis of these patients.
Introduction
Spirometry plays a crucial role in the prognostication, diagnosis, and monitoring of chronic obstructive respiratory diseases, particularly chronic obstructive pulmonary disease (COPD) and asthma (Liou and Kanner, 2009; Halpin et al., 2021). International guidelines recommend the use of spirometry indices, specifically the pre- and post-bronchodilator test (BDT) forced expiratory volume in the first second (FEV1), forced vital capacity (FVC), and FEV1/FVC values, for the diagnosis and evaluation of COPD and asthma (Pellegrino et al., 2005; Halpin et al., 2021; Stanojevic et al., 2021; Reddel et al., 2022). It is important to note that these spirometry indices can be influenced not only by age, sex, and race, but also by factors such as height, weight, and body mass index (Talaminos Barroso et al., 2018; Mozun et al., 2022; Shah et al., 2022).
The impact of COPD and asthma on the global population is significant both financially and medically (GBD Chronic Respiratory Disease Collaborators, 2020). Lung function tests, particularly spirometry indices, should be correctly employed for the detection and treatment of these illnesses, as well as for understanding the factors that may affect them (Dharmage et al., 2023). BMI is a crucial factor associated with the nature and severity of COPD and asthma. Higher BMI has been linked to lower all-cause mortality and a decreased risk of COPD, but conversely, lower BMI has been linked to an increased risk of COPD and its exacerbations (Guo et al., 2016; Zhang et al., 2021; Shin et al., 2022). Furthermore, patients with asthma who have higher BMI also have higher respiratory burden scores (Klepaker et al., 2022). The effect of BMI categories on spirometry indices in COPD and asthma, however, has not been thoroughly researched. Therefore, investigations examining their connections are necessary.
In order to better manage, evaluate, and diagnose COPD and asthma, it may be valuable to recognize BMI differences in spirometry indices. Therefore, the aim of the present study was to explore the association of BMI with spirometry indices in COPD and asthma.
Materials and methods
Study design
This retrospective study included patients with COPD or asthma from the First Affiliated Hospital of Guangzhou Medical University who had at least one BDT between 2017 and 2021. The study was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University (approval NO.2020124). BMI was calculated based on the measurement of height and weight from the BDT record. BMI categories were classified into underweight (BMI< 18.5 kg/m2), normal weight (≥18.5 to <25), overweight (≥25 to <30), and obesity (≥30).
Study population
Patients who underwent BDTs between 2017 and 2021 and had been diagnosed with COPD or asthma were included in the study. COPD was defined as a post-BDT FEV1/FVC ratio less than 0.7 according to the Global Initiative for Chronic Obstructive Lung Disease guidelines (Halpin et al., 2021). Asthma was defined on the basis of a history of asthma diagnosis by a pulmonologist that met the diagnostic criteria of the Global Initiative for Asthma guidelines (Reddel et al., 2022). Exclusion criteria: 1) Quality control of pulmonary function testing was not acceptable; 2) Patients who had other chronic respiratory diseases, such as lung cancer, bronchiectasis, interstitial lung disease; 3) The weight or height value was incomplete.
Bronchodilator tests
BDTs were performed using the MasterScreen-Pneumo PC (Jaeger, Germany) and QuarkPFT (COSMED, Italy) spirometers (Wang et al., 2021). All test procedures and results interpretation were performed by trained technicians based on the American Thoracic Society and European Respiratory Society guidelines (Pellegrino et al., 2005; Graham et al., 2019). At least three acceptable maneuvers were needed and the highest measurement is used. Spirometry parameters including FEV1, FVC, and FEV1/FVC were obtained and expressed as absolute and %predicted (%) values. Reference equations for predicted values of spirometry indices were using the Global Lung Function 2012 equations (Quanjer et al., 2012).
Statistical analysis
Data are presented as absolute numbers (percentages) in case of frequencies, median values and quartiles in case of continuous parameters. Count data were analyzed by using the χ2 test. Median inter-group comparisons were using the Kruskal–Wallis test. A p-value of <0.05 was considered statistically significant. Statistical analyses were performed with SPSS version 26.0.
Results
Prevalence of BMI categories
A total of 3,891 (93.0% male, n = 3619) patients with COPD were included, with a mean BMI of 21.9 ± 3.5 kg/m2, age 66.5 ± 7.8 years. Among them, there were 675 (17.3%) underweight, 2,496 (64.1%) normal weight, 646 (16.6%) overweight, and 74 (1.9%) obesity. There were 1,207 patients with asthma included, mean BMI 23.9 ± 3.3 kg/m2, age 59.7 ± 7.5 years. Among them, there were 63 (5.2%) underweight, 707 (58.5%) normal weight, 393 (32.5%) overweight, and 45 (3.7%) obesity.
Demographic and clinical characteristics
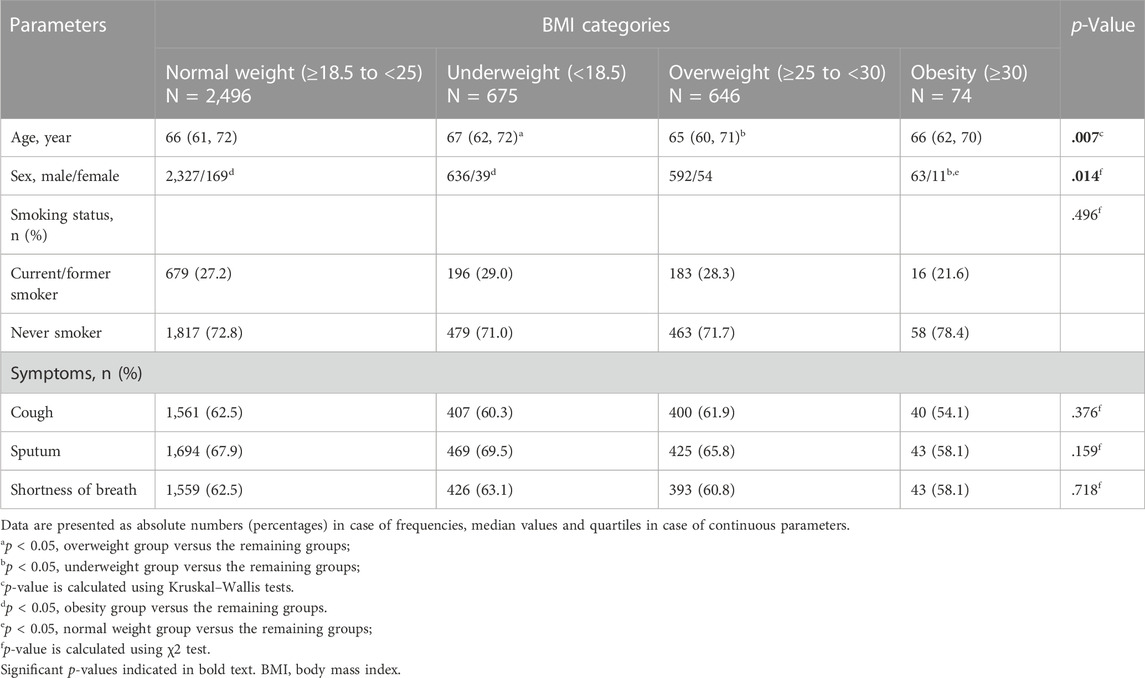
Table 1 demonstrates the demographic and clinical characteristics of patients with COPD. Patients in the underweight group were more likely to be older compared to the overweight group (p = 0.007). In addition, the obesity group showed a lower ratio of female patients in comparison with the underweight and overweight groups (p = 0.014). There were no significant differences among all groups in smoking status and symptoms including cough, sputum, and shortness of breath.
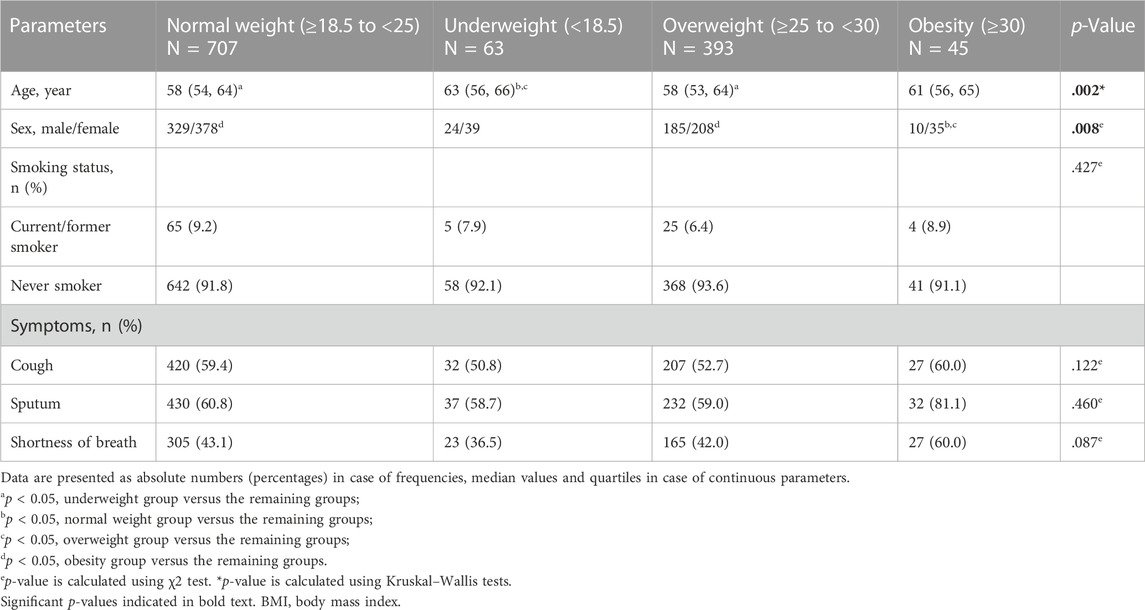
In asthma, patients in the underweight group were older than normal weight and overweight groups (p = 0.002). The obesity group had a lower ratio of female patients when compared with the normal and overweight groups. Same as patients with COPD, patients with asthma showed no significant differences among all groups in smoking status and symptoms. Detailed information can be found in Table 2.
BMI categories difference in spirometry indices
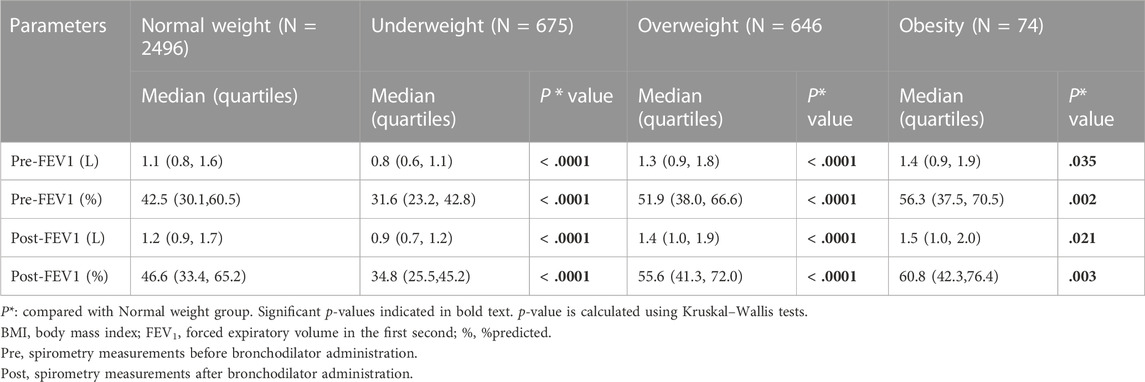
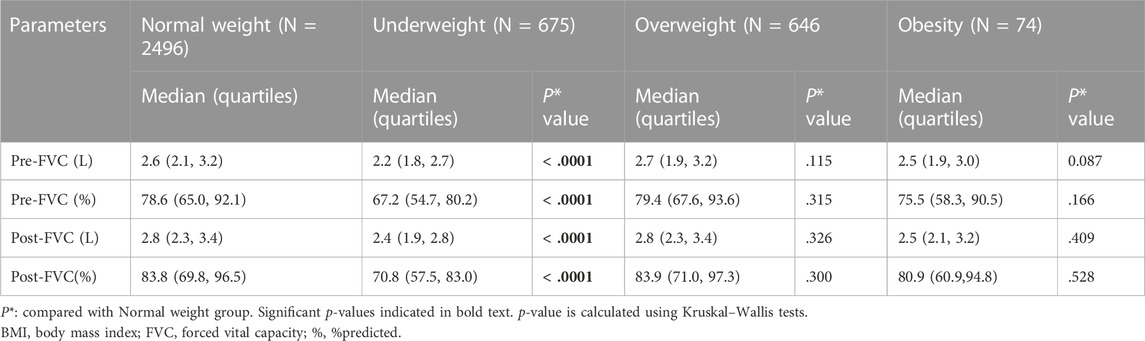
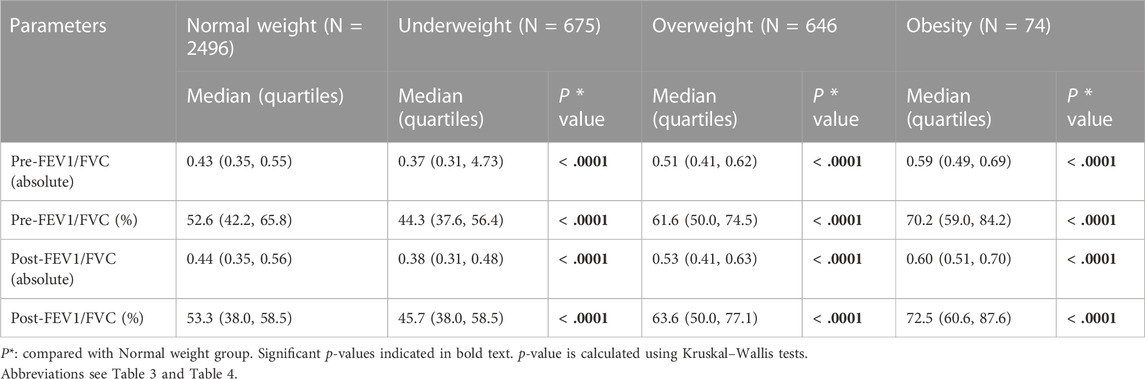
Within the COPD cohort, the normal weight group was used as the reference, underweight group had lower pre-and post FEV1 (L, %), pre- and post FVC (L, %), and pre-and post-FEV1/FVC (absolute value, %) (all p < 0.0001). Overweight and obesity groups had higher pre- and post FEV1 (L, %) (all p < 0.05), and pre-and post-FEV1/FVC (absolute value, %) (all p < 0.0001). However, pre-and post FVC (L, %) showed no significant differences (Table 3; Table 4; Table 5).
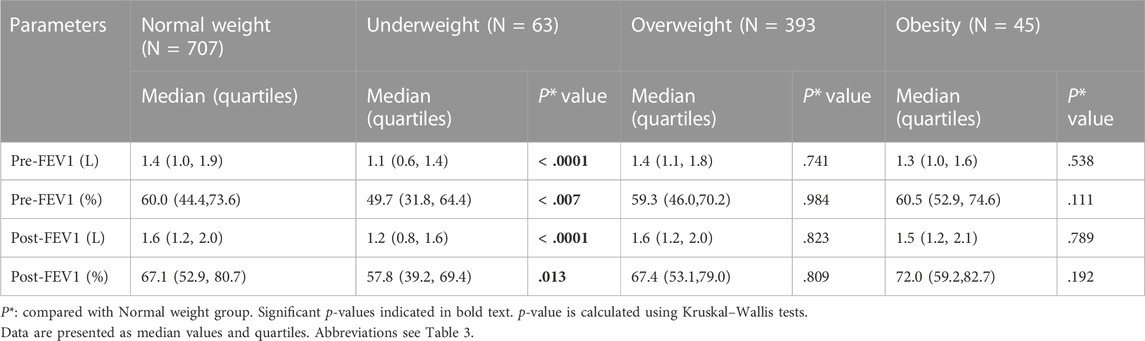
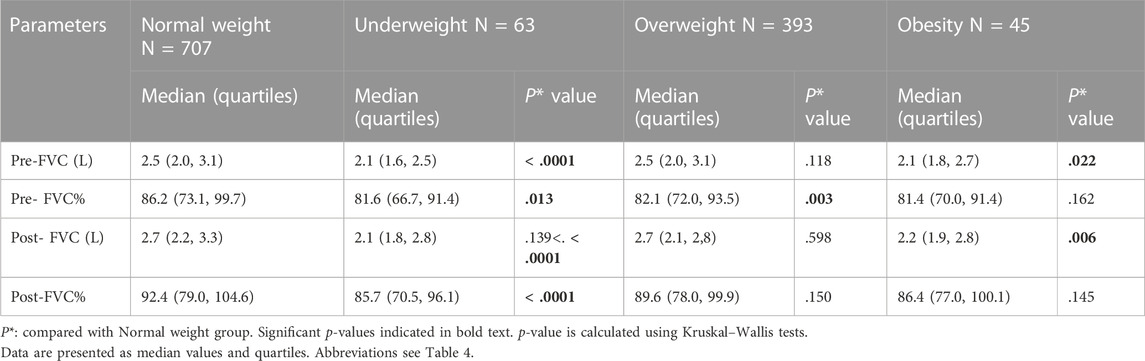
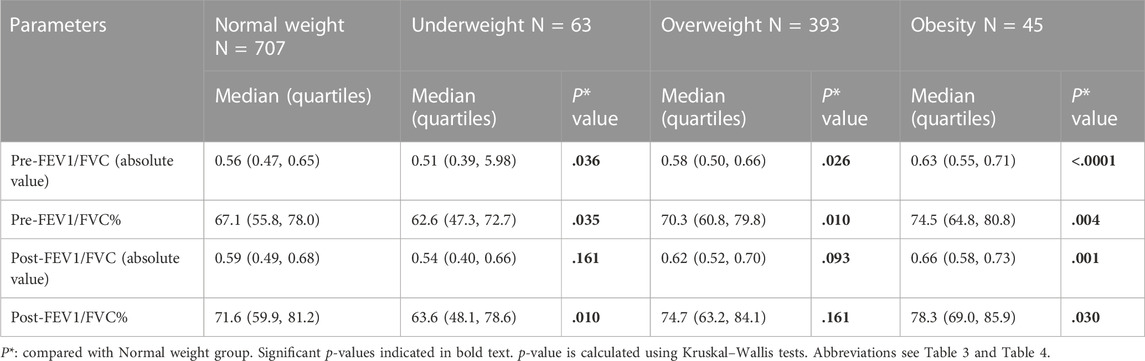
Table 6, Table 7, and Table 8 showed results of patients with asthma that used normal weight group as the reference. Underweight group had lower pre-and post FEV1 (L, %) (all p < 0 .05), pre-and post FVC (L, %) all p < 0.05), pre-FEV1/FVC (absolute value) (p = 0.036), pre-and post- FEV1/FVC (%) (p = 0.035 and p = 0.010, respectively). Overweight and obesity groups had higher pre-FEV1/FVC (absolute value, %) (p = 0.026, p = 0.010, p < 0.0001, p = 0.010, and p = 0.004, respectively). Obesity group showed higher post-FEV1/FVC (absolute value, %) (p = 0.001 and p = 0.030, respectively). What’s more, obesity group had lower pre-and post FVC (L) (p = 0.022 and p = 0.006, respectively), and overweight group had lower pre-FVC% (p = 0.003). However, overweight and obesity groups had no significant differences in pre-and post-FEV1 (L, %) compared with the normal weight group.
Discussion
In the present study, the association of BMI categories of spirometry indices in patients with COPD or asthma were analyzed, respectively. In COPD, the prevalence of underweight was much higher than in obese patients. Underweight could worsen the FEV1%, FVC%, as well as the FEV1/FVC (absolute value, %), conversely overweight and obesity could make FEV1% and FEV1/FVC (absolute value, %) much better in COPD patients. On contrary, patients with asthma showed higher prevalence of overweight and obesity than underweight. Within the cohort of asthma, underweight also decreased FEV1%, FVC%, and FEV1/FVC (absolute value, %), but overweight and obesity did not affect spirometry indices except FEV1/FVC.
In patients with COPD, the proportion of the underweight category is near 20%, moreover, this category was older than the normal weight category. According to a report from World Health Organization, undernutrition is among the key driver of other respiratory diseases, like tuberculosis (World Health Organization, 2022). It serves as a reminder that undernutrition in older COPD patients should be more closely monitored by patients and physicians. Conversely, patients with asthma had a higher prevalence of overweight and obesity. Obesity is regarded as a health epidemic worldwide (Afshin et al., 2017). In asthma, more attention should be paid to the effect of higher BMI categories on pulmonary function.
The association between BMI and lung function in respiratory diseases has been previously examined. Schaeffer et al. (Schaeffer et al., 2022) used linear regression to assess the association of BMI with lung function in interstitial lung disease. They found that total lung capacity and residual volume% were worse in patients with overweight and obese BMI, and the obesity was associated with a lower FVC%. What’s more, the underweight BMI category was also associated with a higher residual volume%. Lee et al. (Lee et al., 2022) explored the risk of impaired lung function among obese individuals without metabolic abnormalities, subjects with metabolically-healthy obesity had the highest FEV1% and FVC% but the lowest FEV1/FVC ratio compared with non-obese and metabolically unhealthy obese subjects. Another study included 72 men with COPD also showed that BMI was positively correlated with FEV1 (r = 0.275, p = 0.020) (Sami et al., 2018). Although there are some similarities to the results of previous studies, our findings have differences. We assessed both pre-BDTs and post-BDTs indices, especially the post-FEV1/FVC ratio< 0.7 is the most crucial parameter for diagnosing COPD, so it is important to assess the association of BMI with this parameter. In addition, our research found no significant difference in FEV1 and FVC but a higher FEV1/FVC ratio in obese asthma patients, which is inconsistent with Lee et al. (Lee et al., 2022). The lower trend of FVC and subtle change of FEV1 may be the reason for the higher FEV1/FVC.
The present study investigated the association of BMI categories with spirometric indices based on patients with moderate to severe ventilatory dysfunction in COPD and asthma. It demonstrates the harm of the underweight BMI category for pulmonary function in both COPD and asthma, which may be explained by nutrient deficiencies. Our findings on gained residual volume in underweight individuals are consistent with a previous study in interstitial lung disease (Schaeffer et al., 2022). In overweight and obesity groups, the higher spirometry indices in COPD were observed. It may due to restriction by the loading of obesity reduced hyperinflation from the balance of obstructive respiratory disease (Ora et al., 2009; Choe et al., 2018). However, excess fat not only promotes the secretion of a range of inflammatory factors, but fat accumulation can also cause internal organs to be squeezed, which affects the breathing of the lung function (Choe et al., 2018). Hence, the relationship between obesity and lung function in COPD patients remains to be further clarified. In contrast, the worse trend of FVC% were found in higher BMI categories in asthma. It is possible due to excess weight exacerbates the restrictive defect of asthma. A previous study also demonstrated reduced lung volumes in obese subjects without lung disease (Jones and Nzekwu, 2006).
Despite the study having explored the association of BMI with spirometry indices, it had some limitations. Firstly, the data we used was all acquired from BDTs, since most of the time BDT was completed when FEV1% < 70%, subjects with normal or mild severity ventilatory dysfunction would be mostly excluded. As a result, we could not know the effect of BMI on these populations. In the future, we should include these subjects to generalize the scope of the study. Secondly, the BDTs records we used were all from the Chinese population. Considering that race is one of the critical impactors of normal spirometry values, it is possible that BMI categories have different effects on other ethnicities. Additionally, we only evaluated COPD and asthma, other common chronic obstructive respiratory diseases, such as bronchiectasis, cystic fibrosis, etc., were not studied.
Conclusion
To conclude, the lowest BMI has a negative impact on spirometry indices in both COPD and asthma. Increasing BMI may positively affect pulmonary function in COPD. Pulmonologists and physicians should pay attention to these effects to better diagnose and manage patients. Maintaining a suitable BMI is important for patients with asthma or COPD. Weight maintenance should be embedded in the management of these illnesses.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University (approval No. 2020-124). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
Study design and hypothesis generation XW, HG, YW, YG, and ZZ. Data acquisition, analysis, or interpretation XW, YW, XY, BS, JA, and YG. Chart review and manuscript preparation XW, HG, YW, and ZZ. Critical revision BS, YG, and ZZ. Funding was obtained by BS, YG, and ZZ. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Science and Technology Program of Guangzhou, China (202007040003); the Guangdong Basic and Applied Fundamental Research Fund (2020A1515110007); the Zhong Nanshan Medical Foundation of Guangdong Province (ZNSA-2020003, No. 202102010347; ZNSA-2020013); and the National Natural Science foundation of China (82100036, 82161138020, and U1801286).
Acknowledgments
We wish to thank Xiangqing Hou who helped the statistical analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BDT, bronchodilator test; BMI, body mass index; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1s; FVC, forced vital capacity; %, %predicted.
References
Afshin A., Forouzanfar M. H., Reitsma M. B., Sur P., Estep K., Lee A., et al. (2017). Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 377, 13–27. doi:10.1056/nejmoa1614362
Choe E. K., Kang H. Y., Lee Y., Choi S. H., Kim H. J., Kim J. S. (2018). The longitudinal association between changes in lung function and changes in abdominal visceral obesity in Korean non-smokers. PLoS One 13, e0193516. doi:10.1371/journal.pone.0193516
Dharmage S. C., Bui D. S., Walters E. H., Lowe A. J., Thompson B., Bowatte G., et al. (2023). Lifetime spirometry patterns of obstruction and restriction, and their risk factors and outcomes: a prospective cohort study. Lancet. Respir. Med. 11, 273–282. doi:10.1016/s2213-2600(22)00364-2
GBD Chronic Respiratory Disease Collaborators (2020). Prevalence and attributable health burden of chronic respiratory diseases, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 8, 585–596. doi:10.1016/S2213-2600(20)30105-3
Graham B. L., Steenbruggen I., Miller M. R., Barjaktarevic I. Z., Cooper B. G., Hall G. L., et al. (2019). Standardization of spirometry 2019 update. An official American thoracic society and European respiratory society technical statement. Am. J. Respir. Crit. Care Med. 200, e70–e88. doi:10.1164/rccm.201908-1590ST
Guo Y., Zhang T., Wang Z., Yu F., Xu Q., Guo W., et al. (2016). Body mass index and mortality in chronic obstructive pulmonary disease: a dose-response meta-analysis. Med. Baltim. 95, e4225. doi:10.1097/MD.0000000000004225
Halpin D. M. G., Criner G. J., Papi A., Singh D., Anzueto A., Martinez F. J., et al. (2021). Global initiative for the diagnosis, management, and prevention of chronic obstructive lung disease. The 2020 GOLD science committee report on COVID-19 and chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 203, 24–36. doi:10.1164/rccm.202009-3533so
Jones R. L., Nzekwu M. M. (2006). The effects of body mass index on lung volumes. Chest 130, 827–833. doi:10.1378/chest.130.3.827
Klepaker G., Henneberger P. K., Torén K., Brunborg C., Kongerud J., Fell A. K. M. (2022). Association of respiratory symptoms with body mass index and occupational exposure comparing sexes and subjects with and without asthma: follow-up of a Norwegian population study (the Telemark study). BMJ Open Respir. Res. 9, e001186. doi:10.1136/bmjresp-2021-001186
Lee J., Park H. K., Kwon M. J., Ham S. Y., Lim S. Y., Song J. U. (2022). The effect of metabolic health and obesity on lung function: a cross sectional study of 114,143 participants from Kangbuk Samsung Health Study. PLoS One 17, e0266885. doi:10.1371/journal.pone.0266885
Liou T. G., Kanner R. E. (2009). Spirometry. Clin. Rev. Allergy Immunol. 37, 137–152. doi:10.1007/s12016-009-8128-z
Mozun R., Ardura-Garcia C., Pedersen E. S. L., Usemann J., Singer F., Latzin P., et al. (2022). Age and body mass index affect fit of spirometry Global Lung Function Initiative references in schoolchildren. ERJ Open Res. 8, 00618–02021. doi:10.1183/23120541.00618-2021
Ora J., Laveneziana P., Ofir D., Deesomchok A., Webb K. A., O'Donnell D. E. (2009). Combined effects of obesity and chronic obstructive pulmonary disease on dyspnea and exercise tolerance. Am. J. Respir. Crit. Care Med. 180, 964–971. doi:10.1164/rccm.200904-0530OC
Pellegrino R., Viegi G., Brusasco V., Crapo R. O., Burgos F., Casaburi R., et al. (2005). Interpretative strategies for lung function tests. Eur. Respir. J. 26, 948–968. doi:10.1183/09031936.05.00035205
Quanjer P. H., Stanojevic S., Cole T. J., Baur X., Hall G. L., Culver B. H., et al. (2012). Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur. Respir. J. 40, 1324–1343. doi:10.1183/09031936.00080312
Reddel H. K., Bacharier L. B., Bateman E. D., Brightling C. E., Brusselle G. G., Buhl R., et al. (2022). Global initiative for asthma strategy 2021: executive summary and rationale for key changes. Am. J. Respir. Crit. Care Med. 205, 17–35. doi:10.1164/rccm.202109-2205pp
Sami R., Sadegh R., Esmailzadehha N., Mortazian S., Nazem M., Zohal M. (2018). Association of anthropometric indexes with disease severity in male patients with chronic obstructive pulmonary disease in qazvin, Iran. Am. J. men's health 12, 1023–1028. doi:10.1177/1557988318760053
Schaeffer M. R., Kumar D. S., Assayag D., Fisher J. H., Johannson K. A., Khalil N., et al. (2022). Association of BMI with pulmonary function, functional capacity, symptoms, and quality of life in ILD. Respir. Med. 195, 106792. doi:10.1016/j.rmed.2022.106792
Shah H., Mali S., Ranga S., Jadhav C., Rukadikar A., Singh A. K., et al. (2022). Effect of body mass index on cardiorespiratory parameters among medical students: a cross-sectional study. Int. J. Physiol. Pathophysiol. Pharmacol. 14, 4–9.
Shin S. H., Kwon S. O., Kim V., Silverman E. K., Kim T. H., Kim D. K., et al. (2022). Association of body mass index and COPD exacerbation among patients with chronic bronchitis. Respir. Res. 23, 52. doi:10.1186/s12931-022-01957-3
Stanojevic S., Kaminsky D. A., Miller M., Thompson B., Aliverti A., Barjaktarevic I., et al. (2021). ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur. Respir. J. 60, 2101499. doi:10.1183/13993003.01499-2021
Talaminos Barroso A., Márquez Martín E., Roa Romero L. M., Ortega Ruiz F. (2018). Factors affecting lung function: a review of the literature. Arch. Bronconeumol (Engl Ed.) 54, 327–332. doi:10.1016/j.arbres.2018.01.030
Wang Y., Chen W., Li Y., Zhang C., Liang L., Huang R., et al. (2021). Clinical analysis of the "small plateau" sign on the flow-volume curve followed by deep learning automated recognition. BMC Pulm. Med. 21, 359. doi:10.1186/s12890-021-01733-x
World Health Organization (2022). Undernutrition, poverty as well as HIV, diabetes and tobacco are among the key drivers of the TB_Poster.
Keywords: asthma, body mass index, chronic obstructive pulmonary disease, spirometry, obese
Citation: Wang X, Gan H, Wang Y, Yu X, An J, Sun B, Gao Y and Zhu Z (2023) Body mass index affects spirometry indices in patients with chronic obstructive pulmonary disease and asthma. Front. Physiol. 14:1132078. doi: 10.3389/fphys.2023.1132078
Received: 26 December 2022; Accepted: 20 November 2023;
Published: 01 December 2023.
Edited by:
Giuseppe Guida, University of Turin, ItalyReviewed by:
Paula Kauppi, Hospital District of Helsinki and Uusimaa, FinlandMaria Michelle Papamichael, La Trobe University, Australia
Copyright © 2023 Wang, Gan, Wang, Yu, An, Sun, Gao and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Baoqing Sun, sunbaoqing@vip.163.com; Yi Gao, mistall2@163.com; Zheng Zhu, ching1262006@126.com
†These authors have contributed equally to this work
 Xiaohu Wang
Xiaohu Wang Hui Gan
Hui Gan Yimin Wang
Yimin Wang Xinxin Yu2
Xinxin Yu2 Zheng Zhu
Zheng Zhu