- 1Susan B. Meister Child Health Evaluation and Research Center, Department of Pediatrics, University of Michigan Medical School, Ann Arbor, MI, United States
- 2Division of General and Community Pediatrics, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States
- 3Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH, United States
- 4Centre for Practice-Changing Research, Ottawa Hospital Research Institute, Ottawa, ON, Canada
- 5Patient/Parent/Caregiver Stakeholder Partners, Denver, CO, United States
- 6School of Nursing, University of Ottawa, Ottawa, ON, Canada
- 7Patient/Parent/Caregiver Stakeholder Partners, Ann Arbor, MI, United States
- 8Department of Pediatrics, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY, United States
- 9Institute of Molecular Medicine, Feinstein Institute for Medical Research, Manhasset, NY, United States
- 10Division of Endocrinology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States
- 11Department of Pediatrics, University of Utah Spencer Fox Eccles School of Medicine, Salt Lake City, UT, United States
- 12Division of Urology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States
- 13Division of Pediatric Surgery, Phoenix Children’s Hospital, Phoenix, AZ, United States
- 14Accord Alliance, Higley, AZ, United States
- 15Division of Pediatric Psychology, Department of Pediatrics, University of Michigan Medical School, Ann Arbor, MI, United States
Introduction: Parents of infants and young children newly diagnosed with differences of sex development (DSD) commonly face medical and psychosocial management decisions at a time when they are first learning about the condition and cannot consult their child for input. The aim of this study was to identify areas of greatest need for parental decisional support.
Methods: 34 parents of children receiving care for DSD at one of three US children’s hospitals participated in a survey to learn what clinical and psychosocial decisions needed to be made on behalf of their child. Parents were then asked to identify and focus on a “tough” decision and respond to questions assessing factors affecting decision-making, decision-making preferences, decisional conflict, and decision regret. Descriptive analyses were conducted.
Results: Decisions about surgery and aspects of sharing information about their child’s condition with others were the two most frequently reported decisions overall, experienced by 97% and 88% of parents, as well as most frequently nominated as tough decisions. Many parents reported mild to moderate levels of decisional conflict (59%) and decision regret (74%). Almost all parents (94%) reported experiencing at least one factor as interfering with decision-making (e.g., “worried too much about choosing the ‘wrong’ option”). Parents universally reported a desire to be involved in decision-making – preferably making the final decision primarily on their own (79%), or together with their child’s healthcare providers (21%). The majority of parents judged healthcare providers (82%) and patient/family organizations (58%) as trustworthy sources of information.
Discussion: Parents of children with DSD encounter medical, surgical, and psychosocial management decisions. Despite difficulties including emotional distress and informational concerns (including gaps and overload), parents express strong desires to play key roles in decision-making on behalf of their children. Healthcare providers can help identify family-specific needs through observation and inquiry in the clinical context. Together with families, providers should focus on specific clinical management decisions and support parental involvement in making decisions on behalf of young children with DSD.
1 Introduction
Defined as congenital conditions in which chromosomal, gonadal, and/or anatomic sex development is atypical, the umbrella term “disorders of sex development” (DSD)1(1) comprises a set of discrete diagnoses that present with a wide range of genital and reproductive anatomies (2, 3). Decisions, including those regarding gender of rearing, genetic testing, genital or gonadal surgery, and disclosure of the diagnosis, commonly arise (2–4).
Birth of a child with a DSD and uncertainties about the child’s physical health, gender, and psychosexual development are characterized as extraordinarily stressful (4, 5) and exert substantial strain on families (6, 7). In addition to healthcare decisions, challenges associated with having a child born with DSD can include changes in parental roles, responsibilities, goals, and social status (8). Parents describe both inadequate information and information overload, medical jargon and dismissive comments from healthcare providers, strong negative emotions (e.g., fear, guilt, uncertainty, shock, disbelief), and feeling overwhelmed (4, 8, 9), resulting in difficulty processing their child’s diagnosis (10). Parents worry that sharing information about their child’s condition will lead to rumors, gossip, and teasing; this, in turn, leads to isolation and withdrawal from usual support systems (4, 11, 12). Recognized by activists and providers, fear of stigmatization (6, 13–15) can precipitate parental decisions to surgically “fix” or “normalize” their child’s appearance before becoming fully informed about all options and properly weighing harms and benefits of surgery (16–19). Decisions involving genital surgery in young children, wherein parents reported being poorly informed or experiencing decisional conflict, were associated with decisional regret (20).
Despite such pressures, parents of children with DSD remain responsible for making decisions on behalf of their children and need to be able to participate in decision-making with clinicians. Following principles of patient- and family-centered care (a term intended to explicitly capture the importance of engaging the family and patient as essential healthcare team members) (21), the objective of shared decision-making (SDM) is to help make informed, preference-based clinical management choices among several relevant options (22). More specifically, SDM is a collaborative process where patients/parents and providers actively engage in healthcare decision-making by recognizing and acknowledging a decision is needed; discussing the best available evidence for each option, as well as their associated benefits and harms; and determining a preferred option by exploring patients’/parents’ informed preferences for option outcomes (23). Decision aids for healthcare decisions are tools that support SDM between patients/parents and providers by making the decision and treatment options explicit, providing evidence-based information about the associated benefits/harms, and helping patients to consider what matters most to them in relation to the possible outcomes (24).
Unmet parental decision-making needs may serve as barriers to applying SDM principles and use of decision aids. A recent study of healthcare providers identified several central “needs” of parents of children with a DSD: addressing parental distress and informational overload; information gaps including knowledge of the condition, options, and their features; and identification and incorporation of parental values for features of options (25). However, studies of decisional needs have not been conducted with parents of children with a DSD (26, 27). The aim of this study was to identify areas of greatest need for parental decisional support by assessing decisional experiences and preferences of parents of children with DSD.
2 Materials and methods
2.1 Study design
Parents of minor patients with DSD were recruited for participation in a web-based cross-sectional descriptive study between July and November 2021. The core Research Team convened a Steering Committee, comprised of those with complementary skills and experiences to those on the Research Team. Healthcare providers specializing in DSD (n=3), those directly affected by DSD (parent and/or adult patient; n=3, 2 of whom serve in patient advocacy leadership roles), and SDM or clinical researchers (n=6, inclusive of a member serving a dual provider/researcher role) comprised the full Research Team and Steering Committee. Including end users throughout the project ensured survey results would be relevant to them (28). The Research Team and Committee co-developed, conducted, and interpreted the findings of a survey focused on elucidating parental decisional needs. The study was guided by the Ottawa Decision Support Framework (ODSF) that conceptualizes the support needed by patients, families, and their healthcare providers for difficult decisions with multiple options whose features are valued differently (29). Recently updated after 20 years of use, the ODSF served to inform the survey development and analysis. Study protocol received ethical approval by the lead site’s Institutional Review Board (IRB), to which other sites’ IRBs had formally ceded oversight.
2.2 Participants and setting
Parents of children being seen for the assessment and/or ongoing clinical management of DSD at one of three medical centers with specialty DSD services were recruited. Patients served as index cases, not participants. DSD was defined following the 2006 Consensus Statement and 2016 Global Update definition: “congenital conditions within which the development of chromosomal, gonadal or anatomical sex is atypical” (2, 3); however, uncomplicated distal hypospadias, Klinefelter and Turner syndromes were excluded, as they do not present parents with the decisions commonly faced by parents of infants and young children with other DSD; e.g., genital and/or gonadal surgery. Case ascertainment lists were derived from electronic medical chart review using ICD-9 and -10 codes and DSD-related keywords (30). Patient age was limited to 18 and younger at the time of parent recruitment. Parent was broadly defined to include biological-, adoptive-, and step-parents, and other guardians who take active roles in managing their child’s condition. All eligible parents meeting those criteria with functional literacy in English were invited to participate.
Each of the three medical centers are children’s hospitals and members of the US-based Differences of Sex Development – Translational Research Network: a consortium of hospitals, medical centers, and a DSD-related non-profit advocacy and educational organization, working together to advance research, education, and clinical (31, 32). Sites regularly see patients aged newborn through young adulthood, with one having a greater focus on adolescent and young adult patients.
2.3 Recruitment and procedures
Participants were provided information about the study by research staff. For those whose clinic visits coincided with the recruitment window, recruitment was accomplished in person; otherwise, the initial contact was by phone. Individualized links to an online consent form and the survey were provided to those indicating interest in participation by email. Up to three reminders to complete the survey were sent after the initial email. Participants were provided a $20 honorarium for their time.
2.4 Materials
A survey, guided by the ODSF, focused on parental decisional needs was developed and included established (the Decisional Conflict (33), Decision-Making Preference (34), and Decision Regret (35) Scales) and novel measures (see Supplementary Material). The Decisional Conflict scale is a 16-item survey, scored 0 (no decisional conflict) to 100 (extremely high decisional conflict), with scores lower than 25 associated with implementing decisions and scores exceeding 37.5 associated with decision delay; test-retest and Cronbach alpha coefficients exceed 0.78; and the measure discriminates between known groups: those who make and delay decisions (effect size range 0.4 to 0.8) (33). The Decision-Making Preference scale assesses the degree of control desired in decision-making using a 5-point response scale, ranging from complete patient/parent control, through collaborative control, to complete healthcare provider control (34). The Decision Regret scale is a 5-item questionnaire; alpha coefficients range from 0.81 to 0.92; scale scores correlate with decision satisfaction (r’s=0.40 to -0.60) and decisional conflict (r’s = 0.31 to 0.52) (35); scores range from 0 to 100, with 0 indicating no decision regret, 1-25 mild regret, and >25 moderate to strong regret (36, 37).
The survey also included new items based on principles of SDM and decision aid development as informed by the ODSF, literature review, collective experiences of the Research Team and Steering Committee, and preliminary results of a recent survey of healthcare provider perspectives on parental decisional needs in DSD (25). After being asked what types of decisions parents have encountered related to their child’s DSD care, parents were asked to focus on a “tough” decision (a decision is tough when there is more than one option and none is clearly the best) and to describe it, including when it occurred. Subsequent survey items were completed in reference to that specific decision and the survey branched using wording to reflect whether the decision occurred in the past or was currently in the process of being made. The Decision Regret Scale and Decisional Conflict Effectiveness subscale were administered to those who indicated their tough decision had been made in the past. Following alpha testing to address functionality and usability, the survey was pilot tested with an adult living with DSD and two parents of a child with DSD focusing on user acceptance – with feedback provided both within free text blocks within the survey and verbally after survey completion.
2.5 Data analysis plan
Descriptive statistics (i.e., frequencies, percentages, means, standard deviations) are reported for quantitative items concerning parental decisional needs. Qualitative items (e.g., participant descriptions of tough decisions) were reviewed by three authors (MG, TS-K, EW) and coded for themes following a phenomenological approach (38) in which responses were read in their entirety, then salient themes were identified and mapped onto to the ODSF. Differences in coding were resolved through discussion that included KS-J and DES. In the one instance where two parents of the same index cases participated, data for both parents were retained given literature showing differences in experiences and needs for both in other pediatric health conditions (39, 40) and a preliminary review of data showing participants described different “tough” decisions experienced at different times in their child’s life.
3 Results
3.1 Participant characteristics
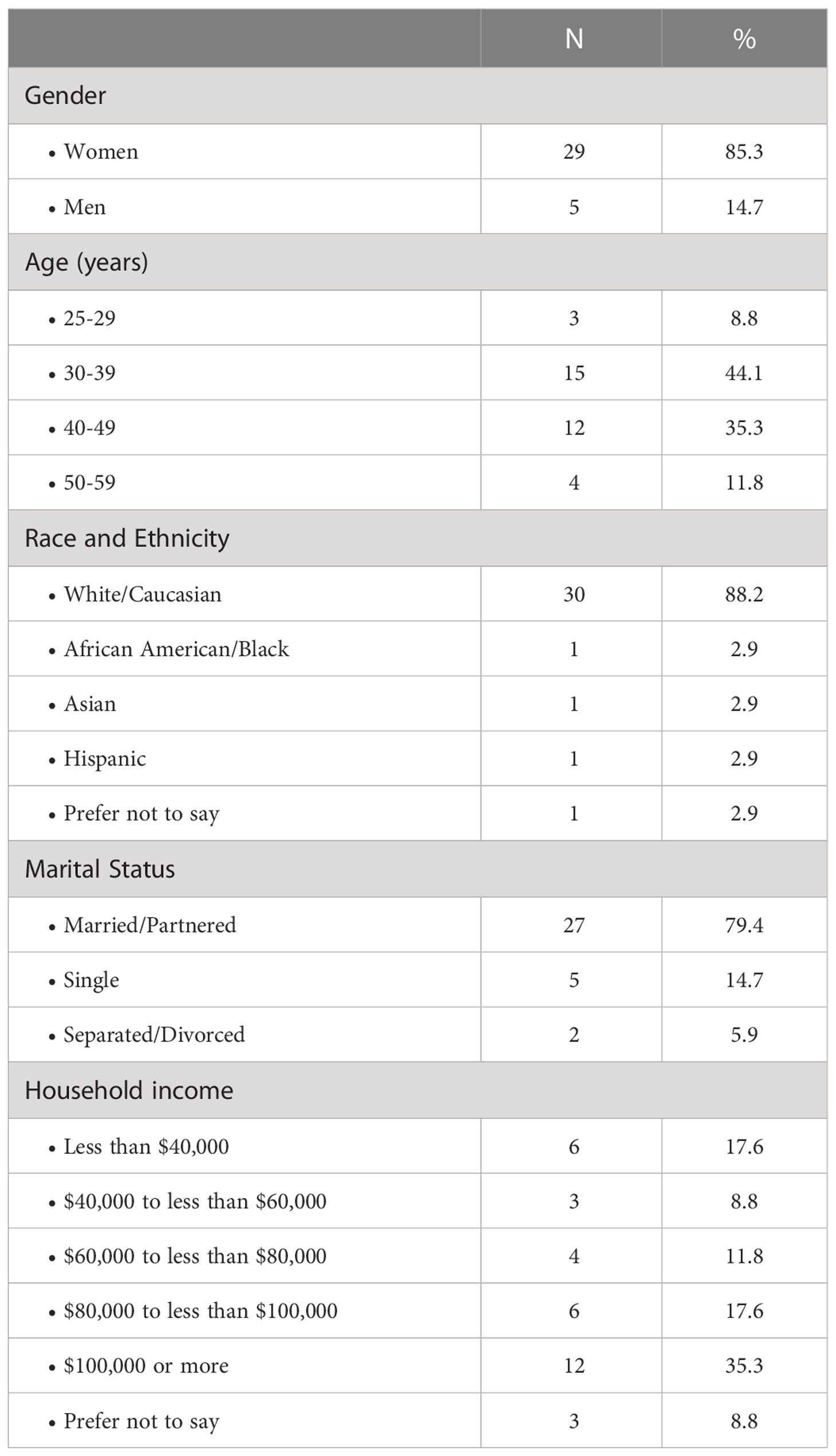
Of 63 parents invited to participate, 39 consented and 34 (54%) completed the survey, representing 33 index cases. Median age group was 30-39 years, most identified as women (n=29, 85%), White/Caucasian (30, 88%), married/partnered (27, 79%), and with a median household income of $80,000 - $100,000 (Table 1). Mean index case age at the time of recruitment was 11.2 ( ± 6.0) years; DSD diagnoses included congenital adrenal hyperplasia (n = 6, 18%), cloacal malformation/bladder exstrophy (6, 18%), complete or mixed gonadal dysgenesis (5, 15%), complete or partial androgen insensitivity syndrome (3, 9%), 17-beta-hydroxysteroid dehydrogenase type 3 deficiency (2, 6%), proximal hypospadias without genetic variant identified (2, 6%), and other individual conditions categorized as 46,XY, 46,XX (4, 12% each), or sex chromosome (1, 3%) DSD.
3.2 Types of decisions
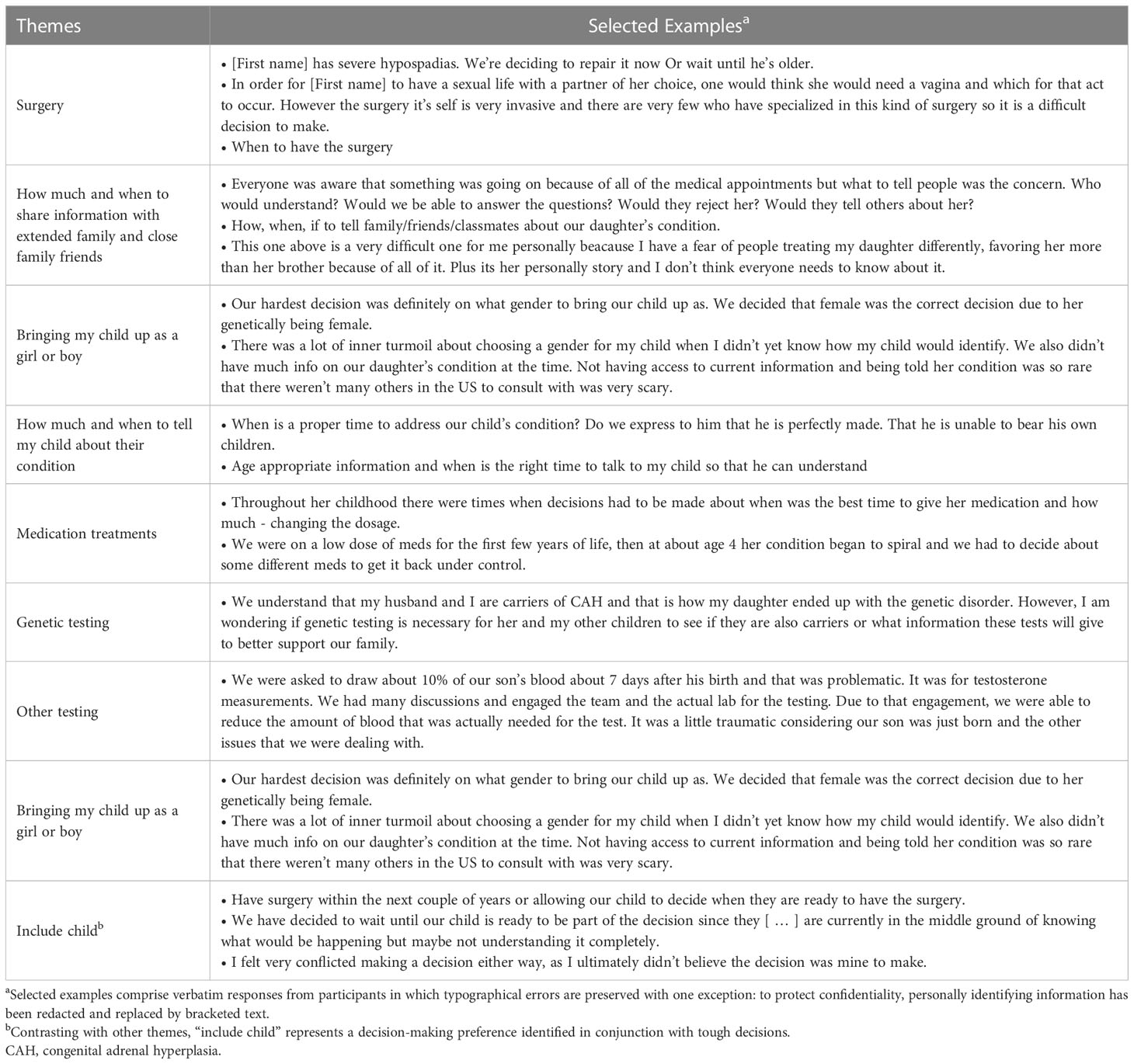
Parents reported being faced with a number of decisions. The two most frequently reported were “Decisions about surgery” (n=33, 97%) and “Decisions about how much and when to share information about my child’s condition to extended family and close family friends” (30, 88%) (Table 2).
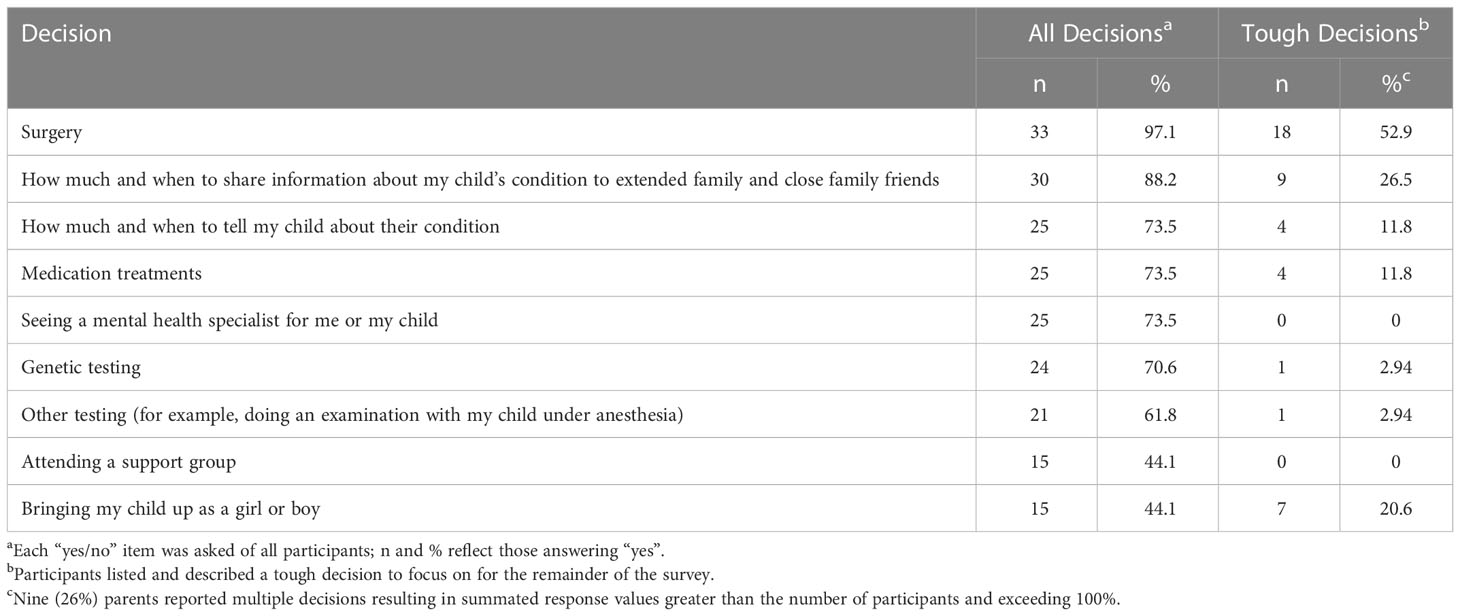
Table 2 Types of decisions made on behalf of children: Number (%) of parents making decisions about a topic.
3.3 Tough decisions
When asked to narrow the decisions to those categorized as “tough” and describe them, seven were identified: those concerning surgery (n=18, 53%); disclosing the child’s medical condition to friends, family and others (9, 26%); gender of rearing (7, 21%); educating the child about their condition and its management (4, 12%); medication treatment (4, 12%); and genetic or endocrine testing (2, 6%) (Tables 2, 3). Nine (26%) parents reported more than one tough decision – some of which were overlapping. Common overlapping concerns were those regarding surgery and gender of rearing/gender identity (e.g., “Raising our daughter as male and not having surgery, [raising] her as female and having surgery”) and how much and when to tell extended family and friends as well as how much and when to educate the child about their own condition (e.g., “Not telling some family/friends. Also not telling our daughter until she is older, for fear she would tell others not understanding the consequences of her sharing.”). The majority (23, 68%) indicated the tough decision occurred in the past and 11 (32%) reported currently making the decision. Of those reporting past decisions, 3 (13%) occurred in within the last year, 5 (22%) 2-4 years ago, and 14 (61%) 5+ years ago; 1 (4%) reported not remembering when.
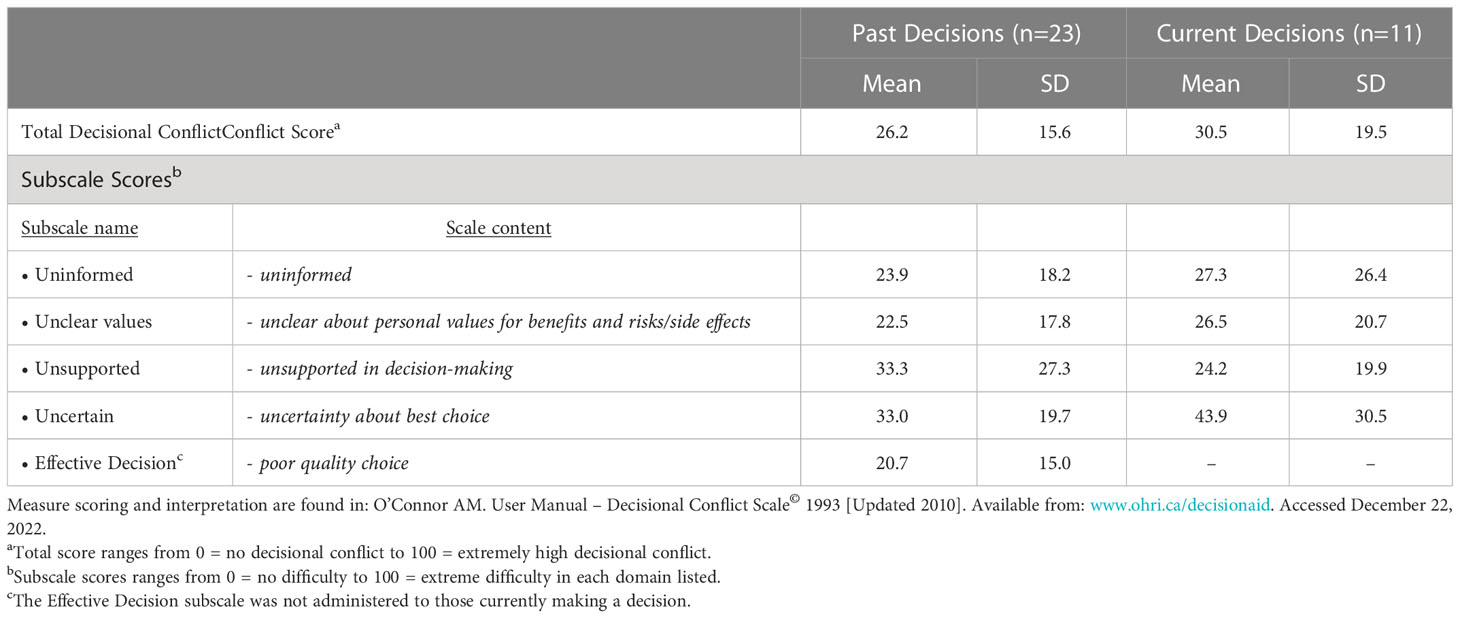
3.4 Decisional conflict and decision regret
Regarding self-identified tough decisions, mean parental total decisional conflict was 28 (± 17) out of 100 (range = 0 to 65; Table 4), with no statistically significant differences between those responding in reference to a past decision (mean = 26 ± 16) versus a current one (mean = 30 ± 19), t(16) = 0.7, p<0.53. Mean subscale scores ranged between 21 and 44. Individual scores varied and 12 (35%) participants had significant decisional conflict exceeding scores of 37.5 out of 100 that is associated with decision delay. Fourteen (41%) had low decisional conflict with scores <25 out of 100.
With regard to individual scale items, the majority of parents disagreed with the statement that the decision was easy to make (22, 65%). Of those whose decision occurred in the past, additional top concerns included not having enough advice to make a decision (9, 39%) and not being able to choose without pressure from others (9, 39%). Of those currently making a tough decision, the majority (7, 64%) reported a lack of feeling sure about what to choose, followed by neither having enough advice (5, 46%) nor being clear about the best choice (5, 46%).
The mean decisional regret score among those whose decision occurred in the past was 18.5 out of 100 ( ± 15.6, range = 0 to 50), with most experiencing either mild (n=10, 43.5%) or moderate to strong (7, 30.4%) regret. There were no discernable patterns between decisional regret scores and specific tough decisions named by participants.
3.5 Factors contributing to difficulty in decision-making
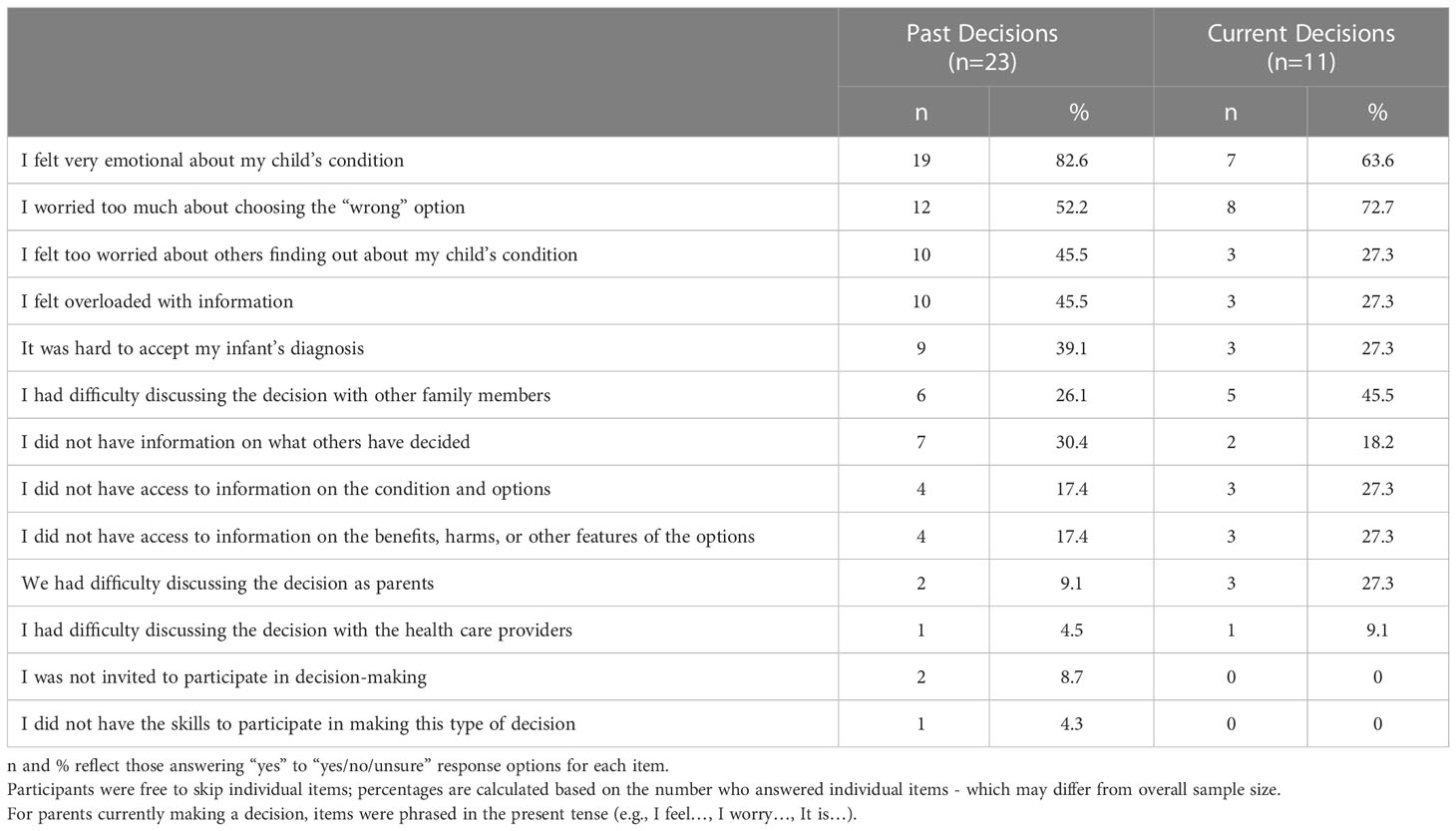
The majority of parents (n=32, 94%) reported at least one factor that they experienced as contributing to difficulty in decision-making – including feeling “very emotional about [their] child’s condition” (n=26, 76%) and “too much [worry] about choosing the ‘wrong’ option” (20, 59%) (Table 5).
These findings are also reflected in words parents used to describe the emotional strain associated with decisions (e.g., “inner turmoil” and “traumatic”), worries in the form of unanswered questions (e.g., “Who would understand? Would they reject her?” and “Do we express to him that he is perfectly made? That he is unable to bear his own children?”), and concerns over not having enough information (e.g., “I am wondering if genetic testing is necessary … or what information these tests will give” and “Not having access to current information … there weren’t many others in the US to consult with”) (Table 3).
Approximately half (46%) of past decision makers reported worrying about others learning about their child’s condition and feeling overloaded with information, compared with 27% of current decision makers. Conversely, approximately half (46%) of current decision makers reported difficulties discussing the decision with other family members, compared with 26% of past decision makers.
3.6 Peer support and resources involved in decision-making
With the exception of one parent, participants reported other people than themselves have been, or currently are, involved in making the tough decision. Most (n=30, 88%) involved their partner/spouse, followed by other family members (7, 30%), and friends (1, 3%). Seven (21%) parents also reported including their child (the patient). Aside from one parent who reported not accessing information and support resources when making decisions, citing “none really available to help make our decision,” most parents (n=28, 82%) reported using information provided by their healthcare provider during consultations to inform decisions, followed by contact with patient or family support groups (10, 29%), written resources (e.g., “materials provided to us by our clinic”; 6, 18%), and websites (5, 15%). Additional resources included self-directed web-based searches and information provided by friends, family, and older patients encountered at clinic visits or accessed through support groups.
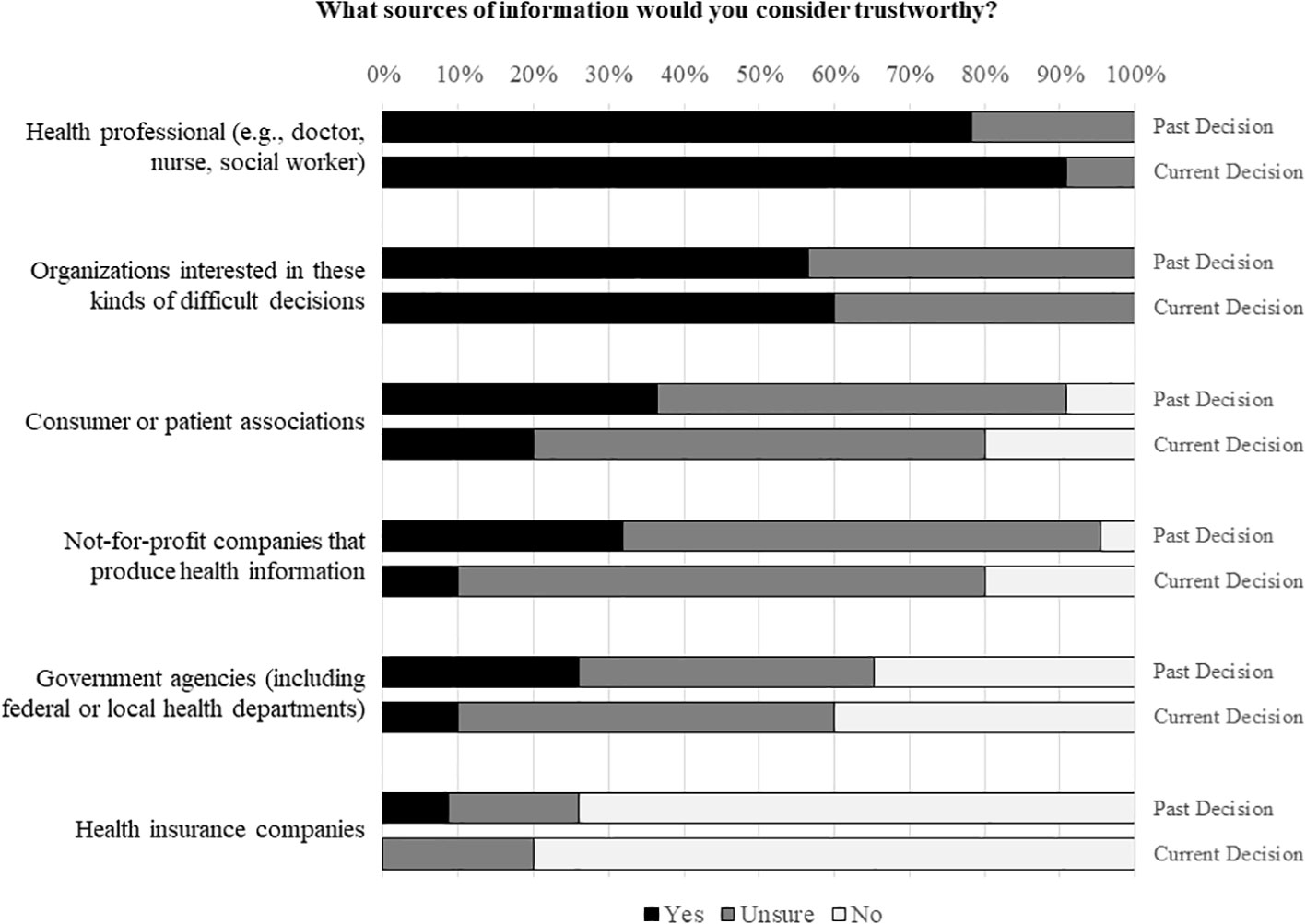
Parents reported varying degrees of doubt and uncertainty about the trustworthiness of some resources, including healthcare providers (n=6, 18% “unsure”; Figure 1). The majority of parents (25, 76%) did not consider health insurance companies as a trustworthy source; an additional six (18%) were unsure. Healthcare providers and organizations interested in these kinds of difficult decisions were rated as trustworthy by most parents (28, 82%; 19, 58%, respectively).
3.7 Decision-making preferences
Apart from one parent (5%) who reported that the tough decision was made entirely by the healthcare provider, most parents reported that either the final decision was one made mostly by themselves while strongly considering the provider’s opinion (n=12, 52%), entirely by themselves (6, 26%), or shared between themselves and the provider (4, 17%). A similar distribution of preferences was seen for those currently making a decision, with most (7, 64%) planning on making the decision themselves while strongly considering the provider’s opinion, (2, 18%) planning on making a shared decision, or (2, 18%) entirely by themselves.
For those who had already made their decisions, when asked how they would have preferred the decision be made if they had to do it all over again, parents reported preferences for arriving at the decision entirely by themselves (n=10, 45%), mostly by themselves with strong consideration of the healthcare provider’s perspectives (7, 32%), or together with the provider (5, 23%). No parents reported a preference for the provider to make the decision either entirely by themselves or mostly by themselves while considering parental perspectives.
In describing tough decisions they had made, four (12%) parents expressed a desire to include the child in decisions about surgery (n=3; e.g., “wait until our child is ready to be part of the decision”) and gender of rearing (n=1; e.g., “I ultimately didn’t believe the decision was mine to make”).
4 Discussion
4.1 Main findings
Our study identified several unmet decisional needs of parents with a child with DSD. Parents encountered several clinical management decisions on behalf of their children with DSD, with those concerning genital or gonadal surgery and discussions about the child’s condition and its management with others (including the child him/herself) most frequently mentioned. Decisions including those about genital or gonadal surgery, disclosure of the child’s condition to extended family and close friends, and gender of rearing were identified as particularly “tough” by parents. The majority of parents reported some level of decisional conflict and decision regret and almost all reported experiencing at least one factor as interfering with decision-making – most often emotions surrounding their child’s condition and worry about choosing the “wrong” option.
Compared with a recent report on healthcare providers’ perceptions (25), parents endorsed encountering these difficulties at rates lower than perceived by providers. Healthcare providers identified several common decisions encountered by parents, the first two described as particularly challenging: whether or not to choose genital or gonadal surgery, pursuing genetic testing beyond karyotype, accessing mental health services, and sharing details of the child’s DSD with relatives or close friends. While overlap between healthcare provider-report and our parent-report findings is apparent (e.g., genital or gonadal surgery; sharing details of the child’s condition), one-to-one correspondence was not observed, with only one (3%) parent reporting on genetic testing and none reporting on seeking mental health services as tough decisions. Our findings were consistent with a systematic review of decisional needs of parents making a wide range of healthcare decisions on behalf of their children that identified three key issues: need for information; talking to others (including concerns about pressure from others); and feeling a sense of control over the process that could be influenced by emotionally charged decisions, the consultation process, and structural or service (27).
A key feature of patient-centered care is meaningful patient and family participation in decisions about care (21, 41). Parents reported experiences of decision-making with healthcare providers that spanned the full range between exclusively parent-driven and exclusively provider-driven decisions. They universally reported a desire to be involved in decision-making – preferably making the final decision primarily on their own or, to a lesser extent, shared with their child’s healthcare providers. To be informed and effective participants in decision-making, parents require trustworthy resources of support and information – most often receiving information from providers and involving their partners in decision-making.
4.2 Strengths and limitations
Survey items primarily focused on the most difficult (“tough”) decisions identified as such by parents to concentrate our efforts at characterizing the features of these decisions, points at which parents experience the greatest decisional needs, and areas where clinicians and potentially others can intervene. Interpreting scale scores of measures indexing the decision-making process (e.g., levels of decisional conflict or regret) must be performed cautiously; such scores do not necessarily equally reflect the experience of the decision-maker across all clinical and psychosocial management issues. Approximately one third of parents reported currently making a “tough” decision; of those whose decision occurred in the past, over half reported decisions occurring five or more years ago, giving rise to the possibility of recall bias affecting scales requiring recollection of events (e.g., decisional conflict), but not those associated with current status (e.g., decisional regret).
DSD are individually rare conditions and our sample is relatively small. These limitations are balanced by the strength of a multisite recruitment strategy in which all eligible parents were invited to participate. Approximately half of those targeted participated: our sample was disproportionately women, White/Caucasian race, and non-Hispanic ethnicity. Notwithstanding the relative demographic homogeneity of our sample, the decision-making concerns and needs of our participants exhibited considerable variability. Indeed, such variability was seen between two parents of a single index case who identified different “tough” decisions experienced at different times. This speaks to a need for parents to be supported both individually and together in clinical practice.
4.3 Implications for care
Parents consistently voice a desire to take an active role in decision-making when decision points and treatment options are identified. Given variability in presenting features of the DSD requiring different decisions, parental decisional needs, and available social and information supports, clinicians are obliged to assess these for each patient (and family) in relation to each decision. High quality decision-making is often predicated on caregivers first resolving the tension experienced between the competing interests of promoting privacy versus establishing secrecy (42) regarding the child’s diagnosis and its implications which may bias decision-making in a manner that does not adequately take into account benefits and harms of all options. Healthcare providers can help identify family-specific needs through observation and inquiry in the clinical context
Some parents expressed a desire to include their child in decisions, but that their children were too young to be meaningfully involved. Healthcare providers can help parents by acknowledging the complexity of the situation and potential for challenges. Providers can help parents identify their own values and preferences and point our areas where differences between their own and those of their child may emerge over time.
4.4 Conclusions
Parents of children with DSD encounter medical, surgical, and psychosocial management decisions. Despite difficulties including emotional distress, worry, and informational concerns (including gaps and overload), parents express strong desires to play key roles in decision-making on behalf of their children. Healthcare providers should screen for and intervene on factors contributing to difficulty in the decision-making process. Educated and informed decision-making, supported by decision aids, can provide a robust mechanism for parent-provider collaboration within a patient- and family-centered care framework.
Data availability statement
The datasets presented in this article are not readily available because the raw qualitative data cannot be sufficiently redacted to protect participant privacy and confidentiality. A dataset including the raw quantitative data supporting conclusions of this article will be made available. Requests to access the datasets should be directed to DES, dsandber@med.umich.edu.
Ethics statement
The studies involving human participants were reviewed and approved by the University of Michigan Medical School - IRBMED. The participants provided their written informed consent to participate in this study.
Author contributions
MG, WB, MC, NL, SL, KP, PS, KS-J, BV, JW, DS, and DES contributed to the conception or design of this work. MG, MC, SL, TS-K, KS-J, EW, DS, and DES contributed to the acquisition, analysis, or interpretation of data. MG and DES completed the original draft of this manuscript. All authors contributed to the critical revision of this manuscript, approved the version to be published, and agreed to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by an award from the Eunice Kennedy Shriver National Institute of Child Health & Human Development R01HD086583.
Conflict of interest
EW is the paid Executive Director of Accord Alliance. WB has common stock holdings in the following publicly traded companies: Pfizer, Merck, Abbott Laboratories, Viatris, and Johnson & Johnson.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer DLJ declared a shared affiliation with the author KS-J, with no collaboration, to the handling editor at the time of review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fruro.2023.1089077/full#supplementary-material
Footnotes
- ^ The umbrella term “disorders of sex development” has been rejected by some patient advocates with concerns that the word “disorder” fosters stigma (1). For this reason, and following the practice of many others in this field, we have substituted “differences for “disorders” which preserves the acronym DSD.
References
1. Davis G. The power in a name: Diagnostic terminology and diverse experiences. Psychol Sexuality. (2013) 5(1):15–27. doi: 10.1080/19419899.2013.831212
2. Lee PA, Houk CP, Ahmed SF, Hughes IA. International consensus conference on intersex organized by the Lawson Wilkins Pediatric Endocrine Society & the European Society for Paediatric Endocrinology. Consensus statement on management of intersex disorders. International consensus conference on intersex. Pediatrics (2006) 118(2):e488–500. doi: 10.1542/peds.2006-0738
3. Lee PA, Nordenstrom A, Houk CP, Ahmed SF, Auchus R, Baratz A, et al. Global disorders of sex development update since 2006: Perceptions, approach and care. Horm Res Paediatr (2016) 85(3):158–80. doi: 10.1159/000442975
4. Crissman HP, Warner L, Gardner M, Carr M, Schast A, Quittner AL, et al. Children with disorders of sex development: A qualitative study of early parental experience. Int J Pediatr Endocrinol (2011) 1:10. doi: 10.1186/1687-9856-2011-10
5. Chase C. What is the agenda of the intersex patient advocacy movement? Endocrinologist (2003) 13(3):240–2. doi: 10.1097/01.ten.0000081687.21823.d4
6. Traino KA, Roberts CM, Fisher RS, Delozier AM, Austin PF, Baskin LS, et al. Stigma, intrusiveness, and distress in parents of children with a disorder/difference of sex development. J Dev Behav Pediatr (2022) 43(7):e473–e482. doi: 10.1097/DBP.0000000000001077
7. Perez MN, Clawson AH, Baudino MN, Austin PF, Baskin LS, Chan YM, et al. Distress trajectories for parents of children with DSD: A growth mixture model. J Pediatr Psychol (2021) 46(5):588–98. doi: 10.1093/jpepsy/jsab004
8. Sanders C, Carter B, Goodacre L. Parents' narratives about their experiences of their child's reconstructive genital surgeries for ambiguous genitalia. J Clin Nurs (2008) 17(23):3187–95. doi: 10.1111/j.1365-2702.2007.02006.x
9. Boyse KL, Gardner M, Marvicsin DJ, Sandberg DE. "It was an overwhelming thing": Parents' needs after infant diagnosis with congenital adrenal hyperplasia. J Pediatr Nurs (2014) 29(5):436–41. doi: 10.1016/j.pedn.2014.01.007
10. Pasterski V, Mastroyannopoulou K, Wright D, Zucker KJ, Hughes IA. Predictors of posttraumatic stress in parents of children diagnosed with a disorder of sex development. Arch Sex Behav (2014) 43(2):369–75. doi: 10.1007/s10508-013-0196-8
11. Duguid A, Morrison S, Robertson A, Chalmers J, Youngson G, Ahmed SF, et al. The psychological impact of genital anomalies on the parents of affected children. Acta Paediatr (2007) 96(3):348–52. doi: 10.1111/j.1651-2227.2006.00112.x
12. Wisniewski AB. Psychosocial implications of disorders of sex development treatment for parents. Curr Opin Urol (2017) 27(1):11–3. doi: 10.1097/MOU.0000000000000344
13. Rolston AM, Gardner M, Vilain E, Sandberg DE. Parental reports of stigma associated with child's disorder of sex development. Int J Endocrinol (2015). doi: 10.1155/2015/980121
14. Traino KA, Baudino MN, Kraft JD, Basile NL, Dattilo TM, Davis MP, et al. Factor analysis of the stigma scale - parent version in pediatric disorders/differences of sex development. Stigma Health (2021) 6(4):390–6. doi: 10.1037/sah0000346
15. Duggan K, McNamara D. The blurred distinction between therapeutic and non-therapeutic medical interventions for intersex children in Australia. Aust J Hum Rights. (2022) 27(2):272–92. doi: 10.1080/1323238x.2021.1996202
16. Ernst MM, Liao LM, Baratz AB, Sandberg DE. Disorders of sex development/intersex: Gaps in psychosocial care for children. Pediatrics (2018) 142(2):e20174045. doi: 10.1542/peds.2017-4045
17. Karkazis K, Tamar-Mattis A, Kon AA. Genital surgery for disorders of sex development: Implementing a shared decision-making approach. J Pediatr Endocrinol Metab (2010) 23(8):789–805. doi: 10.1515/jpem.2010.129
18. Magritte E. Working together in placing the long-term interests of the child at the heart of the DSD evaluation. J Pediatr Urol (2012) 8(6):571–5. doi: 10.1016/j.jpurol.2012.07.011
19. Sandberg DE, Mazur T. A noncategorical approach to the psychosocial care of persons with DSD and their families. In: Kreukels B, Steensma T, de Vries A, editors. Gender dysphoria and disorders of sex development. Focus on sexuality research. Boston: MA: Springer (2014). p. 93–114. doi: 10.1007/978-1-4614-7441-8_5
20. Lorenzo AJ, Pippi Salle JL, Zlateska B, Koyle MA, Bagli DJ, Braga LH. Decisional regret after distal hypospadias repair: Single institution prospective analysis of factors associated with subsequent parental remorse or distress. J Urol (2014) 191(5 Suppl):1558–63. doi: 10.1016/j.juro.2013.10.036
21. American Academy of Pediatrics, Committee on Hospital Care, Institute for Patient-Family-Centered Care. Patient- and family-centered care and the pediatrician's role. Pediatrics (2012) 129(2):394–404. doi: 10.1542/peds.2011-3084
22. Siminoff LA, Sandberg DE. Promoting shared decision-making in disorders of sex development (DSD): Decision aids and support tools. Horm Metab Res (2015) 47(5):335–9. doi: 10.1055/s-0035-1545302
23. Légaré F, Witteman HO. Shared decision-making: Examining key elements and barriers to adoption into routine clinical practice. Health Aff (Millwood) (2013) 32(2):276–84. doi: 10.1377/hlthaff.2012.1078
24. Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev (2017) 4:CD001431. doi: 10.1002/14651858.CD001431.pub5
25. Suorsa-Johnson KI, Gardner MD, Brinkman W, Carley M, Gruppen L, Liang N, et al. A survey of healthcare professionals' perceptions of the decisional needs of parents with an infant born with a disorder/difference of sex development. J Pediatr Urol (2022). doi: 10.1016/j.jpurol.2022.09.015
26. Hoefel L, O'Connor AM, Lewis KB, Boland L, Sikora L, Hu J, et al. 20th anniversary update of the Ottawa decision support framework part 1: A systematic review of the decisional needs of people making health or social decisions. Med Decis Making (2020) 40:555–81. doi: 10.1177/0272989X20936209
27. Jackson C, Cheater FM, Reid I. A systematic review of decision support needs of parents making child health decisions. Health Expectations (2008) 11:232–51. doi: 10.1111/j.1369-7625.2008.00496.x
28. Shippee ND, Domecq Garces JP, Prutsky Lopez GJ, Wang Z, Elraiyah TA, Nabhan M, et al. Patient and service user engagement in research: A systematic review and synthesized framework. Health Expect (2015) 18:1151–66. doi: 10.1111/hex.12090
29. Stacey D, Legare F, Boland L, Lewis KB, Loiselle MC, Hoefel L, et al. 20th anniversary Ottawa decision support framework: Part 3 overview of systematic reviews and updated framework. Med Decis Making (2020) 40(3):379–98. doi: 10.1177/0272989X20911870
30. Hanauer DA, Gardner M, Sandberg DE. Unbiased identification of patients with disorders of sex development. PloS One (2014) 9(9):e108702. doi: 10.1371/journal.pone.0108702
31. Sandberg DE, Gardner M, Callens N, Mazur T, DSD-TRN psychosocial workgroup, the DSD-TRN advocacy advisory network, et al. Interdisciplinary care in disorders/differences of sex development (DSD): The psychosocial component of the DSD-translational research network. Am J Med Genet C Semin Med Genet (2017) 175(2):279–92. doi: 10.1002/ajmg.c.31561
32. Délot EC, Papp JC, DSD-TRN Genetics WorkgroupSandberg DE, Vilain E. Genetics of disorders of sex development: The DSD-TRN experience. Endocrinol Metab Clin North Am (2017) 46(2):519–37. doi: 10.1016/j.ecl.2017.01.015
33. O'Connor AM. User manual - decisional conflict scale. (Ottawa, Canada: Ottawa Hospital Research Institute) (1993). Available at: http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Decisional_Conflict.pdf.
34. Degner LF, Sloan JA. Decision-making during serious illness: What role do patients really want to play? J Clin Epidemiol (1992) 45(9):941–50. doi: 10.1016/0895-4356(92)90110-9
35. O'Connor AM. User manual - decision regret scale. (Ottawa, Canada: Ottawa Hospital Research Institute) (1996). Available at: https://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Regret_Scale.pdf.
36. Becerra Pérez MM, Menear M, Brehaut JC, Légaré F. Extent and predictors of decision regret about health care decisions: A systematic review. Med Decis Making (2016) 36:777–90. doi: 10.1177/0272989x16636113
37. Lognon T, Gogovor A, Plourde KV, Hoyoke P, Lai C, Aubin E, et al. Predictors of decision regret among caregivers of older canadians receiving home care: A cross-sectional online survey. MDM Policy Pract (2022) 7(2):1–17. doi: 10.1177/23814683221116304
38. Creswell JW. Qualitative inquiry & research design: Choosing among five approaches. 2nd ed. Thousand Oaks, CA: Sage Publications, Inc (2007). p. 395.
39. Barrera M, Atenafu E, Doyle J, Berlin-Romalis D, Hancock K. Differences in mothers’ and fathers’ psychological distress after pediatric SCT: A longitudinal study. Bone Marrow Transplant (2012) 47:934–9. doi: 10.1038/bmt.2011.206
40. Sood E, Karpyn A, Demianczyk AC, Ryan J, Delaplane EA, Neely T, et al. Mothers and fathers experience stress of congenital heart disease differently: Recommendations for pediatric critical care. Pediatr Crit Care Med (2018) 19(7):626–34. doi: 10.1097/PCC.0000000000001528
41. Institute of Medicine, Committee on Quality of Health Care in America. Crossing the quality chasm: A new health system for the 21st century. (Washington, DC: The National Academies Press) (2001). doi: 10.17226/10027
Keywords: differences of sex development, disorders of sex development, intersex, decisional needs assessment, shared decision-making, decision-making preferences, decisional conflict
Citation: Gardner M, Brinkman WB, Carley M, Liang N, Lightfoot S, Pinkelman K, Speiser PW, Schafer-Kalkhoff T, Suorsa-Johnson KI, VanderBrink B, Weidler EM, Wisniewski J, Stacey D and Sandberg DE (2023) Decisional support needed when facing tough decisions: Survey of parents with children having differences of sex development. Front. Urol. 3:1089077. doi: 10.3389/fruro.2023.1089077
Received: 03 November 2022; Accepted: 12 January 2023;
Published: 09 February 2023.
Edited by:
Heidi Stephany, University of California, Irvine, United StatesReviewed by:
Deborah Lynn Jacobson, The University of Utah, United StatesKelly Swords, University of California, San Diego, United States
Copyright © 2023 Gardner, Brinkman, Carley, Liang, Lightfoot, Pinkelman, Speiser, Schafer-Kalkhoff, Suorsa-Johnson, VanderBrink, Weidler, Wisniewski, Stacey and Sandberg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: David E. Sandberg, dsandber@med.umich.edu
†These authors share senior authorship
 Melissa Gardner
Melissa Gardner William B. Brinkman2,3
William B. Brinkman2,3 Sophie Lightfoot
Sophie Lightfoot Phyllis W. Speiser
Phyllis W. Speiser Tara Schafer-Kalkhoff
Tara Schafer-Kalkhoff Kristina I. Suorsa-Johnson
Kristina I. Suorsa-Johnson Erica M. Weidler
Erica M. Weidler David E. Sandberg
David E. Sandberg