- Jiangsu Provincial Key Laboratory of Critical Care Medicine, Department of Critical Care Medicine, School of Medicine, Zhongda Hospital, Southeast University, Nanjing, China
Methods of liberation from mechanical ventilation: Which one is best?
As an essential life-saving intervention, mechanical ventilation is also associated with complications which result to higher medical costs and mortality (1, 2). Therefore, it was essential to liberate patients from mechanical ventilation efficacy and safety for the shortest possible duration. Despite many studies comparing the safety and effectiveness of different methods for weaning have been published, many controversial questions remain concerning the best method for this process. Given that studies to date have not investigated the comparative of all available modes of weaning simultaneously, a network meta-analysis may help evaluate the relative effectiveness between all modes from both direct and mixed-treatment comparisons (3).
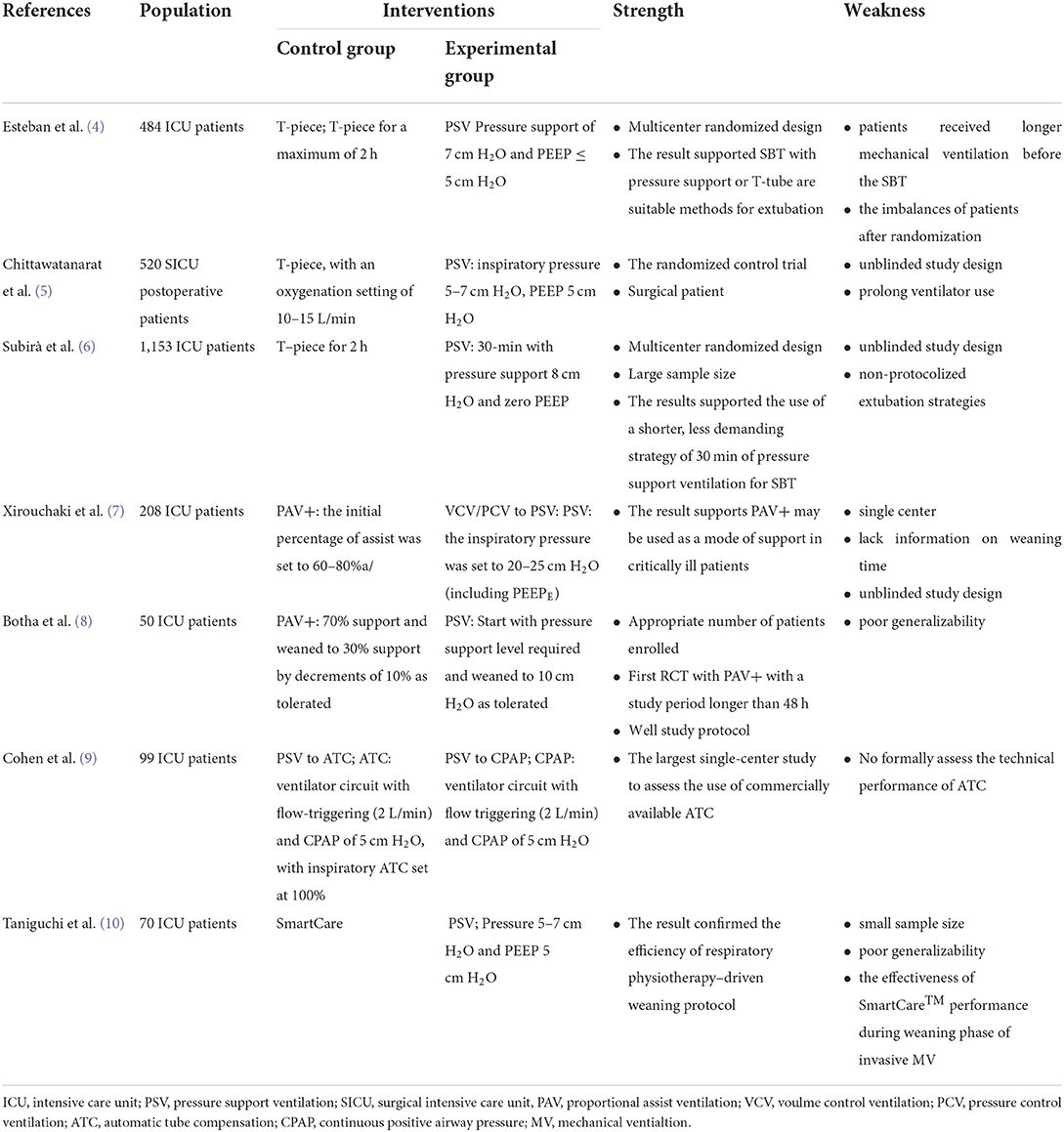
There were two network meta-analysis focuses on the best weaning methods published in this research topic of acute respiratory distress syndrome and mechanical ventilation. Although the study selection criteria were not identical, 12 randomized controlled trials (RCTs) were overlapped in the two studies. The study by Yi et al. including 24 RCTs showed that automatic tube compensation (ATC) obtained superior weaning success compared to T-piece and pressure support ventilation (PSV). Another study by Jhou et al. including 39 RCTs compared the efficacy among 7 modes of weaning and provided evidence that proportional assist ventilation (PAV) has a high probability of being the most effective ventilation mode regarding a higher rate of weaning success, a lower reintubation, and mortality rate. The features of pivotal clinical trials included in the meta-analysis are presented in the Table 1 (4–10). The reliability of these findings should be interpreted cautiously for several reasons. First, these findings were generated from single-center trials with limited sample size. Second, the difficulty of weaning (simple weaning, difficult weaning, and prolonged weaning) and duration of mechanical ventilation vary across studies, which has potential influence on the results of weaning outcome and may introduce a potential bias. Third, the variety of sedation and ventilation setting prior to or during liberation process also impact the clinical efficacy and introduce a potential bias. Further multicenter studies considering different clinical vignettes and respiratory physiology patterns are warranted to gain full insight into the real role of various weaning methods.
Nonetheless, these findings promote pondering deeply over the criteria for the ideal method of ventilator liberation. PSV is the most commonly used mode of weaning in recent decades. In PSV mode, the PS can decrease the work of breathing imposed by the endotracheal tube (11). Short duration of PSV with a low level of assistance was also recommended by the most recent guidelines performed as initial spontaneous breathing trial rather than T-piece or CPAP (12). The network meta-analysis also showed that PSV increased the rate of weaning success when compared with T-piece. However, PSV can only provide a constant positive pressure which may not match the patient's respiratory demand. Of note, Yi et al. found that PAV was superior to PSV regarding weaning success, and Jhou et al. found that ATC was also superior to PSV. A sizeable effect with patient-ventilator asynchrony and over-assistance during PSV weaning might be a possible explanation (13). PAV, which delivered positive pressure ventilation in proportion to instantaneous inspiratory effort, was associated with less patient ventilator asynchrony and lower risk of over-assistance (14). Nevertheless, PAV is relatively complex; indeed, the settings need knowing or estimating the patient's compliance and resistance (15). ATC, which delivered dynamic positive pressure automatically to compensate for the resistance of artificial airway, can improve synchronization between patient and ventilator, and avoided over-assistance (16, 17). However, ATC cannot increase lung ventilation heterogeneity as compared to low PS and PEEP (18). Nonetheless, unloading the respiratory muscle without over-assistance and better patient-ventilator interaction might be essential to the ideal method of weaning.
Neurally adjusted ventilatory assist (NAVA) mode uses the electrical activity of the diaphragm to control the ventilator and delivers pressure support in proportion to patients' neural effort. It has been demonstrated that NAVA improved patient-ventilator interaction and reduced inappropriate ventilator assist when compared with PSV (19, 20). Despite limited real-world experience, NAVA might be ideally suitable for the weaning process. Several studies have shown that NAVA improves the weaning outcome when compared with PSV, especially for patients difficult to wean (13, 21, 22). However, RCTs, comparing the safety and effectiveness between NAVA and other weaning modes, such as PAV and ATC, are absent.
Although, there is still controversy about the best method of liberation from mechanical ventilation, new mode in line with respiratory physiology might be a light at the end of the tunnel.
Author contributions
LL wrote the original version and revised the Editorial.
Funding
This study was supported by Key Research and Development Plan of Jiangsu Province (BE2020786) and 333 High Level Talents Training Project in the sixth phase in Jiangsu.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Esteban A, Anzueto A, Frutos F, Alia I, Brochard L, Stewart TE, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. (2002) 287:345–55. doi: 10.1001/jama.287.3.345
2. Cooper LM, Linde-Zwirble WT. Medicare intensive care unit use: analysis of incidence, cost, and payment. Crit Care Med. (2004) 32:2247–53. doi: 10.1097/01.CCM.0000146301.47334.BD
3. Rouse B, Chaimani A, Li T. Network meta-analysis: an introduction for clinicians. Intern Emerg Med. (2017) 12:103–11. doi: 10.1007/s11739-016-1583-7
4. Esteban A, Alía I, Gordo F, Fernández R, Solsona JF, Vallverdú I, et al. Extubation outcome after spontaneous breathing trials with T-tube or pressure support ventilation. The Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med. (1997) 156:459–65. doi: 10.1164/ajrccm.156.2.9610109
5. Chittawatanarat K, Orrapin S, Jitkaroon K, Mueakwan S, Sroison U. An open label randomized controlled trial to compare low level pressure support and T-piece as strategies for discontinuation of mechanical ventilation in a general surgical intensive care unit. Med Arch. (2018) 72:51–7. doi: 10.5455/medarh.2018.72.51-57
6. Subirà C, Hernández G, Vázquez A, Rodríguez-García R, González-Castro A, García C, et al. Effect of pressure support vs T-Piece ventilation strategies during spontaneous breathing trials on successful extubation among patients receiving mechanical ventilation: a randomized clinical trial. JAMA. (2019) 321:2175–82. doi: 10.1001/jama.2019.7234
7. Xirouchaki N, Kondili E, Vaporidi K, Xirouchakis G, Klimathianaki M, Gavriilidis G, et al. Proportional assist ventilation with load-adjustable gain factors in critically ill patients: comparison with pressure support. Intensive Care Med. (2008) 34:2026–34. doi: 10.1007/s00134-008-1209-2
8. Botha J, Green C, Carney I, Haji K, Gupta S, Tiruvoipati R. Proportional assist ventilation vs. pressure support ventilation in weaning ventilation: a pilot randomized controlled trial. Crit Care Resusc. (2018) 20:33–40. doi: 10.1164/RCCM.2107138
9. Cohen JD, Shapiro M, Grozovski E, Lev S, Fisher H, Singer P. Extubation outcome following a spontaneous breathing trial with automatic tube compensation vs. continuous positive airway pressure. Crit Care Med. (2006) 34: 682-6. doi: 10.1097/01.CCM.0000201888.32663.6A
10. Taniguchi C, Victor ES, Pieri T, Henn R, Santana C, Giovanetti E, et al. Smart Care vs. respiratory physiotherapy-driven manual weaning for critically ill adult patients: a randomized controlled trial. Crit Care. (2015) 19:246. doi: 10.1186/s13054-015-0978-6
11. Nathan SD, Ishaaya AM, Koerner SK, Belman MJ. Prediction of minimal pressure support during weaning from mechanical ventilation. Chest. (1993) 103:1215–9. doi: 10.1378/chest.103.4.1215
12. Ouellette DR, Patel S, Girard TD, Morris PE, Schmidt GA, Truwit JD, et al. Liberation from mechanical ventilation in critically ill adults: an official American college of Chest Physicians/American Thoracic Society clinical practice guideline: inspiratory pressure augmentation during spontaneous breathing trials, protocols minimizing sedation, and noninvasive ventilation immediately after extubation. Ches.t. (2017) 151:166–80. doi: 10.1016/j.chest.2016.10.036
13. Liu L, Xu X, Sun Q, Yu Y, Xia F, Xie J, et al. Neurally adjusted ventilatory assist versus pressure support ventilation in difficult weaning. Anesthesiology. (2020) 132:1482–93. doi: 10.1097/ALN.0000000000003207
14. Alexopoulou C, Kondili E, Plataki M, Georgopoulos D. Patientventilator synchrony and sleep quality with proportional assist and pressure support ventilation. Intensive Care Med. (2013) 39:1040–7. doi: 10.1007/s00134-013-2850-y
15. Lellouche F, Brochard L. Advanced closed loops during mechanical ventilation (PAV, NAVA, ASV, SmartCare). Best Pract Res Clin Anaesthesiol. (2009) 23:81–93. doi: 10.1016/j.bpa.2008.08.001
16. Guttmann J, Bernhard H, Mols G, Benzing A, Hofmann P, Haberthür C, et al. Respiratory comfort of automatic tube compensation and inspiratory pressure support in conscious humans. Intensive Care Med. (1997) 23:1119–24. doi: 10.1007/s001340050467
17. Mols G, Rohr E, Benzing A, Haberthür C, Geiger K, Guttmann J. Breathing pattern associated with respiratory comfort during automatic tube compensation and pressure support ventilation in normal subjects. Acta Anaesthesiol Scand. (2000) 44:223–30. doi: 10.1034/j.1399-6576.2000.440302.x
18. Guérin C, Terzi N, Mezidi M, Baboi L, Chebib N, Yonis H, et al. Low-pressure support vs. automatic tube compensation during spontaneous breathing trial for weaning. Ann Intensive Care. (2019) 9:137. doi: 10.1186/s13613-019-0611-y
19. Pettenuzzo T, Aoyama H, Englesakis M, Tomlinson G, Fan E. Effect of neurally adjusted ventilatory assist on patient-ventilator interaction in mechanically ventilated adults: a systematic review and meta-analysis. Crit Care Med. (2019) 47:e602–9. doi: 10.1097/CCM.0000000000003719
20. Patroniti N, Bellani G, Saccavino E, Zanella A, Grasselli G, Isgrò S, et al. Respiratory pattern during neurally adjusted ventilatory assist in acute respiratory failure patients. Intensive Care Med. (2012) 38:230–9. doi: 10.1007/s00134-011-2433-8
21. Kacmarek RM, Villar J, Parrilla D, Alba F, Solano R, Liu S, et al. Neurally adjusted ventilatory assist in acute respiratory failure: a randomized controlled trial. Intensive Care Med. (2020) 46:2327–37. doi: 10.1007/s00134-020-06181-5
22. Hadfield DJ, Rose L, Reid F, Cornelius V, Hart N, Finney C, et al. Neurally adjusted ventilatory assist vs. pressure support ventilation: a randomized controlled feasibility trial performed in patients at risk of prolonged mechanical ventilation. Crit Care. (2020) 24:220. doi: 10.1186/s13054-020-02923-5
Keywords: weaning from mechanical ventilation, automatic tube compensation, pressure support ventilation, proportional assist ventilation, neurally adjusted ventilatory assist
Citation: Liu L (2022) Methods of liberation from mechanical ventilation: Which one is best? Front. Med. 9:917369. doi: 10.3389/fmed.2022.917369
Received: 27 April 2022; Accepted: 05 July 2022;
Published: 16 August 2022.
Edited by:
Carlos Augusto Camillo, State University of Londrina, BrazilReviewed by:
Paulo André Freire Magalhães, Universidade de Pernambuco, BrazilCopyright © 2022 Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ling Liu, Liulingdoctor@126.com
 Ling Liu
Ling Liu