- 1Department of Gastroenterology, Centro Hospitalar Universitário de São João, Porto, Portugal
- 2World Gastroenterology Organisation (WGO) Gastroenterology and Hepatology Training Center, Porto, Portugal
- 3Faculty of Medicine of the University of Porto, Porto, Portugal
Climate change poses a growing threat to human health and well-being, with emerging evidence pointing to its intricate relationship with liver diseases. Indeed, climate change influences liver diseases through various direct and indirect mechanisms. Alcohol-related liver disease, Metabolic dysfunction-associated liver disease (MASLD), and viral hepatitis are the three most common causes of liver disease, and all are susceptible to the effects of climate change. Shifts in dietary habits driven by altered food availability, substance abuse exacerbated by social instability, extreme weather events affecting healthcare access, and the emergence of waterborne infections are among the factors exacerbating liver disease incidence and severity. On the flip side, healthcare systems, including liver units, significantly contribute to climate change through energy consumption, medical waste, and transportation emissions. The need for sustainable healthcare practices, telemedicine, and waste reduction strategies is becoming increasingly evident. Recognizing this intricate interplay and addressing the dual interaction between climate change and liver disease is imperative for safeguarding human health and reducing the environmental footprint of healthcare facilities. As climate change continues to unfold, understanding its implications for liver disease is critical for public health and environmental sustainability.
1 Introduction
The climate crisis resulting from human activity is one of the main challenges of our time. Indeed, rising temperatures have a significant impact on several sectors of society, and the potential effects on the health of populations are, conceivably, one of the main concerns. In fact, climate change has been identified as the biggest threat to global health in the 21st century. Besides directly affecting the health condition of each individual, climate change impacts the social and environmental determinants of health (1–3).
The healthcare sector is a key player for fostering good health outcomes for the populations. Nevertheless, when considering its environmental impact, we are faced with the paradox regarding the fact the healthcare sector constitutes one of the largest greenhouse gases (GHG) emitters. This reality is easily understandable when we consider that western healthcare systems are large employers and may account for almost 10% of national emissions (4, 5).
Liver disease accounts for 4% of all annual deaths worldwide (6). The incidence of liver disease is intrinsically dependent on human behavior, social context as well as environmental exposures. While these well-defined risk factors open the door for the institution of preventive measures, climate change has the potential to influence all determinants of liver disease, thus contributing to the anticipated increase in the global burden of liver disease (6).
While the available evidence remains scarce and at the level of conjectures, the most relevant scientific societies are increasingly becoming aware of the importance of this situation (7). This short review aims to provide an outlook of the potential impact of climate change on liver disease, as well as on the care for the patient with liver disease and the organization of hepatology centers. Most importantly, this work aims to bring awareness of this increasingly relevant challenge to the medical community, and particularly for hepatologists.
2 Dual interaction between climate change and healthcare
The current climate crises impose an additional stress factor on already saturated healthcare care systems. Indeed, the increase in global temperature is expected to disrupt the normal functioning of healthcare delivery by increasing the burden of disease, disrupting healthcare facilities and supply chains, and increasing the susceptibility for more severe forms of disease (8). Nonetheless, the interaction between healthcare and climate change is bidirectional, with healthcare both contributing to and being impacted by climate change.
2.1 Healthcare contribution to climate change
2.1.1 Energy consumption
Modern healthcare facilities, including hospitals and clinics, are energy-intensive environments. In fact, large energy requirements are imposed by the need to ensure the functioning of medical equipment, as well as provide ventilation, heating and cooling of facilities. In developed countries, the amount of energy consumption has increased in parallel with an increase in healthcare budget in percentage of GDP (9). This energy consumption leads to greenhouse gas emissions, primarily carbon dioxide (CO2). The number of healthcare facilities has been increasing in number and size in the Western hemisphere, and the intensity of energy consumption is calculated to surpass that of commercial buildings three-fold (10). In the US, around 60% of all energy expenditure in healthcare facilities is related to heating and cooling and natural gas is the main source of energy for 90% of buildings (10). Moreover, despite a decrease in energy consumption over the last years for commercial buildings, this reduction was not observed in hospitals, thus underscoring the need for the development of more efficient energy expenditure.
Besides the environmental impact of energy expenditure of healthcare facilities, an increasing attention has been given to the full life cycle of activities related to healthcare delivery. Indeed, a recent study calculated that 45% of GHG emissions of an endoscopy center were related to patient and staff travels, followed by the production and disposal of medical equipment (32%) (11).
2.1.2 Pharmaceuticals and medical waste
The production, use, and disposal of pharmaceuticals contribute to environmental pollution. Additionally, medical waste generated by healthcare facilities, including hazardous materials, requires proper disposal to minimize environmental contamination. Developed countries show higher rates of waste generation, in relation with higher spends in terms of GDP in healthcare (9). Healthcare waste (HCW) accounts for 1-2% of total urban waste (12), and 15% of all HCW is considered hazardous. Practices regarding healthcare waste management are extremely heterogeneous over the globe. Inadequate human resource training raises a significant problem in the treatment of HCW, particularly in developing countries, which poses risks to public health (13).
2.2 Healthcare’s vulnerability to climate change
2.2.1 Disruption of healthcare structure
The increased frequency of extreme weather events can cause damage to healthcare facilities, thus limiting patients’ access and quality of care (8). Besides, these events may compromise communication routes, thus disrupting supply chains. Additionally, the impact of anthropogenic climate change is expected to generate economic struggling, thus limiting the investment in the healthcare system. Importantly, the increase in global temperatures and the rise of sea levels may lead to massive population migration movements, therefore increasing the burden on health systems. Moreover, social instability caused by resource scarcity may lead to conflict with risk of destruction healthcare facilities (14).
2.2.2 Vector-borne diseases
The change in climate patterns can modify the geographical distribution of disease vectors, thus bringing diseases from tropical areas to previously temperate climates (e.g. Dengue fever, Malaria). Moreover, economic and food insecurity, as well as mass migratory movements will lead to the establishment of new human settlements (e.g. refugee camps), potentially leading to overcrowding and increased exposure to contaminated water and disease-spreading vectors (14).
2.2.3 Heat-related illnesses
Rising temperatures can lead to more frequent and severe heatwaves, causing heat-related illnesses and, importantly, decompensating preexisting comorbid conditions, including respiratory, cardiovascular and hepatic disease (15–17). The expected increase in admissions due to heat-related illnesses will increase the burden on healthcare systems, which is particularly worrisome for hotter areas, frequently with low-resource healthcare systems.
2.3 The impact of climate change on liver disease
The interaction between the climate crisis and the care of patients with liver disease is complex, and potentially bidirectional. A direct impact of the climate in liver health has been shown as a component of heat-related illnesses. Indeed, heat stroke can result in hepatocellular injury due to liver hypoperfusion, leading to acute liver injury and acute liver failure (18). Nevertheless, the indirect effects of climate on liver disease, by inducing modifications on patients’ environments, thereby modifying risk factors and the natural evolution of common liver disease etiologies. On the other direction, patients with liver disease often requires multiple visits, follow-up tests, resource-consuming and chronic medication.
2.3.1 Alcohol-related liver disease
Alcohol use is the leading cause of liver disease in the world, and accounts for 60% all cases of cirrhosis in the western hemisphere (6). The prevalence of alcohol use disorder varies greatly between regions but appears higher in high-income countries (6). Several factors influence pathologic patterns of alcohol consumption. The relation between climate change and mental health has been previously acknowledged (19). Climate change generates several stressors, including depression from destruction resulting from extreme weather events, economic difficulties, food insecurity, and displacement. All these factors can contribute to impair the mental health of individuals. In reaction, people may turn to alcohol as a coping mechanism, increasing the risk of heavy drinking and the development of alcoholic liver disease. Furthermore, there is evidence correlating an increase in atmospheric temperature and more deleterious patterns of alcohol use. Indeed, increasing temperatures have been associated with an increase in overall alcohol use, as well as acute poisoning by alcohol and emergency department visits due to alcohol use disorder (20, 21). Inversely, alcohol consumption contributes with a large volume of GHG emissions, therefore contributing to the anthropogenic climate change. Indeed, a Swedish study estimated that the alcohol industry accounted for 3% of GHG emissions, producing an equivalent of 2.4 kg of CO2 per litter (22).
Finally, with increasing frequency of extreme weather events, such as heat waves, the incidence of heat-related illnesses is expected to increase (23). Alcohol may interfere with the perception of heat and regulatory thermoregulation mechanisms, thus increasing the propensity for dehydration, making individuals more susceptible to heat-related complications during extreme weather events, which may further exacerbate the negative effects of alcohol on the liver (24, 25).
2.3.2 Metabolic dysfunction-associated steatotic liver disease
The designation of Metabolic dysfunction-associated steatotic liver disease (MASLD) replaced the term “non-alcoholic fatty liver disease” (26). This etiology is associated with metabolic risk factors, namely the presence of central obesity and diabetes mellitus, affecting 32% of the of the world’s population, and corresponding to the second largest indication for liver transplantation (6).
The increase in the prevalence of MASLD parallels that of obesity and metabolic syndrome (27). The dietary patterns of population are expected to be severely impacted by the anthropogenic climate change (28). These modifications, simultaneously with current patterns of food production, will contribute to the destruction of habitats and loss of biodiversity, which will ultimately limit food availability (29). Food and economic insecurity promote the consumption of highly processed foodstuff, frequently inexpensive, and which contribute greatly to worse metabolic outcomes, exacerbating the obesity epidemics, a major risk factor for MASLD. Moreover, extreme weather events can disrupt food supply chains, leading to food shortages and further influencing dietary habits. Air pollution, particularly in highly populated areas with high concentrations of fine particulate matter may increase the risk of MASLD, as it promotes oxidative stress, systemic inflammation, insulin resistance and impair glucose and triglyceride metabolism (30, 31).
The increase in global temperature, as well as the increasingly prevalent heat waves, are likely to foment sedentarism, as outdoor physical activity becomes unpleasant or contraindicated. Moreover, this may further contribute to feed a vicious circle, whereby a lower predisposition for physical activity will probably contribute an increase in the use of motorized transportation, thus increasing GHG emissions.
2.3.3 Viral hepatitis
Global warming may contribute to increase the frequency of viral hepatitis, both those related to waterborne infections (hepatitis A and E) or those transmitted by parenteral or sexual contact (hepatitis B and C). Indeed, the increasing prevalence of extreme weather events, causing more frequent flooding events may exacerbate the spread of both hepatitis A and E. Moreover, mass population movements from people living in more endangered areas, generating large settlements with poor sanitation, also predisposes to the spread of hepatitis A and E. Besides the potential for increasing number of infections, rising temperatures have been shown to increase in viral pathogenicity, inducing viral replication and mutations (32). The potential for increase in transmission of hepatitis B and C will more probably be a result of the social and economic instability predicted to happen due to the climate crisis. Indeed, social and economic hardship, combined with the dismantlement of healthcare or social facilities for a close contact with vulnerable patients, may increase the exposure to risk factors for hepatitis B and C, namely the use of intravenous drugs.
2.3.4 Other causes of liver disease
The increase in global temperatures has been shown to modulate the typical seasonal pattern of parasitic infections. Fasciolosis is the standard of parasitical liver infection. There is evidence showing climate change driven modifications to the seasonal dynamic of Fasciola hepatica infection (33). Moreover, high-risk areas of infection are predicted to extend to previously low-risk areas (33).
Aflatoxin B1, produced by mycotoxigenic fungi species, including Aspergillus flavus and Aspergillus parasiticus is a known co-factor for hepatocellular carcinoma (34). These molds are particularly prevalent in subtropical regions. Climate change, with increasing ambient temperatures, is driving an increase in the area of prevalence of mycotoxigenic moulds, which are becoming an increasing concern in Europe and North America (35).
3 Call for action for sustainable hepatology
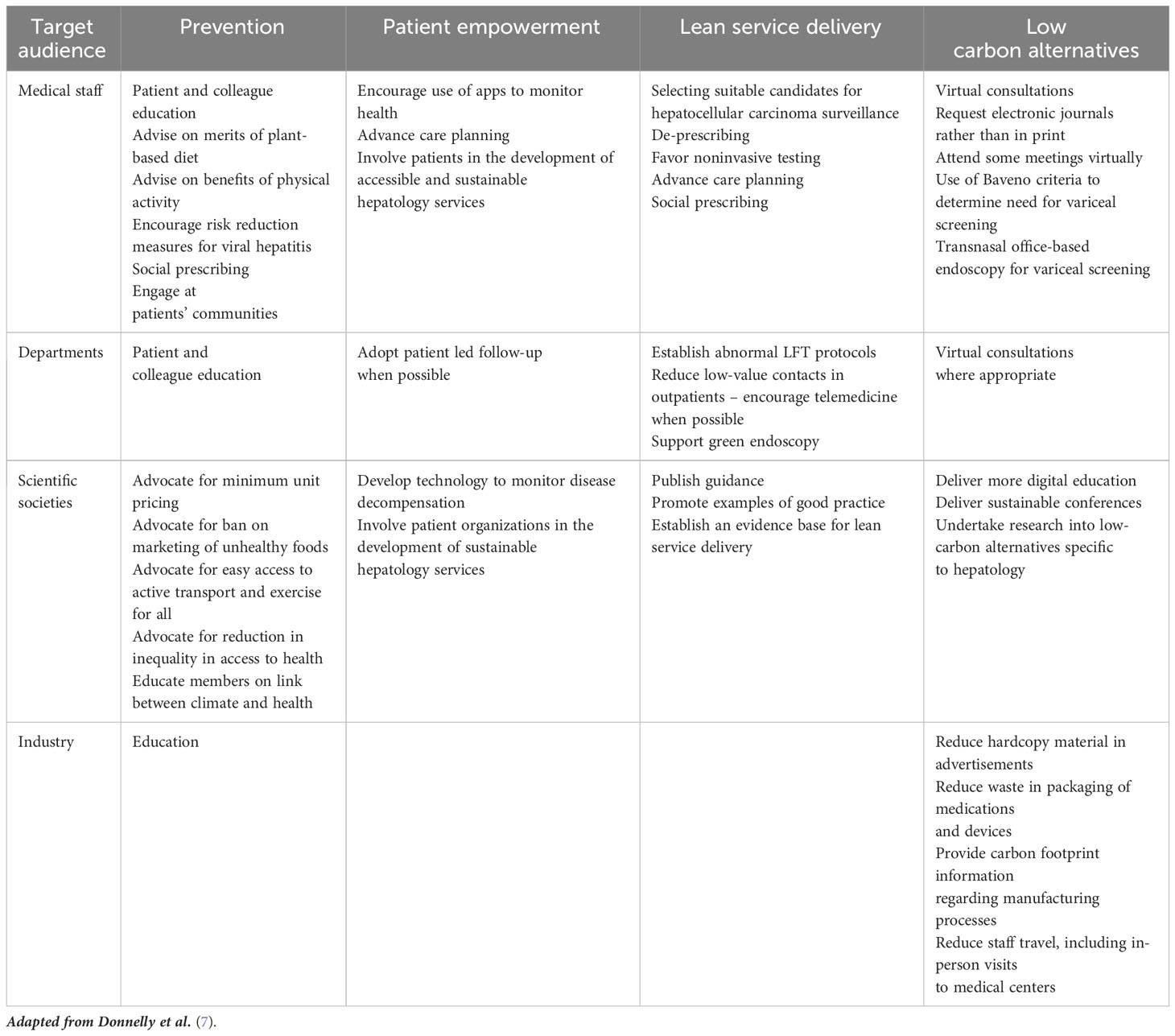
The acknowledgement that medical practice has a significant impact in climate change, scientific societies have been issuing position statements, engaging patients, and healthcare staff to promote more sustainable habits and clinical practices. For Gastroenterology and Hepatology, this movement was initiated by developing standards for the adoption of a “greener” endoscopy practice. More recently, a joint group by the British Association for the Study of the Liver (BASL), the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD) has issued a commentary linking climate change with the care for patients with liver disease (7). This joint position statement offers some guidance regarding the practice of sustainable hepatology. The authors focused on four pillars for sustainable hepatology practice, which included: prevention of disease, patient empowerment, lean service delivery and low carbon alternatives (Table 1).
The incidence of liver disease is intricately dependent of behavioral risk factors, which are often hazardous to the planet themselves. For example, changing the focus of western diet from animal protein and highly processed foods to a plant-based diet would contribute both to decrease the carbon footprint of human feeding but also help mitigating risk factors for liver disease, particularly for MASLD. Additionally, fomenting the practice of physical activity and discouraging the use of motorized transportation would simultaneously contributing to reduce the incidence of MASLD and GHG emissions.
Modern clinical practice is increasingly adopting non-invasive or minimally invasive for the diagnosis and monitoring of diseases. These alternatives frequently have a lower environmental impact comparing to the standard of care. For example, implementing telemedicine appointments for chronically compensated cirrhotic patients, combined with non-invasive tests, may enhance patient compliance and comfort, while reducing the frequency of visits to the clinic. A major example of the utility of non-invasive screening tests in hepatology is the identification of patients with clinically significant portal hypertension using the Baveno VII criteria (36). Selecting patients for variceal screening will help reduce the need for esophagogastroduodenoscopies, therefore mitigating the volume of waste related to endoscopic procedures. The development of standardized and coordinated strategy within each healthcare system will ultimately contribute to improve results. Additionally, besides the reorganization of the healthcare system, the multidirectional interaction between climate change and liver health demands a coordinated and multidisciplinary approach, taking into consideration the insights from scientific societies, patient associations, public health authorities, policy makers, as well as the industry, both medical and alimentary.
The complex interplay between climate change and liver diseases underscores the far-reaching implications of environmental factors on human health. Climate change impacts the incidence, severity, and patient care of liver diseases, including alcohol-related liver disease, MASLD and viral hepatitis. Additionally, liver disease care itself contributes to climate change through energy consumption, pharmaceutical and medical waste, and transportation emissions. Addressing this dual interaction requires a multifaceted approach. Sustainable healthcare practices, telemedicine, waste reduction and recycling, public health strategies, and patient education can collectively reduce the environmental impact of liver disease care while improving patient outcomes. Recognizing the intricate relationship between climate change and liver diseases is essential for promoting a healthier and more sustainable future.
Author contributions
TR: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. GM: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Salas RN, Solomon CG. The climate crisis - health and care delivery. N Engl J Med. (2019) 381:e13. doi: 10.1056/NEJMp1906035
2. Watts N, Amann M, Ayeb-Karlsson S, Belesova K, Bouley T, Boykoff M, et al. The lancet countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet. (2018) 391:581–630. doi: 10.1016/s0140-6736(17)32464-9
3. Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Beagley J, Belesova K, et al. The 2020 report of the lancet countdown on health and climate change: responding to converging crises. Lancet. (2021) 397:129–70. doi: 10.1016/s0140-6736(20)32290-x
4. Service NH. Delivering a ‘Net Zero’ Nation.mal Health Service. London (UK): National Health Service (2020).
5. Eckelman M, Huang K, Lagasse R, Senay E, Dubrow R, Sherman JD. Health care pollution and public health damage in the United States: an update. Health Affairs. (2020) 39:2071–9. doi: 10.1377/hlthaff.2020.01247
6. Devarbhavi H, Asrani SK, Arab JP, Nartey YA, Pose E, Kamath PS. Global burden of liver disease: 2023 update. J Hepatol. (2023) 79:516–37. doi: 10.1016/j.jhep.2023.03.017
7. Donnelly MC, Stableforth W, Krag A, Reuben A. The negative bidirectional interaction between climate change and the prevalence and care of liver disease: A joint bsg, basl, easl, and aasld commentary. J Hepatol. (2022) 76:995–1000. doi: 10.1016/j.jhep.2022.02.012
8. Al-Marwani S. Climate change impact on the healthcare provided to patients. Bull Natl Res Centre. (2023) 47:51. doi: 10.1186/s42269-023-01026-9
9. Vaccari M, Tudor T, Perteghella A. Costs associated with the management of waste from healthcare facilities: an analysis at national and site level. Waste Manag Res. (2018) 36:39–47. doi: 10.1177/0734242x17739968
10. Bawaneh K, Ghazi Nezami F, Rasheduzzaman M, Deken B. Energy consumption analysis and characterization of healthcare facilities in the United States. Energies. (2019) 12:3775. doi: 10.3390/en12193775
11. Lacroute J, Marcantoni J, Petitot S, Weber J, Levy P, Dirrenberger B, et al. The carbon footprint of ambulatory gastrointestinal endoscopy. Endoscopy. (2023) 55:918–26. doi: 10.1055/a-2088-4062
12. Janik-Karpinska E, Brancaleoni R, Niemcewicz M, Wojtas W, Foco M, Podogrocki M, et al. Healthcare waste-a serious problem for global health. Healthcare (Basel). (2023) 11(2):242. doi: 10.3390/healthcare11020242
13. Khan BA, Cheng L, Khan AA, Ahmed H. Healthcare waste management in asian developing countries: A mini review. Waste Manag Res. (2019) 37:863–75. doi: 10.1177/0734242X19857470
14. Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. Managing the health effects of climate change: <Em>Lancet</em> and university college london institute for global health commission. Lancet. (2009) 373:1693–733. doi: 10.1016/S0140-6736(09)60935-1
15. Buttke DE, Raynor B, Schuurman GW. Predicting climate-change induced heat-related illness risk in grand canyon national park visitors. PloS One. (2023) 18:e0288812. doi: 10.1371/journal.pone.0288812
16. Schwartz JD, Lee M, Kinney PL, Yang S, Mills D, Sarofim MC, et al. Projections of temperature-attributable premature deaths in 209 U.S. Cities using a cluster-based poisson approach. Environ Health. (2015) 14:85. doi: 10.1186/s12940-015-0071-2
17. Schulte F, Roosli M, Ragettli MS. Heat-related cardiovascular morbidity and mortality in Switzerland: A clinical perspective. Swiss Med Wkly. (2021) 151:w30013. doi: 10.4414/SMW.2021.w30013
18. Davis BC, Tillman H, Chung RT, Stravitz RT, Reddy R, Fontana RJ, et al. Heat stroke leading to acute liver injury & Failure: A case series from the acute liver failure study group. Liver Int. (2017) 37:509–13. doi: 10.1111/liv.13373
19. Fritze JG, Blashki GA, Burke S, Wiseman J. Hope, despair and transformation: climate change and the promotion of mental health and wellbeing. Int J Ment Health Syst. (2008) 2:13. doi: 10.1186/1752-4458-2-13
20. Pires D, Ambar Akkaoui M, Laaidi K, Chan Chee C, Fifre G, Lejoyeux M, et al. Impact of meteorological factors on alcohol use disorders: A study in emergency departments. Chronobiol Int. (2022) 39:456–9. doi: 10.1080/07420528.2021.2002351
21. Hensel M, Stuhr M, Geppert D, Kersten JF, Lorenz J, Kerner T. Relationship between ambient temperature and severe acute poisoning by alcohol and drugs. Alcohol. (2021) 94:57–63. doi: 10.1016/j.alcohol.2021.04.001
22. Hallström E, Håkansson N, Åkesson A, Wolk A, Sonesson U. Climate impact of alcohol consumption in Sweden. J Cleaner Production. (2018) 201:287–94. doi: 10.1016/j.jclepro.2018.07.295
23. Matsee W, Charoensakulchai S, Khatib AN. Heat-related illnesses are an increasing threat for travellers to hot climate destinations. J Travel Med. (2023) 30(4):1–5. doi: 10.1093/jtm/taad072
24. Sorensen C, Hess J. Treatment and prevention of heat-related illness. N Engl J Med. (2022) 387:1404–13. doi: 10.1056/NEJMcp2210623
25. Pryor RR, Bennett BL, O’Connor FG, Young JM, Asplund CA. Medical evaluation for exposure extremes: heat. Wilderness Environ Med. (2015) 26:S69–75. doi: 10.1016/j.wem.2015.09.009
26. Rinella ME, Lazarus JV, Ratziu V, Francque SM, Sanyal AJ, Kanwal F, et al. A multi-society delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. (2023) 79(6):1542–56. doi: 10.1016/j.jhep.2023.06.003
27. Estes C, Anstee QM, Arias-Loste MT, Bantel H, Bellentani S, Caballeria J, et al. Modeling nafld disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030. J Hepatol. (2018) 69:896–904. doi: 10.1016/j.jhep.2018.05.036
28. Hallam J, Harris NC. What’s going to be on the menu with global environmental changes? Glob Chang Biol. (2023) 29:5744–59. doi: 10.1111/gcb.16866
29. Rampalli KK, Blake CE, Frongillo EA, Montoya J. Why understanding food choice is crucial to transform food systems for human and planetary health. BMJ Glob Health. (2023) 8(5):1–14. doi: 10.1136/bmjgh-2022-010876
30. Guo B, Guo Y, Nima Q, Feng Y, Wang Z, Lu R, et al. Exposure to air pollution is associated with an increased risk of metabolic dysfunction-associated fatty liver disease. J Hepatol. (2022) 76:518–25. doi: 10.1016/j.jhep.2021.10.016
31. Zheng Z, Xu X, Zhang X, Wang A, Zhang C, Hüttemann M, et al. Exposure to ambient particulate matter induces a nash-like phenotype and impairs hepatic glucose metabolism in an animal model. J Hepatol. (2013) 58:148–54. doi: 10.1016/j.jhep.2012.08.009
32. Tarek F, Hassou N, Benchekroun MN, Boughribil S, Hafid J, Ennaji MM. Impact of rotavirus and hepatitis a virus by worldwide climatic changes during the period between 2000 and 2013. Bioinformation. (2019) 15:194–200. doi: 10.6026/97320630015194
33. Fox NJ, White PC, McClean CJ, Marion G, Evans A, Hutchings MR. Predicting impacts of climate change on fasciola hepatica risk. PloS One. (2011) 6:e16126. doi: 10.1371/journal.pone.0016126
34. Hsu IC, Metcalf RA, Sun T, Welsh JA, Wang NJ, Harris CC. Mutational hotspot in the P53 gene in human hepatocellular carcinomas. Nature. (1991) 350:427–8. doi: 10.1038/350427a0
35. Kos J, Anić M, Radić B, Zadravec M, Janić Hajnal E, Pleadin J. Climate change-a global threat resulting in increasing mycotoxin occurrence. Foods. (2023) 12(14):1–18. doi: 10.3390/foods12142704
Keywords: climate change, hepatology, medical waste, metabolic dysfunction-associated steatotic liver disease, alcohol-related liver disease
Citation: Ribeiro T and Macedo G (2024) Climate change and liver disease: a mini review. Front. Gastroenterol. 3:1334877. doi: 10.3389/fgstr.2024.1334877
Received: 07 November 2023; Accepted: 07 February 2024;
Published: 15 May 2024.
Edited by:
Richard Sterling, Virginia Commonwealth University, United StatesReviewed by:
Maryam Alkhatry, Ibrahim Bin Hamad Obaid Allah Hospital, United Arab EmiratesCopyright © 2024 Ribeiro and Macedo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tiago Ribeiro, tiagofcribeiro@outlook.com
 Tiago Ribeiro
Tiago Ribeiro Guilherme Macedo1,2,3
Guilherme Macedo1,2,3