- Department of Radiology, Vachira Phuket Hospital, Phuket, Thailand
Transarterial microembolization (TAME) has gained recognition as a minimally invasive treatment for chronic musculoskeletal pain, demonstrating significant efficacy with a favorable safety profile ( 1, 2). However, complications remain underreported. This case report describes the first documented severe adverse event in a patient with a chronic venous ulcer undergoing TAME for a micro arteriovenous fistula (AVF). The patient developed significant complications, including extensive leg swelling, skin changes, and cellulitis requiring prolonged inpatient care. These findings highlight the importance of patient selection and embolic agent considerations to mitigate potential risks associated with TAME.
Introduction
TAME is an emerging interventional technique for chronic musculoskeletal pain and vascular anomalies, with reported success in osteoarthritis and pain syndromes (2, 3). While previous studies have reported minimal complications, there is limited data on its safety in patients with vascular compromises. This case highlights the first documented severe complication following TAME with Imipenem/Cilastatin (IPM/CS), raising concerns about embolic agent selection and patient eligibility.
Case presentation
A 65-year-old male with a history of chronic venous ulcer presented with persistent leg pain and swelling. Clinical examination revealed an ulcerated lesion over the lower leg with surrounding skin hyperpigmentation and signs of chronic venous insufficiency. Computed tomography angiography identified a micro AVF in the right leg (Figure 1), confirmed by digital subtraction angiography (DSA) (Figure 2). Given his refractory pain and non-healing ulcer, he was referred for TAME as an alternative to surgical management.
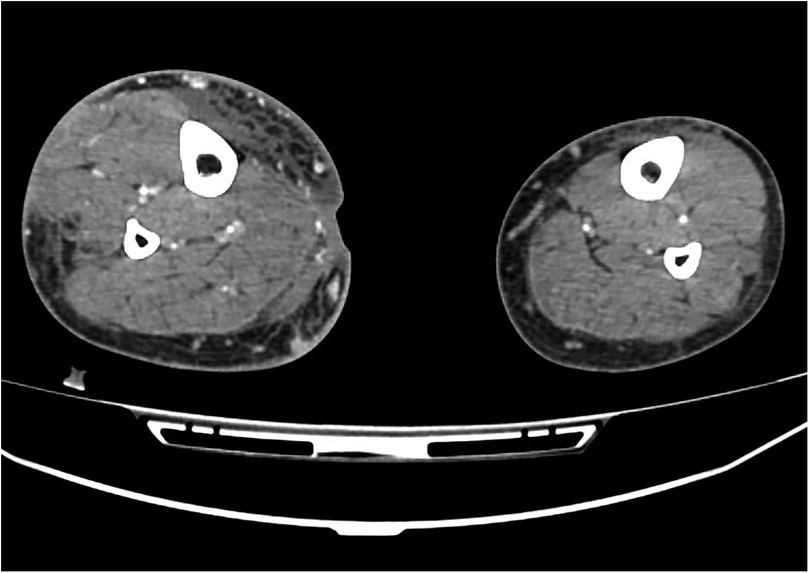
Figure 1. Computed tomography angiography revealed a micro arteriovenous fistula (AVF) in the right leg.
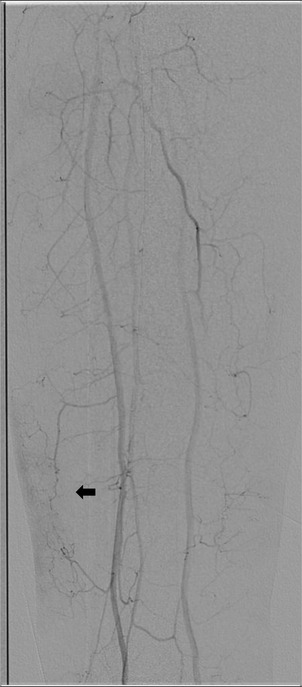
Figure 2. Digital subtraction angiography (DSA) confirmed the presence of abnormal vascular blush (arrow  ).
).
Preprocedural assessment
Baseline laboratory investigations showed normal coagulation parameters and no active infection. Imaging confirmed a high-flow micro AVF supplying the ulcerated region. After multidisciplinary discussion, TAME was planned to use intra-arterial IPM/CS, based on prior studies supporting its efficacy in osteoarthritis and neovascularization (3).
Procedure
A 4-French sheath was introduced via femoral artery access under ultrasound guidance. Superselective catheterization of the target feeding arteries was achieved using a microcatheter. A slow intra-arterial infusion of IPM/CS was performed, with a total of 1.5 ml of IPM/CS (500 mg in 5 ml contrast) administered into the anterior tibial artery under fluoroscopic guidance. Post-embolization angiography confirmed the occlusion of the abnormal microvasculature.
Postprocedural course
The patient was discharged without immediate complications. However, two days later, he returned with worsening lower limb swelling, erythema, and multiple fluid-filled blebs (Figure 3). These symptoms suggested acute tissue ischemia and an inflammatory response, raising concern for severe non-target embolization. The patients developed cellulitis and worsening tissue breakdown necessitated prolonged inpatient care, including intravenous antibiotics, wound debridement, and limb elevation. Over subsequent weeks, the patient gradually improved with conservative management, though ulcer healing was significantly delayed (Figure 4).

Figure 3. Two days post-TAME, the patient developed worsening leg swelling, erythema, and multiple fluid-filled blebs.
Discussion
TAME has been extensively studied for osteoarthritis and chronic pain syndromes (1, 3), yet its use in patients with chronic venous ulcers and vascular compromise remains controversial. Liang et al. (4) reported the safety of IPM/CS infusion in treating hand osteoarthritis, noting only transient swelling and discoloration. Similarly, Kubo et al. (5) found high technical success with minimal complications in a cohort of 92 patients undergoing intra-arterial IPM/CS injection.
However, Lin et al. (6) highlighted potential risks, including arterial dissection and catheter-related complications. Our case presents a novel and severe complication, likely resulting from non-target embolization and impaired microvascular perfusion in an ulcerated limb. The inflammatory response following embolization may have exacerbated tissue hypoxia, leading to severe skin breakdown and prolonged recovery.
This case underscores the importance of careful patient selection, particularly for individuals with preexisting vascular insufficiency. The choice of embolic agent remains critical; while IPM/CS has demonstrated efficacy, its effects on compromised microcirculation warrant further investigation.
Conclusion
This case report highlights a rare but significant complication following TAME in a patient with chronic venous ulcer. While TAME remains a promising technique for chronic pain management, its application in patients with vascular compromise should be approached with caution. Future studies should focus on optimizing embolic agent selection and refining patient eligibility criteria to mitigate risks.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics statement
The studies involving humans were approved by VACHIRA PHUKET HOSPITAL RESEARCH ETHICS COMMITTE (VPHREC). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
WB: Data curation, Writing – review & editing, Investigation, Writing – original draft. PN: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bagla S, Piechowiak R, Sajan A, Orlando J, Hartman T, Isaacson A. Multicenter randomized sham controlled study of genicular artery embolization for knee pain secondary to osteoarthritis. J Vasc Interv Radiol. (2022) 33(1):2–10.e2. doi: 10.1016/j.jvir.2021.09.019
2. Kishore S, Sheira D, Malin ML, Trost DW, Mandl LA. Transarterial embolization for the treatment of chronic musculoskeletal pain: a systematic review of indications, safety, and efficacy. ACR Open Rheumatology. (2022) 4(3):209–17. doi: 10.1002/acr2.11383
3. Okuno Y, Korchi AM, Shinjo T, Kato S, Kaneko T. Midterm clinical outcomes and MR imaging changes after transcatheter arterial embolization as a treatment for mild to moderate radiographic knee osteoarthritis resistant to conservative treatment. J Vasc Interv Radiol. (2017) 28(7):995–1002. doi: 10.1016/j.jvir.2017.02.033
4. Liang K-W, Wang B, Huang H-H, Tsao T-F, Tyan Y-S, Wang P-H. Effectiveness and safety of intra-arterial imipenem/cilastatin sodium infusion for patients with hand osteoarthritis–related interphalangeal joint pain. J Vasc Interv Radiol. (2023) 34(9):1485–92. doi: 10.1016/j.jvir.2023.05.035
5. Kubo T, Miyazaki K, Shibuya M, Sugihara E, Nakata M, Okuno Y. Intra-arterial injection of temporary embolic material through a needle inserted into the radial or ulnar artery for distal and proximal interphalangeal joint osteoarthritis: a retrospective study of 92 patients. Cardiovasc Intervent Radiol. (2023) 46(10):1375–82. doi: 10.1007/s00270-023-03514-x
Keywords: transarterial microembolization, imipenem/cilastatin, chronic venous ulcers, musculoskeletal pain, embolization complications, patient safety
Citation: Boonlorm W and Nisityotakul P (2025) Severe complications following transarterial microembolization for a micro arterio-venous fistula in a patient with chronic venous ulcer: a case report. Front. Radiol. 5:1613940. doi: 10.3389/fradi.2025.1613940
Received: 18 April 2025; Accepted: 3 July 2025;
Published: 18 July 2025.
Edited by:
Genti Xhepa, Ente Ospedaliero Cantonale (EOC), SwitzerlandReviewed by:
Pierluca Torcia, IRCCS Ca 'Granda Foundation Maggiore Policlinico Hospital, ItalyRajesh Kumar, Kerala University of Health Sciences, India
Bow Wang, National Cheng Kung University Hospital, Taiwan
Copyright: © 2025 Boonlorm and Nisityotakul. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Panat Nisityotakul, Y29rb2N1cDEzQGdtYWlsLmNvbQ==
 Wankarn Boonlorm
Wankarn Boonlorm Panat Nisityotakul*
Panat Nisityotakul*
