- Department of Public Health, Institute of Health Science, Wollega University, Nekemt, Ethiopia
Background: Fertility desire in people living with HIV is the desire of people to have children in the future despite a diagnosis of HIV. The desire to have children among reproductive-age women living with HIV has significant implications for the transmission of HIV to sexual partners and newborns in the future. There is no study conducted to determine the magnitude of the fertility desire among women of reproductive age living with HIV in East Wollega western Ethiopia. Therefore this study aimed to determine fertility desire and associated factors among women of reproductive age living with HIV receiving ART.
Objectives: To assess fertility desire and associated factors among reproductive-aged women on antiretroviral treatment in East Wollega, West Ethiopia, 2023.
Methods: A facility-based cross-sectional study was conducted in East Wollega from January 01/2023 to 30/2023. Data was collected from 419 study participants using interviewer-administered structured questionnaires by employing systematic random sampling techniques. Data entry and analysis were performed using Epi Data version 3.1 and SPSS version 23, respectively. Both bivariate and multivariate analyses were carried out using binary logistic regression. Statistical significance was established for variables with P < 0.05 in the multivariate analysis.
Results: Among the 419 respondents, 166 (39.62%) reported that they desired to have children in the future. Age between 18 and 24 years (AOR = 2.49, 95% CI; 1.16, 5.35), having partner Living with HIV: (AOR = 0.50, 95% CI; 0.25, 0.9), and being married (AOR = 2.69, 95% CI; 1.65, 4.39) were significantly associated with fertility desire.
Conclusion: The proportion of women of reproductive age living with HIV who desired children was high in this cohort. Understanding the fertility desire among women living with HIV/AIDS has a significant role in reducing perinatal transmission of HIV. Hence, Health care workers should provide intensive counselling regarding the possibility of the mother-to-child transmission of HIV.
Introduction
Fertility is the ability conceive a child through regular sexual activity. The desire for fertility for people living with HIV is the desire of people to have children in the future despite having a diagnosis of human immunodeficiency virus (HIV) (1–4).
Women living with HIV have decreased desire for fertility due to various opportunistic infections. HIV infection results in decreased spermatozoa production, coital frequency, fetal survival, and partner survival (2, 5–7). According to community perception People living with HIV (PLWH) and related opportunistic infections cannot be sexually active, marry, or commit to divorce (3, 6). Community norms, stigma, and discrimination also influence the desire to have children (8, 9).
HIV can be transmitted from mother to child throughout the antepartum (5%–10%), intrapartum (10%–15%), and postpartum (30%–45%) periods, depending on the timing of infection and the availability of services for prevention of mother-to-child transmission (PMTCT) (4). PMTCT is the main pillar in the reduction of perinatal transmission to less than 2% among the non-breastfeeding population and 5% among the breastfeeding population (2). The aim of the PMTCT program in Ethiopia was to achieve 95% ART coverage for pregnant women living with HIV by 2015 (5).
A 4-pronged approach toward preventing HIV transmission includes preventing unintended pregnancy, preventing HIV transmission from mothers living with HIV to their infants, and providing treatment and support for women infected with HIV, their infants, and their families (4, 5). Couples have the right to marry, express sexuality, and experience parenthood, regardless of their HIV status (2, 8). Fertility desire among women living with HIV ranges from 12.1% in Asian countries to 50.8% in sub-Saharan African countries. In Ethiopia, fertility desire ranges from 34% to 45% (9–11). However, these women face challenges such as high HIV prevalence, poor health systems, and the risk of MTCT (5, 12–14). Decreased fertility desire is influenced by fear of perinatal HIV transmission, preterm delivery, divorce, HIV-related stigma, and poor health status (15–17). Low PMTCT coverage and poor integration with maternal services are the main challenges faced by the Ethiopian government. To address these issues, Ethiopia has adopted the WHO PMTCT strategy, which has increased fertility desire due to improvements in quality of life, survival rate, and reproductive health services (2). There is no study conducted to determine the magnitude of the fertility desire among women of reproductive age living with HIV in east Wollega western Ethiopia. Hence; this study assessed fertility desire among women of reproductive age living with HIV in East Wollega, Ethiopia.
Methods and materials
Study setting and period
The study was conducted in two public hospitals and six health centers in the eastern Wollega zone. The East Wollega Zone is located 333 km from the capital city of Addis Ababa in western Ethiopia. According to the 2007 census, this zone has a total population of 1,213,503 people, of whom 606,379 are men and 607,124 are women. There were 16,623 people currently on ART in the study area, 5,385 of whom were reproductive-aged women. Of the 5,385 reproductive-aged women, 2,311 were receiving ART services at eight randomly selected public health facilities. This study was conducted from January 1, 2023, to January 30, 2023.
Study design
A facility-based cross-sectional study was conducted.
Study population
All reproductive-aged women who were receiving ART during the study period at selected public health facilities in the east Wollega zone.
Inclusion and exclusion criteria
The study enrolled women living with HIV who had a follow-up and lived longer than 6 months. We exclude all women who were critically ill and those who had a hearing problem.
Sample size determination and sampling procedure
The single population proportion formula (P) was used to determine the sample size by considering the following assumptions. Based on the findings from Addis Ababa, the prevalence of fertility desire was 54.6% (10), with a 95% confidence level and a 5% margin of error (d). Finally, with the addition of the 10% nonresponse rate, the final sample size became 419. The total sample size was proportionally allocated to the 8 randomly selected ART-providing public health facilities, and a systematic random sampling technique was employed to recruit the study participants. The first participant was randomly selected, and the remainder of the study unit was recruited based on the calculated kth (K = 5) interval until the required final sample size was achieved (Figure 1).
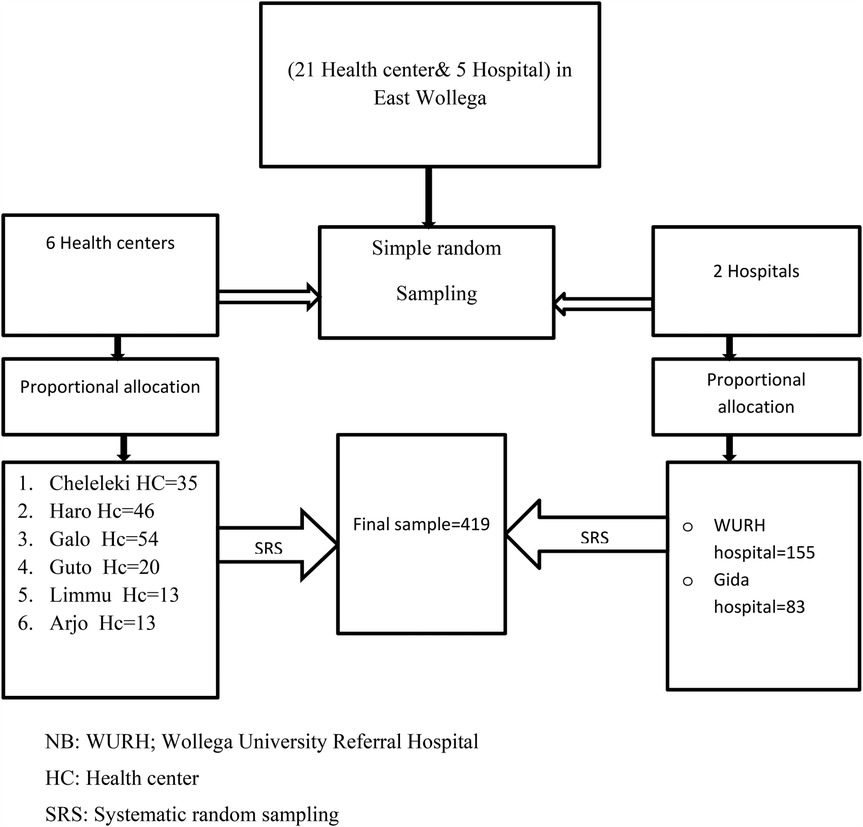
Figure 1. Schematic representation of the sampling procedures, showing the sampling procedure for reproductive-aged women on an ART in public health facilities in the east Wollega zone, Oromia, Ethiopia 2023. NB, WURH; Wollega University Referral Hospital; HC, health center; SRS, systematic random sampling.
Study variables
Dependent variable
Fertility desire (Yes, No).
The independent variables included sociodemographic factors (age, educational level, marital status, occupational status), sex-related factors, family planning, reproductive-related factors, clinical factors related to HIV, partner-related factors, knowledge about PMTCT and MTCT, and community pressure.
Fertility desire
A psychological state in which someone has the personal motivation to have a child. Those who are motivated to have more children in the future have fertility desire. Those who have no motivation to have more children have no fertility desire (10).
Treatment stage
This stage is based on the WHO classification of a patient's clinical condition on ART.
The viral load is the number of RNA copies per milliliter of blood (18).
Regular partner
Women who had regular sexual relationships (19) with men.
Sexually active
Women who have performed at least one sexual practice during the last six months (20).
Community pressure
Women who have community approval/disapproval for having children irrespective of their HIV status. If there is intense pressure from family, spouses and friends to reproduce, this pressure is considered yes, and the reverse is true (5).
Data collection methods and instruments
The data were collected using pretested, interviewer-administered structured questionnaires. The questionnaire was initially prepared in English and then translated into the Afaan Oromo language and returned to English to check for validity and reliability. Data collectors and supervisors were recruited from health professionals in the respective health facilities, and 3 days of training was given prior to data collection on the methods of data handling and supervision accuracy.
Data quality control
The prepared tool was pretested on 5% of the population in the Nekemt Specialist Hospital. The results of the pretest were analyzed, and necessary modifications were made. Three days of training were provided to ensure data quality. The completed questionnaires were cross-checked by supervisors and the principal investigator to ensure data completeness. Data cleaning and checking for missing values were conducted prior to analysis.
Data processing and analysis
The data were entered into EPI Data Version 3.1 and exported to SPSS Version 22.0 for analysis. Descriptive statistics were used to summarise the frequency, percentage, and mean of the characteristics of the study participants. Multicollinearity was assessed by the variance inflation factor (VIF) >10, which was considered problematic. Model fitness was checked by Hosmer and Lemshow's goodness-of-fit test. Binary logistic regression analysis was used to ascertain the associations between explanatory variables and outcomes. Variables with a P-value less than 0.25 in the bivariable analysis were entered into the multivariable analysis. Variables with p < 0.05 in the multivariable logistic regression were considered to have a statistically significant association with the outcome variable.
Results
Sociodemographic characteristics of the study respondents
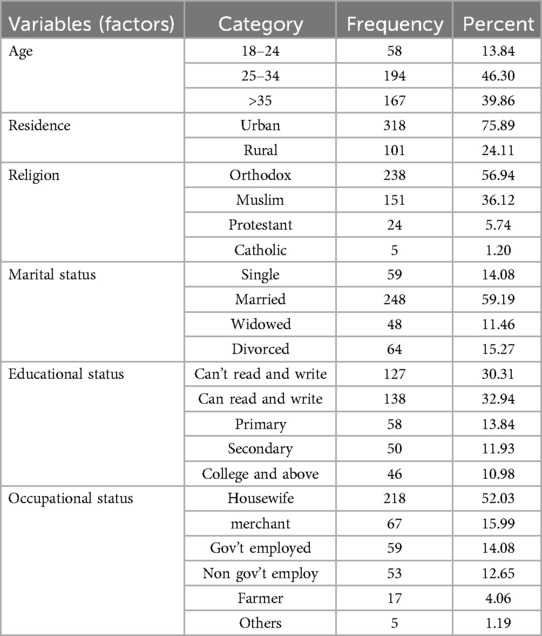
A total of 419 respondents, participated in the study with a response rate of 100%. The mean age of the respondents was 32.8 years (SD ± 6.92), and the majority of the respondents were 24–34 years old, accounting for 194 (46.30%) of the sample. Approximately 318 (75.89%) of the reproductive-age women who participated in the study lived in urban areas. The majority of the study subjects (238, 56.94%) were orthodox Christians and 218 (52.08) were housewives (Table 1).
Reproductive history, family planning, sex-related factors, and reasons for fertility desire
Regarding the desire to have children, approximately 166 (39.62%) respondents said they had a desire for fertility or more children. Seventy-eight percent of the study participants got pregnant at least once during the data collection period among those, 180 (55.02%), became pregnant after receiving an HIV diagnosis. Of the study study subjects, 109 (26.02%) had three or more children. Approximately 215 (64.95%) individuals used contraceptives, 76 (35.35%) of whom used an injectable form of birth control. Of the study subjects 274 (65.39%) disclosed their HIV status to their sexual partners. The time for future child desire was not decided in 65 (39.16%) participants, and approximately 23% of people want to have a child within two to three years. Approximately 154 (36.75%) had community pressures that influenced them to have children (Table 2).
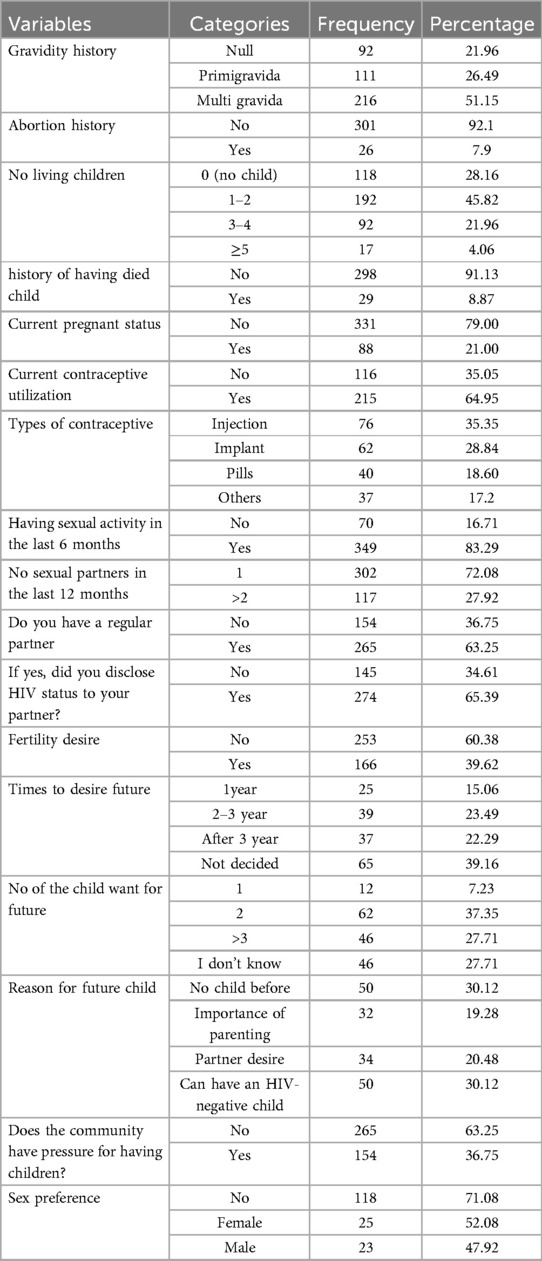
Table 2. Reproductive history, family planning, sexually related factors and reasons for fertility desire among HIV-positive reproductive age women attending ART clinics in east Wollega public health facilities, western Ethiopia, 2023 (n = 419).
Clinical characteristics and knowledge of MTCT and PMTCT
Of the study subjects, 125 (29.83%) and 294 (70.17%) individuals had been on ART for 5 or fewer years and more than 5 years, respectively. Of the total participants 44 (10.5%), 79 (18.85%), and 296 (70.64%) had CD4 counts less than or equal to 200, 201–499, and 500 and greater per microliter of blood, respectively. Of the total participants in the study, 195 (78.31%) responded that their partners' HIV status was positive (Table 3).
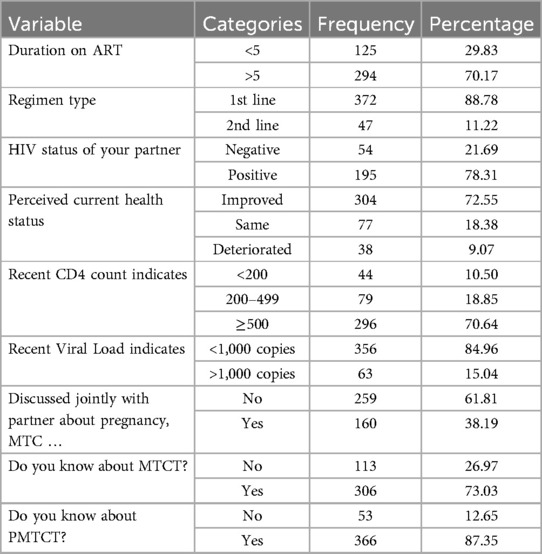
Table 3. Clinical characteristics and knowledge-related factors MTCT and PMTCT among HIV-positive reproductive age women attending ART clinics in east Wollega public health facilities in western Ethiopia, 2023 (n = 419).
Factors associated with fertility desire
The following variables were significantly associated with fertility desire in this study population: age, marital status, having a regular partner, educational status, community pressure, number of living children, and HIV status of the partner. The odds of fertility desire were 2.5 times greater among women aged 18–24 years than among those aged ≥35 years [AOR = 2.5, p = 0.019, 95% CI (1.16, 5.35)]. The odds of having fertility desire were 2.69 times greater among married women than among unmarried women [AOR = 2.69, p = 0.000*, 95% CI (1.65, 4.39)]. Study participants who had a college education or above had 3.02 times greater fertility desire than those who could not read or write [AOR = 3.02, p = 0.008, 95% CI (1.3, 6.84)]. The odds of fertility desire were 2.72 times greater and 3.72 times greater among mothers who had no or less than 2 children, respectively, than among mothers who had more than three children [AOR = 2.72, 95% CI (1.35, 5.5)] and [AOR = 3.72, 95% CI (2.0, 6.8)], respectively (Table 4).
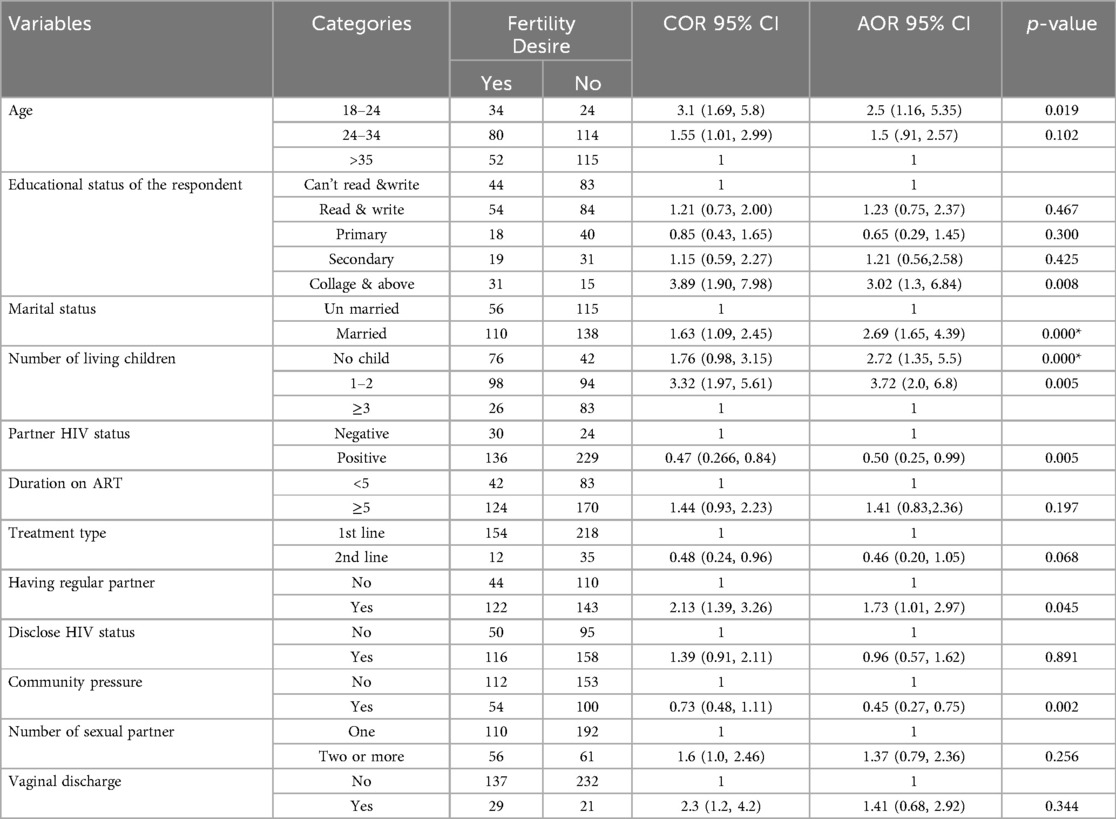
Table 4. Bivariable and multivariable logistic regression analysis of factors associated with fertility desire among PLHIV of reproductive age in east Wollega public health facilities, 2023.
Discussion
The findings of this study showed that 39.6% of the study subjects desire to conceive. This finding was in line with a study conducted in Tanzania and Uganda which ranges from 35% to 39.5 (21–23). However, this percentage was lower than that reported in studies in Addis Ababa (54.6%) (10), Harrison (52.9%) (24), and South Africa (80%) (25). This disparity might be due to differences in the study period, study design, study area, and population under study.
Factors associated with the desire to conceive included being married or having a regular partner (AOR 2.69), having a college education (AOR 3.02), and having no children (AOR 2.72). The odds of having a fertility desire were 2.69 times greater among women who were married or had regular partners compared to those who were unmarried or had irregular partners of reproductive age living with HIV. These findings align with research from India (26), northern Nigeria (27, 28), and Brazil (29). This may be attributed to the fact that being in a committed relationship provides a sense of security and reliable support for raising children. Furthermore, the odds of having a fertility desire among women with regular partners were also 2.69 times greater than those among women with irregular partners, consistent with findings from Addis Ababa (10), Hawasa (8), and Jimma (18). This is due to a greater ability to make shared decisions between the partners on having children who are free from human immune deficiency virus.
Study participants who had a college education or above had 3.02 times greater fertility desire than those who could not read or write. This finding is supported by a study at the Amhara Regional Referral Hospital, which showed that having no formal education decreased fertility desire by 49% (1). This might be attributed to the fact that educated people have better decision-making skills than individuals with no formal education. Further, more educated people have a better understanding of mother to child transmission and available prevention services.
Having a regular partner increases the odds of fertility desire among PLHIV by 2 times compared to those who do not have a regular partner, and having a partner living with HIV decreases fertility desire by 50%. These findings were supported by similar studies in India, Nigeria, and Brazil (26–29). However, this finding contradicts findings from a study conducted in Australia (3, 19). This might be due to greater perceived stigma against their children in the community and lower economic capability for caring for their children whenever both couples are living with HIV.
The odds of fertility desire were 2.72 times greater and 3.72 times greater among mothers who had no children and who had ≤2 children, respectively, than among mothers who had more than three children. This finding is consistent with studies from northern Nigeria (28), Brazil (29), and Uganda (22). This might be attributed to the intensive counseling they received during each delivery at health facilities on PMTCT and reproductive health services and their greater awareness of further pregnancy. However, this finding contradicts findings from a study in Harari. This might be due to the lower PMTCT service and lower engagement in decision making regarding the number of children in this area compared to the current study setting (24).
Limitations of the study
Due to the nature of cross-sectional study design, establishing cause-and-effect relationships is difficult.
Conclusion
In this study, the magnitude of desire for fertility among reproductive-aged women living with HIV was high. Age, marital status, level of education, number of children still alive, having a regular partner, community pressure, and partner HIV status were found to be factors associated with the desire for reproduction among PLHIV.
Recommendation
Based on the findings of the study, the following recommendations have been proposed.
For health care providers, health care facilities, zonal health departments, regional health bureaus and ministries of health
⮚ Health care providers should provide intensive counselling regarding the possibility of the mother to child transmission of HIV. Health care providers should strengthen counseling on MTCT for Women who had no child.
⮚ Health professionals should strengthen the involvement and support of their partner during antenatal care visits and on antiretroviral drug adherence to minimize the risk of HIV transmission.
⮚ The regional health bureau and Zonal Health Department should emphasize the integration of family planning with HIV/AIDS care for women of reproductive age living with HIV to prevent unwanted pregnancy.
⮚ The Ministry of Health should increase services and support for MTCT and PMTCT.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
This study involved human participants and was conducted in accordance with the Declaration of Helsinki and approved by Wollega University ethical review committee with the (protocol number WU/RO/567/2016), and permission to conduct the study in health facilities was secured from the zonal health department and respective health facilities. Informed written consent was obtained from each respondent after the objective and purpose of the study were explained. For participants aged less than 18 years old informed written consent was obtained from the mothers or care givers of the study participants.
Author contributions
WF: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Funding acquisition, Validation.
Funding
The author declares that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
I would like to thank the Wollega University College of Health Sciences Department of Public Health for giving me this opportunity to conduct this research. I would like to thank the East Wollega Health Department and health facility for their cooperation in providing the necessary information for this manuscript. Finally, I would like to thank the study participants and data collectors.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AIDS, acquired immunodeficiency syndrome, AOR, adjusted odd ratio; ART, antiretroviral therapy; COC, combined oral contraceptive; EDHS, Ethiopian Demographic Health Survey; ETB, ethiopian body; HIV, human immune-virus; NGO, nongovernmental organization; PI, principal investigator; PLWHIV, people living with human immune-virus; PMTCT, prevention of mother-to-child transmission; SPSS, statistical package for social science; SRS, systematic random sampling; STI, sexually transmitted infections; WHO, World Health Organization.
References
1. Mekonnen B, Minyihun A. Fertility desire and associated factors among HIV positive women attending ART clinics in Amhara region referral hospitals in northwest Ethiopia, 2017. HIV/AIDS (Auckl). (2019) 11:247. doi: 10.2147/HIV.S221941
2. Shiferaw T, Kiros G, Birhanu Z, Gebreyesus H, Berhe T, Teweldemedhin M. Fertility desire and associated factors among women on the reproductive age group of antiretroviral treatment users in Jimma town, south west Ethiopia. BMC Res Notes. (2019) 12(1):158. doi: 10.1186/s13104-019-4190-7
3. Melaku YA, Zeleke EG, Kinsman J, Abraha AK. Fertility desire among HIV-positive women in Tigray region, Ethiopia: implications for the provision of reproductive health and prevention of mother-to-child HIV transmission services. BMC Womens Health. (2014) 14(1):137. doi: 10.1186/s12905-014-0137-2
4. Federal HIV/AIDS Prevention and Control. Guidelines for Prevention of Mother-to-Child Transmission of HIV in Ethiopia. Addis Ababa: FHAPCO (2007).
5. Demissie DB, Tebeje B, Tesfaye T. Fertility desire and associated factors among people living with HIV attending antiretroviral therapy clinic in Ethiopia. BMC Pregnancy Childbirth. (2014) 14(1):1–10. doi: 10.1186/s12884-014-0382-2
6. Fertility desire and associated factors among ARTuser reproductive-age women in public health-facility in Gondar city administration NorthwestEthiopia.
8. Eniyew MA, Haji Y, Abebe K, Demelash M, Mesfin Y, Embiale A, et al. Fertility desire and associated factors among people on antiretroviral treatment at a public health facility in Hawassa city, southern Ethiopia. Afr Health Sci. (2022) 22(3):24–33. doi: 10.4314/ahs.v22i3.5
9. Haile F, Isahak N, Dessie A. Fertility desire and associated factors among people living with HIV on ART, in Harari Regional State, Eastern Ethiopia. J Trop Dis. (2014) 2(3):11.
10. Adilo TM, Wordofa HM. Prevalence of fertility desire and its associated factors among 15-to 49-year-old people living with HIV/AIDS in Addis Ababa, Ethiopia: a cross-sectional study design. HIV/AIDS (Auckl). (2017) 9:167. doi: 10.2147/hiv.s133766
11. Aylie NS, Dadi LS, Alemayehu E, Mekonn MA. Determinants of fertility desire among women living with HIV in the childbearing age attending antiretroviral therapy clinic at Jimma university medical center, southwest Ethiopia: a facility-based case‒control study. Int J Reprod Med. (2020) 2020:8. doi: 10.1155/2020/6504567
12. Woretaw A, Aemro A. High fertility desire and associated factors among people living with HIV at the University of Gondar specialized hospital, Ethiopia; a cross-sectional study. Research Square [Preprint] (2022):13–5. doi: 10.21203/rs.3.rs-1533073/v1
13. Mohammed F, Assefa N. Determinants of desire for children among HIV-positive women in the Afar region, Ethiopia: case control study. PLoS One. (2016) 11(3):e0150566. doi: 10.1371/journal.pone.0150566
14. Abbawa F, Awoke W, Alemu Y. Fertility desire and associated factors among clients on highly active antiretroviral treatment at finoteselam hospital northwest Ethiopia: a cross sectional study. Reprod Health. (2015) 12(1):1–7. doi: 10.1186/s12978-015-0063-2
15. Melka AS, Wordofa MA, Wossen BA. Determinants of fertility intention among women living with HIV in western Ethiopia: implications for service delivery. Afr J Reprod Health. (2014) 18(4):54–60.
16. Feyissa TR, Harris ML, Forder PM, Loxton D. Fertility among women living with HIV in western Ethiopia and its implications for prevention of vertical transmission: a cross-sectional study. BMJ Open. (2020) 10(8):e036391. doi: 10.1136/bmjopen-2019-036391
17. Amare E, Hailu G, Bogale K, Zewale T. Fertility intention and associated factors among anti-retroviral treatment user. (2019).
18. Arero WD, Teka WG, Hebo HJ, Woyo T, Amare B. Prevalence of long-acting reversible contraceptive methods utilization and associated factors among counseled mothers in immediate postpartum period at Jimma university medical center, Ethiopia. Contracep Reprod Med. (2022) 7(1):1–10. doi: 10.1186/s40834-022-00184-x
19. Bavinton BR, Duncan D, Grierson J, Zablotska IB, Down IA, Grulich AE, et al. The meaning of “regular partner” in HIV research among gay and bisexual men: implications of an Australian cross-sectional survey. The Journal of the International AIDS Society (JIAS). (2016) 22(4):10. doi: 10.1007/s10461-016-1354-5
20. Yan X, Du J, Ji G. Prevalence and factors associated with fertility desire among people living with HIV: a systematic review and meta-analysis. PLoS One. (2021) 16(3):e0248872. doi: 10.1371/journal.pone.0248872
21. Mmbaga EJ, Leyna GH, Ezekiel MJ, Kakoko DC. Fertility desire and intention of people living with HIV/AIDS in Tanzania: a call for restructuring care and treatment services. BMC Public Health. (2013) 13:1–8. doi: 10.1186/1471-2458-13-86
22. Gutin SA, Namusoke F, Shade SB, Mirembe F. Fertility desires and intentions among HIV-positive women during the postnatal period in Uganda. Afr J Reprod Health. (2014) 18(3):67–77.25438511
23. Matovu JK, Makumbi F, Wanyenze RK, Serwadda D. Determinants of fertility desire among married or cohabiting individuals in Rakai, Uganda: a cross-sectional study. Reprod Health. (2017) 14(1):1–11. doi: 10.1186/s12978-016-0272-3
24. Assefa S, Dheresa M, Lami M, Berhanu B, Mohammed H, Sertsu A, et al. Fertility desires of antiretroviral therapy-attending HIV-positive women and its associated factors in Harari region, Ethiopia. Int Health. (2023) 2:ihad030. doi: 10.1093/inthealth/ihad030
25. Myer L, Morroni C, Rebe K. Prevalence and determinants of fertility intentions of HIV-infected women and men receiving antiretroviral therapy in South Africa. AIDS Patient Care STDS. (2007) 21(4):278–85. doi: 10.1089/apc.2006.0108
26. Saya GK, Premarajan KC, Roy G, Sarkar S, Kar SS, Ulaganeethi R, et al. Current fertility desire and its associated factors among currently married eligible couples in urban and rural area of Puducherry, south India. Afr Health Sci. (2021) 21(3):1385–95. doi: 10.4314/ahs.v21i3.50
27. Adah G, Adah R, Agbo H, Zoakah A. Fertility intentions and associated factors of HIV positive women of reproductive age in JOS, northcentral Nigeria. Int J Sex Reprod Health Care. (2021) 4(1):006–12. doi: 10.17352/ijsrhc.000019
28. Kaoje A, Ibrahim M, Njoku C, Gusau G, Saad A, Raji M. Predictors of fertility desire among people living with HIV attending anti-retroviral clinic in a tertiary health facility in Sokoto, northern Nigeria. Sahel Med J. (2015) 18(1):14. doi: 10.4103/1118-8561.152153
Keywords: PLHIV, fertility desire, reproductive women, East Wollega, Ethiopia
Citation: Fikadu W (2025) Fertility desire and associated factors among reproductive age women on anti-retroviral therapy in East Wollega public health facilities, west Ethiopia: facility based cross-sectional study. Front. Reprod. Health 7:1449392. doi: 10.3389/frph.2025.1449392
Received: 14 June 2024; Accepted: 19 May 2025;
Published: 12 June 2025.
Edited by:
Astawus Alemayehu, Haramaya University, EthiopiaReviewed by:
Rosie Mngqibisa, Enhancing care Foundation, South AfricaAnna Bershteyn, New York University, United States
Copyright: © 2025 Fikadu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Worku Fikadu, d2Zpa2FkdTJAZ21haWwuY29t; d29ya3VmaWthZHU4MzI5QGdtYWlsLmNvbQ==
 Worku Fikadu
Worku Fikadu