- 1Department of Public Health, Asirat Woldeyes Health Science Campus, Debrebirhan University, Debrebirhan, Ethiopia
- 2School of Public Health, College of Health Sciences and Medicine, Dilla University, Dilla, Ethiopia
- 3School of Public Health, College of Health Sciences and Medicine, Wolaita Sodo University, Wolaita, Ethiopia
Introduction: Adolescents are defined by the World Health Organization as people aged 10–19, youth 15–24, and young people 10–24. Youth are a demographic that experiences life-threatening physical, emotional, mental, and social changes. Most young individuals are therefore more vulnerable to reproductive health problems than adults for a number of reasons.
Methods: A community-based cross-sectional study was done in Dilla town between January and March 2024 with 536 youths. A survey of houses with young people was followed by the use of a systematic sampling technique. Data was gathered using pretested and structured questionnaires. Coded and entered into EPI INFO version 7 after being verified for completeness, it was then exported to SPSS version 22 for analysis. Both multivariate and bivariate logistic regression were performed. Variables with a p-value <0.2 in bi-variable logistic regression were moved to multivariable logistic regression, and variables with a p-value of <0.05 in multivariable logistic regression were considered statistically significant.
Result: A total of 493 youths participated in this study, with a response rate of 92%. Among them, 271 (55%) of them were under the age group of 21–25 years old, 225 (45.6%) were females, and 214 (43.4%) were protestants. In addition, 287 (58.2%) said that they are ashamed to discuss sexual issues, and a few respondents, 158 (32%), had multiple sexual partners. Most of the respondents (92.1%, 87.4%, 100%, and 72.6%) reported that they had no history of khat chewing, cigarette smoking, shisha smoking, or drinking alcohol, respectively. The overall youth reproductive health problem in Dilla town is 66.1% (95% CI: 62.5–70.4). Being in the age category 21–25 (AOR: 8.52; 95% CI: 4.61–15.76), employed (AOR: 2.12; 95% CI: 1.09–4.13), ashamed to discuss sexual issues (AOR: 6.66; 95% CI: 3.79–11.71), having multiple sexual partners (AOR: 2.01; 95% CI: 1.08–3.73), not using condoms (AOR: 4.05; 95% CI: 2.31–7.11), health facility inconvenience (AOR: 3.2; 95% CI: 1.85–5.55), and drinking alcohol (AOR: 2.28; 95% CI: 1.29–3.99) were found to be significantly associated with youth reproductive health problems.
Conclusion and recommendation: Healthcare facilities should provide comprehensive, age-appropriate, and accurate sexual education as part of specialized reproductive health services for youth that prioritize privacy and nonjudgmental treatment. In addition, screening and early detection of RH problems and engaging in community outreach programs are some of the recommended activities.
Introduction
The World Health Organization defines youth as people between the ages of 15 and 24 who exhibit substantial physiological, psychological, and social changes that put their lives at risk. According to estimates, youth between the ages of 15 and 24 make up 17.0% of the world's population, 20.0% of Sub-Saharan Africa, and 17.9% of Ethiopia's population (1, 2).
Around the world, young people are dealing with a variety of sexual and reproductive health issues, including unintended pregnancy, unsafe abortion, sexually transmitted infections, and human immunodeficiency virus. Young people do not frequently require specialized medical care despite being misunderstood as being in good health. Globally, there are 1.8 billion young people; the majority live in low- and middle-income nations. Young people in low and middle-income nations, numbering 1.3 million, are reported to die every year from preventable causes despite being the healthiest segment of the population (2, 3).
Young people did not have access to proper reproductive health information and services, and they underutilized these services when they were provided. The challenges linked with youth reproductive health have become more serious and complex as a result of this predicament (4). Despite the comprehensive knowledge of HIV and other Reproductive Health (RH) problems increasing around the world, many young people do not have the information or means to protect themselves from these problems. The lack of information about risky sexual behaviors significantly impacts young people, making them more vulnerable to the challenges of early marriage, unwanted pregnancy, HIV, STIs, and other reproductive health problems (5–7).
The majority of young people begin sexual activity throughout their adolescence with several partners before their eighteenth birthday. It is estimated that 30–35 million abortions are performed globally each year, with about half of them being illegal. Teenagers account for a significant part of all abortions. The prevalence of STIs is higher among young people aged 15–24 in Sub-Saharan Africa than in any other age group (8–10).
Nearly 6,000 young individuals between the ages of 15 and 24 get infected with HIV every day around the world. However, only a small percentage of individuals are aware that they are sick. There is a solution to stop HIV/AIDS from spreading, focusing on young people. Today, more than half of those newly infected with HIV are between the ages of 15 and 24 (11, 12).
Early marriage is frequent in many parts of the world, but it is most prevalent in Africa and South Asia. In Nigeria, 76% of females get married by the age of 18, compared to 50% in India. In Nepal, 19% of girls are married before they are 15, and 60% are married by the age of 18 (13).
Early marriage, which roughly corresponds to menarche, and early frequent childbearing with a subsequent abortion, which is often dangerous, or carrying the fetus to full term, which limits their possibilities for socioeconomic growth, are common in Ethiopia. According to findings, children born to teenage mothers have a significantly higher risk of dying early. Unwanted pregnancy among teens was reported to be 30.1% in Gondar, Ethiopia. Unwanted pregnancy among teens was reported to be 30.1% in Gondar, Ethiopia (14–16).
Young people in Ethiopia face complex and interconnected reproductive health issues, which are worsened by societal, economic, environmental, and cultural behaviors. The nature of the issues necessitates a multi-sectorial and integrated approach to teenage reproductive health. Apart from reproductive health, Ethiopian teenagers face a variety of issues, including poverty and traditional and cultural beliefs. Their material, social, and reproductive needs have not received the attention they deserve as a group (6, 17).
People commonly motivated their sexual interactions with youths by offers of monetary gain, gifts, career positions, or promises to send money abroad. This is most common among considerably elderly males, and there are no cultural consequences for it. According to their description, these males simultaneously satisfy the girl's economic demand while also gaining the advantage of being young and seemingly disease-free sex clients (18).
Several factors can affect the health of the adolescent population, including age, cultural views on early marriage, cultural restrictions on contraception use, a lack of understanding about the risks of unprotected sexual activities, and insufficient life skills needed to practice safer sexual behaviors. In many low- and middle-income countries, youth reproductive health problems are largely confounded by limited access to reproductive health treatments, inadequate service provision, and a lack of awareness among unmarried young people (19).
The majority of emerging countries began with national youth strategies. Preventive programs and strategic plans for young generations' sexual and reproductive health problems or issues are few and far between in most developing countries, but national youth policies, programs, and strategies that specifically address and meet young people's sexual and reproductive health needs are common (9).
To address youth reproductive health issues, the Ethiopian Ministry of Health has devised adolescent and youth health strategies. Despite efforts made to increase access to adolescent reproductive health care, utilization remains low, and the youth population is disproportionately affected by reproductive health issues. Researchers conducted various studies on the use of youth reproductive health services and associated factors in Ethiopia. However, there is a paucity of data on youth reproductive health issues, service preferences, and other related aspects. In this context, a study was conducted to assess reproductive health problems, service preferences, and related factors among teenagers in Dilla town, southern Ethiopia.
Methods and materials
Study design and setting
A community-based cross-sectional study was conducted from January to March 2024 in Dilla town, which is located in southern Ethiopia at a distance of 359 km from the capital city of Addis Ababa at an altitude of 1,500–3,000 m above sea level. Its climatic condition is “Woynadega”. Of Dilla Town's approximately 94,148 residents, 34,452 are thought to be young people between the ages of 15 and 24. There are nine kebeles and three sub-cities in the town. Dilla has 1 referral hospital, 2 health centers, 15 private clinics, 18 drugstores, and 4 pharmacies (Figure 1).
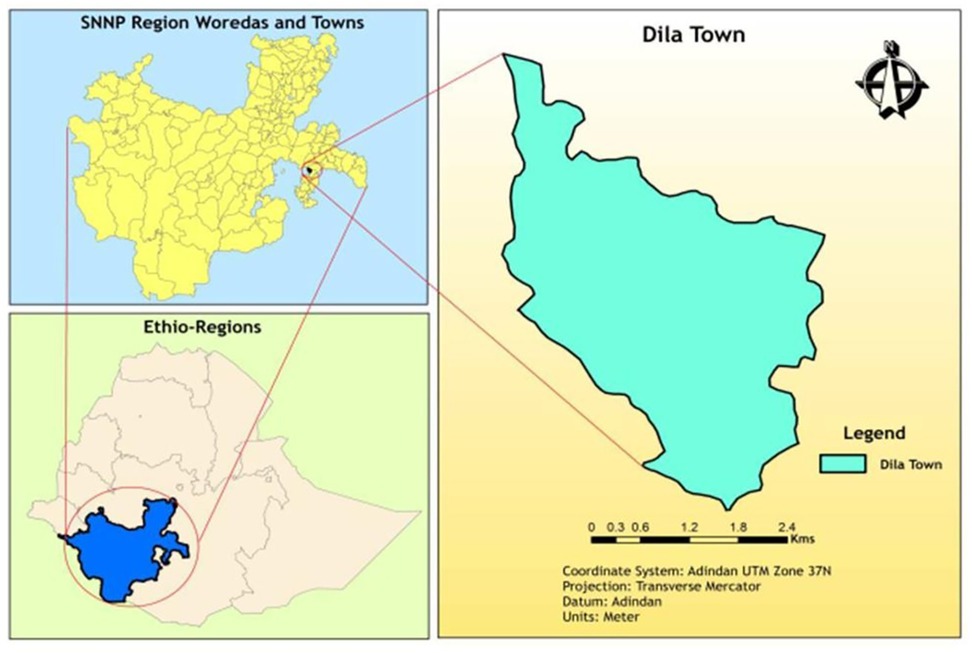
Figure 1. Map of Dilla town, Ethiopia (20).
Source and study population
The source population consisted of all youths living in Dilla town, while the study population consisted of youths from selected kebeles during the data collection period. Youths who were unable to communicate at the time of the study were excluded.
Sample size determination and sampling procedure
The sample size was determined using a single population proportion formula with the following assumption: a significance level of 95%, a 4% margin of error, and a magnitude of youth reproductive health problems of 28.3% from the study in Lay Gayint district, Amhara region (20), and a 10% non-response rate.
where:
n = required sample size, Z α/2 = confidence level (1.96)
p = population proportion (0.283), q = 1-p (0.717)
d =margin of error (0.04)
n = (1.96)2 × (0.283) × (0.717) (0.04)2
n = 3.842 × 0.203/0.0016
n = 0.779/0.0016
n = 488 + 10% non-response rate
n = 536
Thus, according to the above assumptions and the given formula, the total calculated sample size was 536. Using the lottery method, one sub-city and 4 kebeles were selected from Dilla town. The survey was done to identify households having youths in each selected kebele. The calculated sample size was proportionally allocated to the selected kebele, and then the required samples were taken by using a systematic random sampling technique.
Variables and measurements
Youth reproductive health problem was the dependent variable. A participant is considered to have a reproductive health problem if he/she experiences at least one of the major reproductive health problems (unplanned pregnancy, abortion, early sexual initiation, and symptoms of sexually transmitted infections). The independent variables were sex, age, marital status, religion, educational status, occupational status, family condition, parent's job status, family monthly income, pocket money, being ashamed to discuss sexual issues, having multiple sexual partners, using condoms during sexual intercourse, peer influence, convenience of health facilities, utilization of youth reproductive health services, premarital sexual intercourse, contraceptive use, and substance use-related variables (khat chewing, cigarette smoking, shisha smoking, and drinking alcohol) (20–22).
Substance use was measured by asking whether youths were taking any of the three commonly used psychoactive substances: alcohol, cigarettes, and khat in the past 30 days (23).
Early sexual initiation was considered if the participants experienced sexual initiation before 18 years of age (20).
Data collection instruments and quality control
The interviewer-administered questionnaire was developed from previous literature and was prepared in English, then translated to Amharic, and finally back to English to maintain its consistency. The questionnaire was composed of a consent form and questions in three major categories.
Before conducting the actual study, the questionnaire was pretested on 5% (27) of the sample size among youths in Wonago town. After taking necessary corrections and amendments, training was given for six data collectors with a diploma background in health science for 2 days. During the data collection, regular monitoring and supervision were done to verify the consistency, quality, clarity, and completeness of the data. Appropriate coding and data cleaning were carried out to ensure data quality.
Data management and analysis
Data was checked for completeness, coded, and entered into EPI INFO version 7, and then exported to SPSS version 22 for analysis. Descriptive statistics were done, and the results were presented with tables based on the nature of the variables.
Bivariable and multivariable logistic regression was done. The candidate variables with a p-value <0.2 in bivariable logistic regression were moved to multivariable logistic regression to identify their significance with dependent variables, and those variables that affected youth reproductive health were identified by considering a p-value <0.05 with a 95% CI. The Hosmer-Lemeshow goodness-of-fit test was done to assess the adequacy of the logistic regression model, which indicates that the model provides a good fit to the data, as a p-value >0.05 suggests no significant difference between observed and predicted values.
Results
Socio-demographic characteristics of the participants
A total of 493 youths participated in this study, with a response rate of 92%. Among them, 271 (55%) were under the age group of 21–25 years old, 225 (45.6%) were females, and 214 (43.4%) were protestants. Almost all 484 (98.2%) of the participants started school, and 243 (49.3%) had college and above educational status. Just 40 (8.1%) of the participants had a job, and 432 (87.6%) of the participants were single. For everyday expenses, 323 participants, or 65.5%, received pocket money, and 422 participants, or 85.6%, derived their income from their parents. 326 (66.1%) of the participant's family live together, and 224 (45.4%) of the participant's family both work outside the home (Table 1).
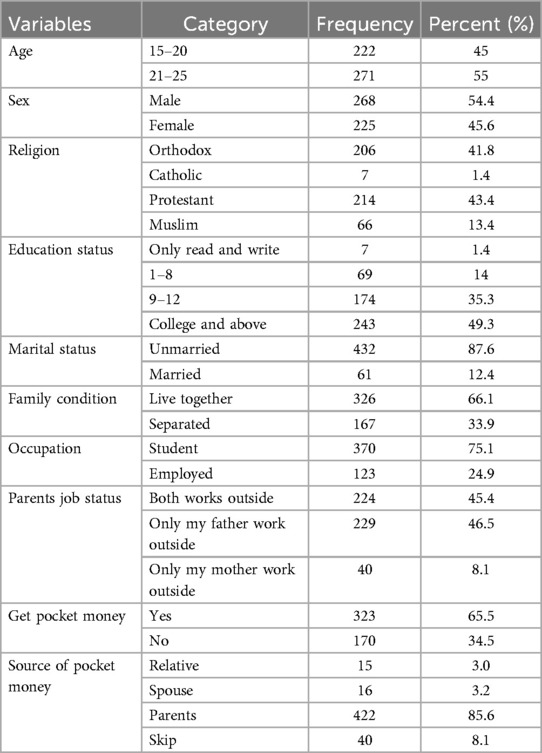
Table 1. Socio-demographic characteristics of youths in the study of reproductive health problem among youths and associated factors in Dilla town, southern Ethiopia.
Reproductive health-related characteristics of respondents
Among participants, 287 (58.2%) said that they were ashamed to discuss sexual issues, and a few respondents, 158 (32%), had multiple sexual partners. More than half of respondents, 308 (62.5%), didn't use condoms during their recent sexual intercourse, and 213 (43.2%) of respondents reported that there was peer influence on sexually related issues. Nearly half of respondents (217, 44%) reported that health facilities were convenient for youths. Only a few youths, 43 (8.7%), use youth reproductive health services; 41 (8.3%) had premarital sexual intercourse; and 120 (24.3%) use modern contraceptive methods (Table 2).
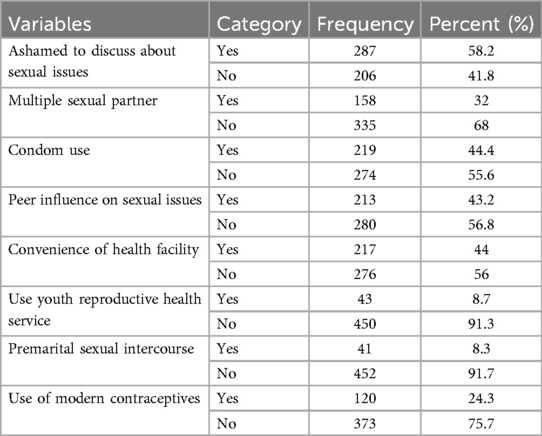
Table 2. Reproductive health characteristics of youths in the study of reproductive health problem among youths and associated factors in Dilla town, southern Ethiopia.
Substance use-related characteristics of respondents
Most of the respondents (92.1%, 87.4%, 100%, and 72.6%) reported that they had no history of chewing khat, smoking cigarettes, smoking shisha, or drinking alcohol, respectively (Table 3).
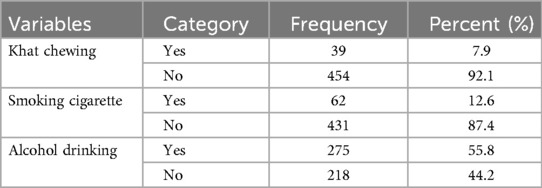
Table 3. Substance use related characteristics of youths in the study of reproductive health problem among youths and associated factors in Dilla town, southern Ethiopia.
Preference for youth's reproductive health services
According to a survey on youth preference for reproductive health care, 238 (48.3%) of respondents said they would rather see a private health provider, and 443 (89.9%) said they did not use the current health facilities for their reproductive health requirements. More than half of the respondents (296, or 60%) wanted the service to take place during regular working hours at the health facility, 262 (53.1%) wanted a discounted rate, 394 (79.9%) wanted the service provider to be young and of the same sex, and 274 (55.6%) wanted the service to be in the town center.
According to the assessment, 374 (75.9%), 337 (68.4%), 331 (67.1%), 491 (99.6%), and 475 (96.3%) of the total respondents said they would prefer to participate in youth health information centers, receive sexual education, receive family planning services, receive partner relationship counseling, and receive information and education on HIV/AIDS and STDs, respectively (Table 4).

Table 4. Preference of youth's reproductive health service in the study of reproductive health problem among youths and associated factors in Dilla town, southern Ethiopia.
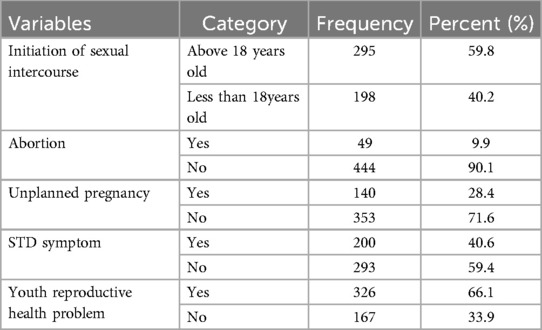
Youth reproductive health problem
In Dilla town, the prevalence of youth reproductive health problems is 66.1% (95% CI: 62.5–70.4). In terms of beginning sexual activity, 275 people (55.7%) did so during the data collection period, and 198 people (40.2%) did so prior to turning 18 years old. Of the respondents, only 140 (28.4%) experienced an unintended pregnancy, and 49 (9.9%) had an abortion. STI symptoms were present in nearly half of the 200 respondents (40.6%) (Table 5).
Factors related to youth reproductive health problems
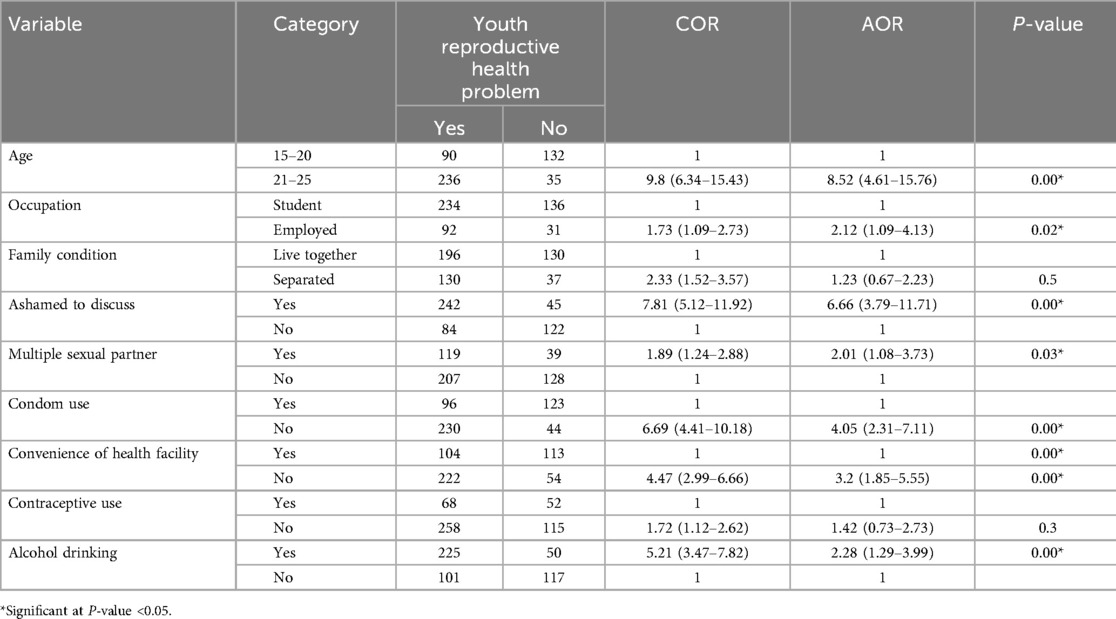
In a bivariable analysis, the following factors were associated with youth reproductive health problems at a P-value <0.2: age, family status, occupation, multiple sexual partners, condom use, health facility convenience, being ashamed to discuss sexual issues, alcohol drinking, and the use of contraceptives.
Multivariable analysis revealed that youth reproductive health problems were significantly associated with age, occupation, condom use, having multiple sexual partners, being ashamed to discuss sexual issues, alcohol drinking, and health facility convenience (P-value <0.05). Model fitness was checked by the Hosmer and Lemeshow goodness of fit test, which was a p-value of 0.18, indicating that the model provides a good fit to the dataset.
Youths aged 21–25 years had 8.52 (AOR: 8.52; 95% CI: 4.61–15.76) times higher chances of experiencing problems related to reproductive health than youths aged 15–20 years. Additionally, youths who were employed were 2.12 (AOR: 2.12; 95% CI: 1.09–4.13) times more likely to have reproductive health problems compared to students.
Moreover, youths who were ashamed to discuss sexual issues were 6.66 (AOR: 6.66; 95% CI: 3.79–11.71) times more likely to have reproductive health problems compared to their counterparts.
Youths who had multiple sexual partners were 2.01 (AOR: 2.01; 95% CI: 1.08–3.73) times more likely to have reproductive health-related problems. Besides, the odds of having reproductive health problems among youths who didn't use condoms during sexual intercourse were 4.05 (AOR: 4.05; 95% CI: 2.31–7.11) times more likely to have reproductive health problems compared to those who were not using them.
Youths who believed health facilities were inconvenient were 3.2 (AOR: 3.2; 95% CI: 1.85–5.55) times more likely to have reproductive health problems compared to their counterparts. On the other hand, youths who drink alcohol were 2.28 (AOR: 2.28; 95% CI: 1.29–3.99) times more likely to have reproductive health problems compared to youths who don't drink alcohol (Table 6).
Discussion
According to this study, 66.1% of young people in Dilla town had reproductive health problems. Factors that were found to be significantly associated with youth reproductive health problems included age, occupation, being ashamed to discuss sexual issues, having multiple sexual partners, condom use, and health facility convenience.
Based on this study, youth reproductive health problems are higher compared to the study done on female high school students in a Lay Gayint district (28.3%) (20). This discrepancy might be due to male youths included in this study, who are greater in number compared to females. Even though reproductive health issues often focus on females, males are also vulnerable to higher-risk sexual behaviors. Some STIs are asymptomatic in males and easily overlooked, which leads to long-term complications and an increased transmission rate.
This study found that 40.6% of participants experienced STI symptoms, 28.4% experienced an unintended pregnancy, and 9.9% experienced an abortion. These rates are greater than those found in a study conducted among students at Ambo University in Central Ethiopia (22.8%, 5%, and 22.5%, respectively) (24). The disparity may result from variations in the study populations. Other study participants, besides students, could not have had access to health education, which caused them to make irresponsible sexual decisions and raised their risk of reproductive sexual problems.
This study found that youth reproductive health service use was only 8.7%, which is low compared to the studies done in Bahir Dar city (32%) (1), Dejen district (45%) (25), and Lay Gayint district (35.6%) (20). The possible explanation for the discrepancy might be due to the difference in economic and educational status among the study participants. Youth from low-income families and lower levels of education face barriers to accessing reproductive healthcare services and are less informed about sexual and reproductive health. Health service utilization plays a great role in improving and maintaining reproductive health. Regular access to and use of reproductive health services can prevent, diagnose, and treat various reproductive health issues.
Youths in the age group of 21–25 years old were 8.52 (AOR: 8.52; 95% CI: 4.61–15.76) times more likely to develop reproductive health problems. And this finding is in line with the study in the Lay Gayint district (20). Since this age group is a period of independence, less parental supervision and guidance may lead youths to be more vulnerable to reproductive health issues and risky sexual behaviors. Peer pressure and a desire to explore their sexuality may exacerbate this risk-taking.
Based on the findings, youths who are employed were 2.12 (AOR: 2.12; 95% CI: 1.09–4.13) times more likely to have reproductive health problems than students. This might be due to employed youths having an income, which may lead to lifestyle changes, including increased alcohol consumption, smoking, or unprotected sexual activity, which contribute to reproductive health issues.
Youths who were ashamed to discuss sexual issues were 6.66 (AOR: 6.66; 95% CI: 3.79–11.71) times more likely to have reproductive health problems than their counterparts, which is in line with the study in Lay Gayint (20). Youths who are not encouraged to talk about sexual concerns may not know enough about safe sexual practices and may be afraid to seek therapy, which could make their problems worse.
Youths who had multiple sexual partners were 2.01 (AOR: 2.01; 95% CI: 1.08–3.73) times more likely to have reproductive health problems than those who didn't have multiple sexual partners. This finding is in line with the study done in Lay Gayint (20). Having multiple sexual partners increases the rate of STI transmission and exposure to other reproductive health problems.
The odds of having reproductive health problems were 4.05 (AOR: 4.05; 95% CI: 2.31–7.11) times higher for youth who did not use condoms during sexual activity. Condoms are highly effective in reducing the transmission of different sexually transmitted diseases and unwanted pregnancies. An urgent report from the WHO regional office for Europe reveals that condom use among youths has declined significantly since 2014. This is putting young people at risk of various reproductive health problems (26).
Youths who perceived that health facilities were not convenient were 3.2 (AOR: 3.2; 95% CI: 1.85–5.55) more likely to have reproductive health problems than those who thought health facilities were convenient, which is in line with the study in Lay Gayint (20). If a health facility is difficult for people to get to and they are not interested in the services it offers, they might not want to visit.
Youths who drink alcohol were 2.28 (AOR: 2.28; 95% CI: 1.29–3.99) times more likely to have reproductive health problems compared to youths who don't drink alcohol. Alcohol consumption increases engagement in risky sexual behaviors, which has an impact on their reproductive health.
Limitation of the study
The chicken-egg paradox is typical in cross-sectional studies, so it would be better if a qualitative study from the perspectives of other stakeholders was included. Since the study's findings are based on young people's self-reported data, social desirability bias may have an impact. Furthermore, this study is restricted to the study region and cannot be extrapolated to the entire southern country.
Conclusion and recommendation
This study revealed that the magnitude of youth reproductive health problems was 66.1%, and age, occupation, shame of discussing sexual issues, multiple sexual partners, condom use, and health facility convenience were found to be significantly associated with youth reproductive health problems.
Government, national, and local health departments should develop policies and implement programs focused on youth reproductive health.
Healthcare facilities should provide comprehensive, age-appropriate, and accurate sexual education as part of specialized reproductive health services for youth that prioritize privacy and nonjudgmental treatment. In addition, screening and early detection of RH problems and engaging in community outreach programs are some of the recommended activities.
Educational institutions have to play a role in promoting healthy behavior by teaching students about responsible decision-making, promoting safe sexual practice, delaying sexual activity, and avoiding risky behaviors that lead to reproductive health problems. Additionally, support students who are at risk of early pregnancy, abuse, or other challenges.
By helping young people at home where social and cultural standards are upheld while fostering health, parents and community leaders can influence views in the community and play a significant part in breaking down cultural barriers. Programs for peer education, advocacy, and resources about youth reproductive health must be offered by NGOs and neighborhood organizations.
Researchers and academics should contribute to understanding youth reproductive health issues through studies and evaluations. Collaborative efforts among these stakeholders are essential to effectively address the reproductive health needs of youths. Further investigation with a large representative sample by incorporating other stakeholders is recommended.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional review board, college of medicine and health sciences, Dilla University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. GZ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. AG: Formal analysis, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The authors received a specific amount of money from Dilla University for data collection purpose in this work.
Acknowledgments
The authors would like to thank all respondents for their willingness to participate in the study. We also appreciate the technical assistance provided by the Dilla University School of Public Health staff, the Kebele office, and the Dilla municipal administration office.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AIDS, acquired immunodeficiency syndrome; AOR, adjusted odd ratio; CI, confidence interval; COR, crude odd ratio; HI, health institution; HIV, human immune-deficiency virus; NGO, non-governmental organization; OR, odds ratio; RH, reproductive health; SPSS, statistical package for social science; STD, sexually transmitted disease; STI, sexually transmitted infection; VCT, voluntary counseling and testing; SRH, sexual and reproductive health; SNNPR, southern nation, nationalities and people region; WHO, World Health Organization.
References
1. Abebe M, Awoke W. Utilization of youth reproductive health services and associated factors among high school students in Bahir Dar, Amhara regional state, Ethiopia. Open J Epidemiol. (2014) 4:70. doi: 10.4236/ojepi.2014.42012
2. Jaleta A, Assefa A, Amentie M. Youth friendly reproductive health service utilization and associated factors among youths in Metekel Zone, North West Ethiopia. Int J Ophthalmol & Vis Sci. (2017) 2(2):59–64. doi: 10.11648/j.ijovs.20170202.14
3. Abawi K, Chandra-Mouli V, Toskin I, Festin MP, Gertiser L, Idris R, et al. E-learning for research capacity strengthening in sexual and reproductive health: the experience of the Geneva foundation for medical education and research and the department of reproductive health and research, world health organization. Hum Resour Health. (2016) 14(1):1–7. doi: 10.1186/s12960-016-0173-0
4. Muntean N, Kereta W, Mitchell KR. Addressing the sexual and reproductive health needs of young people in Ethiopia: an analysis of the current situation. Afr J Reprod Health. (2015) 19(3):87–99. https://hdl.handle.net/10520/EJC17925326897917
5. Berhane F. Health problems and service preferences of school adolescents in Addis Ababa with emphasis on reproductive health (Dissertation). Addis Ababa University (2000).
6. Govindasamy P, Kidanu A, Bantayerga H. Youth Reproductive Health in Ethiopia. Calverton, Maryland: OCR Macro (2002).
7. Bureau PR. The World’s Youth: 2013 Data Sheet. Calverton, MD, Washington, DC, USA: Plan, Ministère de la Santé and ORC Macro (2013).
8. Kilbourne-Broo M, McKay P. Adolescent reproductive health: making a difference. In: 2010 Inter-agency Working Group on Reproductive Health in Crises. Vol. 16. Seattle, Washington: PATH (Program for Appropriate Technology in Health) (1998). p. 1–8.
10. Kassa F. The rates and effects of urban sprawl in developing countries: the case of Addis Ababa, Ethiopia. Intern J Area Stud. (2014) 9(2):135–51. doi: 10.2478/ijas-2014-0009
11. Organization WH. Adolescent Friendly Health Services: An Agenda for Change. (WHO/FCH/CAH/02.14). Geneva: World Health Organization (2003).
12. Williams G, Milligan A, Odemwingie T. A Common Cause: Young People, Sexuality and HIV/AIDS in Three African Countries. London: ActionAid (1997).
13. Organization WH. Young People and HIV/AIDS: Opportunity in Crisis. London: The Stationery Office (2002).
14. Fantahun M, Chala F, Loha M. Knowledge, attitude and practice of family planning among senior high school students in north Gonder. Ethiop Med J. (1995) 33(1):21–9.7895743
15. Bearinger LH, Sieving RE, Ferguson J, Sharma V. Global perspectives on the sexual and reproductive health of adolescents: patterns, prevention, and potential. Lancet. (2007) 369(9568):1220–31. doi: 10.1016/S0140-6736(07)60367-5
16. Godwin J, Szabo G, Sass J, Sauvarin J. Righting the mismatch between law, policy and the sexual and reproductive health needs of young people in the Asia-Pacific region. Reprod Health Matters. (2014) 22(44):137–47. doi: 10.1016/S0968-8080(14)44808-0
17. Bulto GA, Demissie DB, Tulu AS. Respectful maternity care during labor and childbirth and associated factors among women who gave birth at health institutions in the west Shewa zone, Oromia region, central Ethiopia. BMC Pregnancy Childbirth. (2020) 20:1–12. doi: 10.1186/s12884-020-03135-z
18. Korra A, Haile M. Sexual behavior and level of awareness on reproductive health among youths: evidence from Harar, eastern Ethiopia. Ethiop J Health Dev. (1999) 13(2):107–13.
19. Vallès X, Lunzayiladio Lusala P, Devalière H, Metsia-Thiam MM, Aguilar D, Anne-Cheyron AL, et al. Network analysis of knowledge and practices regarding sexual and reproductive health: a study among adolescent street girls in Kinshasa (DRC). Eur J Contracept Reprod Health Care. (2017) 22(1):62–9.
20. Mekie M, Taklual W, Tesfaw A. Youth reproductive health problems, service preference and associated factors among female secondary school students in lay Gayint district of Amhara region, Ethiopia, 2019. Open Public Health J. (2020) 13(1):645. doi: 10.2174/1874944502013010643
21. Fetene N, Mekonnen W. The prevalence of risky sexual behaviors among youth center reproductive health clinics users and non-users in Addis Ababa, Ethiopia: a comparative cross-sectional study. PLoS One. (2018) 13(6):e0198657. doi: 10.1371/journal.pone.0198657
22. Binu W, Marama T, Gerbaba M, Sinaga M. Sexual and reproductive health services utilization and associated factors among secondary school students in Nekemte town, Ethiopia. Reprod Health. (2018) 15:1–10. doi: 10.1186/s12978-018-0501-z
23. Birhanu AM, Bisetegn TA, Woldeyohannes SM. High prevalence of substance use and associated factors among high school adolescents in Woreta town, northwest Ethiopia: multi-domain factor analysis. BMC Public Health. (2014) 14:1–11. http://www.biomedcentral.com/1471-2458/14/118624383435
24. Yared A, Sahile Z, Mekuria M. Sexual and reproductive health experience, knowledge and problems among university students in Ambo, central Ethiopia. BMC Reproductive Health. (2017) 14:1–7. doi: 10.1186/s12978-017-0302-9
25. Dagnew T, Tessema F, Hiko D. Health service utilization and reported satisfaction among adolescents in Dejen district, Ethiopia: a cross-sectional study. Ethiop J Health Sci. (2015) 25(1):17–28. doi: 10.4314/ejhs.v25i1.4
Keywords: reproductive health, southern Ethiopia, problem, youth, factors
Citation: Sertsewold SG, Zenebe GA and Gebrekidan AY (2025) Reproductive health problem among youths and associated factors in Dilla town, southern Ethiopia. Front. Reprod. Health 7:1519024. doi: 10.3389/frph.2025.1519024
Received: 29 October 2024; Accepted: 31 March 2025;
Published: 28 April 2025.
Edited by:
Sultan Hussen Hebo, Arba Minch University, EthiopiaReviewed by:
Aldemir Branco de Oliveira Filho, Federal University of Pará, BrazilAtta Ur Rehman, Shaheed Zulfiqar Ali Bhutto Medical University (SZABMU), Pakistan
Copyright: © 2025 Sertsewold, Zenebe and Gebrekidan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seblewongel Gebretsadik Sertsewold, c2VibGV3b25nZWxuZWduQGdtYWlsLmNvbQ==
 Seblewongel Gebretsadik Sertsewold
Seblewongel Gebretsadik Sertsewold Getachew Assefa Zenebe
Getachew Assefa Zenebe Amanuel Yosef Gebrekidan
Amanuel Yosef Gebrekidan