- 1School of Nursing, Duke University, Durham, NC, United States
- 2Duke Global Health Institute, Duke University, Durham, NC, United States
- 3Department of Biostatistics and Bioinformatics, School of Medicine, Duke University, Durham, NC, United States
- 4Department of Psychiatry and Mental Health, University of Cape Town, Cape Town, South Africa
- 5Neuroscience Institute, University of Cape Town, Cape Town, South Africa
- 6Department of Statistics, NC State University, Raleigh, NC, United States
- 7Department of Paediatrics and Child Health, University of Cape Town, Cape Town, South Africa
- 8Unit on Child & Adolescent Health, SA Medical Research Council, Cape Town, South Africa
- 9Unit on Risk & Resilience in Mental Disorders, SA Medical Research Council, Cape Town, South Africa
Background: Little is known about HIV status disclosure within the social networks of adolescents with perinatally-acquired HIV (APHIV) in sub-Saharan Africa, where HIV prevalence is high and stigma surrounding HIV is pervasive. This study employed egocentric network analysis to characterize HIV disclosure in the social networks of APHIV in Cape Town South Africa. Associations between HIV disclosure and characteristics of APHIV (egos), their relationship to network members (alters), and features of the social network, including ego's network size and alter's centrality within the network, were also examined.
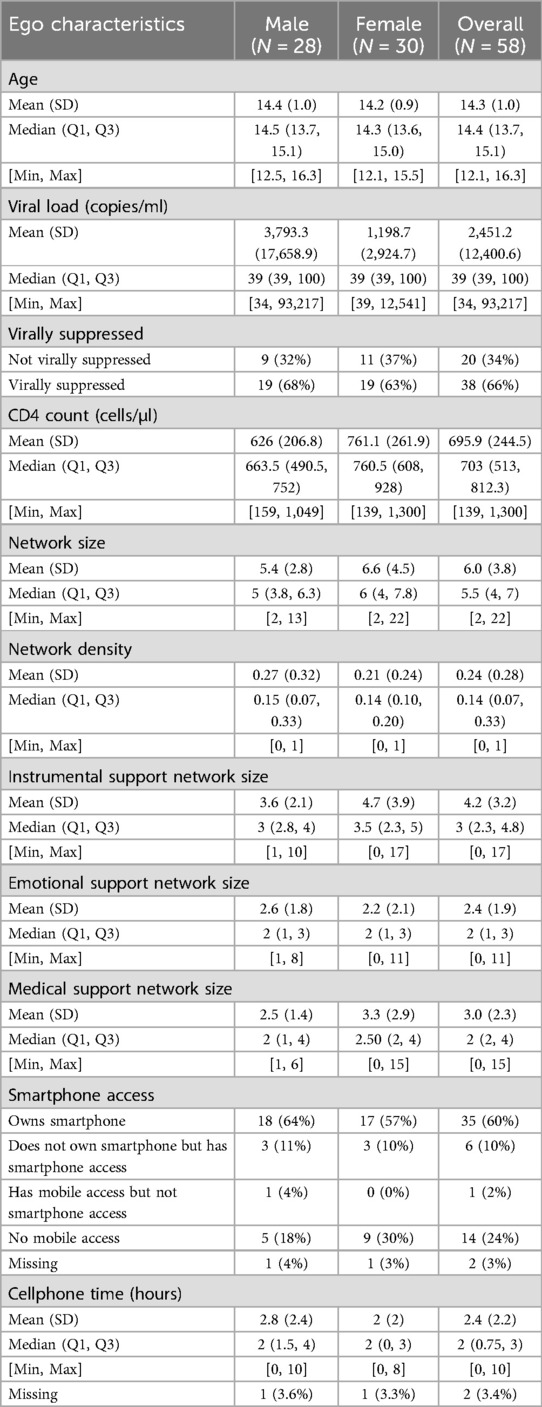
Methods: Network data were collected from 58 APHIV (mean age 14.3 years; 52% female) using a customized touchscreen-based assessment, providing data on 349 ego-alter relationships. Associations with HIV disclosure within the ego-alter pairs were evaluated by adjusted odds ratios (AOR) from multivariable logistic regression with generalized estimating equations, clustering by ego.
Results: Among all ego-alter pairs identified, 36.4% (127/349) were disclosed to by egos. Odds of disclosure did not differ based on the ego's gender or viral suppression. Odds of disclosure were significantly higher when alters were presumed by the ego to have HIV [AOR 6.26; 95% confidence interval (CI): 2.36–16.58, p < 0.001], were more trusted by the ego (AOR 2.84; 95% CI: 1.14–7.06, p = 0.03), or were older than the ego (1-year difference AOR 1.04; 95% CI: 1.02–1.07, p < 0.001). Increasing alter's centrality by 0.01 was associated with an increased odds of disclosure (AOR 1.02; 95% CI: 1.002–1.03, p = 0.03), though overall network size was not associated with increased odds of disclosure. The effect of the ego's emotional support network size on disclosure, however, depended on the type of ego-alter relationship.
Conclusions: HIV status disclosure was low in the social networks of APHIV. Our study found that disclosure was not influenced by network size, gender, or viral suppression but rather by factors related to interpersonal trust and shared experience, such as perceived HIV status of alters, network-level centrality and emotional support network size. The study further highlights the benefits and future potential of using social network data collection and analysis methods to better understand HIV disclosure among adolescents.
1 Introduction
Adolescents with perinatally-acquired HIV (APHIV) face unique challenges in sub-Saharan Africa, where HIV prevalence is high, and stigma surrounding HIV remains pervasive (1, 2). In 2020, approximately 1.8 million adolescents were living with HIV, representing 5% of all people living with HIV (3). Importantly, adolescents living with HIV are the only age group that has not seen significant declines in AIDS-related deaths (4) and adolescents repeatedly demonstrate lower levels of retention in HIV care and adherence to ART compared to older adults (5). These outcomes are thought to be due to numerous challenges experienced by adolescents, including HIV-related stigma, limited youth-friendly healthcare services, and the complexities of navigating a lifelong, stigmatizing chronic illness during a period of significant developmental, psychological, and social changes (6–8).
Disclosure of one's HIV status may open avenues to receiving social support to cope with the challenges unique to living with HIV. Among adults living with HIV in sub-Saharan Africa, disclosure has been linked to improved adherence to antiretroviral therapy (ART) and greater levels of retention in HIV care (9). It has also been shown to be associated with use of maternal health services and services for prevention of mother-to-child transmission of HIV (PMTCT) (10). Disclosure can also play an important role in preventing the onward transmission of HIV by facilitating HIV testing of sexual partners and linking partners to pre-exposure prophylaxis (PrEP). Less is known about the advantages of disclosure for APHIV (11, 12).
Despite its benefits, disclosure comes with the potential risk of stigma, rejection, isolation, and mental distress. These negative consequences may arise from entrenched societal attitudes and misconceptions surrounding HIV, which perpetuate fear and stigma in sub-Saharan Africa (13). Fear and anticipation of these risks is known to limit disclosure (14), and individuals with HIV must balance these potential risks with potential benefits when deciding to disclose their status to somebody new. For adolescents, who may be newly navigating social relationships and seeking peer acceptance, making disclosure decisions may be particularly challenging. Indeed, disclosure-related anxiety was identified as a key theme in a systematic review focused on stigma-related challenges among children and adolescents with HIV, including multiple studies from sub-Saharan Africa (2).
Notably, APHIV have been shown to have lower rates of disclosure compared to adolescents who acquired HIV more recently (15). Disclosure research among APHIV in sub-Saharan Africa has largely focused on examining correlates of disclosure to the adolescents/children who acquired HIV perinatally (16, 17), rather than examining APHIV's disclosure of their status to others (18). In non-African settings, increased disclosure among APHIV has been associated with older age, increased disclosure intentions, and earlier age of learning one's serostatus (19). Qualitative research with APHIV in South Africa has found that APHIV rarely disclose their status due to lack of trust and their fears of further unwanted disclosure, leaving their relationships feeling disconnected and superficial (20). While such fear of HIV status disclosure and stigma have been generally identified in studies of APHIV (6), little remains known about how APHIV navigate the disclosure process within their social networks.
Social networks, which refer to the informal patterns of relationships between individuals, can offer valuable insights into social dynamics, including disclosure and social support. Research has shown that social networks play a critical role in shaping health behaviors among adolescents (21). Social network analysis, a set of methods that focuses on analyzing the patterns of linkages between individuals (22), has been used to deepen our understanding of disclosure of same-sex behaviors among MSM's social networks (23). Notably, this research could further our understanding of disclosure in among APHIV, since existing research on disclosure has yet to explore how the structural and functional aspects of social networks shape HIV disclosure in this population.
Methodological barriers, such as the time-intensive nature of traditional social network assessments, have hindered the collection of comprehensive network data. Advances in technology have addressed many of these challenges, making it feasible to collect detailed social network data in a less burdensome and more efficient and youth friendly manner. Touchscreen-based tools and graph databases, for example, allow study participants and researchers to map social networks with reduced participant fatigue (24). These innovations enable the exploration and analysis of social support, trust, and engagement within networks, which are particularly relevant for APHIV as they navigate disclosure decisions.
This study leverages such technological advancements to explore disclosure within egocentric networks [i.e., personal networks based on the sets of ties that surround each participant (25)] among APHIV in Cape Town, South Africa. The purpose of our study was to characterize HIV disclosure in the social networks of APHIV and to examine the associations between HIV disclosure and characteristics of APHIV (egos), their relationship to network members (alters), and features of the social network, including ego's network size and alter's centrality within the network.
2 Methods
2.1 Procedures
This study was nested within the neurological sub-study of the Cape Town Adolescent Antiretroviral Cohort (CTAAC), a prospective cohort study of APHIV established on ART and matched HIV negative controls in Cape Town, South Africa (26, 27). Adolescents aged between 9 and 14 years old living with perinatally-acquired HIV were recruited for the CTAAC cohort from public sector health care services from across Cape Town. Participants were recruited, between August 2013 through April 2015 from seven clinics providing routine ART services across Cape Town and followed at six-month intervals for study assessments. The inclusion criteria were having been on ART for at least 6 months, knowing their HIV status, and having the ability to follow-up, selected to recruit a generalizable sample of APHIV on ART in the study area. Exclusion criteria included having an uncontrolled medical condition, an identified central nervous system condition, a history of head injury, or a history of perinatal complications or neurodevelopment disorder not attributed to HIV. Adolescents provided assent to participate and their primary caregiver provided written informed consent. A total of 122 APHIV (aged 9–12 years old at baseline) were enrolled in the neurological HIV sub-study (28), and these participants underwent neuroimaging, neuropsychological and mental health assessment at baseline and 36 months. At the 36-month visits, network measures were assessed among 61 APHIV, aged 12–15 years old, who were sampled consequently once the network sub-study was approved. No participants declined to participate in the network assessment.
To collect egocentric network (i.e., personal network) data, we customized a network data capture instrument based on an existing tool, netCanvas (24). NetCanvas was designed to efficiently enumerate egocentric social networks with less burden placed on participants. The tool utilizes touchscreen technology and is designed to be user-centered, with participants completing the assessment themselves with the aid of a research assistant. Our team customized netCanvas for use with isiXhosa-speaking participants in South Africa. The original netCanvas software has continued development and has now become the open-source project Network Canvas (29).
Our customized tool collected egocentric social network data for each participant through the following phases: name generating, name interpreting, and edge generating. In the name generating phase, participants were asked to provide names or nicknames for members of their social networks. Specifically, participants were asked “Who are the people you are closest to? That is, people you see or talk to on a regular basis and share your personal thoughts and feelings with?” To add an individual, participants were instructed to enter the person's first name (or pseudonym), last name (or pseudonym), nickname (optional; if not entered, the app would display initials of first and last name), age, and role (check all that apply including friend, family/relative, romantic partner, acquaintance, and other). Once the participant was done adding people to their network, they were asked a series of additional name generating prompts, including: “If you wanted to talk to someone about things that are very personal and private, is there anybody else you could talk to?” Other name generating prompts included people not already mentioned that the participant could borrow money from, ask advice about health issues or advice about their treatment, friends met at their clinic, and individuals the participant has had sex with.
In the name interpreting phase, respondents provided additional information about these individuals (e.g., demographics, level of trust, HIV disclosure, social support received). Specific questions asked are descried in the Measures section on Alter-level Network Characteristics below. To provide data on social support, participants were instructed to tap on all the people in their network who had provided various types of instrumental social support, emotional social support, and medical-specific social support. Participants were also asked to identify the network members who, to their knowledge of the ego, were living with HIV. Participants were assisted by research assistants who were fluent in both English and isiXhosa.
In the edge generating phase, participants were asked to connect any two network members who are close to each other or have spent time together in the past six months (Figure 1). Network and participant data were stored on encrypted tablets and uploaded to a secure server. All study procedures, for both the larger CTAAC trial as well as this Social Network study, were approved by the Institutional Review Board at Duke University and the Human Research Ethics Committee of the Faculty of Health Sciences at the University of Cape Town.
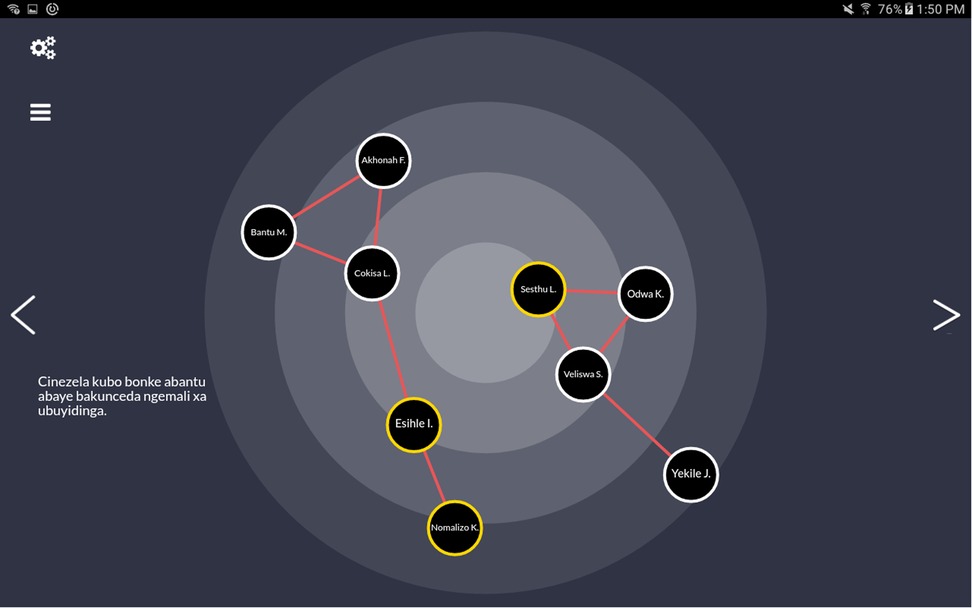
Figure 1. Screenshot of customized tablet-based social network data collection tool depicting a simulated network with 9 alters. HIV disclosure is indicated by yellow highlighting and edges (i.e., social ties between two network members) are denoted as red lines. The data shown are simulated and do not represent real individuals or relationships.
2.2 Measures
2.2.1 Demographic characteristics and clinical measures
As part of the CTAAC study, all participants completed self-reported assessments and provided blood samples at all study visits to obtain clinical data. For this study, demographic measures of interest included participant gender and age at the 36-month assessment. Additionally, HIV-related clinical data collected at the 36-month CTAAC visit included CD4 count and viral suppression (defined as fewer than 50 copies of HIV RNA per milliliter of blood).
2.2.2 Communication characteristics
As part of the customized netCanvas tool, participants were asked about their communication behaviors, including whether they had access to a smartphone and to describe how much time they spent on the phone (in hours) on a typical day.
2.2.3 Ego-level network characteristics
Several ego-level network characteristics were included for each ego. Network size of each ego's network was defined as the number of alters identified by each ego. Network density of each ego was defined as the ratio of the number of edges an ego has over the number of possible edges the ego could have. Edges were defined if there were social connections (very close or spent time together in the past six months) between two alters. Network density ranges from 0 to 1, with lower values suggesting ego's alter network was more sparsely connected (i.e., fewer alters spend time with one another). Emotional support size was defined as the number of alters who were identified as providing emotional support to the ego.
2.2.4 Alter-level characteristics
Participants described the relationship type with each alter (family/relative, friend, romantic partner, acquaintance, other). They also described how frequently they had seen each alter (rarely, weekly, daily), how close they felt to each alter (not very close, somewhat close, very close), how much they trusted each alter (not at all, not very much, somewhat, a lot), and how frequently they communicated with each alter by phone by talking or writing (never, rarely, weekly, daily). Participants also indicated whether each alter provided two types of instrumental support (i.e., they were prompted to “tap on all the people who have given money/given you a place to stay when you needed it”), one type of emotional support (i.e., tap on all the people with whom you have talked to about personal or private matters), and three types of medical support to the ego (i.e., “tap on all the people whom have provided you with information on medical services, helped you get to a medical appointment, or helped you take your medications”). Each type of social support was dichotomized for analysis. HIV disclosure to each alter was assessed with a prompt encouraging the participant to “tap on all the people to whom you have disclosed your HIV status.”
2.2.5 Alter-level network characteristics
The following alter-level network measures were computed for all ego-alter ties. Alter degree was defined as the number of other alters an alter is connected to. Alter harmonic centrality was defined as the mean inverse distance from an alter to other alters. This measure ranges from 0 to 1, with a lower value indicating the alter is more isolated from the other alters.
2.3 Analytic approach
Descriptive statistics were utilized to describe both the characteristics of the egos and the ego-alter pairs. The unit of analysis was an ego-alter pair.
To evaluate the factors associated with disclosure, we formed a base model by considering the following variables: ego viral suppression (yes/no), ego gender, ego's knowledge of whether alter has HIV (yes/no), how much ego trusts alter (not at all, not very much, somewhat, a lot), age difference (alter age minus ego age), and main relationship type between ego and alter (family, friend, other). We first fit the base model with standard logistic regression to check for complete separation and collinearity among variables using the variance inflation factor. Based on the regression diagnostic, we combined the “not at all” and “not very much” response options for trust into one category.
We then considered adding network measures, including alter degree, alter harmonic centrality, emotional support size, medical support size, network density, and network size. This was done by fitting univariable logistic models and by adding each network measure to the base model. Generalized estimating equations (GEE) with robust standard errors and an exchangeable correlation structure for the ego-alter pairs accounting for clustering in egos were adopted in these exploratory models. The GEE framework was chosen over the generalized linear mixed model framework for interpretation reasons since interest was in population estimates of disclosure. For each of the network measures, the odds ratio (OR) from the univariable model and the adjusted odds ratio (AOR) from the multivariable model were estimated with 95% confidence intervals (CIs). The exploratory logistic GEE for emotional support size yielded counterintuitive results for emotional support size, which indicated a negative association of increasing emotional support size with disclosure. This result was counterintuitive because the size of the ego's emotional support network typically has a positive association with disclosure (30). Therefore, potential interactions were explored and an interaction effect of relationship type with emotional support size was identified. Based on the exploratory models, the final logistic GEE model was fit by adding alter harmonic centrality, network size, emotional support size, and interaction between emotional support size and relationship type to the base model.
All statistical analyses were performed in R 4.2.2 (R Core Team, Vienna, Austria). The igraph package was used to calculate the network measures, and the geepack package was used to fit GEE models (31, 32). All hypotheses were evaluated at the 0.05 Type-I level of significance. There was no adjustment for multiple testing as the analysis was exploratory.
3 Results
After excluding egos with missing relationship types, demographic information, or viral suppression status, the study included 58 egos with a total of 349 alters (network members) identified. The characteristics of the egos are presented in Table 1. Out of 58 egos, 52% (30/58) were female. The average age at the time of network measures assessment was 14.3 years [standard deviation (SD) 0.98], and approximately 66% (n = 38) were virally suppressed, with a median viral load of 39 copies/ml (SD 17,658.9 copies/ml). The mean CD4 count was 695.9 cells/μl (SD 244.5 cells/μl). The median network size of each ego was 5.5 individuals [first quartile (Q1) 4 and third quartile (Q3) 7], and network density was relatively low (mean 0.24, SD 0.28). Instrumental, emotional, and medical support network sizes were relatively small, with medians of 3, 2 and 2, respectively. Smartphone ownership or access was reported by 71% (n = 41) of participants; 24% (n = 14) reported no mobile access with the remaining either only having mobile access or missing values. Average cellphone usage time was 2.39 h per day (SD 2.21).
Of 58 egos, 86% (n = 50) had disclosed their HIV status to at least one individual. However, the percentage of alters each ego disclosed to within their network was a median of 33.3%, (Q1 20%, Q3 63%). Table 2 displays alter characteristics, stratified by disclosure. Out of 349 alters, 36.4% (127/349) were disclosed to by an ego. Overall, the majority of alters were family or relatives (66.8%), with friends comprising 23.5%. A higher proportion of disclosed alters were family members (90.6%) compared to not disclosed alters (53.2%), while a lower proportion of disclosed alters were friends (6.3%) compared to not disclosed alters (33.3%). Alters who were disclosed to were also older on average (mean age 37.4, SD 15.7 years) than those who were not disclosed to (mean age 23.4, SD 14.1 years). Disclosed alters were more frequently described as “very close” (76.4%) and trusted “a lot” (75.6%) compared to alters who were not disclosed to (50.9% and 44.1%, respectively). Additionally, disclosed alters were much more likely to provide instrumental (89% vs. 57.7%), emotional (52.8% vs. 32%), and medical support (75.6% vs. 33.8%) than alters who were not disclosed to.
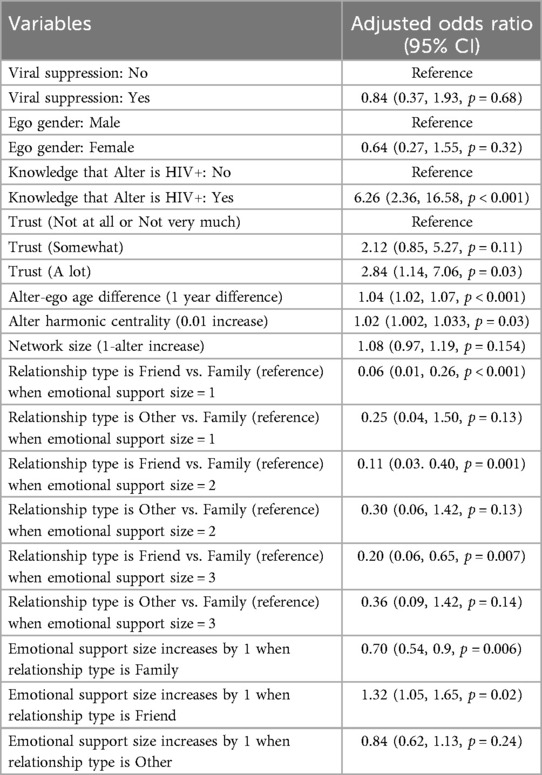
The results from the univariable and multivariable GEE logistic models examining the relationships between network measures and disclosure are summarized in Table 3. Univariable analyses suggested significant positive associations of alter harmonic centrality (OR 1.03, 95% CI: 1.01–1.04, p < 0.001) and network density (OR 1.03, 95% CI: 1.01–1.05, p < 0.001) with disclosure. These associations remained significant in the multivariable models, though the effects were slightly attenuated. After controlling for base variables, a 0.01 increase in alter harmonic centrality was associated with a 2% increase in the odds of disclosure (AOR 1.02, 95% CI: 1.002–1.03, p = 0.02), while a 0.01 increase in network density is associated with a 2% increase in the odds of disclosure (AOR 1.02, 95% CI: 1–1.039, p = 0.045). Emotional support network size was not associated with disclosure in the univariable model (OR 0.89, 95% CI: 0.76–1.04, p = 0.13), but it was significantly associated in the multivariable model; in the multivariable model, each additional alter who provided emotional support was associated with a 26% decrease in the odds of disclosure (AOR 0.74, 95% CI: 0.57–0.96, p = 0.02). This means that on average for two groups who are alike for all variables except for emotional support size, the group with a smaller emotional support size has a higher odds of being disclosed to than a group with a larger emotional support size. Other network measures, including alter degree, medical support size, and network size, did not show significant associations in either univariable or multivariable models.
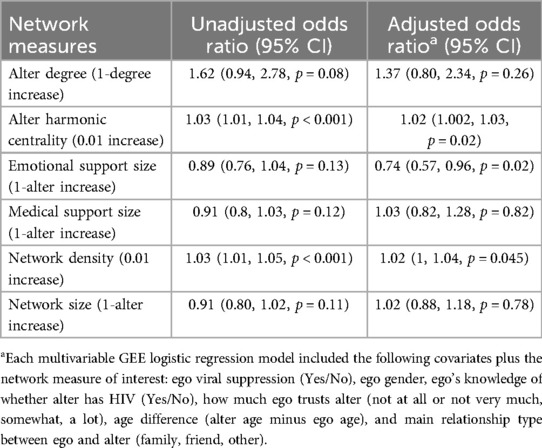
Table 3. Univariable and multivariable GEE logistic regression results for each network measure of interest.
After observing a negative association of emotional support size with disclosure, an interaction of emotional support size with relationship type was included. The results of the final GEE logistic model are summarized in Table 4, which suggest that the odds of disclosure did not differ based on the ego's gender or viral suppression. The odds of disclosure was significantly greater when alters were presumed by the ego to have HIV (AOR 6.26, 95% CI: 2.36–16.58, p < 0.001), trusted a lot by the ego (AOR 2.84, 95% CI: 1.14–7.06 p = 0.03), or older than the ego (1-year difference AOR 1.04, 95% CI: 1.02–1.07, p < 0.001). Increasing alter's centrality by 0.01 was associated with an increased odds of disclosure (AOR 1.02; 95% CI: 1.001–1.03, p = 0.03), though overall network size was not associated with disclosure. The effect of the ego's emotional support network size on disclosure, however, depended on the type of ego-alter relationship. If the alters were family members, the odds of disclosure decreased by 30% as the emotional support size increased by 1 (AOR 0.70, 95% CI: 0.54–0.9, p = 0.006). If the alters were friends, the odds of disclosure increased by 32% as the emotional support size increased by 1 (AOR 1.32, 95% CI: 1.05–1.65, p = 0.016). The emotional support size was not associated with disclosure when the alters were other relationships. Estimated probabilities of disclosure by emotional support size and relationship from the final GEE logistic regression model are visualized in Figure 2.
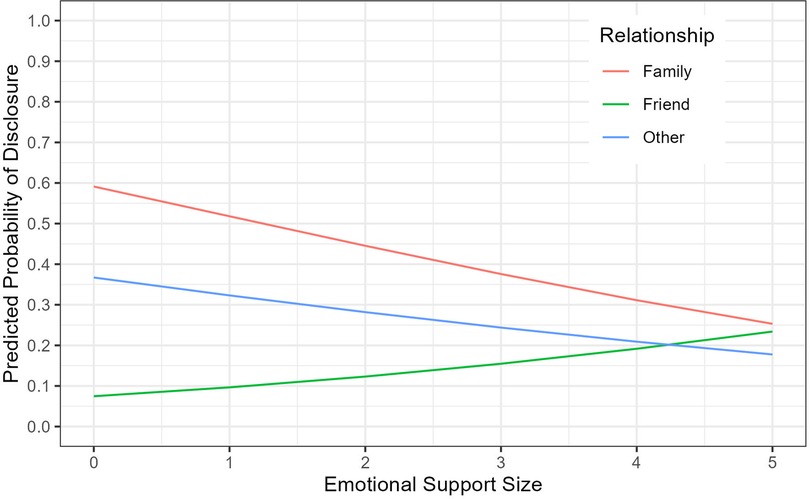
Figure 2. Estimated probabilities of disclosure by emotional support size and relationship from the final GEE logistic regression model.
4 Discussion
The majority (86%) of the adolescents in our study had disclosed their HIV status to at least one person, which is higher than prior studies, which have reported rates of disclosure among adolescents to at least one person from 33% to 66% (11, 15, 33, 34). One study (11) noted that their participants may have interpreted questions on family disclosure to refer to extended family members and not immediate family members. Our approach to first enumerating all current network members, including immediate family members such as biological parents and caregivers, and then asking about disclosure to each individual named was unlikely to have had this issue, potentially explaining the higher levels of disclosure to at least one network member in our study.
HIV disclosure across all social ties within APHIV's social networks was only 36.4%. This relatively low level of disclosure is consistent with previous research that has highlighted the challenges young people face with disclosure (12, 35). For example, a recent systematic review grounded in the Disclosure Process Model (36), which aims to understand why and when people disclose their status, found that anticipated fear and stigma were the most common reason reported for failure to disclose (37). Given the limited levels of disclosure within networks, interventions promoting safe and effective disclosure in this setting may benefit from interventions that support internalized HIV stigma reduction and stigma resistance as well as broader community-level stigma reduction, both of which have been recommended by other disclosure researchers.
Adolescents were more likely to disclose to individuals they trust, perceive as having HIV, or who are older and more central in their social networks. These findings are consistent with previous egocentric network analysis with African American people living with HIV, who were more likely to have disclosed to others who were highly trusted, had a higher level of centrality, and who were also living with HIV (38). Given the sensitive nature of HIV disclosure, it is reasonable that adolescents may feel more comfortable disclosing to individuals they trust. However, due to the cross-sectional design of this study, it is also possible that trust was strengthened following disclosure or that disclosure influenced subsequent perceptions of a network member's trustworthiness. Additionally, network members who are also living with HIV may be better-able to relate and to provide support and guidance than others in the network. Additionally, those who are centrally located within the network may be better positioned to connect the adolescent to others to provide support (38). As such, these findings may reflect adolescents’ efforts to navigate stigma and power within their networks. Disclosing to older and/or more central individuals could connect the adolescents with gatekeepers or advocates who are well-positioned to influence attitudes and norms within their social network.
We also found that disclosed network members were much more likely to provide various types of social support than those who were not disclosed to. These findings are consistent with other studies that have found that individuals are most likely to disclose to family members or close friends (39) and that people with HIV may be often motivated to disclose in order to obtain tangible social support, including transportation to medical appointments or and reminders for treatment adherence (39). These findings highlight the multifaceted nature of disclosure, where the act of disclosing can be both a means to access support as well as an opportunity to deepen social relationships.
While overall network size was not associated with disclosure, the type of relationship between the adolescent and the network member moderated the effect of emotional support network size. Larger emotional support networks were associated with a decreased odds of disclosure to family members but an increased odds of disclosure to friends. These results underscore the potential importance of considering both individual and relational factors when designing interventions to support safe and effective disclosure strategies among APHIV, tailored to the unique social contexts of family and peer relationships. The results also suggest that empowering peers with skills to effectively provide emotional support to each other may serve to increase disclosure in this population.
Our study highlights the benefits and future potential of using social network data collection and analysis methods to better understand disclosure. By using a tablet-based data collection method, we were able to efficiently assess key factors of the adolescent's relationship to multiple individuals. This approach would be well-suited to exploring additional ego-alter characteristics, such as disclosure concerns, characteristics of the disclosure process, and outcomes of disclosure with each alter. Recent research noting the importance of disclosure concerns, for example, highlighted that the effect of disclosure concerns on ART adherence and viral suppression likely depends on which individual(s) are a source of disclosure concerns (40).
Additionally, social network data collection and analysis methods may also be particularly relevant as APHIV continue to grow into young adulthood and engage in sexual relationships. HIV status disclosure has historically been a key component of efforts to prevent the onward transmission of HIV (41). Disclosure has been seen as key to the negotiation of safer sexual behavior, including condom use, and a gateway to engaging partners in HIV testing and care, including pre-exposure prophylaxis (PrEP) for partners without HIV and ART for partners with HIV (42). However, research with adolescents has not found a relationship between disclosing one's HIV status to a partner with safer sexual behavior (11, 33, 43). While HIV disclosure has the potential to lead to the negotiation of safe sexual practices or open pathways to care, it simultaneously requires individuals to confront stigma, navigate complex power dynamics, and be equipped to negotiate safer sex. Using social network analysis methods to explore these dynamics within relationships may be particularly useful, especially in the context of U = U (Undetectable = Untransmittable), which demonstrates that individuals with undetectable viral loads cannot sexually transmit HIV. Recent qualitative research has found that some people with suppressed viral loads feel as though disclosing their HIV status, particularly to sexual partners, is a shared responsibility and that partners should inquire about their HIV status (44). Collecting data on this social context of disclosure (i.e., assessing whether each network member initiated the HIV disclosure process with the adolescent) using tablet-based approaches to network data collection can facilitate our understanding of this topic in the South African context, where awareness of U = U among adolescents and adults with HIV remains low (45, 46).
The findings of our study should be understood within the context of study limitations. The egocentric network data collected in this study were based on the APHIV's self-report and as such, could be biased by the adolescent's perception of social ties between network members. Also, while the use of the tablet-based data collection tool reduced participant burden, there are limitations specific to the way this tool measured binary ego-alter characteristics, like disclosure (and alter's HIV status). This was done by prompting the participant to tap on all the individuals in the network to whom they disclosed (or whom they perceived to be living with HIV). This means that any alters that were not selected by the participant were presumed to be intentionally omitted rather that overlooked unintentionally by the ego. Additionally, the study sample was limited to 58 egos and the sample was recruited from HIV clinics, so the results presented may not generalize to other APHIV, particularly those that are not engaged in HIV care. Also, the findings apply to adolescents who are well established on ART and who's HIV has been well controlled; they may not be applicable to those not on ART or with less well controlled HIV. Finally, the study is hypothesis-generating and exploratory in its nature and therefore did not account for multiple testing.
Findings from this research could have implications for designing interventions that support safe and effective disclosure practices, ultimately enhancing the health and well-being of this population. Network members to whom adolescents have disclosed can potentially impact the adolescents’ treatment adherence and HIV care engagement, and these individuals could be engaged to provide critical social support to the adolescents. These individuals could be explicitly engaged in interventions to promote disclosure as well. For example, a recent feasibility trial testing a 4-session group intervention to promote disclosure among young adults with perinatally-acquired HIV found that outlining external support options would be beneficial (47). Network members to whom adolescents have already disclosed could be leveraged for this role. Our findings also speak to the need for tailored interventions that acknowledge the complexities of disclosure decisions to help APHIV navigate these challenges while promoting autonomy in their disclosure journeys. Given that APHIV are more likely to disclose to trusted individuals and those perceived to be living with HIV, interventions could focus on strengthening social support networks and empowering adolescents with strategies to safely disclose to key support figures. Additionally, our findings emphasize the importance of equipping healthcare providers with the necessary training to address disclosure concerns sensitively. Healthcare workers can play a crucial role in supporting adolescents through the disclosure process by providing guidance, addressing stigma-related fears, and facilitating discussions around disclosure within families and peer networks. Healthcare workers may be particularly well-positioned to provide this support, as they often play a role in informing APHIV of their HIV status (48). Other studies have identified the need for better support at schools, including policies to facilitate disclosure and offer post-disclosure support (49). Finally, community-based programs may offer an important avenue for fostering supportive social environments. Programs that work to reduce HIV stigma at the community level and enhance peer support networks could help create safer spaces for disclosure and, in turn, improve adolescents’ engagement in HIV care. Future research should explore how integrating social network-based approaches into community and clinical settings may further facilitate safe and empowering disclosure practices among adolescents with HIV.
In conclusion, this study highlights the potential role of social networks in shaping HIV disclosure among APHIV. While most participants disclosed their status to at least one person, overall disclosure within social networks remained low, highlighting the need for interventions that address both individual and structural barriers to disclosure. Strengthening trusted relationships and addressing community stigma are essential components of disclosure support strategies. To build on these findings, researchers should employ longitudinal network analysis to examine disclosure within the social context of dynamic relationships. Studies assessing the effectiveness of peer-led disclosure interventions and community stigma-reduction efforts would also provide valuable insights. Policymakers should prioritize initiatives that ensure APHIV receive tailored disclosure support through clinic and community settings. Finally, healthcare providers should receive training in disclosure counseling, stigma reduction strategies, and family engagement approaches to better support APHIV in their disclosure journeys.
Data availability statement
The datasets presented in this article are not readily available because the potential for heightened risk of reidentification of certain data and the sensitive topic of the research (HIV disclosure among adolescents living with HIV). Data may be made available through a data use agreement. Requests to access the datasets should be directed to Marta Mulawa,bWFydGEubXVsYXdhQGR1a2UuZWR1.
Ethics statement
The studies involving humans were approved by Institutional Review Board at Duke University and the Human Research Ethics Committee of the Faculty of Health Sciences at the University of Cape Town. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
MM: Conceptualization, Funding acquisition, Investigation, Writing – original draft, Writing – review & editing. FH: Data curation, Formal Analysis, Writing – review & editing, Methodology. NP: Data curation, Writing – review & editing. MA: Data curation, Methodology, Writing – review & editing. RB: Methodology, Supervision, Writing – review & editing. H-JL: Methodology, Supervision, Writing – review & editing. HZ: Funding acquisition, Writing – review & editing. DS: Funding acquisition, Writing – review & editing. JH: Conceptualization, Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the National Institute of Mental Health of the National Institutes of Health under Award Number K01MH118072 and the National Institute of Allergy and Infectious Diseases under Award Number R25AI140495. The parent study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD074051) and the South African Medical Research Council (SAMRC). Statistical Analysis was supported by the Duke University Center for AIDS Research (CFAR), an NIH funded program (5P30 AI064518).
Acknowledgments
We thank the clinical, laboratory, and data study staff in CTAAC. We are grateful to the Western Cape Health Department and CEO of Red Cross Children's Hospital for support of the parent study. We also express our gratitude to the study participants and their families.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. The Collaborative Initiative for Paediatric HIV Education and Research (CIPHER) Global Cohort Collaboration, Slogrove AL, Schomaker M, Davies MA, Williams P, Balkan S, et al. The epidemiology of adolescents living with perinatally acquired HIV: a cross-region global cohort analysis. PLOS Med. (2018) 15(3):e1002514. doi: 10.1371/journal.pmed.1002514
2. Robinson A, Cooney A, Fassbender C, McGovern DP. Examining the relationship between HIV-related stigma and the health and wellbeing of children and adolescents living with HIV: a systematic review. AIDS Behav. (2023) 27(9):3133–49. doi: 10.1007/s10461-023-04034-y
3. UNAIDS. AIDSinfo Global Data on HIV Epidemiology and Response: Data Sheet. Geneva: UNAIDS (2020).
5. Kim SH, Gerver SM, Fidler S, Ward H. Adherence to antiretroviral therapy in adolescents living with HIV: systematic review and meta-analysis. AIDS. (2014) 28(13):1945–56. doi: 10.1097/QAD.0000000000000316
6. Ashaba S, Zanoni BC, Baguma C, Tushemereirwe P, Nuwagaba G, Kirabira J, et al. Challenges and fears of adolescents and young adults living with HIV facing transition to adult HIV care. AIDS Behav. (2023) 27(4):1189–98. doi: 10.1007/s10461-022-03856-6
7. Bekker LG, Johnson L, Wallace M, Hosek S. Building our youth for the future. J Int AIDS Soc. (2015) 18(2 Suppl 1):20027. doi: 10.7448/IAS.18.2.20027
8. Society for Adolescent Health and Medicine. Improving outcomes for adolescents and young adults living with HIV. J Adolesc Health. (2023) 73(3):605–9. doi: 10.1016/j.jadohealth.2023.05.006
9. Elopre L, Hook EW, Westfall AO, Zinski A, Mugavero MJ, Turan J, et al. The role of early HIV status disclosure in retention in HIV care. AIDS Patient Care STDs. (2015) 29(12):646–50. doi: 10.1089/apc.2015.0205
10. Spangler SA, Onono M, Bukusi EA, Cohen CR, Turan JM. HIV-positive status disclosure and use of essential PMTCT and maternal health services in rural Kenya. J Acquir Immune Defic Syndr 1999. (2014) 67(Suppl 4):S235–242. doi: 10.1097/QAI.0000000000000376
11. Kidman R, Violari A. Growing up positive: adolescent HIV disclosure to sexual partners and others. AIDS Care. (2020) 32(12):1565–72. doi: 10.1080/09540121.2020.1736260
12. Galano E, Turato ER, Succi RC, de Souza Marques HH, Della Negra M, da Silva MH, et al. Costs and benefits of secrecy: the dilemma experienced by adolescents seropositive for HIV. AIDS Care. (2017) 29(3):394–8. doi: 10.1080/09540121.2016.1248891
13. Mokgatle M, Madiba S. Community perceptions of HIV stigma, discriminatory attitudes, and disclosure concerns: a health facility-based study in selected health districts of South Africa. Int J Environ Res Public Health. (2023) 20(14):6389. doi: 10.3390/ijerph20146389
14. Evangeli M, Wroe AL. HIV disclosure anxiety: a systematic review and theoretical synthesis. AIDS Behav. (2017) 21(1):1–11. doi: 10.1007/s10461-016-1453-3
15. Mugo C, Seeh D, Guthrie B, Moreno M, Kumar M, John-Stewart G, et al. Association of experienced and internalized stigma with self-disclosure of HIV status by youth living with HIV. AIDS Behav. (2021) 25(7):2084–93. doi: 10.1007/s10461-020-03137-0
16. Mengesha MM, Teshome A, Ajema D, Tura AK, Hallström IK, Jerene D. The association between HIV diagnosis disclosure and adherence to anti-retroviral therapy among adolescents living with HIV in sub-Saharan Africa: a systematic review and meta-analysis. PLoS One. (2023) 18(5):e0285571. doi: 10.1371/journal.pone.0285571
17. Wondmneh Y. Disclosure Status and associated factors among caregivers of children on antiretroviral therapy in Addis Abeba, Ethiopia: hospital based cross sectional study design. Int Arch Nurs Health Care. (2024) 10(1):195. doi: 10.23937/2469-5823/1510195
18. Siu GE, Bakeera-Kitaka S, Kennedy CE, Dhabangi A, Kambugu A. HIV serostatus disclosure and lived experiences of adolescents at the transition clinic of the infectious diseases clinic in Kampala, Uganda: a qualitative study. AIDS Care. (2012) 24(5):606–11. doi: 10.1080/09540121.2011.630346
19. Weintraub A, Mellins CA, Warne P, Dolezal C, Elkington K, Bucek A, et al. Patterns and correlates of serostatus disclosure to sexual partners by perinatally-infected adolescents and young adults. AIDS Behav. (2017) 21(1):129–40. doi: 10.1007/s10461-016-1337-6
20. Zanoni BC, Archary M, Subramony T, Sibaya T, Psaros C, Haberer JE. Disclosure, social support, and mental health are modifiable factors affecting engagement in care of perinatally-HIV infected adolescents: a qualitative dyadic analysis. AIDS Behav. (2021) 25(1):237–48. doi: 10.1007/s10461-020-02968-1
21. Montgomery SC, Donnelly M, Bhatnagar P, Carlin A, Kee F, Hunter RF. Peer social network processes and adolescent health behaviors: a systematic review. Prev Med. (2020) 130:105900. doi: 10.1016/j.ypmed.2019.105900
22. Luke DA, Harris JK. Network analysis in public health: history, methods, and applications. Annu Rev Public Health. (2007) 28(1):69–93. doi: 10.1146/annurev.publhealth.28.021406.144132
23. Cao B, Saffer AJ, Yang C, Chen H, Peng K, Pan SW, et al. MSM behavior disclosure networks and HIV testing: an egocentric network analysis among MSM in China. AIDS Behav. (2019) 23(5):1368–74. doi: 10.1007/s10461-019-02404-z
24. Hogan B, Melville JR, Phillips II GL, Janulis P, Contractor N, Mustanski BS, et al. Evaluating the paper-to-screen translation of participant-aided sociograms with high-risk participants. Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems; San Jose, California, USA: ACM (2016). p. 5360–71. doi: 10.1145/2858036.2858368 (Accessed May 05, 2021).
25. Marsden PV. Network data and measurement. Annu Rev Sociol. (1990) 16:435–63. doi: 10.1146/annurev.so.16.080190.002251
26. Hoare J, Stein DJ, Heany SJ, Fouche JP, Phillips N, Er S, et al. Accelerated epigenetic aging in adolescents living with HIV is associated with altered development of brain structures. J Neurovirol. (2021) 28:208–16. doi: 10.1007/s13365-021-00947-3
27. Githinji LN, Mahtab S, Zühlke L, Lawrenson J, Myer L, Gray D, et al. Cardiopulmonary dysfunction in perinatally HIV-infected South African adolescents on antiretroviral therapy: baseline findings from the Cape Town adolescent antiretroviral cohort. J Int AIDS Soc. (2019) 22(7):e25340. doi: 10.1002/jia2.25340
28. Sevenoaks T, Fouche JP, Phillips N, Heany S, Myer L, Zar HJ, et al. Childhood trauma and mental health in the Cape Town adolescent antiretroviral cohort. J Child Adolesc Trauma. (2022) 15(2):353–63. doi: 10.1007/s40653-021-00362-0
29. Complex Data Collective 2023. Network Canvas. Complex Data Collective (2023). Available at: https://networkcanvas.com (Accessed December 06, 2024).
30. Latkin C, Yang C, Tobin K, Roebuck G, Spikes P, Patterson J. Social network predictors of disclosure of MSM behavior and HIV-positive serostatus among African American MSM in Baltimore, Maryland. AIDS Behav. (2012) 16(3):535–42. doi: 10.1007/s10461-011-0014-z
31. Halekoh U, Højsgaard S, Yan J. The R package geepack for generalized estimating equations. J Stat Softw. (2006) 15(2):1–11. doi: 10.18637/jss.v015.i02
32. Csardi G, Nepusz T. The igraph software package for complex network research. Inter J Complex Syst. (2006) 1695(5):1–9.
33. Nöstlinger C, Bakeera-Kitaka S, Buyze J, Loos J, Buvé A. Factors influencing social self-disclosure among adolescents living with HIV in Eastern Africa. AIDS Care. (2015) 27(sup1):36–46. doi: 10.1080/09540121.2015.1051501
34. Birungi H, Obare F, Mugisha JF, Evelia H, Nyombi J. Preventive service needs of young people perinatally infected with HIV in Uganda. AIDS Care. (2009) 21(6):725–31. doi: 10.1080/09540120802511901
35. Fair C, Albright J. “Don’t tell him you have HIV unless he’s ‘the one’”: romantic relationships among adolescents and young adults with perinatal HIV infection. AIDS Patient Care STDs. (2012) 26(12):746–54. doi: 10.1089/apc.2012.0290
36. Chaudoir SR, Fisher JD, Simoni JM. Understanding HIV disclosure: a review and application of the disclosure processes model. Soc Sci Med 1982. (2011) 72(10):1618–29. doi: 10.1016/j.socscimed.2011.03.028
37. Gabbidon K, Chenneville T, Peless T, Sheared-Evans S. Self-disclosure of HIV Status among youth living with HIV: a global systematic review. AIDS Behav. (2020) 24(1):114–41. doi: 10.1007/s10461-019-02478-9
38. Hoover MA, Green HD, Bogart LM, Wagner GJ, Mutchler MG, Galvan FH, et al. Do people know I’m Poz?: factors associated with knowledge of serostatus among HIV-positive African Americans’ social network members. AIDS Behav. (2016) 20(1):137–46. doi: 10.1007/s10461-015-1039-5
39. Chapman Lambert C, Tarver WL, Musoke PL, Stringer KL, Whitfield S, Turan B, et al. Complexities of HIV disclosure in patients newly entering HIV care: a qualitative analysis. J Assoc Nurses AIDS Care JANAC. (2020) 31(2):208–18. doi: 10.1097/JNC.0000000000000127
40. Yigit I, Bayramoglu Y, Weiser SD, Johnson MO, Mugavero MJ, Turan JM, et al. Disclosure concerns and viral suppression in people newly initiating HIV care: the role of internalized HIV stigma. J Acquir Immune Defic Syndr 1999. (2021) 86(4):406–12. doi: 10.1097/QAI.0000000000002593
41. Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ. (2004) 9:299–307. Available at: https://iris.who.int/handle/10665/269110
42. Hamzah L, Hamlyn E. Sexual and reproductive health in HIV-positive adolescents. Curr Opin HIV AIDS. (2018) 13(3):230–5. doi: 10.1097/COH.0000000000000456
43. Toska E, Cluver LD, Hodes R, Kidia KK. Sex and secrecy: how HIV-status disclosure affects safe sex among HIV-positive adolescents. AIDS Care. (2015) 27(sup1):47–58. doi: 10.1080/09540121.2015.1071775
44. Roth GH, Walker ER, Talley CL, Hussen SA. “It’s a very grey, very messy area”: a qualitative examination of factors influencing undetectable gay men’s HIV status disclosure to sexual partners. Cult Health Sex. (2023) 25(5):664–79. doi: 10.1080/13691058.2022.2086708
45. Swain S, Inman E, Josipovic D, Violari A, Kidman R. Missed opportunity: low awareness of undetectable equals untransmittable (U=U) among adolescents living with HIV. AIDS Res Ther. (2024) 21(1):69. doi: 10.1186/s12981-024-00659-8
46. Sineke T, Onoya D, Mokhele I, Cele R, Sharma S, Sigasa P, et al. “I was scared dating… who would take me with my status?”-living with HIV in the era of UTT and U=U: a qualitative study in Johannesburg, South Africa. PLoS Glob Public Health. (2023) 3(10):e0000829. doi: 10.1371/journal.pgph.0000829
47. Evangeli M, Gnan G, Musiime V, Fidler S, Seeley J, Frize G, et al. The HIV empowering Adults’ decisions to share: UK/Uganda (HEADS-UP) study-a randomised feasibility trial of an HIV disclosure intervention for young adults with perinatally acquired HIV. AIDS Behav. (2024) 28(6):1947–64. doi: 10.1007/s10461-024-04294-2
48. Kidia KK, Mupambireyi Z, Cluver L, Ndhlovu CE, Borok M, Ferrand RA. HIV status disclosure to perinatally-infected adolescents in Zimbabwe: a qualitative study of adolescent and healthcare worker perspectives. PLoS One. (2014) 9(1):e87322. doi: 10.1371/journal.pone.0087322
49. Moraa H, Njuguna I, Mugo C, Mbwayo A, Nyapara F, Aballa C, et al. “We can tell a good teacher who cares, understands, and can be confidential about it”: youth and caregiver experiences with HIV disclosure to schools in Kenya. Front Public Health. (2023) 11:1172431. doi: 10.3389/fpubh.2023.1172431
Keywords: HIV, disclosure, adolescents, youth, South Africa, network analysis
Citation: Mulawa MI, Hung F, Phillips NJ, Austin MF, Barfield R, Lee H-J, Zar HJ, Stein DJ and Hoare J (2025) HIV disclosure in the social networks of adolescents with HIV in Cape Town, South Africa. Front. Reprod. Health 7:1545039. doi: 10.3389/frph.2025.1545039
Received: 13 December 2024; Accepted: 28 April 2025;
Published: 21 May 2025.
Edited by:
Shan Qiao, University of South Carolina, United StatesReviewed by:
Dereje Bayissa Demissie, St. Paul’s Hospital Millennium Medical College, EthiopiaMichael Evangeli, University of London, United Kingdom
Copyright: © 2025 Mulawa, Hung, Phillips, Austin, Barfield, Lee, Zar, Stein and Hoare. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marta I. Mulawa, bWFydGEubXVsYXdhQGR1a2UuZWR1
 Marta I. Mulawa
Marta I. Mulawa Frances Hung3
Frances Hung3 Nicole J. Phillips
Nicole J. Phillips Richard Barfield
Richard Barfield Heather J. Zar
Heather J. Zar Dan J. Stein
Dan J. Stein