- 1Reproductive Health Department, Yanet-Liyana College of Health Sciences, Hawassa, Ethiopia
- 2School of Public Health, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
Introduction: Utero-vaginal prolapse is a significant public health concern in developing countries such as Ethiopia, where access to health care is limited. It is a major reproductive crisis in women that affects a woman's quality of life and has a great negative impact on women's social, physical, economic, and psychological wellbeing. Despite this, there is limited evidence on risk factors in the study area. Therefore, this study aimed to identify the risk of utero-vaginal prolapse among women visiting gynecologic outpatient departments in governmental hospitals.
Methods: A facility-based unmatched case–control study was conducted among 286 women visiting gynecologic outpatient departments in selected governmental hospitals. The data were collected via a pretested structured questionnaire designed with a Kobo tool box. The Kobo tool is an easy, open electronic data collection tool suitable for field research and helps ensure data security. The data were subsequently exported to SPSS for analysis. Descriptive statistics were performed. To assess associations, independent t-tests and binary and multivariate logistic regression analyses were performed. Finally, a 95% confidence interval and adjusted odds ratio with a p value <0.05 were used to examine the associations between the dependent and independent variables.
Results: A total of 277 respondents, 91 patients with utero-vaginal prolapse and 186 controls, were included in the study. According to the multivariable logistic regression analysis, early childbirth [AOR = 3.98 (95% CI: 1.08–14.58)], a history of multiple pregnancies [AOR = 2.88 (95% CI: 1.27–6.49)], home delivery [AOR = 4.9 (95% CI: 1.3–18.6)], prior pelvic surgery [AOR = 3.9 (95% CI: 1.08–13.8)], and a history of instrumental delivery [AOR = 3.1 (95% CI: 1.08–9.14)] were found to be significant determinants of utero vaginal prolapse.
Conclusion: These findings underscore that in utero vaginal prolapse is a common reproductive health problem. Early childbirth, a history of multiple pregnancies, home delivery, prior pelvic surgery, and a history of instrumental delivery were risk factors for UVP. Therefore, social and health care system determinants are critical. Therefore, prevention of UVP requires promoting health facility deliveries, integrating obstetric care, and addressing the societal norms that may lead to early childbirth. Consequently, context-based interventions addressing these determinants can greatly improve women's quality of life, decrease the prevalence of UVP, and improve overall maternal health.
Introduction
Uterovaginal prolapse (UVP) is defined as descent of the uterus through the vaginal canal due to defects in the supportive structures of the uterus and vagina because of different factors (1). Uterovaginal prolapse is a public health concern worldwide and contributes to reproductive health morbidity among women. The estimated worldwide incidence of pelvic organ prolapse is nearly 9% (1). Given the global increase in the aging population in well-resourced countries, the need for UVP management is anticipated to increase in the coming decades (2). The exact prevalence of utero vaginal prolapse is difficult to determine because many women are symptomatic, but they are not symptomatic due to social factors (3). One population-based study revealed that approximately 3% of the 1961 adult women surveyed reported symptomatic vaginal bulging (4). Globally, from 1990 to 2019, 2%–20% of all women were affected by UVP (5). In addition, the burden of UVP in low- and middle-income countries, particularly in sub-Saharan African countries, is still challenging and increasing and was recently reported to be approximately 20% from 2012 to 2015 (6). These might require different strategies to address the burden.
UVP is a common gynecological problem, and its presentation varies in type and severity among patients. In developed countries, the prevalence is high among postmenopausal women, whereas in developing countries, the condition is common in women of reproductive age (7). It has been argued that prolapse may be more common in resource-constrained settings owing to established factors and heavy physical burdens and that this condition may affect daily life more severely than it does in high-income settings (8). Working on reproductive-age groups is essential for addressing UVP in resource-limited settings.
In Ethiopia, gynecological problems are important public health problems that affect maternal health outcomes and women's productivity. In 2020, the overall incidence of UVP in Ethiopia was estimated to be 23.52% (9). Currently, UVP accounts for 40.7% of major gynecological operations in Jimma (10), followed by hysterectomy (41.1%) and leiomyoma (23%) in Tikur Anbessa (11). This underscores multi-sectoral collaboration to fight against UVP.
The true risk factors associated with UVP are poorly understood. The cause of this disorder is likely multifactorial and attributable to a combination of risk factors, which vary from patient to patient. This might be due to the private and asymptomatic nature of the illness, making UVP the “hidden epidemic” (12). The major risk factors for the development of utero-vaginal prolapse are older age, a family history of UVP, menopause, higher parity, difficult labor and delivery, malnutrition, chronic cough and constipation. Race is also considered a risk factor for prolapse, while African and Asian ethnicity is thought to be protective (13). Elucidating the determinants of UVP is important for designing context-based interventions.
Uterine prolapse is a hidden problem, especially in developing countries such as Ethiopia, where the situation is far worse (14). UVP can severely affect a woman's quality of life, with a great negative impact on women's social, physical, economic, and psychological wellbeing (15). Most importantly, problems or physical disorders that occur in patients with prolapse can reduce women's reproductive health, such as discomfort because of masses in and out of the genitals (14). Despite its burden, there are no national UVP-targeted intervention strategies. Hence, identifying the factors associated with UVP has a great role in the development of intervention strategies.
Although UVP is a preventable and curable condition, it is a prevalent disease that is impacted by various risk factors, but only a few studies exist on its determinants. Identifying key risk factors may enable early detection, prevention, and management measures. Thus, this study aimed to identify risk factors associated with utero vaginal prolapse (UVP) among women attending gynecologic outpatient departments in public hospitals in the Sidama region, Ethiopia. These results provide valuable insight for policymakers, gynecologists, and midwives in the development of preventative methods, the design of patient education, and the development of treatments to minimize the burden of UVP.
Methods and materials
Study design
A facility-based unmatched case‒control study design was used to respond to the research objective.
Study area and period
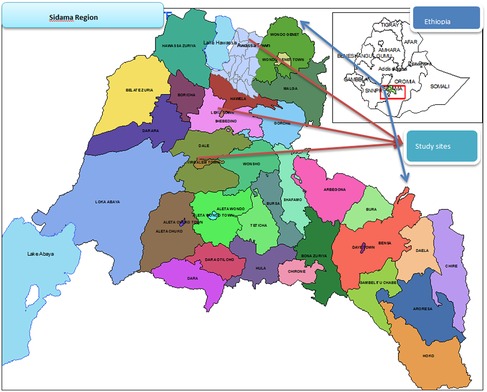
The study was conducted in the Sidama region, which is located in the southern part of Ethiopia. The Sidama region is the tenth region in Ethiopia and is bordered by Oromia in the northeast, Wolayta in the west, and Gedo in the south. According to the Sidama Region Development Corporation, Planning and Statistics 2020, the total estimated population is 4,369,214 million people, 2,201,313 of whom are females (16). According to regional health bureau data, there are 14 primary hospitals, 4 general hospitals, 1 specialized teaching hospital, 124 governmental health centers, 526 health posts and more than 108 private clinics (17). These studies were conducted in governmental hospitals, namely, the Adare, Yirgalem, Leku and Hawassa hospitals (Figure 1), which are 275 km, 325 km, 392 km and 273 km away from Addis Ababa, respectively. The hospitals provide services for the town and surrounding area, including inpatient, outpatient, and chronic disease follow-up services and maternal and child health services. These governmental hospitals have gynecologic outpatient departments (OPDs) and gynecologic wards after they perform different gynecologic operations, including UVP. According to previous reports, the total number of UVP patients was 194, 108, 84 and 93 at Yirgalem, Hawassa Hospital, Adare and Leku hospitals, respectively (18–21). The study was conducted from May 1–July 30, 2023.
Source and study population
Source populations
⮚ The source population included all women who were visiting gynecologic OPDs at government general hospitals in the Sidama region during the study period.
Study populations
Case
⮚ All women older than 18 years who were attending a gynecologic OPD at a selected public hospital in Hawassa town with UVP confirmed by an attending physician during the actual data collection period were considered cases.
Control
⮚ All women who had no UVP but were older than 18 years and were attending selected hospitals for other gynecological care during the actual data collection period composed the study population.
Inclusion and exclusion criteria
Inclusion criteria
⮚ All women older than 18 years old attending gynecology OPD during the actual data collection period in selected public health facilities were included in the study.
Exclusion criteria
⮚ All women who were critically ill or had a previous history of total abdominal or vaginal hysterectomy were excluded from the study.
⮚ Women with grade I UVP, women with cervical elongation, women with total abdominal hysterectomy and vaginal hysterectomy, critically ill women and women with mental problems were excluded from the study.
Sample size determination
The sample size for the case‒control study was determined via the double population proportion formula with epi info version 7, with the following basic assumption: 95% confidence level, 80% power and a case‒to-control ratio of 1:2 (22). In a study performed in Nekemte town, East Wollega Zone, Oromia region, Ethiopia, a family history of UVP was taken as the main exposure variable for utero‒vaginal prolapse, which provided the maximum sample size (23). According to the present study, 5.3% of the controls and 20.7% of the patients had a family history of UVP. Therefore, the use of the stat calc epi info version 7.2 resulted in a total sample size of 260 patients (87 patients and 173 controls). With a 10% nonresponse rate, the total sample size on the basis of Kelsey's estimation was 286 (95 cases and 190 controls) (23, 24).
Sampling technique and sampling procedure
A convenient sampling technique was used for enrolling patients, whereas a systemic sampling technique was used to include controls. The selected public hospitals in the Sidama region were included in the study. Prior to the study, the number of patients who attended the hospital during the past year was checked. The enumeration of the previous one-year cases and controls from the patient/client card was conducted to determine the case and control flow of each hospital with reference to their card number from the obstetric registration book. Then, on the basis of the number of patients/clients, the calculated sample size was proportionally allocated. Finally, every patient and the next two consecutive controls were included in the study until the required sample was met.
Data collection tools and procedure
The data were collected via a pretested and structured questionnaire, which was prepared after different studies were reviewed. The questionnaire is composed of three main parts: mothers’ socio-demographic (socioeconomic) factors, gynecologic and obstetric factors, and medical and personal factors. The tool was translated into the local languages Amharic and Sidamgna to maintain consistency.
Face‒to-face interviews were used to collect the data. Previously, the final version of the questionnaire was designed with a Kobo collection kit installed on an android smartphone. The kobo tool is an easy, open electronic data collection tool suitable for field research and helps ensure data security. The data were subsequently linked to a server and checked for proper functioning. During the data collection period, 4 BSc midwives were used to collect the data, and daily supervision was provided. In addition, the principal investigator and supervisor supervised the daily data gathering in the field.
Data quality assurance
Initially, the investigator developed the English version of the questionnaire after performing a thorough literature analysis. The questionnaire was subsequently translated into the Amharic and Sidamgna versions and then retranslated into English by an expert to ensure consistency. A pretest was conducted at Tula Hospital on 5% of the sample, and minor corrections and modifications were made before actual data collection. In addition, two days of standard training were provided to the data collectors and supervisors to familiarize them with the data collection tools. During the data gathering process, supervision was conducted, and appropriate corrective actions were taken. The collected data were checked for completeness, and any incomplete entries were excluded from the study.
Variables of the study
Dependent variable
Uterovaginal prolapse.
Independent variables
The socioeconomic and demographic factors included place of residence, maternal age, marital status, living arrangement, maternal educational status, husband educational status, occupation, and average monthly income.
The following obstetric and gynecological factors were assessed: parity, gravidity, mode of delivery, place of delivery, duration of labor, induced labor, history of instrumental delivery, episiotomy, vaginal tear, sphincter damage, fundal pressure, ANC follow-up, prior pelvic surgery, and history of blunt/sharp damage to the reproductive or perineum.
The personal and medical factors included a history of cough, hypertension, DM, chronic constipation, a family history of UVP, and a heavy workload.
Operational definitions
Pelvic organ prolapse refers to the abnormal herniation of pelvic viscera, such as the uterus, vaginal vault, bladder, rectum, and small or large bowel, against the vaginal walls or through the vaginal introits (6).
Uterovaginal prolapse is the descent of the uterus/cervix and vaginal segments through the vaginal canal.
Control: Women without UVP who are admitted to the hospital for other gynecological problems will be considered controls.
Data processing and analysis
Once the data were collected, they were downloaded and exported from the kobo tool server in Excel and SPSS label forms and then imported into the Statistical Package for Social Science version 27 for analysis. The data were subsequently cleaned, followed by the identification and examination of outliers via descriptive analysis. Following the process of data cleaning, a descriptive analysis (continuous and categorical) was conducted. The results are presented via frequency tables, textual descriptions, graphs, and measures of central tendency (means) and variability (standard deviations). For continuous variables, the means and standard deviations were utilized. To assess the equality of variance and mean difference in exposure between cases and controls, we used an independent sample t-test. This allowed us to determine the mean difference in exposure between the two groups of people.
Then, bivariable and multivariate analyses were carried out to assess the correlations between the dependent and independent variables. Variables with p values less than 0.25 were candidates for multivariate analysis to account for any potential confounding effects. Finally, a p value <0.05 indicated a statistically significant correlation with the 95% CI and adjusted odds ratio. The Hosmer and Lemeshow goodness-of-fit test was performed to verify model fitness at a p value >0.05. The multi-collinearity of independent variables was tested via variance inflation factors, and a variance inflation factor (VIF) > 10 was considered suggestive of collinearity.
Ethical considerations
Ethical approval was obtained from the research review committee of Yanet-Liyana Health Science College (Ref: LHC/YLCH/OGL/1080/15 and Date: 24/07/2023). The letter of support was subsequently obtained from the Sidama Regional Health Bureau and written to the Adare, Yirgalem, HUCSH and Leku General Hospitals. All ethical issues were addressed during data collection in the field, and written consent was obtained before actual data collection. No personal identifiers were used.
Results
A total of 277 respondents, including 91 patients with UVP and 186 controls without a diagnosis of UVP, were included in the study, for a response rate of 97%.
Socio-demographic factors
The mean (±SD) ages for the cases were 43.9 ± 11.6 years and 33.2 ± 10.8 years for the control group; 49 (53.3%) patients, whereas 43 (46.7%) controls, were ≥40 years old. Among the controls, 120 (80.0%) and 30 (20.0%) patients were from urban areas, respectively. Most of the controls (64, 88.9%) were from college and above. In total, 74 (52.9%) patients were house wives. Seventy-seven (52.9%) controls were married and living together. Among the married women, 55 (73.3%) of the controls had a husband with a college education or above. Additionally, 41 (67.2%) of the controls were government employees (Table 1).
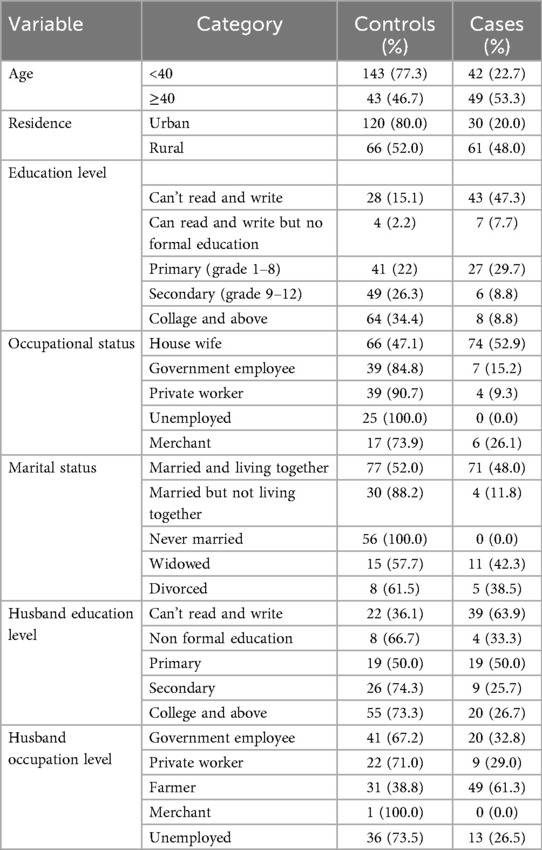
Table 1. Socio-demographic characteristics of the respondents in the Sidama region, southern Ethiopia, 2023.
Obstetric and gynecologic factors
Among the study respondents, 153 (80.5%) were controls, and 37 (19.5%) were married at the age of 18 and above. Among the respondents, 70 (71.4%) controls and 28 (28.6%) patients gave their first birth at the age of 20 years and above. Among the patients, 50 (35.2%) had fewer than 5 live births, and 44 (33.1%) had fewer than 5 pregnancies. The majority (80, 65.6%) of the controls had ANC visits. More than one-fourth of the patients (80; 54.1%) delivered vaginally. More than half of the patients (58.0%) had a history of multiple pregnancies. Among the respondents, 23 (43.4%) were controls, and 30 (56.6%) gave birth at home. Among the patients, 37 (52.9%) had a history of labor greater than or equal to 24 hours. Among the patients, 9 (25.7%), 23 (43.4%) and 8 (29.6%) had a history of instrumental delivery, episiotomy and induced labor, respectively. Among the patients, 12 (27.3%), 3 (27.3%) and 39 (59.1%) had a history of vaginal tear, sphincter damage and fundal pressure, respectively (Table 2).
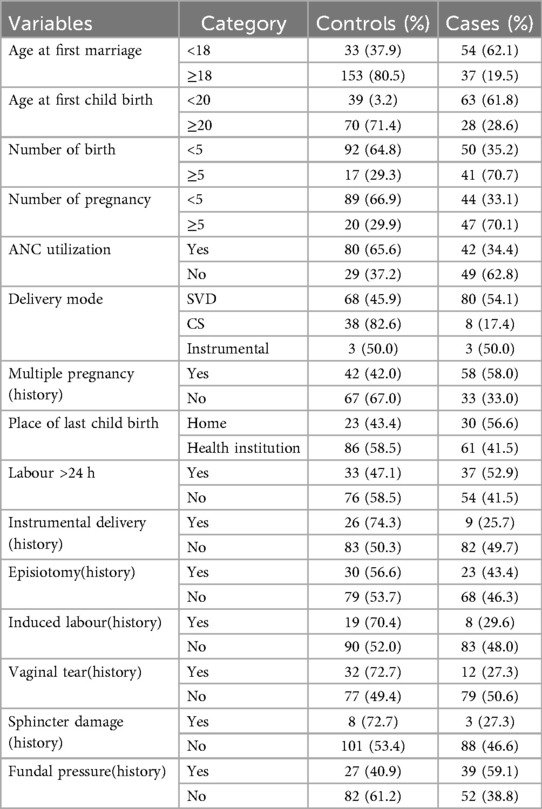
Table 2. Gynaecologic and obstetric characteristics of the respondents from governmental health facilities in Sidama region, southern Ethiopia, 2023.
Among the study respondents, 181 (65.3%) had postpartum rest before starting their usual activity. Among these respondents, 57 (48.3%) patients and 61 (51.7%) controls had less than 42 days of rest.
Medical factors
Among the women involved in the study, 33 (66.0%) controls and 17 (34.0%) patients had a history of chronic cough. Twenty-four (55.8%) controls and 19 (44.2%) patients had chronic constipation. Three (16.7%) and 10 (28.6%) patients had diabetes mellitus and hypertension, respectively.
Individual factors
Among the study respondents, 28 (53.8%) controls and 24 (46.2%) patients had a history of abortion. Among the total patients, 5 (16.1%) and 4 (16.7%) had undergone prior pelvic surgery and reconstruction organ blunt surgery, respectively. Information about the cause of UVP was available for 50 (72.5%) controls and 19 (27.5%) patients. Information about the cause of UVP was available for 35 (87.5%) controls and 5 (12.5%) patients. There were 29 (87.9%) controls and 4 (12.1%) patients with information about aggravating factors of UVP. Among the respondents, 20 (83.3%) controls and 4 (16.7%) patients had a family history of UVP. Among the women involved in the study, 142 (78.0%) controls and 40 (22.0%) patients had a history of heavy objects.
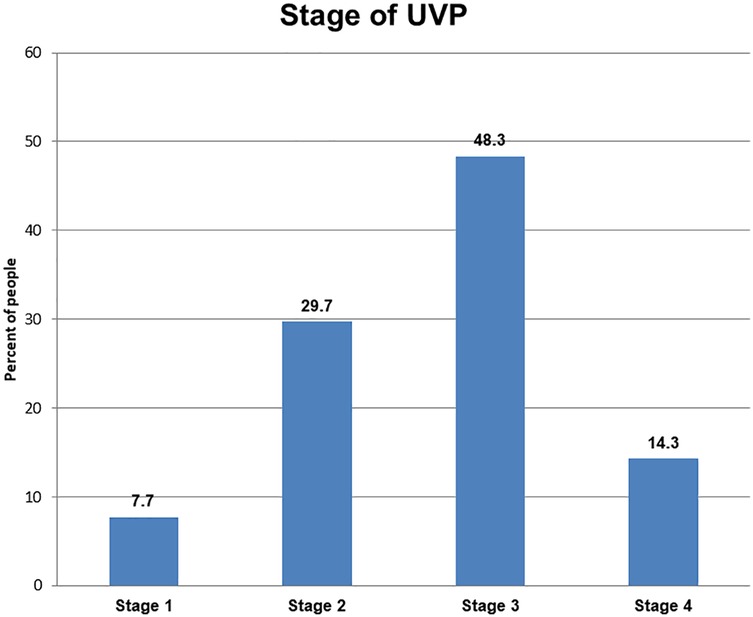
Among all UVP patients, 44 (48.3%) were diagnosed with stage 3 UVP, followed by 29.7% who were diagnosed with stage 2 UVP (Figure 2).
Independent sample t-tests for the mean difference in exposure between cases and controls
To assess the equality of variance and mean difference between cases and controls with respect to exposure factors, in this study, we performed independent sample t-tests. Levene's test for the equality of variances was applied that is, equal variances, p > 0.05, and unequal variances, p < 0.05 to investigate the similarity of variance between cases and controls. Similarly, the mean difference between the case and control groups was determined via a t-test for equality, with corresponding p values applied (i.e., p < 0.05 signifies a significant variation in the means of the two sample groups evaluated). We assumed unequal variance and applied the one-sample t-test, as practically all of the test variables have a variance greater than 4 (25). The factors associated with increased risk of UVP among women were highest educational level (P < 0.0001), respondent marital status (P < 0.001), multiple pregnancies (P < 0.001), history of home delivery (P < 0.001), history of instrumental delivery (P = 0.008), history of fundal pressure during childbirth (P = 0.007), and farming experience (P < 0.001) (Table 3).
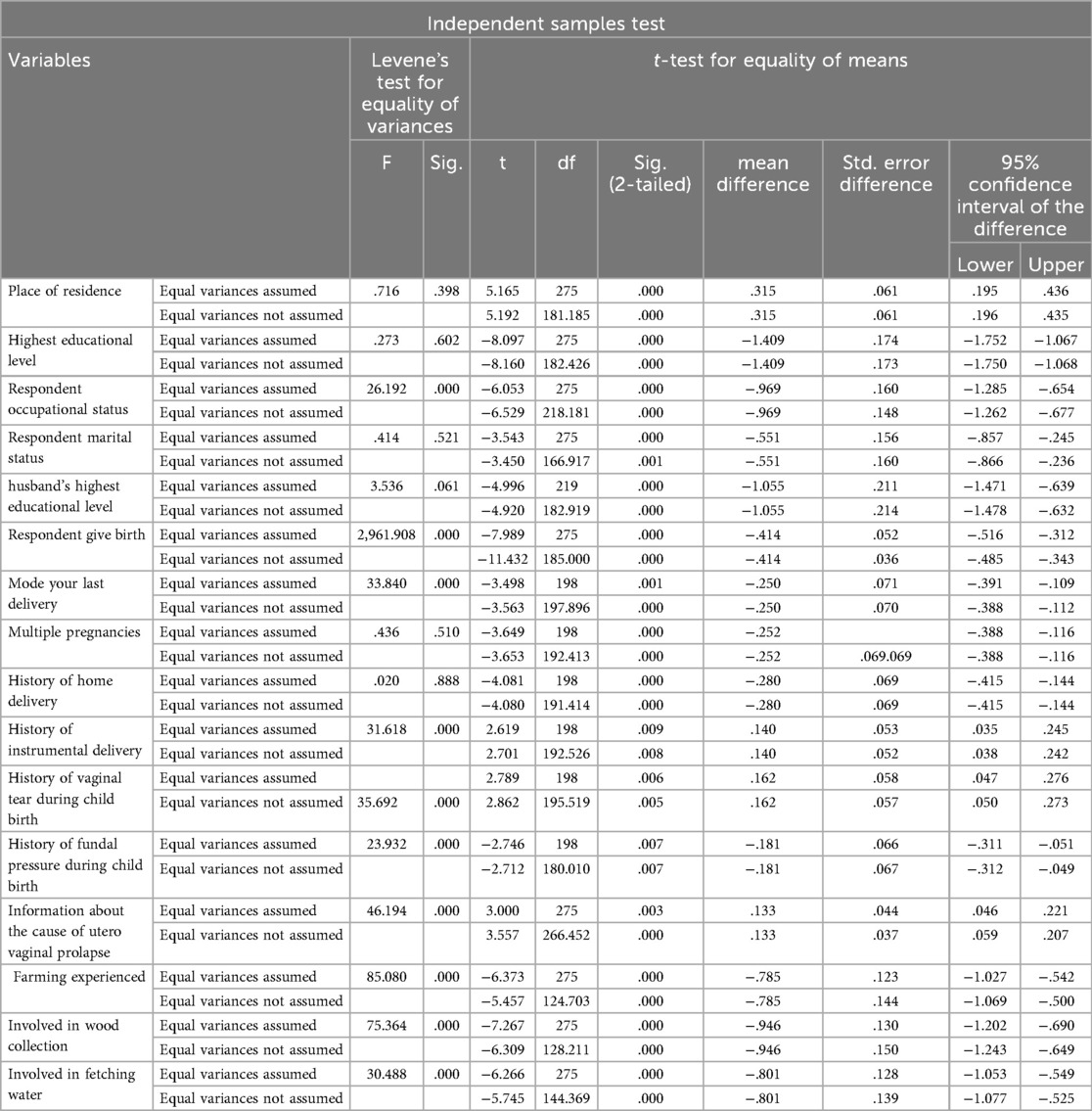
Table 3. Independent sample t-test of respondents for determinants of UVP among women visiting gynaecologic outpatient departments at governmental hospitals in the Sidama region, southern Ethiopia, 2023 (cases = 95, control = 190; total 286.
Determinants of utero-vaginal prolapse
In the bivariate logistic regression analysis, age, residence, education, husband education level, age at child birth, number of births, history of instrumental delivery, number of pregnancies, ANC visit, multiple pregnancies, history of induced labor, prior pelvic surgery, chronic constipation, information about UVP, place of delivery and workload were found to be variables selected for multivariate analysis. On multivariate analysis, age at first childbirth, multiple pregnancies, place of delivery, prior pelvic surgery and history of instrumental delivery were found to be potential determinants of UVP at a p value <0.05.
The odds of developing UVP were 4 times greater among women aged less than 20 years with a first child birth. [AOR = 3.98 (95% CI: 1.1–14.6)]. Women who had a history of multiple pregnancies were approximately three times more likely to develop UVP than their male counterparts were. [AOR = 2.8 (95% CI: 1.3–6.5)]. Women who delivered at home were 5 times more likely to develop UVP than those who delivered at health institutions were [AOR = 4.9 (95% CI: 1.3–18.6)]. Women who had prior pelvic surgery were 4 times more likely to develop this condition than their counterparts were. [AOR = 3.9 (95% CI: 1.1–13.9)]. Women who had a history of instrumental delivery were approximately three times more likely to develop UVP than their counterparts were. [AOR = 3.1 (95% CI: 1.1–9.11)] (Table 4).
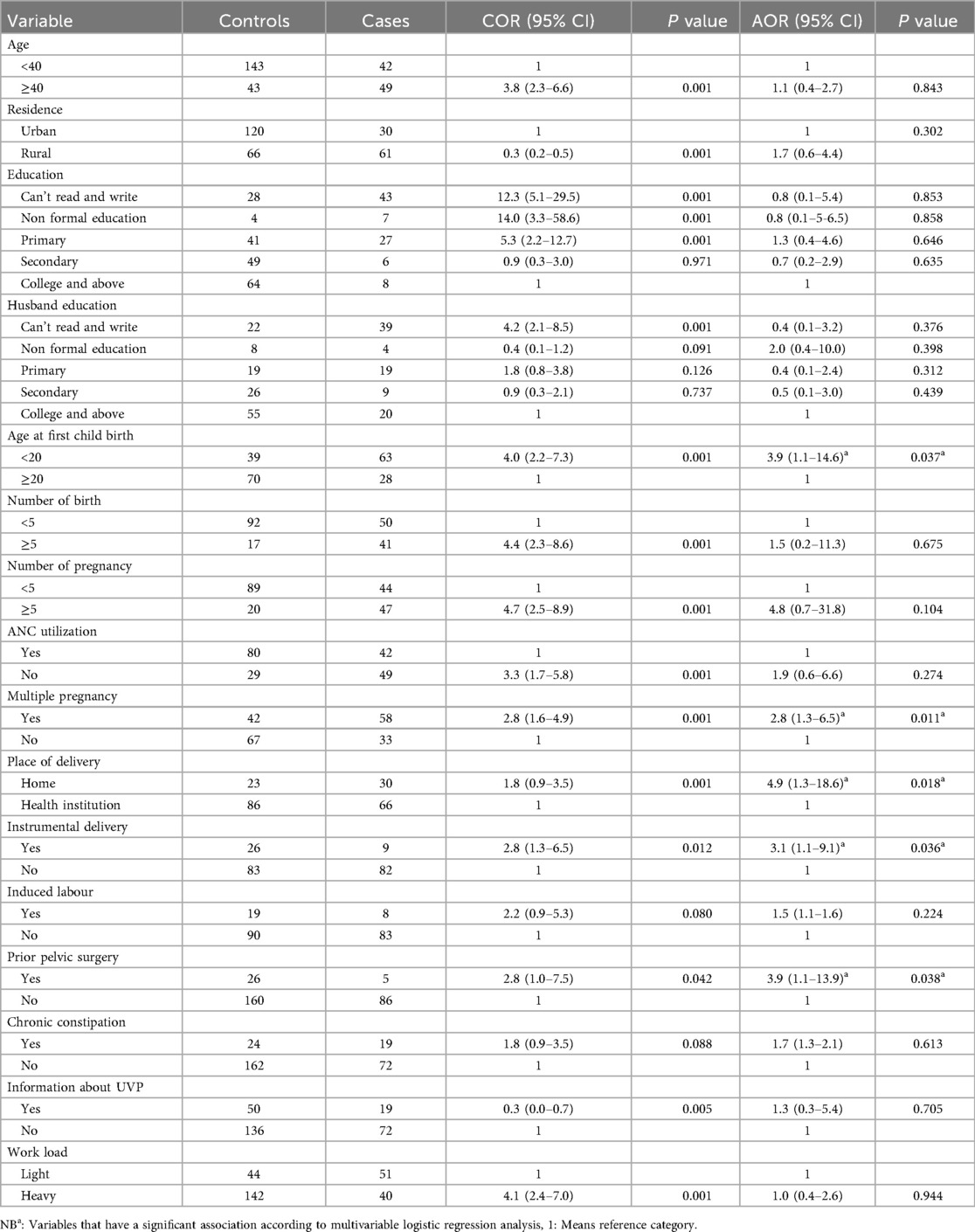
Table 4. Multivariable and bivariable characteristics on determinates of UVP in governmental hospitals in the Sidama region, southern Ethiopia, 2023.
Discussion
This study highlights the key determinants of utero-vaginal prolapse among women visiting gynecology outpatient departments in governmental hospitals in the Sidama region of Ethiopia. After controlling for potential confounders, age at first birth, history of multiple pregnancies, place of delivery, prior pelvic surgery and history of instrumental delivery were found to be potential determinants of UVP.
The findings of this study revealed that women aged less than 20 years with a first child had a 3.9-fold greater chance of developing UVP than their counterparts did. This finding is in agreement with findings from a public referral hospital in the Amhara region and Nepal (26, 27). This might be because the supportive ligament may not mature and may not be strong enough to avoid prolapse of the pelvic muscle below the age of 20. Additionally, findings from Kathmandu, Nepal, revealed that having a child under the age of 20 years was associated with the development of UVP; accordingly, the study cited a possible reason for poor decisions related to personal well-being. Because of poor decisions, women under the age of 20 are unable to discontinue uterine prolapse risk behaviors (28). The possible justification could be that child birth through the vagina at a young age may involve prolonged or obstructed labor that may injure the pelvic floor fascia and muscles.
In this study, women who had a history of multiple pregnancies were 2.8 times more likely to develop UVP than their counterparts were. This finding is congruent with other studies from Bahir Dar, Southeast Nigeria, Pakistan and Turkey (29–32). Another study conducted to assess the morphological characteristics of the pelvic floor musculature between women with twin pregnancies and those with singleton pregnancies revealed that pelvic support undergoes greater changes during twin pregnancy (33). Multiple pregnancies or twin pregnancies can damage the sphincter muscles and ligaments. The possible justification could be that multiple pregnancies may face repeated cycles of stretching and straining during labor to the pelvic floor, which may lead to muscle tone and ligament weakening.
This study revealed that women who delivered at home were 4.9 times more likely to develop UVP than those who delivered at health institutions were. This finding is in line with other findings from Southwest Ethiopia, Wolayta Sodo, South Ethiopia, Tanzania and Nepali (34–37). This finding was also supported by a pooled analysis conducted in Ethiopia, where home delivery resulted in the development of UVP due to a greater risk of prolonged labor and perinatal tears (38). Prolonged labor is a well-established cause of UVP. When the fetal head applies pressure to the pelvic floor for prolonged periods during its engagement in the birth cannula, the pelvic floor muscle, tissue, nerve, and other supporting structures are damaged. This condition may result in the downward displacement of the pelvic organs from their normal position (39). Another possible reason is that home delivery by unskilled attendants causes significant damage to the pelvic support system. This condition may also result in UVP as a long-term complication (27). The possible reasons could be recently home delivery conducted in Ethiopia without skilled birth attends that usually services provided by traditional birth attends or grandmother that may cause improper management of labour that can lead prolong labour/pushing greatly, overstretch and damage in pelvic floor fascia, nerves and muscles. In health facility settings typically employ continuous fetal monitoring, have immediate access to obstetric interventions, and often follow time-bound labor management protocols. In contrast, home delivery may allow for more neglected labor management and may take long durations and less intervention approaches. These factors could influence not only maternal perceptions of the birth experience but also the physiological outcomes observed.
In this study, women who had prior pelvic surgery were 3.9 times more likely to develop UVP. This finding is consistent with findings from Asella Teaching and References Hospital and England (40, 41). Another study from the American College of Obstetricians and Gynecologists revealed that women who underwent primary UVP surgery had an approximately 30%–50% chance of needing a second prolapse surgery (42). This might be because of a high likelihood of pelvic floor muscle injury during surgical procedures. The other reason could be that previous pelvic surgery may weaken ligaments and alter the structures that may reduce pelvic floor strength.
The odds of having UVP were 3.1 times greater among those with a history of instrumental delivery than among their counterparts. These findings were supported by a study conducted in Nekemte, Western Ethiopia (23). This was explained by the fact that forceps delivery is associated with muscle trauma, which results in pelvic floor muscle damage (38). However, this finding was not supported by a meta-analysis conducted in Ethiopia, which revealed no significant difference in UVP between assisted vaginal delivery (including vacuum and forceps) and spontaneous vaginal delivery (43). This was because, according to the pooled estimates, no significant association was found between vacuum delivery and primary UVP (43, 44). The reason could be that prolonged labor pushing, which may precede forceps delivery, may weaken tissues and may cause compression and traction during the prolonged second stage and instrumental extraction, which may lead to trauma to the pelvic floor muscle and fascia.
Implications of the study
The study of risk factors for utero-vaginal prolapse (UVP) among women visiting gynecologic outpatient departments in the Sidama region provides crucial insights into risk factors and potential intervention points for addressing this public health issue. The key implications of these findings are as follows: public health significance implications for women in the early age group and women with multiple births identified as risk factors. We hope these findings provide insight into the design of tailored interventions for most vulnerable groups. In addition, our findings demonstrated that strengthening early screening to detect risk factors is critical to address this problem, so it has clinical practice implications. Furthermore, our findings suggest that strengthening maternal health and obstetric care, such as skilled delivery services, to prevent home delivery and promoting the use of contraceptives to reduce high parity may lead to a reduction in the burden of UVP. These findings underscore policy and program implications. In addition, policymakers should prioritize health education campaigns targeting women and communities to increase awareness of risk factors for uterovaginal prolapse. Therefore, designing tailored interventions for at-risk groups is a nondoubtful action to enhance maternal health and well-being.
Strengths and limitations of the study
In this study, researchers included multiple health facilities, which could help to obtain adequate sample sizes. This study has various limitations, such as the fact that some obstetric characteristics were reported by patients who may have long durations since the patients were asked about their previous history, which may have led to recall bias. Moreover, the study was conducted at a hospital-based scale and did not include a specific population or community; therefore, it may be difficult to generalize the findings to the entire community. In addition, the study did not assess nutritional status.
Conclusion
The current study highlights that pertinent risk factors, such as socio-demographic, obstetric & gynecologic and medical and personal factors, were identified as key determinants of UVP. These findings may require the attention of policy makers to alleviate this problem. Moreover, health professionals should counsel about the consequences and complications of early childbirth, multiple pregnancies, instrumental delivery and the effects of home delivery and their associations with UVP development. In addition, prevention strategies such as pelvic floor muscle training and elective cesarean section for women who are at high risk are recommended to address this problem.
We would like to express our deepest gratitude to Yanet-Liyana College of Health Sciences, Department of Reproductive Health, for providing ethical clearance to conduct this study. Our deepest gratitude goes to Adare, Yirgalem, HUCSH and Leku General Hospital for their support and facilitation during our data collection. We appreciate the study participants who voluntarily participated in the study. We acknowledge our data collectors and supervisors who took part in data collection in the field.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethical approval was obtained from the research review committee of Yanet-Liyana Health Science College (Ref: LHC/YLCH/OGL/1080/15 and Date: 24/07/2023). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing, Supervision. TA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Funding acquisition. MM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing, Funding acquisition, Supervision. AA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issue please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380(9859):2163–96. doi: 10.1016/S0140-6736(12)61729-2
3. Sumathi N, Nandhini CJ. Uterovaginal prolapse-a study in south Indian women. Sch J Appl Med Sci. (2017) 5(4F):1698–704. doi: 10.36347/sjams.2017.v05i04.090
5. Wang B, Chen Y, Zhu X, Wang T, Li M, Huang Y, et al. Global burden and trends of pelvic organ prolapse associated with aging women: an observational trend study from 1990 to 2019. Front Public Health. (2022) 10:975829. doi: 10.3389/fpubh.2022.975829
6. Haylen BT, Ridder DD, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. (2010) 29(1):4–20. doi: 10.1002/nau.20798
7. Brown HW, Hegde A, Huebner M, Neels H, Barnes HC, Marquini GV, et al. International urogynecology consultation chapter 1 committee 2: epidemiology of pelvic organ prolapse: prevalence, incidence, natural history, and service needs. Int Urogynecol J. (2022) 33(2):173–87. doi: 10.1007/s00192-021-05018-z
8. Walker GJ, Gunasekera P. Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J. (2011) 22:127–35. doi: 10.1007/s00192-010-1215-0
9. Gedefaw G, Demis A. Burden of pelvic organ prolapse in Ethiopia: a systematic review and meta-analysis. BMC Womens Health. (2020) 20(1):1–9. doi: 10.1186/s12905-020-01039-w
10. Akmel M, Segni H. Pelvic organ prolapse in Jimma university specialized hospital, southwest Ethiopia. Ethiop J Health Sci. (2012) 22(2):85–92.22876071
11. Gaym A. Elective hysterectomy at Tikur Anbessa teaching hospital, Addis Ababa. Ethiop Med J. (2002) 40(3):217–26.12602245
13. Buchsbaum GM, Duecy EE, Kerr LA, Huang LS, Perevich M, Guzick DS. Pelvic organ prolapse in nulliparous women and their parous sisters. Obstet Gynecol. (2006) 108(6):1388–3. doi: 10.1097/01.AOG.0000245784.31082.ed
14. Bijalwan RP, Bhagavatula M, Semwal VD, Rawat P, Anand V. Morbidity of uterine prolapsed among the women in the Chakrata block of Dehradun district. Indian J Community Health. (2015) 27(1):103–9. https://iapsmupuk.org/journal/index.php/IJCH/article/view/540/540
15. Fritel X, Varnoux N, Zins M, Breart G, Ringa VJ. Symptomatic pelvic organ prolapse at midlife, quality of life, and risk factors. Obstet Gynecol. (2009) 113(3):609. doi: 10.1097/AOG.0b013e3181985312
16. Sidama Region Finance Bureau. Sidama Region Development Corporation Planning and Statistics. Hawassa: SRFB (2020).
17. Sidama Regional Health Bureau. Annual Regional Health Bureau Report. Hawassa: SRHB (2023). p. 1–3.
19. Hawassa University. College of Medicine and Health Science Data. Hawassa: Hawassa Referral Hospital (2023).
22. Fahim NK, Negida A, Fahim AK. Sample size calculation guide - part 3: how to calculate the sample size for an independent case‒control study. Adv J Emerg Med. (2019) 3(2):e20. doi: 10.22114/AJEM.v0i0.138
23. Firdisa G, Tilahun T, Kejela GJ. Determinants of uterovaginal prolapse in western Ethiopia. Int Urogynecol J. (2022) 33(2):421–9. doi: 10.1007/s00192-021-04883-y
24. Li Z, Xu T, Li Z, Gong J, Liu Q, Zhu L. An epidemiologic study of pelvic organ prolapse in rural Chinese women: a population-based sample in China. Int Urogynecol J. (2019) 30(11):1925–32. doi: 10.1007/s00192-018-03859-9
25. Zimmerman DW. Teacher’s corner: a note on interpretation of the paired-samples t-test. J Educ Behav Stat. (1997) 22(3):349–60. doi: 10.3102/10769986022003349
26. Thapa B, Rana G, Gurung S. Contributing factors of utero-vaginal prolapse among women attending in Bharatpur hospital. Js Chitwan Med Coll. (2014) 4(3):38–42. doi: 10.3126/jcmc.v4i3.11939
27. Sirage N, Hailu D, Kahsay T, Amaje E. Determinants of pelvic organ prolapse among gynecologic patients attending public referral hospitals in Amhara region, Ethiopia, 2020: institution-based unmatched case‒control study design. SAGE Open Med. (2022) 10:20503121221094182. doi: 10.1177/20503121221094182
28. Pokharel B, Jain V, Gupta N. Study on factors contributing uterine prolapse among women attending gynecology opd in Kathmandu, Nepal. Int J Heal Sci Res. (2016) 6(1):387–91.
29. Eleje G, Udegbunam O, Ofojebe C, Adichie C. Determinants and management outcomes of pelvic organ prolapse in a low resource setting. Ann Med Health Sci Res. (2014) 4(5):796–801. doi: 10.4103/2141-9248.141578
30. Asresie A, Admassu E, Setegn T. Determinants of pelvic organ prolapse among gynecologic patients in bahir dar, north west Ethiopia: a case–control study. Int J Womens Health. (2016) 8:713–9. doi: 10.2147/IJWH.S122459
31. Jokhio AH, Rizvi RM, MacArthur C. Prevalence of pelvic organ prolapse in women, associated factors and impact on quality of life in rural Pakistan: population-based study. BMC Womens Health. (2020) 20(1):1–7. doi: 10.1186/s12905-020-00934-6
32. Aytan H, Ertunç D, Tok EC, Yaşa O, Nazik H. Prevalence of pelvic organ prolapse and related factors in a general female population. Turk J Obstet Gynecol. (2014) 11(3):176. doi: 10.4274/tjod.90582
33. Kubotani JS, Júnior EA, Zanetti MRD, Passos JP, de Jármy Di Bella ZIK, Júnior JE. Assessing the impact of twin pregnancies on the pelvic floor using 3-dimensional sonography: a pilot study. J Ultrasound Med. (2014) 33(7):1179–83. doi: 10.7863/ultra.33.7.1179
34. Badacho AS, Lelu MA, Gelan Z, Woltamo DD. Uterine prolapse and associated factors among reproductive-age women in south‒west Ethiopia: a community-based cross-sectional study. PLoS One. (2022) 17(1):e0262077. doi: 10.1371/journal.pone.0262077
35. Lema Z, Meskele YBM. Determinants of pelvic organ prolapse among gynecological cases in Wolaita Sodo university referral teaching hospital, southern Ethiopia: a case‒control study. J Biol Agric Healthc. (2015) 5(21):1–10. https://core.ac.uk/download/pdf/234661779.pdf
36. Sharma A, Zhang JP. Risk factors and symptoms of uterine prolapse: reality of Nepali women. Asian Women. (2014) 30(1):81–95. doi: 10.14431/aw.2014.03.30.1.81
37. Masenga GG, Shayo BC, Rasch V. Prevalence and risk factors for pelvic organ prolapse in Kilimanjaro, Tanzania: a population based study in Tanzanian rural community. PLoS One. (2018) 13(4):e0195910. doi: 10.1371/journal.pone.0195910
38. Addisu D, Mekie M, Belachew YY, Degu A, Gebeyehu NA. The prevalence of pelvic organ prolapse and associated factors in Ethiopia: a systematic review and meta-analysis. Front Med (Lausanne). (2023) 10:1193069. doi: 10.3389/fmed.2023.1193069
39. Marsoosi V, Jamal A, Eslamian L, Oveisi S, Abotorabi S. Prolonged second stage of labor and levator ani muscle injuries. Glob J Health Sci. (2015) 7(1):267. doi: 10.5539/gjhs.v7n1p267
40. Obsa MS, Worji TA, Kedir NA, Kute NG. Risk factors for pelvic organ prolapse at asella teaching and referral hospital: unmatched case control study. Front Glob Womens Health. (2022) 3:833823. doi: 10.3389/fgwh.2022.833823
41. Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford family planning association study. BJOG. (1997) 104(5):579–85. doi: 10.1111/j.1471-0528.1997.tb11536.x
42. American College of Obstetricians and Gynecologists and the American Urogynecologic Society; INTERIM UPDATE: This Practice Bulletin is updated as highlighted to reflect the US Food and Drug Administration order to stop the sale of transvaginal synthetic mesh products for the repair of pelvic organ prolapse. Pelvic organ prolapse. Female Pelvic Med Reconstr Surg. (2019) 25(6):397–408. doi: 10.1097/SPV.0000000000000794
43. Leng B, Zhou Y, Du S, Liu F, Zhao L, Sun G, et al. Association between delivery mode and pelvic organ prolapse: a meta-analysis of observational studies. Eur J Obstet Gynecol Reprod Biol. (2019) 235:19–25. doi: 10.1016/j.ejogrb.2019.01.031
Keywords: gynecological outpatient, risk factors, uterine prolapse, women, case control design, public hospitals
Citation: Yosef H, Alemu T, Mengesha MW and Adule A (2025) Risk factors for uterovaginal prolapse among women in public hospitals of Sidama, Ethiopia: a case control study. Front. Reprod. Health 7:1569449. doi: 10.3389/frph.2025.1569449
Received: 31 January 2025; Accepted: 29 August 2025;
Published: 18 September 2025.
Edited by:
Rebekka Einenkel, University of Bonn, GermanyReviewed by:
Azna Zuberi, Northwestern University, United StatesDaniel Berhanie Enyew, Dan, Ethiopia
Copyright: © 2025 Yosef, Alemu, Mengesha and Adule. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tsegaye Alemu, dHNlZ2F5ZWE0OUBnbWFpbC5jb20=
†ORCID:
Tsegaye Alemu
orcid.org/0000-0001-5911-9028
 Hirut Yosef1
Hirut Yosef1 Tsegaye Alemu
Tsegaye Alemu Mekdes Wondirad Mengesha
Mekdes Wondirad Mengesha