- Department of Epidemiology and Biostatistics, School of Public Health Makerere University, Kampala, Uganda
Background: Adolescent girls and young women (AGYW) in Uganda face a disproportionate burden of HIV and unintended pregnancies, with low condom use exacerbating these risks. Despite efforts to promote condom use, uptake remains inconsistent among this young demographic. Additionally, there is limited research on the factors influencing condom use among unmarried sexually active AGYW in Uganda. This study aimed to assess the prevalence and factors associated with condom use in this high-risk group using data from the 2016 Uganda Demographic and Health Survey (UDHS), to inform targeted interventions aimed at improving sexual health outcomes for this specific demographic.
Methods: A cross-sectional analysis was conducted using secondary data from the 2016 UDHS. The study included 2,132 unmarried sexually active AGYW aged 15–24. Data were analyzed using weighted logistic regression to identify factors associated with condom use, adjusting for survey design characteristics. The outcome of interest was condom use and some of the potential predictor variables examined were; age, region, education, wealth, marital status, and exposure to family planning messages. All data processing and analysis was done using STATA v14.
Results: Only 10.36% of AGYW participants reported using condoms. Factors significantly associated with condom use included region (lower use in Northern and Western regions), marital status (lower use among those ever in a union), exposure to family planning messages (higher use), and having multiple sexual partners (higher use). Recent sexual activity was also linked to increased condom use.
Conclusions/Recommendations: The low prevalence of condom use highlights the urgent need for targeted interventions to address barriers such as regional disparities, limited access to sexual health education, and gender dynamics. Recommendations include implementing region-specific sexual health programs, expanding family planning messaging, and establishing youth-friendly health services. Empowering AGYW to negotiate condom use and addressing socio-economic barriers are crucial for improving sexual health outcomes.
Introduction
Globally, adolescent girls and young women (AGYW) continue to bear a disproportionate burden of HIV. In 2019, despite making up only 10% of the population, AGYW aged 15–24 years in sub-Saharan Africa accounted for 24% of new HIV infections (1). This highlights the urgent need for innovative HIV prevention strategies to curb the epidemic within this vulnerable population (2). The vulnerability of adolescent girls and young women (AGYW) to HIV is shaped by a complex interplay of biological, behavioral, social, and structural factors (3). Proximally, the presence of sexually transmitted infections (STIs) increases HIV incidence among young women. Behaviorally, engaging in transactional sex, having multiple sexual partners, substance abuse, and inconsistent condom use elevate their risk of infection (3). Additionally, structural determinants such as parental loss and lack of access to education further contribute to HIV susceptibility (3).
Condom use plays a crucial role in preventing both sexually transmitted infections (STIs), including HIV, and unintended pregnancies, particularly among sexually active individuals (4, 5). When used consistently and correctly, male latex condoms significantly reduce the risk of HIV and other STIs (6). Epidemiological research supports their effectiveness, showing that current HIV prevalence rates would be approximately five times higher without condom use (4). Additionally, condoms provide strong protection against STIs transmitted through genital fluids, such as gonorrhea, chlamydia, and trichomoniasis, further emphasizing their importance in sexual and reproductive health (4).
Uganda has one of the highest adolescent fertility rates in sub-Saharan Africa, with approximately 24% of girls aged 15–19 having begun childbearing in 2022 (7). Additionally, Uganda has a generalized HIV epidemic, with AGYW disproportionately affected. The HIV prevalence among adolescent girls and young women (AGYW) aged 15–24 years is 3.3%, compared to 0.8% among young men (8).
Inconsistent and low use of condoms is one of the main drivers of HIV infection, other sexually transmitted infections (STIs), and unintended pregnancies, particularly among adolescent girls and young women (AGYW) who are at high risk (4). In Uganda, efforts by the government and development partners to promote condom use among AGYW include the provision of free condoms in health facilities, schools, and community centers, as well as HIV counseling and testing services, sexual health education programs, and outreach sensitization campaigns. Despite these efforts, condom use among AGYW remains low (9). This low prevalence of condom use is concerning, given the high rates of HIV and STIs among AGYW in Uganda (8).
Multiple socio-demographic and behavioral factors influence condom use among sexually active AGYW. Studies have shown that age plays a role, with older AGYW (20–24 years) more likely to use condoms compared to younger adolescents (15–19 years), potentially due to greater autonomy and awareness of reproductive health risks (10). Additionally, education level is a significant determinant, with higher levels of education associated with increased condom use due to better access to information on contraception and STI prevention (11, 12). Other factors include economic status, place of residence, number of sexual partners, religion, media exposure, partners influence and substance use (9–11, 13).
Despite the availability of condoms and ongoing efforts to promote their use, there is limited research on the factors influencing condom use among unmarried sexually active AGYW in Uganda. Existing studies often aggregate data across different age groups or marital statuses, which may obscure the unique challenges faced by this demographic. This study aims to investigate the prevalence of condom use among unmarried sexually active young women aged 15–24 years in Uganda and the factors influencing their use, utilizing data from the 2016 UDHS. By addressing these gaps, this research will inform targeted interventions aimed at improving sexual health outcomes among AGYW in Uganda.
Methods
Study design
This was a cross sectional study using secondary data from the 2016 Uganda Demographic Health Survey.
Dependent (outcome variable)
The outcome variable was condom use, which was generated from the variable V312 (Current contraceptive method) in the UDHS 2016 women dataset. DHS experts generally use this variable to estimate the prevalence of condom use among women of reproductive age (12). Condom use variable was coded “yes” if young women declared condom use during the last 4 months preceding the survey, and “no” otherwise. See Table 1 for description and recoding.
Potential predictor variables
The study examines several predictor variables associated with condom use among unmarried sexually active young women aged 15–24 years in Uganda. Age is categorized into two groups: (15–19) and (20–24). Region is divided into (Central, Eastern, Northern, and Western). Place of residence is classified as (Urban and Rural). Religion includes (Anglican, Catholic, Muslim, Pentecostal/Born Again, and Others). Highest level of education is categorized into (No education, Primary, Secondary, and Higher). Wealth index is classified into five levels: (Lowest, Second, Middle, Fourth, and Highest). Ever in union refers to marital status and is divided into (No and Yes). Currently working distinguishes between (No and Yes). Family planning (FP) message exposure is classified as (No and Yes), while FP knowledge is also categorized as (No and Yes). Knowledge of the ovulatory cycle is grouped into (No and Yes). Sexual partners in the last 12 months include (No partner, 1 partner, and 2 or more partners). Recent sexual activity is categorized into (Active last 4 weeks and Not active last 4 weeks). HIV testing history is classified as (No and Yes). Awareness of sexually transmitted infections (STIs) is categorized as (No and Yes). Finally, cigarette or tobacco use is classified into (No and Yes). See Table 1 for full description and re-categorization of the above predictor variables.
Sample design
The 2016 UDHS used the sampling frame of the Uganda National Population and Housing Census (NPHC), conducted in 2014. The census frame is a complete list of all census enumeration areas (EAs) created for the 2014 NPHC. During the NPHC Uganda was divided administratively into 112 districts, these were grouped into 15 regions for this survey. Three special areas, the Lake Victoria islands, the mountain districts, and greater Kampala, were also considered.
The sample was stratified and selected in two stages. In the first stage, 697 EAs (162 and 535 EAs in urban and rural areas respectively) were selected from the 2014 Uganda NPHC. The second stage of sampling constituted households. In each of the 696 accessible selected EAs, a household listing was conducted, and to reduce the workload, any large EA with more than 300 households was segmented for the 2016 UDHS.
A total of 20,880 households were selected for the 2016 UDHS, with 30 households randomly chosen from each enumeration area (EA) or EA segment to ensure representativeness.
Sampling size calculation
A representative sample of 20,880 households was randomly selected for the 2016 Uganda DHS, with 19,088 eligible women being identified. Interviews were completed with 18,506 (97.0%) women and of 18,506 women, 8,058 were adolescent girls and young women aged 15–24. All adolescent girls who were married or living with partners (n = 3,328) were excluded from the analysis. Additionally, adolescent girls and young women who reported not being sexually active (n = 2,597) were also removed. One observation with missing data for the variable recent sexual activity was dropped (n = 1). After these exclusions, the final sample of adolescent girls and young women who met the inclusion criteria for the analysis consisted of 2,132 participants.
Inclusion and exclusion criteria
Inclusion criteria
All Ugandan adolescent girls and young women (15–24) years who were either permanent residents of the selected households or visitors who stayed in the household the night before the survey were eligible to participate.
Exclusion criteria
Any adolescent girls and young women (15–24) who are married, living with partners and have never had sex were excluded from the analysis.
Any adolescent girls and young women (15–24) with missing data were also exclude from the analysis.
Data management and analysis
Data management
The 2016 Uganda Demographic and Health Survey (UDHS) dataset was used for this study, specifically the women's dataset (UGIR7AFL.DTA) for women aged 15–49. The Standard Recode Manual for DHS7 was consulted to understand how the variables were collected and coded. This manual provided guidance on the structure of the dataset, the meaning of variable codes, and the methodology used during data collection.
To ensure data completeness and accuracy, code booking and tabulation of the variables of interest were conducted. This process involved checking the frequency and distribution of each variable to identify any missing or inconsistent data. The variables were categorized as either continuous or categorical and their respective ranges or categories were documented. This step was crucial for understanding the dataset and preparing it for analysis. Some of the variables of interest were recoded and renamed before analysis.
All outcome and potential predictor variables were checked for duplicates and assessed for missing values prior to analysis. Only variables with complete data were included in the final analysis. Data processing and analysis were conducted using STATA version 14.
Univariable analysis
The analysis began by declaring the survey design characteristics using the command “svyset” to account for complex survey design [weighting (wgt), clustering (v021), stratification (v023) were used]. Unweighted frequencies and percentages for the different categories of the variables were obtained through tabulation. Weighted percentages were then calculated by adding the “svy” prefix to the tabulation command, ensuring that the results were representative of the population.
Bivariable analysis
The bivariable analysis aimed to assess the association between each independent variable and the outcome variable (condom use). Weighted cross-tabulations of the outcome variable and each independent variable were conducted to obtain weighted percentages of women who used condoms as form of contraceptive.
Binary logistic regression was used for bivariable analysis to obtain crude odds ratios (CORs), 95% confidence intervals (CIs), and p-values. The “svy” prefix was used to account for the survey design. A significance threshold of p < 0.25 was used at this stage to ensure that potentially important variables were not excluded prematurely. This threshold allowed for the inclusion of variables that might show significance when adjusted for other factors in the multivariable analysis.
The bivariable analysis provided initial insights into the factors associated with condom use, guiding the selection of variables for the multivariable model.
Multivariable analysis
All independent variables that were statistically significant in the bivariable analysis were assessed for multicollinearity prior to inclusion in the multivariable model. Multicollinearity was examined using the “correlate” command in STATA, and a correlation coefficient of 0.4 or higher was considered indicative of high multicollinearity. In cases where two or more variables were highly correlated, one variable was excluded from the multivariable analysis based on prior literature and the strength of association observed in the bivariable analysis.
The multivariable analysis aimed to identify the independent predictors of condom use while controlling for potential confounding factors. Binary logistic regression was used, and the backward elimination method was employed to build the final model. Variables with the least significance (based on p < 0.05) were removed step-by-step. This method ensured that only the most significant predictors remained in the final model.
The goodness of fit of the final model was tested using the “estat gof” command, which yielded a Prob > F = 0.7132, indicating that the model fit the data well. The “svy” prefix was used throughout the regression analysis to account for the survey design.
Results
Background characteristics of unmarried sexually active adolescent girls and young women (15–24)
Table 2 presents the socio-demographic characteristics of unmarried sexually active adolescent girls and young women aged 15–24 years in Uganda. The sample size was 2,132; with 50.75% aged 15–19 and 49.25% aged 20–24. Geographically, 36.38% resided in the Central region, 27.56% in the Eastern region, 15.93% in the Northern region, and 20.13% in the Western region. The majority (67.71%) lived in rural areas. By religious affiliation, 31.36% were Anglican, 38.29% Catholic, 14.10% Muslim, and 13.87% Pentecostal/Born Again. Educationally, 48.82% had primary education, 38.78% secondary, and 11.16% higher education. Wealth distribution showed 34.19% in the highest wealth quintile and 12.28% in the lowest. Additionally, 75.85% had never been in a union, 63.79% were currently working, and 70.73% had exposure to family planning (FP) messages. Knowledge of FP was nearly universal (99.35%), and 85.69% knew their ovulatory cycle. Regarding sexual behavior, 69.52% had one sexual partner in the last 12 months, and 20.16% were sexually active in the last 4 weeks. HIV testing was reported by 82.91%, and 99.86% had heard of STIs. Only 10.36% reported using condoms during their sexual intercourse.
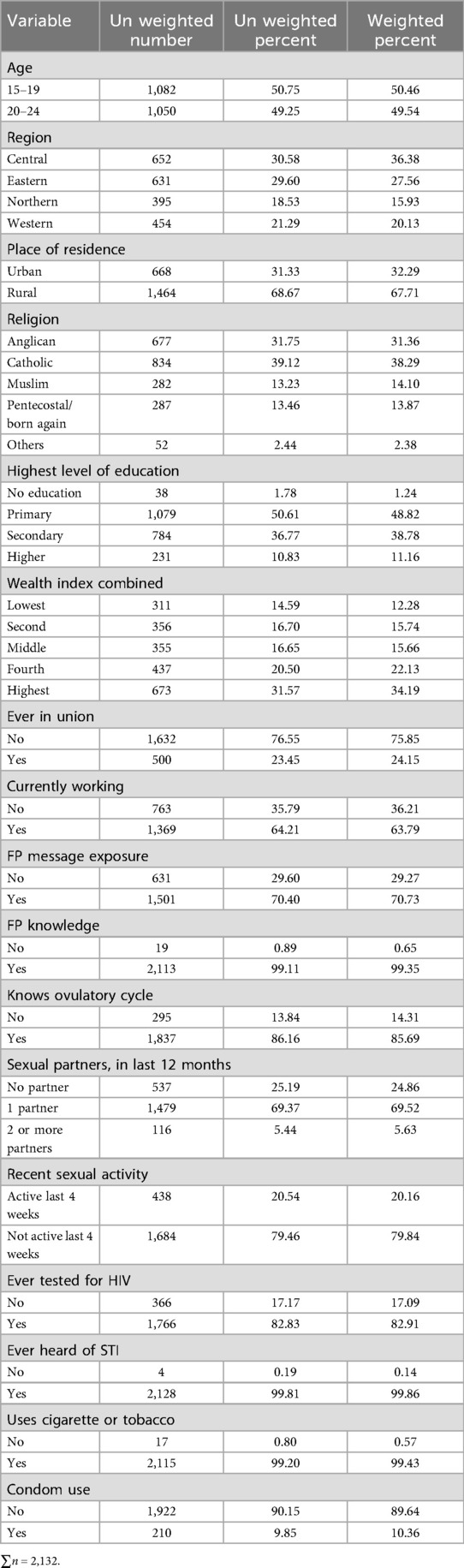
Table 2. The socio-demographic characteristics of single sexually active adolescent girls and young women (15–24).
Prevalence of condom use by socio-demographic characteristics of unmarried sexually active adolescent girls and young women (15–24)
Table 3 shows the prevalence of condom use and crude odds ratios (CORs) by socio-demographic characteristics. Condom use was significantly lower in the Northern (0.84%) and Western (1.19%) regions compared to the Central region (4.64%) (p < 0.01). Rural residents had lower condom use (5.98%) compared to urban residents (4.38%) (p < 0.01). Women with primary education had significantly lower condom use (2.65%) compared to those with higher education (1.98%) (p < 0.001). Women who had ever been in a union had lower condom use (1.14%) compared to those who had never been in a union (9.22%) (p < 0.01). Exposure to FP messages was associated with higher condom use (8.4%) compared to no exposure (1.96%) (p < 0.01). Women with one sexual partner (8.96%) or multiple partners (1.00%) in the last 12 months had significantly higher condom use compared to those with no partner (0.39%) (p < 0.001). Recent sexual activity in the last 4 weeks was associated with higher condom use (4.00%) compared to no recent activity (6.36%) (p < 0.001).
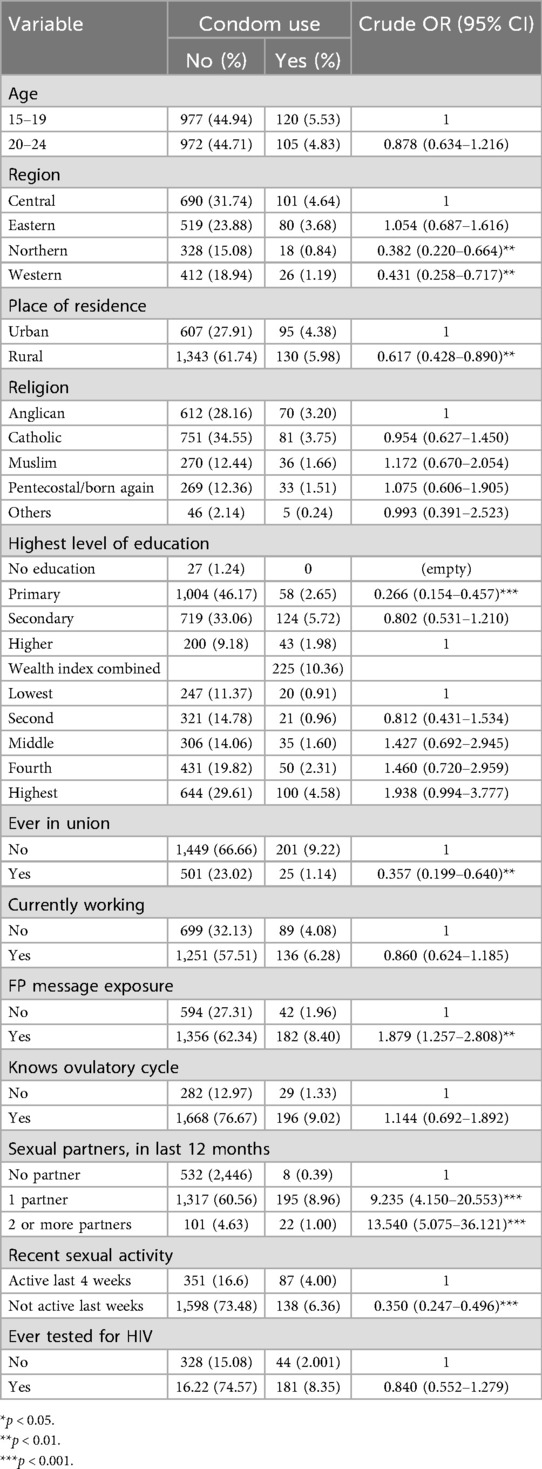
Table 3. Prevalence of condom use by socio-demographic characteristics of single sexually active adolescent girls and young women (15–24) and the crude odds ratios (CORs).
Factors associated with condom use among unmarried sexually active adolescent girls and young women (15–24)
Table 4 presents the adjusted odds ratios (AORs) from the multivariable logistic regression. Women in the Northern (AOR = 0.512, 95% CI: 0.281–0.930) and Western (AOR = 0.489, 95% CI: 0.283–0.843) regions had significantly lower odds of condom use compared to the Central region (p < 0.01). Women who had ever been in a union had lower odds of condom use (AOR = 0.346, 95% CI: 0.188–0.634) compared to those who had never been in a union (p < 0.01). Exposure to FP messages was associated with higher odds of condom use (AOR = 1.669, 95% CI: 1.108–2.512) (p < 0.01). Women with one sexual partner (AOR = 8.102, 95% CI: 3.607–18.201) or multiple partners (AOR = 9.961, 95% CI: 3.668–27.051) in the last 12 months had significantly higher odds of condom use compared to those with no partner (p < 0.001). Not being sexually activity in the last 4 weeks was associated with lower odds of condom use (AOR = 0.504, 95% CI: 0.354-0.719) compared to being sexually active in the last 4 weeks (p < 0.001).
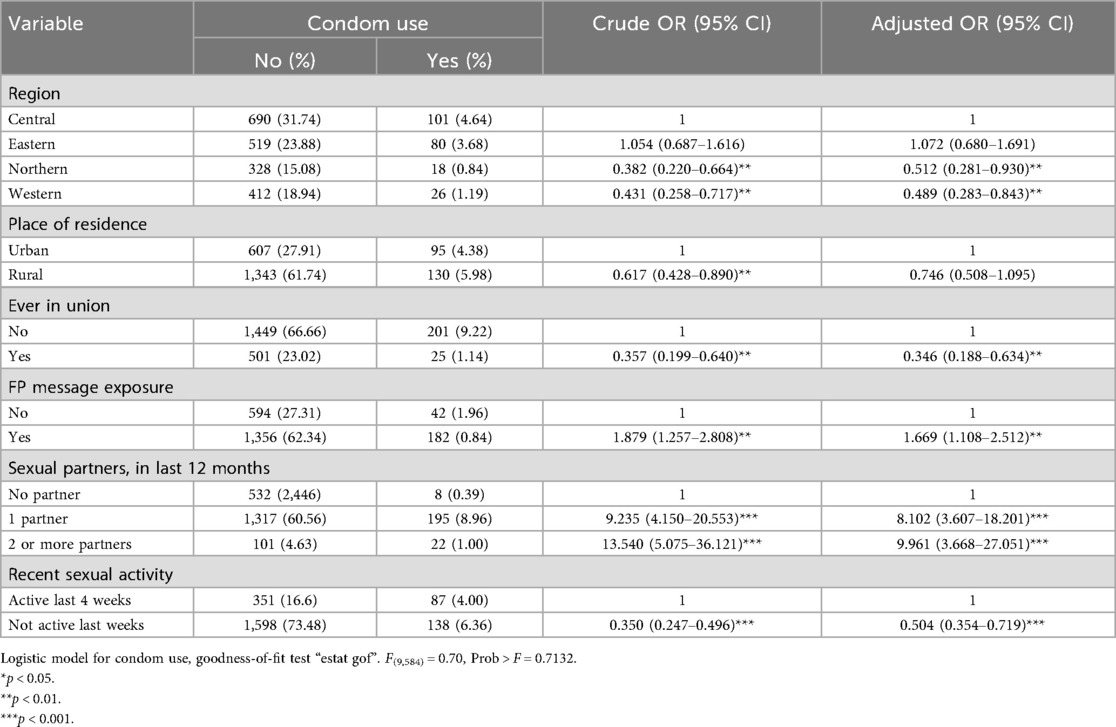
Table 4. Weighted modified logistic regression estimates for condom use by socio-demographic characteristics of single sexually active adolescent girls and young women (15–24) and the adjusted odds ratios (AORs).
Discussion
This study aimed to determine the factors associated with condom use among unmarried sexually active young women aged 15–24 years in Uganda, using data from the 2016 Uganda Demographic and Health Survey (UDHS). The findings revealed a low overall prevalence of condom use among this high-risk population, with notable differences across regions, relationship histories, and behavioral factors. Condom use was more likely among women recently sexually active, those with multiple sexual partners, and those exposed to family planning messages. Conversely, lower condom use was observed among women who had ever been in a union and those living in certain regions. These findings highlight key behavioral and contextual factors that must be addressed to improve protective sexual practices among young Ugandan women.
The analysis revealed that only 10.36% of the participants reported using condoms, highlighting a significant gap in the adoption of protective sexual health practices among this high-risk group. This finding is lower than the prevalence reported in other sub-Saharan African countries, such as Malawi, where 18.5% of young women reported condom use 4 months prior to the survey (14), and Haiti, where 15.4% of sexually active young women reported condom use (11). The low prevalence of condom use in Uganda underscores the urgent need for targeted interventions to address the barriers to condom use among young women, particularly in the context of high HIV prevalence and unintended pregnancies (15).
The study found significant regional disparities in condom use, with lower usage in the Northern and Western regions compared to the Central region. This aligns with findings from Tanzania, where regional variations in condom use were attributed to differences in access to sexual health services and cultural norms (16). The Northern and Western regions of Uganda may face similar challenges, such as limited healthcare infrastructure and conservative cultural attitudes toward condom use. These findings underscore the need for region-specific interventions to address barriers to condom use, particularly in underserved areas.
Women who had ever been in a union had lower odds of condom use, consistent with studies from Malawi and Ethiopia that found married individuals are less likely to use condoms due to perceived lower STI risk within marital relationships (14, 17, 18). However, this perception can increase vulnerability to STIs, particularly in non-monogamous relationships. Interventions should focus on promoting condom use within marital relationships, emphasizing the importance of dual protection against STIs and unintended pregnancies.
Exposure to FP messages was associated with higher condom use, consistent with findings from Nigeria and Malawi (10, 12), that emphasize the role FP messages and media exposure in promoting awareness of the benefits of condom use and provide information on how to access condoms. Expanding FP messaging through media and community outreach programs could further enhance condom use among young women.
Women with one or more sexual partners in the last 12 months had significantly higher odds of condom use, consistent with studies from Brazil, Haiti and Uganda (4, 11, 19). This suggests that women with multiple partners may be more aware of the risks associated with unprotected sex. However, the low overall prevalence of condom use (10.36%) indicates that many young women remain at risk. Interventions should focus on promoting consistent condom use, particularly among women with multiple partners.
Recent sexual activity in the last 4 weeks was associated with higher condom use, consistent with findings from Uganda (9), that found a correlation between sexual contact and condom use. This may reflect increased awareness of the need for protection during recent sexual encounters. However, the low prevalence (4%) of condom use among women who were recently sexually active suggests that many women may not perceive the need for consistent condom use. Public health campaigns should emphasize the importance of consistent condom use, regardless of recent sexual activity.
Study strengths
This study utilized data from the 2016 Uganda Demographic and Health Survey (UDHS), which is a nationally representative dataset. This ensures that the findings are generalizable to the broader population of unmarried sexually active young women aged 15–24 years in Uganda.
The study included a large sample size of 2,132 participants, which enhances the statistical power and reliability of the results. This allows for more analyses that are robust and the identification of significant associations between variables.
The study employed a multivariable logistic regression model will adjusting for survey design characteristics, which offers more accurate estimates and allows accurate understanding of the predictors of condom use.
By focusing on unmarried sexually active young women, the study addresses a high-risk group that is often overlooked in broader sexual health research. This targeted approach provides valuable insights for designing interventions tailored to this demographic.
Study limitations
The study is based on cross-sectional data, which limits the ability to establish causal relationships between the variables.
The data on condom use and sexual behavior were self-reported, which may be subject to social desirability bias. Participants may underreport risky sexual behaviors or over report condom use, leading to potential inaccuracies in the findings.
The study relies solely on quantitative data, which does not provide deeper insights into the barriers and facilitators of condom use among young women in Uganda.
The study focuses exclusively on young women and does not include the perspectives of their male partners. Given the role of gender dynamics in sexual decision-making, understanding male attitudes and behaviors could provide a more comprehensive picture of condom use.
Conclusion
This study highlights the persistently low uptake of condoms among unmarried sexually active adolescent girls and young women (AGYW) in Uganda, underscoring a critical public health concern. The analysis identified key behavioral and contextual factors influencing condom use, suggesting the need for targeted, context-specific interventions. Enhancing access to comprehensive sexual and reproductive health education, particularly through mass media, schools, and community outreach, can play a pivotal role in increasing awareness and acceptance of condom use. Moreover, empowering AGYW with the skills and agency to negotiate safer sexual practices is essential to reducing the risks of HIV, other sexually transmitted infections, and unintended pregnancies. Policymakers and program implementers must prioritize inclusive, youth-friendly strategies that address the unique barriers faced by this population, with particular attention to regional and sociocultural disparities. Strengthening these efforts is vital for advancing sexual and reproductive health outcomes and promoting the well-being of Uganda's young women.
Recommendations
Based on the findings of this study, the following recommendations are proposed to improve condom use among unmarried sexually active AGYW in Uganda:
Tailored sexual health programs should be implemented in the Northern and Western regions, where condom use is significantly lower. These programs should address cultural barriers and improve access to sexual health services. Furthermore, qualitative studies in these regions are essential to gain deeper insights into the specific challenges and barriers influencing condom use, thereby informing more effective, context-sensitive interventions.
Expand the reach of family planning messages through radio, television, and social media to increase awareness of condom use. Messages should be culturally sensitive and address misconceptions about condoms, such as discomfort or reduced sexual pleasure.
Finally, future researchers should conduct longitudinal studies to understand the causal relationships between socio-demographic factors and condom use. Additionally, incorporate qualitative research to explore the barriers and facilitators to condom use and also explore the role of gender and partner dynamics.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://dhsprogram.com/data/dataset/Uganda_Standard-DHS_2016.cfm?flag=0.
Ethics statement
Access to the UDHS datasets was obtained through the DHS Program website (https://dhsprogram.com/data/available-datasets.cfm). Prior to public release, the DHS Program anonymized all data. The 2016 Uganda Demographic and Health Survey received ethical approval from the ICF Institutional Review Board (IRB). Informed verbal consent was obtained from all study participants, with parental or guardian consent secured for minors. Detailed information on the survey procedures is provided in the 2016 UDHS report [14], while additional guidance on data privacy and ethical safe guards is available at; https://dhsprogram.com/Methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm. The authors further affirm that all study procedures were conducted in line with the relevant guidelines and ethical principles outlined in the Declaration of Helsinki.
Author contributions
BT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AK: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. HA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We acknowledge the DHS program for making this data available for public use. We obtained this data from DHS website with permission to use.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AGYW, adolescent girls and young women; AOR, adjusted odds ratio; COR, crude odds ratio; FP, family planning; HBM, health belief model, HIV, human immunodeficiency virus; LMICs, low- and middle-income countries; NGOs, non-governmental organizations; STIs, sexually transmitted infections; UDHS, Uganda Demographic and Health Survey; WHO, World Health Organization.
References
1. UNAIDS. 2020 Global AIDS Update _Seizing the moment_Tackling entrenched inequalities to end epidemics (2020). Available online at: https://www.unaids.org/en/resources/documents/2020/global-aids-report (Accessed February 26, 2025).
2. Matovu JK, Bukenya JN, Kasozi D, Kisaka S, Kisa R, Nyabigambo A, et al. Sexual-risk behaviours and HIV and syphilis prevalence among in-and out-of-school adolescent girls and young women in Uganda: a cross-sectional study. PLoS One. (2021) 16(9):e0257321. doi: 10.1371/journal.pone.0257321
3. Mathur S, Pilgrim N, Patel SK, Okal J, Mwapasa V, Chipeta E, et al. HIV vulnerability among adolescent girls and young women: a multi-country latent class analysis approach. Int J Public Health. (2020) 65:399–411. doi: 10.1007/s00038-020-01350-1
4. Otim B, Okot J, Nantale R, Kibone W, Madraa G, Okot C, et al. Prevalence of condom use and associated factors among undergraduate students of Gulu university (2024).
5. Protogerou C, Johnson BT, Hagger MS. An integrated model of condom use in sub-saharan African youth: a meta-analysis. Health Psychol. (2018) 37(6):586. doi: 10.1037/hea0000604
6. Treibich C, Lépine A. Estimating misreporting in condom use and its determinants among sex workers: evidence from the list randomisation method. Health Econ. (2019) 28(1):144–60. doi: 10.1002/hec.3835
7. UBOS. Uganda Demographic and Health Survey 2022 Kampala, Uganda: Government of Uganda (2023). Available online at: https://www.ubos.org/wp-content/uploads/publications/UDHS-2022-Report.pdf (Accessed December 29, 2024).
8. Muyinda H, Jongbloed K, Zamar DS, Malamba SS, Ogwang MD, Katamba A, et al. Cango Lyec (healing the elephant): HIV prevalence and vulnerabilities among adolescent girls and young women in postconflict northern Uganda. J Acquir Immune Defic Syndr. (2023) 94(2):95–106. doi: 10.1097/QAI.0000000000003234
9. Ssekamatte T, Mugambe RK, Nalugya A, Isunju JB, Matovu JK, Kansiime WK, et al. Predictors of consistent condom use among young psychoactive substance users in Kampala’s Informal settlements, Uganda. Dialogues Health. (2022) 1:100080. doi: 10.1016/j.dialog.2022.100080
10. Bello OE, Ogundele OA, Okunlola OA. Spatial pattern and determinants of non-condom use among sexually active young people in Nigeria: a population-based, cross-sectional study. Sci Rep. (2024) 14(1):20378. doi: 10.1038/s41598-024-71424-0
11. Jean Simon D, Paul B, Kiragu A, Olorunsaiye CZ, Joseph F, Joseph G, et al. Prevalence and factors associated with condom use among sexually active young women in Haiti: evidence from the 2016/17 Haiti demographic and health survey. BMC Womens Health. (2023) 23(1):146. doi: 10.1186/s12905-023-02295-2
12. Maonga BB, Gondwe TS, Machira K. Factors influencing risky sexual behaviours among youths and adults men in Malawi. Stud Ethno-Medicine. (2019) 13(1):44–56.
13. Namasivayam A, Lovell S, Namutamba S, Schluter PJ. Predictors of modern contraceptive use among women and men in Uganda: a population-level analysis. BMJ Open. (2020) 10(2):e034675. doi: 10.1136/bmjopen-2019-034675
14. Jimu SE, Ntoimo LF, Okonofua FE. Prevalence and determinants of condom use among the youth in Malawi: evidence from the 2015/16 Malawi demographic and health survey. Reprod Health. (2023) 20(1):170. doi: 10.1186/s12978-023-01714-9
15. Kavuma D, Ndibazza J, Kirwana VB, Kafeero M, Katongole H, Baluku SP, et al. Factors associated with condom use among out-of-school young people on anti-retroviral therapy in central Uganda. HIV AIDS. (2022) 14:217–30. doi: 10.2147/HIV.S357535
16. Mbotwa CH, Moshi FV, Mosha IH, Kibona SE, Ezekiel MJ. Predictors of condom use among unmarried sexually active women of reproductive age in Tanzania. Tanzan J Health Res. (2022) 23(2):1–11. doi: 10.4314/thrb.v23i2.1
17. Chialepeh WN, Susuman AS. Risk factors of inconsistent condom use among sexually active youths: implications for human immunodeficiency virus and sexual risk behaviours in Malawi. J Asian Afr Stud. (2017) 52(4):484–96. doi: 10.1177/0021909615595992
18. Jara H, Damena M, Urgessa K, Deressa A, Debella A, Mussa I, et al. Consistent condom use and associated factors among sexually active military personnel in eastern Ethiopia: cross-sectional study design. Risk Manag Healthc Policy. (2022) 15:2057–70. doi: 10.2147/RMHP.S375340
Keywords: condom use, contraceptives, adolescent girls and young women, sexually transmitted infections, HIV—human immunodeficiency virus
Citation: Tukamushaba B, Kyomuhangi A and Atwijukiire H (2025) Factors associated with condom use among unmarried sexually active adolescent girls and young women (AGYW) aged 15–24 years: analysis of the Uganda Demographic Health Survey 2016. Front. Reprod. Health 7:1590356. doi: 10.3389/frph.2025.1590356
Received: 29 May 2025; Accepted: 22 August 2025;
Published: 10 September 2025.
Edited by:
Monica Ewomazino Akokuwebe, University of the Witwatersrand, South AfricaReviewed by:
Margaret Kasaro, UNC Global Projects Zambia, ZambiaRavesh Singh, University of KwaZulu-Natal, South Africa
Copyright: © 2025 Tukamushaba, Kyomuhangi and Atwijukiire. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bruce Tukamushaba, YnJ1Y2V0dWthbXVzaGFiYTFAZ21haWwuY29t
 Bruce Tukamushaba
Bruce Tukamushaba Annette Kyomuhangi
Annette Kyomuhangi Humphrey Atwijukiire
Humphrey Atwijukiire