- 1Department of Family Planning, Shanghai Putuo District Maternity and Infant Hospital, Shanghai, China
- 2Division of Chronic Non-Communicable Diseases and Injury Prevention, Shanghai Municipal Center for Disease Control and Prevention, Shanghai, China
- 3Department of Medical Affairs, Huashan Hospital, Fudan University, Shanghai, China
Objective: Curettage is a common treatment for missed abortion (MA). However, intrauterine adhesions (IUA) are a major postoperative problem that can lead to infertility and menstrual abnormalities. This study aimed to evaluate the effectiveness of estradiol-dydrogesterone (ED), auto-crosslinked hyaluronan (AH) gel, and their combination in preventing IUA following MA curettage.
Methods: A retrospective cohort study was conducted between June 2022 and December 2023. A total of 284 women following MA curettage were included, with 265 completing follow-up assessments. Participants were divided into four groups: (1) ED group (oral estradiol-dydrogesterone therapy), (2) AH group (intrauterine AH gel application), (3) ED + AH group (combination therapy), and (4) control group (no intervention). IUA diagnosis was confirmed via hysteroscopy.
Results: The incidence of IUA was significantly lower in the intervention groups compared to the control group (p = 0.001). The IUA rates were 7.94% in the ED group, 6.15% in the AH group, 5.71% in the ED + AH group, and 23.88% in the control group. Logistic regression analysis identified a significant reduction in IUA risk for patients receiving ED (OR = 0.17, p = 0.005), AH (OR = 0.13, p = 0.002), and ED + AH (OR = 0.15, p = 0.005) compared to the control group. Additionally, a history of three or more miscarriages was associated with a higher risk of IUA (OR = 4.34, p = 0.027).
Conclusion: This study demonstrates that prophylactic treatment with ED and/or AH significantly reduces the incidence of IUA following curettage for MA. These findings underscore the importance of individualized endometrial repair and adhesion prevention strategies in preserving female reproductive health.
1 Introduction
Missed miscarriage (MA) is a common early pregnancy complication characterized by the in-utero demise of the embryo or fetus without expulsion of the gestational tissue (1). Due to the frequent absence of typical miscarriage symptoms—such as vaginal bleeding and cramping—diagnosis is often delayed (2). MA is estimated to occur in approximately 13.4%–20% of all pregnancies (3–5). The World Health Organization (WHO) recommends surgical intervention when there is incomplete evacuation of the uterine contents following a MA (2). Although surgical management is generally effective in mitigating complications associated with miscarriage, it carries inherent risks. Notably, intrauterine adhesion (IUA) formation represents a significant postoperative complication, with post-miscarriage curettage being a dominant risk factor (6, 7).A review of 1,856 IUA cases revealed that 66.7% occurred following curettage (8). IUA can lead to various reproductive health issues, including infertility, menstrual irregularities, and recurrent miscarriages (9). As such, the prevention of IUA following curettage for MA has garnered considerable global research attention, with multiple approaches being evaluated (10–15). However, no universally accepted standard treatment has emerged (16), and further research is warranted to identify the most effective preventive strategy (9). aims to evaluate the clinical efficacy of estradiol/dydrogesterone tablets (ED), auto-crosslinked hyaluronan gel (AH), and their combination in preventing IUA after MA curettage, with the ultimate goal of protecting female reproductive health.
2 Methods
2.1 Study design and setting
A retrospective observational cohort study was conducted at the Shanghai Putuo District Maternal and Child Health Centre in China. This retrospective study did not randomize participants; group allocation reflected actual clinical management. Data were collected from patients who underwent curettage for MA between June 2022 and December 2023. Follow-up assessments were performed at three months post-surgery and during the early postmenstrual phase (3–7 days after menstruation). The study was registered in the Chinese Clinical Trial Registry (Registration number: ChiCTR2300078906).
2.2 Participants
Between June 2022 and December 2023, 284 women meeting the diagnostic criteria for MA, as outlined in the Expert Consensus on the Treatment of MA (1), were included. Of these, 265 women were successfully followed up via telephone or outpatient visits, while 19 were excluded due to loss to follow-up.
2.3 Treatment protocol and preventive interventions
Preparatively, detailed medical histories were obtained and patients received standardized health education. Two hours before curettage, all patients were received 0.4 mg misoprostol (0.2 mg/tablet) for cervical priming (17). Under conventional intravenous anesthesia and ultrasonic monitoring, experienced senior doctors performed the curettage, and all specimens were submitted for pathological examination (1). Postoperatively, all patients received antibiotics to infection prophylaxis (18). Based on the preventive interventions for IUA, women were assigned to four groups:
(1) ED group: Women began oral ED therapy (combination of 2 mg estradiol and dydrogesterone 10 mg per tablet) on the night of the operation (one tablet per day for 28 days). Following one treatment course, therapy was resumed on the third day after menstrual recovery for three consecutive courses.
(2) AH group: Women received an intrauterine injection of 3.0 ml AH (3.0 ml/branch) immediately after operation.
(3) ED + AH group: Women received both the intrauterine injection of AH and oral ED therapy as described above.
(4) Control group: Women received no additional perioperative intervention.
2.4 Research variables
2.4.1 Outcome variables
All diagnosed IUA presented with menstrual abnormalities (amenorrhea or hypomenorrhea), consistent with the Chinese Expert Consensus on the Clinical Diagnosis and Treatment of Intrauterine Adhesions (19). Women were followed up by hysteroscopy at three months after surgery or during the early postmenstrual phase (3–7 days after menses). For those presenting with abnormal menstruation or lack of menstrual recovery one-month post-operation, a vaginal ultrasound was performed. Hysteroscopy was then indicated if ultrasound findings revealed an endometrial thickness of less than 6 mm or suspected adhesions.
2.4.2 Control variable
The study identified several covariates based on previous research and data availability, including socio-demographic factors (age, education, BMI) and reproductive characteristics (number of miscarriages and duration of amenorrhea). In this study, duration of amenorrhea was selected over gestational age due to its superior precision in quantifying endometrial exposure to retained tissue and to avoid potential multicollinearity arising from including both variables in the model.
2.5 Statistical analysis
Data analysis was performed using Stata 16.0 (StataCrop, USA). Continuous data with a normal distribution were presented as mean ± standard deviation (χ̅ ± s), and one-way analysis of variance was employed for comparisons among the four groups. Categorical data were expressed as absolute numbers and percentages, with the Fisher exact test applied for groups comparisons. A multivariable logistic regression model was used to evaluate the effects of different preventive interventions and other potential risk factors on the incidence of IUA following MA curettage, a multivariable logistic regression model was applied. A p < 0.05 was considered statistically significant.
2.6 Efforts to address bias
Data were extracted from the hospital's electronic medical records and follow-up documentation. To minimize selection bias, all eligible women during the study period were included. Hysteroscopic evaluations were performed by experienced clinicians who were blinded to the preventive interventions' allocation, and ultrasound assessments were standardized using the same equipment and protocols t across all women. Outcome assessors were also blinded to preventive intervention groups, and baseline demographic and reproductive characteristics were recorded to adjust for potential confounders during statistical analyses.
2.7 Ethical statement
The study was conducted in accordance with the principles of informed consent, voluntary participation, confidentiality, and non-maleficence. Informed consent was obtained from all participants (or their legal guardians), and patient data were anonymized using codes. The study protocol was approved by the Ethics Committee of the Shanghai Putuo District Maternal and Child Health Centre (approval no.: PFYLL-2021003).
3 Result
3.1 General characteristics
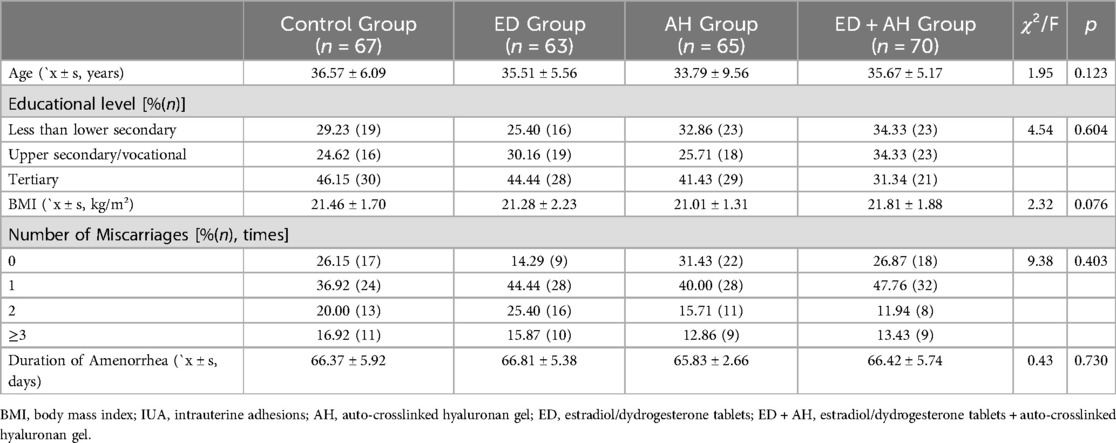
A total of 284 women met the inclusion criteria between June 2022 and December 2023. During the follow-up period, 19 women (6.69%) were lost due to travel, relocation, failure to respond to telephone calls, or lack of cooperation. Losses were distributed as follows: 4 in the control group, 8 in the ED group, 6 in the AH group, and 1 in the ED + AH group. Ultimately, 265 women (93.31%) completed the follow-up, including 67 in the control group, 63 in the ED group, 65 in the AH group, and 70 in the ED + AH group. There were no significant differences among the groups regarding age, BMI, educational level, number of miscarriages, or duration of amenorrhea (all p > 0.05), as shown in Table 1.
3.2 Incidence of IUA at 3 months postoperatively
At the three-month follow-up, the incidence of IUA was compared among the four groups. The ED + AH group exhibited the lowest IUA incidence (4 cases, 5.71%), followed by the AH group (4 cases, 6.15%) and the ED group (5 cases, 7.94%). The control group demonstrated the highest incidence (16 cases, 23.88%). The differences in IUA incidence among the groups were statistically significant (χ2 = 15.58, p = 0.001).
3.3 Multivariable logistic regression analysis
A multivariable logistic regression analysis was performed with demographic characteristics (age, BMI, education) and reproductive characteristics (number of miscarriages, duration of amenorrhea) as explanatory variables, and the preventive method as the independent variable (coded as 0 = control, 1 = AH, 2 = ED, 3 = ED + AH). The analysis indicated that age, BMI, education, and duration of amenorrhea were not significantly associated with IUA. However, the number of miscarriages was positively correlated with IUA risk; notably, women with three or more miscarriages had a significantly higher incidence of IUA (OR = 4.34, p = 0.027). Preventive interventions significantly reduced IUA incidence compared to the control group, with OR values of 0.13, 0.17, and 0.15 for the AH, ED, and ED + AH groups, respectively (p = 0.002, 0.005, and 0.005), as shown in Table 2.
4 Discussion
Curettage performed for MA can result in endometrial damage and subsequent IUA, which may adversely affect fertility (7). This study demonstrated that the application of AH and/or ED significantly reduced the incidence of IUA following MA curettage. Specifically, the IUA incidence was 7.94%, 5.71%, 6.15%, and 23.88% in the ED group, ED + AH group, AH group, and control group, respectively, which consistent with the previously reported range of 3%–38% (11, 12, 20, 21). Multivariable logistic regression analysis indicated that an higher number of miscarriages, particularly three or more miscarriages, was significantly associated with increased IUA risk. In contrast, the use of prophylactic interventions (AH, ED, or their combination) markedly decreased this risk.
The beneficial effects of ED may be attributed to the pharmacological actions of its components. Estradiol promotes endometrial proliferation and repair following curettage, reducing fibrosis and enhancing angiogenesis, which supports the regeneration of stromal tissue, endometrial glands, and blood vessels. Dydrogesterone facilitates the transition of the endometrium to the secretory phase, accelerates menstrual recovery, and increases the viscosity of cervical mucus, thereby reducing infection risk and contributing to IUA prevention (12). Similarly, auto-crosslinked hyaluronan gel functions as a mechanical barrier that prevents adhesion formation between opposing endometrial surfaces. The gel is fully degraded and absorbed within 7–14 days, a timeframe that is critical for proper endometrial healing (14, 22). Previous studies have also reported that both ED and AH can modulate inflammatory responses, promote angiogenesis, and inhibit scar formation, thereby enhancing postoperative healing and preventing IUA (11, 12, 23, 24).
The observation that an increased number of miscarriages elevates the risk of IUA is consistent with prior research (25, 26). Mechanical trauma to the endometrium during curettage is a known precipitating factor for IUA (27, 28). In the context of pregnancy, the endometrial basal layer is highly vascularized and relatively fragile; repeated or deep curettage can damage this layer. Furthermore, the abrupt decline in sex hormones following pregnancy termination reduces angiogenesis and oxygen supply, thereby increasing adhesion factor secretion and delaying endometrial repair (27, 29). In this study, factors such as age, BMI, and menstrual irregularities were not significantly associated with IUA incidence, which corroborates previous findings (25).
Several limitations must be acknowledged. First, the observational study design precludes the establishment of causality between the preventive interventions and the reduced incidence of IUA. Although a significant association was observed, unmeasured factors—such as detailed reproductive and menstrual histories or the timing of topical protective measures—may have contributed to the outcomes. Second, Although patients with preexisting IUA were excluded, detailed classification of prior miscarriage management (e.g., spontaneous miscarriage without intervention vs. induced miscarriage with curettage) was not performed, potentially affecting baseline risk assessment. Third, the single-institution setting may limit the generalizability of the findings. Future multicenter studies are recommended to validate these results and further explore additional risk factors.
5 Conclusion
This study demonstrates that prophylactic treatment with ED and/or AH significantly reduces the incidence of IUA following curettage for MA. These findings underscore the importance of individualized endometrial repair and adhesion prevention strategies in preserving female reproductive health. Further clinical investigations are warranted to evaluate subsequent pregnancy outcomes and to refine prophylactic protocols.
Data availability statement
The raw data supporting the conclusions of this paper are provided by Shanghai Putuo District Maternity and Infant Hospital, Shanghai, China, further inquiries need to apply to hospital for approval. Requests to access the datasets should be directed to LX,eHVlbG9uZ0BodWFzaGFuLm9yZy5jbg==.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Shanghai Putuo District Maternal and Child Health centre. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
HS: Writing – original draft, Data curation, Conceptualization. MS: Writing – original draft, Conceptualization, Data curation. LZ: Writing – original draft, Formal analysis, Data curation. JS: Writing – original draft, Formal analysis, Data curation. LX: Methodology, Writing – review & editing, Supervision, Project administration.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by 2022 Shanghai Putuo District Health Commmission Science and Technology Innovation Project (ptkwws202212).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Family Planning Branch of Chinese Medical Association. Expert consensus on the treatment of missed early miscarriage. Chin J Pract Gynecol Obstet. (2020) 36:70–3. doi: 10.19538/j.fk2020010117
2. World Health Organization. Abortion care guideline.Chapter 3 Recommendations and best practice statements across the continuum of abortion care. (2022) Available online at: https://www.ncbi.nlm.nih.gov/books/NBK578934/ (Accessed February 18, 2025).
3. Wu H-L, Marwah S, Wang P, Wang Q-M, Chen X-W. Misoprostol for medical treatment of missed abortion: a systematic review and network meta-analysis. Sci Rep. (2017) 7:1664. doi: 10.1038/s41598-017-01892-0
4. Lu Z, Hua Y. Study on the relationship between missed abortion in early pregnancy and iodine nutrition. Chin J Fam Plann Gynecotokol. (2023) 15:67–70. doi: 10.3969/j.issn.1674-4020.2023.05.14
5. Mahmoodinasab M, Loripoor M, Vazirinejad R, Aminzadeh F. Effect of misoprostol with and without evening primrose (Oenothera biennis) on induction of missed abortion. Avicenna J Phytomed. (2023) 13:454–62. doi: 10.22038/AJP.2023.22179
6. Salazar CA, Isaacson K, Morris S. A comprehensive review of Asherman’s syndrome: causes, symptoms and treatment options. Curr Opin Obstet Gynecol. (2017) 29:249–56. doi: 10.1097/GCO.0000000000000378
7. Yu D, Wong Y-M, Cheong Y, Xia E, Li T-C. Asherman syndrome–one century later. Fertil Steril. (2008) 89:759–79. doi: 10.1016/j.fertnstert.2008.02.096
8. Sevinç F, Oskovi-Kaplan ZA, Çelen Ş, Ozturk Atan D, Topçu HO. Identifying the risk factors and incidence of asherman syndrome in women with post-abortion uterine curettage. J Obstet Gynaecol Res. (2021) 47:1549–55. doi: 10.1111/jog.14667
9. Freedman MF, Schlaff WD. Avoiding Asherman’s syndrome: refining our approach to uterine evacuation. Fertil Steril. (2021) 116:961–2. doi: 10.1016/j.fertnstert.2021.06.037
10. Hooker AB, de Leeuw R, van de Ven PM, Bakkum EA, Thurkow AL, Vogel NEA, et al. Prevalence of intrauterine adhesions after the application of hyaluronic acid gel after dilatation and curettage in women with at least one previous curettage: short-term outcomes of a multicenter, prospective randomized controlled trial. Fertil Steril. (2017) 107:1223–1231.e3. doi: 10.1016/j.fertnstert.2017.02.113
11. Jing Z, Xue Z, Jing W, Qiong Z. The clinical value of self-crosslinked sodium hyaluronate gel combined with femoston after induced abortion. Matern Child Health Care Chin. (2021) 36:4990–4. doi: 10.19829/j.zgfybj.issn.1001-4411.2021.21.033
12. Li Y, Chen L, Yanyan N, Gao R, Xiaohua L. Effect of high estradiol tablets or estradiol and dicrogesterone tablets treatment for the postoperative recovery of women with missed abortion. Chin J Fam Plann. (2021) 29:914–20. doi: 10.3969/j.issn.1004-8189.2021.05.015
13. Vitale SG, Riemma G, Carugno J, Perez-Medina T, Alonso Pacheco L, Haimovich S, et al. Postsurgical barrier strategies to avoid the recurrence of intrauterine adhesion formation after hysteroscopic adhesiolysis: a network meta-analysis of randomized controlled trials. Am J Obstet Gynecol. (2022) 226:487–498.e8. doi: 10.1016/j.ajog.2021.09.015
14. Fan J, Xie J, Liao Y, Lai B, Zhou G, Lian W, et al. Human umbilical cord-derived mesenchymal stem cells and auto-crosslinked hyaluronic acid gel complex for treatment of intrauterine adhesion. Aging. (2024) 16:6273–89. doi: 10.18632/aging.205704
15. Zhang W, He Y, Chu Y, Zhai Y, Qian S, Wang X, et al. Amorphous curcumin-based hydrogels to reduce the incidence of post-surgical intrauterine adhesions. Regen Biomater. (2024) 11:rbae043. doi: 10.1093/rb/rbae043
16. Ding D-D, Zuo M-Z, Zhou Q, He Z-X. Visual analysis of uterine adhesion research based on CiteSpace: bibliometric analysis from 2006 to 2021. Front Reprod Health. (2022) 4:757143. doi: 10.3389/frph.2022.757143
17. American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Gynecology. ACOG Practice bulletin No. 200: early pregnancy loss. Obstet Gynecol. (2018) 132:e197–207. doi: 10.1097/AOG.0000000000002899
18. ACOG Practice bulletin No. 195: prevention of infection after gynecologic procedures. Obstet Gynecol. (2018) 131(6):e172–89. doi: 10.1097/AOG.0000000000002670
19. Society of Obstetrics and Gynecology CMA. Chinese Expert consensus on the clinical diagnosis and treatment of intrauterine adhesions. Chin J Obstet Gynecol. (2015) 50:881–7. doi: 10.3760/cma.j.issn.0529-567x.2015.12.00120
20. Xiangyun C, Lele R, Qian L. The influence of sodium hyaluronate combined with estradiol valerate used after uterine curettage on intrauterine adhesion and uterine recovery of women with missed abortion. Chin J Fam Plann. (2019) 27:1441–4. 21. doi: 10.3969/j.issn.1004-8189.2019.11.006
21. Xiao S, Wan Y, Zou F, Ye M, Deng H, Ma J, et al. Prevention of intrauterine adhesion with auto-crosslinked hyaluronic acid gel: a prospective, randomized, controlled clinical study. Zhonghua Fu Chan Ke Za Zhi. (2015) 50:32–6. doi: 10.3760/cma.j.issn.0529-567x.2015.01.008
22. Salwowska NM, Bebenek KA, Żądło DA, Wcisło-Dziadecka DL. Physiochemical properties and application of hyaluronic acid: a systematic review. J Cosmet Dermatol. (2016) 15:520–6. doi: 10.1111/jocd.12237
23. Fei Z, Xin X, Fei H, Yuechong C. Meta-analysis of the use of hyaluronic acid gel to prevent intrauterine adhesions after miscarriage. Eur J Obstet Gynecol Reprod Biol. (2020) 244:1–4. doi: 10.1016/j.ejogrb.2019.10.018
24. Guo Y, Shi X, Song D, Liu Y, Huang X, Xiao Y, et al. The efficacy of auto-cross-linked hyaluronic acid gel in addition to oestradiol and intrauterine balloon insertion in the prevention of adhesion reformation after hysteroscopic adhesiolysis. Reprod Biomed Online. (2022) 45:501–7. doi: 10.1016/j.rbmo.2022.04.017
25. Zhu R, Gan L, Wang S, Duan H. A cohort study comparing the severity and outcome of intrauterine adhesiolysis for Asherman syndrome after first- or second-trimester termination of pregnancy. Eur J Obstet Gynecol Reprod Biol. (2019) 238:49–53. doi: 10.1016/j.ejogrb.2019.02.030
26. Li C, Cai A, Sun C, Wu B, Chen X, Mao Y, et al. The study on the safety and efficacy of amnion graft for preventing the recurrence of moderate to severe intrauterine adhesions. Genes Dis. (2020) 7:266–71. doi: 10.1016/j.gendis.2019.03.003
27. Gilman Barber AR, Rhone SA, Fluker MR. Curettage and asherman’s syndrome-lessons to (re-) learn? J Obstet Gynaecol Can. (2014) 36:997–1001. doi: 10.1016/S1701-2163(15)30413-8
28. Mentula M, Männistö J, Gissler M, Heikinheimo O, Niinimäki M. Intrauterine adhesions following an induced termination of pregnancy: a nationwide cohort study. BJOG. (2018) 125:1424–31. doi: 10.1111/1471-0528.15216
Keywords: missed miscarriage, intrauterine adhesions, estradiol-dydrogesterone, auto-crosslinked hyaluronan gel, curettage
Citation: Sheng H, Sui M, Zhang L, Shi J and Xue L (2025) Efficacy of estradiol-dydrogesterone and auto-crosslinked hyaluronan gel in preventing intrauterine adhesions following missed miscarriage curettage: a retrospective observational study. Front. Reprod. Health 7:1602451. doi: 10.3389/frph.2025.1602451
Received: 29 March 2025; Accepted: 27 June 2025;
Published: 14 July 2025.
Edited by:
Sule Yildiz, Koç University School of Medicine, TürkiyeReviewed by:
Moamar Al-Jefout, United Arab Emirates University, United Arab EmiratesSalim Alfred Bassil, Al-Arz Hospital, Lebanon
Copyright: © 2025 Sheng, Sui, Zhang, Shi and Xue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Long Xue, eHVlbG9uZ0BodWFzaGFuLm9yZy5jbg==
†These authors have contributed equally to this work
 Huilin Sheng1,†
Huilin Sheng1,† Long Xue
Long Xue