- 1Routes2Results, London, United Kingdom
- 2Trisha Wood Santos Consulting, LLC, Seattle, WA, United States
- 3Infotrak Research & Consulting Limited, Nairobi, Kenya
Introduction: The World Health Organization (WHO) recently updated its guidelines for HIV post-exposure prophylaxis (PEP). These guidelines recommend community delivery and task-sharing for PEP administration and suggest enhanced adherence counseling for those who initiate PEP. This work provides insights into considerations for optimizing people's knowledge, demand for, use of and adherence to PEP through new channels. This mixed-method study examined five research questions concerning the perceptions and experiences of various groups regarding accessing and utilizing PEP and explored opinions on alternate delivery options to broaden access.
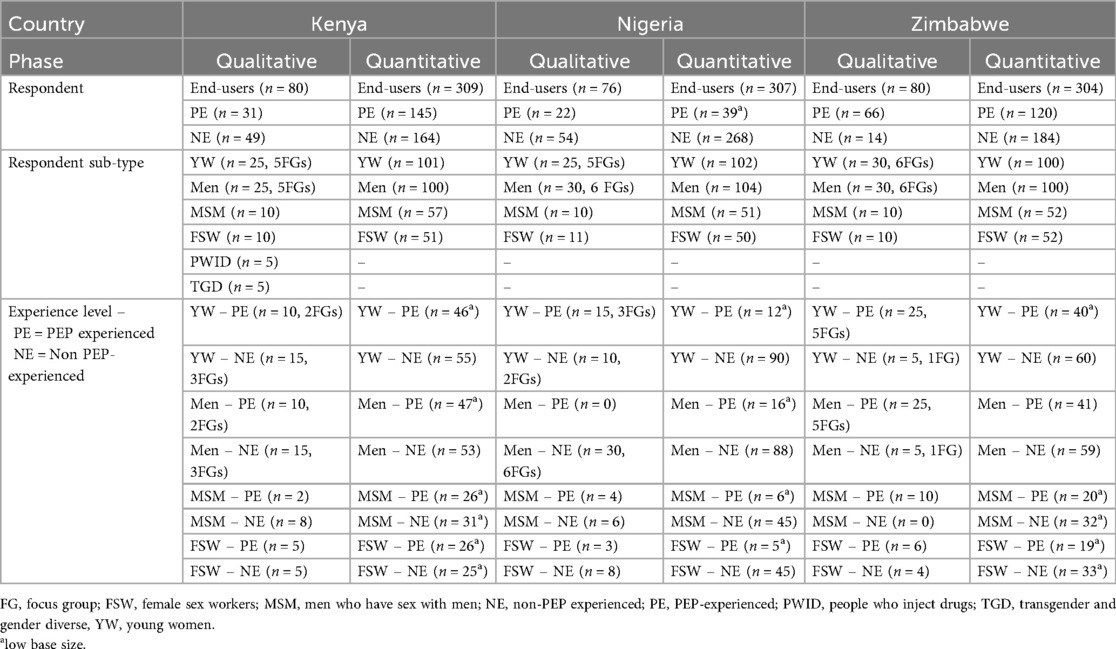
Methods: The total number of end-users interviewed for this study via qualitative and quantitative interview methodologies was 1,156. We spoke with a total of 236 end-users through qualitative Focus Groups (FGs) and in-depth interviews (IDIs) and surveyed 920 end-users with a questionnaire in Kenya, Nigeria and Zimbabwe, including members of key populations (Female Sex Workers, Members of the LGBTQ + Community, People Who Inject Drugs).
Results: Prompted awareness of PEP varied across the study countries (56.2% overall). Healthcare providers (doctors and nurses) were cited by end-user respondents as primary sources of information on HIV and PEP. PEP information evaluation revealed that condomless sex or condom malfunction were the emergency situations that resonated most with end-users. The majority (86.4%) cited a perceived likelihood to use PEP if exposed to HIV. A general hospital was deemed most acceptable for PEP access by end-users in all three countries (81.2%); clinical routes were perceived as preferable in terms of broadening access to PEP, with key reasons being convenience (68.2%), trustworthiness (56.5%) and knowledge (56.5%). End-users emphasized the need for consistent, correct, and supportive interaction points with healthcare providers to complete PEP treatment and follow-up.
Conclusions: WHO's recent update to the PEP guidelines recommends community-based distribution and task-sharing of PEP. Uptake is dependent on confidentiality and privacy of services as well as on increasing awareness and knowledge of the PEP pathway. Provision of PEP by healthcare providers needs to incorporate multiple end-user touch/access-points with emotional support for greater adherence, and our study highlights the different preferences and access contexts among end-users for PEP.
1 Introduction
The World Health Organization (WHO) recently updated its HIV post-exposure prophylaxis (PEP) guidelines to support increased access to PEP (1), with recommendations for community delivery and task-sharing for PEP administration and suggestion of enhanced adherence counseling for those who initiate PEP (2, 3). Studies have shown that end-user and provider awareness, usage of and adherence to PEP could be optimized (4–8).
A 2014 systematic review and meta-analysis of 97 studies on PEP adherence in multiple countries (based on 21,462 PEP initiations) found that non-occupational exposure was the main reason for PEP initiation in 34 studies, occupational exposure in 22 studies, and sexual assault in 26 studies; the remainder (15 studies) reported mixed exposures (9).
Current research indicates a concerted effort is needed to increase awareness of PEP, particularly among the general population and among key populations at risk of contracting HIV who face barriers to accessing HIV-related healthcare. Additionally, efforts should focus on broadening access to PEP and improving users' adherence by understanding the barriers they face and identifying effective strategies to enhance adherence (9–11).
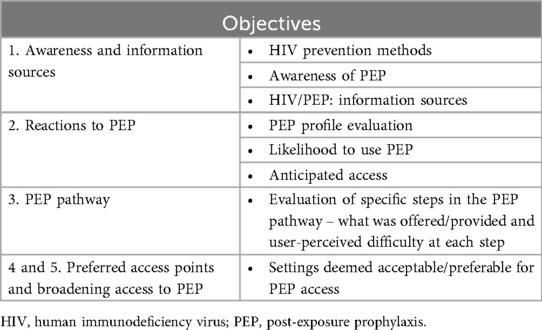
The objectives of this research were to answer five research questions: (1) What is the awareness of PEP among end-users? (2) What are end-users' reactions to PEP information, and what is the perceived likelihood to use PEP? (3) What are the preferred access points for PEP? (4) What do end-users think about the PEP Pathway? (5) What could broadening access look like? Table 1 illustrates specific objectives achieved in this study and how our results are organized.
2 Methods
We employed a mixed-method approach whereby the qualitative and quantitative arms of the research were run simultaneously in Kenya (Nairobi and Mombasa), Nigeria (Lagos and Abuja) and Zimbabwe (Harare and Bulawayo), interviewing potential and experienced end-users (herein all described as “end-users”). The qualitative research comprised in-person in-depth interviews (IDIs) and focus groups (FGs) and the quantitative research was conducted utilizing computer-assisted in-person interviews (CAPI). Respondents were not able to take part in both the qualitative and quantitative phases. All interviews were conducted in safe, confidential (as far as possible, with precautions taken against being overheard) and comfortable locations of the respondents' choice or with respondent approval. All research received ethical approval from in-country local Institutional Research Boards (IRBs). The fieldwork was conducted between October 2023 and January 2024.
2.1 Shared methodology: recruitment method
The recruitment process was consistent across all three countries. Qualitative data were collected via IDIs and FGs. Respondents were recruited using a mixed-sex team of recruiters with screening questionnaires to determine eligibility (programmed and conducted on CAPI devices), which they conducted face-to-face with potential end-users who lived in the target areas. Recruitment teams selected low-income areas within each city, where respondents were recruited from their households, chosen at random through walking (from a landmark such as a clinic, religious building, police station or gas station) or hotspots (such as universities, social spaces and sports venues) whereby the teams attempted door-to-door screening with skips between houses and varied pre-selected locations to ensure a wider recruitment field.
Households to be interviewed were selected using a household selection grid. Upon arrival at the sampled enumeration area, the supervisor identified a starting point, typically a street or a conspicuous landmark within the area. From the landmark, the enumerators randomly selected the first household and, using the skip interval and left-hand (anti-clockwise) rule, sampled additional households for inclusion in the survey. A skip interval of four households was applied, while in areas with flats, only one interview was conducted per flat.
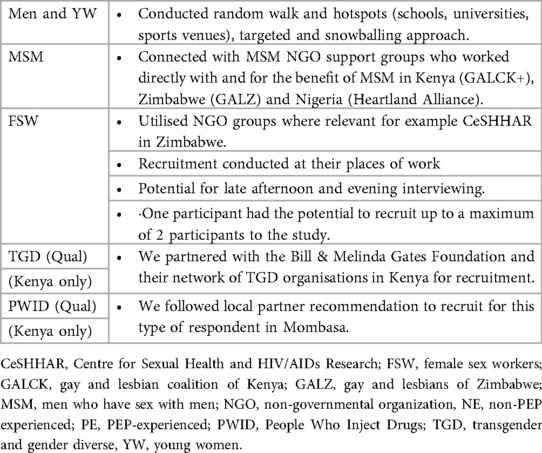
To ensure ethical and effective engagement with hard-to-reach populations, particularly MSM, we employed tailored recruitment strategies through trusted community-based umbrella organizations such as NGOs in Kenya (GALCK+), Zimbabwe (GALZ), and Nigeria (Heartland Alliance), and adapted research materials to suit the contextual needs and preferences of each group. Female Sex Workers were recruited using a snowballing approach at their workplaces, such as nightclubs, bars, and red-light districts. A recruitment factor of three was applied, meaning each participant could refer a maximum of two additional respondents.
Table 2 outlines the recruitment process for each group of participants among the end-user sample. The target population self-reported as sexually active (apart from People Who Inject Drugs), HIV negative and in Socio-Economic Class (SEC) C-D. This research utilized the EquityTool which is a short, country-specific questionnaire to measure relative wealth (12). SEC strata C and D were selected for this research as they encompass the broadest and largest section of the population.
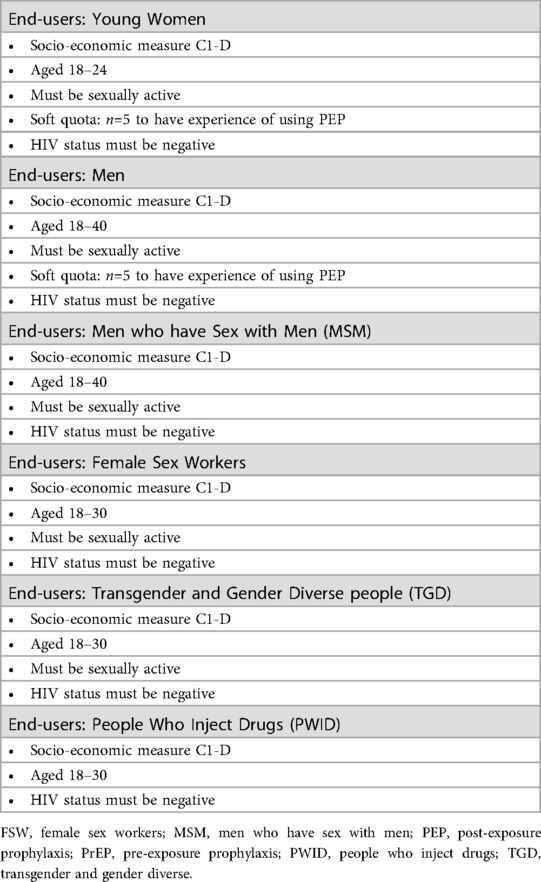
The age ranges selected for both the qualitative and quantitative sample differed depending on the population to ensure adequate representation of that specific group. Young Women had the lowest age range of 18–24 years, Men/Men who have Sex with Men were aged 18–40 years and the remaining three respondent types, Female Sex Workers, Transgender and Gender Diverse people, and People Who Inject Drugs, were aged 18–30 years (see Table 3). Young Women between the ages of 18–24 were chosen to represent the younger age groups who experience the greatest incidence of HIV infection (13). People Who Inject Drugs and Transgender and Gender Diverse people only took part in the qualitative part of the study.
The selection process for respondents varied by target group. At the household level, random selection was applied only to young women and men. The Kish Grid method was used to ensure equal probability selection at the household level. Recruiters listed all eligible household members (within the target age groups) in order of age, from oldest to youngest. The Kish Grid was integrated into a mobile data collection tool, which randomly selected the respondent to be interviewed. Recruitment locations within each region of a country were carefully sampled for both qualitative and quantitative phases to ensure comprehensive coverage and avoid double recruitment.
2.2 Qualitative phase
2.2.1 Sample and data collection
Qualitative data were collected via IDIs and FGs. IDIs lasted 60 min and FGs lasted 120 min. We spoke with a total of 236 end-users. The breakdown of the sample can be seen in Table 4. Focus groups were carried out with men and Young Women, and face-to-face IDIs with key populations (Men who have Sex with Men, Female Sex Workers, Transgender and Gender Diverse people, People Who Inject Drugs) because of a heightened requirement for confidentiality and respondent comfort with discussing sensitive topics.
Infotrak enlisted experienced researchers across the three countries to conduct the data collection exercise. Interviewers selected for the study were required to have two to five years of experience in household data collection, while supervisors needed a minimum of three years of experience overseeing similar exercises. The recruitment process also considered factors such as gender balance and the ability of field staff to communicate effectively with respondents.
To ensure strict adherence to study protocols, Routes2Results and Infotrak developed a comprehensive training manual detailing the procedures and responsibilities for the data collection process. The field teams in each country participated in an intensive three-day training session covering the study background, methodology, research tools (recruitment questionnaires, discussion guides, and structured questionnaires), ethical guidelines (informed consent and participant management), and data quality control measures. The training included mock interviews, role-playing exercises, and discussions on potential field challenges and mitigation strategies. Following the training, a two-day pilot exercise was conducted to familiarize the field team with questionnaire administration and refine interview techniques. Debriefing sessions were then held with both the field team and the Routes2Results (R2R) team to review experiences from the pilot exercise and fine-tune the data collection tools before proceeding with full-scale data collection.
2.2.2 Data analysis
For the qualitative data, codebooks were developed iteratively following review of transcripts by the core study team of four research directors, with at least five years of qualitative analysis experience. This framework was used to code transcripts and identify key themes that emerged from the data. An iterative and systematic process of content and pattern analysis was carried out. The study team used the analytical categories developed as part of the coding framework to derive meaning from the various pieces of evidence to answer the research questions. The study analysis team met regularly to review codebook outputs, with a view to align, calibrate and/or resolve coding challenges; this included discussion and consensus-building, revisiting the codebook, and third-party review.
2.3 Quantitative phase
2.3.1 Sample and data collection
The sample size was drawn on a stratified quota basis. Data were collected via face-to-face CAPI with a total of 920 end-users, stratified into two major cities and areas within them in Kenya (Nairobi and Mombasa), Nigeria (Lagos and Abuja) and Zimbabwe (Harare and Bulawayo) (Supplementary Table S3). Stratified quotas indicate that there was a predetermined number of study respondents to be recruited per location and category. Each study region was assigned a specific quota per respondent category to ensure adequate representation of the target respondents across the three countries.
Quota sampling was used to allocate samples for each respondent category. Surveys lasted between 35 and 48 min, with the consent of the respondents granted where interviews overran. The target population for the quantitative phase mirrored that of the qualitative phase. Other demographic information for end-users was captured during the interviews (Supplementary Table S3); this did not, however, determine eligibility.
For data collection, mobile phones/tablets with offline data storage capability were used and data were automatically uploaded when an internet connection was available. All interviews were audio-recorded, transcribed, and, where necessary, translated prior to analysis.
The research teams, comprising female interviewers and recruiters and mixed-sex supervisors, were briefed and trained. Pilot interviews were observed across all countries, ensuring adherence to objectives, processes and ethical considerations. Interviews were conducted by experienced interviewers in the local language or English, based on respondent preference.
2.4 Data analysis
The closed-ended quantitative data were analyzed using International Business Machines (IBM)'s Statistical Package for the Social Sciences (SPSS). Data were initially analyzed by total base size and were then further analyzed after division into PEP-experienced and non-experienced respondents, and, for end-users, into specific populations. Results from Young Women and Men are presented separately for each country; although results from the Female Sex Worker and Men who have Sex with Men samples are also presented separately, these are indicative findings because of the low sample size.
The clean dataset was coded prior to statistical analysis. All statistical analysis was undertaken using SPSS. Advanced analytical tools and approaches were used to make inferences about the target populations. Statistical adjustments of the data were applied where necessary. In accordance with the conventional acceptance of statistical significance at a P-value of 0.05 or 5%, confidence intervals (CI) were calculated at a confidence level of 95%.
In general, if an observed result was statistically significant at a P-value of 0.05, then the null hypothesis did not fall within the 95% CI. Statistical significance is observed when data in one country was different from findings in the others and not due to chance. Significance was analyzed via column proportions and column means tests.
2.5 Stimuli
End-users were shown stimuli (Figures 1, 2). All materials were translated, and translations were offered throughout the interview to ensure optimal understanding of the research questions and maximize ease of conversation for the respondent.
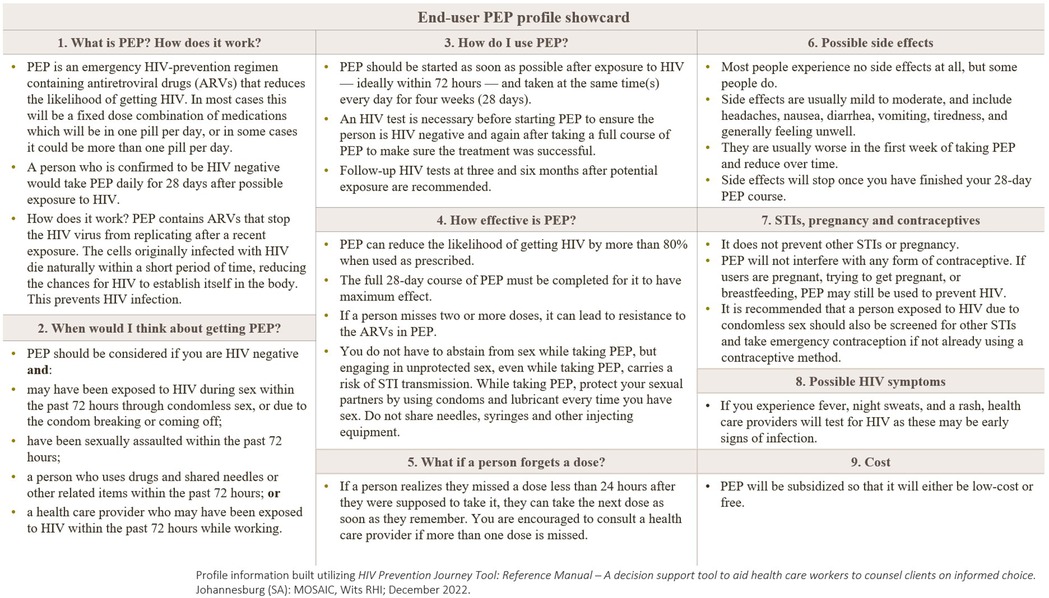
Figure 1. End-user PEP product profile (showcard) presented to survey participants. Information stimulus. The showcard summarizes: what PEP is and how it works (28-day antiretroviral regimen initiated ≤72 hours after exposure); when to consider PEP (sexual, needle-sharing, occupational exposure, or sexual assault among HIV-negative individuals); how to use PEP (daily dosing for 28 days with HIV testing before, at completion, and at 3 and 6 months); effectiveness with adherence; guidance for missed doses; common, usually mild side effects; notes on STIs, pregnancy, and contraceptives; symptoms suggestive of acute HIV infection; and typical cost/subsidy information. After viewing the profile, participants were asked follow-up questions about the content. ARV, antiretroviral; STI, sexually transmitted infection.
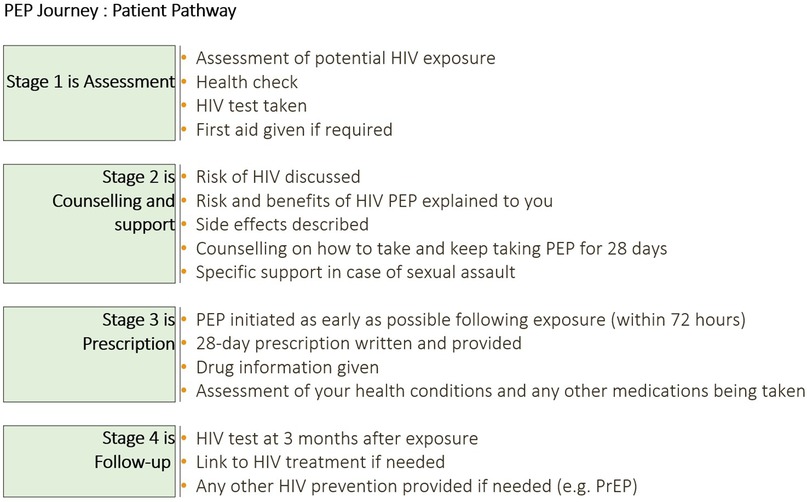
Figure 2. PEP journey—patient pathway showcard presented to survey participants. A visual used to prime respondents on the steps of HIV post-exposure prophylaxis care: Stage 1—Assessment (exposure assessment, health check, HIV test, first aid as needed); Stage 2—Counselling and support (discussion of HIV risk; explanation of PEP risks/benefits and possible side effects; adherence counselling for 28 days; specific support after sexual assault); Stage 3—Prescription (PEP initiation as early as possible and within 72 hours; 28-day prescription; drug information; review of co-morbidities and concomitant medicines); Stage 4—Follow-up (HIV test at 3 months; linkage to HIV treatment if positive; provision of other prevention options, e.g., PrEP). PEP, post-exposure prophylaxis; PrEP, pre-exposure prophylaxis.
2.6 Translations
All informed consent forms, stimuli and research materials were translated into the main languages spoken in the areas where fieldwork was conducted (Kiswahili in Kenya, Pidgin and Yoruba in Nigeria and Shona and Ndebele in Zimbabwe). Respondents were able to choose languages for written materials and discussion, and to switch if preferred.
2.7 Data collection
All interviews were conducted by interviewers from Infotrak (fieldwork partner) who were trained in market research methodologies and were native speakers.
3 Results
The results of this research are ordered according to the research objectives outlined in Table 1.
3.1 Sources of information on HIV prevention
3.1.1 HIV prevention methods
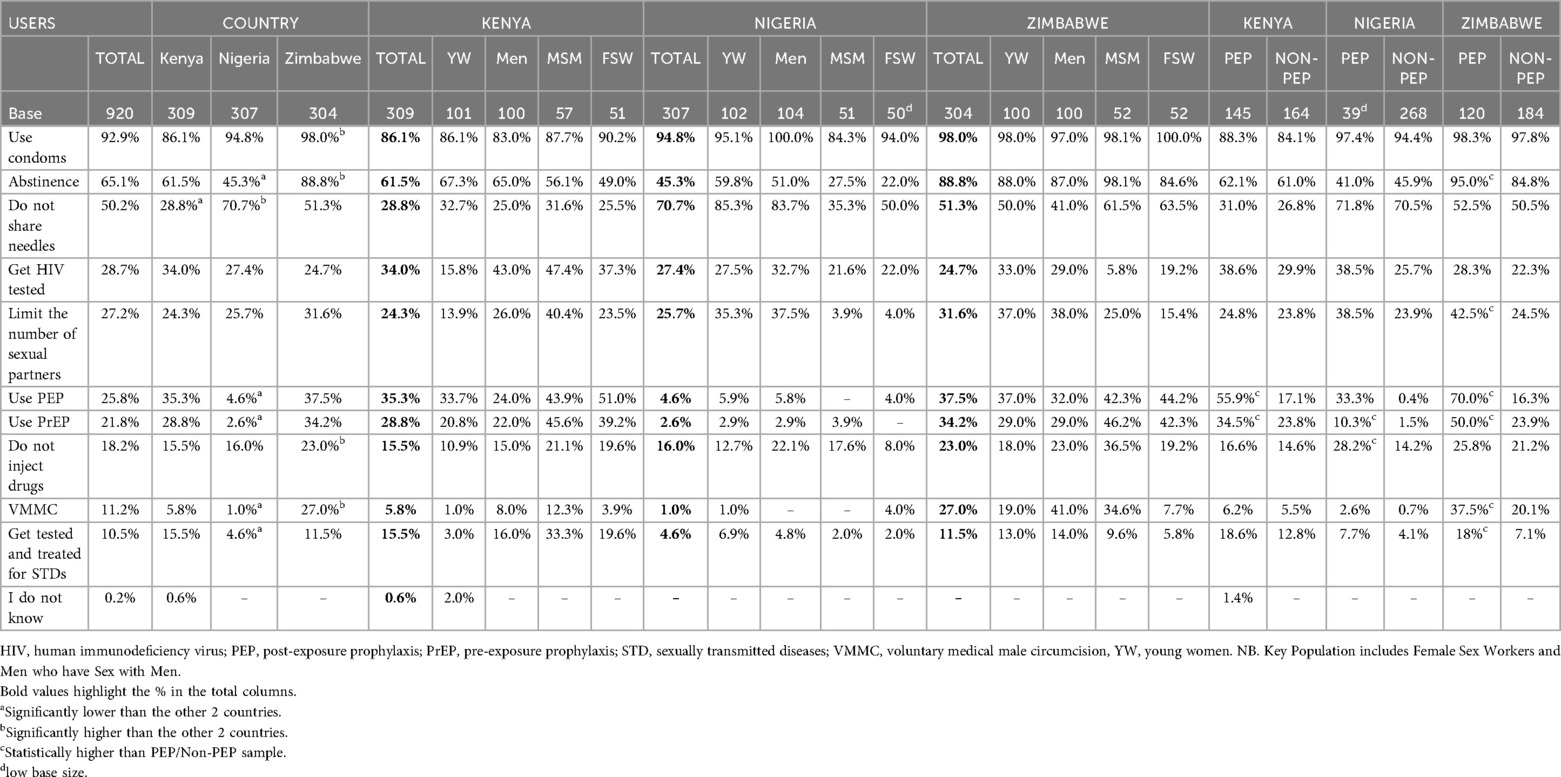
Quantitative Table 5, unprompted recall of known HIV prevention methods, shows that condom use was the most widely known method across all countries (Kenya 86.1%, Nigeria 94.8% and Zimbabwe 98.0%—significantly high) followed by abstinence (61.5%, 45.3% and 88.8% respectively, Zimbabwe significantly high) and not sharing needles [28.8%, 70.7% (Nigeria—significantly high) and 51.3%, respectively].
PrEP (Pre-Exposure Prophylaxis) or PEP use were cited via unprompted recall by 21.8 and 25.8% respectively of end-users overall. In Kenya and Zimbabwe, Female Sex Workers and Men who have Sex with Men demonstrated greater awareness of PrEP and PEP as an HIV prevention method (Kenya, awareness of PrEP: Female Sex Workers 39.2% and Men who have Sex with Men 45.6%; Zimbabwe 42.3% and 46.2% respectively. Kenya, awareness of PEP: Female Sex Workers 51.0% and Men who have Sex with Men 43.9%; Zimbabwe 44.2% and 42.3% respectively).
3.1.2 Awareness of PEP
Quantitative Table 6 illustrates that prompted awareness of PEP (i.e., those who did not spontaneously cite PEP as an HIV prevention method as an answer to the previous question) varied across the countries. While overall almost 3 in 5 end-users cited that they had not heard of PEP (56.2%), this was driven by lack of awareness in Nigeria (79.9%) which was significantly high, followed by Zimbabwe (51.6%) and Kenya (26.0%). There was significantly higher awareness of PEP across all end-user types in Kenya (70.2–73.1%), followed by Female Sex Workers and Men who have Sex with Men in Zimbabwe (58.6% and 53.3% respectively). PEP awareness was lowest in Nigeria (15.4%), with the majority of end-user types (Young Women 83.3%, men 82.7%, Female Sex Workers 77.1% and Men who have Sex with Men 70.6%) not aware of PEP. To note, discrepancy on awareness of PEP (unprompted recall 25.8% overall, Table 5 vs. prompted recall 41.1% overall, Table 6) is expected, as prompted awareness typically reveals latent familiarity; while many participants may not think of PEP spontaneously, a proportion do recognize it when prompted.
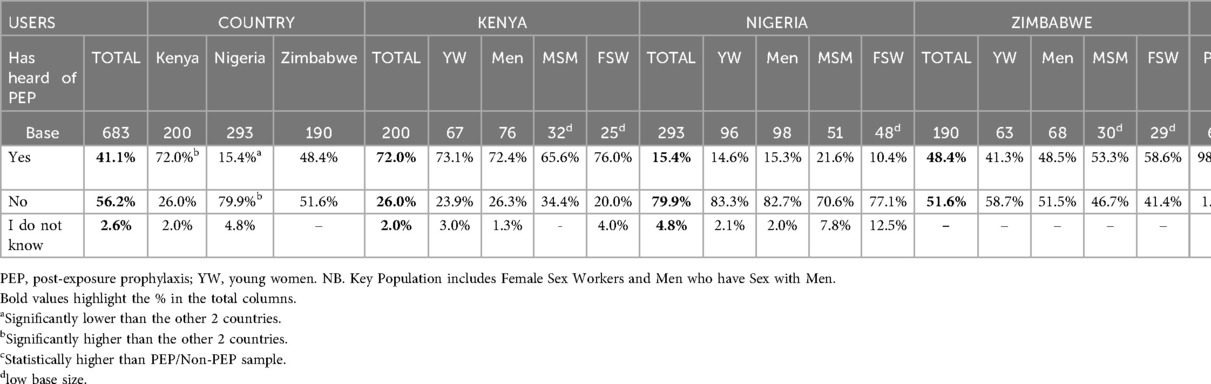
Table 6. Prompted awareness of PEP (asked to users who did not mention PEP previously as a method to prevent HIV).
3.1.3 HIV/PEP: information sources
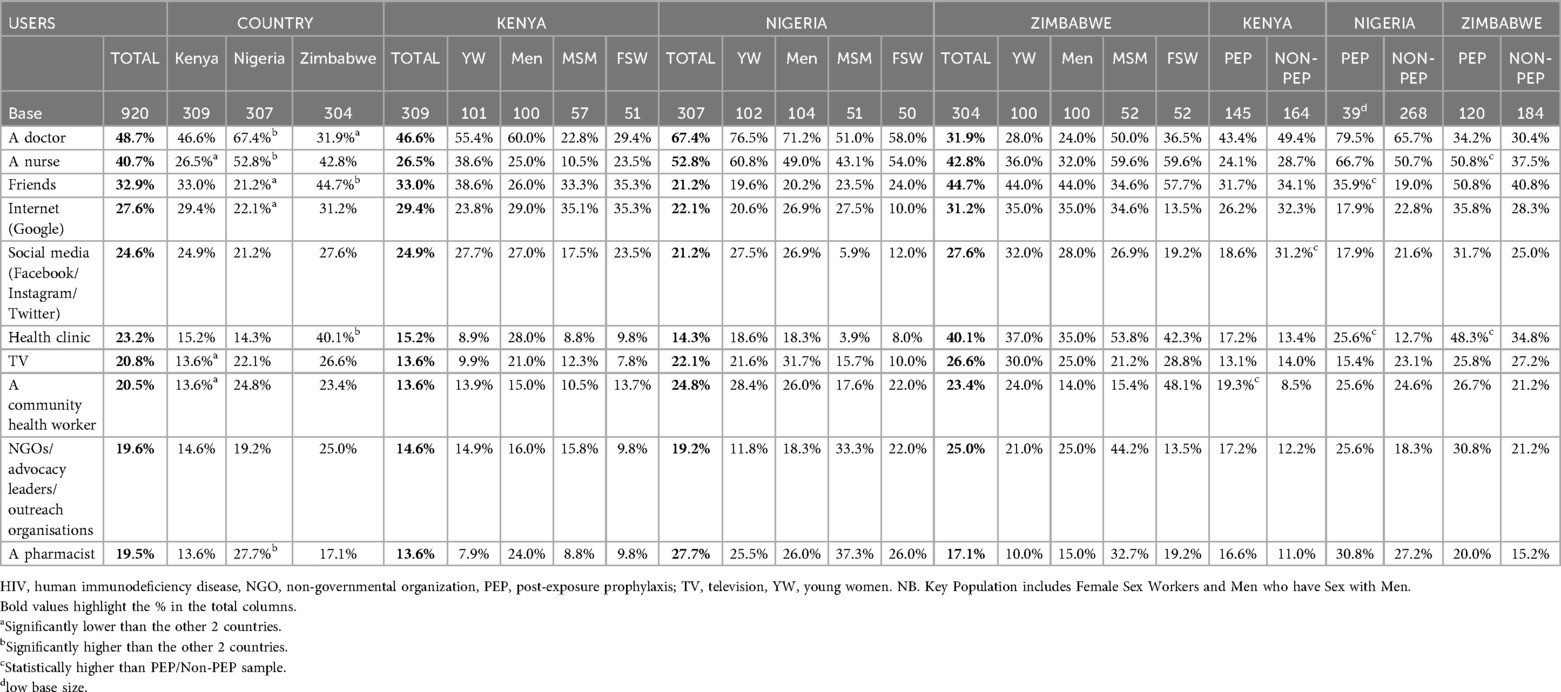
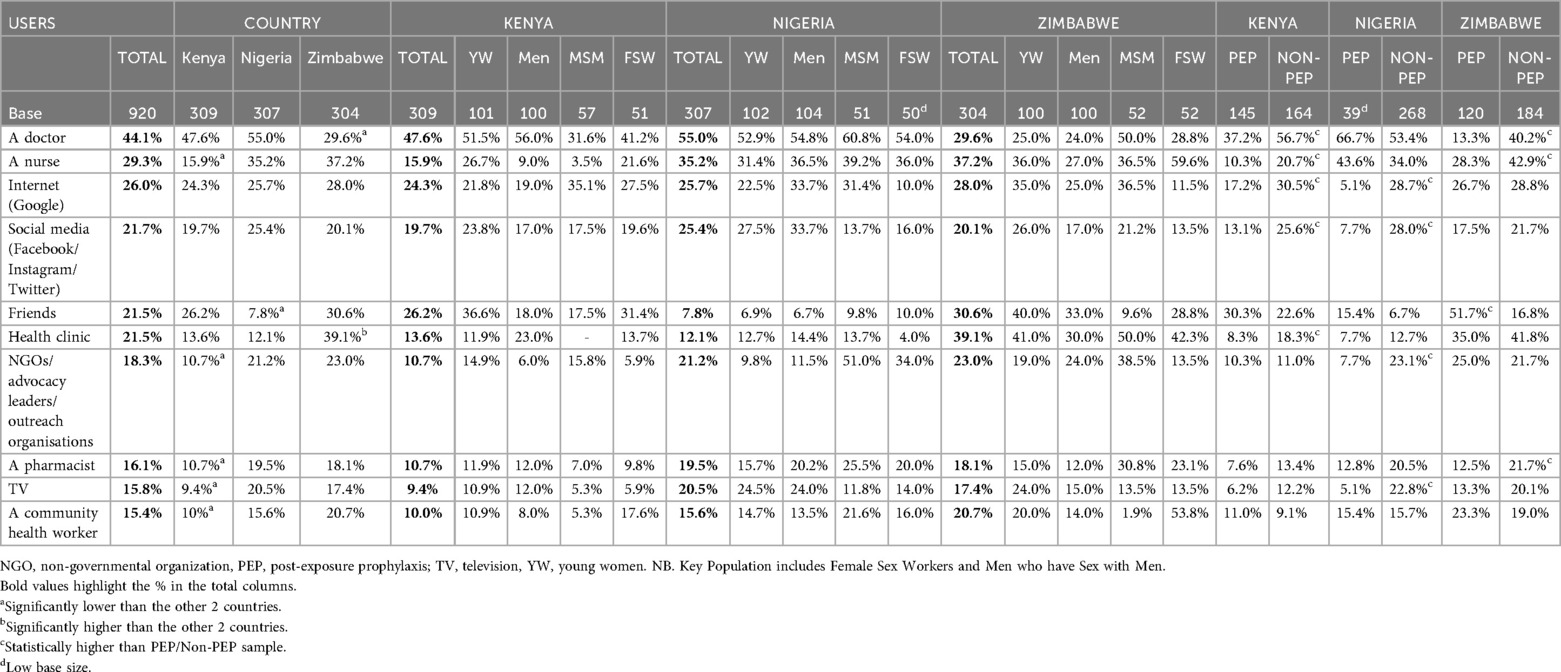
Quantitative Tables 7, 8 display all sources used to obtain information about HIV and PEP across all respondent types. Overall, the greatest number of participants cited doctors as a current source of information on HIV (48.7%, significantly higher in Nigeria) and PEP (44.1%), followed by nurses (40.7% for HIV and 29.3% for PEP), friends (32.9% for HIV and 21.5% for PEP) and the internet (27.6% for HIV and 26.0% for PEP).
3.2 Reactions to PEP
3.2.1 PEP profile evaluation
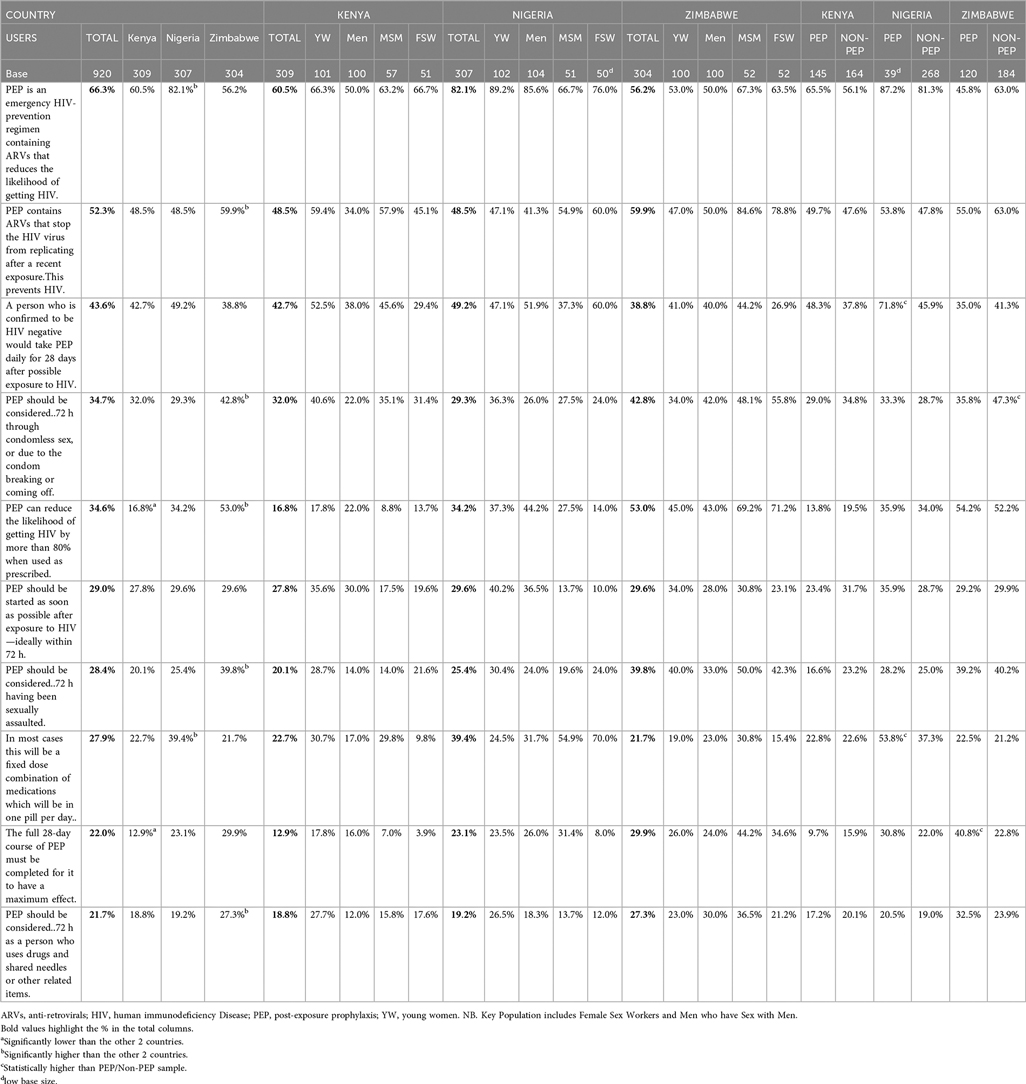
Quantitative End-users were shown PEP information in the form of a profile (Figure 1). The top four statements selected as positives across all respondent types are shown in Table 9. The two most selected statements illustrate how messages around PEP as an emergency HIV prevention option were considered positive.
Qualitative The scenarios outlined in the profile which would prompt seeking PEP that resonated most for end-users were those considered emergency situations, including condomless sex or condom malfunction, sexual assault/rape, not knowing the status of a (new) sexual partner, needle sharing or accidental cuts/exposure to blood, and financial pressures (accepting more money for condomless sex, e.g., when monthly rent is due). Sex workers explained during IDIs how financial pressures can result in taking risks:
“PEP is a very great tool in my life. As a sex worker, these HIV prevention methods are not 100% efficient. Usually, I use condoms, and sometimes they break, exposing us. Some clients will come and pay good money and say I don't want a condom; I need money, so I sleep with such a man without protection.” Female Sex Worker
The PEP profile information (Figure 1) was described as educational, clear and helpful; many respondents asked to keep the profile, and/or stated that it should be shared widely within the community.
“Ok, I like that it has been explained—how the PEP actually works in the body and how it prevents it because I only knew that it prevents but not how it does that. Because I think it’s explaining every detail.” Transgender or Gender Diverse respondent
Those who had taken PEP before had mixed views as to whether they were given the same information as in the profile:
“I didn’t get all this information when I got PEP. It was a friend of mine, so the friend of mine just told me that I need to use it daily for 28 days, that I should swallow this thing that it will help to prevent HIV basically.” Female Sex Worker
“So, this is more information than the hospital. In the hospital, they tell you to take it for 28 days, and you go sort yourself out thereafter. Seriously, I wasn't told anything else; I was just instructed to go and get tested, then come back and get the medication and go home.” Female Sex Worker
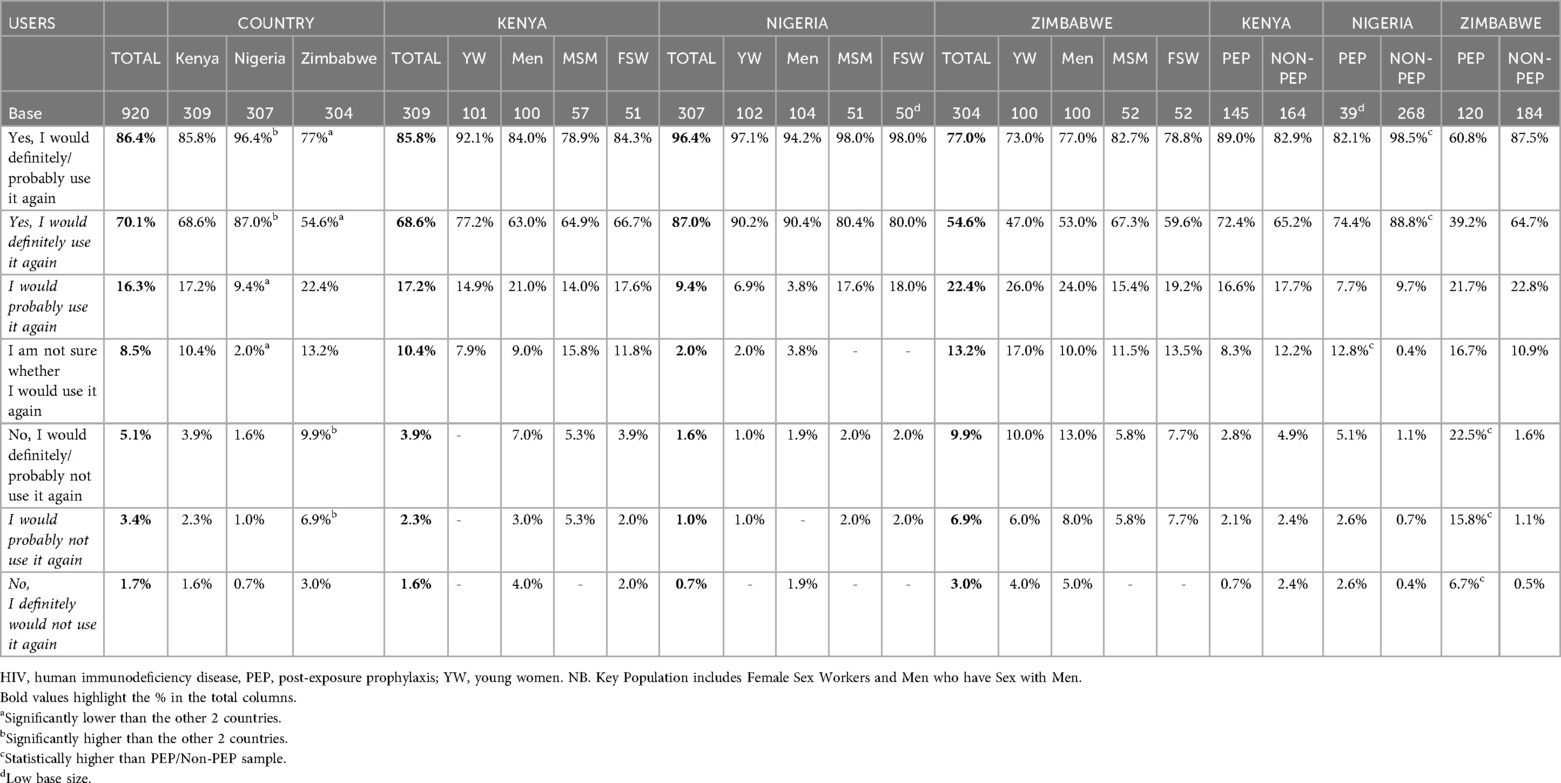
3.2.2 Perceived likelihood to use PEP
Quantitative Table 10 shows the perceived likelihood to use across all respondent types. The vast majority of end-users reported likelihood to use PEP if exposed to HIV (86.4% overall), after reading the PEP profile (Figure 1) which included a list of scenarios defining exposure.
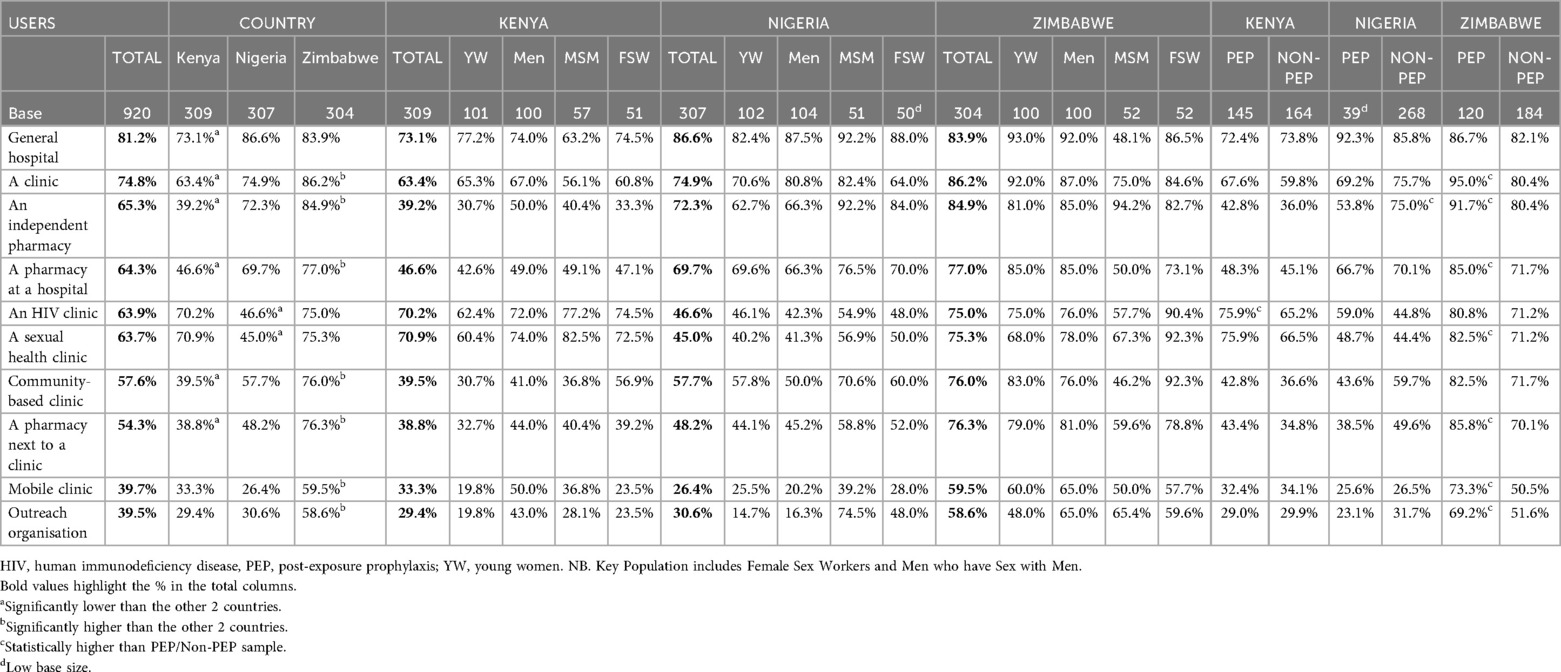
4 Preferred access points for PEP
Quantitative Table 11 shows perceived preference for places where PEP is or could be provided. Most respondents selected, from a pre-defined list, a general hospital as the place where they would prefer to access PEP (81.2% overall). Most respondents from Zimbabwe found all options acceptable (at least 58.6%), with a significantly higher number selecting community-based and outreach services. In Kenya and Zimbabwe, sexual health and HIV clinics were selected more often by Men who have Sex with Men than general hospitals, with the converse being the case in Nigeria.
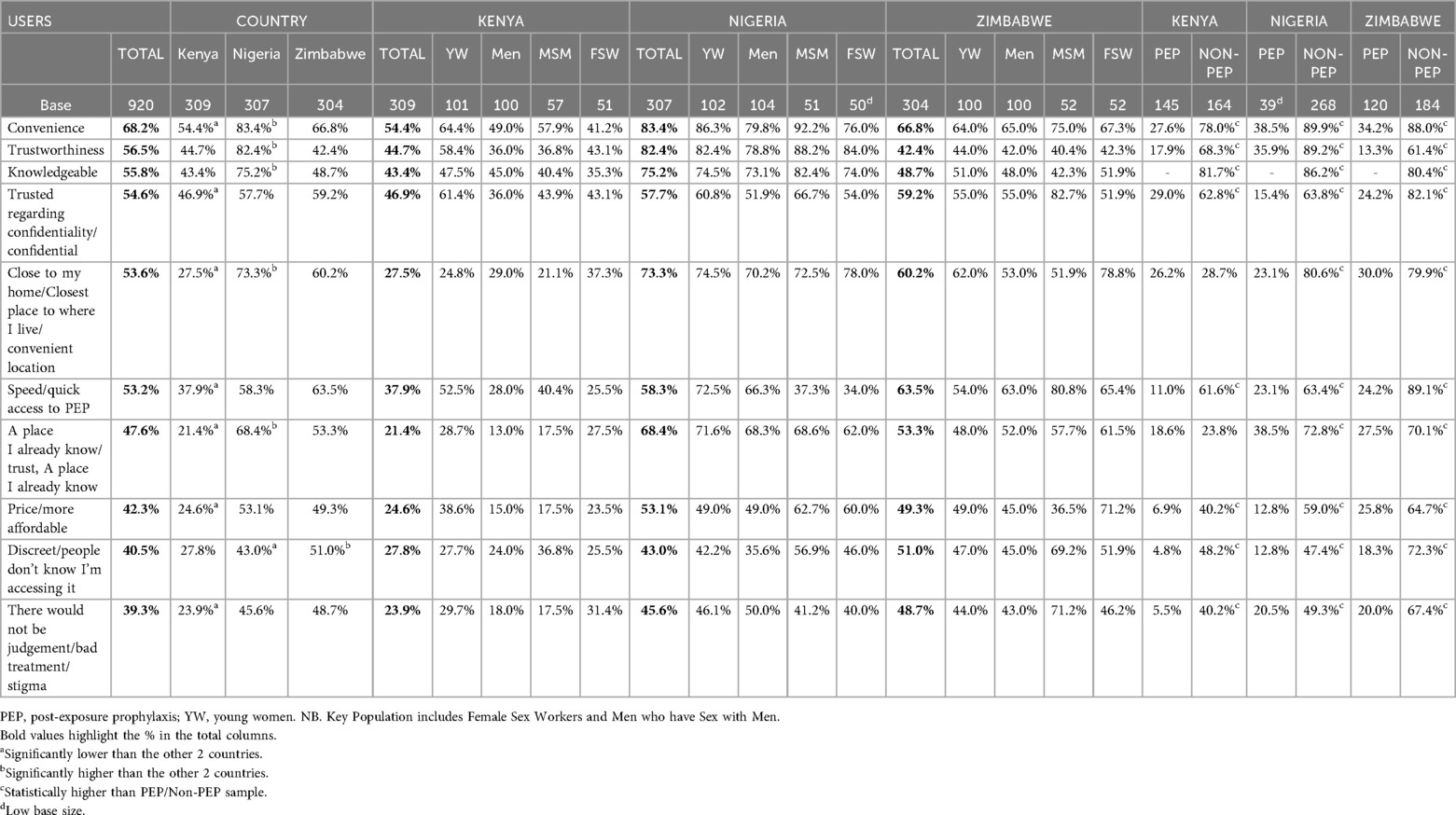
Convenience was cited as the top reason (with moderators using a pre-defined list to code participants' verbal responses) in all three countries for choice of location (68.2% overall) (Table 12). This was followed by trustworthiness (82.4% in Nigeria, significantly high) or trust in upholding confidentiality (59.2% in Zimbabwe). Furthermore, the need for rapid access was reported by end-users in Nigeria—close to my home (73.3%) – and Zimbabwe: quick access to PEP (63.5%). While convenience reasons were frequently cited, key populations in Nigeria and Zimbabwe tended to value trust regarding confidentiality (mean values 60.4% and 67.3%) and discretion (mean values 51.5% and 60.6% respectively) most highly. Lastly, end-users cited knowledgeable staff as an important reason in choosing a location to access PEP (55.8% overall; 43.4% in Kenya, 75.2% in Nigeria and 48.7% in Zimbabwe).
5 PEP pathway
5.1 Recall of PEP pathway among end-users with PEP experience
Quantitative Among PEP-experienced end-users (n = 304), there was high recall of the steps in the WHO PEP pathway having been carried out or available when they accessed PEP (Figure 2). Excluding some steps that would be case-specific (such as provision of first aid, specific support in case of sexual assault, and link to HIV treatment if needed), recall scores ranged from 81.6–98.4% overall (Supplementary Table S4).
5.2 Perceived ease/difficulty of each step of PEP pathway
End-users also perceived all steps of the PEP pathway to be very easy or easy, reporting overall scores of 77.2–92.0% (Supplementary Table S1).
Qualitative Nearly all end-users described the counseling and support stage of the WHO PEP pathway (Figure 2) as the most important. End-users described a set of information and support points which they felt would assist PEP treatment initiation and completion, which included: empathetic assessment, clear and correct advice at prescription, checking in to support with side effects within the first and second weeks, and reminders for follow-up HIV tests at 3 and 6 months. Prospects of PEP completion were considered compromised in the absence of correct advice and support:
“I think counseling and support are the most important aspects because when seeking PEP, individuals are often traumatized and uncertain about the consequences of their actions, so l think having adequate proper counseling and support is crucial during such a vulnerable time.” MSM
“I consider counseling essential in the whole experience because it was counseling that made me resilient in taking the PEP pills. My health advisor encouraged me to keep on taking the PEP pills, so I would say counseling is critical in the experience of side effects as you take PEP.” Young Woman
Figure 3 PEP pathway support points.
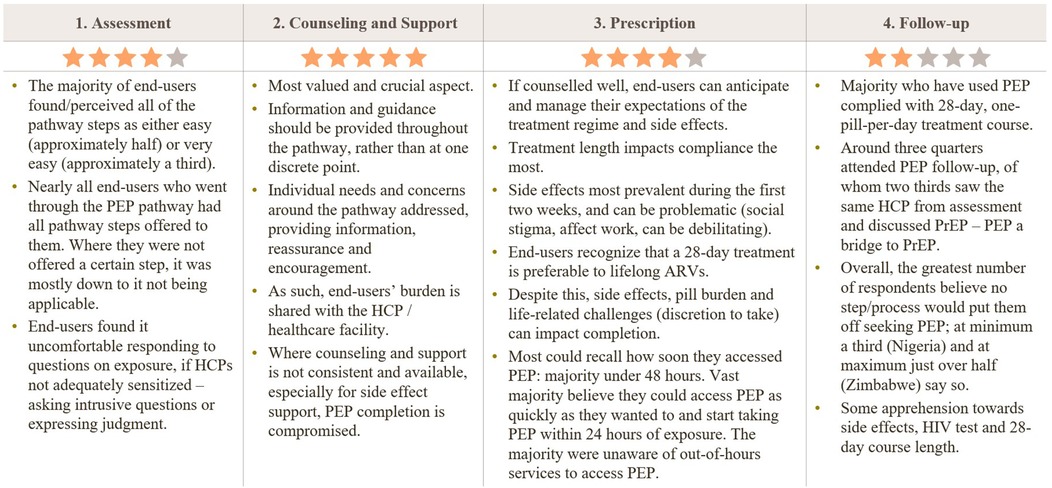
Figure 3. Participant perceptions of the PEP care pathway by stage. Star ratings summarize how positively end-users viewed each stage (1 = lowest, 5 = highest): Assessment ★★★★☆; Counseling & Support ★★★★★; Prescription ★★★★☆; Follow-up ★★★☆☆. Key themes: most steps were perceived as easy/very easy and usually offered when applicable; some discomfort answering exposure questions if health-care providers (HCPs) were not sensitized. Counseling/support was the most valued element-information should be continuous, tailored to needs, and available for side-effect management; when inconsistent, completion suffers. During prescription, good counseling helps set expectations; 28-day duration most affects adherence; early side effects (first two weeks) and pill burden can hinder completion; many accessed PEP within 48 hours but were often unaware of out-of-hours services. For follow-up, most completed the 28-day course and ∼¾ attended follow-up, ∼⅔ with the same HCP; PEP often served as a bridge to PrEP. Overall, many reported that no step would deter them, though some expressed apprehension about side effects, HIV testing, and the 28-day course. HCP, health-care provider; ARV, antiretroviral; PrEP, pre-exposure prophylaxis.
6 Broadening access
Quantitative Clinical routes (general hospital, clinic, pharmacy) were perceived as the most important means of broadening access to PEP (60+% overall) (Supplementary Table S2). Outreach and community-based services were perceived by many as potentially acceptable access points (39.5%, 57.6%). Non-clinical and alternative point-of-sale (POS) technologies (such as vending machines and websites) were least preferred by end-users (<30%), along with police stations (9.1%).
Qualitative Figure 4 outlines the preferences of each group of respondents regarding their ideal scenarios for accessing PEP, including locations, personnel and environment.
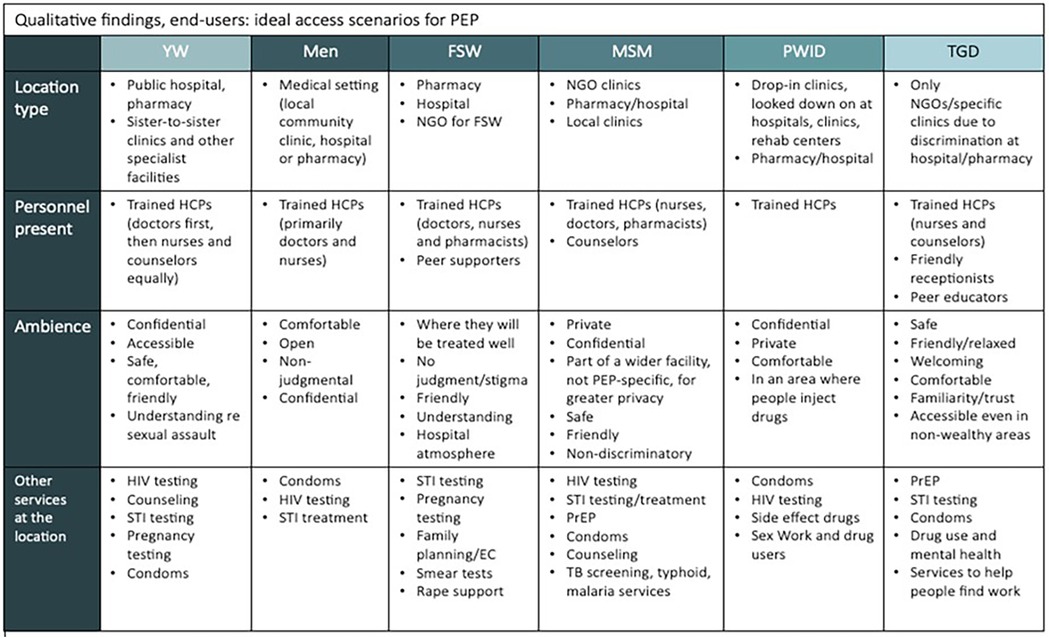
Figure 4. Ideal access scenarios for PEP across end-user groups (qualitative findings). Matrix summarizing what participants said would make PEP most accessible for them, by population group—location type, personnel present, ambience, and co-located services. Common preferences included access through routine clinical venues (hospitals, pharmacies, clinics), interaction with trained health-care providers, and private, non-judgmental settings. Group-specific notes: YW favored public hospitals/pharmacies and “sister-to-sister” clinics; men preferred general medical settings; FSW preferred pharmacies/hospitals and NGO facilities with peer supporters; MSM preferred NGO/local clinics and pharmacies; PWID emphasized drop-in or rehab-linked services in comfortable, stigma-free spaces; TGD favored NGO/specialty clinics due to discrimination in mainstream facilities, with friendly reception and peer educators. Desired co-services included HIV and STI testing/treatment, PrEP, condoms, pregnancy testing and emergency contraception, TB/malaria screening, mental-health and substance-use support, and services for sex workers and people who inject drugs. YW, young women; FSW, female sex workers; MSM, men who have sex with men; PWID, people who inject drugs; TGD, transgender and gender diverse; HCP, health-care provider; PrEP, pre-exposure prophylaxis.
The majority of end-users stated they would want to access PEP in a clinical setting:
“It would be either a clinic or hospital. There will be a qualified medical practitioner. It would be an enclosed, clean and well-equipped room.” Man aged 18–40
Through qualitative discussions it became clear that those prioritizing privacy, in particular respondents from key populations, felt uncomfortable with accessing PEP through community avenues:
“I'll go to the clinics but not the community facilities. The outreach is better than the community-based facilities. If you go to the community, everyone has their thoughts and can even tell people about your status.” Female Sex Worker
There were mixed responses to the technology-based options (vending machines and websites/apps), with those who were in favor praising the convenience, speed, non-time-limited access and perceived privacy. Objections unique to the technology-based options could be divided into two categories, principled and practical. Principled concerns included lack of counseling and ability to ask questions, lack of privacy (vending machines) and potential for misuse, especially for a sensitive and time-dependent intervention like PEP:
“Someone who doesn't have full information about it might dispense it, use it, maybe overdose or under-dose. It does not have the relevant information yet. It is not something like a rubber that you use and throw away. This is something that goes into your body, and it might affect the functioning of your body.” Transgender or Gender Diverse respondent
This highlights the need to balance innovation with safeguards that address user trust and support needs, particularly in contexts where stigma and misinformation may already undermine service uptake.
Practical concerns included whether the medication in machines would be in-date, whether the medication from websites or machines would be genuine, whether the websites would be trustworthy, and that there would be a need for reliable access to the internet:
“There are lots of fake websites and to avoid fraudsters who might be making wrong drugs.” Man aged 18–40
7 Discussion
The study results indicate that there is latent potential to expand access to and use of PEP for HIV prevention through increased awareness, broadened accessibility, and enhanced support for initiation and continuation. These findings align with WHO's recent recommendations and suggestions in the updated HIV PEP guidelines (1). This study contributes knowledge on PEP preferences, awareness and access among end-users. It also examines preferred PEP access points for different populations, evaluates the WHO PEP pathway, and provides recommendations for expanding access to PEP and support for continuation.
7.1 Awareness and acceptability of PEP
Recommendations for use of PEP to prevent HIV infection were developed decades ago, but awareness remains low (4, 7, 8, 10, 11, 15–19). Our study confirms low awareness of PEP with less than 40% of end-users in Kenya and Zimbabwe and less than 5% in Nigeria spontaneously identifying PEP as an HIV prevention method. When prompted, a greater proportion of respondents knew of PEP, particularly in Kenya (72.0%), but still less than 50% in Nigeria and Zimbabwe. In particular, Nigeria's notably low PEP awareness likely reflects broader structural challenges i.e., pervasive HIV-related stigma and limited access to tailored services for key populations in healthcare settings affecting uptake and engagement of such services (20). These findings reiterate the need to increase awareness and knowledge of PEP through multiple channels and to include key messages around when to seek PEP, urgency around initiation, and reassurance that PEP's benefits outweigh the downsides of taking it (10, 11, 15–19). This would facilitate greater uptake and completion of PEP, and potentially lower HIV transmission in the community (21, 22).
End-user acceptability of PEP has not been widely studied, but it has been found to be acceptable in some settings (15, 23). Our study found high acceptability, indicated by more than 80% of all end-users stating they are likely to use PEP if exposed to HIV. Furthermore, the PEP profile information was found to be useful, and in some cases, more useful than information received by those who had previously used PEP. Barriers such as poor counseling, limited ongoing support, misinformation or no information, and stigma against certain groups or behaviors can contribute to limited uptake or adherence of PEP (4, 16, 19, 24–31). This emphasizes a need for ongoing support to improve PEP uptake and completion.
7.2 PEP pathway
Our study illustrates the benefits and utility of WHO's PEP Pathway (assessment, counseling and support, prescription, and follow-up), with most end-users indicating that the steps are largely followed. End-users recommended consistent and appropriate support points throughout the pathway to ensure successful completion of the regimen and management of side effects. Fundamentally, this includes sharing more information about PEP in the counseling stage, such as the profile used in our study. Providing follow-up reminders or visits for medication management (and side effects) or other related needs are also recommended (32, 33). These findings align with other studies suggesting enhanced counseling and support for clients seeking PEP could increase continuation and improve clinical outcomes (11, 14, 28, 34, 35).
7.3 Broadening access
As with other HIV services, expanding access to PEP will require consideration of the needs and preferences of different populations and adaptation of delivery models for different needs. Our study reinforced this with a variety of preferred locations for accessing PEP identified. Most preferred a clinical setting, but the type varied from public hospitals or pharmacies for Young Women to community clinics for men to drop-in clinics for People Who Inject Drugs. Universally, end-users expressed the need for confidential, private services where they will be treated well without judgment or stigma, which was reiterated throughout the study and aligns with findings from other studies on the need to maintain privacy and confidentiality for PEP, and HIV services more broadly (7, 8, 19, 24, 25, 36–38).
Expanding access points for PEP will be important to increase use. Although our study found that most end-users prefer a general hospital for accessing PEP, this may be a reflection of the current PEP availability (19). Outreach and community-based outlets could be important for broadening access as end-users also value convenience and speed in accessing PEP. Community Health Workers (CHWs) may be well-placed to provide ongoing support and follow-up functions from the PEP pathway if the locations and providers exhibit other valued factors such as trustworthiness, confidentiality and knowledge of PEP. Other studies also point to the potential for expanded access to PEP through new channels including pharmacies and community-based distribution (16, 38–43). The least preferred locations for accessing PEP are point-of-sale outlets like vending machines or websites. Increased access to PEP through diverse, convenient locations shows promise, but more research is needed to understand and address end-user concerns related to privacy and confidentiality in these locations. These concerns are of high importance and must be addressed for any access point.
7.4 Strengths and limitations
Our study has many limitations as it focused on people's perception of PEP and, in some cases, their experience using PEP. The findings are largely formative, with the output intended to support WHO's updated PEP guidelines for expanding access through community-based channels and task-sharing. It was not within the scope of the study to identify any causal links to use or continuation of PEP. The themes and user insights identified are not generalizable or representative of the national populations, as the sample of participants was only a partial geographic sample within the target countries. It is likely that the views of some groups were not covered, and others may be under-represented in these data; furthermore, there could be confounding factors influencing preferences such as gender, age, and previous PEP experience.
7.5 Implications for practice and future research
This study confirms that PEP remains under-utilized as an HIV prevention method. WHO's new PEP guidelines recommend providing access at the community level and through task-sharing and suggest that consistent and appropriate support can improve uptake and adherence. Our study provides additional insights into the needs and preferences of different groups when accessing PEP and suggests that programs ensure access through diverse settings. The study also highlights low awareness of PEP and recommends generating broad awareness through diverse communication channels, as preferred information sources vary by group and country. Most importantly, the study highlights the need for multiple support points during the PEP pathway to ensure adherence. This will require leveraging the pathway to provide non-judgmental and informative access points for end-users to seek PEP and advice involving the community and other healthcare professionals who provide this kind of support efficiently (due to the 48–72 h window time restriction).
8 Conclusions
Preventing new HIV acquisition is becoming more challenging as incidence declines in many countries. Increasing access and use of PEP when someone has had a possible exposure is a promising approach to help close the gap on new acquisitions. Our study confirmed the overall appeal of PEP as a prevention method and offered insights into expanding access and improving uptake and continuation. WHO's recent update to the PEP guidelines recommends community-based distribution and task-sharing, which will help expand access points. Minimizing stigma associated with PEP use, however, will be critical for uptake, and this includes ensuring confidentiality and privacy of services, while increasing awareness and understanding of the prevention method. Additionally, provision of PEP from any type of provider needs to incorporate an empathetic approach and critical access points during PEP treatment to ensure correct and timely use, as well as to provide accurate information and emotional support for greater adherence. Our study highlights the different preferences among end-users regarding PEP, and future research should explore the programmatic requirements for offering PEP within a community through diverse channels and approaches to meet the needs of the different populations, as well as innovations to focus support points for greater continuation rates.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by AMREF ESRC (Kenya); UI/UCH EC (Nigeria); Medical Research Council of Zimbabwe (Zimbabwe). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MouE-S: Investigation, Methodology, Supervision, Conceptualization, Funding acquisition, Writing – review & editing, Formal analysis, Visualization, Writing – original draft, Project administration. RE: Writing – review & editing, Writing – original draft. MonE-S: Writing – original draft. IG-G: Writing – review & editing. KK: Writing – original draft, Writing – review & editing. TW: Writing – review & editing, Writing – original draft. RM: Writing – review & editing. EM: Writing – review & editing. JL: Funding acquisition, Writing – review & editing, Supervision, Investigation, Project administration, Visualization, Methodology, Writing – original draft, Conceptualization, Formal analysis.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded through a research grant from the Bill & Melinda Gates Foundation (INV ID: 053221). The contents of this article are the responsibility of the authors and do not necessarily reflect the views of the Bill & Melinda Gates Foundation. The funder had the following involvement with the study: determining country locations, research objectives and review and approval of all materials used to include stimuli. The funder was not involved in the study research collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Acknowledgments
The authors thank the participants who shared their time and perspectives to explore PEP. The authors also thank important study collaborators, including those in fieldwork: InfoTrak Research and Consulting Limited. We acknowledge Siobhan Malone, The Bill & Melinda Gates Foundation, for research leadership and manuscript review. We acknowledge the WHO team including Rachel Baggaley, Virginia MacDonald, Michelle Rodolph, for their advice and guidance during the research. We acknowledge Heather-Marie Schmidt of UNAIDS for help and guidance during this research. We acknowledge Tom Donelon for his editorial review. We acknowledge Izaak Lucas for his support during fieldwork and in updating the manuscript after review.
Conflict of interest
The authors declare that they all work for private companies: Routes2Results, Infotrak Research and Consulting Limited, and Trisha Wood Santos Consulting, LLC. TW was employed by LLC.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frph.2025.1606013/full#supplementary-material
Supplementary Table S3 | Reported demographics: Relationship status, number of children, healthcare facility most often used, healthcare insurance, work status, highest level of schooling achieved, religion and regional split.
Supplementary Table S4 | (PEP Experienced Users only): Recall of specific services offered within the PEP pathway.
Abbreviations
AIDS, acquired immune deficiency syndrome; ART, antiretroviral Treatment; BMGF, Bill & Melinda Gates Foundation; CAPI, Computer Assisted Personal Interviewing; CeSHHAR, Centre for Sexual Health and HIV/AIDS Research; CHW, Community Health Worker; FGs, focus groups; FSW, female sex workers; GALCK, Gay and Lesbian Coalition of Kenya; GALZ, Association of LGBTI people in Zimbabwe; HIV, Human Immunodeficiency Virus; IBM, International Business Machines; IDI, in-depth interviews; IRB, Institutional Review Board; KG, Kindergarten; LGBT, Lesbian, Gay, Bisexual and Transgender; MOH, Ministry of Health; MSM, men who have sex with men; NGO, Non-Governmental Organization; NSDCC, National Syndemic Disease Control Council; PEP, post-exposure prophylaxis; PE, PEP-experienced; POS, point of sale; NE, non PEP-experienced; PrEP, pre-exposure prophylaxis; PWID, People Who Inject Drugs; R2R, Routes2Results; SPSS, Statistical Package for the Social Sciences; STI, Sexually Transmitted Infection; TGD, Transgender and Gender Diverse; TV, Television; WHO, World Health Organization; YW, Young Women; ZCC, Zion Christian Church.
References
1. Macdonald V, Rodolph M, Ford N, Nunez MP, Schmidt H-M. Guidelines for HIV Post-exposure prophylaxis. Geneva: World Health Organization (2024). Available online at: https://iris.who.int/bitstream/handle/10665/378221/9789240095137-eng.pdf?sequence=1 (Accessed September 9, 2024).
2. Bentz L, Enel P, Dunais B, Durant J, Poizot-Martin I, Tourette-Turgis C, et al. Evaluating counseling outcome on adherence to prophylaxis and follow-up after sexual HIV-risk exposure: a randomized controlled trial: AIDS Care: Vol 22, No 12 (tandfonline.com).
3. Impact of telephonic psycho-social support on adherence to post-exposure prophylaxis (PEP) after rape: AIDS Care: Vol 22, No 10 (tandfonline.com).
4. Tekalign T, Awoke N, Eshetu K, Gelaw Walle B, Teshome Guta M. HIV/AIDS post-exposure prophylaxis knowledge and uptake among health professionals in Africa: systematic review and meta-analysis. HIV Med. (2022) 23(8):811–24. doi: 10.1111/hiv.13271
5. Mushambi F, Timire C, Harries AD, Tweya H, Goverwa-Sibanda TP, Mungofa S, et al. High post-exposure prophylaxis uptake but low completion rates and HIV testing follow-up in health workers, Harare, Zimbabwe. J Infect Dev Ctries. (2021) 15(4):559–65. doi: 10.3855/jidc.12214
6. Dayyab FM, Iliyasu G, Habib AG. Adherence to HIV postexposure prophylaxis in a Major Hospital in Northwestern Nigeria. Infect Control Hosp Epidemiol. (2018) 39(2):247–8. doi: 10.1017/ice.2017.276
7. Restar AJ, Tocco JU, Mantell JE, Lafort Y, Gichangi P, Masvawure TB, et al. Perspectives on HIV Pre- and post-exposure prophylaxes (PrEP and PEP) among female and male sex workers in Mombasa, Kenya: implications for integrating biomedical prevention into sexual health services. AIDS Educ Prev. (2017) 29(2):141–53. doi: 10.1521/aeap.2017.29.2.141
8. Izulla P, McKinnon LR, Munyao J, Ireri N, Nagelkerke N, Gakii G, et al. Repeat use of post-exposure prophylaxis for HIV among Nairobi-based female sex workers following sexual exposure. AIDS Behav. (2016) 20(7):1549–55. doi: 10.1007/s10461-015-1091-1
9. Ford N, Irvine C, Shubber Z, Baggaley R, Beanland R, Vitoria M, et al. Adherence to HIV postexposure prophylaxis: a systematic review and meta-analysis. AIDS. (2014) 28(18):2721–7. doi: 10.1097/QAD.0000000000000505
10. Jin J, Sun R, Mu T, Jiang T, Dai L, Lu H, et al. Awareness and use of post-exposure prophylaxis for HIV prevention among men who have sex with men: a systematic review and meta-analysis. Front Med (Lausanne). (2021) 8:783626. doi: 10.3389/fmed.2021.783626
11. Olsthoorn AV, Sivachandran N, Bogoch I, Kwantampora J, Kimani M, Kimani J, et al. Barriers to the uptake of postexposure prophylaxis among Nairobi-based female sex workers. AIDS. (2016) 30(1):99–103. doi: 10.1097/QAD.0000000000000884
12. Equity Tool [Internet]. (2024). The EquityTool. Available online at: https://www.equitytool.org/ (Accessed February 5, 2024).
13. Risher KA, Cori A, Reniers G, Marston M, Calvert C, Crampin A, et al. Eaton JW; ALPHA network. Age patterns of HIV incidence in eastern and Southern Africa: a modelling analysis of observational population-based cohort studies. Lancet HIV. (2021) 8(7):e429–39. doi: 10.1016/S2352-3018(21)00069-2
14. Stoner MCD, Nguyen N, Kilburn K, Gómez-Olivé FX, Edwards JK, Selin A, et al. Age-disparate partnerships and incident HIV infection in adolescent girls and young women in rural South Africa. AIDS. (2019) 33(1):83–91. doi: 10.1097/QAD.0000000000002037
15. Logie CH, Wang Y, Lalor P, Williams D, Levermore K. Pre and post-exposure prophylaxis awareness and acceptability among sex workers in Jamaica: a cross-sectional study. AIDS Behav. (2021) 25(2):330–43. doi: 10.1007/s10461-020-02972-5
16. Ayieko J, Petersen ML, Kabami J, Mwangwa F, Opel F, Nyabuti M, et al. Uptake and outcomes of a novel community-based HIV post-exposure prophylaxis (PEP) programme in rural Kenya and Uganda. J Int AIDS Soc. (2021) 24(6):e25670. doi: 10.1002/jia2.25670
17. Ajayi AI, Yusuf MS, Mudefi E, Adeniyi OV, Rala N, Goon DT. Low awareness and use of post-exposure prophylaxis among adolescents and young adults in South Africa: implications for the prevention of new HIV infections. Afr J AIDS Res. (2020) 19(3):242–8. doi: 10.2989/16085906.2020.1811356
18. Miller L, Otieno B, Amboka S, Kadede K, Odeny D, Odhiambo H, et al. “Something like that”: awareness and acceptability of HIV PrEP and PEP among Kenyan adolescents. Int J Behav Med. (2024). doi: 10.1007/s12529-024-10290-6
19. Allan-Blitz LT, Mayer KH. Missed opportunities: a narrative review on why nonoccupational postexposure prophylaxis for HIV is underutilized. Open Forum Infect Dis. (2024) 11(8):ofae332. doi: 10.1093/ofid/ofae332
20. Priddy FH, Adebajo SB, Mamulwar M, Nwachukwu SO, Inyang BJ, Onwumere CC. Ensuring equitable access to quality HIV care for affected populations in Nigeria: experiences from the society for family health. J Int AIDS Soc. (2025) 28(4):e12077709. PMID: 38942977
21. The pre-exposure prophylaxis (PrEP) consciousness of black college women and the perceived hesitancy of public health institutions to curtail HIV in black women | BMC Public Health | Full Text (biomedcentral.com)
22. Uptake and outcomes of a novel community-based HIV post-exposure prophylaxis (PEP) programme in rural Kenya and Uganda - Ayieko - 2021 - Journal of the International AIDS Society - Wiley Online Library.
23. Wang L, Huai P, Jiao K, Liu Y, Hua Y, Liu X, et al. Awareness of and barriers to using non-occupational post-exposure prophylaxis among male clients of female sex workers in two cities of China: a qualitative study. Sex Health. (2021) 18(3):239–47. doi: 10.1071/SH20203
24. Nyblade L, Stockton MA, Saalim K, Rabiu Abu-Ba’are G, Clay S, Chonta M, et al. Using a mixed-methods approach to adapt an HIV stigma reduction to address intersectional stigma faced by men who have sex with men in Ghana. J Int AIDS Soc. (2022) 25(Suppl 1):e25908. doi: 10.1002/jia2.25908
25. Nyblade L, Stockton MA, Giger K, Bond V, Ekstrand ML, Lean RM, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. (2019) 17(1):25. doi: 10.1186/s12916-019-1256-2
26. Lusaka M, Crowley T. Administering human immunodeficiency virus post-exposure prophylaxis: challenges experienced by mothers in Lusaka, Zambia. South Afr J HIV Med. (2021) 22(1):1183. doi: 10.4102/sajhivmed.v22i1.1183
27. Philbin MM, Hirsch JS, Wilson PA, Ly AT, Giang LM, Parker RG. Structural barriers to HIV prevention among men who have sex with men (MSM) in Vietnam: diversity, stigma, and healthcare access. PLoS One. (2018) 13(4):e0195000. doi: 10.1371/journal.pone.0195000
28. Tetteh RA, Nartey ET, Lartey M, Mantel-Teeuwisse AK, Leufkens HGM, Nortey PA, et al. Adverse events and adherence to HIV post-exposure prophylaxis: a cohort study at the korle-bu teaching hospital in Accra, Ghana. BMC Public Health. (2015) 15:573. doi: 10.1186/s12889-015-1928-6
29. Wang Z, Yuan T, Fan S, Qian HZ, Li P, Zhan Y, et al. HIV Nonoccupational postexposure prophylaxis among men who have sex with men: a systematic review and meta-analysis of global data. AIDS Patient Care STDS. (2020) 34(5):193–204. doi: 10.1089/apc.2019.0313
30. Zhou L, Assanangkornchai S. Current perspectives on the determinants of acceptability of Pre-exposure prophylaxis and nonoccupational post-exposure prophylaxis among people at risk for HIV: a scoping review. Int J Environ Res Public Health. (2022) 19(19):12605. doi: 10.3390/ijerph191912605
31. Isano S, Wong R, Logan J, El-Halabi S, El-Khatib Z. Barriers to post exposure prophylaxis use among men who have sex with men in sub-saharan Africa: an online cross-sectional survey. Prev Med Rep. (2020) 19:101100. doi: 10.1016/j.pmedr.2020.101100
32. Real-time monitoring and just-in-time intervention for adherence to pre-exposure prophylaxis among men who have sex with men in China: a multicentre RCT study protocol | BMC Public Health | Full Text (biomedcentral.com)
33. Identifying Best Practices for Increasing HIV Pre-exposure Prophylaxis (PrEP) Use and Persistence in the United States: A Systematic Review | AIDS and Behavior (springer.com)
34. Abrahams N, Jewkes R. Barriers to post exposure prophylaxis (PEP) completion after rape: a South African qualitative study. Cult Health Sex. (2010) 12(5):471–84. doi: 10.1080/13691050903556316
35. Beer L, Williams D, Tie Y, McManus T, Yuan AX, Crim SM, et al. The capacity of HIV care facilities to implement strategies recommended by the ending the HIV epidemic initiative: the medical monitoring project facility survey. J Acquir Immune Defic Syndr. (2023) 94(4):290–300. doi: 10.1097/QAI.0000000000003290
36. Nyblade L, Ndirangu JW, Speizer IS, Browne FA, Bonner CP, Minnis A, et al. Stigma in the health clinic and implications for PrEP access and use by adolescent girls and young women: conflicting perspectives in South Africa. BMC Public Health. (2022) 22(1):1916. doi: 10.1186/s12889-022-14236-z
37. Smith MK, Xu RH, Hunt SL, Wei C, Tucker JD, Tang W, et al. Combating HIV stigma in low- and middle-income healthcare settings: a scoping review. J Int AIDS Soc. (2020) 23(8):e25553. doi: 10.1002/jia2.25553
38. Cai X, Fisher CB, Alohan D, Tellone S, Grov C, Cohall A, et al. Sexual and gender minority Individuals’ interest in sexual health services at collective sex venues in New York city. AIDS Behav. (2023) 27(3):761–71. doi: 10.1007/s10461-022-03808-0
39. Malama K, Logie CH, Narasimhan M, Ouedraogo L, Asmani C, Elamin H, et al. Short communication: awareness of HIV self-care interventions across global regions: results from a values and preferences survey. AIDS Res Hum Retroviruses. (2022) 38(8):645–8. doi: 10.1089/aid.2021.0200
40. Nyamuzihwa T, Tembo A, Martyn N, Venter F, Maimin J, Houghton J, et al. The South African community pharmacy sector-an untapped reservoir for delivering HIV services. Front Reprod Health. (2023) 5:1173576. doi: 10.3389/frph.2023.1173576
41. Brennan LM, Stickney KE, Allen GP, Springer S, Dube A, Bolduc C. Specialty pharmacy interventions benefit patients receiving HIV post-exposure prophylaxis. J Am Pharm Assoc (2003). (2024) 64(4):101915. doi: 10.1016/j.japh.2023.09.001
42. Kabami J, Koss CA, Sunday H, Biira E, Nyabuti M, Balzer LB, et al. Randomized trial of dynamic choice HIV prevention at antenatal and postnatal care clinics in rural Uganda and Kenya. J Acquir Immune Defic Syndr. (2024) 95(5):447–55. doi: 10.1097/QAI.0000000000003383
Keywords: HIV prevention, health-disparate minority and vulnerable populations, sexual and gender minorities, drug users, sex workers, transgender persons, WHO
Citation: El-Sahn M, Elliott R, El-Sahn M, Garcia-Gurtubay I, Kong K, Wood Santos T, Mulwa R, Muthoka E and Lucas J (2025) Qualitative and quantitative research on preferences and perceptions regarding HIV post-exposure prophylaxis among young women, men, female sex workers, members of the LGBTQ + community and people who inject drugs in Kenya, Nigeria and Zimbabwe. Front. Reprod. Health 7:1606013. doi: 10.3389/frph.2025.1606013
Received: 4 April 2025; Accepted: 1 September 2025;
Published: 9 October 2025.
Edited by:
Teiichiro Shiino, National Center For Global Health and Medicine, JapanReviewed by:
Dazon Dixon Diallo, SisterLove Inc, United StatesPerez Livias Moyo, National University of Science and Technology, Zimbabwe
Copyright: © 2025 El-Sahn, Elliott, El-Sahn, Garcia-Gurtubay, Kong, Wood Santos, Mulwa, Muthoka and Lucas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Moushira El-Sahn, bW91c2hpcmFAcm91dGVzMnJlc3VsdHMub3Jn
 Moushira El-Sahn
Moushira El-Sahn Rose Elliott1
Rose Elliott1 Trisha Wood Santos
Trisha Wood Santos