- 1Department of Social Policy and Intervention, University of Oxford, Oxford, United Kingdom
- 2Desmond Tutu HIV Centre, University of Cape Town, Cape Town, South Africa
- 3MRC International Statistics and Epidemiology Group, Department of Infectious Disease Epidemiology, London School of Hygiene & Tropical Medicine, London, United Kingdom
- 4Centre for Social Science Research, Department of Sociology, University of Cape Town, Cape Town, South Africa
- 5Department of Psychiatry, University of Cape Town, Cape Town, South Africa
Introduction: Pregnant or parenting adolescent girls and young women (PPYW) are at greater risk of sexual exposure to HIV than their peers, yet tailored HIV prevention efforts for PPYW remain limited.
Methods: We analysed cross-sectional data (2020–2023) from a sample of PPYW (median age 21.5, IQR = 20.3–22.5) in the Eastern Cape, South Africa.
Results: Approximately 88% of PPYW who were HIV-negative (n = 646) had a HIV test in the last few years. Of these—58% knew about PrEP (n = 328). Of those who knew about PrEP, 31% had ever been offered PrEP (n = 100; 15% of HIV-negative PPYW), and 62% of those who were offered PrEP had ever taken PrEP (n = 62; 10% of HIV-negative PPYW). Compared to PPYW who have not had a HIV test in the last few years, PPYW who had accessed HIV testing were more likely to be aware of PrEP (aOR = 2.39, 95% CI:1.44–3.97, p = 0.001), have been offered PrEP (aOR = 2.96, 95% CI:1.16–7.55, p = 0.023), and taken PrEP (aOR = 4.57, 95% CI:1.09–19.16, p = 0.038).
Conclusions: This study highlights missed opportunities in PrEP delivery and offers recommendations to enhance PrEP awareness and uptake among PPYW. Despite high HIV testing rates in this key population, awareness of PrEP, its offer, and uptake remain low.
1 Introduction
Pregnant or parenting adolescent girls and young women (PPYW) face a heightened risk of acquiring HIV due to a mix of biological vulnerability and social and structural inequalities (1–3). This group is a key priority for HIV prevention in Eastern and Southern Africa, where they continue to carry a disproportionate share of new infections. In 2023, adolescent girls and young women (AGYW) were three times more likely to acquire HIV compared to males of the same age (4). South Africa remains at the epicentre of the epidemic, with close to eight million people living with HIV (5). Oral pre-exposure prophylaxis (PrEP) offers strong protection against HIV when taken consistently and plays an important role in preventing mother-to-child transmission during pregnancy for women who are HIV-negative (6).
Since its introduction in South Africa in 2016, oral PrEP has been a key component of the country's HIV prevention strategy (7). PrEP is safe to use during pregnancy and breastfeeding, and in 2020, South Africa updated its national guidelines to include pregnant and breastfeeding women (PBW) who test negative on routine HIV testing in the eligibility criteria for PrEP (8–10). Moreover, the guidelines identify PBW as a key population at heightened risk of HIV exposure, and stipulate that they should receive counselling and be offered HIV prevention measures, including PrEP (7). The policy shift recognised the vulnerabilities faced by PPYW, highlighting the importance of scaling up HIV prevention within this group (7). Recent research has also highlighted the importance of understanding PrEP uptake and use among pregnant and breastfeeding women, a high-priority population for HIV prevention (11–13). The 2022 South Africa Antenatal HIV Sentinel Survey reported low levels of PrEP awareness and coverage among pregnant women, highlighting the need to better understand gaps in PrEP awareness and uptake among this population (14). But much of the research to date has centred on adult populations, with limited attention given to the specific experiences and needs of young women, especially PPYW.
Studies from Eastern and Southern Africa suggest that PPYW face a higher likelihood of living with HIV than their peers who have not had children (15, 16). This increased risk is shaped by a range of factors, including relationships with older partners, experiences of transactional sex, and irregular or infrequent condom use. Many only begin using contraception after their first pregnancy and often rely on methods like injectables or oral contraceptives, which offer no protection against HIV (15). As a result, they remain vulnerable to HIV infection during earlier and subsequent periods of sexual activity (17, 18). Furthermore, PPYW often face exacerbated challenges, including school drop-out, unemployment, poverty, social isolation, loss of social support, stigma, and negative experiences at health facilities, all of which act as barriers to PrEP access and uptake (19–25). Limited exposure to comprehensive sexual education due to school drop-out could also impact HIV prevention awareness among PPYW (26). Yet PPYW are under-researched in HIV prevention, especially regarding PrEP.
A scoping review examining factors influencing PrEP uptake and continuation among AGYW identified several key barriers, including low awareness of PrEP, limited access to health services, and negative experiences with clinic staff (27). Furthermore, fears related to potential effects on their foetus during pregnancy and navigating the postpartum period poses additional challenges for PPYW, further highlighting this population to be a priority population for PrEP interventions (27). Evidence also suggests that sociodemographic factors, including younger age and lower socioeconomic status, significantly influence PrEP awareness, uptake and continuation among AGYW (28–30). Understanding how these factors affect PrEP uptake is key to developing effective, context-specific interventions to increase PrEP utilisation among PPYW.
This study used a PrEP cascade framework to investigate awareness, reach, and uptake among PPYW in a PrEP-naïve community. The PrEP cascade is used as an implementation science tool to identify gaps in the delivery of HIV prevention services, particularly among underserved populations (31). Applying this framework enables a stepwise analysis of where and why PPYW may be lost along the PrEP pathway—from HIV testing to PrEP awareness, offer, and uptake. offering insights into where interventions may be needed to better reach PPYW. To our knowledge, this is one of the first studies to apply a PrEP cascade specifically among PPYW, a group recognised as being at very high risk for HIV but often overlooked in prevention research. Data were collected between 2020 and 2023, soon after the PrEP guidelines in South Africa was extended to pregnant and breastfeeding women. Despite this policy change, PrEP was rarely offered to PPYW in our study, underscoring persistent barriers in service delivery and signalling missed prevention opportunities at a critical stage of programme expansion.
2 Methods
2.1 Study design and participants
This study is a cross-sectional analysis of longitudinal cohort, which surveyed 986 PPYW (including those living with HIV) in the Eastern Cape, South Africa between December 2020 and March 2023. The baseline data collection occurred between 2018 and 2019. Participants were recruited through a combination of strategies including: through an existing study, schools, door-to-door, malls, referrals, and through public health-care facilities [more detail on the recruitment strategy is described elsewhere (17)]. The study took place in a peri-urban and rural health district of the Eastern Cape province, which had the second highest antenatal HIV prevalence rates in South Africa at 32.9% in 2022 (32).
In 2020–2023, 87% of participants who participated at baseline (2018–2019) were re-interviewed, with 2% refusing (n = 24), 10% lost to follow-up (n = 113), and 1% passed away (n = 9). All eligible participants who completed follow-up interviews were included in this study; missing data were minimal and participants with missing values for key measures were excluded from analysis. This study utilised cross-sectional data from the most recent follow-up, as PrEP-related information was not collected at baseline (2018–2019). This reflects the timing of the inclusion of pregnant and breastfeeding women in national PrEP rollout in South Africa, which began in 2020. All participants in this cohort were recruited as mothers under 24 years of age at baseline. As this analysis uses follow-up data, some participants had aged beyond 24 by the time of data collection, resulting in an upper age limit of 28. Including these participants allows us to capture the experiences of young mothers as they transition into later young adulthood.
2.2 Data collection
Trained research assistants conducted telephone interviews with participants during remote data collection activities necessitated by COVID-19 lockdown restrictions, which began at the end of March in 2020 and ended in June 2022. Although data collection continued until March 2023, we continued using remote methods to ensure participant safety and study continuity. Structured questionnaires were administered in participants' preferred language (isiXhosa or English) (33). Questionnaires were translated from English into isiXhosa, and then back-translated into English to ensure accuracy and cultural appropriateness. The full questionnaires for the study are available at https://www.heybaby.org.za/research, and the measures used in this analysis can be found in Supplementary Appendix S1. The questionnaire was developed using validated measures that had been previously applied in South Africa where possible. For constructs without existing local measures, items were developed by the study team, drawing on prior literature and tailored to the context of the participants. Data collection tools were piloted with a subset of participants to ensure clarity and appropriateness (25).
2.3 Ethical considerations
The study received ethical approval from the Universities of Oxford (CUREC ref: R48876/RE003) and Cape Town (HREC ref: 226/2017; 027/2024), and local governmental and provincial bodies. Informed consent was obtained from all participants, and from their caregivers for participants who were <18 years old. Measures were taken to ensure their privacy and confidentiality throughout the study. Participants were not given any financial incentives but received airtime/data worth R30.00 as a token of appreciation.
2.4 Measures
The primary outcome for this analysis is the PrEP cascade, adapted from HIV prevention cascades in existing literature (34). In this study, each step was measured using binary variables. The PrEP cascade begins by assessing whether participants had accessed HIV testing since their baseline interview (2017–2019), with an average interval of three years between interviews, as HIV testing is expected to facilitate subsequent PrEP offer in accordance with South African guidelines (7). We then assessed awareness of PrEP (HIV-negative participants were asked “Do you know about PrEP?” after a brief introduction and explanation of PrEP—yes vs. no). This was followed by whether participants were ever offered PrEP (only those who responded that they knew PrEP answered: “Have you ever been offered PrEP?”—yes vs. no), and finally whether they had ever taken PrEP when offered (only those who said they were offered PrEP answered: “Have you ever taken PrEP?”—yes vs. no).
Binary variables were created from survey questions. Sociodemographic factors include age (<20 years old vs. ≥20 years old), and age at first childbirth (<20 years old vs. ≥20 years old). The <20 years age cut-off was selected based on national definitions of adolescent childbearing used in South African demographic and health research (35). Other factors include multiple parity (≥2 children vs. only one child), enrolled in school or in employment (vs. not enrolled in school or employed), type of housing (formal vs. informal), household poverty [ability to afford the eight highest socially-perceived necessities, based on South African survey measures—including school fees, school uniform, school supplies, shoes, clothes—vs. lack of access (35)], and food insecurity (at least one day without enough food at home in the past week vs. enough food).
Factors on clinic experiences were also included to identify whether clinic experiences impacted PrEP uptake, as seen in other studies identified in a scoping review (27). These were measured through perceived interactions with clinic staff using binary variables: staff never displaying anger, clinic staff always having time to provide necessary assistance, and participants' confidence that their information would be kept safe and confidential. All measures were self-reported (details on all measures can be found in Supplementary Appendix S1).
2.5 Statistical analysis
First, descriptive analyses were conducted to examine the relationship between one's history of HIV testing since baseline with socio-demographic variables and the PrEP cascade. Participants who had not tested for HIV were retained in the denominator at each step of the cascade, ensuring that their awareness, offer, and uptake of PrEP were captured and directly comparable to those who had tested. Secondly, multivariable logistic regression was used to evaluate the association between HIV testing and the PrEP cascade steps (awareness, offer, and uptake), controlling for sociodemographic variables including age, age at first childbirth, multiple parity, enrolled in school or working, type of housing, household poverty, and food insecurity. Adjusted odds ratios (aORs) with 95% confidence intervals (CIs) are reported to assess the strength of these associations. Statistical significance was defined as p < 0.05.
Finally, stepwise multivariable regression models were used to identify factors significantly associated with PrEP awareness. For the smaller samples of PrEP offered (n = 100) and PrEP taken (n = 62), stepwise regression was deemed inappropriate due to the increased risk of overfitting and unreliable parameter estimates. We selected variables for the models following Hosmer and Lemeshow's purposeful selection of variables, based on theoretical considerations from existing literature (36). In the first model, we applied forward selection and included all sociodemographic factors, HIV testing, and clinic experience variables hypothesised as potential covariates. The second model included only factors that were significant at a 10% level (p < 0.1). The third and final model included only factors significant at the 5% level (p < 0.05). The goodness-of-fit of the logistic regression model was assessed using the Hosmer-Lemeshow test (36). All analysis was conducted using STATA17 (37).
3 Results
The study included n = 646 HIV-seronegative PPYW, aged 16–28 years (median age 21.5, IQR = 20.3–22.5). One in five (20%, n = 130) were <20 years old, and the majority (96%, n = 604) had their first child before age 20. Only 2% were pregnant at the time of data collection. Almost one in four (23%, n = 149) had two or more children, and 32% (n = 206) lived in informal housing. Only 13% (n = 83) lived with no poverty (household could afford all basic necessities), and 36% (n = 234) did not experience food insecurity in the past week. More than half (55%, n = 355) were either in school/university or employed (see Table 1).
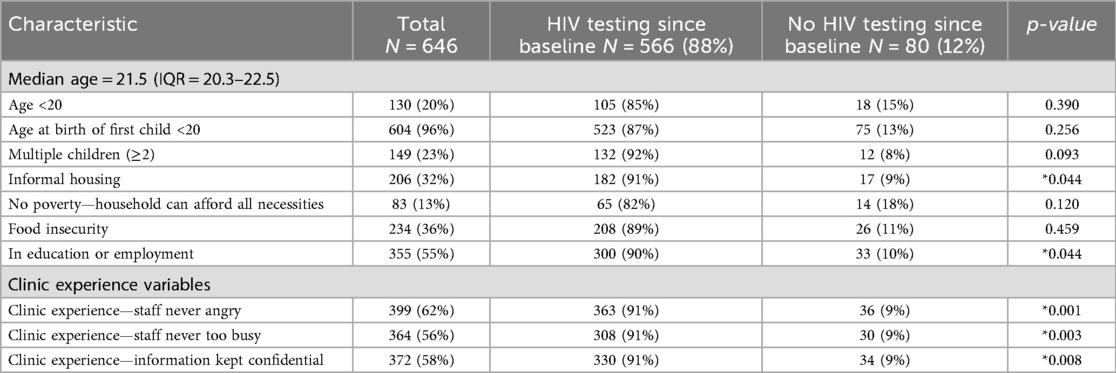
Table 1. Sample characteristics of pregnant or parenting adolescent girls and young women in the Eastern Cape, South Africa (2020–2023).
3.1 The PrEP cascade
Among those surveyed, 88% (n = 566) reporting having had a HIV test since baseline. However, cascade progression dropped steeply at each step: only 58% of those tested (n = 328) were aware of PrEP; among those aware, only 31% (n = 100) had ever been offered PrEP; and among those offered PrEP, 62% (n = 62) had ever taken PrEP (see Figure 1). Among the 80 participants who did not report having a HIV test since baseline, 33% (n = 26) were aware of PrEP, 6% (n = 5) had been offered PrEP, and 3% (n = 2) reported ever initiating PrEP.
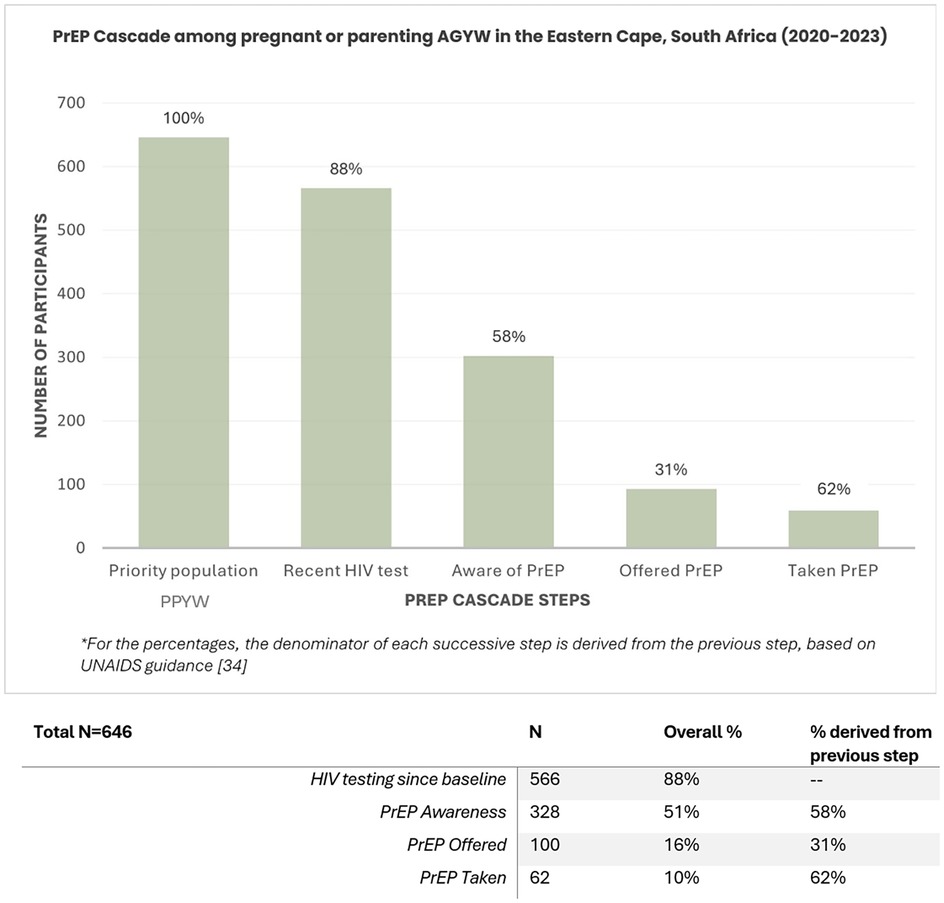
Figure 1. PrEP Cascade among pregnant or parenting adolescent girls and young women in Eastern Cape, South Africa (2020-2023).
In adjusted multivariable regression models, HIV testing was significantly associated with advancing through all stages of the PrEP cascade among PPYW, after adjusting for age, parity, school enrolment or employment, poverty status, food insecurity, and housing type. PPYW who had accessed HIV testing since baseline were two times more likely to be aware of PrEP (aOR = 2.39, 95% CI: 1.44–3.97, p = 0.001). HIV testing was also significantly associated with higher odds of PPYW being offered PrEP (aOR = 2.96, 95% CI: 1.16–7.55, p = 0.023), and with higher rates of PrEP uptake (aOR = 4.57, 95% CI: 1.09–19.16, p = 0.038) (see Table 2).
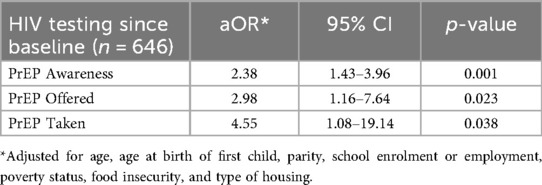
Table 2. Multivariable regression results for associations between HIV testing since baseline and prEP awareness, offer, and uptake among pregnant or parenting adolescent girls and young women in the eastern cape, South Africa (2020–2023).
3.2 Factors associated with PrEP awareness in stepwise regression
The Hosmer-Lemeshow test indicated a satisfactory fit with a chi-square statistic of 0.06 and a p-value of 0.9715, suggesting that the model adequately represents the observed data (36). The final model of the stepwise regression indicates a few significant predictors of PrEP awareness among participants (see Table 3). School enrolment/being employed was the only sociodemographic variable that was significantly associated with increased PrEP awareness (aOR = 1.66; 95% CI: 1.21–2.27, p = 0.002). HIV testing since baseline remained significantly associated with increased PrEP awareness (aOR = 2.13; 95% CI: 1.29–3.53, p = 0.003). Positive clinic experience as reported by absence of anger from clinic staff was also significantly associated with greater PrEP awareness (OR = 1.46; 95% CI: 1.05–2.03, p = 0.023).
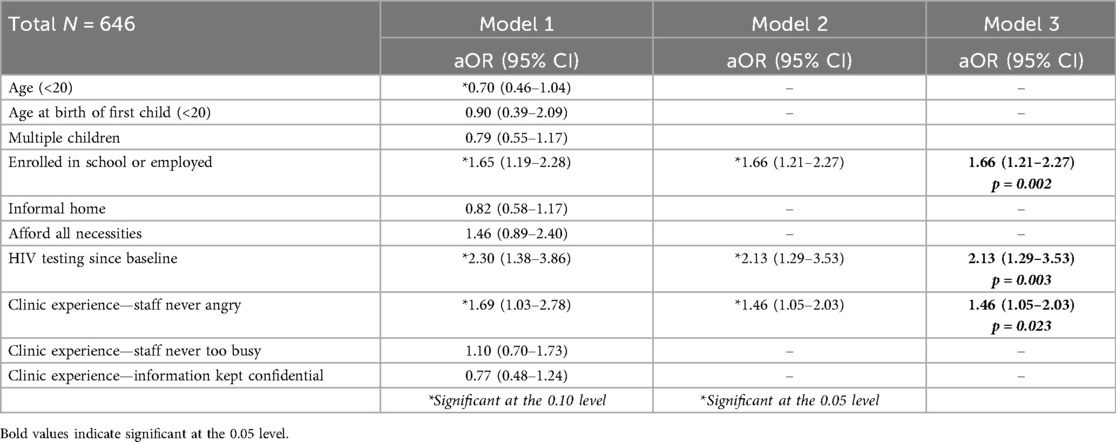
Table 3. Factors associated with PrEP awareness among pregnant or parenting adolescent girls and young women in the Eastern Cape, South Africa (2020–2023).
4 Discussion
Using a PrEP cascade framework, our findings show gaps in PrEP awareness, offer, and uptake among PPYW in South Africa, a population at heightened risk of HIV acquisition, but insufficiently reached by existing HIV prevention programmes. This study was conducted in a community with limited prior exposure to PrEP; there were no widespread PrEP programmes in place at the time of data collection. Therefore, the low levels of awareness and offer observed are likely reflective of broader systemic issues in introducing and scaling up PrEP in settings where it has not yet been meaningfully implemented. Even among PPYW who were recently in contact with the healthcare system, including HIV testing, only half were aware of PrEP and fewer than one in five had ever been offered it. Yet, among those offered PrEP, nearly two-thirds reported initiating it, suggesting unmet demand and underutilised opportunities within existing service delivery platforms—aligning with findings from previous studies (27).
These findings show that there are critical gaps in the implementation of PrEP within routine care and the missed opportunities to engage this key population through existing health system touchpoints. Our results align with recent guidance from AVAC, which emphasises the need for youth-focused PrEP delivery in South Africa and other countries in the region and highlighting the importance of closing implementation gaps to reach adolescent and young populations effectively (38). Similar gaps in PrEP cascades and barriers to PrEP access have been observed in studies, including DREAMS, conducted in other sub-Saharan African countries such as Kenya, Uganda and Zimbabwe, as synthesised in our recent scoping review (25). This suggest that these gaps are not unique to PPYW in South Africa, highlighting the need for regional strategies to strengthen service delivery and expanding equitable access.
Our findings indicate that the primary gap in the PrEP cascade is between HIV testing and PrEP offer. While most participants had recently had HIV testing, the majority had not been offered PrEP. Among PPYW who were offered PrEP, approximately two-thirds accepted it. Although we did not directly ask participants whether they interested in taking PrEP, the observed pattern suggest that low uptake may not be due to lack of interest but because of limited access, consistent with findings from studies. Previous research has highlighted potential provider or system-level barriers, such as inconsistent risk assessments, limited provider capacity or confidence, or lack of adherence to PrEP guidelines (27, 31, 39, 40). Although South African PrEP guidelines recommend offer to individuals at substantial risk, it remains unclear whether PPYW are being systematically assessed or categorised as eligible.
PrEP should be made available and accessible in services that are already accessed by PPYW, including sexual reproductive health, family planning, and child health clinics. This requires not only policy alignment but also the allocation of resources, training, and support to overcome existing barriers to integration (41, 42). Looking ahead, as long-acting PrEP modalities such as the dapivirine vaginal ring and injectables, i.e., Cabotegravir (bi-monthly) and Lenacapavir (twice-yearly), becomes more widely available, effective integration would also be crucial to maximise their uptake and adherence among PPYW—a key population that could benefit significantly from long-acting PrEP (43–45). Given the low levels of PrEP offer observed in our cascade, ensuring that PPYW are informed about and offered long-acting PrEP modalities will be critical to maximising uptake and adherence in this underserved population and to closing gaps in the PrEP cascade.
In our study, PPYW who were not engaged in school or work were less likely to be aware of PrEP. This suggests that they may be more socially and economically marginalised, with fewer opportunities for health education and service uptake. Previous research has identified pregnancy and early motherhood as major drivers of school dropout among AGYW in South Africa, and few return to finish their education, limiting future employment opportunities (22–24). The DREAMS PrEP Choice Study in South Africa found that most participants received services from educational and training institutions (46). These findings highlight the importance of targeted outreach strategies beyond formal institutions to reach PPYW who are structurally and socially marginalised. Addressing barriers like inflexible health services, limited access to information platforms, as well as low educational attainment and poverty, may help to increase PrEP adherence among these underserved young women (47, 48).
In addition, PPYW are often stigmatised and face judgemental attitudes from health care workers due to being young mothers, which is a well-documented barrier to healthcare (19, 20). Not experiencing anger from clinic staff when discussing sensitive topics was associated with higher PrEP awareness. This finding reinforces the critical role of a supportive, non-judgmental healthcare environment in promoting PrEP awareness for young women, as shown in other studies (27).
4.1 Limitations
The cross-sectional approach does not allow for causal associations to be established between predictors and PrEP cascade outcomes, and we cannot determine the directionality of associations. The possibility for reversed associations cannot be ruled out (e.g., whether increased PrEP awareness leads to increased HIV testing) or the potential effects of confounding factors on observed associations. The reliance on self-reported data for HIV testing, PrEP awareness, and uptake may have introduced bias because clinic records were not obtained. PrEP awareness was measured using a single binary question, which does not capture participants' depth of knowledge, including understanding of side effects or adherence requirements. Participants may have been likely to underreport their use of PrEP due to stigma around disclosing sexual activity and community stigma around PrEP due to its connection with HIV, potentially leading to an underestimation of PrEP coverage in the study findings. While validated measures were used where possible, some questionnaire items were adapted or developed for this study; however, they were piloted with a subset of participants to ensure clarity and relevance. We also could not conduct stepwise regression with PrEP offer and uptake due to the small sample sizes for the two variables. In addition, although uptake among participants who were offered PrEP was relatively high, our data cannot confirm whether this is due to selective offering by providers.
While recruitment strategies focused on creating a representative sample of PPYW through health facility- and community-based recruitment, findings may not be generalisable to PPYW in different regions of South Africa or other countries with distinct cultural, economic, or healthcare contexts. This study was conducted during the period of South Africa's COVID-19 lockdowns and the period of recovery. As such, it offers valuable insight into how PrEP access and uptake among PPYW were shaped during a time of significant disruption as well as in the months that followed. We also did not collect data on PrEP persistence, which would provide valuable insights for this population in future research. We also did not collect data on PrEP awareness among participants who reported living with HIV; examining this in future research could provide valuable insights.
5 Conclusions
This study showed how, despite their elevated HIV acquisition risk, PPYW in South Africa continue to be left behind in HIV prevention programmes. In communities where PrEP has not been introduced through implementation programmes, awareness is low, and opportunities to deliver it during routine healthcare are missed. Our findings highlight the fact that many participants had recent contact with health services but were not informed of or offered PrEP, indicating systemic inadequacies rather than a lack of demand. Improving access means more than just making PrEP available—it needs to be integrated into the services PPYW already use, such as antenatal clinics, child health visits, and sexual and reproductive healthcare. However, for this to work, health workers need to receive practical support and training, and clinics must provide a safe, non-judgmental environment for young women.
At the same time, broader challenges that PPYW face need to be considered. Barriers such as dropping out of education early and limited employment opportunities all influence how and whether young moms may seek or keep healthcare. Tackling these concerns in conjunction with service delivery improvements will be critical to ensure that PPYW does not fall behind. Being out of school or unemployed can cut people off from information and can make clinic visits difficult. Policies and services that support education, employment, and parenting could make a meaningful difference in their ability to engage with healthcare. As longer-acting PrEP options become available, these findings offer practical insights into how programmes can better meet the needs of young pregnant or parenting women. PPYW are often left out of HIV prevention strategies. Reaching them with the right tools, delivered in the right ways, is essential to reducing new infections in this priority population.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available due to privacy or ethical restrictions. Requests to access the datasets should be directed to https://static1.squarespace.com/static/5ef06d788b06a83de4933740/t/64941fdf78be1d23e279538a/1687429087463/20190513_DataUseUndertaking_MASTER.pdf.
Ethics statement
The study received ethical approval from the Universities of Oxford and Cape Town, and local governmental and provincial bodies. Informed consent was obtained from all participants, and from their caregivers for participants who were >18 years old.
Author contributions
JC-C: Formal analysis, Methodology, Writing – original draft, Investigation, Writing – review & editing, Conceptualization. LB: Supervision, Conceptualization, Writing – review & editing. JJ: Investigation, Writing – review & editing, Data curation. CW: Investigation, Data curation, Writing – review & editing. LC: Funding acquisition, Writing – review & editing, Conceptualization. ET: Writing – review & editing, Conceptualization, Investigation, Funding acquisition, Supervision.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the UKRI GCRF Accelerating Achievement for Africa’s Adolescents (Accelerate) Hub (Grant Ref: ES/S008101/1); the Fogarty International Center, National Institute on Mental Health, National Institutes of Health under Award Number K43TW011434 (the content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health); the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (no. 771468); Oak Foundation [Grant Number: OFIL-20-057]; and the National Research Foundation: Human and Social Dynamics for Development 2022 [Grant number: 136531].
Acknowledgments
We express our profound gratitude to all research participants, as well as their families and communities, for their time and interest in participating in the HEY BABY Study. The HEY BABY Fieldwork Team was responsible for the data collection. We are also grateful to members of the HEY BABY research team who contributed to data cleaning and preparation. Furthermore, all research tools and data collection methods were developed in consultation with the Teen Advisory Group. We would also like to thank Professor Francesca Little (Professor of Statistics, University of Cape Town) for reviewing the statistical analysis conducted in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frph.2025.1648786/full#supplementary-material
References
1. Lewis L, Kharsany ABM, Humphries H, Maughan-Brown B, Beckett S, Govender K, et al. HIV Incidence and associated risk factors in adolescent girls and young women in South Africa: a population-based cohort study. PLoS One. (2022) 17(12):e0279289. doi: 10.1371/journal.pone.0279289
2. Harrison A, Colvin CJ, Kuo C, Swartz A, Lurie M. Sustained high HIV incidence in young women in Southern Africa: social, behavioral, and structural factors and emerging intervention approaches. Curr HIV/AIDS Rep. (2015) 12(2):207–15. doi: 10.1007/s11904-015-0261-0
3. Dellar RC, Dlamini S, Karim QA. Adolescent girls and young women: key populations for HIV epidemic control. J Int AIDS Soc. (2015) 18(2 Suppl 1):64–70. doi: 10.7448/ias.18.2.19408
4. Joint United Nations Programme on HIV/AIDS. UNAIDS report. The Urgency of now: AIDS at a Crossroads—2024 Global AIDS Update. Geneva (2024). Available online at: https://www.unaids.org/sites/default/files/media_asset/2024-unaids-global-aids-update_en.pdf (Accessed May 12, 2025).
5. Joint United Nations Programme on HIV/AIDS. South Africa | UNAIDS Country Factsheets. (2024). Available online at: https://www.unaids.org/en/regionscountries/countries/southafrica (Accessed October 21, 2024).
6. Joseph Davey DL, Bekker LG, Gomba Y, Coates T, Myer L, Johnson LF. Modelling the potential impact of providing pre-exposure prophylaxis (PrEP) in pregnant and breastfeeding women in South Africa. AIDS. (2019) 33(8):1391. doi: 10.1097/QAD.0000000000002221
7. National Department of Health South Africa. Updated Guidelines for the Provision of Oral Pre-Exposure Prophylaxis (PrEP) to Persons at Substantial Risk of HIV Infection 2021. (2021). Available online at: https://knowledgehub.health.gov.za/system/files/elibdownloads/2023-04/PrEP%2520Guidelines%2520Update%252012%2520%2520Nov%2520%25202021%2520Final.pdf (Accessed September 17, 2024).
8. Bekker LG, Brown B, Joseph-Davey D, Gill K, Moorhouse M, Delany-Moretlwe S, et al. Southern African Guidelines on the safe, easy and effective use of pre-exposure prophylaxis: 2020. South Afr J HIV Med. (2020) 21(1):1152. doi: 10.4102/sajhivmed.v21i1.1152
9. Mofenson LM, Munderi P. Safety of antiretroviral prophylaxis of perinatal transmission for HIV-infected pregnant women and their infants. J Acquir Immune Defic Syndr. (2002) 30(2):200–15. doi: 10.1097/00042560-200206010-00010
10. Davey J, Pintye DL, Baeten J, Aldrovandi JM, Baggaley G, Bekker R, et al. Emerging evidence from a systematic review of safety of pre-exposure prophylaxis for pregnant and postpartum women: where are we now and where are we heading? J Int AIDS Soc. (2020) 23(1):e25426. doi: 10.1002/jia2.25426
11. Joseph Davey D, Malaba TR. Oral PrEP safety in pregnancy with longitudinal follow-up of children for 36 months. Lancet Glob Health. (2025) 13(3):e379–80. doi: 10.1016/s2214-109x(24)00531-x
12. Joseph Davey DL, Bekker LG, Gorbach PM, Coates TJ, Myer L. Delivering PrEP to pregnant and breastfeeding women in sub-Saharan Africa: the implementation science frontier. AIDS. (2017) 31(16):2193. doi: 10.1097/QAD.0000000000001604
13. Chen-Charles J, Vos D, Vundhla L, Gebengu P, Rousseau A, Bekker E, et al. Empowering Women’s PrEP choices: qualitative insights into long-acting PrEP preferences and decision-making during pregnancy and breastfeeding in South Africa and Botswana. AIDS Beha. (2025) 2025:1–16. doi: 10.1007/s10461-025-04856-y
14. Shangase N, Kufa T, Cheyip M, Puren A. PrEP awareness and coverage: results from the 2022 South Africa antenatal HIV sentinel survey. AIDS Behav. (2025) 29(5):1692–703. doi: 10.1007/s10461-024-04609-3
15. Toska E, Laurenzi CA, Roberts KJ, Cluver L, Sherr L. Adolescent mothers affected by HIV and their children: a scoping review of evidence and experiences from sub-Saharan Africa. Glob Public Health. (2020) 15(11):1655–73. doi: 10.1080/17441692.2020.1775867
16. Groves AK, Gebrekristos LT, Smith PD, Stoebenau K, Stoner MC, Ameyan W, et al. Adolescent mothers in eastern and Southern Africa: an overlooked and uniquely vulnerable subpopulation in the fight against HIV. J Adolesc Health. (2022) 70(6):895–901. doi: 10.1016/j.jadohealth.2021.12.012
17. Toska E, Cluver L, Laurenzi CA, Wittesaele C, Sherr L, Zhou S, et al. Reproductive aspirations, contraception use and dual protection among adolescent girls and young women: the effect of motherhood and HIV status. J Int AIDS Soc. (2020) 23(5):e25558. doi: 10.1002/jia2.25558
18. Groves AK, Maman S, Stankard PH, Gebrekristos LT, Amon JJ, Moodley D. Addressing the unique needs of adolescent mothers in the fight against HIV. J Int AIDS Soc. (2018) 21(6):e25155. doi: 10.1002/jia2.25155
19. Marais L, Brown JL, Sharp C, Sales JM, Lenka M, Rani K, et al. Youth-centered clinics: the voices of adolescent sesotho-speaking girls from mangaung, South Africa. Sage Open. (2022) 12(2):1–7. doi: 10.1177/21582440221089969
20. Sewpaul R, Crutzen R, Dukhi N, Sekgala D, Reddy P. A mixed reception: perceptions of pregnant adolescents’ experiences with health care workers in Cape Town, South Africa. Reprod Health. (2021) 18(1):167. doi: 10.1186/s12978-021-01211-x
21. Anakpo G, Kollamparambil U. Teenage motherhood and child outcomes: evidence from South Africa. South Afr J Childhood Educ. (2021) 11:1–21. doi: 10.4102/sajce.v11i1.972
22. Commission for Gender Equality. Learner pregnancy-policy interplay: School dropout of adolescent girls during pregnancy and in the postpartum period in selected South African provinces. (2023). Available online at: https://cge.org.za/wp-content/uploads/2023/07/cge-teenage-pregnacy-report.pdf (Accessed September 17, 2024).
23. Ardington C, Menendez A, Mutevedzi T. Early childbearing, human capital attainment, and mortality risk: evidence from a longitudinal demographic surveillance area in rural-KwaZulu-Natal, South Africa. Econ Dev Cult Change. (2015) 63(2):281–317. doi: 10.1086/678983
24. Jochim J, Meinck F, Steventon Roberts KJ, Wittesaele C, Langwenya N, Toska E, et al. Which factors affect postpartum educational enrollment of adolescent mothers in South Africa? A latent class analysis. Psychol Health Med. (2022) 27(sup1):138–54. doi: 10.1080/13548506.2022.2108085
25. Toska E, Saal W, Chen Charles J, Wittesaele C, Langwenya N, Jochim J, et al. Achieving the health and well-being sustainable development goals among adolescent mothers and their children in South Africa: cross-sectional analyses of a community-based mixed HIV-status cohort. PLoS One. (2022) 17(12):e0278163. doi: 10.1371/journal.pone.0278163
26. George G, Beckett S, Reddy T, Govender K, Cawood C, Khanyile D, et al. Role of schooling and comprehensive sexuality education in reducing HIV and pregnancy among adolescents in South Africa. J Acquir Immune Defic Syndr. (2022) 90(3):270–5. doi: 10.1097/QAI.0000000000002951
27. Chen-Charles J, Joseph Davey D, Toska E, Seeley J, Bekker LG. PrEP uptake and utilisation among adolescent girls and young women in Sub-Saharan Africa: a scoping review. AIDS Behav. (2025) 2025:1–21. doi: 10.1007/s10461-025-04656-4
28. Ekwunife OI, Ejie IL, Okelu V, Mita C, Durosinmi-Eti O, Powell A, et al. Interventions to increase the uptake and continuation of pre-exposure prophylaxis (PrEP) by adolescent girls and young women at high risk of HIV in low-income and middle-income countries: a scoping review. BMJ Glob Health. (2022) 7(12):e009474. doi: 10.1136/bmjgh-2022-009474
29. Terefe B, Jembere MM, Asgedom DK, Lakew AM. Knowledge and attitude to HIV pre exposure prophylaxis among women in five sub-Saharan African countries: a multilevel model analysis of population-based survey 2021–2022. BMC Public Health. (2024) 24(1):1–14. doi: 10.1186/s12889-024-18717-1
30. Jackson-Gibson M, Ezema AU, Orero W, Were I, Ohiomoba RO, Mbullo PO, et al. Facilitators and barriers to HIV pre-exposure prophylaxis (PrEP) uptake through a community-based intervention strategy among adolescent girls and young women in seme sub-county, Kisumu, Kenya. BMC Public Health. (2021) 21(1):1–13. doi: 10.1186/s12889-021-11335-1
31. Skovdal M, Magoge-Mandizvidza P, Dzamatira F, Maswera R, Nyamukapa C, Thomas R, et al. Improving access to pre-exposure prophylaxis for adolescent girls and young women: recommendations from healthcare providers in eastern Zimbabwe. BMC Infect Dis. (2022) 22(1):1–10. doi: 10.1186/s12879-022-07376-5
32. Kufa-Chakezha T, Shangase N, Singh B, Cutler E, Aitken S, Cheyip M, et al. The 2022 antenatal HIV sentinel survey—Key findings. Public Health Bulletin South Africa. Available online at: https://www.phbsa.ac.za/wp-content/uploads/2024/01/PHBSA-HIV-Antenatal-Survey-Report.pdf (Accessed March 21, 2025).
33. Dunkley Y, Langwenya N, Malunga S, Kelly J, Toska E. A rapid review of research methodologies for remote research among young people in sub-Saharan Africa. Cape Town. (2021). (CSSR). Report No.: 463. Available online at: https://www.researchgate.net/publication/351824816_A_rapid_review_of_research_methodologies_for_remote_research_among_young_people_in_sub-Saharan_Africa?channel=doi&linkId=60ac15c545851522bc151d20&showFulltext=true (Accessed September 17, 2024).
34. Schaefer R, Gregson S, Fearon E, Hensen B, Hallett TB, Hargreaves JR. HIV Prevention cascades: a unifying framework to replicate the successes of treatment cascades. Lancet HIV. (2019) 6(1):e60–6. doi: 10.1016/S2352-3018(18)30327-8
35. Statistics South Africa. Demographic Profile of Adolescents in South Africa. Pretoria. (2018). Report No.: 03-00–10. Available online at: https://www.statssa.gov.za/publications/Report%2003-00-10/Report%2003-00-102016.pdf (Accessed May 25, 2025).
36. Hosmer DW, Lemeshow S. Applied Logistic Regression. 3rd ed. Hoboken, NJ: Wiley (2000). Available online at: https://onlinelibrary.wiley.com/doi/book/10.1002/0471722146
37. StataCorp. Stata Statistical Software: Release 17. College Station, TX, United States: StataCorp LLC (2022).
38. AVAC. Getting PrEP Rollout Right This Time: Lessons from the Field. (2025). Available online at: https://www.prepwatch.org/wp-content/uploads/2025/06/GettingRolloutRightThisTime_June2025.pdf (Accessed September 15, 2025).
39. O’Malley G, Beima-Sofie KM, Roche SD, Rousseau E, Travill D, Omollo V, et al. Health care providers as agents of change: integrating PrEP with other sexual and reproductive health services for adolescent girls and young women. Front Reprod Health. (2021) 3:668672. doi: 10.3389/frph.2021.668672
40. Chimbindi N, Mthiyane N, Zuma T, Baisley K, Pillay D, McGrath N, et al. Antiretroviral therapy based HIV prevention targeting young women who sell sex: a mixed method approach to understand the implementation of PrEP in a rural area of KwaZulu-Natal, South Africa. AIDS Care. (2022) 34(2):232–40. doi: 10.1080/09540121.2021.1902933
41. World Health Organization. Consolidated guidelines on differentiated HIV testing services: web annex C: GRADE table and systematic review: should HIV self-testing be used to support PrEP delivery. (2024). Available online at: https://iris.who.int/handle/10665/377893 (Accessed November 15, 2024).
42. Vanhamel J, Rotsaert A, Reyniers T, Nöstlinger C, Laga M, Van Landeghem E, et al. The current landscape of pre-exposure prophylaxis service delivery models for HIV prevention: a scoping review. BMC Health Serv Res. (2020) 20(1):1–18. doi: 10.1186/s12913-020-05568-w
43. Bekker LG, Das M, Abdool Karim Q, Ahmed K, Batting J, Brumskine W, et al. Twice-yearly lenacapavir or daily F/TAF for HIV prevention in cisgender women. New Engl J Med. (2024) 391(13):1179–92. doi: 10.1056/NEJMoa2407001
44. Fonner VA, Ridgeway K, Van Der Straten A, Lorenzetti L, Dinh N, Rodolph M, et al. Safety and efficacy of long-acting injectable cabotegravir as preexposure prophylaxis to prevent HIV acquisition. AIDS. (2023) 37(6):957–66. doi: 10.1097/QAD.0000000000003494
45. World Health Organization. WHO recommends the dapivirine vaginal ring as a new choice for HIV prevention for women at substantial risk of HIV infection. (2021). Available online at: https://www.who.int/news/item/26-01-2021-who-recommends-the-dapivirine-vaginal-ring-as-a-new-choice-for-hiv-prevention-for-women-at-substantial-risk-of-hiv-infection (Accessed March 28, 2021).
46. Naidoo NP, Mthimkulu N, Jama N, Chidumwa G, Chabalala B, Mhakakora T, et al. Community PrEP delivery for adolescent girls and young women: insights from the DREAMS PrEP choice study in Johannesburg, South Africa. Front Reprod Health. (2025) 7:1474067. doi: 10.3389/frph.2025.1474067
47. Jochim J, Meinck F, Toska E, Roberts K, Wittesaele C, Langwenya N, et al. Who goes back to school after birth? Factors associated with postpartum school return among adolescent mothers in the Eastern Cape, South Africa. Glob Public Health. (2023) 18(1):2049846. doi: 10.1080/17441692.2022.2049846
48. Luthuli S, Haskins L, Mapumulo S, Rollins N, Horwood C. I decided to go back to work so I can afford to buy her formula”: a longitudinal mixed-methods study to explore how women in informal work balance the competing demands of infant feeding and working to provide for their family. BMC Public Health. (2020) 20(1):1847. doi: 10.1186/s12889-020-09917-6
Keywords: pre-exposure prophylaxis, PrEP cascade, adolescent girls and young women, pregnant women, parenting women, HIV prevention, sub-Saharan Africa
Citation: Chen-Charles J, Bekker L-G, Jochim J, Wittesaele C, Cluver L and Toska E (2025) Missed HIV prevention opportunities: the PrEP cascade among pregnant or parenting adolescent girls and young women in South Africa. Front. Reprod. Health 7:1648786. doi: 10.3389/frph.2025.1648786
Received: 17 June 2025; Accepted: 26 September 2025;
Published: 17 October 2025.
Edited by:
Edith Nakku-Joloba, Makerere University, UgandaReviewed by:
Wei Li Adeline Koay, Medical University of South Carolina, United StatesEnos Moyo, University of KwaZulu-Natal, South Africa
Karla Reyna Navarro Fuentes, Instituto Mexicano del Seguro Social, Delegación Chiapas, Mexico
Copyright: © 2025 Chen-Charles, Bekker, Jochim, Wittesaele, Cluver and Toska. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jenny Chen-Charles, amVubnkuY2hlbjFAYWx1bW5pLmxzaHRtLmFjLnVr
 Jenny Chen-Charles
Jenny Chen-Charles Linda-Gail Bekker2
Linda-Gail Bekker2 Elona Toska
Elona Toska