- 1School of Nursing, Faculty of Community and Health Sciences, University of the Western Cape, Cape Town, South Africa
- 2Postdoctoral research Fellow at Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
- 3Department of Obstetrics and Gynecology, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
Background: Post-abortion family planning (PAFP), ideally initiated within 48 h, is crucial for preventing unplanned pregnancies. Repeat-induced abortion remains a significant challenge to the sexual and reproductive health of women. Despite numerous systematic reviews and meta-analyses, inconsistent findings still hinder effective policy formulation and clinical decision-making. In Africa, high rates of unsafe abortion and unintended pregnancy persist, exacerbated by socioeconomic and health system barriers. This umbrella review consolidates global evidence on the prevalence, determinants, and use of PAFP to inform health policy, strengthen service delivery, and promote reproductive health equity, especially in regions with limited access to safe abortion services and contraception.
Methods: An umbrella review of systematic reviews and meta-analyses based on observational studies was conducted. The methodological quality of the included studies was assessed using the Assessment of Multiple Systematic Reviews tool. Heterogeneity was assessed using Cochran's Q and I2 statistics, while publication bias was evaluated using Egger's test and funnel plots. A random-effects meta-analysis was used to estimate the pooled effect size, with analyses performed using Stata version 19. Subgroup analyses were performed by country and continent. Pooled results were synthesized using random-effects meta-analysis models. The review protocol was registered with PROSPERO (CRD420251089314).
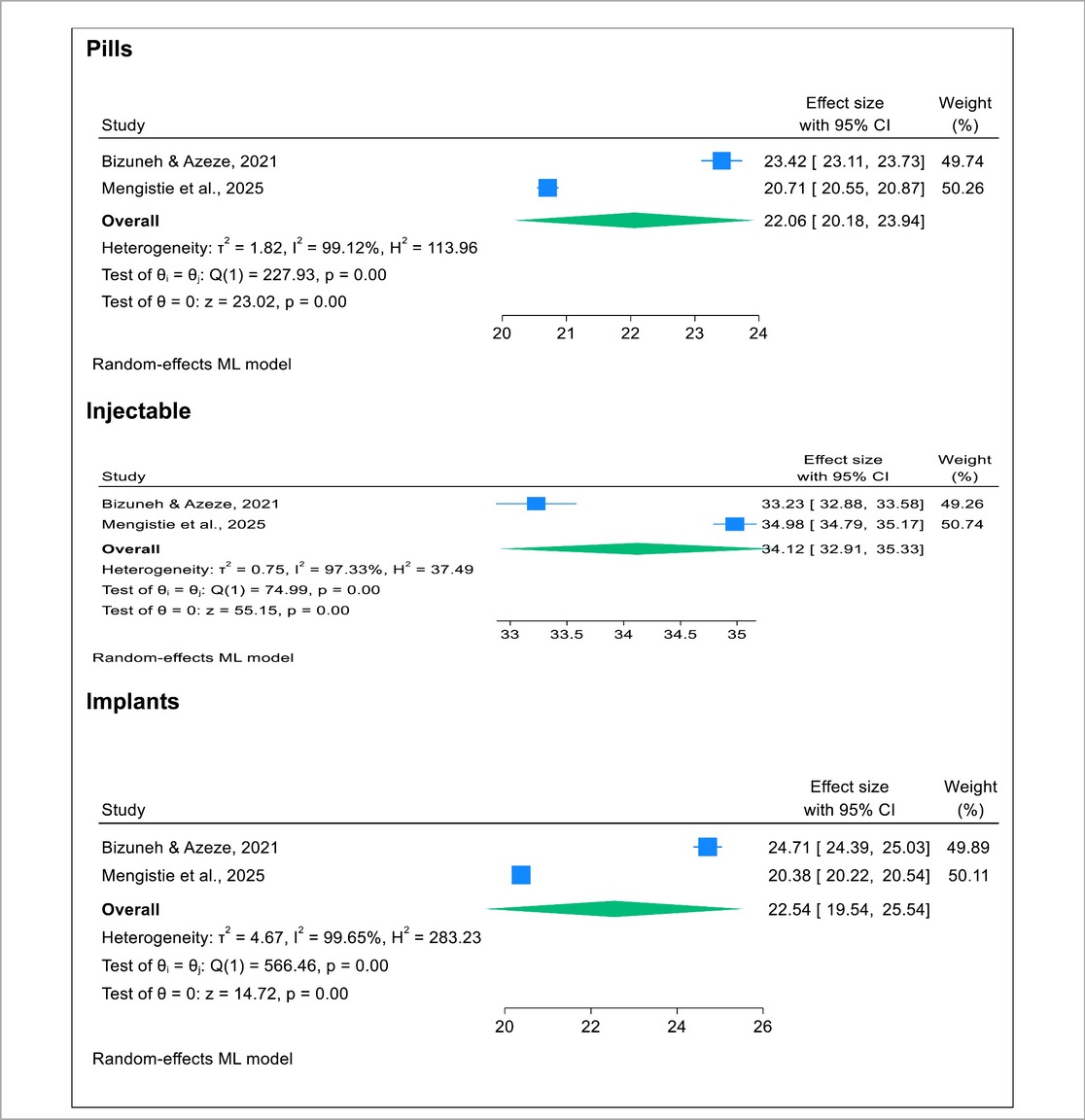
Result: This umbrella review included six systematic reviews and meta-analyses, comprising 198 primary studies conducted across 44 African countries, with a combined sample size of 420,832 women of reproductive age assessing post-abortion family planning utilization. This umbrella review found that the pooled prevalence of post-abortion family planning utilization among women of reproductive age in Africa was 62.82% (95% CI: 59.24%–66.40%), indicating substantial uptake but with high heterogeneity across studies (I2 = 98.81%). A subgroup umbrella meta-analysis revealed that the pooled prevalence of post-abortion family planning utilization was 69.31% (95% CI: 64.27%–74.35%) in Ethiopia, compared to 60.29% (95% CI: 57.11%–63.47%) in other African countries. This study determined that injectables were the most commonly utilized post-abortion family planning method (34.12%), followed by pills and implants, each with a nearly equal share of 22%. This umbrella review identified key pooled determinants of post-abortion family planning utilization among women of reproductive age in Africa, including marital status (being married), younger maternal age (15–24 years), educational attainment, receipt of post-abortion family planning counseling, prior use of family planning, history of abortion, unintended pregnancy, and contraceptive knowledge.
Conclusion and recommendation: The high prevalence of PAFP utilization in Africa (62.82%), and particularly in Ethiopia (69.31%), reflects encouraging progress. However, the fact that 37.18% of post-abortion women in Africa and 30.69% in Ethiopia still do not use PAFP underscores a critical gap that demands targeted policy action. The predominance of injectable contraceptives highlights the need to expand access to a broader range of methods, including long-acting reversible contraceptives, to support informed and voluntary choice. Policymakers and health planners in Africa should urgently strengthen reproductive health policies by implementing a comprehensive, multipronged strategy to ensure universal access to post-abortion care.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD420251089314, PROSPERO CRD420251089314.
Introduction
According to a 2023 report by the World Health Organization (WHO), over 700 women died daily that year from preventable pregnancy and childbirth complications. Approximately 75% of maternal deaths were due to severe bleeding, infections, high blood pressure, delivery complications, and unsafe abortions, most of which are treatable (1, 2). The WHO defines abortion as the termination of a pregnancy before 20 weeks of gestation or when the fetus weighs less than 500 g. Abortion may occur spontaneously (miscarriage) or be induced. Safe abortions are those that follow WHO-recommended methods appropriate for the duration of pregnancy and are performed by trained providers using either medication or simple outpatient procedures (3, 4). Abortion is a complex issue influenced by religious, moral, cultural, and political factors and remains a significant public health concern. Over a quarter of the global population lives under restrictive abortion laws. Despite legal status, abortions continue to occur and nearly half are unsafe, performed by unskilled providers or in unhygienic conditions (5).
A study by Bell et al. on the global epidemiology of induced abortion found that over 73 million abortions occur annually worldwide. While abortion rates are declining in high-resource settings, they remain stable in low- and middle-resource countries, where unsafe abortions persist as a major cause of maternal mortality (6).
According to the 2023 Comprehensive Abortion Care (CAC) report by the WHO, maternal mortality in Southeast Asia decreased by 57.3% between 2007 and 2017; however, unsafe abortion remains a significant concern. CAC, which includes post-abortion family planning, plays a crucial role in improving maternal health. Limited data collection continues to hinder accurate assessment of service accessibility and quality (7).
The 2022 WHO Abortion Care Guideline emphasizes the importance of safe, accessible services, including self-managed medical abortion and expanded provider roles. These updated guidelines strengthen post-abortion family planning by promoting autonomy, community-based care, and improved access to abortion pills; these measures are key to reducing repeat unintended pregnancies and enhancing reproductive health through evidence-based, rights-centered service delivery across diverse legal and clinical settings (8).
According to Kim et al., CAC provides safe, accessible, and woman-centered services encompassing pre-abortion, abortion, and post-abortion care. CAC helps reduce maternal mortality and can be delivered by various healthcare providers. However, barriers such as restrictive laws and provider beliefs persist. A holistic, rights-based approach is essential to improving health outcomes and promoting gender equality, especially in humanitarian settings (9). The 2022 WHO Abortion Care Guideline frames access to safe abortion, including post-abortion family planning, as a health and human rights priority. It promotes immediate initiation of contraception after abortion and expands provider roles to include community health workers and pharmacists (9, 10).
Regarding post-abortion care, a previous scoping review by Macleod et al. reported that non-barrier contraceptive use ranged from 15% to 76%, unintended pregnancy from 24% to 91%, and abortion from 11% to 48% (11). A systematic review of randomized controlled trials identified that the key contributing factors included alcohol use, violence, health system failures, socioeconomic challenges, and pregnancy desire linked to non-paying partners (12). Kim et al., along with the World Health Organization, emphasized that comprehensive abortion care is essential for safeguarding sexual and reproductive health (SRH), saving lives, and preserving dignity. The WHO guideline promotes accessible, evidence-based care to ensure safe, effective, and equitable services (9, 10).
Sub-Saharan Africa accounts for 29% of global unsafe abortions and 62% of abortion-related deaths, largely due to restrictive laws, poor post-abortion care, and limited access to contraception (13). Another study by Woldemichael et al. underscored the critical role of post-abortion family planning (PAFP) in reducing unintended pregnancies and unsafe abortions in Eastern Africa. Utilization rates of PAFP range from 53.7% to 67.86% and are influenced by factors such as education, counseling, and marital status. Injectables and implants were identified as the most preferred methods (14, 15). Despite its benefits, nearly half of women in some areas still do not utilize PAFP, highlighting the need for improved counseling and awareness.
Previous systematic reviews and meta-analyses have reported inconsistent prevalence rates of post-abortion family planning (PAFP) utilization in Eastern Africa and Ethiopia, ranging from 67.86% to 74.56%. Factors influencing uptake include counseling, prior contraceptive use, marital status, and education, with injectables, implants, and pills identified as the most preferred methods (15–18). Although PAFP utilization remains below WHO targets, it shows promise in reducing unintended pregnancies and repeat abortions (9, 10).
However, existing reviews differ in scope, methodology, and regional focus, resulting in fragmented and contradictory findings that hinder effective policy formulation and clinical decision-making. Many prior reviews lack a comprehensive synthesis and overlook contextual factors affecting PAFP uptake. This umbrella review aims to consolidate evidence from published systematic reviews and meta-analyses to provide a clearer understanding of the prevalence and determinants of PAFP among women of reproductive age in Africa. The findings will inform health policy, improve service delivery, and promote reproductive health equity in low-resource settings.
Review objectives
1. To synthesize evidence from systematic reviews and meta-analyses on the prevalence of post-abortion family planning utilization among women in Africa;
2. To identify pooled predictors of post-abortion family planning utilization among women in Africa; and
3. To evaluate the effectiveness of post-abortion care interventions among women of reproductive age in Africa.
Methods
This umbrella review was conducted following established methodologies for synthesizing multiple systematic reviews (19). The procedure adheres to the umbrella review methodology developed by the Joanna Briggs Institute (20). It involved a systematic synthesis of eligible systematic reviews and meta-analyses (SRMs) summarizing the global prevalence, determinants, and post-abortion care interventions related to pregnancy termination.
This umbrella review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines and was registered in PROSPERO under reference number CRD420251089314.
Operational definitions
Umbrella Review: An umbrella review is a systematic synthesis of multiple systematic reviews and meta-analyses on a specific topic. It provides a high-level overview of existing evidence; identifies patterns, gaps, and inconsistencies; and offers comprehensive insights to inform policy and practice (19).
Post-Abortion Family Planning (PAFP): PAFP refers to the provision and uptake of contraceptive services immediately following an abortion. It aims to prevent unintended pregnancies and repeat abortions by offering timely, informed, and voluntary access to family planning methods (9, 10).
Determinants: In the context of this review, determinants are factors that influence the utilization of post-abortion family planning services. These may include sociodemographic characteristics (e.g., age, marital status, and education), prior contraceptive use, receiving counseling, and access to healthcare services (15–18).
Search strategy
Six major international online databases—PubMed, Scopus, Science Direct, Web of Science, and databases specific to systematic reviews and meta-analyses such as the Cochrane Database of Systematic Reviews and the Database of Abstracts of Reviews of Effects—were searched for systematic reviews and meta-analyses (SRMs) examining the prevalence, determinants, and utilization of post-abortion family planning among women of reproductive age globally. A comprehensive search strategy was employed using adapted PICO questions, developed from relevant keywords and Medical Subject Headings (MeSH) terms. These search terms were combined using Boolean operators “OR” and “AND” to ensure a thorough and inclusive search.
(a) Population: females (adolescents, youths, and women of reproductive age) who have undergone an abortion.
(b) Intervention: utilization of any post-abortion family planning service or method (counseling, method availability, etc.).
(c) Comparison: women of reproductive age post-abortion who were not offered post-abortion family planning services.
(d) Outcome: prevalence, determinants, and uptake of post-abortion family planning.
(e) Study design: systematic reviews and meta-analyses of observational studies.
(f) Setting (context): Africa.
Both published and unpublished studies were included in this umbrella review.
A comprehensive literature search was conducted between 12 June and 1 July 2025, without restrictions on publication date, and included all relevant studies published up to 1 July 2025. Two independent researchers conducted the search, and any discrepancies were resolved through discussion and consensus with the remaining authors.
A sample search strategy for PubMed was developed using a combination of Medical Subject Headings (MeSH) terms and free-text keywords. The PubMed search string included terms such as ((((((Abortion OR “Abortion, Induced”/trends[Mesh] OR Prevalence OR Epidemiology OR Magnitude) AND (determinants OR associated factors OR predictors) AND post-abortion contraceptive uptake OR (“Contraceptive Agents”, OR (family planning use OR family planning utilization OR family planning uptake OR family planning services OR contraceptive use OR contraceptive utilization OR contraceptive uptake OR birth control OR fertility control OR population control) AND (systematic review and meta-analysis)). The complete search strategy details are provided in Supplementary File 1: Search strategy.docx.
Inclusion criteria
This umbrella review included all available systematic reviews and meta-analyses (SRMs) that met predefined eligibility criteria: a clearly defined literature search strategy, quality appraisal of included studies using appropriate tools, and a standardized approach to pooling data and summarizing estimates among women of reproductive age. Both published and unpublished studies were considered, with inclusion limited to those written in English. A comprehensive literature search was conducted between 12 June and 1 July 2025, covering studies published from 1 January 2000 to 1 July 2025. This broad inclusion period aimed to capture diverse evidence across time and regions, ensuring a robust synthesis of findings related to post-abortion family planning (PAFP) utilization in Africa.
Exclusion criteria
Studies were excluded if they did not report on the prevalence or determinants of post-abortion family planning (PAFP) utilization among women of reproductive age. Qualitative reviews, narrative reviews, editorials, correspondence, abstracts, and methodological papers were also excluded. Additionally, literature reviews lacking a clearly defined research question, search strategy, or article selection process were not considered. This rigorous screening process ensured the inclusion of high-quality and relevant evidence to support a comprehensive synthesis of PAFP utilization in Africa.
Data extraction
Data from the included SRM studies were extracted using a standardized Excel form. The extracted information included study identification; review objectives; prevalence and risk factors of induced, repeat, and unsafe abortions; associated outcomes; and post-abortion care. Additional data covered effect sizes (OR/RR with 95% CI), the number and design of primary studies, sample sizes, methods and scores used for publication bias and quality assessment, data synthesis models, and key conclusions. Full details of the extraction process are provided in Supplementary Files 3–3.2.
Risk of bias assessment
All included studies were critically appraised to assess the validity and scoring of their findings. This umbrella review used the Assessment of Multiple Systematic Reviews (AMSTAR-2) tool to ensure the methodological and evidence quality of the included SRM studies (19, 21) (details are provided in Supplementary File 2: AMSTAR-2 .xlsx).
Data synthesis
Both narrative (qualitative) and quantitative approaches were used to summarize the findings of the included SRM studies. When multiple estimates were reported for the magnitude, associated factors, or adverse outcomes of pregnancy termination (including induced, repeat, and unsafe abortions among reproductive-age women), the range of estimates was presented, and a pooled summary estimate was calculated. The choice of meta-analysis model was guided by the level of heterogeneity, assessed using Higgins' I2 statistic (22). Due to the anticipated high between-study heterogeneity, the DerSimonian–Laird random-effects model was employed (22).
Publication bias was assessed if at least 10 studies were included, as this is the minimum typically required for such evaluation (19, 23). The meta-analysis involved calculating pooled estimates of sensitivity, specificity, positive predictive value, and true positives, either directly reported or derived from the included studies. Heterogeneity was evaluated using both Cochran's Q test and the I2 statistic (24). An I2 value greater than 50% and a Cochran's Q test p-value <0.05 were considered indicative of significant heterogeneity, warranting the use of a random-effects model (24).
Pooled estimates were calculated using STATA version 17, employing the “metaprop” command with sample size as the weighting variable and 95% confidence intervals. Quantitative analyses were conducted using STATA version 17.0. A summary of predictors of pregnancy termination and post-abortion care utilization, along with their respective odds ratios, was computed.
Ethical consideration
This study did not require ethical approval or informed consent from participants, as it utilized data solely extracted from previously published SRM studies.
Results
Study screening and selection
Two reviewers independently screened the titles and abstracts of 89 systematic reviews and meta-analyses (Supplementary File 1: Search strategy). From this initial screening, 27 articles were selected for full-text review. An additional six articles were identified through reference lists and other databases, resulting in a total of 33 articles undergoing full-text assessment. Of these, 16 met the inclusion criteria for this umbrella review of systematic reviews and meta-analyses (12, 15, 16, 18, 25–36). The number of studies identified, included, and excluded at each stage of the selection process is illustrated in the PRISMA flowchart (Figure 1). The primary reasons for exclusion at the full-text review stage, as indicated in the PRISMA diagram, were ineligible outcomes and study protocols.
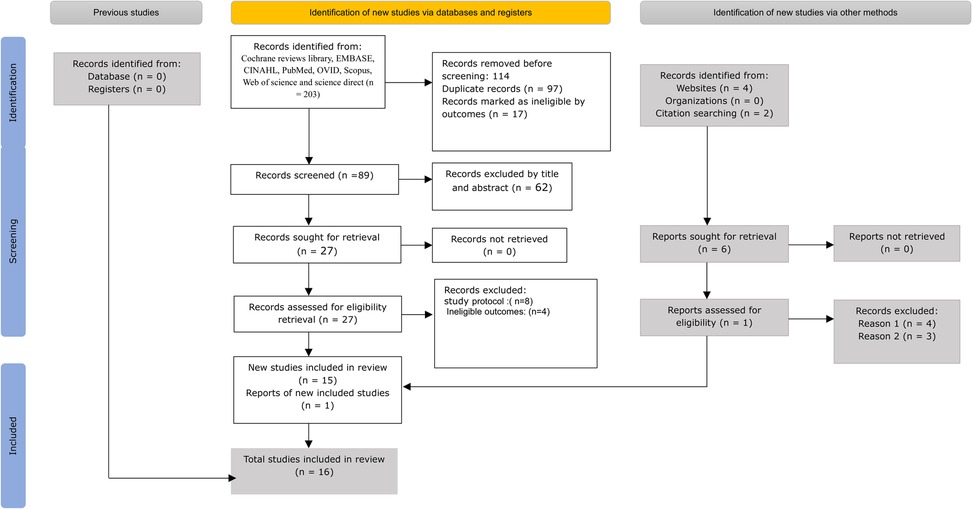
Figure 1. PRISMA 2020 flow diagram for new systematic reviews, which include searches of databases, registers, and other sources (37) from 2000 to 2025.
Highlights of conclusions by authors across systematic reviews and meta-analyses of post-abortion family planning utilization
This umbrella review synthesizes findings from multiple systematic reviews and meta-analyses focused on post-abortion family planning utilization in Africa. Bizuneh and Azeze identified key determinants of PAFP uptake in Eastern Africa, including marital status, multiparty, and history of abortion, receipt of counseling, and prior contraceptive use (15). Dagnew and Asresie reported that post-abortion care uptake across Africa stands at 58.78%, falling short of WHO recommendations. A notable decline in uptake was observed between 2020 and 2023, with injectable contraceptives being the most commonly used method. The authors emphasized the need for improved education, awareness, and client-centered counseling (18). Mengistie et al. found that post-abortion contraceptive use in sub-Saharan Africa remains low. They advocated for scaling up utilization through enhanced educational attainment, stronger advocacy for contraceptive options, and comprehensive post-abortion counseling services (26).
This umbrella review synthesizes findings from multiple systematic reviews and meta-analyses focused on post-abortion family planning utilization in Africa. Beyene et al. reported that PAFP utilization remains suboptimal, with key influencing factors including marital status, educational level, receipt of counseling, prior contraceptive use, and age. These insights are critical for informing reproductive health policy and service delivery (16). Similarly, Wake et al. found that the pooled prevalence of post-abortion contraceptive use in Ethiopia was low, with significant associations observed for counseling and prior use of modern contraceptives (27). Cherie et al. also concluded that family planning utilization among women receiving abortion services in Ethiopia falls below both WHO and national standards (25). Receipt of counseling and a history of contraceptive use were identified as strong predictors of uptake. Collectively, these findings highlight the need for strengthened counseling services and targeted interventions to improve post-abortion contraceptive use in Ethiopia (16, 25, 27). Table 1 summarizes the total number of included studies, study settings, number of countries represented, overall sample sizes, and key conclusions reported by the authors.
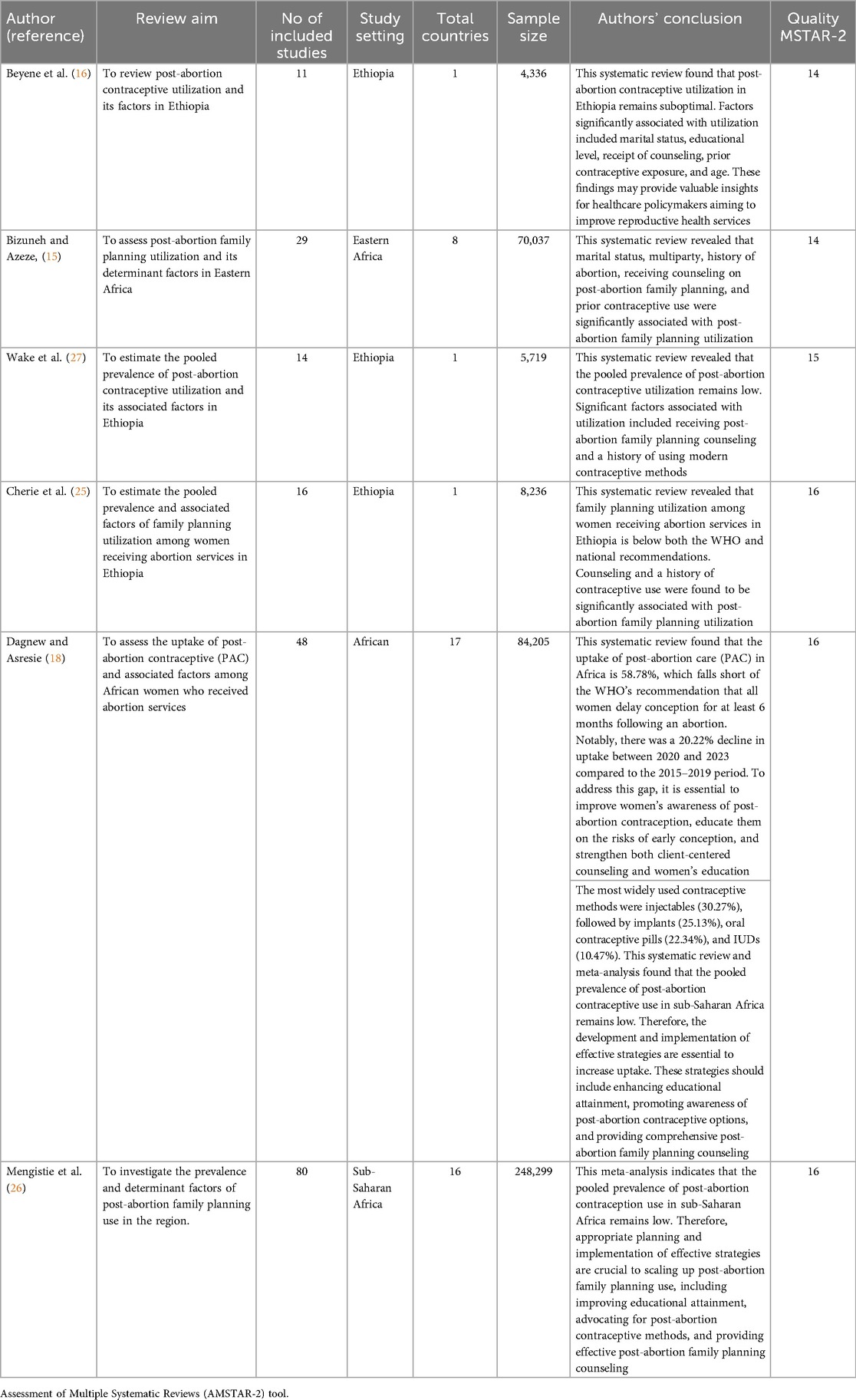
Table 1. Summary of the total number of included studies, study settings, number of countries represented, overall sample size, and key conclusions reported by the authors, 2013–2025.
Post-abortion family planning utilization-related characteristics
This umbrella review synthesizes findings from multiple systematic reviews and meta-analyses focused on post-abortion family planning utilization across various African regions. The studies included in the review, published between 2021 and 2025, collectively provide insights into the prevalence, determinants, and regional disparities in post-abortion family planning (PAFP) uptake. Post-abortion family planning reviews mainly focus on Ethiopia and broader African regions, including Eastern, Western, Northern, Central, Southern, and sub-Saharan Africa (15, 16, 18, 25–27). The number of studies included per review ranged from 2 to 80, with sample sizes between 274 (18) and 248,299 (26). Utilization rates varied across regions, with Ethiopia recording the highest at 74.56% (16) and Western Africa recording the lowest at 51.48%. Moderate uptake was observed in Southern (62.23%), Central (60.96%), and Northern Africa (58.78%) (18). All studies underwent clear quality assessments, with consistent AMSTAR-2 ratings between 14 and 16, ensuring methodological rigor and reliability across findings. Detailed results are presented in Table 2.
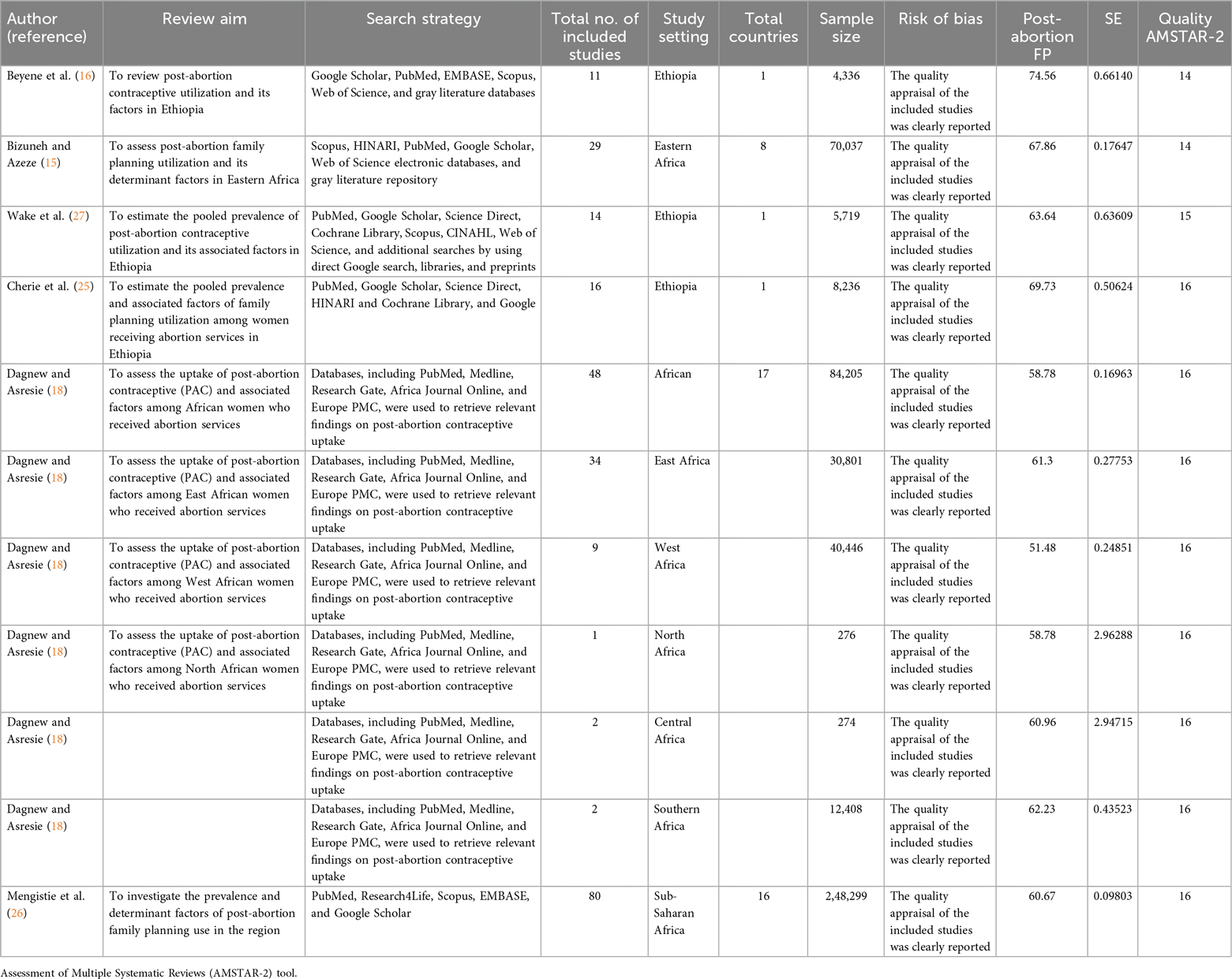
Table 2. Characteristics of included systematic reviews and meta-analyses on post-abortion family planning utilization, 2021–2025.
Pooled prevalence of post-abortion family planning utilization in Africa
This umbrella review included six systematic reviews and meta-analyses comprising 198 primary studies conducted across 44 African countries, with a combined sample size of 420,832 women of reproductive age assessing post-abortion family planning utilization (15, 16, 18, 25–27). Further details on PAFP utilization are provided in Supplementary File 3.
This umbrella review of systematic reviews and meta-analyses found that the pooled prevalence of post-abortion family planning utilization among women of reproductive age in Africa was 62.82% (95% CI: 59.24%–66.40%), indicating substantial uptake but with high heterogeneity across studies (I2 = 98.81%). Detailed results are provided in Figure 2.
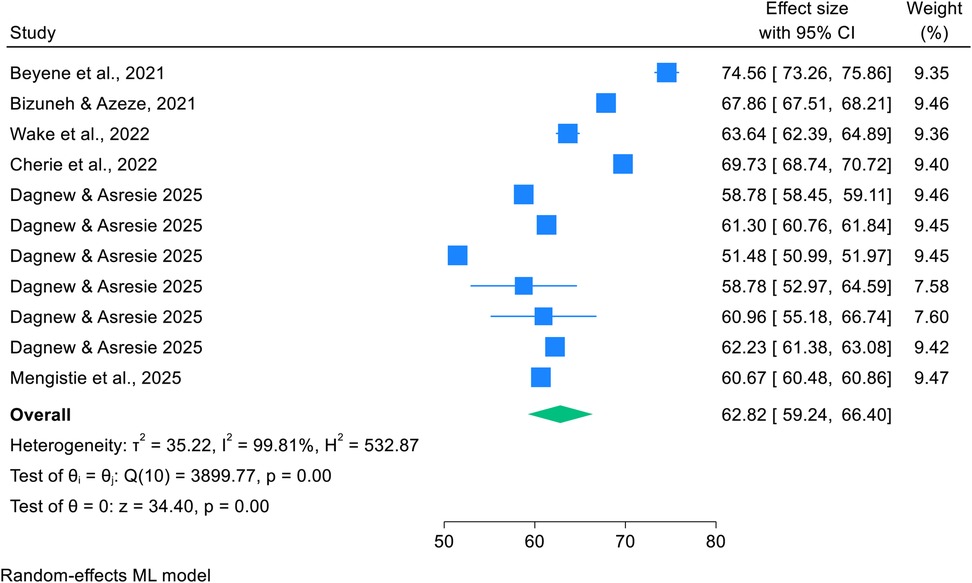
Figure 2. Forest plot showing pooled prevalence of post-abortion family planning utilization among women of reproductive age in Africa in 2025.
Subgroup analysis by country
A subgroup umbrella meta-analysis revealed that the pooled prevalence of post-abortion family planning utilization was 69.31% (95% CI: 64.27%–74.35%) in Ethiopia (16, 25, 27), compared to 60.29% (95% CI: 57.11%–63.47%) in other African countries (15, 18, 26), indicating substantial heterogeneity (I2 = 98.20%). Detailed results are provided in Figure 3.
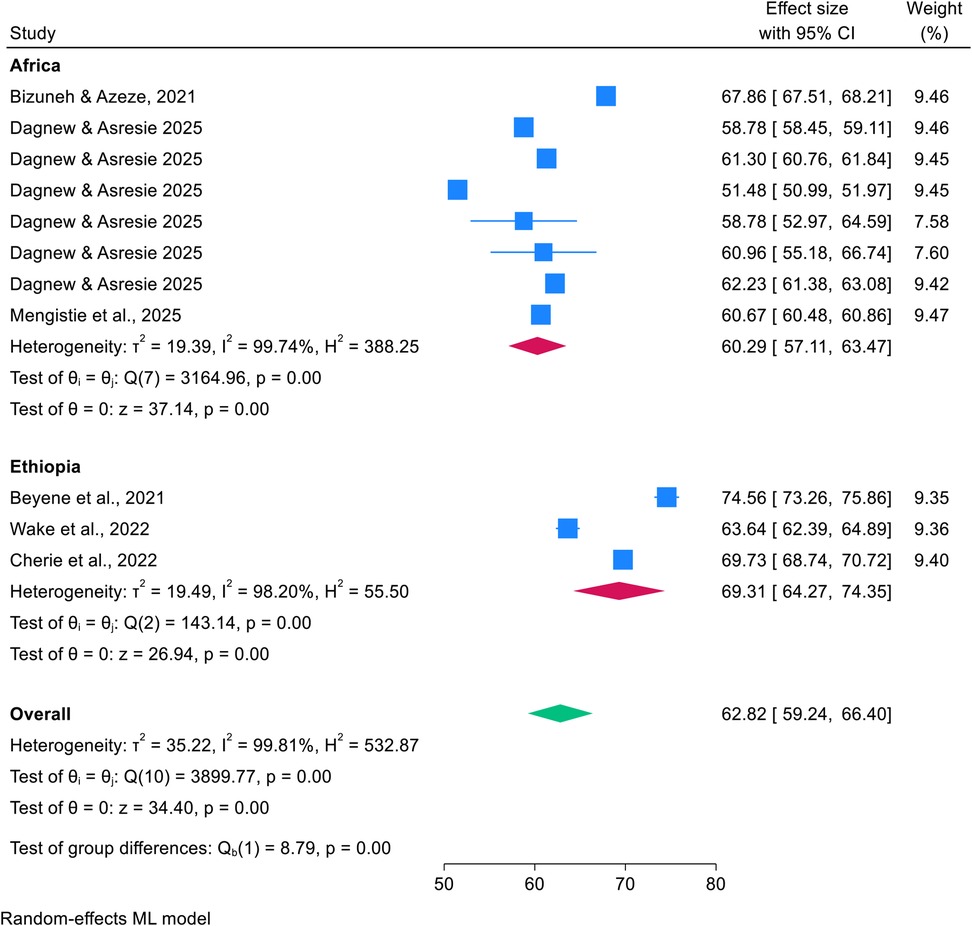
Figure 3. Forest plot showing the subgroup analysis by country for pooled prevalence of post-abortion family planning utilization among women of reproductive age in Africa in 2025.
The Galbraith plot showed high heterogeneity, with no studies falling outside the 95% confidence band. The symmetry around the red regression line suggests low publication bias. However, the extensive spread of points confirms substantial variability, supporting the observed I2 = 99.81% heterogeneity. Further details are shown in Figure 4.
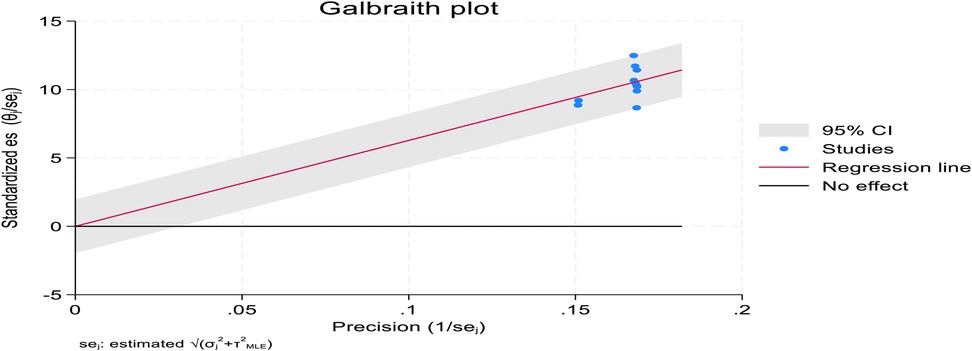
Figure 4. Galbraith plot showing high heterogeneity among included studies on post-abortion family planning utilization among women of reproductive age in Africa in 2025.
Publication bias assessment
Publication bias was assessed using a funnel plot, which appeared asymmetric and skewed to the right. However, Egger's regression test (PV = 0.7517) confirmed the absence of significant publication bias (Figure 5).
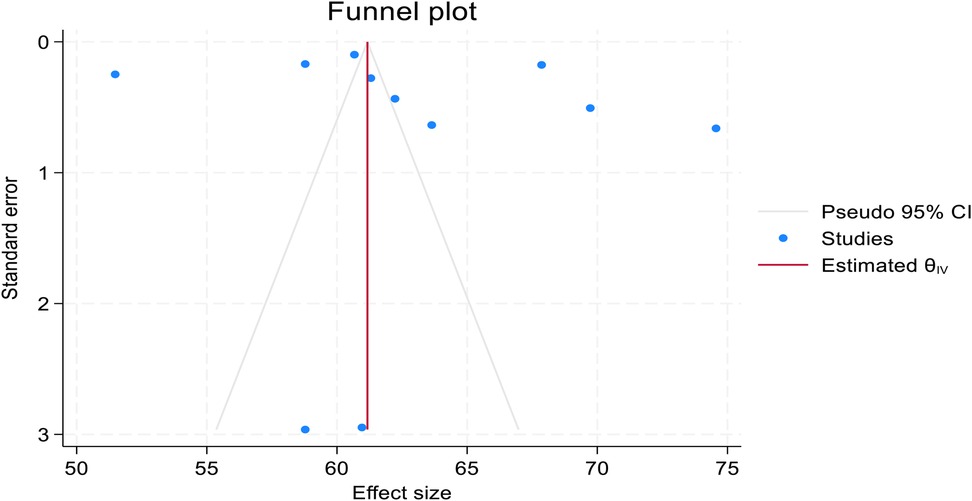
Figure 5. Funnel plot showing asymmetric distribution of included studies in pooled prevalence of post-abortion family planning utilization among women of reproductive age in Africa in 2025.
Based on the trim-and-fill analysis, the linear estimator imputed three studies on the right (11 + 2 imputed = 13 studies). The pooled African prevalence of post-abortion family planning utilization among women of reproductive age increased from 62.810% (59.062%–66.558%) to 64.589% (60.591%–68.587%) after the trim-and-fill analysis. Both have narrow confidence intervals, suggesting high precision. This implies that the true effect size might be underestimated when considering only the observed studies. As shown in Figure 5, the funnel plots appeared symmetric after the trim-and-fill analysis, with the linear estimator imputing two studies on the right (Figure 6).
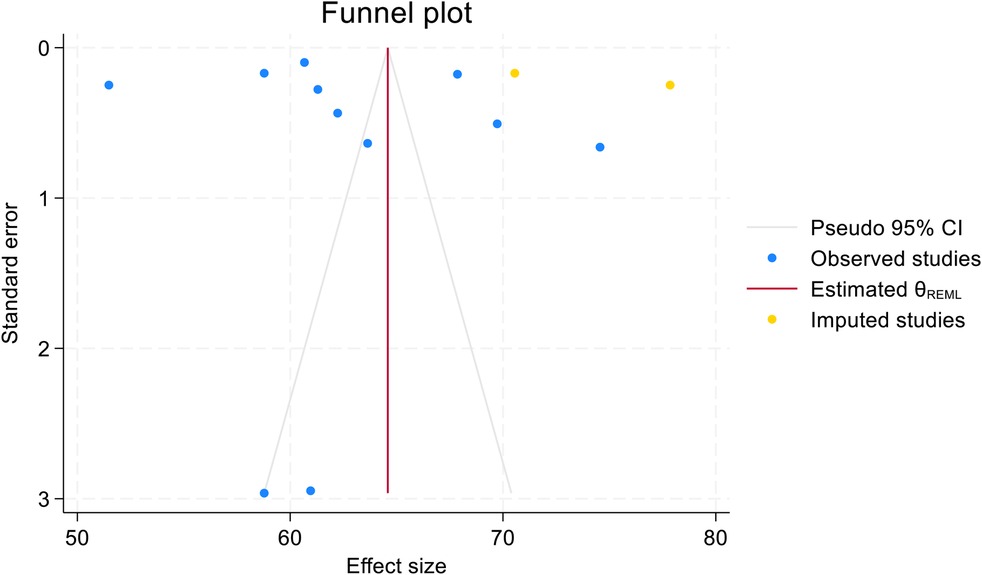
Figure 6. Funnel plot showing symmetric distribution of included studies in pooled prevalence of post-abortion family planning utilization among women of reproductive age in Africa in 2025.
Common types of post-abortion family planning utilization (PAFP)
This study determined that, among family planning methods used during post-abortion care in Africa, injectables were the most commonly utilized (34.12%), followed by pills and implants, each with a nearly equal share of 22% (15, 26). Further details on types of methods used are provided in Supplementary File 3.1 and Table 3.
Pooled key determinants of post-abortion family planning (FP) utilization
This umbrella review synthesized evidence to identify the key determinants of post-abortion family planning (FP) utilization among women of reproductive age in Africa. The analysis revealed that married women were significantly more likely to use FP services (AOR: 2.64; 95% CI: 2.09–3.19), as were younger women aged 15–24 years (AOR: 5.87; 95% CI: 2.44 –9.30). Educational attainment was positively associated with FP uptake (AOR: 2.22; 95% CI: 1.54–2.90), while receiving post-abortion FP counseling substantially increased utilization (AOR: 3.98; 95% CI: 3.31–4.65). Prior use of FP (AOR: 4.30; 95% CI: 2.91–5.70), history of abortion (AOR: 2.10; 95% CI: 1.79–2.42), unintended pregnancy (AOR: 4.06; 95% CI: 2.70–5.41), and contraceptive knowledge (AOR: 2.58; 95% CI: 2.19–2.97) were also identified as significant predictors. Despite the high heterogeneity across studies (I2 > 99%), the findings consistently underscore the critical role of education, counseling, and reproductive history in shaping post-abortion FP utilization. Further details on the identified factors for FP utilization are provided in Supplementary File 3.2 and Table 4.
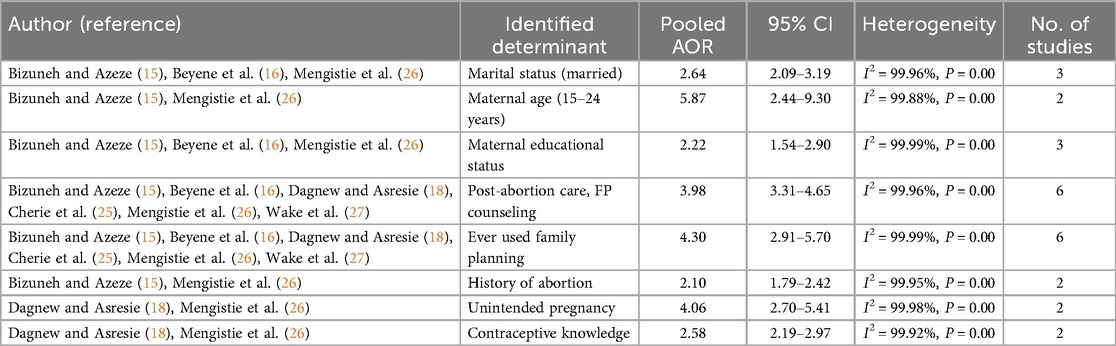
Table 4. Pooled key determinants of post-abortion family planning (FP) utilization among women of reproductive age in 2025.
Post-abortion family planning (FP) utilization interventions
Recent findings from previous meta-analyses of prospective or randomized controlled studies on post-abortion family planning (FP) interventions highlight several key insights. For instance, a study by Buckingham et al. found that immediate postpartum use of long-acting reversible contraceptives (LARCs) is generally acceptable among adolescents, particularly when side effects are minimal and decision-making autonomy is respected. However, evidence on post-abortion LARC use among adolescents remains limited (28). Similarly, Roe and Bartz concluded that most reversible contraceptive methods are safe following surgical abortion, although the optimal timing for initiation varies in cases of medical abortion. They emphasized that abortion care presents a critical opportunity to offer access to long-acting contraceptive methods (30).
Further, Schmidt-Hansen et al. reported that early administration of LARCs during medical abortion enhances user satisfaction and reduces the risk of unintended pregnancies. Early insertion of intrauterine devices (IUDs) was associated with increased uptake and continued use, supporting equitable, person-centered care (33).
Another study by Sedlecky and Stanković found that immediate post-abortion initiation of reliable contraception, combined with adolescent-centered counseling, effectively prevents repeat pregnancies. While LARC methods are safe, maintaining long-term adherence may be challenging (34). In China, Wang et al. observed that post-abortion care significantly improved reproductive outcomes, including increased contraceptive use and reduced repeat abortions, although they noted the need for high-quality research to optimize service delivery (36).
Rogers and Dantas highlighted that access to contraception and SRH information following abortion is often hindered by limited education and negative provider attitudes. They emphasized the importance of culturally safe counseling to improve contraceptive acceptance (31). Similarly, Rossier et al. found that abortion disclosure within social networks is influenced by stigma and the desire for anonymity. Informal medical abortion use did not significantly affect disclosure patterns, underscoring the need for stigma-sensitive interventions to enhance access to care (32). Table 5 summarizes the key findings on the impacts of post-abortion family planning (FP) interventions and the significant conclusions reported by the authors.
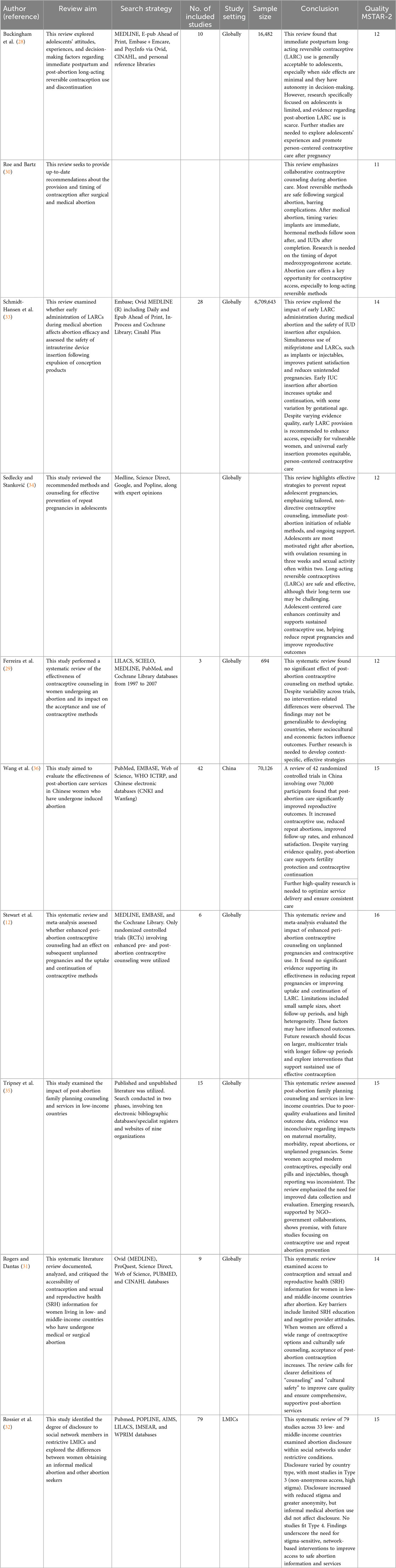
Table 5. Summary of key findings on intervention impacts of post-abortion family planning (FP) utilization, highlighting the conclusions reported by each author in 2025.
Discussion
This umbrella review of systematic reviews and meta-analyses found that the pooled prevalence of post-abortion family planning utilization among women of reproductive age in Africa was 62.82% (95% CI: 59.24%–66.40%), with Ethiopia showing a higher rate of 69.31% compared to 60.29% in other African countries. Injectables were the most commonly used method, followed by pills and implants.
This study identified key pooled determinants that influence post-abortion family planning use in Africa, including being married, younger age (15–24), higher educational attainment, prior contraceptive use, abortion history, unintended pregnancy, and receiving counseling. These determinants suggest that targeted education, counseling, and support for young, unmarried, and less-informed women could improve utilization rates. Furthermore, this umbrella review found that previous post-abortion family planning interventions improve reproductive outcomes by increasing contraceptive use and reducing repeat abortions. All included studies underwent thorough quality assessments, consistently receiving AMSTAR-2 ratings between 14 and 16, confirming strong methodological rigor and reliability across the findings.
This umbrella review of systematic reviews and meta-analyses found that the pooled prevalence of post-abortion family planning utilization among women of reproductive age in Africa was 62.82% (95% CI: 59.24%–66.40%) (15, 16, 18, 25–27) with Ethiopia showing a higher rate of 69.31% (16, 25, 27) compared to 60.29% in other African countries (15, 18, 26). This is further supported by another study, which emphasized the critical role of PAFP in reducing unintended pregnancies and unsafe abortions in Eastern Africa, reporting utilization rates between 53.7% and 67.86% (14, 15). Although these figures fall short of WHO targets, they reflect meaningful progress in preventing unintended pregnancies and repeat abortions. The higher PAFP uptake observed in Ethiopia may reflect better access to nationally integrated abortion and post-abortion family planning services, increased awareness, and more effective service delivery systems (38). However, the fact that nearly half of the women in some regions still do not use PAFP underscores the urgent need for improved counseling, education, and culturally tailored interventions to address regional disparities and enhance family planning services across the continent (9, 10).
This study identified several pooled key determinants influencing PAFP utilization in Africa, including marital status, younger age (15–24), higher education, prior contraceptive use, abortion history, unintended pregnancy, and receipt of counseling (15, 16, 18, 25–27). These findings align with previous reviews, which consistently highlight education, marital status, and counseling as major factors influencing PAFP uptake (15–18). These determinants suggest that targeted education, counseling, and support for young, unmarried, and less-informed women could improve utilization rates.
Furthermore, this umbrella review found that previous post-abortion family planning (PAFP) interventions significantly improved reproductive outcomes by increasing contraceptive use and reducing repeat abortions. For example, immediate initiation of contraception and adolescent-focused counseling have proven effective, although maintaining long-term adherence to long-acting reversible contraceptives (LARCs) remains challenging. Persistent barriers such as limited education, provider bias, and stigma continue to restrict access to care and discourage open disclosure. Addressing these issues requires culturally sensitive, stigma-aware counseling approaches to enhance service delivery and promote acceptance of family planning interventions (31–34, 36). These findings are further supported by the 2022 WHO Abortion Care Guideline, which frames safe abortion and PAFP as health and human rights priorities. The guideline advocates for immediate post-abortion contraception and the expansion of provider roles, including community health workers and pharmacists, to reduce repeat unintended pregnancies and improve maternal health through accessible, high-quality care (9, 10).
Strengths and limitations of the umbrella review
Strengths of the study
This umbrella review provides a robust and comprehensive synthesis of existing systematic reviews and meta-analyses on post-abortion family planning (PAFP) utilization among women of reproductive age in Africa. By consolidating fragmented evidence, it offers clearer insights into prevalence patterns and key determinants that are critical for informing health policy and improving service delivery. This study applied rigorous inclusion criteria and quality appraisal methods using the AMSTAR-2 tool, with scores ranging from 14 to 16, thereby ensuring methodological integrity. Its regional focus enhances contextual relevance, addressing the unique challenges and opportunities within African health systems. Furthermore, the review identifies research gaps and offers policy-relevant, evidence-based recommendations aimed at promoting reproductive health equity in low-resource settings. The inclusion of both published and unpublished studies strengthens the comprehensiveness of the evidence base, while the exclusion of low-quality and non-systematic literature ensures the reliability and clarity of the findings.
Limitations
While this umbrella review offers a comprehensive synthesis of systematic reviews and meta-analyses on post-abortion family planning (PAFP) in Africa, several limitations should be acknowledged. First, the findings are influenced by the quality of the included reviews, which may vary in methodological rigor. Despite efforts to minimize bias, publication bias remains a concern, as studies reporting significant results are more likely to be published. Second, variability in the definitions and measurements of PAFP across studies may affect the comparability and interpretation of pooled estimates. Third, the exclusion of non-English publications and qualitative studies may limit the depth and contextual richness of the findings, particularly in understanding cultural and systemic barriers to PAFP uptake. Finally, it is important to note that self-managed abortions are often underreported or undetected in facility-based studies, which may lead to underestimation of post-abortion family planning needs. These limitations suggest the need for more inclusive and methodologically diverse research to fully capture the complexity of PAFP utilization in African settings.
Implications for public health and policy
The findings of this umbrella review underscore the urgent need for targeted policy interventions to improve post-abortion family planning (PAFP) utilization across Africa.
First, integrating PAFP counseling into routine post-abortion care is essential to ensure that women receive timely, informed, and supportive guidance on contraceptive options. This integration should be standardized across all health facilities and embedded within national reproductive health protocols.
Second, targeted interventions are needed for vulnerable groups, particularly younger women and those with low educational attainment, who face greater barriers to accessing family planning services. Youth-friendly and culturally sensitive approaches should be prioritized to address these disparities.
Third, strengthening health systems is critical to reducing regional inequalities in PAFP access. This includes improving service delivery infrastructure, training healthcare providers, and expanding outreach programs in underserved areas. By addressing these policy gaps, countries can move closer to achieving reproductive health equity and reducing the incidence of unintended pregnancies and repeat abortions.
Strengthening health systems and community-based delivery of culturally sensitive, rights-based family planning services is essential to reduce repeat abortions and improve maternal health outcomes across the continent.
Conclusion and recommendations
This umbrella review found that the pooled prevalence of post-abortion family planning (PAFP) utilization among women of reproductive age in Africa is 62.82%, with Ethiopia showing a higher uptake of 69.31%. Key determinants influencing PAFP use include younger age (15–24 years), being married, higher educational attainment, prior contraceptive use, history of abortion, unintended pregnancy, and receiving counseling. These factors highlight the need for targeted, equity-driven interventions.
To address the gaps in post-abortion family planning (PAFP) utilization across Africa, a coordinated, multisectoral strategy is essential. Governments, health systems, educational institutions, and community organizations must work in collaboration to strengthen reproductive health policies and ensure universal access to post-abortion care. Key actions include the following:
Integrating PAFP counseling into all levels of post-abortion care to support informed decision-making and continuity of contraceptive use;
Expanding access to a diverse range of contraceptive methods, particularly LARCs, to promote choice and reduce repeat abortions;
Targeting vulnerable populations, especially younger women and those with limited education, through youth-friendly services, community outreach, and tailored communication strategies; and
Strengthening health systems, especially in underserved regions, by investing in provider training, infrastructure, and equitable service delivery.
These measures will promote reproductive health equity, reduce unintended pregnancies, and improve maternal health outcomes across the continent.
Future research should explore the longitudinal outcomes of PAFP interventions, assess the impact of culturally tailored counseling strategies, and incorporate qualitative studies to better understand contextual barriers. Such efforts will support evidence-based policymaking and promote reproductive health equity across Africa.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
DK: Writing – review & editing, Formal analysis, Resources, Writing – original draft, Methodology, Validation, Data curation, Software, Visualization, Supervision, Investigation, Conceptualization, Funding acquisition, Project administration. DD: Investigation, Methodology, Conceptualization, Data curation, Software, Writing – review & editing, Visualization, Validation, Resources, Supervision, Funding acquisition, Formal analysis, Writing – original draft, Project administration. SG: Supervision, Validation, Project administration, Conceptualization, Data curation, Writing – review & editing, Funding acquisition, Methodology, Writing – original draft, Formal analysis, Software, Resources, Visualization, Investigation.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to thank the Faculty of Medicine and Health Sciences, Stellenbosch University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence, and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frph.2025.1687886/full#supplementary-material
Abbreviations
AMSTAR, Assessment of Multiple Systematic Reviews; CI, confidence interval; CAC, comprehensive abortion care; FP, family planning; IUD, intrauterine device; LARCs, long-acting reversible contraceptives; MeSH, medical subject headings; PAFP, post-abortion family planning; OR, odds ratio; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analysis; PICO, Patient/Population, Intervention, Comparison, and Outcome; SAMM, severe acute maternal morbidity; SRMs, systematic reviews and meta-analyses; WHO, World Health Organization.
References
1. Cresswell JA, Alexander M, Chong MYC, Link HM, Pejchinovska M, Gazeley U, et al. Global and regional causes of maternal deaths 2009–20: a WHO systematic analysis. Lancet Glob Health. (2025) 13(4):e626–34. doi: 10.1016/S2214-109X(24)00560-6
2. World Health Organization. Trends in Maternal Mortality Estimates 2000 to 2023: Estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. Geneva: World Health Organization (WHO) (2025). Available online at: https://www.who.int/publications/i/item/9789240108462 (Accessed June 18, 2025).
3. World Health Organization. Access to Safe Abortion Critical for Health of Women and Girls. Geneva: World Health Organization (WHO) (2022). Available online at: http://www.who.Int/news/item/09-03-2022-access-to-safe-abortion-critical-for-health-of-women-and-girls (Accessed June 10, 2025).
5. Treder KM, Amutah-Onukagha N, White KO. Abortion bans will exacerbate already severe racial inequities in maternal mortality. Women's Health Issues. (2023) 33(4):328–32. doi: 10.1016/j.whi.2023.04.007
6. Bell SO, Shankar M, Moreau C. Global epidemiology of induced abortion, in Oxford Research Encyclopedia of Global Public Health. (2021).
7. World Health Organization. Comprehensive Abortion Care: A Health Facility Assessment Tool, in Comprehensive Abortion Care: A Health Facility Assessment Tool. (2023).
8. Gerdts C, Bell SO, Shankar M, Jayaweera RT, Owolabi O. Beyond safety: the 2022 WHO abortion guidelines and the future of abortion safety measurement. BMJ Glob Health. (2022) 7(6):e009557. doi: 10.1136/bmjgh-2022-009557
9. Kim CR, Lavelanet A, Ganatra B. Enabling access to quality abortion care: WHO’s abortion care guideline. Lancet Glob Health. (2022) 10(4):e467–8. doi: 10.1016/S2214-109X(21)00552-0
10. World Health Organization. Abortion Care Guideline. Geneva: World Health Organization (2022). Available online at: https://pesquisa.bvsalud.org/portal/resource/pt/who-349316 (Accessed June 18, 2025).
11. Macleod CI, Reynolds JH, Delate R. Women who sell sex in Eastern and Southern Africa: a scoping review of non-barrier contraception, pregnancy and abortion. Public Health Rev. (2022) 43:1604376. doi: 10.3389/phrs.2022.1604376
12. Stewart H, McCall SJ, McPherson C, Towers LC, Lloyd B, Fletcher J, et al. Effectiveness of peri-abortion counselling in preventing subsequent unplanned pregnancy: a systematic review of randomised controlled trials. J Fam Plann Reprod Health Care. (2016) 42(1):59–67. doi: 10.1136/jfprhc-2014-101096
13. Ngalame AN, Tchounzou R, Neng HT, Mangala FGN, Inna R, Kamdem DM, et al. Improving post abortion care (PAC) delivery in Sub-Saharan Africa: a literature review. Open J Obstet Gynecol. (2020) 10(9):1295–306. doi: 10.4236/ojog.2020.1090119
14. Woldemichael D, Agero G, Jima A, Woldemichael B. Postabortion family planning utilization and associated factors among women seeking abortion services: a cross-sectional study. Can J Fam Youth. (2023) 15(3):157–71. doi: 10.29173/cjfy29953
15. Bizuneh AD, Azeze GG. Post-abortion family planning use, method preference, and its determinant factors in Eastern Africa: a systematic review and meta-analysis. Syst Rev. (2021) 10(1):172. doi: 10.1186/s13643-021-01731-4
16. Beyene FY, Tesfu AA, Wudineh KG, Sendeku FW, Ayenew AA. Utilization and its factors of post abortion modern contraceptive in Ethiopia: a systematic review and meta-analysis. Reprod Health. (2021) 18(1):143. doi: 10.1186/s12978-021-01195-8
17. Che Y, Liu X, Zhang B, Cheng L. Oral contraception following abortion a systematic review and meta-analysis. Medicine (Baltimore). (2016) 95(27):16. doi: 10.1097/MD.0000000000003825
18. Dagnew GW, Asresie MB. Post-abortion contraceptive uptake, choices, and factors associated with it among women seeking abortion services in Africa: a systematic review and meta-analysis. Front Glob Womens Health. (2025) 6:1478797. doi: 10.3389/fgwh.2025.1478797
19. Valentine JC, Pigott TD, Rothstein HR. How many studies do you need? A primer on statistical power for meta-analysis. J Educ Behav Stat. (2010) 35(2):215–47. doi: 10.3102/1076998609346961
20. Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. JBI Evid Implement. (2015) 13(3):132–40. doi: 10.1097/XEB.0000000000000055
21. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Br Med J. (2017) 358:j4008. doi: 10.1136/bmj.j4008
22. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21(11):1539–58. doi: 10.1002/sim.1186
23. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7(3):177–88. doi: 10.1016/0197-2456(86)90046-2
24. Chandler J, Cumpston M, Li T, Page MJ, Welch VJ. Cochrane Handbook for Systematic Reviews of Interventions. Hoboken: Wiley (2019), Vol. 4.
25. Cherie N, Gebrie N, Yasin T. Post abortion contraceptive use and determinant factors in Ethiopia: a systematic review and meta-analysis. Curr Women's Health Rev. (2022) 18(2):27–37. doi: 10.2174/1573404817666210315150854
26. Mengistie BA, Abiy SA, Anteneh TA, Wubneh SB, Andualem F, Melese M, et al. Post-abortion family planning use and its determinants among women who received abortion care in Sub-Saharan Africa: a systematic review and meta-analysis. Syst Rev. (2025) 14(1):1–17. doi: 10.1186/s13643-025-02837-9
27. Wake GE, Fitie GW, Tizazu MA. A systematic review and meta-analysis on post-abortion contraceptive utilization and associated factors in Ethiopia. Front Public Health. (2022) 10:883710. doi: 10.3389/fpubh.2022.883710
28. Buckingham P, Moulton JE, Subasinghe AK, Amos N, Mazza D. Acceptability of immediate postpartum and post-abortion long-acting reversible contraception provision to adolescents: a systematic review. Acta Obstet Gynecol Scand. (2021) 100(4):629–40. doi: 10.1111/aogs.14129
29. Ferreira ALCG, Lemos A, Figueiroa JN, de Souza AI. Effectiveness of contraceptive counselling of women following an abortion: a systematic review and meta-analysis. Eur J Contracept Reprod Health Care. (2009) 14(1):1–9. doi: 10.1080/13625180802549970
30. Roe AH, Bartz D. Contraception after surgical and medical abortion: a review. Obstet Gynecol Surv. (2017) 72(8):487–93. doi: 10.1097/OGX.0000000000000463
31. Rogers C, Dantas JAR. Access to contraception and sexual and reproductive health information post-abortion: a systematic review of literature from low- and middle-income countries. J Fam Plann Reprod Health Care. (2017) 43(4):309–18. doi: 10.1136/jfprhc-2016-101469
32. Rossier C, Marchin A, Kim C, Ganatra B. Disclosure to social network members among abortion-seeking women in low-and middle-income countries with restrictive access: a systematic review. Reprod Health. (2021) 18(1):114. doi: 10.1186/s12978-021-01165-0
33. Schmidt-Hansen M, Hawkins JE, Lord J, Williams K, Lohr PA, Hasler E, et al. Long-acting reversible contraception immediately after medical abortion: systematic review with meta-analyses. Hum Reprod Update. (2020) 26(2):141–60. doi: 10.1093/humupd/dmz040
34. Sedlecky K, Stanković Z. Contraception for adolescents after abortion. Eur J Contracept Reprod Health Care. (2016) 21(1):4–14. doi: 10.3109/13625187.2015.1082175
35. Tripney J, Bird K, Kwan I, Kavanagh J. The impact of post-abortion care family planning counselling and services in low-income countries: a systematic review of the evidence. (2011).
36. Wang X, Deng M, Zhu Y, Wu S, Mao Q, Wang H. Effectiveness of post-abortion care services to protect women’s fertility in China: a systematic review with meta-analysis. PLoS One. (2024) 19(6):e0304221. doi: 10.1371/journal.pone.0304221
37. Page MJ, Boutron I, Tetzlaff JM, Chou R, Lalu MM, Mayo-Wilson E, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
Keywords: Africa, determinants, global health policy, post-abortion family planning utilization, prevalence, umbrella review, women of reproductive aget
Citation: Kaura DK, Demissie DB and Gebhardt S (2025) Evidence and determinants of post-abortion family planning utilization among women of reproductive age in Africa: an umbrella review. Front. Reprod. Health 7:1687886. doi: 10.3389/frph.2025.1687886
Received: 18 August 2025; Accepted: 22 October 2025;
Published: 13 November 2025.
Edited by:
Monica Ewomazino Akokuwebe, University of the Witwatersrand, South AfricaReviewed by:
John Cleland, University of London, United KingdomBerhanemeskel Weldegerima Atsbeha, University of Gondar, Ethiopia
Copyright: © 2025 Kaura, Demissie and Gebhardt. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dereje Bayissa Demissie, Mjc3ODYwMDVAc3VuLmFjLnph
 Doreen Kainyu Kaura1
Doreen Kainyu Kaura1 Dereje Bayissa Demissie
Dereje Bayissa Demissie Stefan Gebhardt
Stefan Gebhardt