- 1Graduate Program in Rehabilitation Sciences, Universidade Nove de Julho, São Paulo, Brazil
- 2Pediatric Department, Federal University of São Paulo, São Paulo, Brazil
- 3Child Development and Exercise Center, University Medical Center Utrecht, Utrecht, Netherlands
Background: Oxygen uptake (VO2) evaluations by cardiopulmonary exercise test is expensive and time-consuming. Estimating VO2 based on a field test would be an alternative.
Objective: To develop and validate an equation to predict VO2peak based on the modified shuttle test (MST).
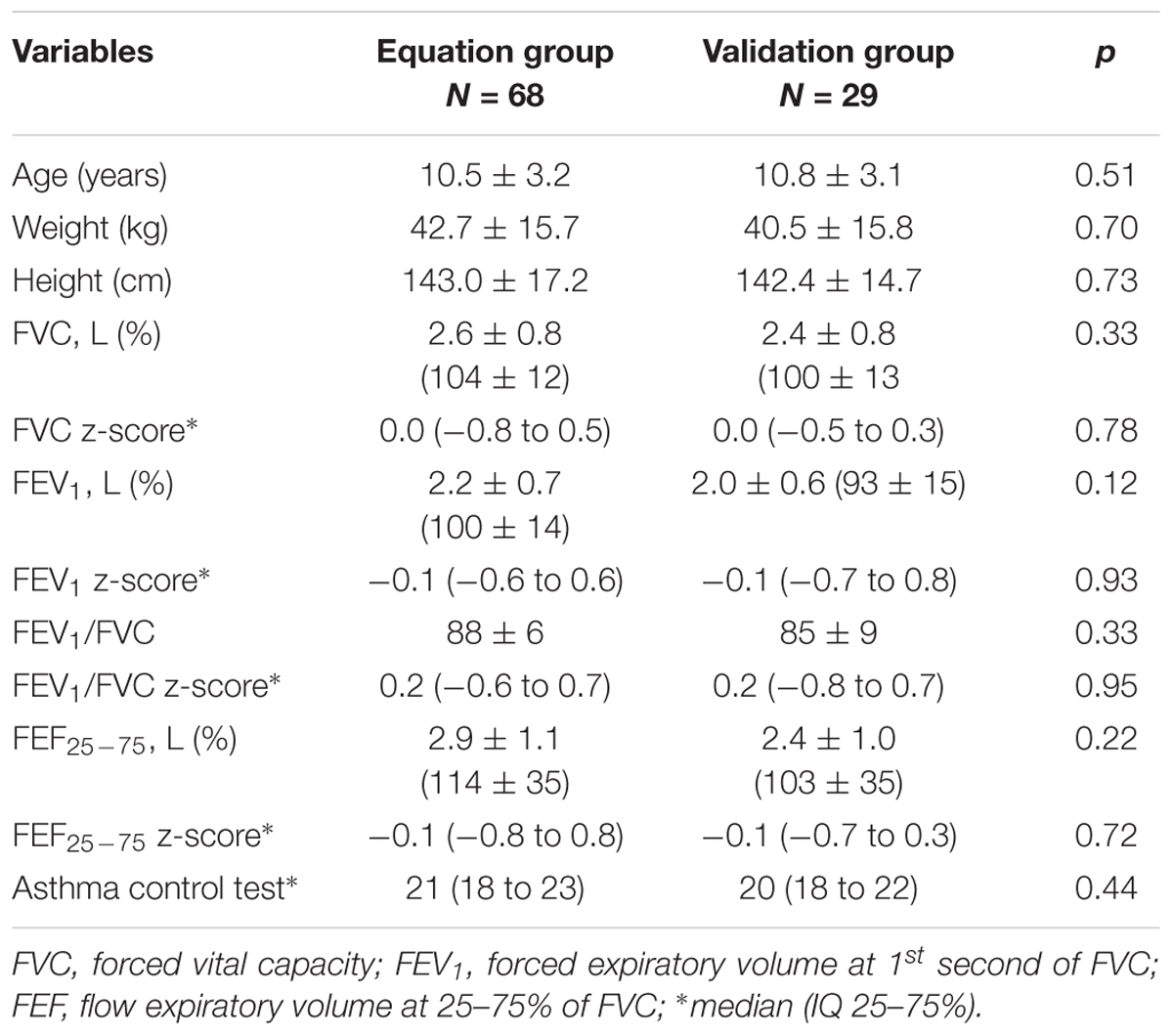
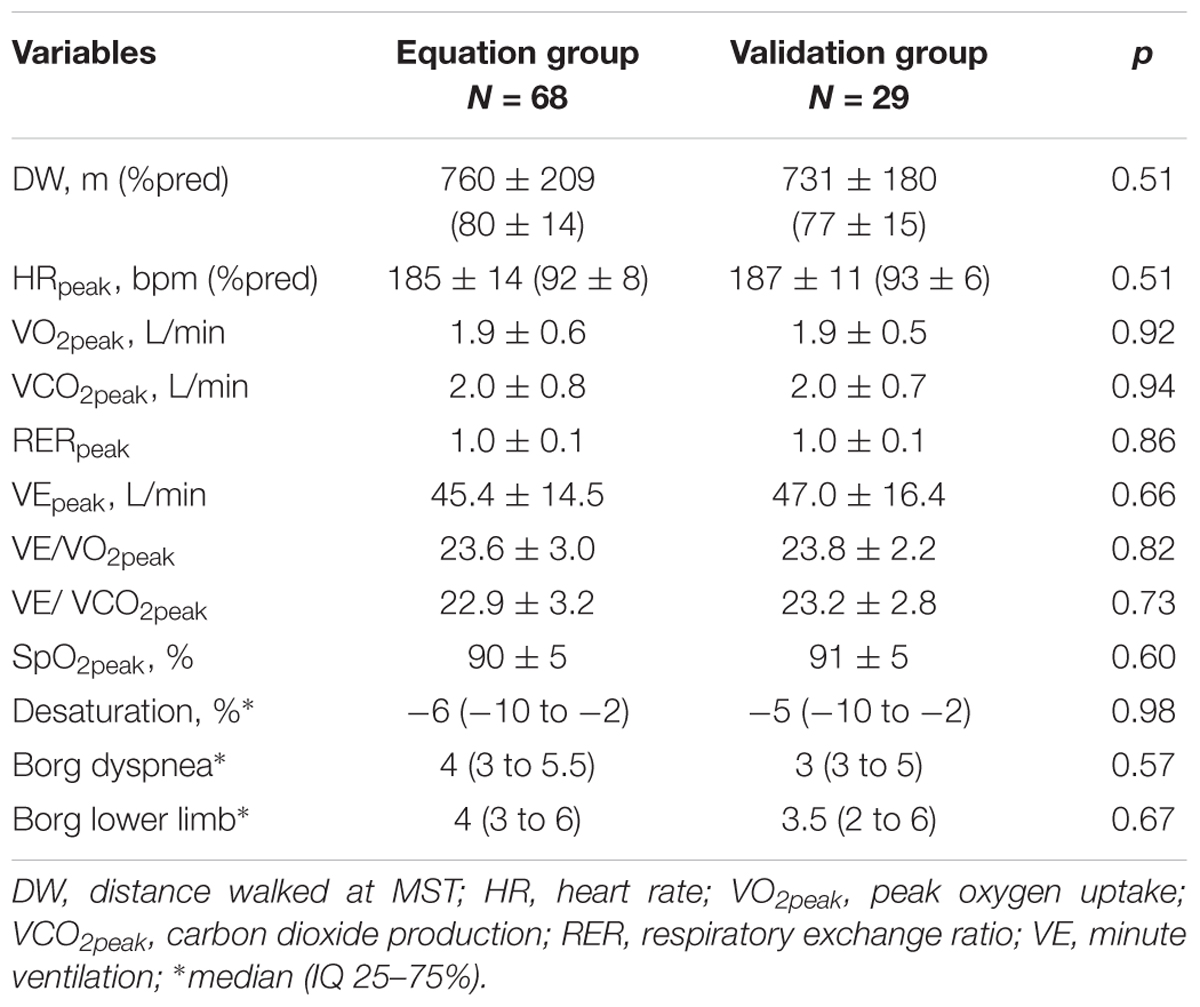
Methods: Cross sectional study, with 97 children and adolescents with asthma. Participants were divided in two groups: the equation group (EG), to construct the equation model of VO2peak, and the cross-validation group (VG). Each subject performed the MST twice using a portable gas analyzer. The peak VO2peak during MST was used in the equation model. The patients’ height, weight, gender, and distance walked (DW) during MST were tested as independent variables.
Results: The final model [-0.457 + (gender × 0.139) + (weight × 0.025) + (DW × 0.002)] explained 87% of VO2peak variation. The VO2peak predicted was similar to VO2peak measured by gas analyzer (1.9 ± 0.5 L/min and 2.0 ± 0.5 L/min, respectively) (p = 0.67), and presented significant ICC 0.91 (IC95% 0.77 to 0.96); p < 0.001. The Bland–Altman analysis showed low bias (-0.15 L/min) and limits of agreement (-0.65 to 0.35 L/min). There was no difference in DW between EG (760 ± 209 m) and VG (731 ± 180 m), p = 0.51.
Conclusion: The developed equation adequately predicts VO2peak in pediatric patients with asthma.
Introduction
Asthma is a prevalent chronic pulmonary disease in the childhood. It is usually characterized by chronic airway inflammation that results in a decreased aerobic capacity, and its prevalence is increasing in many countries (Global Initiative for Asthma [GINA], 2014).
Cardiorespiratory fitness is considered an important marker of health in youth, since high cardiorespiratory fitness in youth have shown to track do adult ages (Hallal et al., 2006). In addition, children with higher cardiorespiratory fitness present lower prevalence of cardiovascular risk factors including obesity and high blood pressure (Boddy et al., 2014; Burns et al., 2016). Therefore, assessment of cardiorespiratory fitness can provide valuable information regarding health status in pediatric populations.
The measurement of maximal peak oxygen uptake (VO2max) have been considered the gold standard for cardiorespiratory fitness assessment (American Thoracic Society, 2003). However, due to its cost and time to assessment, field tests, such as incremental shuttle-walk test, have been proposed to assess cardiorespiratory fitness in clinical settings (Singh et al., 2014). In patients with asthma, a previous study analyzed the validity of shuttle-run test (Ahmaidi et al., 1993), a progressive externally-paced field test, to predict VO2peak in adolescents with asthma, and observed that the shuttle-run test has sufficient validity to assess oxygen uptake. However, the severer asthmatic patients could not perform the shuttle-run because there is a high speed increasing.
In this context, field tests that includes walking, such as shuttle-walk test (Singh et al., 1992) or modified shuttle-walk test (Bradley et al., 1999) (MST), have been proposed for patients with pulmonary diseases. The studies have observed significant correlations between the performance in incremental shuttle-walk test and VO2peak, in adults with various chronic conditions, including asthma (Noonan and Dean, 2000; Mayorga-Vega et al., 2015). However, whether similar relationships occur in children or adolescents with asthma is unknown. Thus, the aims of the current study were (1) to evaluate the relationship between MST and VO2peak in children and adolescents with asthma, and (2) to develop and validate an equation to predict VO2peak based on MST test.
Materials and Methods
Patients
Patients between 6 and 18 years of age were recruited in 2013 through 2015 from the Pediatric Department of the Federal University of São Paulo, Brazil. All patients had been diagnosed by a pediatric physician, according to the GINA steps (Global Initiative for Asthma [GINA], 2014), as having asthma for at least 6 months, and had been on a stable treatment regime for at least 3 months. Patients were excluded from this study when no regular medication regime was being followed, if any exacerbation had occurred in the last 4 weeks before inclusion, or if the patient was not able to perform any of the tests needed for this study.
Patients were divided into two groups: (1) the equation group (EG), which included patients who were studied to construct the equation model of VO2peak, and (2) a cross-validation group (VG), which included patients for preliminary validation of the equation model. Patients were included in the study after their legal guardians read, agreed to, and signed the informed consent form, and the patient had signed the informed consent if they were 12 years of age or older. The study was approved by the Associaçao Educacional Nove de Julho Ethical Committee, São Paulo, Brazil (#738192/2014).
Study Design and Protocol
This is a cross sectional study. All outcome measurements needed for this study were taken on two different days. The outcome measurements that were assessed included an asthma control questionnaire, lung function spirometry (pre- and post-bronchodilator), the MST and the cardiopulmonary exercise test (CPET). The MST and CPET were performed on different days, in random order.
Asthma Control Questionnaire
The asthma control test (ACT) is a simple questionnaire to assess asthma control based on patient views, used for patients over 12 years old. The children’s ACT (C-ACT) is used for children 4 through 11 years old (Liu et al., 2007). Each question is answered on a scale of 1 (worst) to 5 (best). The highest total score for ACT is 25, and for C-ACT is 27. Asthma is considered controlled when the score is 20 or over. A score of 16 to 19 is considered partially-controlled asthma, and 15 or under is uncontrolled asthma (Liu et al., 2007).
Lung Function
Spirometry was performed with ULTIMA CPX equipment (MGC Diagnostics Corporation. Saint Paul, MN, United States). The technical procedure, acceptance criteria and reproducibility were according to ATS/ERS statement (Wanger et al., 2005). The patients repeated the test after use of a bronchodilator (salbutamol, 400 μg). The forced vital capacity (FVC), expiratory forced volume at the first second (FEV1), FEV1/FVC, and forced expiratory flow at 25 to 75% of FVC (FEF25-75) were expressed in liters and percentage of predict value (Polgar and Promadhat, 1971), and z-score based on the mean value.
Modified Shuttle Test
The modified shuttle test (MST) was performed in a 10-m-long corridor according to the previous description (Bradley et al., 1999). It is an externally-paced test dictated by an audio signal. The test has 15 levels, in which the speed increases every minute, ranging from 1.8 to 10.2 km/h, and requires the patient to walk/run at the increasing speed. The test was halted if the patient was not able to reach the distance two consecutive times, if he/she needed to stop due to fatigue or breathlessness, or if SpO2 fell below 82% (Singh et al., 2014). Each patient performed the test twice on the same day, with a 30-min rest in between. Heart rate, measured with a Polar FT70® monitor, and SpO2, measured with a handheld oximeter (920M, Philips®, United States) were continuously evaluated. The modified Borg scale was used to observe lower limb fatigue and dyspnea at the beginning and end of the test (Borg, 1982). The greatest DW for the two MST, expressed in meters and as a percentage of predicted value (Lanza et al., 2015), was used for analysis as an outcome.
Cardiopulmonary Exercise Test
The CPET was performed to identify if MST was maximal test. The cycle ergometer (Corival®, LODE BV Medical Technology, Groningen, Netherlands) was used. After 2 min of unloaded cycling, the load was increased (10 to 20 watts/minute) (Godfrey et al., 1971), and the test was aimed to last between 8 and 12 min (American Thoracic Society, 2003). The heart rate and SpO2 were continuously recorded. Blood pressure was measured every 2 min during the test. Modified Borg dyspnea and Modified Borg lower limb were assessed at beginning and the end of the test. The primary outcome of CPET was the VO2peak.
All patients performed the MST and CPET while connected to a validated (Kautza et al., 2004) system for gas exchange analyses (VO2000, MedGraphics Corporation®, Saint Paul, MN, United States). The VO2, pulmonary dioxide production (VCO2), the relationship between them (RER: VCO2/VO2), and minute ventilation (VE) were continuously measured.
Statistical Analysis
The Shapiro–Wilk test was used to determine the normality of the data. The variables were described by mean ± SD or median (IQ 25 to 75%), according to the normality of the data. The paired t-student test was used to compare the characteristics between CPET and MST. The unpaired Student’s t-test or Mann–Whitney U-test was used to compare the characteristics of CPET and MST between EG and VG groups. The Pearson’s coefficient of correlation was performed to study the correlation between VO2peak and age, height, weight, and distance walked. Subsequently, the multiple backward linear regression analysis was performed to identify predictors of the dependent variable (VO2peak) measured during MST. Age, height, weight, sex, and distance walked during MST were tested as independent variables. To validate the equation, the measured VO2peak of the VG patients was compared to the predicted VO2peak. The intraclass correlation coefficient (ICC) and its 95% confidence interval (CI) were calculated using an absolute agreement definition, to evaluate the relative reliability between VO2peak measured and predicted. The agreement between VO2peak measured and predicted was assessed by Bland–Altman analysis. A sample size of at least 15 patients per variable was used in the final equation model developed using linear regression. The post hoc power of the validation group was calculated.
SPSS version 20 (Chicago, IL, United States) statistical software was used in the study. A p-value less than 0.05 was considered statistically significant.
Results
A total of 153 children and adolescents with asthma were invited to participate, of which 97 were included (34 did not sign the informed consent form, 17 had asthma exacerbation occurring in the past 4 weeks, and five failed to follow the test procedure). Assuming a ratio 2:1, a total of 68 patients were randomly included in the equation group (56% boys). Another 29 VG patients (61% boys) were evaluated to validate the equation. They also had normal lung function and a median GINA step of 3 (2 to 4), Table 1.
Of 84 (86%) of 97 patients performed the CPET according to the recommendations. The variables of CPET and MST were compared to be sure that a field test (the MST) had similar responses to the gold standard test. They had a significantly higher VO2peak at MST (1.9 ± 0.6 L/min) than they did at CPET (1.5 ± 0.4 L/min), p < 0.001. A similar result was observed for their heart rate (MST: 186 ± 13 bpm vs. CPET: 178 ± 11 bpm; p < 0.001), but not statically difference for RERpeak between tests (MST: 1.1 ± 0.1 vs. CPET: 1.1 ± 0.1; p = 0.29).
All patients stopped the MST at maximal effort (leg fatigue or breathlessness reported on the Borg scale, or incapacity to follow the test speed). There was a significant association between VO2peak, distance walked, age, weight, and height (r > 0.7; p < 0.05) for the EG (Figure 1). The final model of the linear multiple regression analysis included gender, weight, and distance walked during MST. The standardized coefficient β is shown in Table 2.
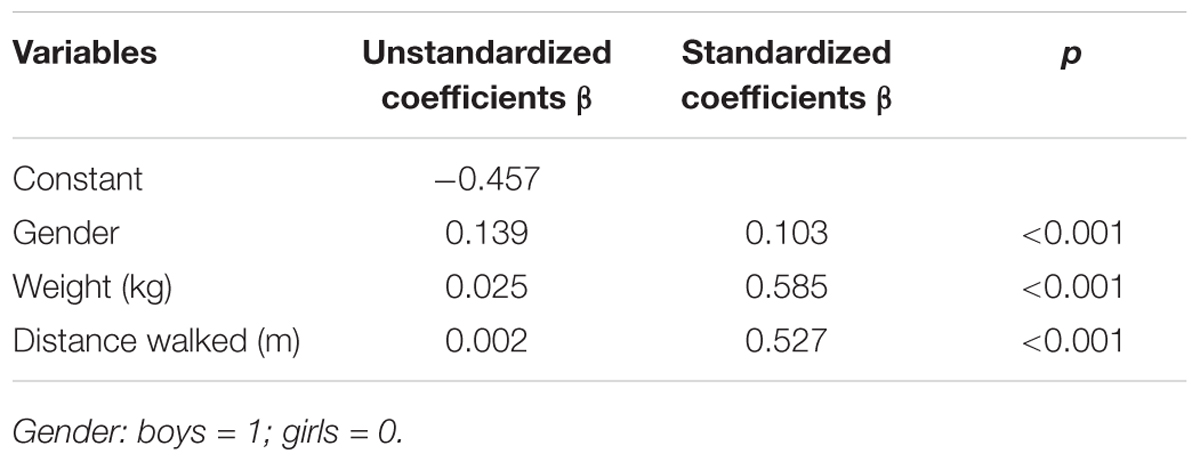
TABLE 2. Predicted variables for peak oxygen uptake, VO2peak in L/min, based on the modified shuttle test obtained from multiple linear regression analysis.
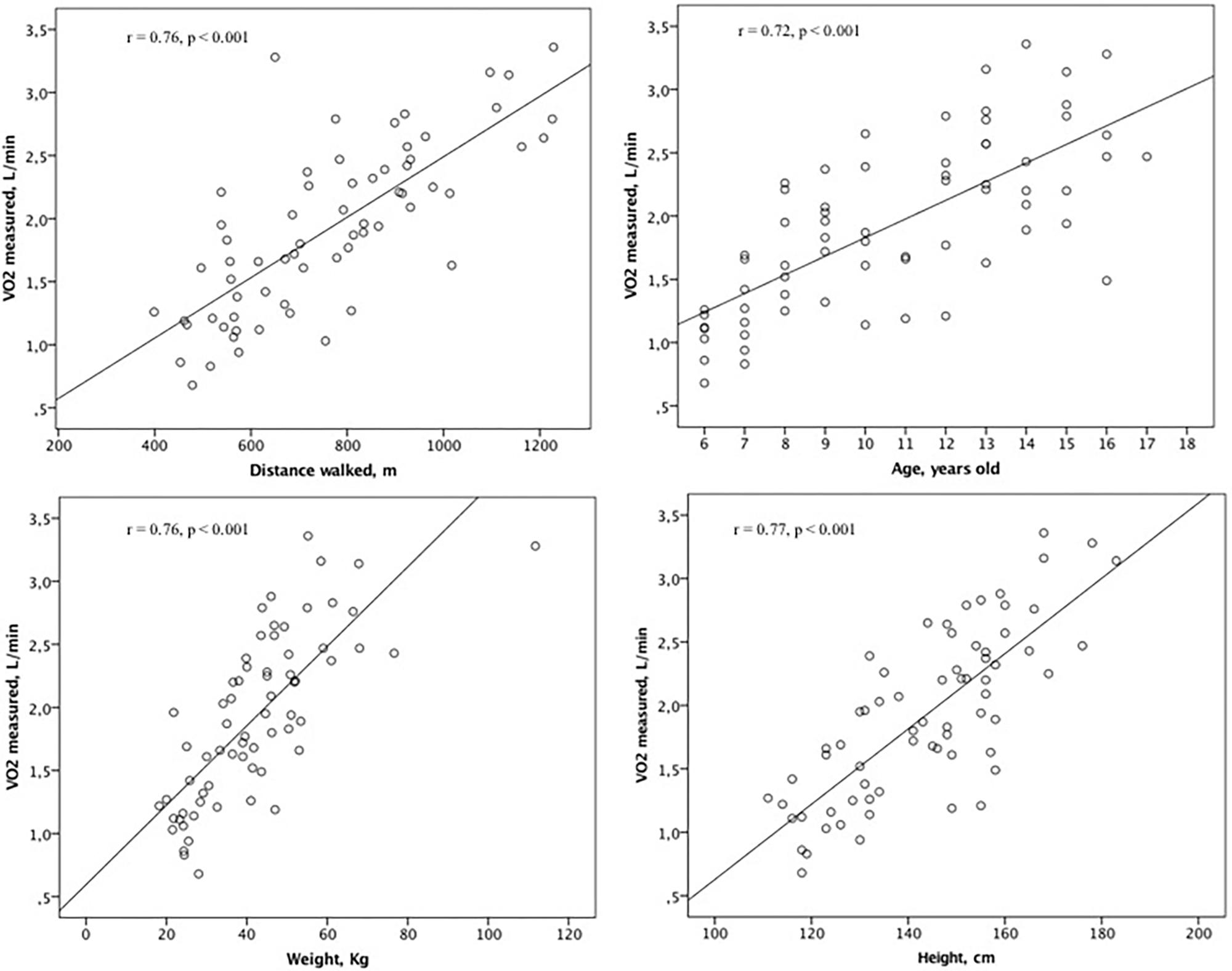
FIGURE 1. Association between VO2peak, distance walked, age, weight, and height for the equation group.
Adjusted R2: 0.87; SEE: 0.24;
Gender: boys = 1; girls = 0;
Weight: kg;
DW: distance walked at MST, in meters.
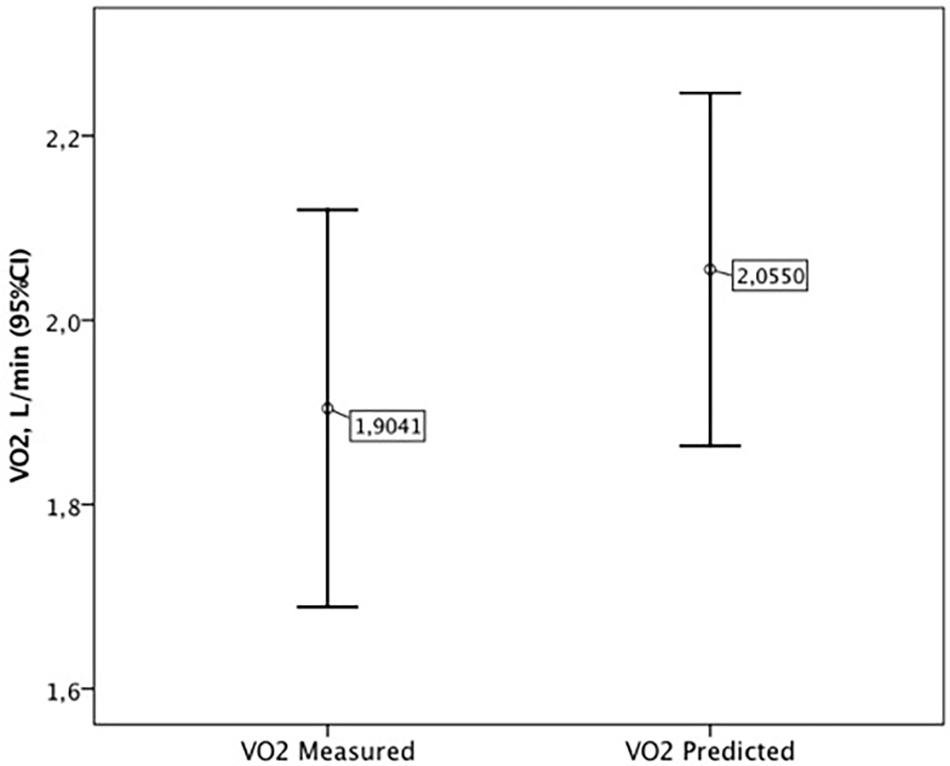
There was no difference between the equation and validations groups in the variables at the peak of MST (Table 3). No adverse events were reported during or after the MST. The VO2peak measured during the MST of the validation group (1.9 ± 0.5 L/min) was not different of the VO2peak predicted by the equation (2.0 ± 0.5 L/min), p = 0.67 (Figure 2). The post hoc power between the VO2peak measured and predicted was 83%.
The ICC of the VO2peak measured and predicted in the validation group was highly significant (ICC: 0.91, CI95% 0.77 to 0.96; p < 0.001). The Bland–Altman analysis showed a mean bias of -0.15 L/min, with the limits of agreement ranging from -0.65 to 0.35 L/min.
Discussion
The main results of the present study were: (i) gender, weight, and DW during MST explained 87% of the variance in VO2peak; (ii) There was no difference between the equation and validations groups in the variables at the peak of MST; (iii) The ICC of the VO2peak measured and predicted in the validation group was highly significant; (iv) MST elicited higher peak VO2 and heart rate than CPET.
It was observed highest VO2peak and heart rate during MST compared to the CPET. This result occurred because the CPET was performed on a cycle ergometer and MST is a walk/run test. The CPET is considered a gold standard assessment for exercise capacity, regardless of whether it is performed on a treadmill or a cycle ergometer (American Thoracic Society, 2003), but it is known that VO2peak is higher on a treadmill (Maffeis et al., 1994).
As expected weight and gender were included in the VO2peak prediction equation. It is known that the absolute peak oxygen uptake is related to a child’s growth (Vinet et al., 2003). Usually, the VO2peak is 20% higher in children than in adults (Williams et al., 1985). This is because children have higher capillary and mitochondrial density, and oxidative enzyme activity than do adults (Williams et al., 1985; Rowland et al., 2000; Armstrong and Barker, 2009). Gender also influences the VO2peak (Rowland et al., 2000). Girls have usually lower VO2peak levels compared to boys, at least for the onset of puberty (Armstrong and Welsman, 1994). Oxygen uptake is related to the stroke volume of the heart, which is greater in boys, justifying the gender differences (Willmore et al., 2008). Additionally, boys have a higher percentage of free-fat mass (especially after puberty) compared to girls, which further increases their oxygen uptake during maximal exercise (Rowland et al., 2000; Vinet et al., 2003).
In same way, the distance walked was included in the final model of VO2peak equation. Because of the incremental increase of the walking speed every minute of MST, the distance walked is related to the intensity of the exercise, and hence, the oxygen uptake. This is in agreement with previous studies in adults (Léger et al., 1988; Larsen et al., 2002; Weisgerber et al., 2009; Ross et al., 2010) that also included the distance walked to predict VO2peak. However, in these studies this variable explained less than 50% of the VO2peak, while in the current study DW, gender and weight explained 87%. This can be justified because these independent variables are proportional related to the oxygen uptake.
This is the first study to determine an equation for prediction of VO2peak based on the MST in children and adolescents with asthma. The results in the cross-validation asthmatic patients revealed a high correlation between the predicted and obtained VO2peak, with small bias between them -0.15 L/min. In addition, although there was a wide limit of agreement, greater than 0.5 L/min (∼25% of VO2peak), it is similar to the results of Ahmaidi et al. (1993) who observed similar variability (∼25% of VO2peak) between VO2peak measured and predicted in a study of patients with adolescents with asthma.
In practical terms, our proposed equation to estimate VO2peak in children and adolescents from 6 to 18 years with asthma presented psychometric characteristics similar than other equations in adolescent and adult patients with asthma. The MST seems to be an appropriate test to evaluate pediatric patients, because it is performed at a wide range of speeds, and this avoids floor or ceiling effects (Saglam et al., 2016).
The limitation of this study includes the small number of patients with severe asthma (GINA step 5), which reduced the external validity for the equation in this subgroup of patients. The CPET was not properly performed in all participants, but more than 80% of them performed it. There was not included a control group of healthy participants, and whether differences exist between healthy and asthmatic youth cannot be determined. However, considering that equations for this specific group was not available until now, the inclusion of only asthmatic still relevant to determine an equation for pulmonary chronic conditions.
Conclusion
The developed equation indicated high correlation and low bias in the prediction VO2peak based in the MST in pediatric patients with asthma. Therefore, this test can be a useful alternative to assess VO2peak in clinical settings.
Author Contributions
FL had substantial contributions to the study including: conceptualization/design; supervision/oversight; funding acquisition; formal analysis; drafting significant parts of the work. MR and RS had substantial contributions to the study including: methodology, investigation, data curation. RR-D, GW, and DS had substantial contributions to the study including: critically revising it so as to contribute to the interpretation. MvB, HH, SDC, and TT had substantial contributions to the study including: analysis and interpretation of research data drafting significant parts of the work or critically revising.
Funding
This study was supported by São Paulo Research Foundation (FAPESP) (Grant No. 2014/12040-0) and (Grant No.2018/13654-9). RS was supported by São Paulo Research Foundation (FAPESP) (Grant No. 2016/17553-0).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Ahmaidi, S. B., Varray, A. L., Savy-Pacaux, A. M., and Prefaut, C. G. (1993). Cardiorespiratory fitness evaluation by the shuttle test in asthmatic subjects during aerobic training. Chest 103, 1135–1141. doi: 10.1378/chest.103.4.1135
American Thoracic Society (2003). American College of Chest Physicians. ATS/ACCP Statement on cardiopulmonary exercise testing. Am. J. Respir. Crit. Care Med. 167, 211–277. doi: 10.1164/rccm.167.2.211
Armstrong, N., and Barker, A. R. (2009). Oxygen uptake kinetics in children and adolescents: a review. Pediatr. Exerc. Sci. 21, 130–147. doi: 10.1123/pes.21.2.130
Armstrong, N., and Welsman, J. R. (1994). Assessemt and interpretation of aerobic fitness in children and adolescents. Exerc. Sport Sci. Rev. 22, 435–476. doi: 10.1249/00003677-199401000-00016
Boddy, L. M., Murphy, M. H., Cunningham, C., Breslin, G., Foweather, L., Gobbi, R., et al. (2014). Physical activity, cardiorespiratory fitness, and clustered cardiometabolic risk in 10- to 12-year-old school children: the REACH Y6 study. Am. J. Hum. Biol. 26, 446–451. doi: 10.1002/ajhb.22537
Borg, G. A. (1982). Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 14, 377–381. doi: 10.1249/00005768-198205000-00012
Bradley, J., Howard, J., Wallace, E., and Elborn, S. (1999). Validity of a modified shuttle test in adult cystic fibrosis. Thorax 54, 437–439. doi: 10.1136/thx.54.5.437
Burns, R. D., Brusseau, T. A., Fang, Y., Fu, Y., and Hannon, J. C. (2016). Waist-to-Height ratio, aerobic fitness, and cardiometabolic risk in hispanic children from low-income U.S. Schools. Pediatr. Exerc. Sci. 28, 388–396. doi: 10.1123/pes.2016-0016
Global Initiative for Asthma [GINA] (2014). Available at: www.ginasthma.org
Godfrey, S., Davies, C. T., and Wozniak, E. (1971). Cardio-respiratory response to exercise in normal children. Clin. Sci. 40, 419–431. doi: 10.1042/cs0400419
Hallal, P. C., Victora, C. G., Azevedo, M. R., and Wells, J. C. (2006). Adolescent physical activity and health: a systematic review. Sports Med. 36, 1019–1030. doi: 10.2165/00007256-200636120-00003
Kautza, B. C., Kastello, G., and Sothmann, M. S. (2004). Validation of MedGraphics’ VO2000 portable metabolic analyzer and a modified pneumotachometer. Med. Sci. Sports Exerc. 3:S222. doi: 10.1249/00005768-200405001-01063
Lanza, F. C., Zagatto Edo, P., Silva, J. C., Selman, J. P., Imperatori, T. B., Zanatta, D. J., et al. (2015). Reference equation for the incremental shuttle walk test in children and adolescents. J. Pediatr. 167, 1057–1061. doi: 10.1016/j.jpeds.2015.07.068
Larsen, G. E., George, J. D., Alexander, J. L., Fellingham, G. W., Aldana, S. G., and Parcell, A. C. (2002). Prediction of maximum oxygen consumption from walking, jogging, or running. Res. Q. Exerc. Sport 73, 66–72. doi: 10.1080/02701367.2002.10608993
Léger, L. A., Mercier, D., Gadoury, C., and Lambert, J. (1988). The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 6, 93–101. doi: 10.1080/02640418808729800
Liu, A. H., Zeiger, R. S., Sorkness, C. A., Mahr, T., Ostrom, N., Burguess, S., et al. (2007). Development and cross-sectional validation of the childhood asthma control test. J. Allergy Clin. Immunol. 119, 817–825. doi: 10.1016/j.jaci.2006.12.662
Maffeis, C., Schena, F., Zaffanello, M., Zoccante, L., Schutz, Y., and Pinelli, L. (1994). Maximal aerobic power during running and cycling in obese and non-obese children. Acta Paediatr. 83, 113–116. doi: 10.1111/j.1651-2227.1994.tb12965.x
Mayorga-Vega, D., Aguilar-Soto, P., and Viciana, J. (2015). Criterion-related validity of the 20-m shuttle run test for estimating cardiorespiratory fitness: a meta-analysis. J. Sports Sci. Med. 14, 536–547.
Noonan, V., and Dean, E. (2000). Submaximal exercise testing: clinical application and interpretation. Phys. Ther. 80, 782–807.
Polgar, G., and Promadhat, V. (1971). Pulmonary Function Testing in Children: Techniques and Standards. Philadelphia, PA: Saunders.
Ross, R. M., Murthy, J. N., Wollak, I. D., and Jackson, A. S. (2010). The six minute walk test accurately estimates mean peak oxygen uptake. BMC Pulm. Med. 10:31. doi: 10.1186/1471-2466-10-31
Rowland, T., Goff, D., Martel, L., and Ferrone, L. (2000). Influence of cardiac functional capacity on gender differences in maximal oxygen uptake in children. Chest 117, 629–635. doi: 10.1378/chest.117.3.629
Saglam, M., Vardar-Yagli, N., Savci, S., Inal-Ince, D., Aribas, Z., Bosnak-Guclu, M., et al. (2016). Six minute walk test versus incremental shuttle walk test in cystic fibrosis. Pediatr. Int. 58, 887–893. doi: 10.1111/ped.12919
Singh, S. J., Morgan, M. D., Scott, S., Walters, D., and Hardman, A. E. (1992). Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax 47, 1019–1024. doi: 10.1136/thx.47.12.1019
Singh, S. J., Puhan, M. A., Andrianopoulos, V., Hernandes, N. A., Mitchell, K. E., Hill, C. J., et al. (2014). An official systematic review of the European Respiratory Society/American thoracic society: measurement properties of field walking tests in chronic respiratory disease. Eur. Respir. J. 44, 1447–1478. doi: 10.1183/09031936.00150414
Vinet, A., Mandigout, S., Nottin, S., Nguyen, L., Lecoq, A. M., Courteix, D., et al. (2003). Influence of body composition, hemoglobin concentration, and cardiac size and function of gender differences in maximal oxygen uptake in prepubertal children. Chest 124, 1494–1499. doi: 10.1378/chest.124.4.1494
Wanger, J., Clausen, J. L., Coates, A., Pedersen, O. F., Brusasco, V., and Burgos, F. (2005). ATS/ERS task force. Standardisation of the measurement of lung volumes. Eur. Respir. J. 26, 511–522. doi: 10.1183/09031936.05.00035005
Weisgerber, M., Danduran, M., Meurer, J., Hartmann, K., Berger, S., and Flores, G. (2009). Evaluation of Cooper 12-minute walk/run test as a marker of cardiorespiratory fitness in young urban children with persistent asthma. Clin. J. Sport Med. 19, 300–305. doi: 10.1097/JSM.0b013e3181b2077a
Williams, C. A., Carter, H., Jones, A. M., and Doust, J. H. (1985). Oxygen uptake kinetics during treadmill running in boys and men. J. Appl. Physiol. 90, 1700–1706. doi: 10.1152/jappl.2001.90.5.1700
Keywords: shuttle test, asthma, oxygen uptake, prediction equation, validation
Citation: Lanza FC, Reimberg MM, Ritti-Dias R, Scalco RS, Wandalsen GF, Sole D, van Brussel M, Hulzebos HJ, Dal Corso S and Takken T (2018) Validation of the Modified Shuttle Test to Predict Peak Oxygen Uptake in Youth Asthma Patients Under Regular Treatment. Front. Physiol. 9:919. doi: 10.3389/fphys.2018.00919
Received: 19 April 2018; Accepted: 25 June 2018;
Published: 24 July 2018.
Edited by:
Keith Russell Brunt, Dalhousie University, CanadaReviewed by:
Iulia Ioan, Hôpital d’Enfants, FranceManuel Sanchez-Solis, Hospital Universitario Virgen de la Arrixaca, Spain
Copyright © 2018 Lanza, Reimberg, Ritti-Dias, Scalco, Wandalsen, Sole, van Brussel, Hulzebos, Dal Corso and Takken. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fernanda C. Lanza, bGFuemFmZUBnbWFpbC5jb20= Raphael Ritti-Dias, cmFwaGFlbHJpdHRpQGdtYWlsLmNvbQ==
 Fernanda C. Lanza
Fernanda C. Lanza Mariana M. Reimberg
Mariana M. Reimberg Raphael Ritti-Dias
Raphael Ritti-Dias Rebeca S. Scalco
Rebeca S. Scalco Gustavo F. Wandalsen2
Gustavo F. Wandalsen2 Marco van Brussel
Marco van Brussel H. J. Hulzebos
H. J. Hulzebos Simone Dal Corso
Simone Dal Corso Tim Takken
Tim Takken