- 1Department of Internal Medicine, Wayne State University, Detroit, MI, United States
- 2College of Medicine, University of Nebraska Medical Center, Omaha, NE, United States
- 3Touro College of Osteopathic Medicine, Middletown, NY, United States
With more than 54 million cases worldwide, the novel coronavirus disease 2019 (COVID-19) has disrupted every aspect of public life and poses an ever-growing burden on an already strained healthcare system. The emergence of new COVID-19 hot-spots and super-spreader events are placing an immense amount of stress on hospital systems responding to the increased influx of critically ill patients. Healthcare workers and frontline physicians disproportionately bear the additional physical and psychological burdens associated with the appearance of a new hot-spot. However, the mental health implications of COVID-19 for physicians are not well understood. In this perspective piece, we discuss widespread effects of the ongoing pandemic on physician mental health and how blockchain infrastructure can enable digital health technologies in supporting data-driven fatigue mitigation interventions. This is particularly applicable to simplifying physician workflows in newly emerging hot-spots.
1 Introduction
Physician burnout can be defined as a globally prevalent work-associated syndrome involving three domains: Emotional exhaustion, depersonalization and a sense of reduced personal accomplishment (West et al., 2016; West et al., 2018). The incidence rate of burnout associated symptoms that have been linked to adverse effects on patient care and physician health exceeds 50% in studies covering both physicians-in-training and practicing physicians (Dyrbye and Shanafelt, 2011; Shanafelt et al., 2017a). Historically, burnout was thought to be a late-career phenomenon (McCray et al., 2008). However, more recent studies have suggested that younger physicians have twice the risk of work-related stress and that onset of burnout may occur as early as residency training (McCray et al., 2008; Busireddy et al., 2017). More importantly, gender is not an independent predictor of burnout. Adjusting for age, studies have found that female physicians have 40–60% increased odds of fatigue and burnout compared to their male counterparts (Dewa et al., 2014). This problem represents a public health crisis with long-lasting negative impact on individual physicians, patients, and the overall public-health crisis response systems (Dewa et al., 2017).
Physician burnout can lead to severe personal and professional consequences if it remains unaddressed. We can classify the detrimental consequences in two broad categories: physical and psychological (Rothenberger, 2017; Han et al., 2019). The psychological consequences manifest as emotional exhaustion which includes feeling “spent” at the end of a shift, feelings of not having made any significant contributions to patient care, and not having any empathy left to offer to patients from an emotional standpoint (Linzer et al., 2001; Chopra et al., 2004). Depersonalization includes feelings of treating patients as an amalgam of lab values rather than human beings, and becoming more careless in patient care without considering alternatives. The issue of tracking burnout has been complicated by the fact that most physicians refuse to acknowledge their symptoms and refuse to admit that they can be affected by burnout (Shanafelt et al., 2017b; Panagioti et al., 2018). A refusal to seek mental health help has led to a two-fold increased risk of suicidal ideation. Data supports that front-line physicians, during non-pandemic times, are at a far higher risk of suicide (28–40 per 100,000) compared to the general population (12 per 100,000) (Jager et al., 2017; Schwenk and Gold, 2018). On the other hand, the physical toll of the psychological stress manifests often as hypertensive disease and substance abuse disorder (Bianchi et al., 2017; Patel et al., 2018).
A lack of tools for tracking symptoms of severe stress integrated into a physician’s daily workflow, combined with paucity of data on prediction of early burnout signs limit timely interventions. Even though physician burnout has been a systemic problem for a number of years, COVID-19 has magnified the scope within the new hot-spots with an unpredictable influx of patients. As such, data-driven interventions to alleviate stress are integral in order to keep the workforce of a healthcare organization active and alert. Digital health technologies provide a window of opportunity to capture a digital fingerprint that can guide workflow decisions for hospital leadership. In addition, the use of a blockchain can provide a robust pandemic response infrastructure with live-reporting of clinical outcomes and data for epidemiologists from a hot-spot. In order to better understand how blockchain infrastructure can help during the pandemic, we must first understand the major source of stressors for physicians during the pandemic.
2 Lessons Learned From COVID-19 Stressors on Hospital Systems
The COVID-19 pandemic was, and continues to be, uncharted territory for all healthcare workers in the system in a multitude of aspects. All healthcare workers are having to face an unprecedented amount of occupational stress, from having to make critical ethical decisions to worrying about their health of themselves and their families. Some major sources of stress for frontline workers originate from making moral decisions regarding allocation of resources, scarce availability of PPE, self-imposed isolation from family members, and general uncertainty about the capacity of the healthcare system to handle the steadily rising volume of cases. The increase in cases is presenting in two major ways: Waves of new cases rising in major cities, and hot-spots developing in rural or remote areas that are already strained for healthcare resources. It is the development of new hotspots in resource-limited settings that are contributing the most to physician burnout.
Greenberg et al. describes a unique type of pressure coined as “moral injury” elicited by the pandemic which can be characterized as a mental illness in situ, where necessary actions taken for general public health violates one’s own moral compass (Greenberg et al., 2020). The Institute for Health Metrics and Evaluation (IHME) has projected that the demand for mechanical ventilators will overcome supply and that mobilizing the Strategic National Stockpile and overhauling commercial manufacturers will not be adequate to cover the surge of new cases (Institute for Health Metrics and Evaluation (IHME), 2015). The necessary triage and allocation of scarce resources in times of need, such as mechanical ventilators, is a prime example of the “moral injury” healthcare workers are having to face. Many groups, as a result, have proposed ethical guidelines regarding the allocation of mechanical ventilators, such as prioritizing patients who are likely to recover as well as removing patients from ventilators to provide lifesaving resources for patients with more favorable prognosis (Emanuel et al., 2020). Others argue that prioritizing longevity over maximizing lives saved is inherently discriminatory with regards to disability, socioeconomic status, race, and insurance status (Brown and Goodwin, 2020). With such discordance toward a consensus for ethical allocation of scarce resources in dire times in need, the onus is set on the leaders of the healthcare teams to decide, leaving frontline workers exposed to such moral trauma.
Apart from insidious psychological injury, it is being seen in preliminary data from China and Italy that frontline medical workers are already reporting high rates of depression (50.3%), anxiety (44.6%), and insomnia (34.0%) far above the typical historical proportions seen in an already high-risk population (Gold, 2020). Survey from a tertiary infectious disease hospital in China showed incidence of anxiety in 23.04% of staff and post traumatic stress disorder (PTSD) in 27.39% of all workers (Huang et al., 2020). Recent meta-analysis of past viral outbreaks showed that clear institutional communication and access to adequate personal protective equipment (PPE) were associated with reduced morbidity (Kisely et al., 2020). Healthcare workers in the COVID-19 pandemic, in particular, face such a challenge of profound and widespread lack of PPE as well as discordance in reuse policy, seen by varying guidelines from different medical bodies (Godlee, 2020). The combination of such a multitude of factors creates a much greater psychological bearing on today’s frontline healthcare workers. Due to the scarcity of PPE for in-house employees, staff are not only having to worry about covid-19 transmission from patients, but also from coworkers, resulting in chronic anxiety and risk for development of PTSD. Given the circumstances, it is not surprising that PTSD is a primary concern in this population. Santarone et al. describes a need to establish a hierarchy of needs to support healthcare workers’ mental health (Santarone et al., 2020). Specifically speaking, they suggest prioritizing physical wellbeing, followed by psychological needs, and finally the needs of families. Regarding physical wellbeing, availability of PPE is continuously emphasized as a top priority. Simply put, addressing healthcare workers’ physical wellbeing is critical and essential before the discussion of psychological needs can begin to be addressed.
An increasing need for integration of training for healthcare workers regarding monitoring psychosocial needs and giving support to colleagues and patients is made apparent (Pfefferbaum and North, 2020). One hospital in Hunan Province, China responded to the new unparalleled stressors on employees by implementing psychological interventions that allowed staff to temporarily isolate, while providing necessary food and supplies as well as training for identification and response to psychological trauma among a multitude of other institutional policies promoting mental health and counseling. Such measures showed an improvement in staff’s overall mental health and was described as instrumental for better control of infectious diseases (Chen et al., 2020). Specifically in the hot zone of Wuhan, psychological intervention support teams composed of psychiatrists, technical support staff, and mental health hotline volunteers were established with good response from medical workers (Kang et al., 2020). While there is currently no guidance about best practices for preserving mental health of frontline healthcare workers, institution-wide initiatives were seen to improve staff’s trust as well as overall mental outlook.
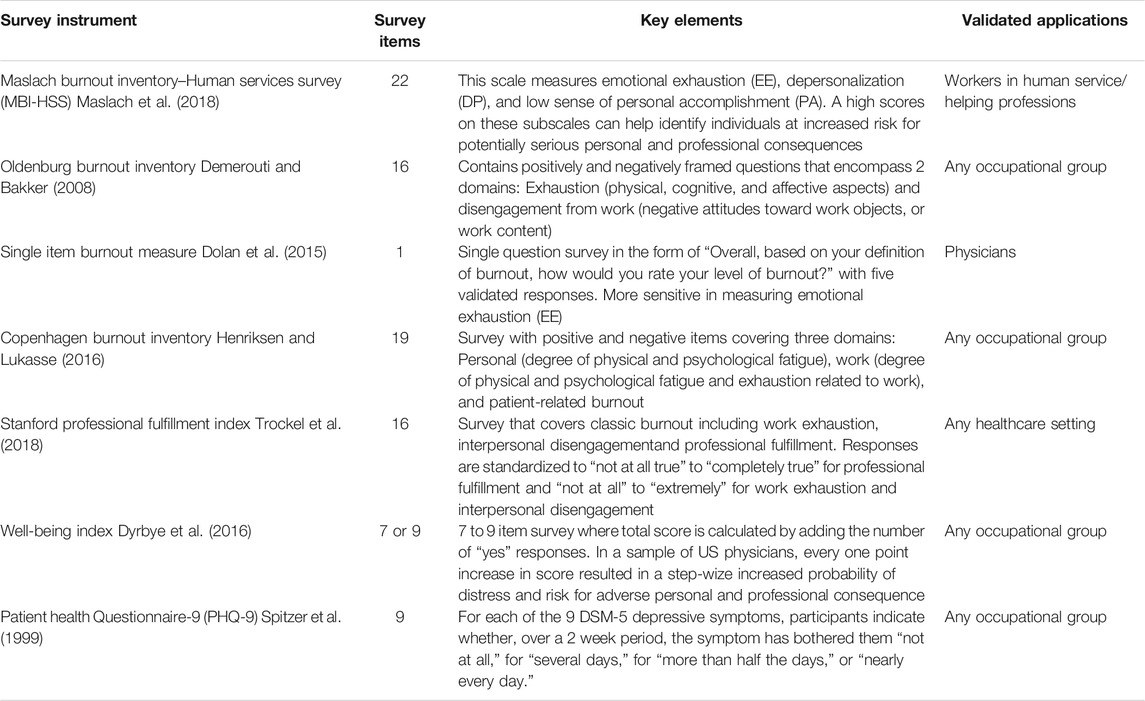
A brief overview of seven most common validated instruments for measuring burnout across multiple industries is reviewed in Table 1 below. Significant challenges exist in active data collection and reporting on fatigue mitigation during a pandemic with any validated instrument (Dyrbye et al., 2009). Traditional methods are less transparent in regards to visibility of raw-data which leads to information silos and the actionable data loses value. Incorporating a blockchain could enforces more transparency via the use of smart contracts that reward for quicker uploads of raw-data and attaches value to the amount of data submitted. A more detailed description of how blockchain can enable burnout tracking is provided in the next section.
3 Blockchain Enabled Healthcare
A blockchain is a decentralized technological construct that enables transactions between two parties without the need for a clearing house or a trusted authority. The first implementation of a blockchain was found embedded in Bitcoin as a solution for providing trustless transactions, however, in recent years, there is a stronger focus on extending the capabilities of blockchain as a technology (Drescher, 2017). This section is a brief review of blockchain technology, various deployment approaches, the risks associated with each, and a model that can work for tracking physician fatigue data. Essentially, a blockchain carries detailed records of transactions embedded in a block, the fundamental unit of value on a blockchain. These records are immutable, and current applications focus on extending this feature to function as an audit log with meta-data appended. A blockchain can be thought of as a series of blocks strung together in a logical and time-wize manner containing detailed histories of each transaction–A digital version of the classic ledger.
Traditionally, a blockchain operates within the context of a broader protocol (called a decentralized ledger protocol) that defines adjustable parameters for a blockchain and the settings unique to an implementation. For a blockchain to be functional, it needs users in two different respects: A set of participants on the network who can assemble transactions into blocks (called miners), and a larger set of users who carry out transactions and grow the blockchain network as a whole. Miners maintain the integrity of the blockchain and are rewarded in return for each block assembled. The order in which blocks can be assembled and transactions included is guided by a consensus algorithm. This algorithm decides how the network as a whole reaches a finality on the order of transactions that every participant will agree upon. Over time, newer implementations of blockchain use different consensus mechanisms, new block structure and reward incentives to scale the blockchain network.
The use of blockchain is nascent in healthcare, however, blockchain based ventures tackling medical health data and records are emerging. Due to the complexity of data and legal nature of healthcare, blockchain implementations will require significant modifications to meet compliance. An important question revolves around data ownership and flow of information in accordance with the Health Insurance Portability and Accountability Act (HIPAA). Fully decentralized systems with complete anonymity of network are not compatible with HIPPA, therefore, more nuanced implementations will be needed (Zhang and Lin, 2018). There are three broad categories:
1. Public: This is an open-blockchain model similar to Bitcoin where anyone can join, become a miner and contribute to creating blocks on the network. In addition, anyone can audit or read ongoing activities on the blockchain network. The main risk of running a public network is that by design, we are unaware of the identity of miners. This works in a transaction-heavy network such as Bitcoin, but will not be compatible with existing healthcare systems or regulations.
2. Private: A private blockchain implementation only allows a select known group of participants to join a blockchain network. These participants are verified by a network operator or a set protocol defined by the network. In this case, only known participants can assemble blocks, collect block rewards and maintain the integrity of a shared ledger. Due to the private nature, the network operators will have disproportionate privileges on the blockchain. In addition, without an element of public verifiability, we run the risk of turning the blockchain implementation into another data-silo where information can be stored but not broadly acted upon.
3. Permissioned: This is a hybrid between public and private blockchain implementations. In this case, blocks contain information or code that can only be executed by parties that have the appropriate access privileges. Anyone can join the network, mine and assemble blocks, however, the smart contracts and chaincode associated with blocks can only be executed on the blockchain by the parties with appropriate permissions. For instance, let us imagine a supply chain implementation using a blockchain to track farm produce that is shipped to customers. The farmer and a customer can sign a smart contract to ensure payment within a certain period of time, and a shipping company can be involved in providing timely updates on tracking uploaded to the blockchain. In this case, a permissioned blockchain would allow the shipping company to provide updates and information on warehouse operations, however, the shipping company cannot see the contract code or any payment details. A public-private interface is being adopted widely by many enterprise-grade applications.
A summary of the three aforementioned implementations is provided below in Table 2 (Zheng et al., 2017).
More recently, consortia blockchain implementations have gained more interest and become mainstream for enterprise and life-science applications. A consortium is a collaborative venture formed by companies in the same vertical with similar interests to share resources and build products in the blockchain space while also protecting their competitive advantage. Sharing domain expertize among member companies allows for a more deliberate approach to a nascent market for new products. These implementations are usually based on permissioned blockchains with a heavier focus on governance and simplified blockchain parameters. The consortium has a clearly defined leading group with inclusionary criteria for bringing on new members, and bylaws that are agreed upon democratically by the members. In a consortia, not every participating member has privileges to mine and assemble a block. The miners or validators are already known, and often sign contracts to be verified, for instance in the case of running nodes containing healthcare information compliant with HIPAA. Voting and governance structures are built into the consortium via a governance board so that any conflicts can be resolved on-chain by participating members. This allows for more transparent decision making and a clear pipeline for decisions that will be implemented on the ledger.
The most striking difference between other blockchain implementations and a consortium blockchain is the consensus mechanism. In a public deployment, there are multiple levels of security embedded into the consensus algorithm so that blocks can be assembled reliably and to maintain network integrity. This allows multiple parties to conduct transactions without the need to identify each other on the blockchain, or a central authority. However, in a consortium, the validators are already known, and therefore, some layers of redundant security can be removed. This results in a significant performance boost and a high transaction throughput.
Shared resources and services in a consortium are crucial for members, particularly in regards to legal and marketing support. Hashed Health is an example of the healthcare consortium described above, moving toward having a complete on-chain governance system. Member companies under the Hashed Health umbrella would be operating on at least 2 blockchains: As a member of a governance blockchain for the consortium, and as a leading group of a permissioned blockchain linked to the member's business model. Members mostly use the governance blockchain to receive technical expertize and essential services from established providers tailored to consortium members. As an example, ProCredEx is a credentialing exchange service under the Hashed Health umbrella that stores and verifies credentialing information (including licensure) for physicians. This exchange can further onboard members such as hospitals or clinics that need credentialing information for employment. The selected data is released and made available to exchange members in a fraction of the time compared to traditional mechanisms.
To track physician wellness data, a healthcare consortium model with a permissioned blockchain implementation will be the most appropriate. This model allows for granular control over sharing the data-points that are uploaded to the blockchain with all interested parties. For instance, biometric data with the ability to predict mood would only be shared between a physician and a therapist, however, a broader assessment of health can be made available to organizations that join the consortium under a HIPAA agreement to tailor interventions. In this manner, interventions in the form of adjunct therapies such as psychotherapy, yoga or meditation classes, gym memberships can be associated with a prior set of data and prospectively look at future improvement. Blockchain acts as a decentralized connector to move data on physician fatigue and track how it is being utilized by various services. Similar to the ProCredEx example, members of this physician wellness exchange can access data and provide timely recommendations.
4 Discussion and Recommendations
A central tenet of blockchain technology is to enable decentralized and secure sharing of verified information among individuals or organizations. Concordantly, it can be paired with an oracle to import accurate external events and cryptographic hashing to de-identify patient information. In that sense, the privacy of users and individuals contributing data can be protected while reporting on live-data. Following are five use-cases where a blockchain can augment existing systems and help reduce physician burnout when a new hot-spot emerges:
Fatigue prediction and mitigation: Digital health devices such as a Fitbit or a tracker with accessible API can be used to track steps during the day, and monitor sleep-cycle patterns through the night (Classen et al., 2018; Liang and Chapa-Martell, 2019). Data generated from such a device can be uploaded into a decentralized storage model (such as IPFS) via a smart contract and utilized by computational models to create a personalized fatigue-scale (Wei, 2014). Once the de-identified data has been registered within decentralized storage, it can be shared responsibly with access permissions through a blockchain (Lee et al., 2019). This can allow epidemiologists and other mental health experts to look at real-time trends and determine the proper time to intervene in a hot-spot as physicians see case surges. This can also help plan for better allocation of duty hours for physicians actively managing COVID patients, and to raise an alert for hospital leadership to consult mental health services in case of dangerously high fatigue trends (Shafagh et al., 2017). Presently, this idea is being applied through an app called Intern + that uses Fitbit-based data to predict fatigue for medical trainees. In a similar fashion, the integration of a blockchain would extend this application to capture real-time data on physician fatigue from a hot-zone.
Color coins: Colored tokens can be instantiated and given to front-line physicians for tracking pandemic-specific health parameters with a slight degree of autonomous response to out of proportion values (Rosenfeld, 2012; Liang et al., 2016). For instance, the colored coins can be tied to a fund established by the hospital leadership to pay for any mental health services needed by the physicians. The token can be liquidated immediately within the hospital network and services rendered without delay, as opposed to the traditional reimbursement model which takes time. Tokenization can allow the consolidation of a digital fingerprint into a profile incorporating fatigue metrics and duty hours. Additionally, using the colored-coin type technology, we can follow up on physician mental health longitudinally, long after the pandemic is over to monitor for development of PTSD. This was seen in front-line physicians working through the SARS, MERS and Ebola epidemics.
Supply chain management: The supply chain for hospitals has been very unreliable during the COVID-19 pandemic, and this has become a major source of added stress and uncertainty. PPE has been consistently running low during case surges, while requisition and redistribution of any incoming PPE has become equally difficult. Over the last few years, blockchain-based supply chain management applications have shown tremendous promise in accurate tracking of supplies. Registering a new hospital to use blockchain-based supply chain can streamline the process of managing essential drugs needed for intubation, ventilators, basic medical supplies, and PPE (Anand et al., 2016; Saberi et al., 2019). Once a supply chain has been set up, a dashboard pulling data from the blockchain can demonstrate the current status of supplies in addition to future incoming orders. This can help further reduce the level of uncertainty about having basic supplies during a case-surge. Emergency supply chains powered by rigorous tracking should be part of an overall pandemic response and blockchain can assist in setting up the infrastructure at a fraction of the cost (Hackius and Petersen, 2017; Blossey et al., 2019; Cole et al., 2019; Queiroz et al., 2019).
Credentialing: For a new physician to start working in a new hospital system, they must first undergo credentialing. The process of credentialing for physicians includes verification and review of licensure, educational history, regulatory history, etc. It can involve contacting more than a dozen entities over several months, and the delay can be detrimental to the facilities needing relief from an influx of patients. This is particularly true for hospitals in remote or rural areas that already suffer from staffing shortages in non-pandemic times. In addition, the physician has to enroll in new payer networks to accept reimbursement through insurance payments and this step can take months. A blockchain-based credentialing system (such as ProCredEx) can maintain verified identities, and any hospital systems in a hot-spot can join this exchange to transfer over the credentials. This can drastically shorten the time-frame needed for credentialing and rapidly activate new physicians for work.
Outpatient visits and telehealth: COVID has made it difficult for patients receiving chronic care to see their primary physicians without the risk of being exposed. In addition, with clinics transitioning to telehealth, billing and care coordination have become more complex to setup. Ultimately, this delay in service due to the transition affects care of the most vulnerable patient populations. Centers for Medicare and Medicaid Services (CMS) has created new incentives to reduce the administrative burden of telehealth visits, however, transitioning to new platforms and workflows come with significant stressors. To help with billing and staffing issues, blockchain companies such as Solve. Care have launched Global Telehealth Exchange, a consortium-type service that provides billing support to member physicians (Chamola et al., 2020). Subsidizing established blockchain platforms like Solve. Care can help new physicians join the consortium at a fraction of the cost, and the members can significantly reduce the administrative overhead. Additionally, using the blockchain can greatly increase the security of billing systems while meeting all compliance standards.
4.1 Informed Consent
A blockchain model that collects sensitive data such as biometric health information needs to be governed by an ethical framework that describes the process of obtaining informed consent of participants, objectives of the study and criteria for meaningful use of the data. Transparency, fairness, and security are the three pillars necessary to establish an ethical baseline during data collection. Informed consent of participants can be recorded on the blockchain via smart contracts (Benchoufi et al., 2017).
The mechanism of setting up a multi-party contract associated with wallet addresses can also be used to record informed consent. In addition, the participants can revoke consent from their end at any point during the study period. Figure 1 visually describes the process of recording and revoking informed consent through a smart contract.
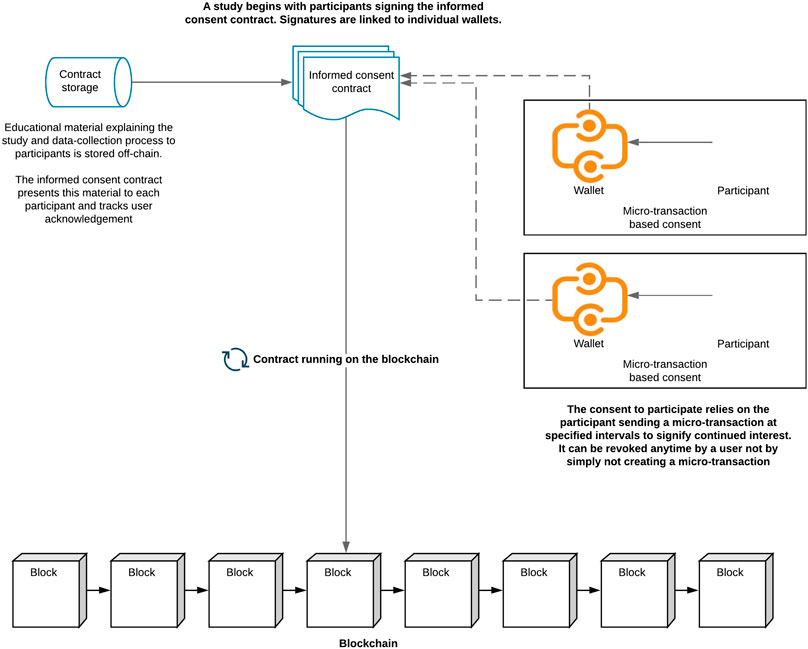
FIGURE 1. Informed consent smart contract constantly updates on the blockchain. Each user consents to the contract via microtransactions that are sent periodically to maintain participation in the study. Revoking consent simply requires no further transaction from the user-wallet.
4.2 Ethical Frameworks for Data Collection and Study Design
The development of ethical frameworks that govern the collection of research and informed consent has been an active area of research. The SATORI EU project (Stakeholders Acting Together On the ethical impact assessment of Research and Innovation) is an example of such collaborative effort that provides broad, actionable policy guidelines for ethical assessment of data collection (Brey et al., 2017). SATORI was a 4 years study that aimed to identify and standardize principles, protocols and best practices for ethical assessment of research proposals and collection of data. In addition, the study identified new areas and provided recommendations where gaps exist, particularly for emerging technologies such as mHealth and privacy in the healthcare space.
Recently, the Digital Medicine Society (DiMe) released a playbook for how to incorporate digital health devices (wearables specifically) into clinical practice, clinical trials and population health surveillance. The core focus on the playbook is providing a practical framework for identification of digital measures that are most meaningful to patients, and how to capture them in meaningful ways from clinical research (Manta et al., 2020). We can use the four-step framework described in the playbook to think about physician burnout:
Meaningful aspect of health: The first step is identification of a disease process (physiological or psychological) that is negatively impacting the quality of life for a patient
Concept of interest: Once a disease process is identified, the second step is to synthesize measurable element(s) or variable(s) from that meaningful aspect of health
Outcome to be measured: The third step is to describe how to measure the variables and track them over time as active interventions are being applied.
Endpoints: Th final step is capturing how the variables that we track respond to interventions that we introduced.
4.3 Blockchain and Internet-of-Things (IoT) Interoperability
A recent study by Slamon et al. (Slamon et al., 2018) studied heart-rate variability using a wearable “smart shirt” in critical care physicians during patient rounds and emergent procedures such as central line insertion. The study had a small sample size of physicians, however, it demonstrated an increase in physiological parameters as a result of working in a high-stress environment. In addition, this study provides a model for biometric variables that will need to be tracked in future when more biometric resources are accessible. Eventually, larger prospective studies will be needed to quantify the long-term physiological impact of such stressors on physician burnout.
A significant barrier in converting actionable data into effective policy is that once a study is completed, the raw data collected from the study remains in solos and loses value. In addition, there are technical limitations in designing studies for scale with multiple devices due to poor device interoperability. Open APIs and standards are helping solve this problem by creating tools that export health data in a reliable manner. For instance, most wearable smart health devices have extensible APIs that allow for event reporting and exporting data in commonly used formats such as JSON. Programmatic access to smart devices turns the blockchain into a serial messaging bus that coordinates biometric summary from multiple devices with smart contracts that can act upon data (Classen et al., 2018). Currently, there are three major blockchain projects focused inter-blockchain communication and IoT interoperability:
1. Polkadot landscape allows for parachains (parallel chains) which are essentially custom blockchains that become part of the global Polkadot mainnet (Wood et al., 2016). A Polkadot Relay Chain becomes a connector between the various parachains and coordinates with the mainchain. Formally, a parachain is a data structure that commonly takes the form of a blockchain and can be verified by validators on Polkadot Relay Chain. The parachains inherit security mechanisms from the relay chain and can communicate with other parachains via the Cross-chain Massage Passing (XCMP) protocol. Each parachain can be created with different characteristics and structure for specific use-cases and applications, but all parachains are required to surrender any native consensus mechanisms to the global Polkadot consensus. Parachains can have a native tokens pegged to the main chain and build off-chain economies relying on the global consensus. The validator set ensures the overall integrity of blocks and transactions generated on a parachain and provide cross-compatibility with the main chain. The parallel nature of parachains allows for rapid transaction processing and overall scalability benefits to mainnet. Parachains are maintained by a collator node that acts as an overseer by retaining all the transactional information, produce new blocks and pass them along to the Relay Chain for inclusion in the mainnet.
2. Cosmos is a major blockchain interoperability effort built on Tendermint protocol where independent blockchains called zones are plugged into the larger Cosmos network. All the zones are connected to the Cosmos Hub and can communicate with each other through secure message passing protocols. Cosmos network uses the Inter Blockchain Communication protocol for inter-chain messaging, and this standardized protocol is also deployed by the central hub. New zones can be added to the network, and inherit the security mechanism from Cosmos mainnet due to the standardized protocol. A major distinguishing factor for Cosmos is that zones maintain their own consensus mechanism due to a sharding consensus scheme.
3. Ark Ecosystem is a collection of blockchains that are connected by a smart bridge to enable interoperability (Zhao et al., 2020; Košič et al., 2018). Any member of the ecosystem can push and deploy a blockchain within the Ark Network with minimal effort and the deployed blockchains would inherit the consensus and security mechanisms from the main-net. SmartBridge is a communication layer between various blockchains, allowing transfer of data and different coins or Ark native currency through the network. If the two blockchains are SmartBrdige compatible, transactions from one chain to another can be used to trigger an event via the Ark wallet (Schulte et al., 2019). Encoded listeners are hubs that listen to SmartBridge transactions to assist in cross-chain communication and watch for triggering events. In exchange for the listening service, the hub gets a portion of the transaction fees as a reward through the SmartBridge. A very ambitious feature in Ark Ecosystem is the use of an application development interface that allows developers to build applications in programming languages familiar to them and currently, Ark supports Python, Ruby, Java and Elixir.
COVID-19 presents a new challenge for everyone in the healthcare space, and it is easy to overlook emotional and psychological well-being as a key contributor to healthcare worker’s efforts toward tackling the pandemic. For the first time in almost a century, healthcare professionals are having to make difficult ethical decisions, predisposing themselves to moral trauma. Even though the use of blockchain in healthcare applications is nascent, this pandemic presents with opportunities to fix technological gaps in our healthcare system. More research funding to formally study the role blockchain-based infrastructure can play in disaster mitigation and alleviating physician burnout during otherwise dire times is warranted and recommended.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
VD conceived of the presented idea. All authors surveyed the literature, discussed the results and contributed to the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Anand, A., McKibbin, M., and Pichel, F. (2016). “Colored coins: Bitcoin, blockchain, and land administration,” in Annual world bank conference on land and poverty, Washington, DC, March 20–24, 2017 (Washington DC: The World Bank).
Benchoufi, M., Porcher, R., and Ravaud, P. (2017). Blockchain protocols in clinical trials: transparency and traceability of consent. F1000Res. 6, 66. doi:10.12688/f1000research.10531.1
Bianchi, R., Schonfeld, I. S., and Laurent, E. (2017). Physician burnout is better conceptualised as depression. Lancet 389 (10077), 1397–1398. doi:10.1016/S0140-6736(17)30897-8
Blossey, G., Eisenhardt, J., and Hahn, G. (2019). “Blockchain technology in supply chain management: an application perspective,” in Proceedings of the 52nd Hawaii international conference on system sciences, Grand Wailea, Maui, Jan 8–11, 2019 (Honlolelu: AISeL), 9.
Brey, P., Shelley-Egan, C., Rodrigues, R., and Jansen, P. (2017). “The ethical assessment of research and innovation–A reflection on the state of the art (based on findings of the SATORI project), in Finding common ground: consensus in research ethics across the social sciences (Advances in Research Ethics and Integrity). Copenhagen: Emerald Publishing Limited, 1, 185–198.
Brown, M. J., and Goodwin, J. (2020). Allocating medical resources in the time of covid-19. N. Engl. J. Med. 382 (22), e79. doi:10.1056/NEJMc2009666
Busireddy, K. R., Miller, J. A., Ellison, K., Ren, V., Qayyum, R., and Panda, M. (2017). Efficacy of interventions to reduce resident physician burnout: a systematic review. J. Grad. Med. Edu. 9 (3), 294–301. doi:10.4300/JGME-D-16-00372.1
Chamola, V., Hassija, V., Gupta, V., and Guizani, M. (2020). A comprehensive review of the COVID-19 pandemic and the role of IoT, drones, AI, blockchain, and 5G in managing its impact. IEEE Access 8, 90225–90265. doi:10.1109/access.2020.2992341
Chen, Q., Liang, M., Li, Y., Wang, L., Fei, D., Jincai, G., et al. (2020). Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiat. 7 (4), e15–e16. doi:10.1016/S2215-0366(20)30078-X
Chopra, S. S., Sotile, W. M., and Sotile, M. O. (2004). STUDENTJAMA. Physician burnout. Jama 291 (5), 633. doi:10.1001/jama.291.5.633
Classen, J., Wegemer, D., Patras, P., Spink, T., and Hollick, M. (2018). Anatomy of a vulnerable fitness tracking system. Proc. ACM Interact. Mob. Wear. Ubiq. Technol. 2 (1), 1–24. doi:10.1145/3191737
Cole, R., Stevenson, M., and Aitken, J. (2019). Blockchain technology: implications for operations and supply chain management. Scm 24 (4), 469–483. doi:10.1108/scm-09-2018-0309
Demerouti, E., and Bakker, A. B. (2008). “The Oldenburg Burnout Inventory: a good alternative to measure burnout and engagement,” in Handbook of stress and burnout in health care. Hauppauge, NY: Nova Science Publishers, 65–78.
Dewa, C. S., Loong, D., Bonato, S., Thanh, N. X., and Jacobs, P. (2014). How does burnout affect physician productivity?. A systematic literature review. BMC Health Serv. Res. 14 (1), 325. doi:10.1186/1472-6963-14-325
Dewa, C. S., Loong, D., Bonato, S., and Trojanowski, L. (2017). The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ open 7 (6), e015141. doi:10.1136/bmjopen-2016-015141
Dolan, E. D., Mohr, D., Lempa, M., Joos, D., Fihn, S. D., Nelson, K. M., et al. (2015). Using a single item to measure burnout in primary care staff: a psychometric evaluation. J. Gen. Intern. Med. 30, 582–587. doi:10.1007/s11606-014-3112-6
Dyrbye, L. N., Satele, D., and Shanafelt, T. (2016). Ability of a 9-item well-being index to identify distress and stratify quality of life in United States workers. J. Occup. Environ. Med. 58, 810–817. doi:10.1097/JOM.0000000000000798
Dyrbye, L. N., and Shanafelt, T. D. (2011). Physician burnout: a potential threat to successful health care reform. Jama 305 (19), 2009–2010. doi:10.1001/jama.2011.652
Dyrbye, L. N., West, C. P., and Shanafelt, T. D. (2009). Defining burnout as a dichotomous variable. J. Gen. Intern. Med. 24, 440. doi:10.1007/s11606-008-0876-6
Emanuel, E. J., Persad, G., Upshur, R., Thome, B., Parker, M., Glickman, A., et al. (2020). Fair allocation of scarce medical resources in the time of covid-19. N. Engl. J. Med. 382 (21), 2049–2055. doi:10.1056/NEJMsb2005114
Gold, J. A. (2020). Covid-19: adverse mental health outcomes for healthcare workers. BMJ 369, m1815. doi:10.1136/bmj.m1815
Greenberg, N., Docherty, M., Gnanapragasam, S., and Wessely, S. (2020). Managing mental Health challenges faced by healthcare workers during covid-19 pandemic. BMJ 368, m1211. doi:10.1136/bmj.m1211
Hackius, N., and Petersen, M. (2017). “Blockchain in logistics and supply chain: trick or treat?. Indigitalization in supply chain management and logistics: smart and digital solutions for an industry 4.0 environment,” in Proceedings of the Hamburg international conference of logistics (HICL), Hamburg, Germany, October, 2017 (Berlin, Germany: epubli GmbH), 23, 3–18.
Han, S., Shanafelt, T. D., Sinsky, C. A., Awad, K. M., Dyrbye, L. N., Fiscus, L. C., et al. (2019). Estimating the attributable cost of physician burnout in the United States. Ann. Intern. Med. 170 (11), 784–790. doi:10.7326/M18-1422
Henriksen, L., and Lukasse, M. (2016). Burnout among Norwegian midwives and the contribution of personal and work-related factors: a cross-sectional study. Sex Reprod. Health. 9, 42–47. doi:10.1016/j.srhc.2016.08.001
Huang, J. Z., Han, M. F., Luo, T. D., Ren, A. K., and Zhou, X. P. (2020). Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 38 (3), 192–195. doi:10.3760/cma.j.cn121094-20200219-00063
Institute for Health Metrics and Evaluation (IHME) (2015). Institute for Health Metrics and Evaluation (IHME). Available at: https://covid19.healthdata.org/projections (Accessed April 6, 2020).
Jager, A. J., Tutty, M. A., and Kao, A. C. (2017). Association between physician burnout and identification with medicine as a calling. Mayo Clin. Proc. 92 (3), 415–422. doi:10.1016/j.mayocp.2016.11.012
Kang, L., Li, Y., Hu, S., Yang, C., Yang, B. X., Wang, Y., et al. (2020). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiat. 7 (3), e14. doi:10.1016/S2215-0366(20)30047-X
Kisely, S., Warren, N., McMahon, L., Dalais, C., Henry, I., and Siskind, D. (2020). Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ 369, m1642. doi:10.1136/bmj.m1642
Košič, K., Černec, R., Barnsley, A., and Thoorens, F. X. (2018). “Building an open-source blockchain ecosystem with ARK,” in OTS 2018 Sodobne informacijske tehnologije in storitve, Storitve, Maribor, June 18–19, 2018 (Slovenia: University Press), 45.
Lee, S. H., Ha, Y., Jung, M., Yang, S., and Kang, W. S. (2019). The effects of a mobile wellness intervention with Fitbit use and goal setting for workers. Telemed. J. E Health 25 (11), 1115–1122. doi:10.1089/tmj.2018.0185
Liang, Z., and Chapa-Martell, M. A. (2019). “Combining resampling and machine learning to improve sleep-wake detection of Fitbit wristbands,” in 2019. IEEE international conference on healthcare informatics (ICHI), Xi'an, China, June 10–13, 2019 (Tokyo: IEEE), 1–3.
Liang, Z., Ploderer, B., Martell, M. A. C., and Nishimura, T. (2016). “A cloud-based intelligent computing system for contextual exploration on personal sleep-tracking data using association rule mining,” in ISICS 2016. Communications in Computer and information science. Cham, Switzerland: Springer, 83–96.
Linzer, M., Visser, M. R., Oort, F. J., Smets, E. M., McMurray, J. E., and De Haes, H. C. (2001). Predicting and preventing physician burnout: results from the United States and Netherlands. Am. J. Med. 111 (2), 170–175. doi:10.1016/s0002-9343(01)00814-2
Manta, C., Patrick-Lake, B., and Goldsack, J. C. (2020). Digital measures that matter to patients: a framework to guide the selection and development of digital measures of health. Digit Biomark 4 (3), 69–77. doi:10.1159/000509725
Maslach, C., Jackson, S. E., and Leiter, M. P. (2018). Maslach burnout inventory manual 4th Edn. Menlo Park, CA: Mind Garden, Inc.
McCray, L. W., Cronholm, P. F., Bogner, H. R., Gallo, J. J., and Neill, R. A. (2008). Resident physician burnout: is there hope? Fam. Med. 40 (9), 626.
Panagioti, M., Geraghty, K., Johnson, J., Zhou, A., Panagopoulou, E., Chew-Graham, C., et al. (2018). Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern. Med. 178 (10), 1317–1331. doi:10.1001/jamainternmed.2018.3713
Patel, R., Bachu, R., Adikey, A., Malik, M., and Shah, M. (2018). Factors related to physician burnout and its consequences: a review. Behav. Sci. 8 (11), 98. doi:10.3390/bs8110098
Pfefferbaum, B., and North, C. S. (2020). Mental health and the covid-19 pandemic. N. Engl. J. Med. 383, 510. doi:10.1056/NEJMp2008017
Queiroz, M. M., Telles, R., and Bonilla, S. H. (2019). Blockchain and supply chain management integration: a systematic review of the literature. Supply Chain Manag.: Int. J. 25, 241–254. doi:10.1108/SCM-03-2018-0143
Rothenberger, D. A. (2017). Physician burnout and well-being: a systematic review and framework for action. Dis. Colon Rectum 60 (6), 567–576. doi:10.1097/dcr.0000000000000844
Saberi, S., Kouhizadeh, M., Sarkis, J., and Shen, L. (2019). Blockchain technology and its relationships to sustainable supply chain management. Int. J. Prod. Res. 57 (7), 2117–2135. doi:10.1080/00207543.2018.1533261
Santarone, K., McKenney, M., and Elkbuli, A. (2020). Preserving mental health and resilience in frontline healthcare workers during COVID-1. Am. J. Emerg. Med. 38 (7), 1530–1531. doi:10.1016/j.ajem.2020.04.030
Schulte, S., Sigwart, M., Frauenthaler, P., and Borkowski, M. (2019). “Towards blockchain interoperability,” in International conference on business process management: blockchain and central and eastern europe forum. Cham, Switzerland: Springer, 3–10.
Schwenk, T. L., and Gold, K. J. (2018). Physician burnout-A serious symptom, but of what? Jama 320 (11), 1109–1110. doi:10.1001/jama.2018.11703
Shafagh, H., Burkhalter, L., Hithnawi, A., and Duquennoy, S. (2017). “Towards blockchain-based auditable storage and sharing of iot data,” in Proceedings of the on Cloud Computing Security Workshop, Dallas Texas, November 3, 2017 (New York, NY: Association for Computing Machinery), 45–50.
Shanafelt, T., Goh, J., and Sinsky, C. (2017a). The business case for investing in physician well-being. JAMA Intern. Med. 177 (12), 1826–1832. doi:10.1001/jamainternmed.2017.4340
Shanafelt, T. D., Dyrbye, L. N., and West, C. P. (2017b). Addressing physician burnout: the way forward. Jama 317 (9), 901–902. doi:10.1001/jama.2017.0076
Slamon, N. B., Penfil, S. H., Nadkarni, V. M., and Parker, R. M. (2018). A prospective pilot study of the biometrics of critical care practitioners during live patient care using a wearable “Smart Shirt”. J. Intens. Crit. Care 4 (2), 10. doi:10.21767/2471-8505.100112
Spitzer, R. L., Kroenke, K., and Williams, J. B. (1999). Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. J. Am. Med. Assoc. 282 (18), 1737–1744. doi:10.1001/jama.282.18.1737
Trockel, M., Bohman, B., Lesure, E., Hamidi, M. S., Welle, D., Roberts, L., et al. (2018). A brief instrument to assess both burnout and professional fulfillment in physicians: reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Acad. Psychiatr. 42 (1), 11–24. doi:10.1007/s40596-017-0849-3
Wei, J. (2014). How wearables intersect with the cloud and the internet of things : considerations for the developers of wearables. IEEE Consum. Electron. Mag. 3 (3), 53–56. doi:10.1109/mce.2014.2317895
West, C. P., Dyrbye, L. N., Erwin, P. J., and Shanafelt, T. D. (2016). Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 388 (10057), 2272–2281. doi:10.1016/S0140-6736(16)31279-X
West, C. P., Dyrbye, L. N., and Shanafelt, T. D. (2018). Physician burnout: contributors, consequences and solutions. J. Intern. Med. 283 (6), 516–529. doi:10.1111/joim.12752
Zhang, A., and Lin, X. (2018). Towards secure and privacy-preserving data sharing in e-health systems via consortium blockchain. J. Med. Syst. 42 (8), 140. doi:10.1007/s10916-018-0995-5
Zhao, D. (2020). “Cross-blockchain transactions,” in Conference on innovative data systems research, Amsterdam, Netherlands, January 12–15, 2020 (CIDR).
Keywords: COVID- 19, blockchain, burnout –professional, physician, moral injury
Citation: Dhillon V, Xu T and Parikh C (2021) Blockchain Enabled Tracking of Physician Burnout and Stressors During the COVID-19 Pandemic. Front. Blockchain 3:586742. doi: 10.3389/fbloc.2020.586742
Received: 24 July 2020; Accepted: 21 December 2020;
Published: 18 February 2021.
Edited by:
Jane Thomason, University College London, United KingdomReviewed by:
Valentine Joseph Gandhi Bavanirajan, USAID/Indonesia and The Development CAFE, IndonesiaAriana Fowler, Independent Researcher, New York City, NY, United States
Copyright © 2021 Dhillon, Xu and Parikh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vikram Dhillon, dmRoaWxsb25AbWVkLndheW5lLmVkdQ==
 Vikram Dhillon
Vikram Dhillon Tailong Xu
Tailong Xu Chirag Parikh
Chirag Parikh