Abstract
The purpose of the meta-analysis of randomized trials was to analyze the significance of ethnicity on the effect of sodium reduction (SR) on blood pressure (BP) by estimating the effect of SR on BP in Asians, Blacks and Whites under conditions, which were adjusted with respect to baseline BP, baseline sodium intake and quantity of SR. Relevant studies were retrieved from a pool of 167 RCTs published in the period 1973–2010 and identified in a previous Cochrane review. 9 Asian, 9 Black, and 74 White populations standardized with respect to the range of baseline blood pressure, the range of baseline sodium, duration of SR (at least 7 days) and baseline sodium intake (at maximum 250 mmol) intake were included. In the cross-sectional analysis, there was no difference in change in SBP to SR between the ethnic groups, but there was a small difference in SR induced change in DBP between Blacks and Whites (p = 0.04). The comparison of changes in SBP and DBP to SR in ethnic groups compared in identical studies showed no statistically significant differences between the groups.
Introduction
The effect of sodium reduction (SR) on blood pressure (BP) is smaller in persons with normal blood pressure than in hypertensive persons (Graudal et al., 1998, 2011). A recent dose-response analysis showed a dose-response relationship between SR and effect on BP in study populations with a mean BP above 130/80 mmHg, but not in study populations with a mean BP below 130/80 mmHg, unless SR was applied on study populations with an extreme sodium intake above about 6 g sodium (14.5 g salt) (Graudal et al., 2015). These findings indicate that the effect of SR depends on the baseline blood pressure, the baseline sodium intake and the quantity of SR. Hypothetically, the duration of SR could also be an important determinant of the effect of SR on BP, but a detailed analysis of 15 longitudinal RCTs, which investigated participants repeatedly during up to 6 weeks, showed that the effect of SR on BP was similar during the observation period from 1 to 6 weeks indicating that the duration of SR beyond 1 week does not influence the effect of SR on BP (Graudal et al., 2015).
Our previous meta-analysis showed that the effect of SR on SBP was higher in Asian hypertensive persons (10.2 mmHg) than in White (5.5 mmHg) and Black hypertensive persons (6.4 mmHg) (Graudal et al., 1998). Furthermore the effect of SR on SBP was higher in Black persons with a normal blood pressure (4.0 mmHg) than in Asian (1.3 mmHg) and White persons with a normal BP (1.3 mmHg) (Graudal et al., 1998). However, a subsequent analysis of Blacks showed that the difference between Blacks and Whites was small, if studies investigating extreme sodium reductions were eliminated (Graudal and Alderman, 2014). The reason for ethnic differences are not defined and could be due to different baseline blood pressures, sodium intakes and doses of SR or other confounders, rather than genetic differences.
The purpose of the present supplementary analysis of our previous meta-analysis of randomized trials (Graudal et al., 2011) was to analyze the significance of ethnicity on the effect of SR on BP by estimating the effect of SR on BP in Asians, Blacks and Whites under conditions, which were adjusted with respect to baseline BP, baseline sodium intake and quantity of SR.
Material
Relevant studies were retrieved from a pool of 167 RCTs published in the period 1973–2010 and identified in a Cochrane review in 2011 (Graudal et al., 2011). Search methods for identification of these 167 studies are previously described in detail (Graudal et al., 2011).
Methods
Eligibility criteria
Trials randomizing participants to two different sodium intakes were included provided that the sodium intake was measured as 24-h urinary excretion (Graudal et al., 2011). Baseline BP was used to define the study groups to ensure that the baseline BP was similar across the three ethnic study groups. The most extreme sodium intake in the world's populations is about 6 g sodium (14.5 g salt) (McCarron et al., 2013; Powles et al., 2013), corresponding to about 250 mmol, and we therefore excluded studies with sodium intakes above this level, as such intakes reflected an experimental situation rather than a population norm. In a series of longitudinal RCTs we have showed that the effect of SR on BP is at maximum after 1 week (Graudal et al., 2015). As we do not know whether this effect is reached before 1 week, we excluded studies with a shorter duration than 1 week.
In order to avoid excluding the relatively few studies, which have been performed in Blacks and Asians, the baseline systolic BP (SBP) range of these study groups were used to define the baseline SBP range of the white comparator study groups.
Bias
The following factors were analyzed across the defined ethnic groups to evaluate the comparability of the groups: Age, baseline SBP, baseline diastolic BP (DBP), baseline sodium intake and the quantity of sodium reduction.
Statistical analysis
In this re-analysis featuring improved control for blood pressure and the extent of salt intake and salt reduction the individual study data were integrated in meta-analyses separately for Asians, Blacks, and Whites, and the integrated summary data for each of the groups were then compared versus each other. As well the separate meta-analyses as the comparisons of the summary data for each ethnic group were performed by means of the inverse variance method (continuous data) in Review Manager (RevMan) [Computer program], version 5.1. Copenhagen: The Nordic Cochrane Centre, the Cochrane Collaboration, 2008.
A supplementary meta-regression analysis of Ethnicity versus effect on blood pressure (separate analyses for SBP and DBP) adjusted for amount of sodium reduction, baseline blood pressure (SBP and DBP), age, and the duration of the sodium reduction intervention was performed by means of the multiple regression analysis package in Statview 5.0.
Results
Study selection
The study groups were defined from 167 references (Graudal et al., 2011). Some references reported separate data on sodium sensitive and sodium resistant participants. These were integrated before inclusion in the meta-analysis. Some references included separate analyses on hypertensive and normotensive persons or on different ethnic groups. These were included as separate data. The total number of study groups in the 167 references (Graudal et al., 2011) was 184. 16 study groups of mixed ethnic populations were excluded. Two Black populations with duration of sodium reduction less than 7 days were excluded. As it was the objective to match studies for each ethnic group according to range of SBP, all Asian and Black populations were ranked with respect to baseline SBP. Ten Asian study populations had a mean baseline SBP in the range 113–158 mm Hg and 12 Black populations had mean baseline SBP in the range of 108–156 mmHg. We excluded the one study with the lowest baseline SBP of 108 mmHg, as this was outside the 113–158 range defined by the Asian populations. In this study SBP raised 0.5 mmHg when sodium intake was reduced. The remaining 11 studies had a baseline SBP range of 113–156 mmHg and thus were comparable to the Asian population concerning this range. As SBP in the 144 studies of white populations varied in the range of 105–179 mmHg, 15 with baseline SBP above 158 mmhg and 18 with a baseline SBP in the range of 105–112 mmHg were excluded. Five white study populations with no information on baseline SBP were also excluded, leaving 106 study populations with a baseline SBP in the range of 113–158. Then 1 study of Asians, 2 studies of blacks and 21 studies of whites with a high sodium intake above 250 mmol and 11 white populations with duration of SR less than 7 days were excluded. Thus, 9 Asian populations (6 references, Table 1), 9 black populations (7 references, Table 1) and 74 white populations (70 references, Table 1) standardized with respect to the range of baseline blood pressure, duration of SR (at least 7 days) and baseline sodium intake (at maximum 250 mmol) were included.
Table 1
| Eth. | Authors | Dur. | BP | N | Age | HS | LS | B SBP | B DBP | E SBP | SSE | E DBP | DSE | References |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | Ishimitsu | 7 | N | 7 | 53 | 217 | 22 | 116 | 77 | −2.0 | 4.3 | −2.0 | 3.6 | Clin. Sci. 1996; 91, 293–298. |
| A | Ishimitsu | 7 | H | 23 | 55 | 217 | 24 | 157 | 95 | −15.7 | 6.0 | −5.5 | 3.2 | Clin. Sci. 1996; 91, 293–298. |
| A | Uzu | 7 | H | 70 | 51 | 204 | 31 | 154 | 94 | −15.6 | 7.4 | −5.0 | 3.1 | AJH 1999; 12, 35–39. |
| A | Suzuki | 7 | H | 20 | 59 | 167 | 51 | 157 | 92 | −4.0 | 2.0 | −2.6 | 1.3 | Hypertension 2000; 35, 864–868. |
| A | Nakamura | 42 | N | 38 | 47 | 240 | 216 | 113 | 66 | 2.0 | 2.0 | −5.5 | 3.0 | Circ. J. 2003;67, 530–534. |
| A | Nakamura | 42 | TH | 26 | 47 | 240 | 216 | 140 | 90 | −5.8 | 4.9 | −1.3 | 3.3 | Circ. J. 2003;67, 530–534. |
| A | Takahashi | 365 | N | 341 | 56 | 248 | 209 | 123 | 74 | −2.3 | 1.2 | −1.2 | 1.0 | J. Hypertens. 2006; 24, 451–8. |
| A | Takahashi | 365 | TH | 107 | 56 | 248 | 209 | 143 | 83 | −5.2 | 2.4 | 0.1 | 1.7 | J. Hypertens. 2006; 24, 451–458. |
| A | He | 42 | H | 29 | 47 | 176 | 108 | 142 | 92 | −5.4 | 1.9 | −2.2 | 1.0 | Hypertension 2009; 54, 482–488. |
| B | Dubbert | 90 | TH | 67 | 61 | 194 | 160 | 138 | 86 | −1.4 | 3.8 | −0.5 | 1.7 | Behav. Ther. 1995; 26, 721–732. |
| B | Sacks | 30 | N | 68 | 48 | 141 | 64 | 129 | 84 | −6.4 | 1.2 | −4.0 | 0.8 | NEJM 2001; 344, 3–10. |
| B | Sacks | 30 | H | 46 | 48 | 141 | 64 | 143 | 89 | −8.6 | 1.2 | −5.3 | 0.8 | NEJM 2001;344:3-10. |
| B | Appel | 105 | TH | 142 | 66 | 145 | 116 | 128 | 71 | −5.0 | 1.7 | −2.9 | 1.2 | Arch. IM 2001; 161, 685–693. |
| B | Palacios | 21 | N | 15 | 12 | 109 | 35 | 113 | 59 | 3.4 | 1.5 | −0.1 | 1.9 | JCEM 2004; 89, 1858–1863. |
| B | Forrester (Ni) | 21 | N | 58 | 47 | 127 | 53 | 115 | 73 | −4.8 | 1.5 | −3.2 | 1.0 | J. Hum. Hypertens. 2005; 19, 55–60. |
| B | Forrester (Ja) | 21 | N | 56 | 41 | 155 | 68 | 126 | 76 | −5.1 | 1.5 | −2.2 | 1.5 | J. Hum. Hypertens. 2005; 19, 55–60. |
| B | Swift | 28 | H | 40 | 50 | 167 | 89 | 156 | 100 | −8.0 | 2.1 | −3.0 | 1.1 | Hypertension 2005; 46, 308–312. |
| B | He | 42 | H | 69 | 50 | 165 | 121 | 149 | 90 | −4.8 | 1.2 | −2.2 | 0.7 | Hypertension 2009; 54, 482–488. |
| W | Skrabal | 14 | N | 20 | 23 | 200 | 50 | 125 | 73 | −2.7 | 2.1 | −3.0 | 1.5 | Lancet 1981; II, 895–900. |
| W | Ambrosioni | 42 | H | 25 | 23 | 120 | 60 | 130 | 75 | −2.2 | 1.6 | −0.4 | 1.2 | Hypertension 1982; 4, 789–794. |
| W | Beard | 84 | TH | 90 | 49 | 161 | 37 | 141 | 87 | −5.2 | 4.9 | −3.4 | 2.9 | Lancet. 1982; II, 455–458. |
| W | Puska | 72 | N | 38 | 40 | 167 | 77 | 131 | 82 | −1.5 | 4.5 | −2.1 | 2.8 | Lancet 1983; I, 1–5. |
| W | Puska H | 72 | H | 34 | 40 | 167 | 77 | 147 | 98 | 1.8 | 5.6 | 0.5 | 3.1 | Lancet 1983; I, 1–5. |
| W | Watt | 28 | H | 18 | 52 | 143 | 87 | 150 | 91 | −0.5 | 1.5 | −0.3 | 0.8 | BMJ 1983; 286, 432–6. |
| W | Skrabal | 14 | N | 52 | 23 | 194 | 38 | 121 | 64 | −3.1 | 4.4 | −1.9 | 2.6 | Hypertension 1984; 6, 152–158. |
| W | Fagerberg | 63 | H | 30 | 51 | 195 | 96 | 149 | 98 | −3.7 | 7.1 | −3.1 | 4.1 | BMJ 1984; 288, 11–14. |
| W | Maxwell | 84 | H | 30 | 47 | 200 | 39 | 148 | 98 | −2.0 | 6.7 | 2.0 | 3.8 | Arch. IM 1984; 144, 1581–1584. |
| W | Richards | 28 | H | 12 | 36 | 180 | 80 | 137 | 86 | −4.0 | 2.8 | −3.0 | 2.3 | Lancet 1984; I, 757–761. |
| W | Tuthill | 56 | N | 191 | 16 | 126 | 65 | 113 | 70 | 0.0 | 1.1 | 0.0 | 1.3 | Tox. Ind. Health 1985; 1, 35–43. |
| W | Skrabal | 14 | N | 62 | 23 | 194 | 40 | 120 | 64 | −3.1 | 2.2 | −1.5 | 0.9 | SJCLI 1985; 176(S), 47–57. |
| W | Teow | 14 | N | 9 | 25 | 240 | 40 | 114 | 66 | −0.6 | 1.2 | −2.7 | 1.4 | Clin. Exp. Hypertens. 1986; A7, 1681–1695. |
| W | ANHMRC | 84 | H | 100 | 53 | 150 | 80 | 150 | 94 | −4.8 | 3.9 | −4.2 | 1.9 | J. Hypertens. Suppl. 1986; 4, S629-S637. |
| W | Fuchs | 9 | N | 17 | 20 | 241 | 12 | 117 | 57 | −3.6 | 2.2 | 1.9 | 1.0 | Braz. J. Med. Biol. Res. 1987; 20, 25–34. |
| W | Morgan | 60 | TH | 20 | 61 | 135 | 78 | 143 | 82 | −6.0 | 9.0 | −4.0 | 4.3 | Lancet 1987; I, 227–230. |
| W | Grobee | 42 | H | 40 | 24 | 129 | 57 | 143 | 78 | −0.8 | 1.5 | −0.8 | 1.4 | BMJ 1987; 293, 27–29. |
| W | McGregor | 30 | TH | 15 | 52 | 183 | 83 | 150 | 97 | −13.0 | 3.3 | −9.0 | 3.1 | BMJ 1987; 294, 531–534. |
| W | Morgan | 14 | H | 8 | 63 | 135 | 68 | 149 | 96 | −7.0 | 3.0 | −6.0 | 3.0 | J. Hypertens. 1988; 6(Suppl. 4), S652–S654. |
| W | Sudhir | 12 | N | 6 | 35 | 163 | 29 | 129 | 81 | −7.9 | 3.4 | −5.0 | 2.1 | Clin. Sci. 1989; 77, 605–610. |
| W | Hargreaves | 14 | N | 8 | 23 | 155 | 49 | 129 | 66 | −6.0 | 2.2 | −3.0 | 2.0 | Clin. Sci. 1989; 76, 553–557. |
| W | ANHMRC | 48 | H | 103 | 58 | 153 | 90 | 154 | 95 | −5.5 | 1.5 | −2.8 | 0.8 | Lancet 1989; 1, 399–402. |
| W | Schmid | 7 | N | 9 | 32 | 210 | 20 | 125 | 75 | −3.0 | 1.9 | 3.0 | 1.6 | J. Hypertens. 1990; 8, 277–283. |
| W | Schmid H | 7 | H | 9 | 36 | 210 | 29 | 147 | 93 | −6.0 | 3.1 | −1.9 | 2.1 | J. Hypertens. 1990; 8, 277–283. |
| W | Sharma | 7 | N | 40 | 25 | 239 | 25 | 113 | 71 | −2.1 | 1.1 | −3.1 | 1.0 | Hypertension 1990; 16, 407–413. |
| W | Friberg | 13 | N | 10 | 33 | 152 | 35 | 114 | 69 | 0.0 | 2.0 | −1.0 | 2.0 | Hypertension 1990; 16, 121–130. |
| W | Del Rio | 14 | H | 15 | 49 | 190 | 90 | 149 | 94 | −3.4 | 2.0 | −1.1 | 1.8 | Rev. Clin. Esp. 1990; 186, 5–10. |
| W | Parker | 28 | TH | 59 | 52 | 142 | 69 | 138 | 85 | 1.3 | 2.2 | 0.6 | 0.9 | Hypertension 1990; 16, 398–406. |
| W | Howe | 28 | N | 90 | 13 | 179 | 98 | 115 | 60 | −1.0 | 0.7 | −0.6 | 0.7 | J. Hypertens. 1991; 9, 181–186. |
| W | Mascioli | 28 | N | 48 | 52 | 179 | 109 | 131 | 84 | −3.6 | 0.9 | −2.3 | 0.8 | Hypertension 1991; 17(Suppl. 1), I21–I26. |
| W | Egan H | 7 | H | 18 | 35 | 214 | 20 | 124 | 78 | −2.7 | 5.5 | −1.7 | 3.5 | AJH 1991; 4, 416–421. |
| W | Gow | 7 | N | 9 | 0 | 111 | 17 | 120 | 68 | −8.0 | 1.6 | −3.0 | 2.2 | EJCP 1992; 43, 635–638. |
| W | Cobiac | 28 | N | 106 | 67 | 148 | 75 | 132 | 77 | −2.8 | 1.6 | −1.0 | 1.8 | J. Hypertens 1992; 10, 87–92. |
| W | Benetos | 28 | H | 20 | 42 | 163 | 85 | 149 | 93 | −6.5 | 1.9 | −3.7 | 1.3 | J. Hypertens, 1992; 10, 355–360. |
| W | Sciarrone | 56 | TH | 91 | 54 | 134 | 52 | 136 | 83 | −5.8 | 4.1 | −0.4 | 2.3 | J. Hypertens 1992; 10, 287–298. |
| W | Nestel | 42 | N | 66 | 66 | 157 | 91 | 125 | 73 | −3.2 | 2.7 | −1.4 | 2.0 | J. Hypertens 1993; 11, 1387–1394. |
| W | Del Rio | 14 | H | 30 | 49 | 199 | 48 | 156 | 96 | −1.4 | 1.8 | −0.5 | 1.3 | JIM 1993; 233, 409–414. |
| W | Zoccali | 7 | H | 15 | 45 | 217 | 54 | 144 | 92 | −14.0 | 2.5 | −8.0 | 1.4 | J. Hypertens. 1994; 12, 1249–1253. |
| W | Jula | 365 | H | 76 | 44 | 166 | 109 | 147 | 97 | −6.7 | 3.9 | −3.8 | 1.7 | Circulation 1994; 89, 1023–1031. |
| W | Howe | 42 | TH | 56 | 55 | 158 | 78 | 145 | 81 | −4.2 | 2.9 | −1.5 | 1.9 | J. Hum. Hyp. 1994; 8, 43–49. |
| W | Miller | 14 | N | 36 | 23 | 191 | 133 | 118 | 62 | 1.9 | 1.6 | −0.1 | 1.5 | Psychosom. Med. 1995; 57, 381–389. |
| W | Fliser | 7 | N | 7 | 26 | 203 | 23 | 114 | 71 | −1.1 | 2.9 | −0.7 | 1.8 | EJCI 1995; 25, 39–43. |
| W | Arrol | 182 | TH | 181 | 55 | 122 | 106 | 145 | 89 | −0.4 | 3.4 | −1.2 | 2.1 | NZ Med. J. 1995; 108, 266–268. |
| W | Dubbert | 90 | TH | 55 | 63 | 200 | 145 | 148 | 85 | −1.4 | 3.8 | −0.5 | 1.7 | Behav. Ther. 1995; 26, 721–732. |
| W | Grey | 7 | N | 34 | 23 | 185 | 52 | 116 | 70 | 1.0 | 1.2 | 1.0 | 0.9 | AJH 1996; 9, 317–322. |
| W | Feldman H | 7 | H | 8 | 27 | 182 | 6 | 126 | 79 | 2.6 | 2.9 | 1.6 | 1.8 | CPT 1996; 60, 444–451. |
| W | Schorr | 28 | N | 16 | 64 | 166 | 105 | 140 | 84 | −1.0 | 2.7 | 0.0 | 1.7 | J. Hypertens 1996; 14, 131–135. |
| W | Cappucio | 30 | N | 18 | 67 | 167 | 91 | 149 | 85 | −8.1 | 2.8 | −3.9 | 1.5 | Lancet 1997; 350, 850–854. |
| W | van Buul | 196 | N | 232 | 28 | 140 | 75 | 122 | 71 | 0.0 | 1.8 | 0.0 | 1.2 | Hyp. Preg. 1997; 16, 335–346. |
| W | Meland | 56 | H | 16 | 50 | 191 | 125 | 146 | 95 | −4.0 | 2.5 | −3.0 | 1.4 | SJCLI 1997; 57, 501–506. |
| W | Feldman | 7 | N | 8 | 33 | 207 | 48 | 130 | 82 | 0.0 | 5.5 | 0.0 | 3.6 | AJH 1999; 12, 643–647. |
| W | Barba | 7 | N | 7 | 32 | 177 | 23 | 118 | 74 | −3.2 | 5.5 | −2.1 | 3.5 | J. Hypertens. 2000; 18, 615–621. |
| W | Sacks | 30 | N | 54 | 49 | 141 | 64 | 129 | 84 | −4.0 | 1.2 | −1.4 | 0.8 | NEJM 2001; 344, 3–10. AIM 2001; 135, 1019–1028. |
| W | Sacks H | 30 | H | 37 | 49 | 141 | 64 | 143 | 89 | −6.6 | 1.2 | −2.7 | 0.8 | NEJM 2001; 344, 3-10. AIM 2001; 135, 1019–1028. |
| W | Seals | 90 | H | 35 | 64 | 132 | 86 | 143 | 78 | −8.0 | 2.6 | −2.0 | 1.7 | J. Am. Coll. Cardiol. 2001; 38, 506–513. |
| W | Appel TH | 105 | TH | 471 | 66 | 145 | 105 | 128 | 71 | −4.0 | 1.0 | −1.6 | 0.7 | Arch. IM 2001; 161, 685–693. |
| W | Johnson | 14 | H | 40 | 69 | 185 | 112 | 150 | 83 | −4.5 | 2.1 | −0.6 | 1.5 | J. Hypertens. 2001; 19, 1053–1060. |
| W | Manunta | 14 | H | 20 | 48 | 177 | 67 | 152 | 99 | −5.2 | 2.0 | −3.3 | 2.0 | Hypertension 2001; 38, 198–203. |
| W | Kleij | 7 | N | 27 | 24 | 236 | 50 | 119 | 74 | 0.2 | 3.3 | 0.1 | 2.1 | JASN 2002; 13, 1025–1033. |
| W | Kerstens | 7 | N | 28 | 23 | 248 | 42 | 115 | 72 | 3.1 | 2.0 | 2.0 | 1.3 | JCEM 2003; 88, 4180–4185. |
| W | Nowson | 28 | N | 92 | 45 | 139 | 51 | 123 | 75 | −0.7 | 0.8 | 0.0 | 0.6 | J. Nutr. 2003; 133, 4118–4123. |
| W | Palacios | 21 | N | 8 | 13 | 120 | 34 | 113 | 55 | −0.1 | 1.5 | 4.2 | 1.7 | JCEM 2004; 89, 1858–1863. |
| W | Gates | 28 | H | 12 | 64 | 155 | 60 | 140 | 84 | −3.0 | 1.8 | −1.2 | 1.5 | Hypertension 2004; 44, 35–41 |
| W | Damgaard | 7 | N | 12 | 57 | 188 | 59 | 124 | 77 | 0.0 | 4.7 | 0.0 | 3.0 | AJP RICP 2006; 290, R1294–R1301. |
| W | Melander | 28 | M | 39 | 53 | 140 | 51 | 144 | 91 | −6.0 | 1.2 | −2.3 | 0.9 | J. Hypertens. 2007; 25, 619–627. |
| W | Dengel | 8 | H | 28 | 63 | 191 | 36 | 152 | 79 | −10.0 | 3.6 | −4.0 | 3.6 | Physiol. Res. 2007; 56, 393–401. |
| W | Jessani | 7 | N | 184 | 50 | 138 | 57 | 122 | 79 | −1.0 | 0.8 | −1.0 | 0.8 | AJH 2008; 21: 1238–1244. |
| W | Dickinson | 14 | N | 29 | 53 | 156 | 64 | 116 | 73 | −5.0 | 1.5 | −1.0 | 1.1 | AJCN 2009; 89, 485–490. |
| W | He | 42 | H | 71 | 52 | 165 | 110 | 146 | 90 | −4.8 | 1.2 | −2.2 | 0.7 | Hypertension 2009; 54, 482–488. |
| W | Meland | 56 | H | 46 | 56 | 126 | 83 | 156 | 93 | −5.0 | 3.8 | −5.0 | 1.4 | SJPHC 2009; 27, 97–103. |
| W | Nowson TH | 98 | TH | 35 | 59 | 113 | 69 | 130 | 80 | −5.5 | 2.7 | −3.6 | 1.6 | Nutr. Res. 2009; 29, 8–18. |
| W | Nowson | 98 | N | 59 | 59 | 113 | 69 | 131 | 81 | −1.1 | 2.0 | 0.3 | 1.5 | Nutr. Res. 2009; 29, 8–18. |
| W | Weir | 28 | H | 132 | 52 | 208 | 85 | 139 | 87 | −9.4 | 1.0 | −5.7 | 0.7 | J. Cardiovasc. PT 2010; 15, 356–363. |
| W | Starmans-Kool | 14 | N | 10 | 32 | 191 | 94 | 114 | 65 | −2.0 | 3.4 | 0.0 | 3.4 | J. Appl. Physiol. 2011; 110, 468–471. |
Baseline data, blood pressure outcome data and references of included studies.
Eth, Ethnicity; A, Asian; B, Black; W, White; NI, Nigeria; Ja, Jamaica; ANHMRC, Australian National Health and Medical Research Council; Dur, Duration (Days); BP, Blood pressure; H, Hypertension; TH, Treated hypertension; N, Normotension; Age, Age (years); HS, High sodium intake (mmol); LS, Low sodium intake (mmol); B., Baseline; E, Effect; SBP, Systolic blood pressure; DBP, Diastolic blood pressure; SSE, Systolic blood pressure standard error; DSE, Diastolic blood pressure standard error.
Table 1 shows the references, baseline characteristics and the individual study data of the 9 Asian, 9 Black, and 74 White populations included in the present study. Summary measures of baseline variables and BP effects of Asians, Blacks and Whites are shown in Table 2. There was no statistical difference in sex distribution although there was a trend toward a higher fraction of females in Asians. Asians were significantly older and had a significantly higher sodium intake than Blacks and Whites. Still the effect of SR on SBP and DBP did not differ from the effect in Blacks and Whites.
Table 2
| Asians (A) | Blacks (B) | Whites (W) | W (A)* | Significance | |
|---|---|---|---|---|---|
| N studies | 9 | 9 | 74 | 39 | |
| N participants | 661 | 561 | 3782 | 2779 | |
| Female % | 58 | 45 | 45 | 0.21 | |
| Mean (95% CI) | |||||
| Sodium reduction (SR) mmol | 97.89 [46.46, 149.31] | 63.16 [48.86, 77.46] | 102.91 [92.20, 113.63] | 66.12 [58.49, 73.75] | B vs. W 0.006 |
| Age, years | 52.30 [49.52, 55.08] | 46.83 [25.41, 68.25] | 43.04 [39.64, 46.44] | 49.14 [43.57, 54.70] | A vs. W: 0.03 |
| Baseline SBP, mm Hg | 138.29 [126.71, 149.87] | 132.84 [125.30, 140.37] | 133.58 [130.75, 136.41] | 137.24 [133.39, 141.09] | NS |
| Baseline DBP, mm Hg | 84.68 [78.03, 91.33] | 80.90 [75.01, 86.80] | 80.69 [78.20, 83.18] | 82.43 [79.04, 85.82] | NS |
| Baseline sodium intake | 217.48 [194.68, 240.28] | 148.70 [133.28, 164.12] | 167.67 [161.17, 174.17] | 137.43 [133.17, 141.68] | A vs. B and A vs. W: 0.00001 |
| Effect SBP, mm Hg | −3.83 [−6.35, −1.31] | −4.68 [−7.10, −2.26] | −3.24 [−4.01, −2.46] | −3.06 [−3.94, −2.18] | NS (Figure 1) |
| Effect DBP, mm Hg | −1.99 [−3.04, −0.94] | −2.99 [−3.95, −2.02] | −1.54 [−2.05, −1.03] | −1.51 [−2.04, −0.98] | B vs. W: 0.04 B vs. W (A): 0.013 (Figure 1) |
Baseline variables and blood pressure effects in populations of Whites, Blacks, and Asians balanced with respect to baseline blood pressure unadjusted and adjusted for sodium reduction.
Sodium reduction adjusted to Blacks by elimination of all studies of Whites with SR > 90 mmol.
Figure 1 shows the comparisons between ethnic groups of the summary measures of SBP and DBP. Cross-sectional data for all included studies are shown in Figure 1, lines 1,3,5,8, 10, and 12. In addition the results from studies investigating at least two ethnic groups are shown in lines 2, 4, 6, 9, 11, and 13. The differences between the ethnic groups are substantially smaller than in the original analyses (Graudal et al., 2011). The effect of SR on DBP showed a significant difference between Blacks and Whites. The differences were generally smaller and not statistically significant when comparing the data obtained from studies investigating two or three ethnic groups in identical studies (Figure 1, lines 2, 4, 6, 9, 11, and 13) than when comparing data across studies (Figure 1, lines 1,3,5,8, 10, and 12).
Figure 1
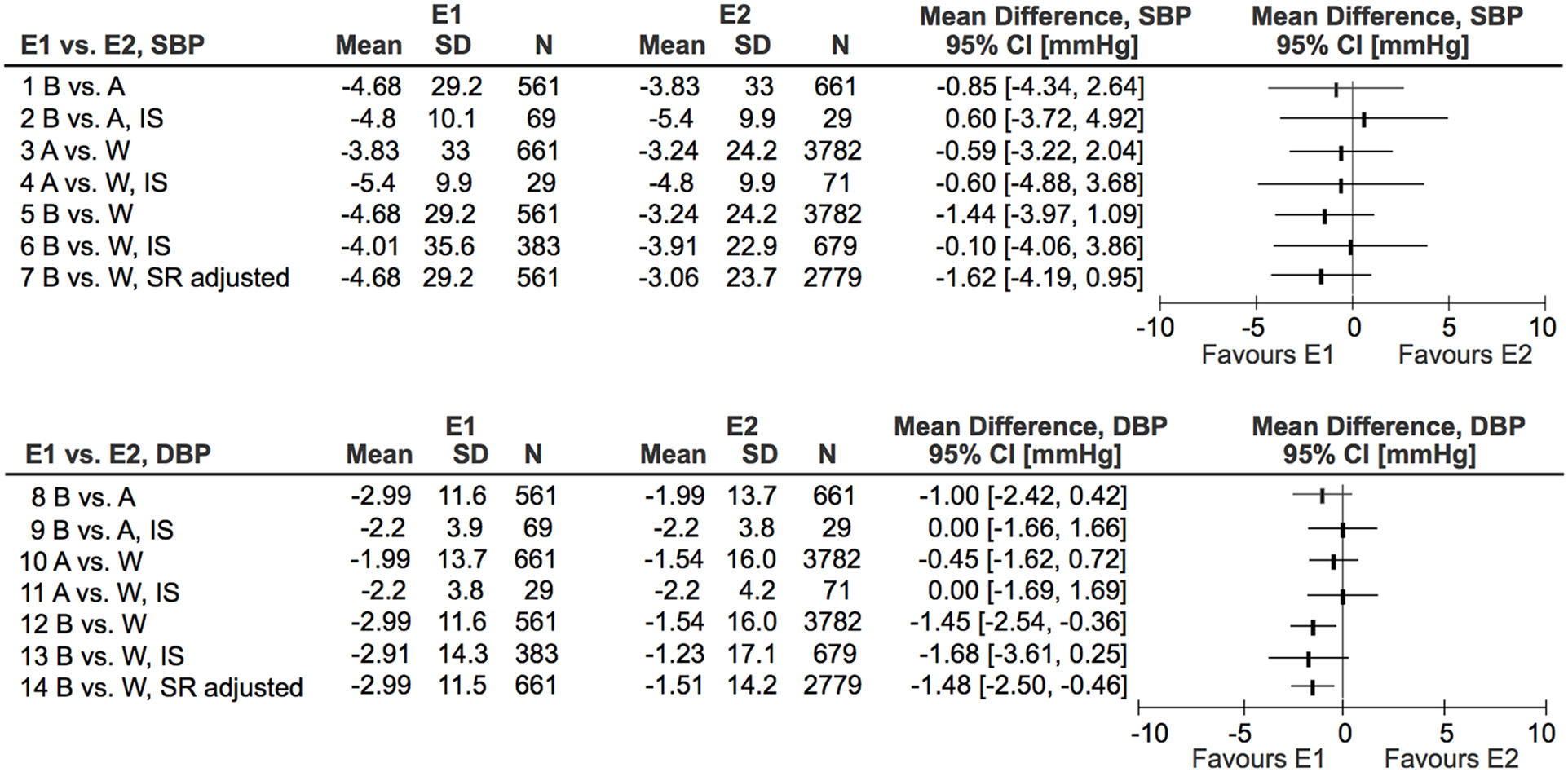
Differences in effect of sodium reduction on systolic and diastolic blood pressure (SBP and DBP) between Asians (A), Blacks (B), and Whites (W). E, Ethnic group; IS, Identical study.
Supplementary analyzes
As the attempt to adjust the ethnic groups did not completely succeed, we supplied with a supplementary meta-regression analysis of ethnicity versus effect on blood pressure adjusted for amount of sodium reduction, baseline blood pressure, age, the duration of the sodium reduction intervention and the female percentage. This analysis shows that there is a statistically significant difference in SBP effect between the ethnic groups, both unadjusted and adjusted, but clinically the difference is small (about 1 mmHg) (Table 3). There were no differences in DBP effect between the ethnic groups (Table 3).
Table 3
| 1: Ethnicity N = 92 (univariate) | 2: 1 + Sodium reduction | 3: 2 + Baseline blood pressure | 4: 3 + Age | 5: 4 + Duration | 6: 5 + Female% | |
|---|---|---|---|---|---|---|
| Effect SBP, | 1.28 (0.039) | 1.32 (0.032) | 1.15 (0.026) | 1.08 (0.032) | 1.12 (0.03) | 1.07 (0.043) |
| Effect DBP, | 0.63 (0.083) | 0.60 (0.10) | 0.50 (0.14) | 0.46 (0.17) | 0.55 (0.11) | 0.61 (0.077) |
Regressionkoefficient, mmHg (p-value) in univariate and multivariate regressionanalyses adjusted for additional confounders.
In another additional analysis we excluded 35 study populations of Whites with a high sodium reduction to adjust the quantity of sodium reduction in Blacks and Whites (Table 2, column 5). This only changed the outcome blood pressures marginally (Figure 1, lines 7 and 14).
Discussion
The present study, which attempted to adjust for baseline blood pressure and the quantity of sodium reduction showed that Asians had a non-significant trend toward a higher BP response to SR than whites, but they were also older, had a non-significantly higher mean baseline BP and a significantly higher baseline sodium intake (Table 2). Blacks had a non-significant trend toward a higher SBP response and a significant trend toward a higher DBP response to SR than Whites while matching the Whites on other baseline variables except quantity of SR (Table 2). The difference was unchanged after adjusting for quantity of SR (Table 2). The supplementary meta-regression analyses adjusted for confounders confirmed that the ethnic differences in blood pressure response to sodium reduction were small, although marginally significant for SBP. Thus there may be an unexplained additional effect of SR on BP, especially in Blacks, which however is small compared to previous unadjusted findings (Graudal et al., 2011). One explanation could be that there are few studies in Asians and Blacks. This might increase the risk of publication bias as suggested by our previous cumulative meta-analysis (Graudal et al., 1998), which showed a higher effect of SR on BP after publication of the first 7–8 studies, whereas a smaller and more stable effect was manifest after the publication of about 15 studies. This assumption is also indicated by the fact that the comparisons of Asian, Black, and White study populations from identical studies showed no statistical differences between the ethnic groups (Figure 1). The heterogeneity between the baseline characteristics was large and therefore it was difficult to adjust all 3 study-groups to identical baseline values, because adjustment of one baseline value created another imbalance between other baseline variables. However, in spite of these variations, the differences in effects of SR on BP between the ethnic groups were small.
Our results are in accordance with a recent co-operation between Cuban, Canadian, and American researchers, who compared Black and White Cubans living under similar socio-economic conditions and found that “skin color was unrelated to mean blood pressure or hypertensive status” (Ordúñez1 et al., 2013). The background for this study was the assumption by many scientists that the excess burden of hypertension among blacks was an inevitable phenomenon. However, the authors concluded that social conditions rather than ethnic group may determine the general development of excess hypertension in Blacks (Ordúñez1 et al., 2013). In that context it should be emphasized that the sodium reduction RCTs of Whites generally are performed in Europeans and Americans, whereas the RCTs of Blacks are performed in Black Americans and Africans, who socioeconomically are not comparable to White Americans and Europeans. In that context it is interesting that after adjustment for important confounders the difference between Whites and Blacks was small. If we had been able to adjust for socio-economic differences this last small difference in effect on DBP might have disappeared.
The possibility that socioeconomic conditions has an important influence on BP may also be reflected in the BP development in the United States during the 20th century. Not only did BP fall markedly in each new 10–year birth cohort from 1887 to 1975, the slope of the BP increase with age of each of these cohorts also decreased (Goff et al., 2001). The total fall in BP during the 20th century was dramatic and cannot solely be explained by the introduction of antihypertensive treatments, low-fat diets or decrease in the use of tobacco, as the BP fall started long before these interventions. The enormous socio-economic development in the United States is a much more likely explanation. Recently the fall in BP seems to have stopped, maybe due to the present overweight epidemic (Goff et al., 2012). In the Cuban study the mean SBP was about 120 mmHg (adults > 15 years) and the percentage of hypertension was about 31% in both Blacks and Whites. In US the mean SBP was about 127 mmHg for Blacks and about 122 mmHg for Whites (adults > 18 years) (Wright et al., 2011). The percentage of hypertension is about 37% for Blacks and 30% for Whites (Wright et al., 2011).
An IOM report from 2004 recommended that all African Americans eat less than 1500 mg of sodium, whereas whites could eat up to 2300 mg of sodium (Institute of Medicine, 2004). In contrast the recent IOM report from 2013 (Institute of Medicine, 2010) concluded “Given this background, overall, the committee found that the available evidence on associations between sodium intake and direct health outcomes is consistent with population-based efforts to lower excessive dietary sodium intakes, but it is not consistent with recommendations that encourage lowering of dietary sodium in the general population to 1500 mg per day. Further, as noted in the 2010 DGAC report, population subgroups, including those with diabetes, CKD, or preexisting CVD, individuals with hypertension, pre-hypertension, persons 51 years of age and older, and African Americans represent, in aggregate, a majority of the general U.S. population. Thus, when considered in light of the current state of the evidence on associations between sodium intake and direct health outcomes for these subgroups, except when data specifically indicate they are different, there is not sufficient evidence to support treating them differently from the general U.S. population.” The present study is in accordance with the 2013 IOM conclusion indicating no true ethnic dependent sensitivity to sodium.
In conclusion, ethnic differences in blood pressure response to sodium reduction seem smaller than previously observed. When the effect of SR on BP was adjusted for baseline blood pressure and quantity of sodium reduction there was a small statistically significant ethnic difference in SBP response and DBP response depending on the statistical method used, but the comparisons of Asian, Black and White study populations from studies investigating ethnic groups in identical studies showed no statistical differences in effect of SR on SBP or DBP between the ethnic groups in accordance with the conclusion of the 2013 IOM report. Whether the small observed differences in the present study are due to socio-economic factors or genetic factors remains to be setteled. Public guidelines like the American Guidelines (U.S. Department of Agriculture and U.S. Department of Health and Human Services 2010) might be changed to recommend the same levels of sodium intake irrespective of ethnicity.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Statements
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1
Goff D. C. Jr. Gillespie C. Howard G. Labarthe D. R. (2012). Is the obesity epidemic reversing favorable trends in lood pressure? Evidence from cohorts born between 1890 and 1990 in the United States. Ann. Epidemiol. 22, 554–561. 10.1016/j.annepidem.2012.04.021
2
Goff D. C. Jr. Howard G. Russell G. B. Labarthe D. R. (2001). Birth cohort evidence of population influences on blood pressure in the United States, 1887-1994. Ann. Epidemiol. 11, 271–279. 10.1016/S1047-2797(00)00224-6
3
Graudal N. Alderman M. H. (2014). Response to “Article on sodium intake should include ethnic disclaimer.”Am. J. Hypertens. 27, 1232. 10.1093/ajh/hpu148
4
Graudal N. A. Galløe A. M. Garred P. (1998). Effects of sodium restriction on blood pressure, renin, aldosterone, catecholamines, cholesterols. JAMA279, 1383–1391. 10.1001/jama.279.17.1383
5
Graudal N. A. Hubeck-Graudal T. Jurgens G. (2011). Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst. Rev. 11:CD004022. 10.1002/14651858.CD004022.pub3
6
Graudal N. A. Hubeck-Graudal T. Jurgens G. McCarron D. A. (2015). The significance of duration and dose of sodium reduction intervention in normotensive and hypertensive individuals. A meta-analysis. Adv. Nutr. 6, 169–177. 10.3945/an.114.007708
7
Institute of Medicine (IOM). (2004). Dietary Reference Intakes: Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: National Academies Press.
8
Institute of Medicine (IOM). (2010). Sodium Intake in Populations: Assessment of Evidence. Washington, DC: National Academies Press.
9
McCarron D. A. Kazaks A. G. Geerling J. C. Stern J. S. Graudal N. A. (2013). Normal range of human dietary sodium intake: a perspective based on 24-hour urinary sodium excretion worldwide. Am. J. Hypertens. 26, 1218–1223. 10.1093/ajh/hpt139
10
Ordúñez1 P. Kaufman J. S. Benet M. Morejon A. Silva L. C. Shoham D. A. et al . (2013). Blacks and whites in Cuba have equal prevalence of hypertension: confirmation from a new population survey. BMC Public Health13:169. 10.1186/1471-2458-13-169
11
Powles J. Fahimi S. Micha R. Khatibzadeh S. Shi P. Ezzati M. et al . (2013). Global Burden of Diseases Nutrition and Chronic Diseases Expert Group(NutriCoDE). Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open3:e003733. 10.1136/bmjopen-2013-003733
12
U.S. Department of Agriculture and U. S. Department of Health and Human Services (2010). Dietary Guidelines for Americans. Available online at: www.dietaryguidelines.gov
13
Wright J. D. Hughes J. P. Ostchega Y. Yoon S. S. Nwankwo T. (2011). Mean Systolic and Diastolic blood pressure in adults aged 18 and over in the United States, 2001–2008. Natl. Health Stat. Rep. 35, 1–24.
Summary
Keywords
blood pressure, dietary sodium, dietary salt, ethnicity, meta-analysis
Citation
Graudal N and Jürgens G (2015) The blood pressure sensitivity to changes in sodium intake is similar in Asians, Blacks and Whites. An analysis of 92 randomized controlled trials. Front. Physiol. 6:157. doi: 10.3389/fphys.2015.00157
Received
27 February 2015
Accepted
29 April 2015
Published
21 May 2015
Volume
6 - 2015
Edited by
Alexander John Rouch, Oklahoma State University Center for Health Sciences, USA
Reviewed by
Bruce N. Van Vliet, Memorial University of Newfoundland, Canada; Ningjun Li, Virginia Commonwealth University, USA
Copyright
© 2015 Graudal and Jürgens.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Niels Graudal, Department of Rheumatology, University Hospital of Copenhagen, Blegdamsvej 9, DK 2100 Copenhagen, Denmark graudal@dadlnet.dk
This article was submitted to Integrative Physiology, a section of the journal Frontiers in Physiology
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.