- 1Department of Cardiac Rehabilitation, Guangdong Provincial People’s Hospital, Guangzhou, China
- 2Department of Rehabilitation Medicine, The Fifth Affiliated Hospital of Guangzhou Medical University, Guangzhou, China
- 3Department of Rehabilitation Medicine, Guangzhou Medical University, Guangzhou, China
- 4Guangzhou Key Laboratory of Enhanced Recovery After Abdominal Surgery, The Fifth Affiliated Hospital of Guangzhou Medical University, Guangzhou, China
Objective: Mask plays an important role in preventing infectious respiratory diseases. The influence of wearing masks in physical exercise on the human body needs to be studied. The purpose of this study is to explore the influence of wearing surgical masks on the cardiopulmonary function of healthy people during exercise.
Methods: The physiological responses of 71 healthy subjects (35 men and 36 women, age 27.77 ± 7.76 years) to exercises with and without surgical masks (mask-on and mask-off) were analyzed. Cardiopulmonary function and metabolic reaction were measured by the cardiopulmonary exercise test (CPET). All tests were carried out in random sequence and should be completed in 1 week.
Results: The CPETs with the mask-on condition were performed undesirably (p < 0.05), and the Borg scale was higher than the mask-off (p < 0.001). Rest oxygen uptake () and carbon dioxide production (CO2) with the mask-on condition were lower than mask-off (p < 0.01), which were more obvious at peak exercise (O2peak: 1454.8 ± 418.9 vs. 1628.6 ± 447.2 ml/min, p < 0.001; CO2peak: 1873.0 ± 578.7 vs. 2169.9 ± 627.8 ml/min, p = 0.005), and the anaerobic threshold (AT) brought forward (p < 0.001). At different stages of CPET with the mask-on condition, inspiratory and expiratory time (Te) was longer (p < 0.05), and respiratory frequency (Rf) and minute ventilation (E) were shorter than mask-off, especially at peak exercise (Rfpeak: 33.8 ± 7.98 vs. 37.91 ± 6.72 b/min, p < 0.001; Epeak: 55.07 ± 17.28 vs. 66.46 ± 17.93 l/min, p < 0.001). VT was significantly lower than mask-off just at peak exercise (1.66 ± 0.45 vs. 1.79 ± 0.5 l, p < 0.001). End-tidal oxygen partial pressure (PetO2), end-tidal carbon dioxide partial pressure (PetCO2), oxygen ventilation equivalent (E/O2), and carbon dioxide ventilation equivalent (E/CO2) with mask-on, which reflected pulmonary ventilation efficiency, were significantly different from mask-off at different stages of CPET (p < 0.05), but no significant difference in percutaneous oxygen saturation (SpO2) was found. Differences in oxygen pulse (O2/HR), oxygen uptake efficiency slope (OUES), work efficiency (△O2/△W), peak heart rate (HR), and peak systolic blood pressure (BP) existed between two conditions (p < 0.05).
Conclusion: Wearing surgical masks during aerobic exercise showed certain negative impacts on cardiopulmonary function, especially during high-intensity exercise in healthy young subjects. These results provide an important recommendation for wearing a mask at a pandemic during exercises of varying intensity. Future research should focus on the response of wearing masks in patients with related cardiopulmonary diseases.
Introduction
In 2020, a new type of coronavirus swept the world, which was highly contagious and harmful, seriously endangering human health, even causing death and affecting social stability. At present, there has been no specific drug to treat the COVID-19 virus, so it is very important to actively prevent its transmission (Indu et al., 2020). The main modes of transmission include airborne transmission, aerosol transmission, and contact transmission (Fink et al., 2020). The role of the mask in other respiratory diseases has been confirmed (Liang et al., 2020). There has been also evidence that masks could help to prevent the spread of COVID-19 (Chan et al., 2020; Tirupathi et al., 2020). A study in the United States showed that if 80% of the people in New York wore a mask with moderate efficiency (50%), the peak daily mortality could have been reduced by 34–58%. Even wearing masks with low efficiency (20%) in low-risk areas still had a certain effect, which could have been reduced community transmission in COVID-19 (Eikenberry et al., 2020). Therefore, on April 3, 2020, the US Centers for Disease Control and Prevention (CDC) recommended that the public should wear a mask when going out (Islam et al., 2020). Although the marketing of vaccines is conducive to the control of transmission in COVID-19, the daily protection work cannot be ignored. In this year, the mask has become an essential part of daily life and work.
At present, most research studies on the effects of wearing masks on human physiology have addressed the safety and performance of mask before it was put on the market. Some research suggested that wearing masks could impact human physiological functions, especially cardiopulmonary function, such as increased airway resistance, hypoxia, carbon dioxide retention, and other lung function changes, leading to increased heart load, insufficient coronary perfusion, decreased muscle aerobic metabolism, increased anaerobic metabolism, and even affecting renal function and immune function (Lee and Wang de, 2011; Chandrasekaran and Fernandes, 2020). Wearing masks will also increase temperature, humidity, and discomfort on the face (Scarano et al., 2020), and affect exercise performance (Driver et al., 2021). The type of mask, the time of wearing the mask, the type and intensity of the activity, and the environment will have different effects. The limited small sample study indicated that it was relatively safe to wear surgical masks or filter masks (such as N95) for daily activities and short-term low-intensity exercise (Goh et al., 2019). There were few reports on the physiological changes of the human body when wearing masks for moderate and high-intensity exercise. Research on 16 athletes demonstrated that after wearing masks, the maximum oxygen uptake (O2) and ventilation decreased, and 11 athletes had acute dyspnea at the peak of maximal exercise test (Egger et al., 2021). Athletes with good cardiopulmonary reserve function had such changes, not to mention ordinary healthy people. Fikenzer et al. (2020) conducted cardiopulmonary exercise tests (CPETs) on 12 healthy men under different masks. The results showed that surgical masks and FFP2/N95 masks could reduce ventilation, exercise endurance, and comfort. Lässing et al. (2020) tested 14 healthy men with constant power exercise and found out that the peak heart rate (HR) and cardiac output (CO) were larger when wearing surgical masks, but there were no differences in the changes in blood pressure (BP) and blood lactate. However, the research of Shaw K demonstrated that wearing masks for strenuous exercise had no obvious effect on the exercise performance of healthy young people, such as percutaneous oxygen saturation (SpO2), tissue oxygenation index, exercise maximum load, exercise HR, and rating of perceived exertion (RPE) (Shaw et al., 2020). A study on sarcopenia patients also showed that when wearing surgical or FFP2 masks for resistance training the changes in HR, HR variability, blood lactic acid concentration, self-perceived fatigue, and muscle strength were similar with not wearing masks (Ramos-Campo et al., 2021).
The influence of masks on human cardiopulmonary function during exercise remains unclear, and proper exercise training is an effective measure to prevent diseases and improve the prognosis of diseases. In the ongoing epidemic, people still need to wear masks for a long time, so it is necessary to further study the influence of wearing masks on human cardiopulmonary function. Therefore, this study intends to explore the effect of surgical masks in healthy people by monitoring the changes in cardiopulmonary function and metabolic parameters to guide safe exercise while wearing surgical masks.
Materials and Methods
Subjects
The research is a self-controlled trial, which has been approved by the Ethics Committee of Guangdong Provincial People’s Hospital (ethics number: GDREC2020145H) and can be consulted in the Chinese Clinical trial registry (No. ChiCTR2000033449). Healthy subjects were recruited from June 1, 2020 to July 31, 2020. The inclusion criteria of the study included subjects between 18 and 40 years old, who participated voluntarily, passed PAR-Q questionnaire screening, had normal rest electrocardiogram and static lung function, and had signed informed consent. The presence of any of the following conditions would not be allowed to participate in the study, including the history of COVID-19 infection, previous cardiopulmonary diseases (such as asthma, chronic bronchitis, pulmonary fibrosis, emphysema, and congenital heart disease), situations (such as exercise asthma and epilepsy) that may deteriorate due to exercise, physical disability caused by articulations or neuromuscular diseases, lower respiratory tract infection in the past 2 weeks, acute upper respiratory tract infection or symptomatic rhinitis in the past 1 week, mental or cognitive disabilities, smoking, pregnancy, menstrual period and lactation period, and other contraindications of CPET.
Study Design
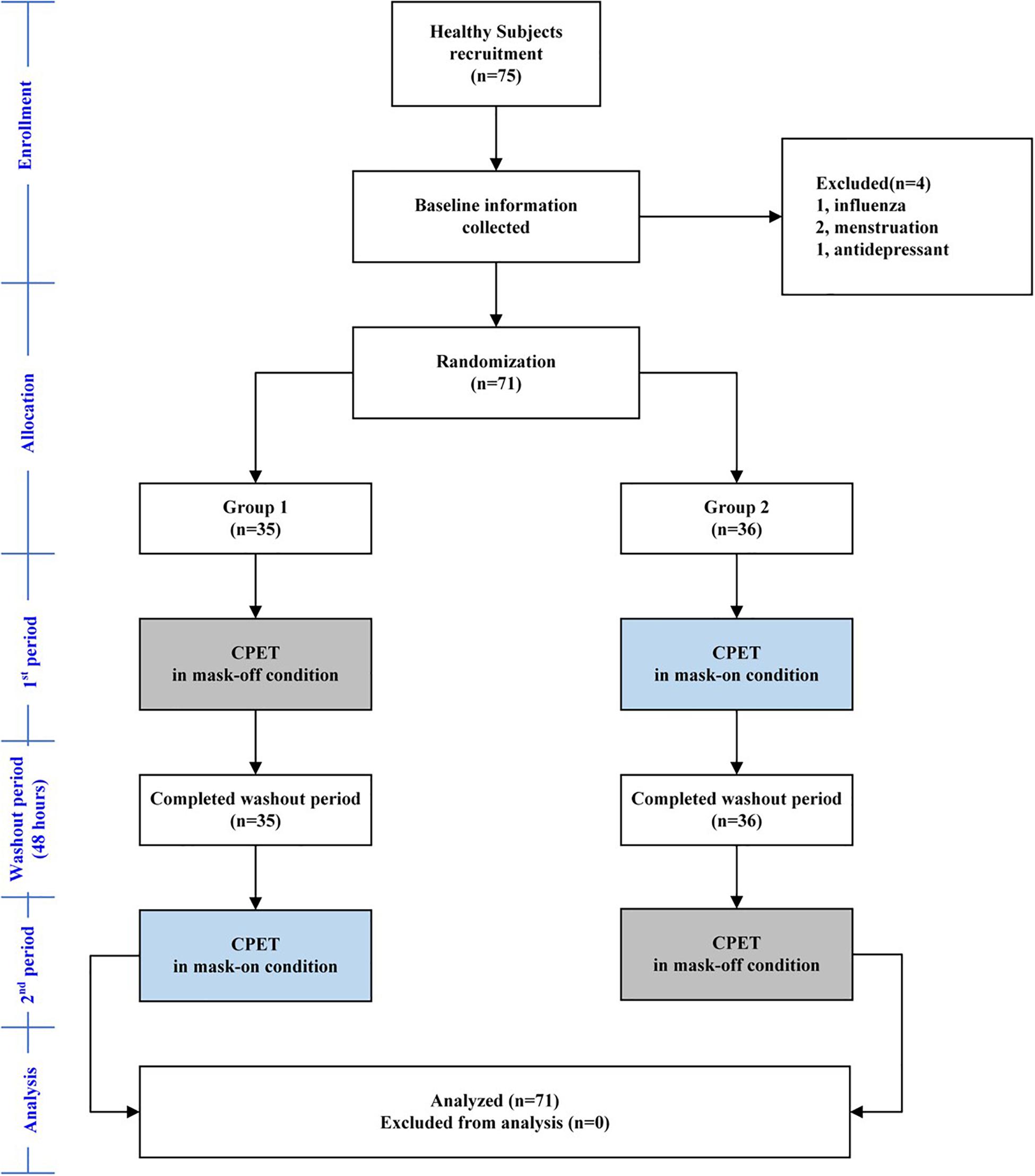
Every subject was asked to go to the hospital to complete the CPET two times. The two tests were carried out under conditions A (mask-on) and B (mask-off). The interval between the two tests was at least 24 h and completed within 1 week. Every subject was randomly assigned to CPET according to AB sequence or BA sequence (flow chart is as Figure 1). All CPETs were completed by one professional. When subjects entered the experiment, medical data were collected, and vital signs, height, weight, rest electrocardiogram, and static lung function tests were carried out by special personnel.
Masks
All subjects were provided with typical and widely used disposable ear-hanging surgical masks for adults (Guangzhou Tianhe Haozheng Sanitary Materials Factory, Guangzhou, China). The spirometry mask (V2 MASK, United States) used in CPET was selected according to the face shape of subjects and required to wear comfortably. The spirometry mask was placed over the surgical masks and fixed with head straps in a leak-proof manner (Figure 2). Before each CPET, an air leakage test was conducted to confirm whether the mask fits correctly. The tester completely blocked the ventilation valve of the spirometry mask with the palm of the hand. Then, the subjects breathed with maximal force against the mask to check for leaks (Figure 2). This maneuver was repeated until no acoustic, visual, and sensory indications of leakage were detectable.
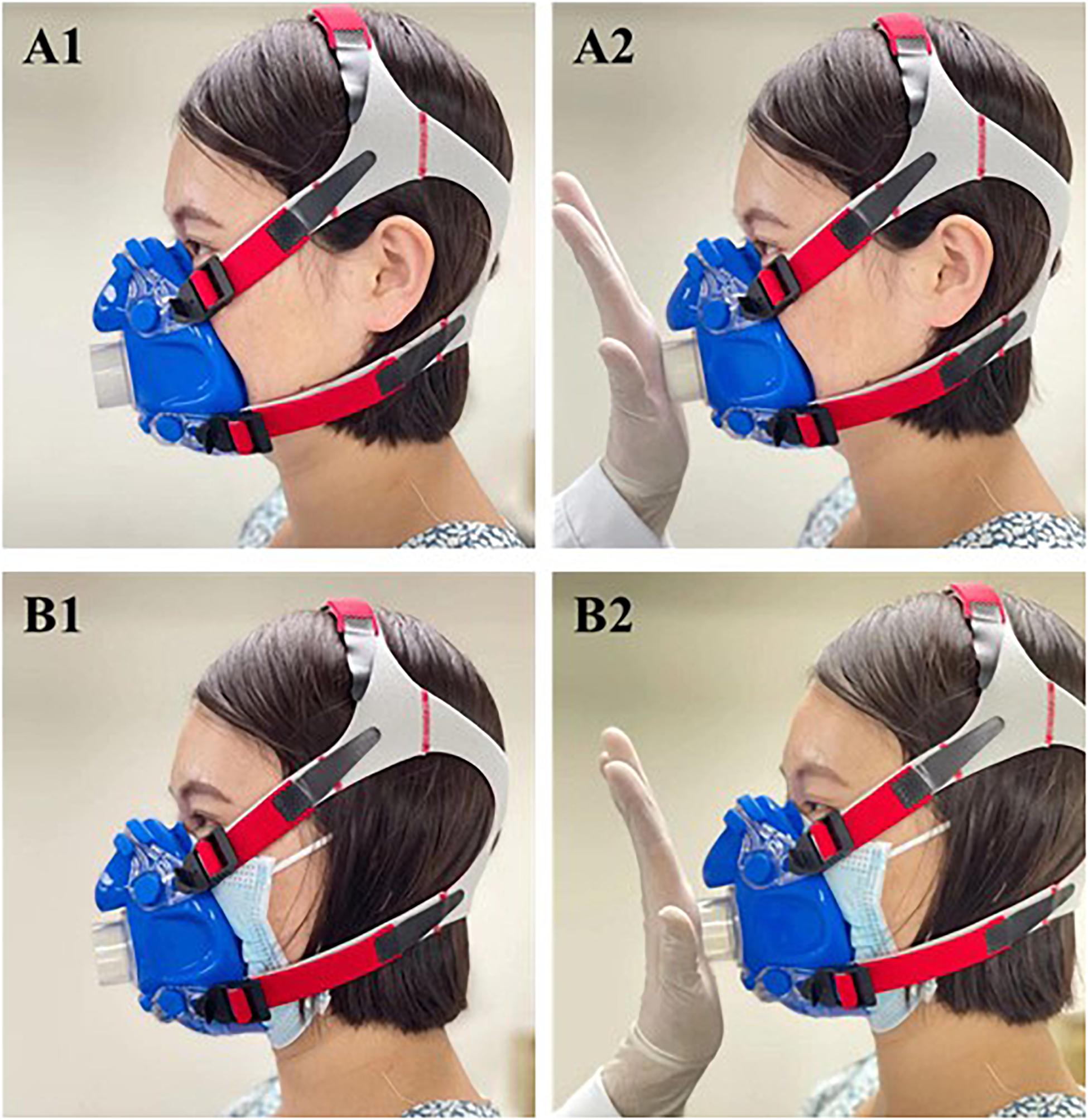
Figure 2. Fit comparison of mask-on and mask-off condition. (A1) Mask-off condition. (A2) Fit test in mask-off condition. (B1) Mask-on condition. (B2) Fit test in mask-on condition.
Testing Equipment
Cardiopulmonary Exercise Test
The CPET was performed with JAEGER Master Screen CPX (Germany) system and the cycle ergometer (Ergoline 150P, Germany). Calibration of the gas analyzer was performed before each test, including flow sensor calibration, indoor air calibration, standard balance gas (using 16%O2, 5%CO2, and N2) calibration, and delay calibration. Subjects were asked to take more than 2 h after eating without satiety, were advised to avoid eating foods containing caffeine and alcohol at least 12 h before the test, and were ensured to take adequate rest the day before the test.
Cardiopulmonary Exercise Test Protocol
The CPETs were performed using a ramped cycle ergometer protocol, and incremental power was calculated to let subjects finish the exercise load test in 8–12 min. The incremental power selection was calculated with the following formulas (Costa et al., 2015):
Specific Process
First, the forced vital capacity (FVC), forced expiratory volume in one second (FEV1), FEV1/FVC, and maximum minute ventilation (MVV) were measured. Then, while the subject was wearing a spirometry mask connected with a gas analyzer, a 12-leads ECG was connected, BP cuff and fingertip oxyhemoglobin saturation meter were adjusted, and the seat height of the cycle ergometer was set. Next, the subjects rested for 2 min in a sitting position, collecting rest real-time gas metabolism and ECG data. After 2-min warming up with 0 W, the subjects pedaled the cycle according to the set incremental power (15–25 W/min) until exhaustion, and the pedaling speed was kept at about 60 RPM. The test system automatically collected real-time gas metabolism data through the gas analyzer, ECG, and BP data through telemetry cardiogram monitor, and automatically calculated average values every 10 s of parameters that reflect metabolism, gas exchange, ventilation efficiency, and cardiovascular function, according to the oxygen concentration, carbon dioxide concentration, and respiratory flow rate measured breath-by-breath. When the subjects reached the best effort standard (Dougherty et al., 2018), which met at least three of the following items: (1) RPE ≥ 17; (2) respiratory exchange rate (RER) ≥ 1.10; (3) HRpeak reaches more than 90% of the predicted maximum HR; (4) O2 increases <200 ml (as increased power) or reached other criteria for terminating exercise test, the subjects pedaled for 3 min at 0 W, resting in the sitting position for 3 min to finish the test.
Criteria for Terminating the Exercise Test
The test can be terminated when any of the following items are met:
1. Pedal to exhaustion (RPE ≥ 17–18), the pedaling speed cannot be maintained, lower than 40 RPM.
2. Clinical symptoms: fatigue or dyspnea, severe chest pain; systolic BP decreased by 10 mmHg; cerebral ischemic symptoms, such as dizziness and headache; poor peripheral circulation, such as the face is pale and BP cannot be measured; the subject asked to stop strongly.
3. ECG changes: exercise-induced ST-segment depression ≥ 3 mm or ST-segment elevation > 1 mm; HR did not increase but decreased as exercise intensity increased; the ECG axis was extremely offset; ventricular tachycardia; supraventricular tachycardia; frequent ventricular extrasystoles caused or aggravated by exercise; indoor conduction block caused by exercise.
4. Metabolic index: RER was above 1.15; SpO2 dropped below 86%, and respiratory rate was more than 50 beats/min. Oxygen pulse and O2 appeared to plateau or decrease. HR reserve (HRR) and breathing reserve (BR%) were exhausted.
Rating of Perceived Exertion and Borg Dyspnea Scale
After each CPET, the subjects were asked about the degree of discomfort or intolerance using RPE and Borg dyspnea scale. RPE was scored from 6 to 20, indicating extremely light to exhaustion. Borg dyspnea scale was from 0 to 10, indicating no dyspnea at all to extremely severe dyspnea.
Outcomes
This study obtained data of the following parameters:
(1) CPET performance: CPET test duration, maximum power, RPE score, and Borg dyspnea scale.
(2) Parameters reflecting metabolism: O2, carbon dioxide production (CO2), metabolic equivalent (MET), RER, and percentage of oxygen uptake at anaerobic threshold (AT) in predicted maximal oxygen uptake (O2@AT/O2max pre %). Among them, AT was determined by the V-slope method.
(3) Parameters reflecting lung ventilation and ventilation efficiency: inspiratory time (Ti), expiratory time (Te), respiratory frequency (Rf), tidal volume (VT), minute ventilation volume (E), end-tidal oxygen partial pressure (PetO2), end-tidal carbon dioxide partial pressure (PetCO2), oxygen ventilation equivalent (E/O2), and carbon dioxide ventilation equivalent (E/CO2), carbon dioxide ventilation equivalent slope (E/CO2 Slope), and BR% and SpO2.
(4) Parameters reflecting cardiovascular function: oxygen pulse (O2/HR), work efficiency (△O2/△W), oxygen uptake efficiency slope (OUES), BP, HR, and HRR.
The main outcome measures were E, Vt, PetCO2, O2, O2/kg, CO2, O2/HR, and OUES.
Sample Size Estimation
According to the pre-experiment results, the main outcome measure was O2peak/kg, and the software G∗Power 3.1.92 was used. The authors assumed that the risk was 0.05 and the risk was 0.95, the average difference of O2peak/kg between two groups of CPETs (with and without masks) was 11.7 (SD is 13.27) ml/min/kg. The results showed that 44 subjects were needed.
Statistical Analysis
SPSS 25.0 statistical software was used for data processing. The measurement data were tested for normality, and the normal distribution data were expressed in mean ± SD ( ± s) and the non-normal distribution data was expressed in the median; enumeration data used cases and the rate (%). Paired t-test was used for self-comparison of normal distribution variables; the Wilcoxon rank-sum test was used for self-comparison of non-normal distribution variables. The significance level was set at p < 0.05.
Results
Baseline Characteristic
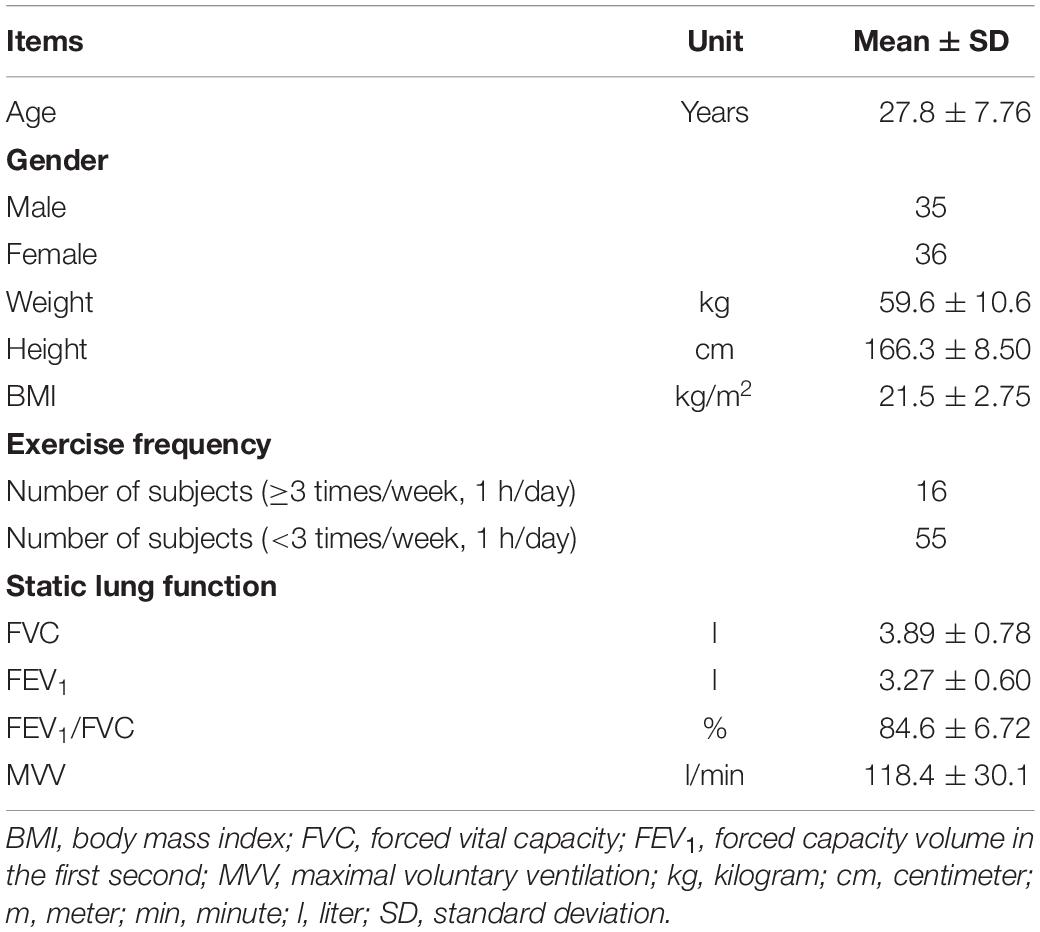
A total of 75 subjects were recruited, in which 4 subjects were excluded because 1 had influenza, 2 were menstruating, and 1 was under antidepressant. So, 71 healthy subjects (men 35, women 36) were recruited through outpatient service, with an average age of 27.77 ± 7.76 years and an average BMI of 21.46 ± 2.75 kg/m2. Among them, 77% of subjects exercised less than three times per week and 1 h per day. The mean FVC, FEV1, FEV1/FVC, and MVV of subjects were 3.89 ± 0.78 l, 3.27 ± 0.60 l, 84.62 ± 6.72%, and 118.40 ± 30.10 l, respectively (Table 1).
Cardiopulmonary Exercise Test Performances
The CPET test time was slightly shorter in mask-on condition than mask-off (7.97 ± 1.50 vs. 8.20 ± 1.39 min, p = 0.052), and the maximum power in mask-on condition was also significantly lower than mask-off (142.9 ± 44.22 vs. 149.8 ± 46.04 W, p < 0.001). The RPE and the Borg scale of the two conditions were significantly different (p < 0.001), and the Borg scales of the mask-on condition were higher (5.69 ± 1.62 vs. 4.78 ± 1.72, p < 0.001) (Table 2).
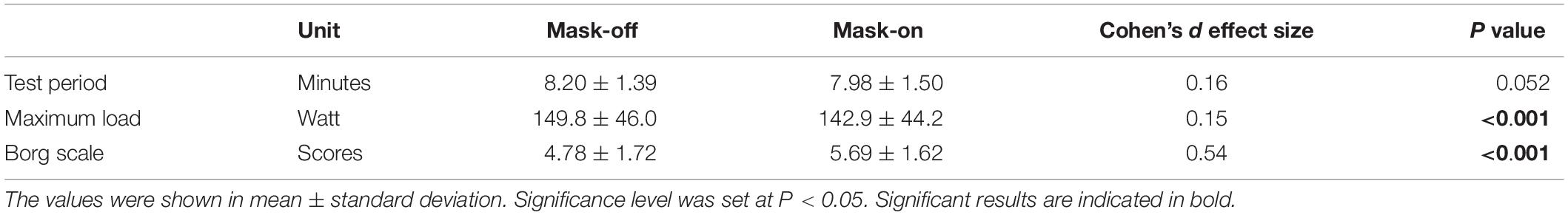
Table 2. The comparison of cardiopulmonary exercise performance between mask-on and mask-off condition.
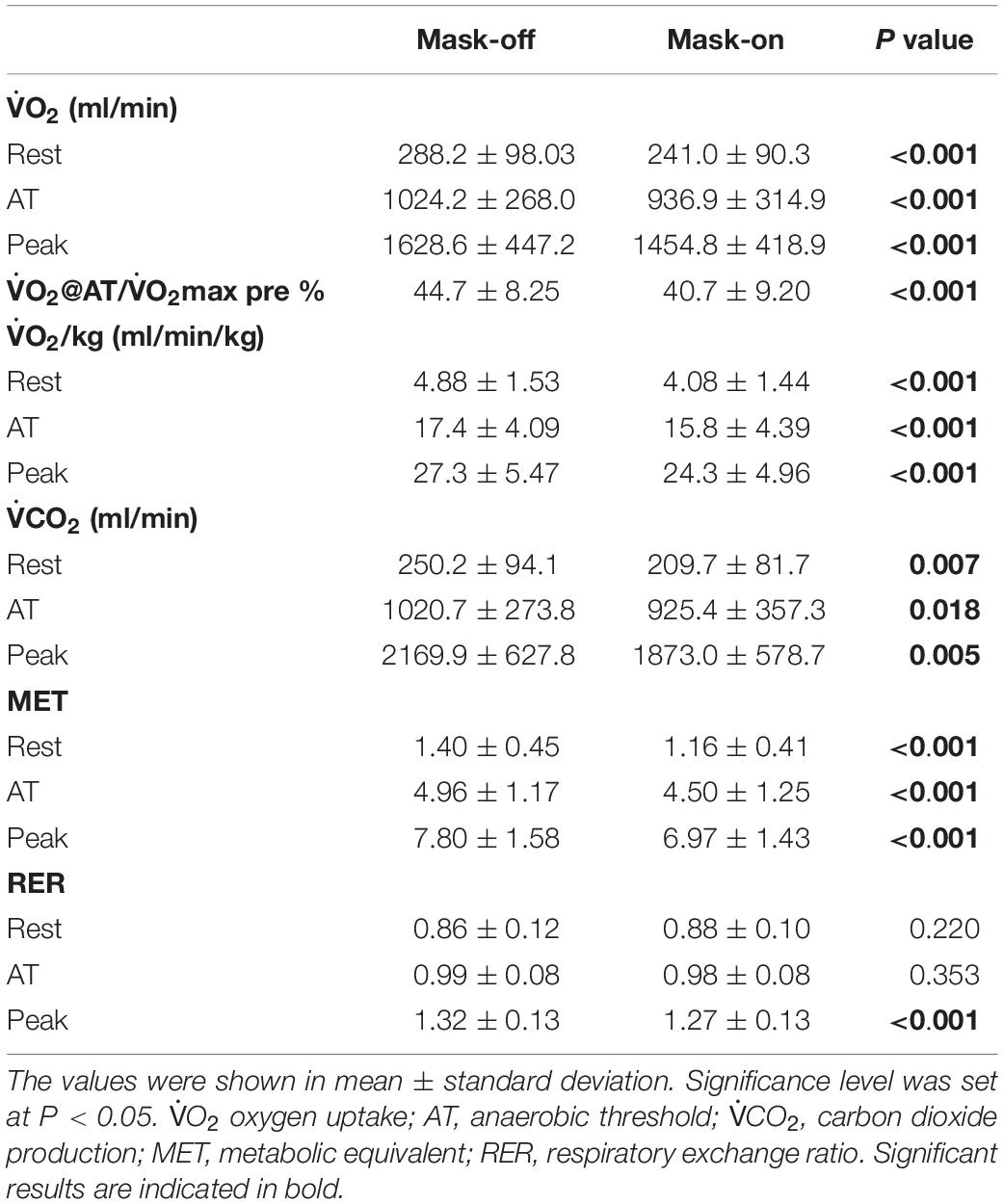
Metabolic Reaction Parameters
The results of metabolic reaction parameters showed that O2, O2/kg, and MET of mask-off and mask-on were significantly different in each stage of CPET (p < 0.001), and O2peak and O2peak/kg of mask-on was significantly lower than mask-off (O2peak: 1454.8 ± 418.9 vs. 1628.6 ± 447.2 ml/min, p < 0.001; O2peak/kg: 24.33 ± 4.96 vs. 27.3 ± 5.47 ml/min/kg, p < 0.001). There were significant differences in both conditions on O2@AT/O2 max pre % (p < 0.001). The O2 of mask-on was lower than mask-off in the rest period of CPET (209.7 ± 81.74 vs. 250.2 ± 94.14 ml/min, p = 0.007), and the difference was more significant in the peak exercise period (1873.0 ± 578.7 vs. 2169.9 ± 627.8 ml/min, p = 0.005). There were significant differences in both conditions on RER only at peak exercise (p < 0.001) (Table 3).
Lung Function Parameters
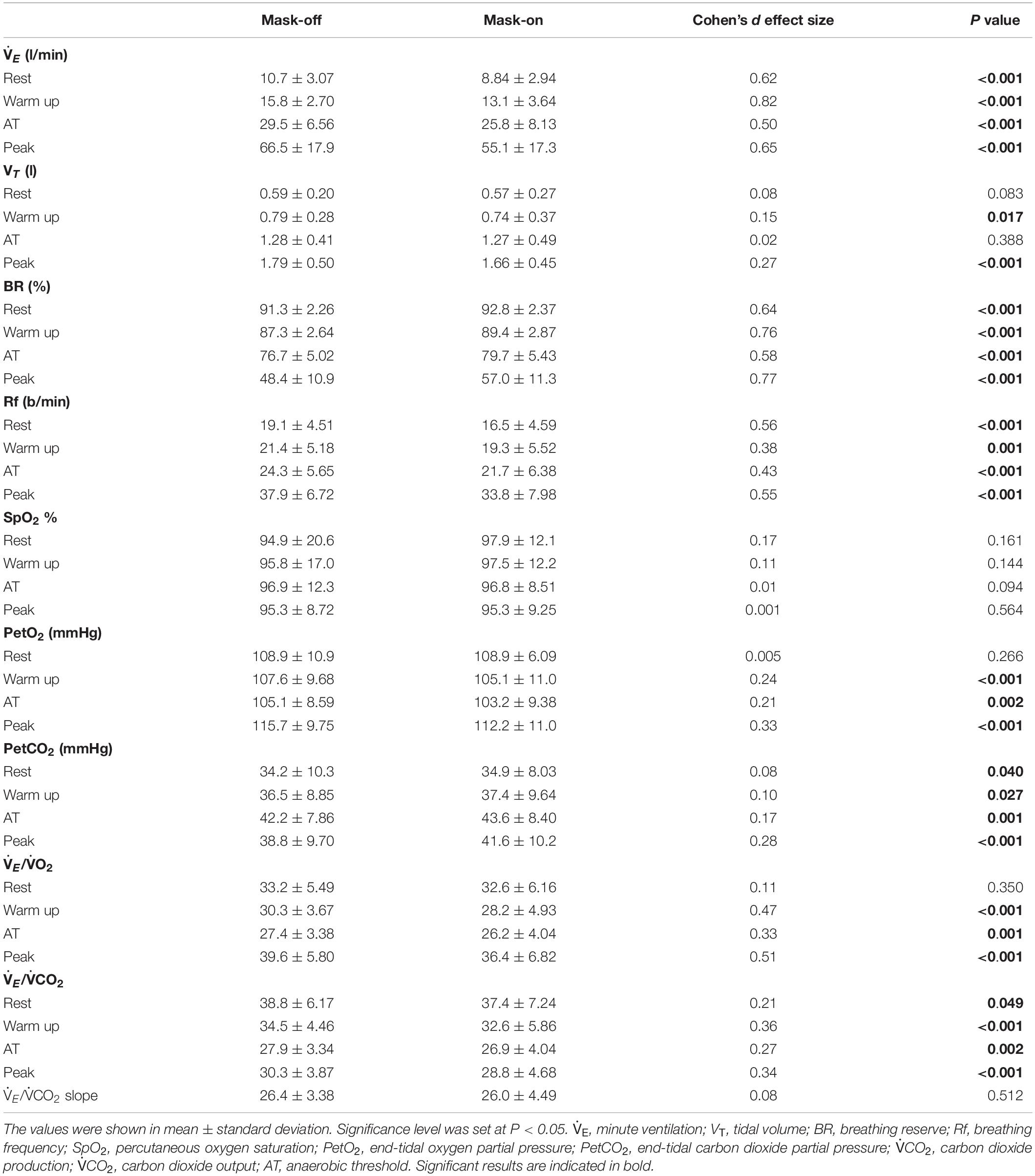
The results of lung ventilation response parameters showed that at different stages of CPET with mask-on condition, Ti and Te were longer than mask-off (p < 0.05). The differences of Ti between mask-on and mask-off at rest, AT and peak period were 0.39 ± 0.76 s (p < 0.001), 0.30 ± 0.37 s (p < 0.001) and 0.20 ± 0.27 s (p < 0.001), respectively. The differences of Te between mask-on and mask-off at rest, AT and peak period were 0.21 ± 0.64 s (p = 0.008), 0.14 ± 0.47 s (p = 0.016) and 0.05 ± 0.27 s (p = 0.164), respectively (Figure 3).
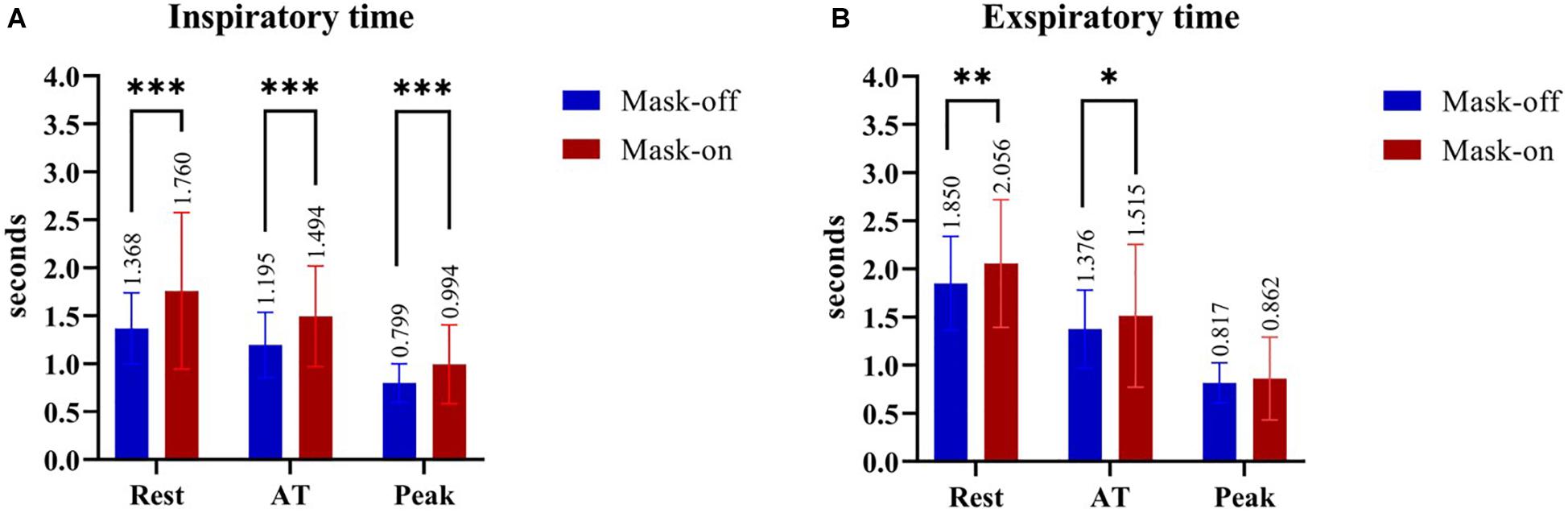
Figure 3. The comparison between mask-on and mask-off condition in the inspiratory time (A) and expiratory time (B) during different stages of the CPET, respectively. *P ≤ 0.05; ** P ≤ 0.01; ***P ≤ 0.001. AT, anaerobic threshold; CPET, cardiopulmonary exercise test.
Respiratory frequency and E of mask-on were lower than mask-off at each stage of CPET (p < 0.05), especially at peak exercise (Rfpeak: 33.8 ± 7.98 vs. 37.91 ± 6.72 b/min, p < 0.001;Epeak: 55.07 ± 17.28 vs. 66.46 ± 17.93 l/min, p < 0.001), and VT was significantly lower than mask-off just at peak exercise (1.66 ± 0.45 vs. 1.79 ± 0.5 l, p < 0.001). BR% of mask-on was higher than mask-off at all stages of CPET (p < 0.001). There was no significant difference between mask-off and mask-on in SPO2 (p > 0.05) (Table 4).
The result of pulmonary ventilation efficiency parameters showed that there were no significant differences in PetO2 and E/O2 between mask-off and mask-on during the rest period (p > 0.05), but PetO2 and E/O2 of mask-on during warm-up period to peak exercise period were lower than mask-off (p < 0.05). At all stages of CPET, PetCO2 of mask-on was higher than mask-off and E/CO2 was lower than mask-off (p < 0.05), but there was no significant difference in E/CO2 slope between them (p > 0.05) (Table 4).
Cardiovascular Reaction Parameters
The result of cardiovascular response parameters showed that O2/HR, OUES, and △O2/△W of mask-on was significantly lower than mask-off (O2peak/HR: 8.82 ± 2.6 vs. 9.51 ± 2.48 ml/beat, p< 0.001; OUES: 1641.2 ± 449.5 vs. 1914.4 ± 498.3 ml/min/l/min, p < 0.001; △O2/△W: 8.04 ± 1.03 vs. 8.55 ± 0.9 mlO2/W, p = 0.002), while HR, HRR, and systolic BP were significantly different at peak exercise (p < 0.05), and diastolic BP had no significant difference at different stages of CPET (p > 0.05) (Table 5).
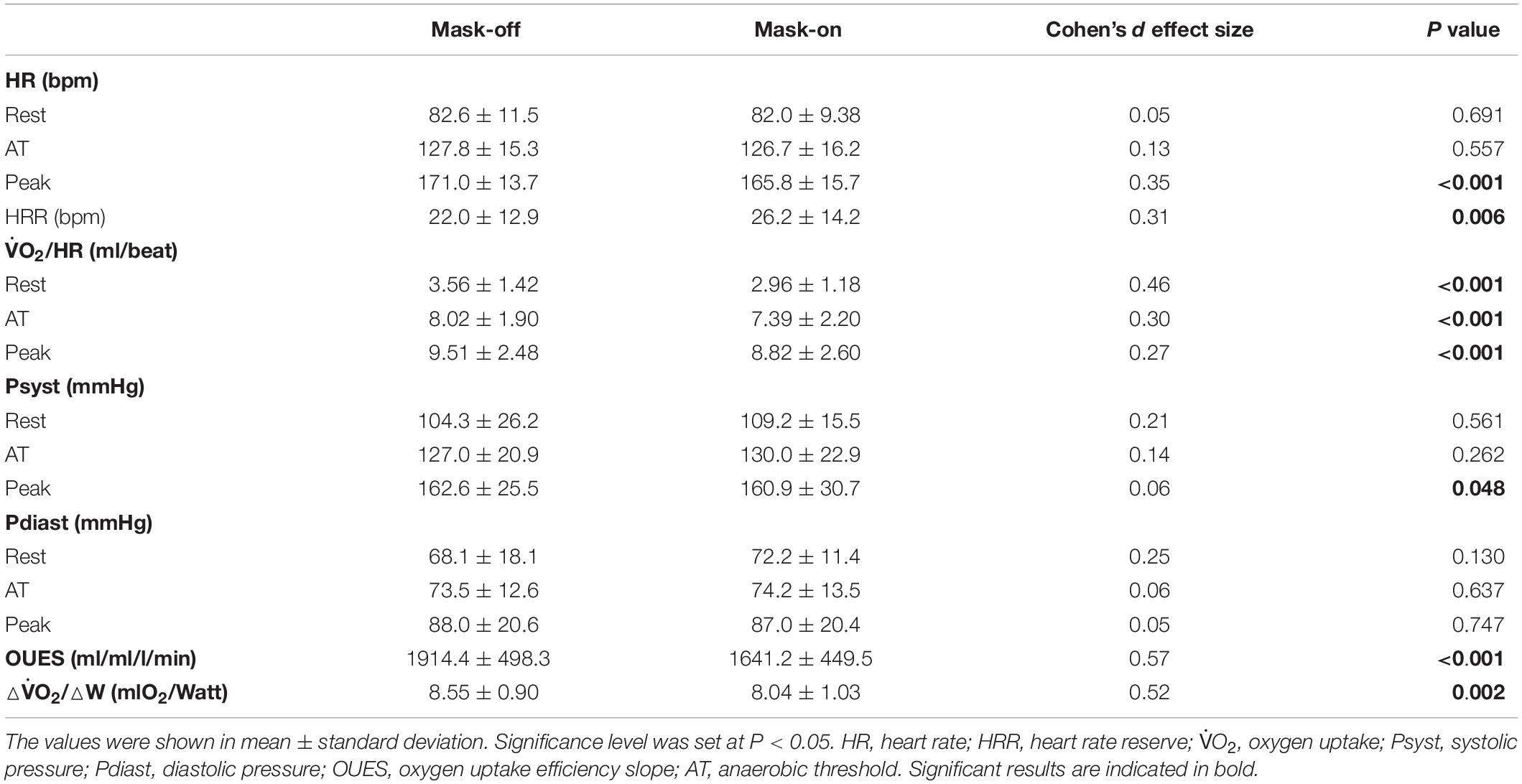
Table 5. The comparison of cardiovascular reaction parameters between mask-on and mask-off condition.
Adverse Event Reported
No adverse events such as hypoxemia, myocardial ischemia, arrhythmia, and hypoperfusion occurred in any of the subjects in this study.
Discussion
Mask could effectively prevent infectious respiratory diseases, and the role of the mask in COVID-19 has been confirmed (Dharmadhikari et al., 2012; Chu et al., 2020). This study selected surgical mask and investigated the physiological effects of masks on healthy people under exercise load through self-comparison. The result demonstrated that that mask had significant effects on cardiopulmonary function (including E, VT, Rf, BR%, CO2, PETO2, PETCO2, E/O2, E/CO2, O2/HR, OUES, and △O2/△W) and cardiopulmonary fitness or exercise endurance (such as O2peak and O2peak/kg), and lung function was significantly affected.
First, surgical masks influenced the performance in CPET. This research suggested that the exercise test time and a maximum power of healthy subjects wearing masks were lower than those without masks, and the dyspnea index was increased. In the study on 31 adults (Driver et al., 2021) cloth face masks led to a 14% reduction in exercise time and attributed to perceived discomfort (such as feeling increasingly short of breath and claustrophobic at higher exercise intensities) associated with mask-wearing. Therefore, masks could affect the exercise performance and subjective feelings of healthy subjects.
Second, surgical masks had influences on lung function. Both this study and Mapelli’s (Mapelli et al., 2021) study found out that after wearing masks, Ti and Te increased since rest period, especially Ti, which indirectly reflected that masks could increase the inspiratory and expiratory resistance of the oronasal airway. The increase of facial temperature and humidity during exercise could also cause moisture and deformation of the mask, which could further increase respiratory resistance. Different types of masks cause different respiratory resistance, which led to the greater the respiratory resistance, the larger the dead space, and the greater the influence on the ventilation function and ventilation efficiency (Jones et al., 1971). Studies had shown that after wearing N95 filter masks, the inspiratory and expiratory resistance increased by 0.43 and 0.23 mmH2O, respectively (Roberge et al., 2010a). An animal study measured the maximum speed of six horses in the treadmill exercise test, and then exercised on the treadmill at the maximum speeds of 50, 75, and 100%, respectively with and without masks. The results showed that compared with those without masks, the difference of peak inspiratory pressure between trachea and pharynx increased negatively, peak expiratory pressure between trachea and pharynx increased positively, and Rf was lower (p < 0.05) (Holcombe et al., 1996). The increase of respiratory resistance prolonged the breathing time to meet the ventilation needs, which led to the slowdown of Rf after wearing a mask. Meanwhile, the increase of respiratory resistance and the slowdown of Rf led to the decrease of VT, showing insufficient ventilation, resulting in the decrease of E and the increase of BR%. This study confirmed that Rf, VT, and E decreased and BR% increased after wearing surgical masks, especially in the peak period of exercise. Seo et al. (2017) tested nine healthy men wearing masks with different inspiratory resistances, and the results also showed that Rf and E decreased with the increase of inspiratory resistance. However, Roberge et al. studies20 healthy adult subjects walking on a flat plate at a speed of 5.6 km/h for 1 h with or without wearing surgical masks, and the results showed that wearing masks caused an increase in Rf by 1.6 beats/min (p = 0.02) (Roberge et al., 2012). It was also observed that the subjects walked at the same speed for 1 h while wearing N95 masks, and the Rf of the mask group increased by 1.4–2.4 beats/min (p < 0.05) compared with the control group (Kim et al., 2013). The exercise method used in these two studies was to walk on a flat plate at a constant speed, with limb muscles and even chest muscles participating in the exercise for a longer period. However, this study used cycle ergometer incremental exercise, with mainly lower limb muscles participating for a shorter time, so there were differences in breathing patterns between them, and individual differences of the subjects could also affect the results. In addition, in this study, although VT and E decreased after wearing surgical masks, they were all in the normal range, and SpO2 did not decrease during the whole exercise process, which did not cause the compensatory mechanism of the body. If the subjects exercised in high intensity for a longer time, it might cause compensatory acceleration of Rf (Qiu and Wang, 2012). According to the results of this study, the respiratory pattern change caused by wearing surgical masks was insufficient ventilation, which affected the ventilation function.
The increase of respiratory resistance after wearing masks would increase the work done by respiratory muscles and affected the gas exchange and ventilation efficiency. In this study, O2, CO2, PetO2, E/O2, and E/CO2 all decreased and PetCO2 increased after wearing surgical masks. The changes existed in the rest period or warm-up exercise and became more significant as exercise intensity increased. As inspiratory resistance increased, the inhaled oxygen concentration decreased, which led to the decrease of O2 and PetO2. E decreased more significantly than O2, so E/O2 decreased. The study showed that E/O2 could be decreased by 12–31% with the increase of inspiratory resistance (Caretti and Whitley, 1998). In addition, the expiratory resistance increased and the dead space increased, resulting in a decrease in CO2 and a higher PaCO2, showing a relative carbon dioxide retention performance (Holcombe et al., 1996). Umutlu et al. (2021) also indicated that O2, CO2, and E decreased significantly during aerobic exercise (p < 0.001). Because E decreased more significantly than CO2, so the decrease in E/CO2 was well proved in this study. However, due to the limited discharge of carbon dioxide, the concentration of carbon dioxide in the mask and inhaled increased (Roberge et al., 2010b; Smith et al., 2013). Therefore, this study observed that PetCO2 was higher when wearing surgical masks than mask-off (p < 0.001). Roberge et al. (2012) also found out that after wearing masks, the percutaneous carbon dioxide partial pressure increased by 2.17 mmHg (P = 0.0006), and a similar change existed when exercising with N95 mask (Kim et al., 2013; Goh et al., 2019). Epstein et al. (2021) found PetCO2 increased with the increase of exercise load after wearing N95 masks, and it increased by 8 mmHg at peak exercise. It could be seen that wearing masks presented pathophysiological changes similar to COPD, which would reduce ventilation efficiency, especially during high-intensity exercise. In this study, no hypoxemia occurred in healthy subjects, which was related to the strong compensatory ability of healthy people. However, for patients with respiratory diseases, such as COPD or heart failure, the above physiological changes might aggravate the condition of the patient (Hopkins et al., 2021). Therefore, such patients were required to be fully evaluated before exercising with masks.
Third, surgical masks influenced cardiopulmonary fitness and exercise endurance. Cardiopulmonary fitness has been listed as the fifth vital sign by AHA, which not only reflected exercise endurance but also was an effective index for disease occurrence risk and death risk (Ross et al., 2016). Maximum O2 was often used to evaluate cardiopulmonary fitness. The walking test (6 min) was a simple and easy method to evaluate cardiopulmonary fitness and exercise endurance. Person et al. (2018) randomly divided 44 healthy people into a mask-on and a mask-off group and conducted a 6 min walking test, respectively. The results showed that the 6 min walk distance, HR, and SpO2 did not change significantly, and only the dyspnea index increased significantly. The 6 min walking test was a kind of sub-maximal exercise test, which was not accurate enough to fully reflect the cardiopulmonary function and metabolism, however, CPET was more accurate. Through CPET, this study found out that O2 had decreased since the rest period, and O2peak was decreased by about 11% (p < 0.001). After wearing FFP2/N95 mask, O2peak could decrease by 13% (Fikenzer et al., 2020). In the study of Driver et al., cloth face masks led to a 29% decrease in O2max (p < 0.001) (Driver et al., 2021). Dressendorfer et al. (1977) showed that O2peak after wearing masks was 10–15% lower than the reference range, accompanied by a slight decrease in CO2 and RER. If the mask was removed before the peak exercise, both O2 and E could be significantly increased, and exercise could be maintained for at least 1 min. The increase of respiratory resistance decreased the concentration of inhaled oxygen, caused the respiratory muscles to do extra work, and increased oxygen consumption, which led to the changes in the above-mentioned lung function. In addition, the heat and humidity of the mask increased during exercise (Roberge et al., 2012; Scarano et al., 2020). All mentioned above could cause a decrease in O2, shorten the exercise time, and decreased the maximum power in exercise tests (Johnson, 2016). The AT was also an index reflecting the aerobic capacity of the body. A Japanese study of six young men showed that surgical masks did not affect the AT during treadmill exercise (Otsuka et al., 2020). In Egger’s research on athletes, surgical masks or N95 masks led to a reduction in O2max, but there was no significant difference in the AT, which might be related to the strong aerobic metabolism ability and cardiopulmonary fitness of athletes (Egger et al., 2021). However, the AT and O2@AT/O2max pre % were significantly different in this study, suggesting that AT appeared ahead of schedule. Relative carbon dioxide retention after wearing masks led to anaerobic metabolism ahead of schedule. Therefore, wearing masks would affect cardiopulmonary fitness and reduce exercise endurance. There might be safety risks for patients with cardiopulmonary disease, and such patients needed to be fully evaluated.
Fourth, surgical masks influenced cardiovascular function. In general, the blood flow is redistributed during exercise, and the blood flow of the myocardium increased to ensure the blood pumping function of the heart. The excitation of the sympathetic nerve led to the enhancement of cardiac systolic function, the increase of stroke volume (SV), HR, CO, and BP. After wearing masks, the airway resistance increased, the negative pressure of the chest increased when inhaling, and the blood flow increased as well, increasing cardiac preload (Cooke et al., 2006). On the other hand, the contraction of peripheral vessels and the increase of cardiac afterload during exercise could cause the compensatory increase of SV, HR, and CO, and at the same time increased the extra work of the heart, which led to the decrease of work efficiency and oxygen utilization capacity of the heart (Cheyne et al., 2020). Umutlu et al. (2021) conducted CPET and walk test on 14 sedentary volunteers (all on a treadmill), showing that HR systolic BP and diastolic BP increased significantly after wearing masks (p < 0.01). Lässing et al. (2020) studied the changes in cardiopulmonary function during constant power test with surgical masks and found that HRpeak increased significantly (p < 0.01), SV and CO increased slightly (p > 0.05), and arteriovenous oxygen difference (avDO2) decreased significantly (p = 0.02). This study suggested that the decrease of O2 after wearing masks was mainly related to the decrease of avDO2 (O2 = CO × avDO2), while the change of lung function caused by wearing a mask could lead to the decrease of avDO2; thus, the decrease of O2 was mainly related to the change of lung function. However, Fikenzer et al. (2020) adopted the step-by-step incremental protocol for CPET. The results showed that the HRpeak of exercise decreased when wearing surgical masks and FFP2/N95 masks, but it was more significant when wearing surgical masks (p < 0.05), and the SV and CO were slightly higher than those without masks (p > 0.05). Similarly, in this study, the HRpeak of healthy volunteers decreased when exercising with surgical masks (p < 0.05), which might be related to the different CPET protocols and the short exercise time of CPET. There might be an obvious compensatory increase in HR for long-term high-intensity exercise, which needed further study. In addition, surgical masks led to a significant decrease in O2/HR, OUES (ratio of O2 to the logarithm of ventilation volume), and △O2/△W in this study, which was mainly related to the decrease of O2, indicating that wearing masks caused the decrease of oxygen transport capacity of heart and oxygen utilization capacity of the body in healthy people.
To summarize, surgical masks had a certain influence on the heart function of healthy people during exercise, which was mainly due to the limitation of lung function. For patients with heart diseases, this influence might be enlarged due to the damage of heart compensatory function.
Limitations
First, all the subjects included in this study were healthy people of low age, and the results could not reflect the influence of surgical masks on exercise cardiopulmonary function of middle-aged and elderly people and patients with cardiopulmonary disease. Second, this study did not combine blood gas analysis to accurately evaluate metabolism, which could more effectively reflect aerobic and anaerobic metabolism in vivo by measuring arterial oxygen partial pressure, carbon dioxide partial pressure, and lactic acid value.
Conclusion
Wearing surgical masks during aerobic exercise showed certain negative impacts on cardiopulmonary function, especially during high-intensity exercise in healthy young subjects. These results provide an important recommendation for wearing a mask at a pandemic during exercises of varying intensity. Future research should focus on the response of wearing masks in patients with related cardiopulmonary diseases.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by the Research Ethics Committee Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GZ and ML assisted in the subject recruitment, data collection, data analysis, and writing. MZ, XC, JY, SZ, and AY assisted with the data collection and data analysis. YZ, QL, and JL assisted with the data analysis. LG and HO assisted with the study design, data analysis, and manuscript editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Caretti, D. M., and Whitley, J. A. (1998). Exercise performance during inspiratory resistance breathing under exhaustive constant load work. Ergonomics 41, 501–511. doi: 10.1080/001401398186973
Chan, J. F., Yuan, S., Zhang, A. J., Poon, V. K., Chan, C. C., Lee, A. C., et al. (2020). Surgical masks Partition Reduces the Risk of Non-contact Transmission in a Golden Syrian Hamster Model for Coronavirus Disease 2019 (COVID-19). Clin. Infect. Dis. 71, 2139–2149. doi: 10.1093/cid/ciaa644
Chandrasekaran, B., and Fernandes, S. (2020). “Exercise with facemask; Are we handling a devil’s sword?” - A physiological hypothesis. Med. Hypotheses 144:110002. doi: 10.1016/j.mehy.2020.110002
Cheyne, W. S., Harper, M. I., Gelinas, J. C., Sasso, J. P., and Eves, N. D. (2020). Mechanical cardiopulmonary interactions during exercise in health and disease. J. Appl. Physiol. 128, 1271–1279. doi: 10.1152/japplphysiol.00339.2019
Chu, D. K., Akl, E. A., Duda, S., Solo, K., Yaacoub, S., and Schünemann, H. J. (2020). Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 395, 1973–1987.
Cooke, W. H., Lurie, K. G., Rohrer, M. J., and Convertino, V. A. (2006). Human autonomic and cerebrovascular responses to inspiratory impedance. J. Trauma 60, 1275–1283. doi: 10.1097/01.ta.0000221348.82115.a2
Costa, D. C., Santi, G. L., Crescêncio, J. C., Seabra, L. P., Carvalho, E. E., Papa, V., et al. (2015). Use of the Wasserman equation in optimization of the duration of the power ramp in a cardiopulmonary exercise test: a study of Brazilian men. Braz. J. Med. Biol. Res. 48, 1136–1144. doi: 10.1590/1414-431x20154692
Dharmadhikari, A. S., Mphahlele, M., Stoltz, A., Venter, K., Mathebula, R., Masotla, T., et al. (2012). Surgical face masks worn by patients with multidrug-resistant tuberculosis: impact on infectivity of air on a hospital ward. Am. J. Respir. Crit. Care Med. 185, 1104–1109. doi: 10.1164/rccm.201107-1190oc
Dougherty, R. J., Lindheimer, J. B., Stegner, A. J., Van Riper, S., Okonkwo, O. C., and Cook, D. B. (2018). An Objective Method to Accurately Measure Cardiorespiratory Fitness in Older Adults Who Cannot Satisfy Widely Used Oxygen Consumption Criteria. J. Alzheimers Dis. 61, 601–611. doi: 10.3233/jad-170576
Dressendorfer, R. H., Wade, C. E., and Bernauer, E. M. (1977). Combined effects of breathing resistance and hyperoxia on aerobic work tolerance. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 42, 444–448. doi: 10.1152/jappl.1977.42.3.444
Driver, S., Reynolds, M., Brown, K., Vingren, J. L., Hill, D. W., Bennett, M., et al. (2021). Effects of wearing a cloth face mask on performance, physiological and perceptual responses during a graded treadmill running exercise test. Br. J. Sports Med. [Epub ahead of print].
Egger, F., Blumenauer, D., Fischer, P., Venhorst, A., Kulenthiran, S., Bewarder, Y., et al. (2021). Effects of face masks on performance and cardiorespiratory response in well-trained athletes. Clin. Res. Cardiol. 1–8. [Epub ahead of print].
Eikenberry, S. E., Mancuso, M., Iboi, E., Phan, T., Eikenberry, K., Kuang, Y., et al. (2020). To mask or not to mask: modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Model 5, 293–308. doi: 10.1016/j.idm.2020.04.001
Epstein, D., Korytny, A., Isenberg, Y., Marcusohn, E., Zukermann, R., Bishop, B., et al. (2021). Return to training in the COVID-19 era: the physiological effects of face masks during exercise. Scand. J. Med. Sci. Sports 31, 70–75. doi: 10.1111/sms.13832
Fikenzer, S., Uhe, T., Lavall, D., Rudolph, U., Falz, R., Busse, M., et al. (2020). Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin. Res. Cardiol. 109, 1522–1530. doi: 10.1007/s00392-020-01704-y
Fink, J. B., Ehrmann, S., Li, J., Dailey, P., McKiernan, P., Darquenne, C., et al. (2020). Reducing aerosol-related risk of transmission in the Era of COVID-19: an interim guidance endorsed by the International Society of Aerosols in Medicine. J. Aerosol Med. Pulm. Drug Deliv. 33, 300–304. doi: 10.1089/jamp.2020.1615
Goh, D. Y. T., Mun, M. W., Lee, W. L. J., Teoh, O. H., and Rajgor, D. D. (2019). A randomised clinical trial to evaluate the safety, fit, comfort of a novel N95 mask in children. Sci. Rep. 9:18952.
Holcombe, S. J., Beard, W. L., and Hinchcliff, K. W. (1996). Effect of a mask and pneumotachograph on tracheal and nasopharyngeal pressures, respiratory frequency, and ventilation in horses. Am. J. Vet. Res. 57, 250–253.
Hopkins, S. R., Dominelli, P. B., Davis, C. K., Guenette, J. A., Luks, A. M., Molgat-Seon, Y., et al. (2021). Face Masks and the Cardiorespiratory Response to Physical Activity in Health and Disease. Ann. Am. Thorac. Soc. 18, 399–407. doi: 10.1513/annalsats.202008-990cme
Indu, P., Rameshkumar, M. R., Arunagirinathan, N., Al-Dhabi, N. A., Valan Arasu, M., and Ignacimuthu, S. (2020). Raltegravir, Indinavir, Tipranavir, Dolutegravir, and Etravirine against main protease and RNA-dependent RNA polymerase of SARS-CoV-2: a molecular docking and drug repurposing approach. J. Infect. Public Health 13, 1856–1861. doi: 10.1016/j.jiph.2020.10.015
Islam, M. S., Rahman, K. M., Sun, Y., Qureshi, M. O., Abdi, I., Chughtai, A. A., et al. (2020). Current knowledge of COVID-19 and infection prevention and control strategies in healthcare settings: a global analysis. Infect. Control Hosp. Epidemiol. 41, 1196–1206. doi: 10.1017/ice.2020.237
Johnson, A. T. (2016). Respirator masks protect health but impact performance: a review. J. Biol. Eng. 10:4.
Jones, N. L., Levine, G. B., Robertson, D. G., and Epstein, S. W. (1971). The effect of added dead space on the pulmonary response to exercise. Respiration 28, 389–398. doi: 10.1159/000192827
Kim, J. H., Benson, S. M., and Roberge, R. J. (2013). Pulmonary and heart rate responses to wearing N95 filtering facepiece respirators. Am. J. Infect. Control 41, 24–27. doi: 10.1016/j.ajic.2012.02.037
Lässing, J., Falz, R., Pökel, C., Fikenzer, S., Laufs, U., Schulze, A., et al. (2020). Effects of surgical face masks on cardiopulmonary parameters during steady state exercise. Sci. Rep. 10:22363.
Lee, H. P., and Wang de, Y. (2011). Objective assessment of increase in breathing resistance of N95 respirators on human subjects. Ann. Occup. Hyg. 55, 917–921.
Liang, M., Gao, L., Cheng, C., Zhou, Q., Uy, J. P., Heiner, K., et al. (2020). Efficacy of face mask in preventing respiratory virus transmission: a systematic review and meta-analysis. Travel Med. Infect. Dis. 36:101751. doi: 10.1016/j.tmaid.2020.101751
Mapelli, M., Salvioni, E., De Martino, F., Mattavelli, I., Gugliandolo, P., Vignati, C., et al. (2021). You can leave your mask on”: effects on cardiopulmonary parameters of different airway protection masks at rest and during maximal exercise. Eur. Respir. J. [Epub ahead of print].
Otsuka, A., Komagata, J., and Sakamoto, Y. (2020). Wearing a surgical masks does not affect the anaerobic threshold during pedaling exercise. J. Hum. Sport Exerc. 17:4.
Person, E., Lemercier, C., Royer, A., and Reychler, G. (2018). [Effect of a surgical masks on six minute walking distance]. Rev. Mal. Respir. 35, 264–268.
Qiu, M., and Wang, S. (2012). Effect of respirator resistance on tolerant capacity during graded load exercise. J. Huazhong Univ. Sci. Technolog. Med. Sci. 32, 434–437. doi: 10.1007/s11596-012-0075-x
Ramos-Campo, D. J., Pérez-Piñero, S., Muñoz-Carrillo, J. C., López-Román, F. J., García-Sánchez, E., and Ávila-Gandía, V. (2021). Acute Effects of Surgical and FFP2 Face Masks on Physiological Responses and Strength Performance in Persons with Sarcopenia. Biology 10:213. doi: 10.3390/biology10030213
Roberge, R. J., Bayer, E., Powell, J. B., Coca, A., Roberge, M. R., and Benson, S. M. (2010a). Effect of exhaled moisture on breathing resistance of N95 filtering facepiece respirators. Ann. Occup. Hyg. 54, 671–677.
Roberge, R. J., Coca, A., Williams, W. J., Powell, J. B., and Palmiero, A. J. (2010b). Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir. Care 55, 569–577.
Roberge, R. J., Kim, J. H., and Benson, S. M. (2012). Absence of consequential changes in physiological, thermal and subjective responses from wearing a surgical mask. Respir. Physiol. Neurobiol. 181, 29–35. doi: 10.1016/j.resp.2012.01.010
Ross, R., Blair, S. N., Arena, R., Church, T. S., Després, J. P., Franklin, B. A., et al. (2016). Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement From the American Heart Association. Circulation 134, e653–e699.
Scarano, A., Inchingolo, F., and Lorusso, F. (2020). Facial skin temperature and discomfort when wearing protective face masks: thermal infrared imaging evaluation and hands moving the mask. Int. J. Environ. Res. Public Health 17:4624. doi: 10.3390/ijerph17134624
Seo, Y., Vaughan, J., Quinn, T. D., Followay, B., Roberge, R., Glickman, E. L., et al. (2017). The effect of inspiratory resistance on exercise performance and perception in moderate normobaric hypoxia. High Alt. Med. Biol. 18, 417–424. doi: 10.1089/ham.2017.0103
Shaw, K., Butcher, S., Ko, J., Zello, G. A., and Chilibeck, P. D. (2020). Wearing of Cloth or Disposable Surgical Face Masks has no Effect on Vigorous Exercise Performance in Healthy Individuals. Int. J. Environ. Res. Public Health 17:8110. doi: 10.3390/ijerph17218110
Smith, C. L., Whitelaw, J. L., and Davies, B. (2013). Carbon dioxide rebreathing in respiratory protective devices: influence of speech and work rate in full-face masks. Ergonomics 56, 781–790. doi: 10.1080/00140139.2013.777128
Tirupathi, R., Bharathidasan, K., Palabindala, V., Salim, S. A., and Al-Tawfiq, J. A. (2020). Comprehensive review of mask utility and challenges during the COVID-19 pandemic. Infez. Med. 28, 57–63.
Umutlu, G., Acar, N. E., Sinar, D. S., Akarsu, G., and Güven, E. (2021). Yildirim İ. COVID-19 and physical activity in sedentary individuals: differences in metabolic, cardiovascular, and respiratory responses during aerobic exercise performed with and without a surgical face masks. J. Sports Med. Phys. Fitness [Epub ahead of print].
Keywords: surgical masks, cardiopulmonary fitness, exercise endurance, ventilation, end-tidal carbon dioxide partial pressure
Citation: Zhang G, Li M, Zheng M, Cai X, Yang J, Zhang S, Yilifate A, Zheng Y, Lin Q, Liang J, Guo L and Ou H (2021) Effect of Surgical Masks on Cardiopulmonary Function in Healthy Young Subjects: A Crossover Study. Front. Physiol. 12:710573. doi: 10.3389/fphys.2021.710573
Received: 22 May 2021; Accepted: 26 July 2021;
Published: 10 September 2021.
Edited by:
Elisabetta Salvioni, Monzino Cardiology Center (IRCCS), ItalyReviewed by:
Susanna Sciomer, Sapienza University of Rome, ItalyCosimo Carriere, University of Trieste, Italy
Copyright © 2021 Zhang, Li, Zheng, Cai, Yang, Zhang, Yilifate, Zheng, Lin, Liang, Guo and Ou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lan Guo, Z3VvbGFuMTk5M0AxMjYuY29t; Haining Ou, b3VoYWluaW5nQGd6aG11LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Guolin Zhang1†
Guolin Zhang1† Qiang Lin
Qiang Lin Haining Ou
Haining Ou