Abstract
Background: The primary phase time constant of pulmonary oxygen uptake kinetics (τp) during submaximal efforts is longer in middle-aged people with type 2 diabetes (T2D), partly due to limitations in oxygen supply to active muscles. This study examined if a high-intensity “priming” exercise (PE) would speed τp during a subsequent high-intensity cycling exercise in T2D due to enhanced oxygen delivery.
Methods: Eleven (4 women) middle-aged individuals with type 2 diabetes and 11 (4 women) non-diabetic controls completed four separate cycling bouts each starting at an ‘unloaded’ baseline of 10 W and transitioning to a high-intensity constant-load. Two of the four cycling bouts were preceded by priming exercise. The dynamics of pulmonary and muscle deoxygenation (i.e. deoxygenated haemoglobin and myoglobin concentration [HHb + Mb]), were calculated from breath-by-breath and near-infrared spectroscopy data at the vastus lateralis, respectively.
Results: At baseline τp, was slower (p < 0.001) in the type 2 diabetes group (48 ± 6 s) compared to the control group (34 ± 2 s) but priming exercise significantly reduced τp (p < 0.001) in type 2 diabetes (32 ± 6 s) so that post priming exercise it was not different compared with controls (34 ± 3 s). Priming exercise reduced the amplitude of the slow component (As) in both groups (type 2 diabetes: 0.26 ± 0.11 to 0.16 ± 0.07 L/min; control: 0.33 ± 0.13 to 0.25 ± 0.14 L/min, p < 0.001), while [HHb + Mb] kinetics remained unchanged.
Conclusion: These results suggest that in middle-aged men and women with T2D, PE speeds τp likely by a better matching of O2 delivery to utilisation and reduces the As during a subsequent high-intensity exercise.
1 Introduction
Type 2 diabetes (T2D) is a major chronic condition with a concerning rapidly increasing global prevalence. Importantly, men and women with T2D demonstrate a consistent impairment in cardiorespiratory capacity reflected by a decreased peak oxygen uptake (peak) (Green et al., 2015), that is an independent predictor of all-cause mortality (Wei et al., 2000). In addition, at the onset of moderate-intensity exercise a slowed primary phase time constant of pulmonary oxygen uptake () kinetics (τp) is observed in young and middle-aged people with T2D (Bauer et al., 2007; Mac Ananey et al., 2011; O'Connor et al., 2012; Kiely et al., 2015; O'Connor et al., 2015). Similarly, recent evidence suggests that compared with controls, in middle-aged individuals with T2D τp is also slowed during exercise transitions from a moderate-intensity baseline to high-intensity (i.e work-to-work transitions) (Gildea et al., 2021b). While τp is a well-established key determinant of exercise tolerance (Jones and Poole, 2005; Goulding et al., 2021), the mechanisms for the constrained τp in T2D remain to be elucidated, but accumulating evidence suggests that impairments in oxygen supply to the active musculature (Padilla et al., 2006; MacAnaney et al., 2011; Kiely et al., 2014) and a subsequent mismatch of local O2 delivery to muscle (Bauer et al., 2007; Gildea et al., 2019; Rocha et al., 2019; Gildea et al., 2021b) play an important role.
The impediments in kinetics in T2D are also apparent during high-intensity exercise transitions initiated from rest or ‘unloaded’ baseline, with Brandenburg et al. (1999) showing a significantly slower mean response time (MRT) of the kinetics in females with T2D compared with BMI-matched controls. Nevertheless, Mac Ananey et al. (2011) showed a non-significant tendency for a slower MRT and τp (∼13% and ∼5% respectively) during high-intensity cycling transitions initiated from static rest in females with T2D of similar characteristics, compared with BMI-matched controls (Mac Ananey et al., 2011). Noteworthy, when transitions are initiated from static (instead of ‘unloaded’) rest, τp has been shown to be ∼15% longer when the time delay is not constrained (Whipp et al., 1982) as was the case therein (Mac Ananey et al., 2011), potentially influencing their findings.
Importantly, abrupt or sudden transitions to high-intensity activity (i.e. running, cycling or stair climbing) from rest or very light activity are akin to those in daily life (such as commuting to work), so, there is a need to examine interventions that may enhance the dynamic response during these exercise transitions in T2D. In this regard, studies in healthy active individuals presenting with an initial fast τp show that an acute prior bout of heavy-intensity “priming” exercise (PE) does not alter τp during subsequent high-intensity upright cycling exercise initiated from rest (Burnley et al., 2000; Burnley et al., 2001; Burnley et al., 2002a; Koppo and Bouckaert, 2002; Sahlin et al., 2005). This is likely because PE appears to facilitate muscle oxygen delivery rather than specific metabolic pathways and in these healthy active individuals τp seems limited by the later (i.e. intracellular energetics) (Gerbino et al., 1996; Sahlin et al., 2005; Jones et al., 2006). However, PE accelerates the MRT of the overall dynamic response in these healthy participants typically through an increase in the primary phase amplitude of the ( Ap) and/or reducing the slow component amplitude of the , the latter being potentially related to the reduced requirement for type II muscle fiber activation after PE (DiMenna et al., 2008). On the contrary, when kinetics are further slowed as a direct consequence of impaired O2 delivery and reduced perfusion pressure to active muscles, as is observed during supine or prone high-intensity exercise (Rossiter et al., 2001; Jones et al., 2006; Goulding et al., 2017), PE accelerates τp in the respective subsequent bouts of high-intensity exercise, possibly due to improved blood flow distribution, and/or reduced muscle fatigue to active muscles (DiMenna et al., 2010).
Thus, considering that O2 supply to the muscle seems to be constrained in individuals with T2D, and high-intensity priming exercise has been proposed as an intervention that can augment the delivery of O2 to the muscle, we tested the hypothesis that PE would reduce τp in a subsequent bout of high-intensity exercise initiated from unloaded exercise in this population. Given that alterations exist in muscle fiber type in the T2D skeletal muscle, with individuals with T2D possessing larger proportions of type II and lower proportions of type I fibers than controls (Marin et al., 1994), we also hypothesized that in individuals with T2D PE would reduce the As. To shed light on contributions of muscle fractional O2 extraction to any PE-induced changes in kinetics, this study measured rates of muscle deoxygenation (i.e., deoxygenated haemoglobin and myoglobin, [HHb + Mb]) using near-infrared spectroscopy (NIRS). In addition, the age of participants was limited to less than 60 years to control for the potential confounding effects of age on the T2D-induced effects on exercise tolerance (Wilkerson et al., 2011; O'Connor et al., 2015).
2 Methods
2.1 Participants and recruitment
A total of 22 individuals, 11 with T2D (7 men/4 women) and 11 healthy controls (7 men/4 women) volunteered and provided written informed consent to take part in this study (Table 1). Recruitment for the control group was undertaken from the general population, whilst individuals with T2D were recruited from outpatient diabetes clinics of two hospitals in Dublin (i.e. St. Vincent’s University Hospital and St. Columcille’s Hospital). Four of the women participating in this study were premenopausal (2 T2D and 2 Control) and four were postmenopausal (2 T2D and 2 Control) not undergoing hormone replacement therapy. All participants were non-smokers (not smoking during the previous 12 months) and physically inactive [(≤150 min week−1 of moderate-intensity (<ventilatory threshold, VT) exercise in the preceding 6 months] (McKay et al., 2022). The latter status was confirmed by participants wearing RT3 triaxial accelerometers (Stayhealthy Inc., CA) over a 5-day period (Table 1) (Rowlands et al., 2004). Participants’ time since diagnosis of T2D was between 2 and 10 years (mean ± SD = 4.5 ± 3.2 yrs) and had HbA1c levels below 10%. In addition, exclusion criteria included the use of β-blockers or insulin, clinical evidence of liver or renal disease, if they suffered from persistent proteinuria (urine protein >200 mg/dl) or had high creatinine levels (suggestive of renal disease, which can alter exercise performance); autonomic insufficiency/dysfunction, symmetrical neuropathy, abnormal cardiac function, or evidence of ischaemic heart disease. Regarding medication, two individuals in the control group were on statins whilst participants with T2D were treated with either oral (n = 9) and/or subcutaneous (n = 2) hypoglycaemic agents (only metformin, n = 5; metformin and sulphonylurea, n = 1; SGLT-2 inhibitors, n = 1; GLP-1, n = 1), as well as antihypertensive medication (ACE inhibitor, n = 3; ARBs, n = 2; CCBs, n = 3) and statins (n = 6). The study received ethical approval from both Trinity College Dublin (TCD), and St Vincent’s Healthcare research ethics committees.
TABLE 1
| Controls | T2D | p-value | |
|---|---|---|---|
| n | 11 | 11 | |
| Physical characteristics | |||
| Sex (male, female), n | 7, 4 | 7, 4 | |
| Age, yr | 40 (18) | 43 (14) | 0.21 |
| Stature, m | 1.70 ± 0.08 | 1.71 ± 0.09 | 0.77 |
| BMI, kg/m2 | 30.9 ± 3.9 | 30.8 ± 4.6 | 0.97 |
| Body Mass, kg | 88 (17) | 92 (33) | 0.97 |
| Fat layer VL, mm | 7.9 (7.4) | 6.0 (2.5) | 0.25 |
| HbA1c, % | 5.1 ± 0.1* | 7.4 ± 1.7 | 0.02 |
| FPG, mmol/L | 4.3 ± 0.7* | 8.6 ± 3.5 | 0.01 |
| Time since diagnosis, yr | 4.5 ± 3.2 | ||
| , L/min | 2.50 ± 0.52* | 1.94 ± 0.49 | 0.02 |
| , mL.kg−1.min−1 | 28.4 ± 6.6* | 21.3 ± 3.59 | 0.01 |
| POpeak, W | 199 ± 53* | 149 ± 43 | 0.03 |
| Habitual physical activity | |||
| Inactive, h/day | 19.4 ± 1.6 | 18.4 ± 0.3 | 0.19 |
| Light, h/day | 3.7 ± 1.3 | 5.0 ± 0.3 | 0.06 |
| MVPA, h/day | 0.86 ± 0.60 | 0.69 ± 0.29 | 0.56 |
Physical characteristics, peak exercise values, and activity levels.
Data are means ± SD, for variables that were normally distributed and median with interquartile range in parentheses for variables that showed significant skewness and were not normally distributed in one or both groups. n, no. of participants. BMI, body mass index; VL, vastus lateralis; HbA1c, glycosylated haemoglobin; FPG, fasting plasma glucose; MVPA, moderate-to-vigorous physical activity; , oxygen uptake; PO, power output. *Significantly different from T2D (p < 0.05).
2.2 Experimental procedures
2.2.1 Overview
Upon successful completion of a treadmill stress test (Bruce protocol) at St Columcille’s Hospital, participants attended the testing laboratories on two separate occasions. The participants in the control group completed all tests in the University’s human performance laboratory whilst participants with T2D did so in the exercise testing facility at St Columcille's Hospital. Visit one consisted of participants completing a maximal cycling test to exhaustion to measure peak oxygen uptake (peak). In visit 2, participants completed four exercise transitions from a baseline of 10 W (i.e. unloaded) to high-intensity, of which two were preceded by PE. Cycling tests were completed in the upright position on an Excalibur Sport cycle ergometer (Lode B.V, Groningen, Netherlands). Participants were asked to avoid the consumption of caffeine, alcohol and non-prescribed nutritional supplements together with any arduous physical activities during the 24 h preceding each visit. Menstrual cycle was controlled for when scheduling the visits of the premenopausal participants in this study, with testing taking place during the mid-follicular phase of their menstrual cycle (days 5–12, self-determined).
2.2.2 Visit 1: Maximal cycling test to exhaustion
All participants completed a ramp incremental cycling test to volitional exhaustion with an initial work rate of 10 W for 2 min (i.e., ‘unloaded’ cycling) followed by a progressive increase in power output of 10–25 W/min (based on each individual’s physical activity level). Participants were required to maintain a constant cadence throughout the test, self-selecting a pedalling rate between 60 and 75 rpm. Test termination occurred when participants had a cadence reduction of 10 rpm for more than 5s. At the end of the test peak work rate was determined as the highest power output achieved, whilst was determined as the highest value (15-s average) attained. The V-slope method was used to determine VT (Beaver et al., 1986).
2.2.3 Visit 2: Four cycling exercise transitions
All participants completed four identical 9-min cycling exercise bouts transitioning from an ‘unloaded’ power output of 10 W (3 min) to a constant-load of 50% delta (50%Δ) (6 min). The latter intensity was determined from the results of the maximal cycling test by adding the 50% difference between the power outputs at and VT to the power output at VT. All participants completed the four bouts of exercise in the same order. Two of the bouts (bouts 1 and 3) were carried out without PE (50%Δ unprimed) and two bouts (bouts 2 and 4) were completed preceded by PE (50%Δ primed) (Figure 1). The unprimed 50%Δ bouts were used as PE. A resting period of 12 min was used between the first and second bouts, and the third and fourth bouts; whilst a 45–60 min seated rest period was used between the second and third bouts. The longer resting period was important to ensure that participant’s physiological parameters returned to a baseline state so as not to affect subsequent kinetics parameters. This was determined by measuring these parameters in a subgroup of 11 participants with T2D, albeit employing a single high-intensity transition which is consistent with previous reports in healthy active individuals (Burnley et al., 2006). Participants’ gas exchange/ventilatory variables, muscle oxygenation/deoxygenation and heart rate (HR) data were measured continuously throughout each exercise bout.
FIGURE 1
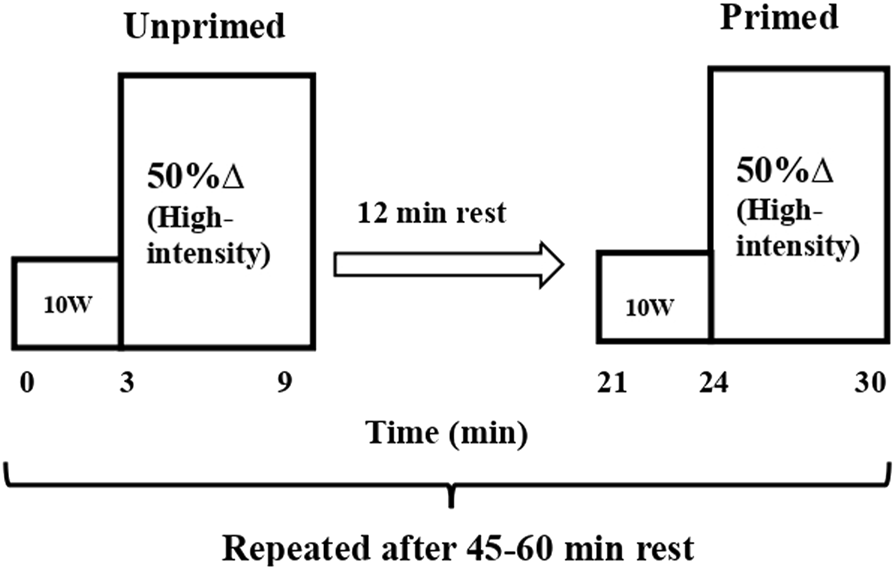
Schematic representation of the protocol. Unprimed and primed cycling step transitions performed at high-intensity cycling exercise (Δ50%; the sum of the power output at VT and 50% of the difference between the power output at VT and peak). All step transitions, each lasting 6 min, were preceded by 3 min of cycling at 10 W (i.e. ‘baseline’ cycling). Unprimed and primed transitions were separated by 12 min of passive rest. The 2 step transitions (unprimed and primed) were repeated following 45–60 min of passive rest within the same laboratory visit.
2.3 Measures
2.3.1 Pulmonary gas exchange and heart rate
Breath-by-breath data was continuously obtained during exercise by participants wearing a facemask that was connected to a metabolic gas analysis system (Innocor, Innovision A/S, Odense, Denmark). Parameters analysed were oxygen consumption, carbon dioxide production, respiratory exchange ratio and minute ventilation. Calibration of equipment was undertaken before each use according to the recommendations of the manufacturer. In addition, calibration of the system’s oxygen and photoacoustic sensors is undertaken periodically (every 6–12 months) by the manufacturer. A heart rate monitor was used to measure HR at 5 s intervals (Polar S610i, Polar Ltd., Finland).
2.3.2 Muscle deoxygenation and tissue oxygenation index
Muscle oxygenation (O2Hb + Mb), deoxygenation (HHb + Mb) and tissue oxygenation index (TOI) data were acquired using a continuous wave NIRS system (Niro 200NX; Hamamatsu, Japan). This device uses the spatially resolved spectroscopy (SRS) technique and modified Beer-Lambert (MBL) principle. Detailed information about this technique and its application during exercise is available elsewhere (Ferrari et al., 2011). In the present study this measurement was undertaken in the vastus lateralis (VL) muscle of the participant’s right quadriceps given the VL is the primary locomotor muscle during leg cycling (Laplaud et al., 2006; Okushima et al., 2016). In order to ensure good quality signals, necessary skin preparation was undertaken involving shaving any hair present and cleaning the area with alcohol. After the skin was dried, the probes in their rubber holder were securely positioned on the muscle, between 10 and 16 cm above the femoral condyle using transparent adhesive tape. A dark elastic bandage was also used to further protect the probes from external light and movement. The depth of the area being measured is approximately one-half the distance between the emitter and the receiver probes (∼1.5 cm). Therefore, ultrasound measurements of the skin and adipose tissue at the probe location were taken in all participants using the B-mode of a 2D ultrasound (Zonare Ultra Smart Cart, Software version 4.7, United States) to ensure that data collected was representative of the muscle tissue. This was confirmed with all participants having less than 1.5 cm of adipose tissue thickness at the probe location.
2.4 Data analysis
2.4.1 Oxygen uptake kinetics
The linear interpolation method was used to estimate second by second values from the breath-by-breath data for each transition. Data was then aligned to ensure that the start of the exercise bout was time 0. To achieve a single smoothed averaged response for each participant, data were ensemble- and time-averaged into 5s bins. A biexponential (Eq. 1) function was then used to fit these responses:
In the above function (t) is (absolute) at a given time (t); baseline represents the mean in the last 30 s of the “unloaded” cycling; Amplitudes (A), time delays (TD) and time constants (τ) for primary (p) and slow component (s) phases are represented as Ap, As, TDp, TDs, τp, and τs respectively. Time constant is the time that takes to reach 63% of the amplitude of the corresponding phase. F1 and F2 are two conditional expressions that ensure the fitting of the phase is restricted to the period at and beyond the time delay associated with that phase. The initial 20 s of the response data from the start of the cycling bout (i.e. cardiodynamic phase) were omitted but the TDp was allowed to vary freely so that the fit could be optimised (Murias et al., 2011). A monoexponential curve was fitted to calculate mean response time (MRT) and ascertain the overall kinetics during high-intensity cycling irrespective of the different phases. A weighted nonlinear least-squares regression (TableCurve 2D, Systat, United States) was used to fit all response data. During the initial fit of the model, only data points within the 95% prediction interval were included. The average of the final 30 s of the was calculated to represent the end of exercise response (i.e. End A). The latter was then used to calculate the absolute As that is ( baseline + Ap) subtracted from End A, while TDs was constrained. The As was also calculated relative to the entire response (As/(Ap + As)). The end of exercise gain, representing the functional gain of the overall response, was also calculated by subtracting baseline from End A and normalised to the difference in power outputs between the unloaded and high-intensity cycling.
2.4.2 [HHb + Mb] kinetics and tissue oxygenation index
The muscle deoxygenation (i.e. Δ[HHb + Mb]) response during high-intensity cycling was collected at a frequency of 1 Hz, was ensemble-averaged and time averaged into 5 s bins for each participant and was fitted using the same biexponential function (Eq. 1). TD was determined by visually inspecting a consistent rise from the pre-transition level since the Δ[HHb + Mb] is known to present a TD at the start of exercise before increasing in an exponential manner. This phenomenon has been suggested to reflect a close association between local oxygen delivery and muscular oxygen consumption (DeLorey et al., 2003; Grassi et al., 2003). Muscle deoxygenation data was therefore fitted from the TD onwards. The sum of TD and t was used to determine the effective response time (τ′Δ[HHb + Mb]) representing the time course for the primary phase of the Δ [HHb + Mb] response. Baseline TOI was calculated as the 30 s preceding each transition, and the End TOI as the final 30 s of exercise. ΔTOI was calculated by subtracting baseline TOI from End TOI.
2.4.3 Heart rate kinetics
The heart rate data was fitted using a monoexponential function (Eq. 2) with the fitting window constrained to TDs:
In the above function HR baseline represents the mean HR in the last 30 s of the “unloaded” cycling.
2.5 Statistical analysis
The Shapiro-Wilk’s test was used to assess the normal distribution of the data. Between group comparisons of participants’ characteristics and peak performance data were undertaken using an unpaired Student’s t-test (for parametric data) or a Mann-Whitney U test (for non-parametric data). A two-way mixed model ANOVA [condition (unprimed, primed) x diabetes status (T2D, Control)] and the post hoc Tukey test were used to analyse all the dynamic response data for oxygen uptake, heart rate and muscle deoxygenation as well as TOI responses. p < 0.05 was used to determine statistical significance. Results from parametric analyses are presented as mean ± SD whereas non-parametric results are presented using median and interquartile ranges.
3 Results
3.1 Participant characteristics
Unsurprisingly, individuals with T2D had significantly higher HbA1c and fasting plasma glucose levels than healthy individuals (Table 1). Importantly, the T2D and control groups were matched according to sex distribution, age, BMI, body mass and activity levels.
3.2 Peak exercise responses
Individuals with T2D had significantly lower absolute peak, peak normalised to body mass, and peak power output than healthy individuals (Table 1).
3.3 Effect of priming exercise on oxygen uptake kinetics
The primed and unprimed dynamic response characteristics of at high-intensity cycling exercise transitions for each group are presented in Table 2. The responses for a representative individual with T2D and a healthy control are presented in Figure 2. Individual τp and As responses are provided in Figure 3. The unprimed τp and MRT were significantly longer in individuals with T2D compared with healthy controls (p < 0.001 for both parameters). PE significantly reduced MRT (p < 0.001) in the T2D and control groups; however, no group difference was present (p = 0.053) during the subsequent exercise transition (diabetes status × condition interaction, p < 0.001). PE also elicited a reduction in τp in individuals with T2D (p < 0.001) but not in the healthy controls (p = 0.98) so that τp was not different between groups after PE (diabetes status × condition interaction, p < 0.001). In addition, subsequent to PE, As was reduced while baseline was increased in both the T2D and healthy control groups (condition effect, p < 0.001 for both parameters).
TABLE 2
| Unprimed | Primed | |||
|---|---|---|---|---|
| Controls | Type 2 diabetes | Controls | Type 2 diabetes | |
| n | 11 | 11 | 11 | 11 |
| Baseline L/min | 1.02 ± 0.23 | 0.90 ± 0.16 | 1.18 ± 0.23* | 0.96 ± 0.20* |
| Ap, L/min | 1.04 ± 0.41 | 0.79 ± 0.28 | 1.09 ± 0.38 | 0.80 ± 0.29 |
| τp, s | 34 ± 2† | 48 ± 6 | 34 ± 3 | 32 ± 6* |
| As, L/min | 0.33 ± 0.13 | 0.26 ± 0.11 | 0.25 ± 0.14* | 0.16 ± 0.07* |
| As, % | 24.5 ± 7.0 | 25.6 ± 10.5 | 18.5 ± 7.0* | 17.6 ± 6.6* |
| TDs, s | 121 ± 24 | 138 ± 35 | 130 ± 26 | 139 ± 40 |
| end A, L/min | 2.39 ± 0.61† | 1.95 ± 0.40 | 2.52 ± 0.59† | 1.93 ± 0.45 |
| MRT, s | 67 ± 5† | 81 ± 13 | 57 ± 4* | 64 ± 9* |
| End-exercise gain, mL.min−1.W−1 | 9.7 ± 1.6 | 10.1 ± 1.7 | 9.5 ± 1.2 | 9.2 ± 1.8 |
Dynamic response characteristics of oxygen uptake () at high-intensity cycling exercise transitions.
Data are means ± SD; n = no. of participants. A, amplitude; τ, time constant; end A, steady-state oxygen uptake () response; TD, time delay; p, primary phase; s slow component phase. *p < 0.05 vs. unprimed within the same diabetes status group (i.e. within controls or within Type 2 diabetes). †p < 0.05 vs. participants with type 2 diabetes within the same condition (i.e. within unprimed or primed).
FIGURE 2
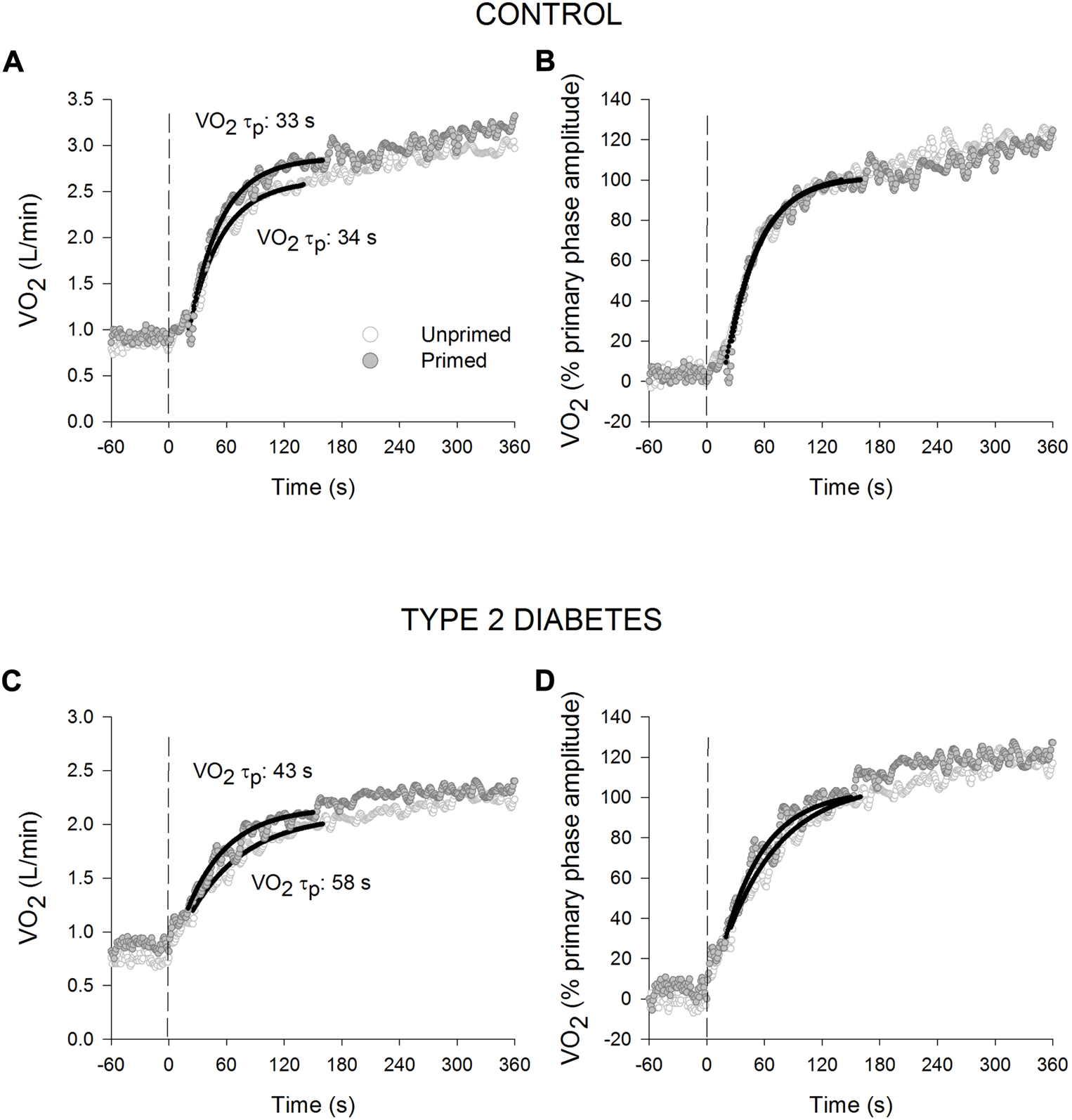
Oxygen uptake () responses for a representative healthy control ((A): absolute values; (B): normalised to the % primary phase amplitude) and an individual with type 2 diabetes ((C): absolute values; (D): normalised to the % primary phase amplitude) during high-intensity cycling transitions without priming exercise (open circles) and with priming exercise (solid circles). The vertical line illustrates the abrupt transition to the higher work rate. The continuous lines of best fit illustrate the primary phase of the oxygen uptake () response. Note the relatively slower response of the primary phase of the response in the unprimed compared with the primed bout in T2D.
FIGURE 3
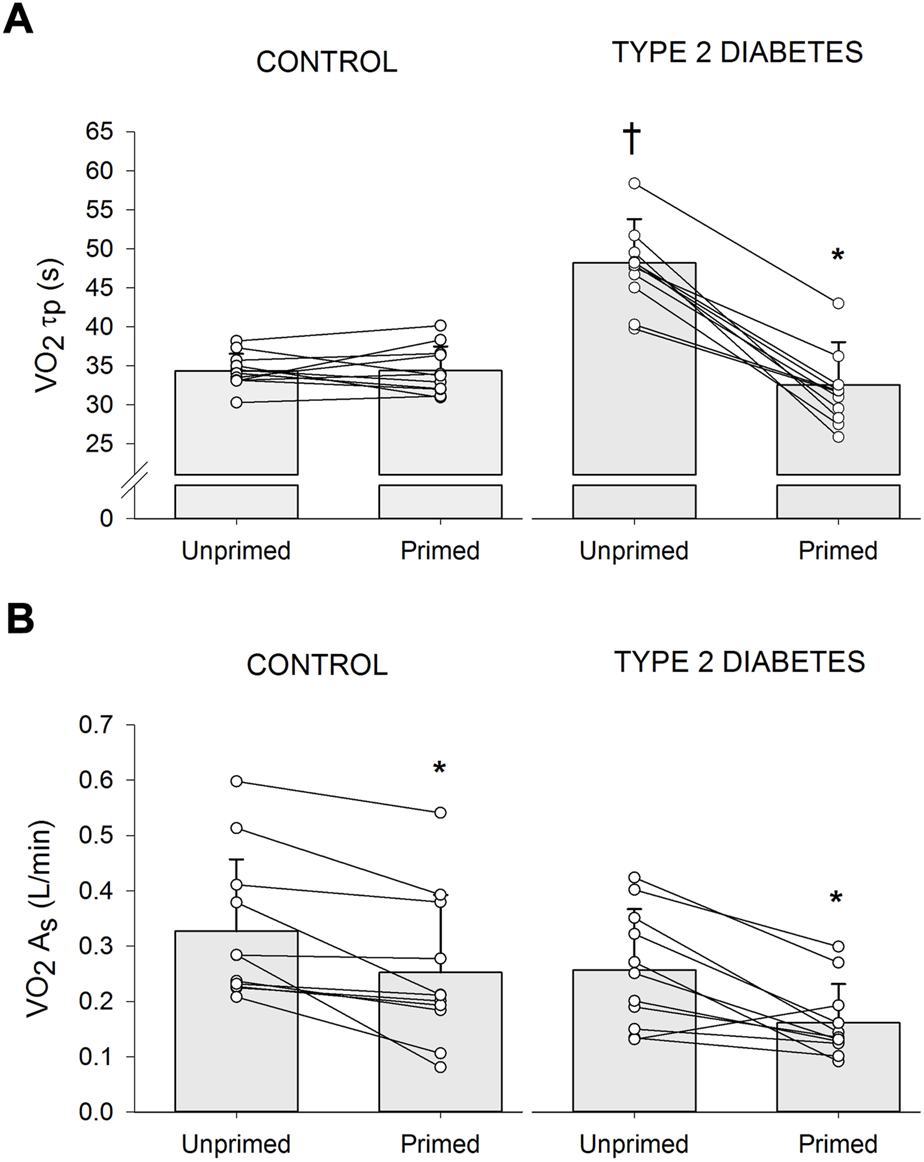
Individual and mean ± SD (bar graph) changes in time constant of the primary phase of oxygen uptake (τp) (A) and amplitude of the slow component ( As) (B) in participants with type 2 diabetes (n = 11) and healthy controls (n = 11) during high-intensity cycling transitions without priming exercise (unprimed) and with priming exercise (primed). *p < 0.05 vs. unprimed within the same diabetes status group (i.e., within controls or within Type 2 diabetes). †p < 0.05 vs. healthy controls within the same condition (i.e., within unprimed or primed).
3.4 Effect of priming exercise on Δ [HHb + Mb] kinetics and tissue oxygenation index responses
Table 3 presents the parameter estimates for Δ[HHb + Mb] kinetics and TOI responses whereas Figure 4 shows the Δ[HHb + Mb] responses for representative individuals. No statistical group difference was observed in the unprimed parameter estimates. PE resulted in significantly elevated levels of baseline Δ [HHb + Mb] in T2D (p < 0.001) and a tendency for higher levels in controls (p = 0.08) (group × condition interaction, p = 0.04). Participants with T2D showed a larger ratio of the modelled amplitudes of Δ [HHb + Mb]/Δ than controls (main effect of group, p = 0.01). None of the remaining [HHb + Mb] kinetics parameters were affected by PE. Estimates of baseline TOI as well as ΔTOI were higher during the primed bout in individuals with T2D (p < 0.01 for both) but not controls (p = 0.7 and 0.9 respectively) (group × condition interaction, p = 0.02 and 0.01 respectively).
TABLE 3
| Unprimed | Primed | |||
|---|---|---|---|---|
| Controls | Type 2 diabetes | Controls | Type 2 diabetes | |
| n | 11 | 11 | 11 | 11 |
| Baseline Δ [HHb + Mb], μM*cm | −50 ± 36 | −61 ± 62 | −33 ± 39 | −16 ± 50* |
| Δ [HHb + Mb] Ap, μM*cm | 90 ± 84 | 135 ± 75 | 87 ± 87 | 141 ± 87 |
| Δ [HHb + Mb] TDp, s | 10 ± 2 | 10 ± 2 | 10 ± 2 | 11 ± 2 |
| Δ [HHb + Mb] τp, s | 13 ± 9 | 12 ± 5 | 13 ± 7 | 12 ± 4 |
| Δ [HHb + Mb] τ′, s | 23 ± 9 | 22 ± 5 | 23 ± 7 | 23 ± 4 |
| Primary phase Δ [HHb + Mb]/Δ As, μM*cm (L/min) | 83 ± 63† | 170 ± 70 | 83 ± 74† | 171 ± 95 |
| Δ [HHb + Mb] As, μM*cm | 20 ± 17 | 21 ± 16 | 21 ± 17 | 18 ± 16 |
| Baseline TOI, % | 75 ± 6 | 70 ± 5 | 76 ± 6 | 74 ± 5* |
| Δ TOI % | 7.4 ± 4.8 | 6.5 ± 4.5 | 7.4 ± 5.5 | 9.3 ± 6.0* |
Dynamic response characteristics of Δ [HHb + Mb] and TOI during high-intensity cycling exercise transitions.
Values are means ± SD; n = no. of participants. A, amplitude; τ, time constant; TD, time delay; p, primary phase; s slow component phase; τ, time constant; τ′, effective response time (τ + TD); [HHb + Mb], deoxygenated haemoglobin and myoglobin concentration; TOI, tissue oxygenation index; oxygen uptake. *p < 0.05 vs. unprimed within the same diabetes status group (i.e. within controls or within Type 2 diabetes). †p < 0.05 vs. participants with type 2 diabetes within the same condition (i.e. within unprimed or primed).
FIGURE 4
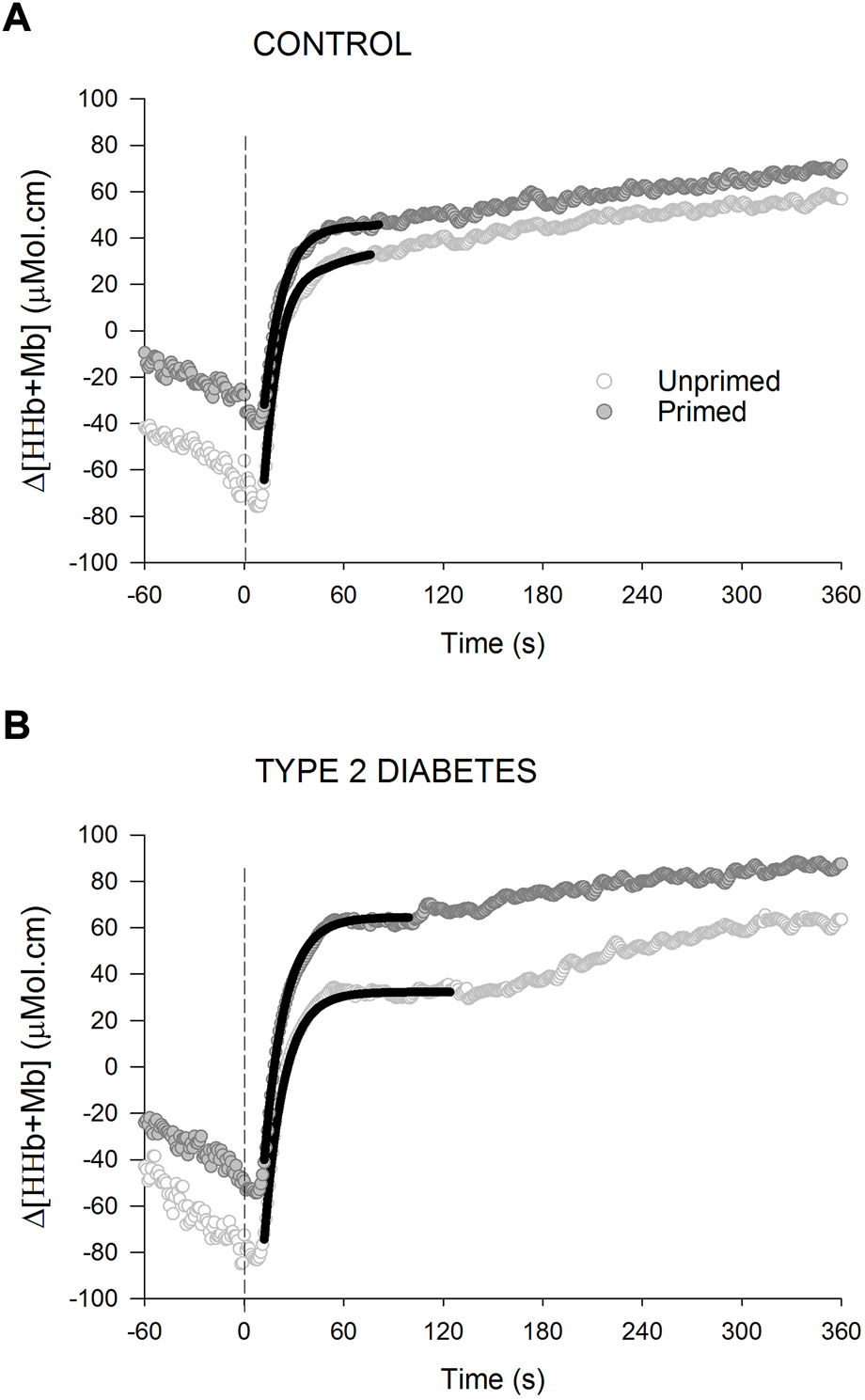
Changes in deoxygenated hemoglobin and myoglobin concentration [Δ (HHb + Mb)] for a representative healthy control (A) and an individual with type 2 diabetes (B) during high-intensity cycling transitions without priming exercise (open circles) and with priming exercise (solid circles). The vertical line illustrates the abrupt transition to the higher work rate. The continuous black lines of best fit illustrate the primary phase of the Δ (HHb + Mb) response. Note the time constant of the primary phase of the Δ [HHb + Mb] response is not affected by prior priming exercise in any of the 2 groups.
3.5 Effect of priming exercise on heart rate kinetics
The HR τ was significantly longer in individuals with T2D compared with healthy controls (main effect of group, p < 0.01), but PE did not affect HR τ in any of the groups (T2D unprimed: 56 ± 3 s, T2D primed: 55 ± 2 s; controls unprimed: 51 ± 3 s, controls primed: 50 ± 5 s). Baseline HR was higher in T2D (main effect of group, p = 0.04) and subsequent to PE it increased (main effect of condition, p < 0.001) in both groups (T2D unprimed: 109 ± 14 beats. min−1, T2D primed: 118 ± 13 beats. min−1; controls unprimed: 98 ± 9 beats. min−1, controls primed: 106 ± 10 beats. min−1). End-exercise HR was not different among groups, but it increased following PE (main effect of condition, p = 0.017) in both groups (T2D unprimed: 157 ± 12 beats. min−1, T2D primed: 159 ± 13 beats. min−1; controls unprimed: 156 ± 16 beats. min−1, controls primed: 162 ± 15 beats. min−1).
4 Discussion
In agreement with our primary hypothesis, this study presents for the first-time evidence that in middle-aged individuals with T2D PE reduces τp during high-intensity exercise initiated from unloaded exercise without changes in the dynamic response of Δ [HHb + Mb]. In addition, consistent with our second hypothesis, PE significantly reduced the As during the high-intensity exercise bout. Together, these priming exercise-induced effects rendered a reduction in the MRT response.
4.1 Effect of priming exercise on oxygen uptake τp
In the present study, τp responses observed during high-intensity upright cycling transitions were significantly amplified in individuals with T2D (48 s) than controls (32 s) leading to a longer MRT in T2D compared with controls. This is consistent with previous results from Brandenburg et al. (1999) who showed a significantly longer MRT during high-intensity cycling transitions in females with T2D compared with BMI-matched controls (Brandenburg et al., 1999), although Mac Ananey et al. (2011) only observed a tendency for longer kinetics in females with T2D of similar characteristics (Mac Ananey et al., 2011). Importantly, we have recently reported in a subgroup of participants who took part in the present study, that T2D slows τp during transitions to both, moderate-intensity (Rocha et al., 2019; Rocha et al., 2020) as well as high-intensity work-to-work (Gildea et al., 2021b) transitions. Hence, the present study extends the findings of a blunted kinetics response to moderate and high-intensity work-to-work exercise to that of high-intensity exercise initiated from unloaded exercise, at least in middle-aged individuals with T2D when compared with carefully matched healthy controls.
The performance of a PE bout herein resulted in a subsequent significant reduction in this τp among individuals with T2D but not in those without, bringing the primed τp in T2D in line with the control group. These findings suggest that when the dynamic response of is impaired by limitations in O2 delivery, as is the case in T2D (Bauer et al., 2007; MacAnaney et al., 2011; Kiely et al., 2014), PE speeds τp in the subsequent exercise bout. This notion is supported by studies that have explored these responses when exercising in the prone and supine positions (Rossiter et al., 2001; Jones et al., 2006; Goulding et al., 2017), thus, compromising exercising muscle perfusion pressure and O2 delivery (Egaña et al., 2010; Egaña et al., 2013). For instance, an investigation where healthy participants performed high-intensity cycling bouts with and without PE in the supine posture, Jones et al. (2006) observed that PE induced a 37% reduction (p < 0.05) in τp (38 s ± 18 s vs. 24 ± 9, s) in the subsequent bout, that was in line with that reported in the unprimed upright posture (Jones et al., 2006). Thus, findings from the current study expand the recently reported findings by our group of a significant speeding in τp following priming exercise during moderate-intensity (Rocha et al., 2019; Rocha et al., 2020) as well as high-intensity work-to-work exercise (Gildea et al., 2021b) to that of high-intensity exercise initiated from light exercise in individuals with T2D who are younger than 60 years of age.
The notion that priming exercise enhanced O2 supply in the subsequent exercise transition in T2D is evidenced by an increased TOI which suggests an increase in O2 availability, likely mediated by a PE-induced increased vasodilation and muscle blood flow at the beginning of the subsequent exercise (Gerbino et al., 1996). However, given that the NIRS-derived overall muscle deoxygenation kinetics and/or amplitude were not affected by PE herein, there is the possibility that the priming-induced reduction in τp in T2D was also partly mediated by an improved intracellular O2 utilization, likely mediated by the upregulation of rate-limiting mitochondrial oxidative enzymes (Gurd et al., 2006; Gurd et al., 2009) and elevated mitochondrial calcium concentrations (Wüst and Stienen, 2018). On the other hand, the fact that HR kinetics were not altered following PE suggests that central mechanisms (i.e. quicker delivery) did not influence the priming response.
4.2 Effect of priming exercise on oxygen uptake slow component
In the present study, PE significantly reduced both τp, and As during the high-intensity transition in participants with T2D. However, in the control group, although PE reduced the As subsequently shortening the overall MRT of the response, τp remained unaffected. These findings in control individuals are consistent with the current evidence on the influence of PE on subsequent transitions to heavy/severe-intensity upright cycling exercise initiated from an unloaded baseline in healthy participants (Burnley et al., 2000; Burnley et al., 2001; Scheuermann et al., 2001; Burnley et al., 2002a; Burnley et al., 2002b; Fukuba et al., 2002; Burnley et al., 2006; Jones et al., 2006; Goulding et al., 2017).
The priming-induced reduction in the slow component of the present study can likely be attributed to alterations in motor unit recruitment patterns. For instance, our group has recently shown (Gildea et al., 2021b) a priming-induced reduction in iEMG between the end of exercise and the time of the onset of As (ΔiEMGend-TDs) upon transition to a subsequent high-intensity cycling bout, albeit from an elevated baseline (work-to-work), concomitant with a significant reduction in the As. Although, herein, iEMG was not measured, it is possible that PE induced a decreased requirement for additional type II muscle fiber activation during the subsequent high-intensity cycling bout, thereby reducing the associated cost of muscle fiber activation (DiMenna et al., 2008). By reducing dependency on these less efficient muscle fibers, the increase in sustained metabolic acidosis, a likely mediator of [PCr] and slow components, can be slowed (Poole et al., 1988; Poole et al., 1991; Barstow et al., 1996; Rossiter et al., 2002; Krustrup et al., 2004). Alternatively, PE could facilitate an increased and more homogenous muscle perfusion within the active musculature, which is supported by the observed elevated baseline TOI during the primed bout in T2D herein. Consequently, the reliance on [PCr] degradation and glycogenolysis would be reduced, attenuating the rate of fatigue development and thus, delaying motor unit recruitment (DiMenna et al., 2010). In addition, this altered muscle activation response to priming exercise concomitant with the elevated TOI is consistent with the ‘oxygen-conforming’ effect, which has been demonstrated under involuntary and voluntary small muscle activation (Fitzpatrick et al., 1996; Drouin et al., 2022), although the mechanisms governing the oxygen-conforming response remain to be elucidated.
The observed PE-induced reduction in the As during high-intensity cycling in T2D, is all the more pertinent given individuals with T2D possess a 2-fold increase in type IIb fibers (Mogensen et al., 2007), demonstrate attenuated motor unit firing patterns in the VL compared with healthy controls (Watanabe et al., 2012; Watanabe et al., 2013) and tend to have lower dissociating capacity of myoglobin at intensities above VT (Miyamoto et al., 2020). Nevertheless, it is important to note that not all studies support the association between neuromuscular activation and the slow component (Scheuermann et al., 2001; Garland et al., 2006; Cannon et al., 2007), and this is possibly due to the variability associated with measurements and normalization of iEMG.
With this new physiological insight of impaired kinetics during high-intensity exercise transitions in T2D that are affected by limitations in O2 delivery, future studies should investigate if exercise training mitigates these impairments. This will be practically relevant as high-intensity exercise transitions replicate metabolic transitions akin to those in daily life such as initiating sudden transitions to rapid walking, running, or stair climbing. While recent studies have demonstrated that time-efficient high-intensity interval training as well as longer-duration moderate-intensity continuous exercise training interventions seem effective in enhancing τp during moderate-intensity transitions (Green et al., 2020; Gildea et al., 2021a) as well as high-intensity work-to-work transitions (Gildea et al., 2022) in T2D, new studies should explore if these exercise training interventions of different doses can influence the kinetics response during high-intensity transitions.
5 Limitations
Our results are limited to middle-aged mixed groups of men and women, hence, further studies should explore sex- and/or age-related differences in these outcomes. Even if our protocol did not allow block randomization, the sequence of the unprimed and primed exercise transitions was the same for all participants; hence, this likely has a minor impact on the interpretation of the current findings.
6 Conclusion
The present study showed that a preceding high-intensity exercise (i.e. warm-up) or priming exercise accelerated the overall MRT of the dynamic response during high-intensity transitions in middle-aged individuals with T2D. This finding was attributed to a speeding of the primary phase time constant of and a reduction in the amplitude of the slow component while PE did not affect the dynamic response of muscle deoxygenation. Thus, in the presence of the likely diminished vasomotor responses in T2D, it is likely that undertaking a prior high-intensity exercise bout resulted in a more appropriate distribution of blood flow within the working muscle microvasculature, serving to alleviate the metabolic debacle to maintain .
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Faculty of Health Science Research Ethics Committee, Trinity College Dublin and St Vincent’s Healthcare Ethics and Medical Research Committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
JR, NG, DO’S, SG and ME conceived and designed the research and analyzed data. JR and NG conducted experiments and collected all participant data. NG and ME drafted the paper. All authors interpreted data and contributed to the writing of the final paper. All authors contributed to the article and approved the submitted version.
Funding
This publication has emanated from research conducted with the financial support of the Health Research Board (Grant No HRA_POR/2073/274).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
BarstowT. J.JonesA. M.NguyenP. H.CasaburiR. (1996). Influence of muscle fiber type and pedal frequency on oxygen uptake kinetics of heavy exercise. J. Appl. Physiol.81, 1642–1650. 10.1152/jappl.1996.81.4.1642
2
BauerT. A.ReuschJ. E.LeviM.RegensteinerJ. G. (2007). Skeletal muscle deoxygenation after the onset of moderate exercise suggests slowed microvascular blood flow kinetics in type 2 diabetes. Diabetes Care30, 2880–2885. 10.2337/dc07-0843
3
BeaverW. L.WassermanK.WhippB. J. (1986). A new method for detecting anaerobic threshold by gas exchange. J. Appl. Physiol.60, 2020–2027. 10.1152/jappl.1986.60.6.2020
4
BrandenburgS. L.ReuschJ. E.BauerT. A.JeffersB. W.HiattW. R.RegensteinerJ. G. (1999). Effects of exercise training on oxygen uptake kinetic responses in women with type 2 diabetes. Diabetes Care22, 1640–1646. 10.2337/diacare.22.10.1640
5
BurnleyM.DoustJ. H.BallD.JonesA. M. (2002a1985). Effects of prior heavy exercise on VO(2) kinetics during heavy exercise are related to changes in muscle activity. J. Appl. Physiol.93, 167–174. 10.1152/japplphysiol.01217.2001
6
BurnleyM.DoustJ. H.CarterH.JonesA. M. (2001). Effects of prior exercise and recovery duration on oxygen uptake kinetics during heavy exercise in humans. Exp. Physiol.86, 417–425. 10.1113/eph8602122
7
BurnleyM.DoustJ. H.JonesA. M. (2002b). Effects of prior heavy exercise, prior sprint exercise and passive warming on oxygen uptake kinetics during heavy exercise in humans. Eur. J. Appl. Physiol.87, 424–432. 10.1007/s00421-002-0647-8
8
BurnleyM.DoustJ. H.JonesA. M. (2006). Time required for the restoration of normal heavy exercise VO2 kinetics following prior heavy exercise. J. Appl. Physiol.101, 1320–1327. 10.1152/japplphysiol.00475.2006
9
BurnleyM.JonesA. M.CarterH.DoustJ. H. (2000). Effects of prior heavy exercise on phase II pulmonary oxygen uptake kinetics during heavy exercise. J. Appl. Physiol.89, 1387–1396. 10.1152/jappl.2000.89.4.1387
10
CannonD. T.KolkhorstF. W.CiprianiD. J. (2007). Electromyographic data do not support a progressive recruitment of muscle fibers during exercise exhibiting a VO2 slow component. J. Physiol. Anthropol.26, 541–546. 10.2114/jpa2.26.541
11
DeloreyD. S.KowalchukJ. M.PatersonD. H. (2003). Relationship between pulmonary O2 uptake kinetics and muscle deoxygenation during moderate-intensity exercise. J. Appl. Physiol.95, 113–120. 10.1152/japplphysiol.00956.2002
12
DimennaF. J.WilkersonD. P.BurnleyM.BaileyS. J.JonesA. M. (2010). Priming exercise speeds pulmonary O2 uptake kinetics during supine "work-to-work" high-intensity cycle exercise. J. Appl. Physiol.108, 283–292. 10.1152/japplphysiol.01047.2009
13
DimennaF. J.WilkersonD. P.BurnleyM.JonesA. M. (2008). Influence of priming exercise on pulmonary O2 uptake kinetics during transitions to high-intensity exercise from an elevated baseline. J. Appl. Physiol.105, 538–546. 10.1152/japplphysiol.90357.2008
14
DrouinP. J.ForbesS. P. A.LiuT.LewL. A.Mcgarity-ShipleyE.TschakovskyM. E. (2022). Muscle contraction force conforms to muscle oxygenation during constant-activation voluntary forearm exercise. Exp. Physiol.107 (11), 1360–1374. 10.1113/ep090576
15
EgañaM.ColumbD.O'donnellS. (2013). Effect of low recumbent angle on cycling performance, fatigue, and V O(2) kinetics. Med. Sci. Sports Exerc.45, 663–673. 10.1249/MSS.0b013e318279a9f2
16
EgañaM.RyanK.WarmingtonS. A.GreenS. (2010). Effect of body tilt angle on fatigue and EMG activities in lower limbs during cycling. Eur. J. Appl. Physiol.108, 649–656. 10.1007/s00421-009-1254-8
17
FerrariM.MuthalibM.QuaresimaV. (2011). The use of near-infrared spectroscopy in understanding skeletal muscle physiology: Recent developments. Philos. Trans. A Math. Phys. Eng. Sci.369, 4577–4590. 10.1098/rsta.2011.0230
18
FitzpatrickR.TaylorJ. L.MccloskeyD. I. (1996). Effects of arterial perfusion pressure on force production in working human hand muscles. J. Physiol.495 (3), 885–891. 10.1113/jphysiol.1996.sp021640
19
FukubaY.HayashiN.KogaS.YoshidaT. (2002). VO(2) kinetics in heavy exercise is not altered by prior exercise with a different muscle group. J. Appl. Physiol.92, 2467–2474. 10.1152/japplphysiol.00207.2001
20
GarlandS. W.WangW.WardS. A. (2006). Indices of electromyographic activity and the "slow" component of oxygen uptake kinetics during high-intensity knee-extension exercise in humans. Eur. J. Appl. Physiol.97, 413–423. 10.1007/s00421-006-0185-x
21
GerbinoA.WardS. A.WhippB. J. (1996). Effects of prior exercise on pulmonary gas-exchange kinetics during high-intensity exercise in humans. J. Appl. Physiol.80, 99–107. 10.1152/jappl.1996.80.1.99
22
GildeaN.McdermottA.RochaJ.CrognaleD.NevinA.O'sheaD.et al (2022). Low-volume HIIT and MICT speed VO(2) kinetics during high-intensity "work-to-work" cycling with a similar time-course in type 2 diabetes. J. Appl. Physiol.133, 273–287. 10.1152/japplphysiol.00148.2022
23
GildeaN.McdermottA.RochaJ.O'sheaD.GreenS.EgañaM. (2021a). Time-course of Vo(2) kinetics responses during moderate-intensity exercise subsequent to HIIT versus moderate-intensity continuous training in type 2 diabetes. J. Appl. Physiol.130, 1646–1659. 10.1152/japplphysiol.00952.2020
24
GildeaN.RochaJ.McdermottA.O'sheaD.GreenS.EgañaM. (2019). Influence of type 2 diabetes on muscle deoxygenation during ramp incremental cycle exercise. Respir. Physiol. Neurobiol.269, 103258. 10.1016/j.resp.2019.103258
25
GildeaN.RochaJ.O'sheaD.GreenS.EgañaM. (2021b). Priming exercise accelerates pulmonary oxygen uptake kinetics during "work-to-work" cycle exercise in middle-aged individuals with type 2 diabetes. Eur. J. Appl. Physiol.121, 409–423. 10.1007/s00421-020-04518-y
26
GouldingR. P.RocheD. M.MarwoodS. (2017). Prior exercise speeds pulmonary oxygen uptake kinetics and increases critical power during supine but not upright cycling. Exp. Physiol.102, 1158–1176. 10.1113/ep086304
27
GouldingR. P.RossiterH. B.MarwoodS.FergusonC. (2021). Bioenergetic mechanisms linking V˙O2 kinetics and exercise tolerance. Exerc. Sport Sci. Rev.49, 274–283. 10.1249/jes.0000000000000267
28
GrassiB.PogliaghiS.RampichiniS.QuaresimaV.FerrariM.MarconiC.et al (2003). Muscle oxygenation and pulmonary gas exchange kinetics during cycling exercise on-transitions in humans. J. Appl. Physiol.95, 149–158. 10.1152/japplphysiol.00695.2002
29
GreenS.EgañaM.BaldiJ. C.LambertsR.RegensteinerJ. G. (2015). Cardiovascular control during exercise in type 2 diabetes mellitus. J. Diabetes Res.2015, 654204. 10.1155/2015/654204
30
GreenS.KielyC.O'connorE.GildeaN.O'sheaD.EgañaM. (2020). Effects of exercise training and sex on dynamic responses of O(2) uptake in type 2 diabetes. Appl. Physiol. Nutr. Metab.45, 865–874. 10.1139/apnm-2019-0636
31
GurdB. J.PetersS. J.HeigenhauserG. J.LeblancP. J.DohertyT. J.PatersonD. H.et al (2009). Prior heavy exercise elevates pyruvate dehydrogenase activity and muscle oxygenation and speeds O2 uptake kinetics during moderate exercise in older adults. Am. J. Physiol. Regul. Integr. Comp. Physiol.297, R877–R884. 10.1152/ajpregu.90848.2008
32
GurdB. J.PetersS. J.HeigenhauserG. J.LeblancP. J.DohertyT. J.PatersonD. H.et al (2006). Prior heavy exercise elevates pyruvate dehydrogenase activity and speeds O2 uptake kinetics during subsequent moderate-intensity exercise in healthy young adults. J. Physiol.577, 985–996. 10.1113/jphysiol.2006.112706
33
JonesA. M.BergerN. J.WilkersonD. P.RobertsC. L. (2006). Effects of "priming" exercise on pulmonary O2 uptake and muscle deoxygenation kinetics during heavy-intensity cycle exercise in the supine and upright positions. J. Appl. Physiol.101, 1432–1441. 10.1152/japplphysiol.00436.2006
34
JonesA. M.PooleD. C. (2005). Oxygen uptake dynamics: From muscle to mouth--an introduction to the symposium. Med. Sci. Sports Exerc.37, 1542–1550. 10.1249/01.mss.0000177466.01232.7e
35
KielyC.O'connorE.O'sheaD.GreenS.EgañaM. (2014). Hemodynamic responses during graded and constant-load plantar flexion exercise in middle-aged men and women with type 2 diabetes. J. Appl. Physiol.117, 755–764. 10.1152/japplphysiol.00555.2014
36
KielyC.RochaJ.O'connorE.O'sheaD.GreenS.EgañaM. (2015). Influence of menopause and Type 2 diabetes on pulmonary oxygen uptake kinetics and peak exercise performance during cycling. Am. J. Physiol. Regul. Integr. Comp. Physiol.309, R875–R883. 10.1152/ajpregu.00258.2015
37
KoppoK.BouckaertJ. (2002). The decrease in VO(2) slow component induced by prior exercise does not affect the time to exhaustion. Int. J. Sports Med.23, 262–267. 10.1055/s-2002-29080
38
KrustrupP.SoderlundK.MohrM.BangsboJ. (2004). The slow component of oxygen uptake during intense, sub-maximal exercise in man is associated with additional fibre recruitment. Pflugers Arch.447, 855–866. 10.1007/s00424-003-1203-z
39
LaplaudD.HugF.GrelotL. (2006). Reproducibility of eight lower limb muscles activity level in the course of an incremental pedaling exercise. J. Electromyogr. Kinesiol.16, 158–166. 10.1016/j.jelekin.2005.04.002
40
Mac AnaneyO.MaloneJ.WarmingtonS.O'sheaD.GreenS.EgañaM. (2011). Cardiac output is not related to the slowed o2 uptake kinetics in type 2 diabetes. Med. Sci. Sports Exerc.43, 935–942. 10.1249/MSS.0b013e3182061cdb
41
MacananeyO.ReillyH.O'sheaD.EgañaM.GreenS. (2011). Effect of type 2 diabetes on the dynamic response characteristics of leg vascular conductance during exercise. Diab. Vasc. Dis. Res.8, 12–21. 10.1177/1479164110389625
42
MarinP.AnderssonB.KrotkiewskiM.BjorntorpP. (1994). Muscle fiber composition and capillary density in women and men with NIDDM. Diabetes Care17, 382–386. 10.2337/diacare.17.5.382
43
MckayA. K. A.StellingwerffT.SmithE. S.MartinD. T.MujikaI.Goosey-TolfreyV. L.et al (2022). Defining training and performance caliber: A participant classification framework. Int. J. Sports Physiol. Perform.1, 317–331. 10.1123/ijspp.2021-0451
44
MiyamotoT.WatanabeK.FukudaK.MoritaniT. (2020). Near-infrared spectroscopy of vastus lateralis muscle during incremental cycling exercise in patients with type 2 diabetes. Phys. Ther. Res.23, 23–30. 10.1298/ptr.E9984
45
MogensenM.SahlinK.FernstromM.GlintborgD.VindB. F.Beck-NielsenH.et al (2007). Mitochondrial respiration is decreased in skeletal muscle of patients with type 2 diabetes. Diabetes56, 1592–1599. 10.2337/db06-0981
46
MuriasJ. M.SpencerM. D.KowalchukJ. M.PatersonD. H. (2011). Influence of phase I duration on phase II VO2 kinetics parameter estimates in older and young adults. Am. J. Physiol. Regul. Integr. Comp. Physiol.301, R218–R224. 10.1152/ajpregu.00060.2011
47
O'connorE.GreenS.KielyC.O'sheaD.EgañaM. (2015). Differential effects of age and type 2 diabetes on dynamic vs. peak response of pulmonary oxygen uptake during exercise. J. Appl. Physiol.118, 1031–1039. 10.1152/japplphysiol.01040.2014
48
O'connorE.KielyC.O'sheaD.GreenS.EgañaM. (2012). Similar level of impairment in exercise performance and oxygen uptake kinetics in middle-aged men and women with type 2 diabetes. Am. J. Physiol. Regul. Integr. Comp. Physiol.303, R70–R76. 10.1152/ajpregu.00012.2012
49
OkushimaD.PooleD. C.BarstowT. J.RossiterH. B.KondoN.BowenT. S.et al (2016). Greater V O2peak is correlated with greater skeletal muscle deoxygenation amplitude and hemoglobin concentration within individual muscles during ramp-incremental cycle exercise. Physiol. Rep.4, e13065. 10.14814/phy2.13065
50
PadillaD. J.McdonoughP.BehnkeB. J.KanoY.HagemanK. S.MuschT. I.et al (2006). Effects of Type II diabetes on capillary hemodynamics in skeletal muscle. Am. J. Physiol. Heart Circ. Physiol.291, H2439–H2444. 10.1152/ajpheart.00290.2006
51
PooleD. C.SchaffartzikW.KnightD. R.DerionT.KennedyB.GuyH. J.et al (1991). Contribution of exercising legs to the slow component of oxygen uptake kinetics in humans. J. Appl. Physiol.71, 1245–1260. 10.1152/jappl.1991.71.4.1245
52
PooleD. C.WardS. A.GardnerG. W.WhippB. J. (1988). Metabolic and respiratory profile of the upper limit for prolonged exercise in man. Ergonomics31, 1265–1279. 10.1080/00140138808966766
53
RochaJ.GildeaN.O'sheaD.GreenS.EgañaM. (2019). Influence of priming exercise on oxygen uptake and muscle deoxygenation kinetics during moderate-intensity cycling in type 2 diabetes. J. Appl. Physiol.127, 1140–1149. 10.1152/japplphysiol.00344.2019
54
RochaJ.GildeaN.O'sheaD.GreenS.EgañaM. (2020). Reply to Senefeld et al. J. Appl. Physiol.128, 227. 10.1152/japplphysiol.00804.2019
55
RossiterH. B.WardS. A.KowalchukJ. M.HoweF. A.GriffithsJ. R.WhippB. J. (2002). Dynamic asymmetry of phosphocreatine concentration and O(2) uptake between the on- and off-transients of moderate- and high-intensity exercise in humans. J. Physiol.541, 991–1002. 10.1113/jphysiol.2001.012910
56
RossiterH. B.WardS. A.KowalchukJ. M.HoweF. A.GriffithsJ. R.WhippB. J. (2001). Effects of prior exercise on oxygen uptake and phosphocreatine kinetics during high-intensity knee-extension exercise in humans. J. Physiol.537, 291–303. 10.1111/j.1469-7793.2001.0291k.x
57
RowlandsA. V.ThomasP. W.EstonR. G.ToppingR. (2004). Validation of the RT3 triaxial accelerometer for the assessment of physical activity. Med. Sci. Sports Exerc.36, 518–524. 10.1249/01.mss.0000117158.14542.e7
58
SahlinK.SorensenJ. B.GladdenL. B.RossiterH. B.PedersenP. K. (2005). Prior heavy exercise eliminates VO2 slow component and reduces efficiency during submaximal exercise in humans. J. Physiol.564, 765–773. 10.1113/jphysiol.2005.083840
59
ScheuermannB. W.HoeltingB. D.NobleM. L.BarstowT. J. (2001). The slow component of O(2) uptake is not accompanied by changes in muscle EMG during repeated bouts of heavy exercise in humans. J. Physiol.531, 245–256. 10.1111/j.1469-7793.2001.0245j.x
60
WatanabeK.GazzoniM.HolobarA.MiyamotoT.FukudaK.MerlettiR.et al (2013). Motor unit firing pattern of vastus lateralis muscle in type 2 diabetes mellitus patients. Muscle Nerve48, 806–813. 10.1002/mus.23828
61
WatanabeK.MiyamotoT.TanakaY.FukudaK.MoritaniT. (2012). Type 2 diabetes mellitus patients manifest characteristic spatial EMG potential distribution pattern during sustained isometric contraction. Diabetes Res. Clin. Pract.97, 468–473. 10.1016/j.diabres.2012.03.004
62
WeiM.GibbonsL. W.KampertJ. B.NichamanM. Z.BlairS. N. (2000). Low cardiorespiratory fitness and physical inactivity as predictors of mortality in men with type 2 diabetes. Ann. Intern. Med.132, 605–611. 10.7326/0003-4819-132-8-200004180-00002
63
WhippB. J.WardS. A.LamarraN.DavisJ. A.WassermanK. (1982). Parameters of ventilatory and gas exchange dynamics during exercise. J. Appl. Physiol. Respir. Environ. Exerc. Physiol.52, 1506–1513. 10.1152/jappl.1982.52.6.1506
64
WilkersonD. P.PooleD. C.JonesA. M.FulfordJ.MawsonD. M.BallC. I.et al (2011). Older type 2 diabetic males do not exhibit abnormal pulmonary oxygen uptake and muscle oxygen utilization dynamics during submaximal cycling exercise. Am. J. Physiol. Regul. Integr. Comp. Physiol.300, R685–R692. 10.1152/ajpregu.00479.2010
65
WüstR. C. I.StienenG. J. M. (2018). Successive contractile periods activate mitochondria at the onset of contractions in intact rat cardiac trabeculae. J. Appl. Physiol.124, 1003–1011. 10.1152/japplphysiol.01010.2017
Summary
Keywords
near-infrared spectroscopy, oxygen extraction, cycling, exercise tolerance, oxygen uptake slow component
Citation
Rocha J, Gildea N, O’Shea D, Green S and Egaña M (2022) Priming exercise accelerates oxygen uptake kinetics during high-intensity cycle exercise in middle-aged individuals with type 2 diabetes. Front. Physiol. 13:1006993. doi: 10.3389/fphys.2022.1006993
Received
29 July 2022
Accepted
31 October 2022
Published
18 November 2022
Volume
13 - 2022
Edited by
Michael E Tschakovsky, Queen’s University, Canada
Reviewed by
Christopher Hearon, University of Texas Southwestern Medical Center, United States
Toshiaki Miyamoto, Hyogo University of Health Sciences, Japan
Updates
Copyright
© 2022 Rocha, Gildea, O’Shea, Green and Egaña.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mikel Egaña, megana@tcd.ie
†These authors have contributed equally to this work and share first authorship
This article was submitted to Exercise Physiology, a section of the journal Frontiers in Physiology
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.