- Department of Urology, Yantai Yuhuangding Hospital, Qingdao University, Yantai, China
Background: Horseshoe kidney (HSK) has always been a challenge for urologists depending on its particular anatomy. We report a case of renal tumor in a patient with HSK, who underwent tumor resection by retroperitoneal robot-assisted laparoscopic partial nephrectomy.
Case Presentation: A 47-year-old man with HSK presented to our hospital with a solid renal mass. Computed tomography urography (CTU) showed a 4.3 × 4.4-cm mass in the upper pole of the right kidney. The patient received retroperitoneal robot-assisted laparoscopic partial nephrectomy on the basis of CT three-dimensional (3D) reconstructions.
Conclusion: The present case report highlights the feasibility of retroperitoneal robot-assisted laparoscopic partial nephrectomy for horseshoe kidney and the advantages of preoperative CT scan with three-dimensional reconstructions.
Introduction
Horseshoe kidney (HSK) is an anatomical deformity, which originates from renal fusion anomaly (1). Over the past 10 years, the therapeutic treatments of renal tumor associated with HSK are rarely reported. Furthermore, treatments correlative with robot-assisted laparoscopic surgery are seldom (2, 3). Vascular distribution of HSK can be diverse and provides one of the greatest challenges to the surgeon.
Recently, CT three-dimensional (3D) reconstructions have become a hot spot in partial nephrectomy, and several cases were reported to describe its significant effect in selective artery clamping and renal parenchyma protection. Moreover, all cases indicated that this reconstruction technique contributed to renal function (4–6). In general, CT three-dimensional reconstruction is more suitable for tumors associated with HSK because of its complex vascular anatomy. Theoretically, appropriate artery clamping can protect renal function to a maximum for this kind of disease.
We describe here a case of a clear cell carcinoma located on a HSK that was successfully treated with robot-assisted partial nephrectomy. Besides, we emphasize the utility of 3D CT scan images in selective artery clamping and surgery planning aiming at propagating the experiences of our center for curing this rare disease.
Case Presentation
A 47-year-old man was referred to our clinic with HSK because of a solid renal mass measuring 4.1 cm × 4.3 cm incidentally found on CT. The tumor HU values on a plain CT scan were 40 ± 11.7 HU. The patient had no hematuria and loin pain. A blood test revealed leukocytosis [12.51 × 109 white blood cells (WBC)/L], while other laboratory tests were all negative, such as urine culture and cytology. The chest CT revealed no abnormalities. In addition, the patient had a medical history of hypertension and cerebral ischemia.
Preoperative CTU showed a fusion anomaly in the lower pole of both kidneys and a 4.3 × 4.4-cm mass in the upper pole of the right kidney (Figure 1A). CT angiography (CTA) was performed with contrast medium, revealing that one artery supplied the isthmus from the abdominal aorta and no other obvious abnormalities were observed in both renal arteries (Figures 1B, 2B). On CT three-dimensional reconstructions, the right renal artery had three branches, one of which supplied the mass (Figure 2A). Based on these results, we evaluated the complexity of the tumor (cT1bN0M0; R.E.N.A.L. nephrometry score: 3 + 1 + 2 + 3 = 9p).
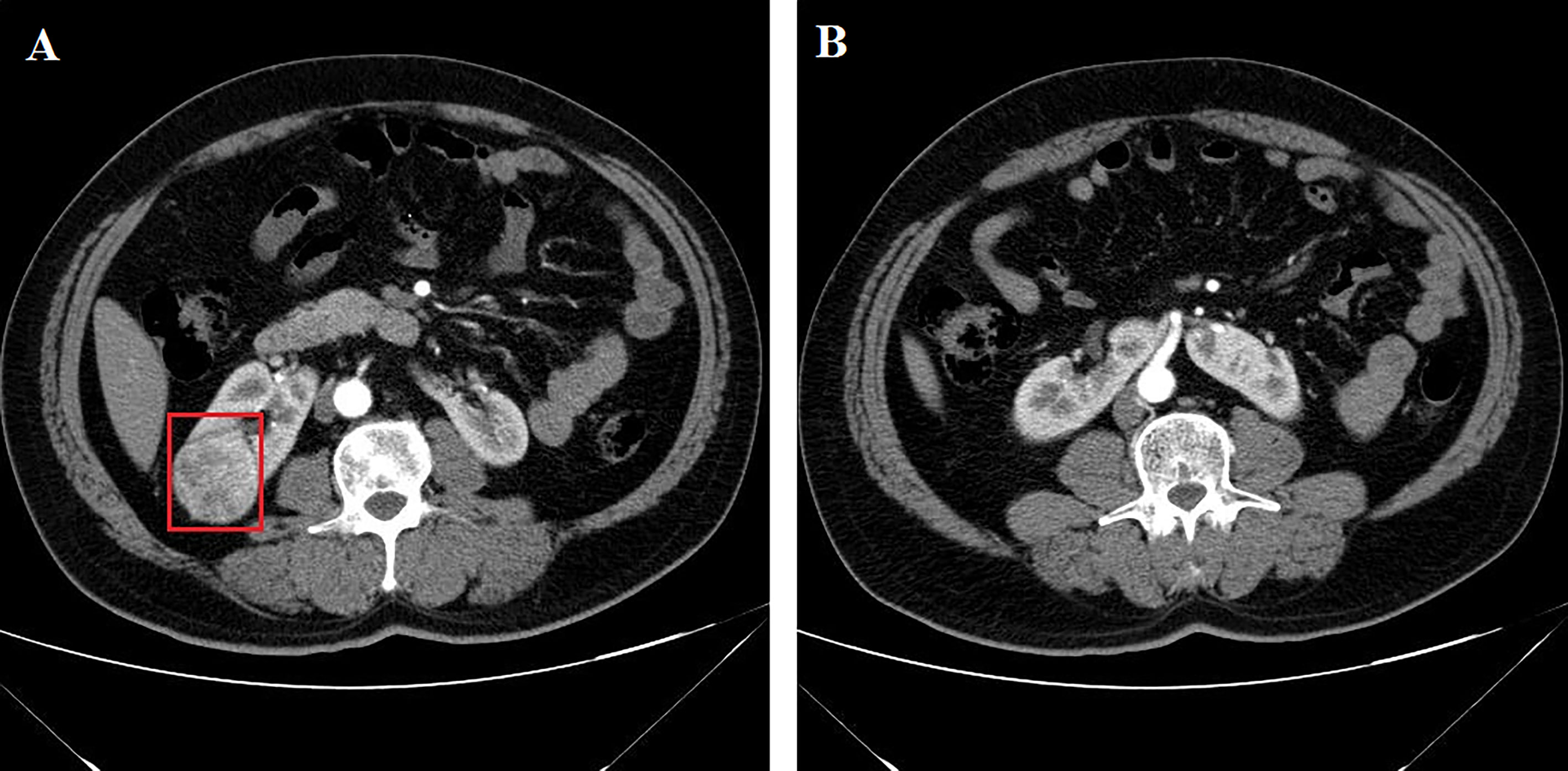
Figure 1 Kidney CTA of the patient. (A) A 4.3-cm mass is located in the right kidney (red square). (B) Axial section reveals the vascular supply of the isthmus.
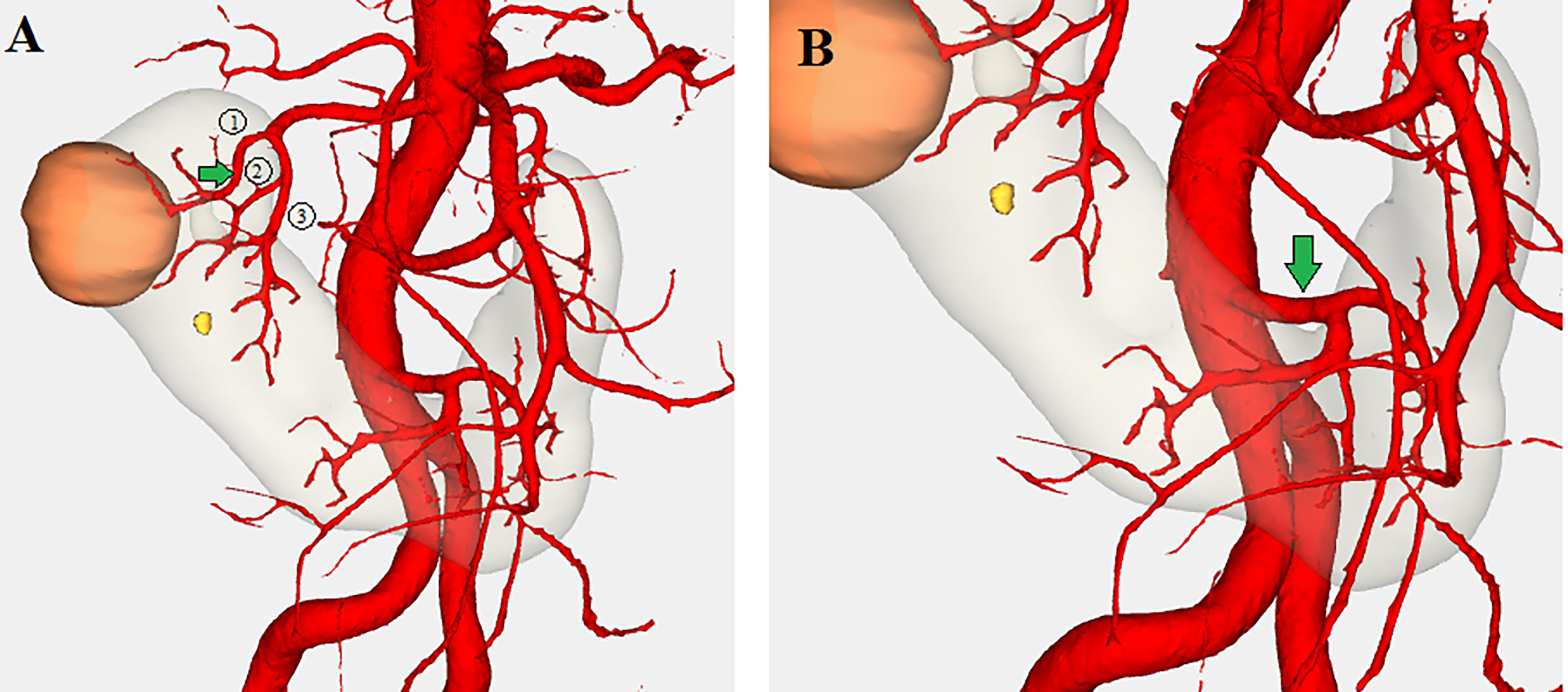
Figure 2 3D reconstructions of the patient. (A) A branch artery from the right renal artery supplies the mass (green arrow). (B) One artery arising from the abdominal aorta supplies the isthmus (green arrow) (orange: renal tumor, gray: kidney, red: artery).
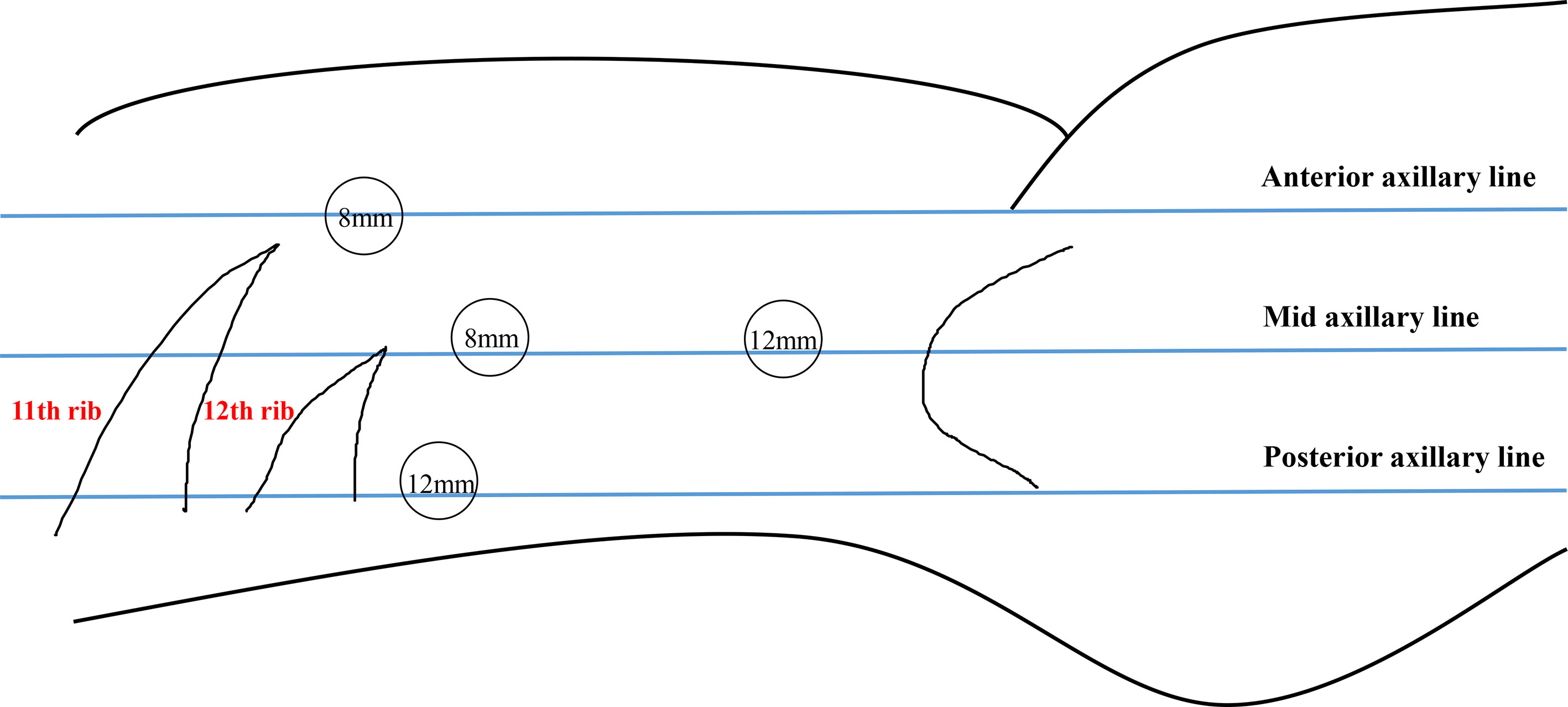
A surgical procedure was performed using da Vinci robot-assisted laparoscopic partial nephrectomy (da Vinci X). The patient was placed in the left lateral decubitus position (full flank position). We performed the surgical procedure through retroperitoneal access and four trocars (Figure 3). The skin was incised at the costal margin on the posterior axillary line (Figure 3), and the retroperitoneal space was created by compressing the balloon dilator. A 12-mm trocar was placed 5 cm above the iliac crest in the midaxillary line for placement of the laparoscope. The robotic trocar was placed 2 cm below the costal margin of the anterior axillary line, 2 cm below the costal margin of the midaxillary line, and 2 cm below the costal margin of the posterior axillary line, respectively. The distance between each trocar was approximately 8 cm. Then, the surgeon cleaned the extraperitoneal fat and opened the perirenal fascia. By removing perirenal fat, the two renal arteries were exposed (Figure 4A). The tumor, about 3 * 3 cm in size, was located at the upper pole of the kidney (Figure 4B). The adipose tissue around the mass was dissociated and the adipose tissue on the surface of the tumor was retained. According to the applied three-dimensional reconstructions, the two renal arteries were blocked (Figure 4C). Next, the surgeon removed the tumor along the edge of the tumor, and the resection edge was at least 0.5 cm from the tumor margin. The wound was closed with barbed suture and continuous suture. The suture direction was to enter from the renal sinus and collector system and to exit from the surface of the renal parenchyma (Figure 4D). A drainage tube was placed in the incision above the iliac crest of the right midaxillary line. The surgery lasted for approximately 150 min and warm ischemia time was 20 min with 100 ml of intraoperative bleeding. Postoperative recovery was uneventful and the patient was discharged at day 6 after the operation with no complications. Pathologic examination of cores indicated renal clear cell carcinoma (Fuhrman grade III T1bN0M0; renal scores = 9p).
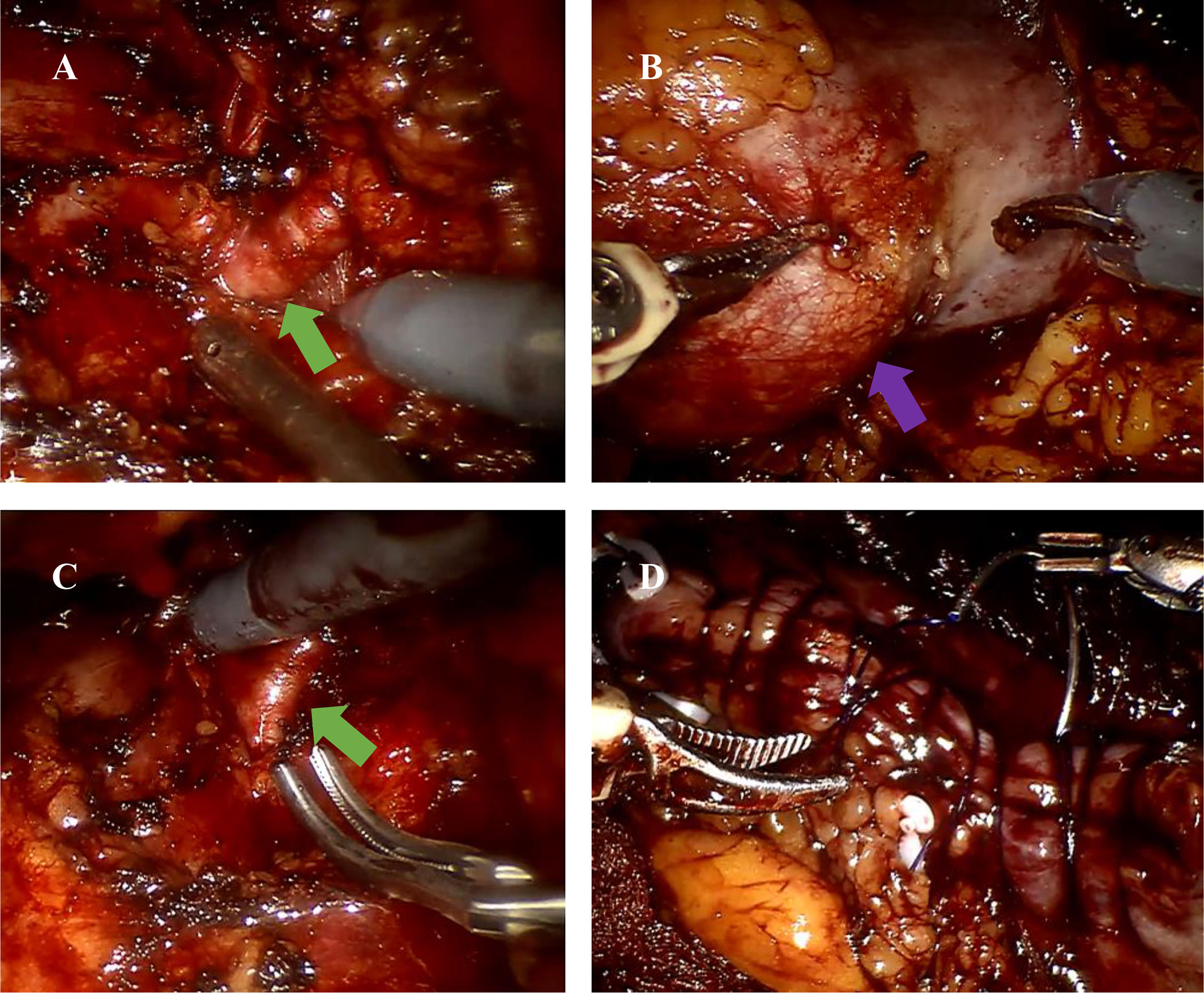
Figure 4 Images of the surgical procedure. (A) The right renal artery was isolated (green arrow). (B) The right renal tumors were exposed (purple arrow). (C) The right renal artery was occluded (green arrow). (D) The kidney was sutured.
Discussion
HSK is a common congenital renal malformation, which is mostly developed in early fetal life. Its main anatomical features are complicated vascular networks. Prior reports have shown that the number of renal arteries in HSK is twice that of normal kidney (7). In addition, patients with HSK have an increased risk of infection, stones, and even tumors due to abnormal fusion of the kidneys on both sides, resulting in changes in the position of the kidney, ureter, and pelvis (8). Therefore, the difficulty of laparoscopic partial nephrectomy increases significantly due to the unique anatomy of HSK. In our case, we chose to perform retroperitoneal robot-assisted laparoscopic partial nephrectomy. It is expected to provide a novel proposal for patients with such disease treatment.
Several lines of evidence suggested better results in robotic than laparoscopic partial nephrectomies (9, 10). The robotic systems were designed to reduce the challenges posed by the complex anatomical structures of HSK. The main advantage of this procedure is that it provides a wide surgical view. Surgeons can use robotic arms to dissect blood vessels and resect lesions more flexibly. Given the complex anatomy of HSK and its blood supply, we suggested that three-dimensional reconstructions are applied before surgery, because it can clearly visualize the three-dimensional anatomy of the procedure area and aid surgeons in identifying a complex horseshoe vascular system preoperatively better. In this case, we selectively occluded the branches of the renal artery rather than the trunk of the renal artery by referring to the reconstructed 3D images, thereby decreasing the damage due to ischemia–reperfusion injury in other nephron. A growing body of evidence also emphasized the importance of preoperative three-dimensional reconstructions for patients with partial nephrectomy of HSK in surgical planning (2, 11). Furthermore, our case indicated that retroperitoneal access was an effective approach for carcinoma in HSK. Informed consent was obtained from the patient for surgery. Although the transperitoneal approach can provide the operator with a better surgical field, there is also an increased risk of visceral damage and ileus after surgery. The vascularization of HSK is very heterogeneous and intraoperative bleeding was difficult to control. A retroperitoneal approach can better process blood vessels, avoid viscera damage, and reduce postsurgical adhesions (12). The robotic systems may help the operator to have more flexibility in blocking blood vessels. Molina and Gill (13) also documented that the retroperitoneal approach may work better for tumors located in the posterolateral side. Until now, there have only been four cases that characterize robot-assisted partial or heminephrectomy for renal tumors with fusion anomalies of the kidney (2, 14–16). Three of them reported that surgery was performed through a transperitoneal approach (14–16). To our knowledge, little has been reported about retroperitoneal robot-assisted laparoscopic partial nephrectomy with HSK.
Conclusion
Retroperitoneal robotic-assisted laparoscopic partial nephrectomy combined with CT scan with three-dimensional reconstructions for HSK with renal tumor is a feasible procedure.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Ethics Statement
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor of this journal.
Author Contributions
JPW and JTW designed the research and revised the paper. YL and FS collected and analyzed the patient data. DZ drafted the paper. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by grants from the National Nature Science Foundation of China (Nos. 81870525 and 81572835) and Taishan Scholars Program of Shandong Province (No. tsqn201909199).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
HSK, horseshoe kidney; CTU, computed tomography urography; 3D, three-dimensional; CTA, computed tomography angiography.
References
1. Natsis K, Piagkou M, Skotsimara A, Protogerou V, Tsitouridis I, Skandalakis P, et al. Horseshoe Kidney: A Review of Anatomy and Pathology. Surg Radiol Anat (2014) 36(6):517–26. doi: 10.1007/s00276-013-1229-7
2. Raman A, Kuusk T, Hyde ER, Berger LU, Bex A, Mumtaz F. Robotic-Assisted Laparoscopic Partial Nephrectomy in a Horseshoe Kidney. A Case Report and Review of the Literature. Urology (2018) 114:e3–5. doi: 10.1016/j.urology.2017.12.003
3. Yoshino T, Wake K, Sugitani T, Kodama K, Shiina H, Yasumoto H, et al. Laparoscopic Pyelolithotomy in a Horseshoe Kidney : A Case Report and Review of the Literature. Hinyokika Kiyo (2017) 63(4):157–61. doi: 10.14989/ActaUrolJap_63_4_157
4. Ukimura O, Nakamoto M, Gill IS. Three-Dimensional Reconstruction of Renovascular-Tumor Anatomy to Facilitate Zero-Ischemia Partial Nephrectomy. Eur Urol (2012) 1):211–7. doi: 10.1016/j.eururo.2011.07.068
5. Porpiglia F, Fiori C, Checcucci E, Amparore D, Bertolo R. Hyperaccuracy Three-Dimensional Reconstruction Is Able to Maximize the Efficacy of Selective Clamping During Robot-Assisted Partial Nephrectomy for Complex Renal Masses. Eur Urol (2018) 5):651–60. doi: 10.1016/j.eururo.2017.12.027
6. Wang J, Lu Y, Wu G, Wang T, Wang Y, Zhao H, et al. The Role of Three-Dimensional Reconstruction in Laparoscopic Partial Nephrectomy for Complex Renal Tumors. World J Surg Oncol (2019) 17(1):159. doi: 10.1186/s12957-019-1701-x
7. Majos M, Polguj M, Szemraj-Rogucka Z, Arazińska A, Stefańczyk L. The Level of Origin of Renal Arteries in Horseshoe Kidney vs. In Separated Kidneys: CT-Based Study. Surg Radiol Anat (2018) 4010(10):1185–91. doi: 10.1007/s00276-018-2071-8
8. Babu C, Sharma V, Gupta OMP. Renal Fusion Anomalies: A Review of Surgical Anatomy. Anat Physiol S5-001:564–72. doi: 10.4172/2161-0940.S5-00
9. Luciani LG, Chiodini S, Mattevi D, Cai T, Puglisi M, Mantovani W. Robotic-Assisted Partial Nephrectomy Provides Better Operative Outcomes as Compared to the Laparoscopic and Open Approaches: Results From a Prospective Cohort Study. J Robot Surg (2017) 113(3):333–9. doi: 10.1007/s11701-016-0660-2
10. Leow JJ, Heah NH, Chang SL, Chong YL, Png KS. Outcomes of Robotic Versus Laparoscopic Partial Nephrectomy: An Updated Meta-Analysis of 4,919 Patients. J Urol (2016) 1965(5):1371–7. doi: 10.1016/j.juro.2016.06.011
11. Nikoleishvili D, Koberidze G. Retroperitoneoscopic Partial Nephrectomy for a Horseshoe Kidney Tumor. Urol Case Rep (2017) 13:31–3. doi: 10.1016/j.eucr.2017.03.013
12. Lee JW, You SH, Han DY, et al. Retroperitoneoscopic Nephrectomy for a Horseshoe Kidney With Unilateral Severe Hydronephrosis and Ureteral Hypoplasia. Korean J Urol (2009) 50:512–5.
13. Molina WR, Gill IS. Laparoscopic Partial Nephrectomy in a Horseshoe Kidney. J Endourol (2003) 17(10):905–6. doi: 10.1089/089277903772036244
14. Fujihara A, Hongo F, Narukawa T, et al. Robot-Assisted Laparoscopic Partial Nephrectomy for Horseshoe Kidney: A Case Report. IJU Case Rep (2019) 2(6):308–11. doi: 10.1002/iju5.12108
15. Rogers CG, Linehan WM, Pinto PA. Robotic Nephrectomy for Kidney Cancer in a Horseshoe Kidney With Renal Vein Tumor Thrombus: Novel Technique for Thrombectomy. J Endourol (2008) 22(8):1561–3; discussion 1563. doi: 10.1089/end.2008.0043
Keywords: renal tumor, horseshoe kidney, robot-assisted laparoscopic partial nephrectomy, retroperitoneal, three-dimensional reconstructions
Citation: Zhang D, Lu Y, Sun F, Yao H, Wu J and Wang J (2021) Retroperitoneal Robot-Assisted Laparoscopic Partial Nephrectomy for Horseshoe Kidney: A Case Report. Front. Urol. 1:776995. doi: 10.3389/fruro.2021.776995
Received: 14 September 2021; Accepted: 18 October 2021;
Published: 09 December 2021.
Edited by:
Juan Gomez Rivas, Hospital Clínico San Carlos, SpainReviewed by:
Cristian Fiori, University of Turin, ItalyPablo Abad López, Hospital Clínico San Carlos, Spain
Copyright © 2021 Zhang, Lu, Sun, Yao, Wu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jipeng Wang, MjQxMDk1NDQ1NUBxcS5jb20=; Jitao Wu, d2p0dXJvbG9neUAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Dongxu Zhang
Dongxu Zhang Youyi Lu†
Youyi Lu† Jitao Wu
Jitao Wu