- 1Faculty of Architecture, Walailak University, Nakhon Si Thammarat, Thailand
- 2Faculty of Architecture, Chiang Mai University, Chiang Mai, Thailand
This research aims to explore the factors related to the physical environment in outpatient departments (OPD) that influence the hospital design process in public hospitals in Thailand after the COVID-19 pandemic. Additionally, it seeks to establish design guidelines for preventing respiratory diseases. This is a qualitative study involving 50 participants, including 20 medical personnel and 30 patients and their relatives, based on the Clinic Design Post-Occupancy Evaluation Toolkit. Data collection was conducted in three stages: (1) observing the physical environment using a checklist derived from the Clinic Design Post-Occupancy Evaluation Toolkit, (2) conducting surveys using the Analytic Hierarchy Process (AHP) questionnaire, and (3) interviews to assess impacts on mental health and the prevention of airborne respiratory diseases. The AHP ranking results indicated that issues concerning space screening, furniture arrangement, ventilation, recreational reception areas, lighting, and space layout are concerns expressed by medical personnel, patients, and their relatives in the outpatient departments of both buildings. Thematic analysis of focus group discussions among medical personnel, patients, and their relatives identified three main factors and two design recommendations to help prevent the spread of COVID-19 and respiratory disease: (1) Improving the outpatient waiting area environment to reduce the spread of infectious diseases. (2) Enhancing space management and screening processes.
1 Introduction
The COVID-19 pandemic, which began in 2020, has severely impacted healthcare systems worldwide, with a total of 4.7 million reported cases and approximately 34,000 deaths in Thailand (Soria et al., 2021; Cheung, 2020; World Health Organization, 2022a; World Health Organization, 2022b). This crisis has forced hospitals to urgently adapt their building designs to prevent the spread of the virus and create environments that promote the wellbeing of hospital users (Thai Health Coding Center, 2021; Waroonkun and Prugsiganont, 2022; Mhalla, 2020). Hospitals are high-risk environments for the accumulation and transmission of infectious diseases, particularly respiratory illnesses (Health-care administration, 2021). In response, hospitals in Thailand must comply with the Thai Healthcare Accreditation Standard (Thai Health Coding Center, 2021) to prevent the spread of infectious diseases while ensuring safety and wellbeing for all users. As COVID-19 has now become an endemic disease, hospital design must effectively address this reality, incorporating adaptability for future outbreaks (Health-care administration, 2021).
According to the data, the COVID-19 outbreak situation in Nakhon Si Thammarat province still requires continuous monitoring and control (Thai Health Coding Center, 2021; Waroonkun and Prugsiganont, 2022; Mhalla, 2020; Health-care administration, 2021; Amos et al., 2020). During 2023–2024, the number of infected individuals increased by 468, which is considered high for this province. The infected patients are spread across 19 districts, with Mueang District reporting the highest number of cases at 278, followed by Tha Sala District with 37 cases and Pak Phanang District with 21 cases. Notably, Tha Sala District has shown a continuous increase in infections. The latest data from September 2023 indicates that the number of cases in this district continues to rise, with up to 19 new cases recorded in a single day. As a result, public health authorities are closely monitoring the situation while preparing tertiary hospitals in the district to accommodate the increasing number of patients (Thailand Ministry of Public Health, 2020).
Walailak University Medical Center Hospital serves as a central hub for providing highly complex medical services and accommodates a large number of users. As a result, the study and development of design approaches for this hospital are crucial for improving the quality of medical services and preventing future disease outbreaks, in line with the preparedness policies of public health authorities (Thai Health Coding Center, 2021; Waroonkun and Prugsiganont, 2022; Mhalla, 2020; Health-care administration, 2021; Amos et al., 2020; Thailand Ministry of Public Health, 2020). However, a review of the relevant literature and previous studies reveals that most research has focused on the design and renovation of hospitals in major urban areas or tertiary-level hospitals located in resource-rich provinces such as Bangkok or other provinces with large medical centers. In contrast, Nakhon Si Thammarat Province, despite experiencing a continuous increase in COVID-19 cases and playing a crucial role in providing medical services to the upper southern region of Thailand, still lacks in-depth studies that address the specific local context. This includes both the physical challenges faced by hospitals and the design approaches that respond to the post-COVID-19 situation. This gap is particularly evident in tertiary-level institutions such as Walailak University Medical Center Hospital, which possesses unique characteristics as a provider of medical services as well as a hub for health-related research and education (Thai Health Coding Center, 2021). The aforementioned knowledge gap, combined with the ongoing need for vigilance regarding disease outbreaks in Nakhon Si Thammarat Province, underscores the importance of systematically developing hospital spaces—particularly in outpatient departments (OPDs), which serve as high-traffic areas and potential hotspots for disease transmission. These spaces must be carefully examined to identify physical environmental challenges that may hinder effective infection control and the promotion of wellbeing. Accordingly, this study aims to:
1. To examine the physical environmental issues of the outpatient department (OPD) at Walailak University Medical Center Hospital in the post-COVID-19 period.
2. To establish guidelines for designing respiratory disease prevention measures.
The case study focuses on the outpatient building of Walailak University Medical Center Hospital. These objectives lead to the following research questions.
RQ1: Does hospital building design contribute to reducing the spread of COVID-19?
RQ2: What are the design guidelines to prevent the spread of COVID-19 and promote wellbeing in public tertiary hospitals?
This study aims to address the challenges of the healthcare system after the COVID-19 outbreak by balancing infection control measures with the enhancement of user experience in hospitals in a sustainable manner.
2 Literature review
2.1 Space design
2.1.1 Concepts on the healthcare service system
The healthcare service system encompasses medical and public health services aiming at health promotion, disease prevention, diagnosis, and treatment (West, 2020) In Thailand, healthcare facilities are categorized into three levels: primary, secondary, and tertiary care. As of now, there are a total of 38,512 healthcare facilities in the country, comprising 13,364 public healthcare facilities (34.7%) and 25,148 private healthcare facilities (65.3%) (Thai Health Coding Center, 2021). When considering the size and capacity of medical services, it is found that primary healthcare facilities account for a total of 37,857 establishments, representing 98.3% of all healthcare facilities. The remaining 664 facilities (1.7%) fall under secondary and tertiary care. Among these, 294 facilities (0.7%) are public hospitals under the Ministry of Public Health, local administrative organizations, state enterprises, and the Bangkok Metropolitan Administration. The other 370 facilities (0.9%) are private hospitals (Ministry of Public Health, 2016). The number of public healthcare facilities has proven insufficient to meet the demand for patient care in certain regions, particularly during the COVID-19 pandemic. When compared to Thailand’s population of over 66 million, the availability of only 13,364 public healthcare facilities equates to approximately one facility per 5,000 people. This disparity becomes even more pronounced when considering secondary and tertiary hospitals, of which there are only 294 across the country. Such figures underscore the strain placed on the healthcare system during public health emergencies. The rapid increase in patient numbers, inversely proportional to the limited availability of healthcare facilities, significantly impeded efforts to control the spread of COVID-19 (Thai Health Coding Center, 2021). This highlights the lack of adequate facilities to handle patient surges. The inverse relationship between the high number of patients and the limited number of healthcare facilities has made it challenging to control the spread of COVID-19 (World Health Organization, 2022a; World Health Organization, 2022b; Waroonkun and Prugsiganont, 2022).
2.1.2 The outbreak of respiratory infectious diseases including COVID-19
Over the past 5 years (2020–2024), respiratory infectious diseases—particularly COVID-19—have had a profound impact on global public health. According to the World Health Organization (WHO), more than 7 million deaths worldwide have been attributed to COVID-19 during this period. Notably, over the past two decades, there has been a rise in the number of viral outbreaks capable of spreading through airborne droplets or contact with bodily fluids from infected individuals (Centers for Disease Control and Prevention (CDC), 2014; 2023). The spread of respiratory infectious diseases, such as COVID-19, influenza, and severe acute respiratory syndrome (SARS), has demonstrated the ability of viruses to cause widespread outbreaks. This highlights the necessity of coordinated efforts among various sectors to control the disease effectively (Thai Health Coding Center, 2021; Waroonkun and Prugsiganont, 2022). In order to control the spread of the virus and reduce the potential impacts on society as a whole, patients within hospitals and healthcare personnel are considered high-risk groups for exposure to respiratory infectious diseases, including COVID-19, due to their close proximity to infected patients (Amos et al., 2020).
2.1.3 Hospital waiting area
The waiting area in hospitals is a crucial component of the healthcare system, especially in outpatient departments. It serves as the first point of contact for patients with infectious diseases such as COVID-19 and respiratory illnesses, necessitating screening procedures to separate these patients from those with general conditions (Thailand Ministry of Public Health, 2020; West, 2020; Ministry of Public Health of Thailand, 2016; Centers for Disease Control and Prevention (CDC), 2023). The environment of such areas can significantly impact patient satisfaction and their emotional wellbeing. Previous research has shown that appropriate waiting area design helps reduce stress, creates positive experiences, and prevents the spread of infections (Akanbi et al., 2017). A well-designed environment in waiting areas, such as space screening, furniture arrangement, lighting, color, sound, and efficient space utilization, can reduce patient anxiety and decrease the risk of infections within hospitals (Ulrich et al., 2004; Ulrich et al., 2008; Beauchemin and Hays, 1996). It also helps reduce the likelihood of patient dissatisfaction regarding waiting times (Douglas and Douglas, 2004).
2.2 Space management
2.2.1 Evidence-based design
Evidence-Based Design is a design approach based on the use of data and scientific evidence in planning, developing, and evaluating the impact of design on users. Especially in the context of healthcare settings, Evidence-Based Design is widely recognized as playing a significant role in promoting healthcare quality and improving the environment to suit both patients and medical staff (Hamilton and Watkins, 2009).
The concept of Evidence-Based Design can be defined as a ‘design process’ that guides empirical understanding of the impact of the physical healthcare environment on safety, efficiency, and clinical outcomes (Hamilton and Watkins, 2009; Beauchemin and Hays, 1996; Blomkvist et al., 2005; Malkin, 2008). The application of EBD not only improves the quality of life for patients but also supports medical staff in performing their duties more effectively. Additionally, evidence-based design helps reduce long-term costs by lowering accident rates and health issues in healthcare settings (Ulrich et al., 2008; Beauchemin and Hays, 1996; Douglas and Douglas, 2004; Hamilton and Watkins, 2009).
2.2.2 Post occupancy evaluation and clinic design
2.2.2.1 Post-Occupancy Evaluation toolkit
Post-Occupancy Evaluation (POE) is a crucial process for analyzing and assessing the use of a building after construction and occupancy, especially in the context of clinic design. POE plays an important role in determining whether the building environment meets the needs of users appropriately, in terms of actual use, work efficiency, and user satisfaction (Ulrich et al., 2008; Preiser and Vischer, 2005; Verderber and Refuerzo, 2006; Zimring et al., 2010). The Post-Occupancy Evaluation Toolkit is designed to support data collection and analysis. The POE process consists of three stages: Indicative POEs, which are preliminary assessments to identify problems; Diagnostic POEs, which involve detailed analysis of issues and causes; and Investigative POEs, which are in-depth evaluations to find solutions and recommendations that can be used to improve design or management (Zimring et al., 2010; Turpin-Brooks and Viccars, 2006). The POE process covers various dimensions: 1. Data collection, both quantitative and qualitative, such as surveys, user feedback, and observations. 2. Design and space utilization analysis, such as the flexibility of space and management of personal areas. 3. Resource management, such as evaluating energy use and building materials (Gifford, 2007; Gilby et al., 2006; Preiser, 2001; Preiser, 1995).
2.2.3 Analytic hierarchy process
The Analytic Hierarchy Process (AHP) is a multi-criteria decision-making (MCDM) method used to prioritize and select the best alternatives in complex situations. This concept was developed by Thomas L. Saaty in 1980. The AHP calculation relies on pairwise comparisons to assess the relative importance of criteria and alternatives. This process helps make decision-making more structured and transparent (Saaty, 1980) The AHP calculation process can be summarized as follows:
1. Hierarchy Construction: Establishing a hierarchy to reflect the structure of the problem.
2. Pairwise Comparison: The decision-maker compares criteria or alternatives in pairs using a relative scale of 1-9 defined by Saaty (e.g., 1 = equally important, 9 = most important). The resulting data is organized into a matrix.
Example matrix for three criteria:
3. Calculation of Relative Weights
4. Consistency Check: AHP uses the Consistency Ratio (CR) to check whether the comparisons are consistent. It is calculated by:
where CI = (λ_max - n)/(n - 1) and RI is the Random Index.
CR ≤ 0.10 indicates consistent comparisons.
5. Synthesis of Option Scores:
The relative weights of the criteria and the scores of the options are multiplied together to find the total score for each option (Saaty, 1980; Ramanathan, 2001).
3 Methodology
3.1 Research design
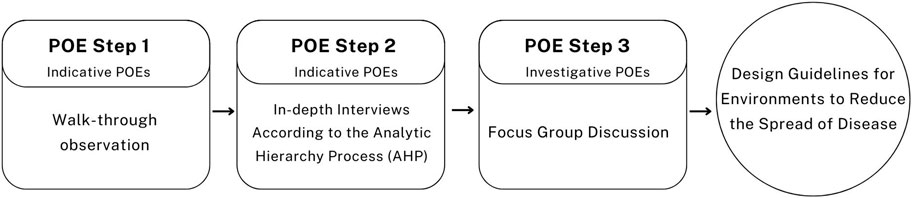
This study was conducted using a qualitative research methodology, incorporating a three-step Post-Occupancy Evaluation (POE) process for data collection. The three steps include observation, questionnaires, and focus group discussions, as illustrated in Figure 1 of this article. The details of each step are as follows:
• Step 1: Walk-through observation This process is widely recognized in architectural and design research (Waroonkun and Prugsiganont, 2022; Geng et al., 2021; Pilosof, 2021; Fronczek-Munter and Prugsiganont, 2018). Observation allows researchers to directly understand the context of the study area. Data were collected through photography to document architectural elements in detail and architectural plans to analyze spatial structure and functional layout. This process provides clear physical data, serving as a crucial foundation for analyzing the impact of building design on users.
• Step 2: AHP base-survey Based on the Analytic Hierarchy Process (AHP) theory, this step is designed to efficiently collect data for identifying decision-making criteria and prioritizing factors in complex research studies. It also enhances the effectiveness of designing and developing spaces (Saaty, 1980; Guilemany et al., 2011; Gulwadi et al., 2009).
• Step 3: Focus Group Discussion This step involved focus group discussions with medical personnel, patients, and their relatives in the outpatient department. It was designed to provide participants with the opportunity to exchange opinions and discuss potential solutions. Specifically, the discussion focused on the suitability of space design for preventing the spread of respiratory diseases, including COVID-19. This method enhances in-depth understanding through collaborative discussions, particularly on issues that remained unclear from the survey in Step 2 (Kevern and Webb, 2001; Kvande et al., 2017).
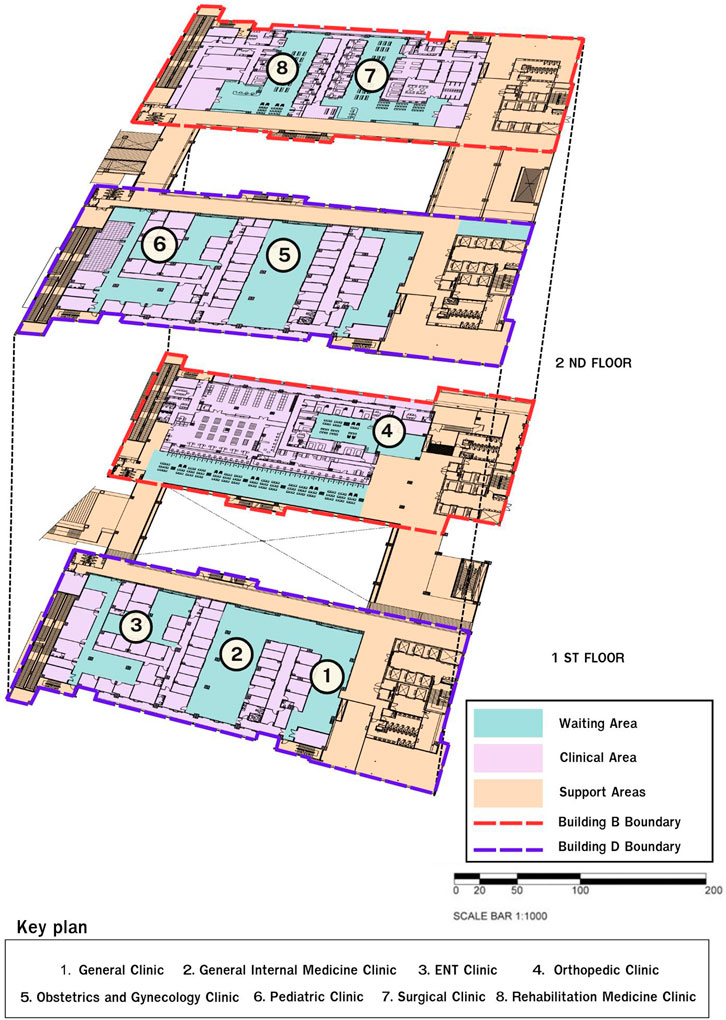
3.2 Case description
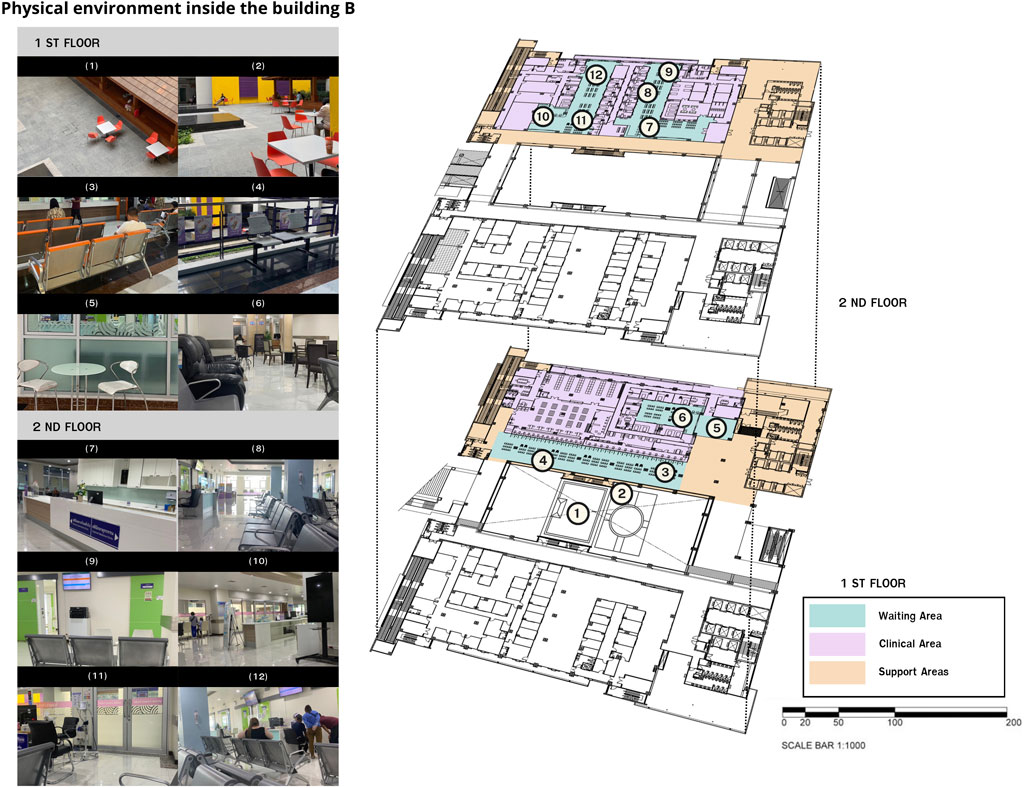
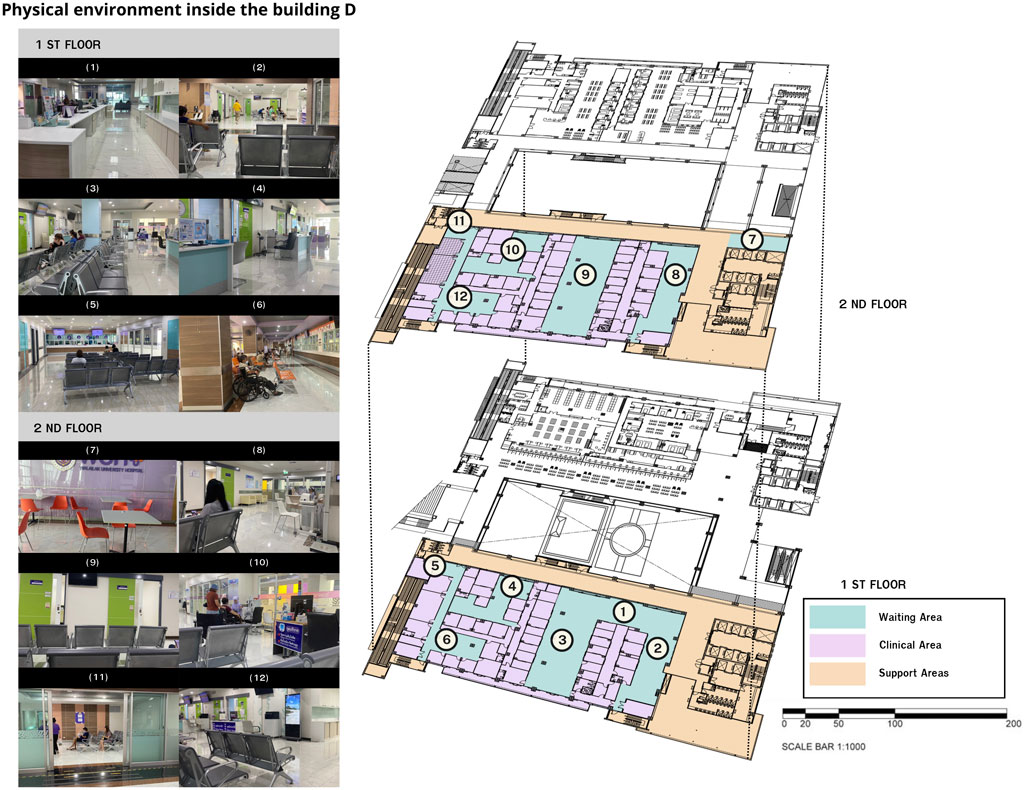
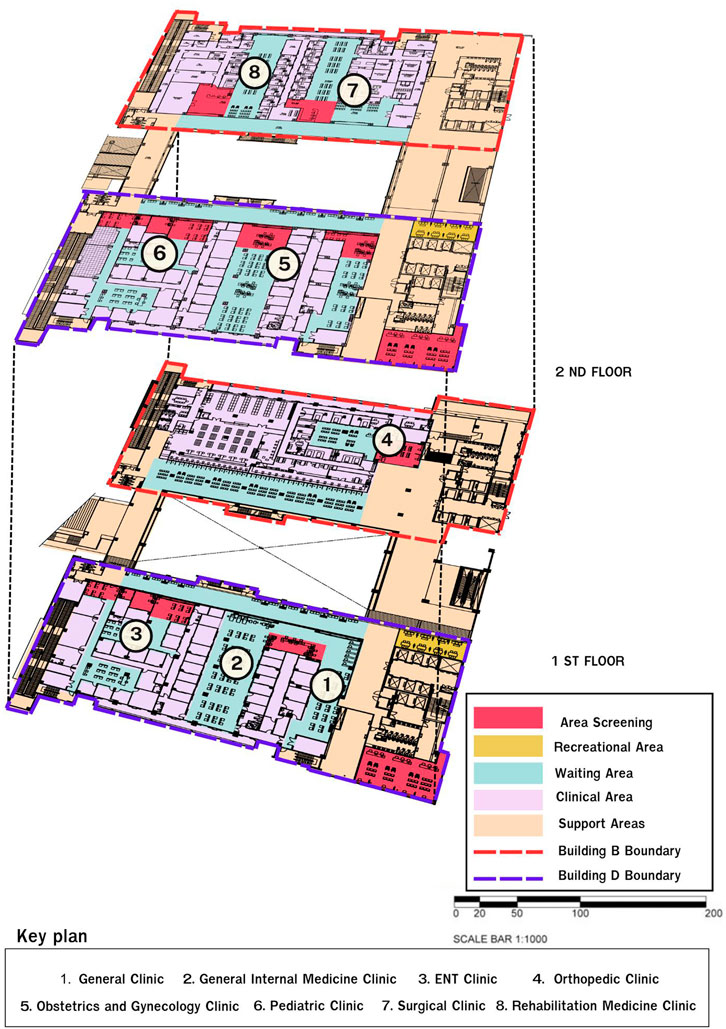
The first step of this study involved observing the indoor environment, with data collected through walk-through observation. This process was conducted in two outpatient department buildings: Building B: Orthopedic Clinic, Surgery and Aesthetic Clinic, and Rehabilitation Medicine Clinic. Building D: General Medicine Clinic, Internal Medicine Clinic, Otolaryngology (ENT) Clinic, Obstetrics and Gynecology Clinic, and Pediatrics Clinic. Both buildings are located at Walailak University Medical Center Hospital, a tertiary hospital that serves as a medical hub for the upper southern region, offering highly specialized services and accommodating a large number of users. It has the capacity to support up to 426 patient beds. The design of the outpatient departments in both buildings can be divided into three main functional areas as follows. Figure 2 illustrates the overall layout of both buildings:
1. Waiting Area (Blue) includes the history-taking areas, the waiting areas and the nurses’ stations.
2. Clinical Area (Purple) including the examination rooms.
3. Support Areas (Light Orange) including the hospital corridors, restrooms, elevators, stairs, and emergency exits.
3.3 Participants
This study aims to examine the physical environment of the outpatient department (OPD) at Walailak University Medical Center Hospital in the post-pandemic period of respiratory infectious diseases, including COVID-19. The focus is on the differences in the usage and context of all outpatient departments to identify design strategies that can help prevent the spread of diseases.
The second and third data collection phases included questionnaires and interviews with medical personnel, patients, and patients’ relatives. This part of the study involved 50 participants, consisting of 29 users from Building D and 21 users from Building B. Participants were between 18 and 70 years old and had direct experience using the studied facilities. In the initial phase, participants were provided with information about the study’s objectives. Subsequently, questionnaires were distributed, followed by interviews to gather additional data on various environmental factors. This study received ethical approval from the Human Research Ethics Committee of the Institute of Research and Innovation Promotion for Excellence, Walailak University (Approval Code: WU-EC-AR-1-313-67).
3.4 Data collection
The data collection process was conducted in three phases as follows:
3.4.1 Phase 1: Walk-through observation
Observation of the outpatient department (OPD) across eight clinics was carried out between September and October 2024. Data on the current physical environment of the outpatient department was collected through walk-through observation, including photographic documentation and time-stamped records of space usage. The focus was on building layout and functionality (Prugsiganont and Jensen, 2019). In this phase, researchers conducted walk-through observations across all eight clinics in the outpatient department, accompanied by medical personnel, following the hospital’s safety regulations.
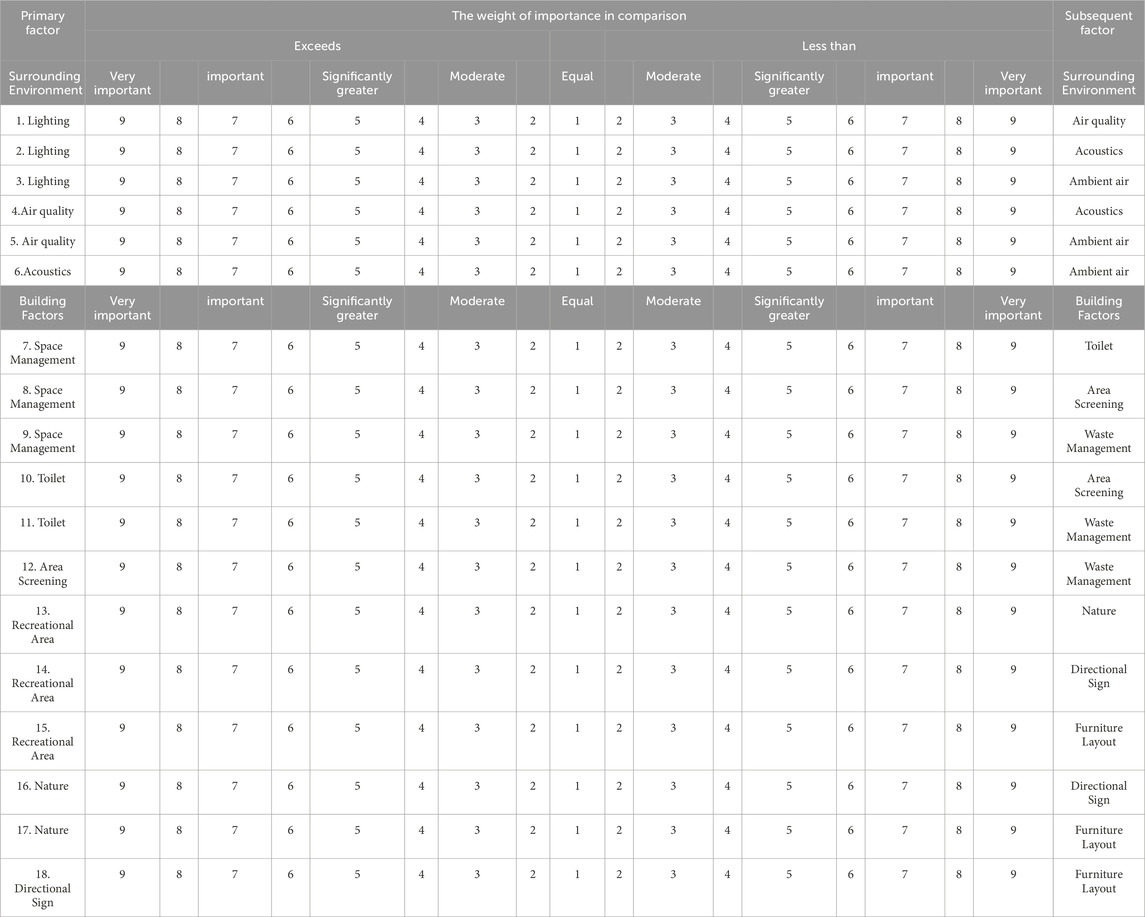
3.4.2 Phase 2: AHP-based survey
The questionnaire was designed to record the prioritization of various physical environmental factors. The survey items were adapted from the checklist factors identified in Phase 1, allowing for a comparative analysis of their importance. The questionnaire consisted of 21 items. The questionnaire was designed to compare factors in pairs. Respondents took approximately 10–15 min to complete the survey, rating each pair on a scale from 1 to 9: Score 1: Both factors are equally important. Score 9: The evaluated factor is significantly more important than the other. The factors were categorized into three main groups, with each group containing sub-factors that were paired for comparison, as shown in Table 1.
3.4.3 Step 3: Focus group
Bryman and Bell (2011) describe this technique as “an interview method involving more than one participant, typically at least four.” The emphasis is on interaction and responses to others’ viewpoints. Participants in this stage are the same individuals from the questionnaire phase, as they possess valuable information for the study (Bryman and Bell, 2011; Saunders et al., 2016). The focus group discussions were held between October and December 2024, lasting between 20 and 30 min. The discussions consisted of 12 questions, as shown in Table 2. The sessions were conducted with audio recordings of the conversation. Preliminary design suggestions derived from the analysis of the OPD building observations and questionnaires from medical personnel, patients, and their relatives were presented during the focus group discussions. Participants were able to debate and evaluate these suggestions, offering recommendations for adjustments or providing additional clarifications based on their real-life experiences.
Table 2. Set of questions regarding environmental factors influencing the prevention of disease outbreaks.
3.5 Data analysis
Empirical data was analyzed in three steps as follows:
Step 1: Physical Environment Observation
The data were analyzed using a checklist, architectural floor plans, and photographs taken during the walk-through observations of each area to highlight specific details of the layout. Information was gathered about the current physical environment of the hospital’s OPD, covering all eight clinics, along with additional notes on various areas of the outpatient department (OPD).
Step 2: AHP based-survey. The questionnaire was analyzed using the analytic hierarchy process (AHP). The results were compared in tables.
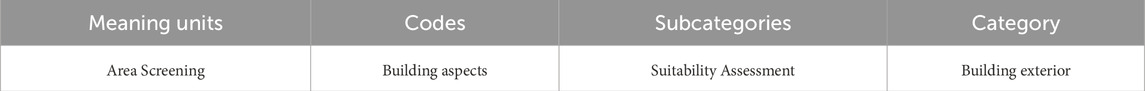
Step 3: Focus Group The interviews were analyzed using content analysis (Waroonkun and Prugsiganont, 2022; Corbin and Strauss, 2015). The researcher transcribed the interviews from the audio recordings and divided the transcript text into meaning units. These units were then abbreviated into condensed meaning units and coded by searching for key phrases related to the physical problems of the OPD buildings. The condensed meaning units were grouped into categories, sub-categories and themes (Erlingsson and Brysiewicz, 2017). Examples of semantic units, concise semantic units, codes, subcategories, and categories presented in Table 3.
4 Result
4.1 Building observation
Walk-through observations combined with photography reflect the current physical environment of both outpatient department (OPD) buildings.
Figures 3, 4 illustrate the physical layout of the interior environment within the buildings. The waiting areas, highlighted in blue, include the history-taking zones, general waiting areas, and nurse stations in both buildings, which were arranged after the COVID-19 outbreak. An evaluation of hospital layouts showed that the hospital has set up waiting areas, including its circulation in the middle of the clinic (Figures 3, 4). The circulation connects to the examination rooms of various clinics. However, the waiting area arrangement leads to crowding within the clinics, clinic entrances, and corridors, especially during the morning (8:00 a.m. to 12:00 p.m.). This is due to the insufficient waiting space to accommodate many patients and their relatives. On average, there are about 120–180 patients per day in each clinic, and there is not enough seating available for patients. As a result, most patients have to stand while waiting inside the clinics. The primary issues with the waiting areas include inadequate space allocation, poor furniture arrangement, absence of recreational areas, improper space layout, and insufficient ventilation. Furthermore, several damp corners were identified within the hospital, such as in front of restrooms and elevators, which may serve as potential breeding grounds for pathogens. The lack of queue management has also contributed to congestion in these areas.
4.2 AHP ranking findings
This study utilized a pairwise comparison questionnaire to evaluate the relative importance of different factors in all eight clinics. The results were then analyzed using the Analytic Hierarchy Process (AHP), which allowed for the ranking of these factors. The Consistency Ratio (CR) and Consistency Index (CI) were calculated, where the CR must be less than 0.1 to be considered consistent (Saaty, 1980) (Table 4). The results are as follows: Surrounding Environment of Building D. Surrounding environment (SE) CR = 0.02; CI = 0.05 Building Environment (BE) CR = 0.01; CI = 0.08 Interior Environment (IE) CR = 0.02; CI = 0.04 Surrounding environment of Building B (SE) CR = 0.02; CI = 0.04 Building Environment (BE) CR = 0.01; CI = 0.08 Interior Environment (IE) CR = 0.02; CI = 0.06.
The study found that space screening was the most important factor for patients, their relatives, and medical staff in both clinic groups, with scores of 0.45 for Building D and 0.43 for Building B. The next most important factors for Building B were air quality (0.29) and wayfinding signs (0.25). For Building D, the next factors were furniture arrangement (0.39) and lighting (0.34). This highlights that the physical environment of the building, particularly space screening, is a factor that should be improved to enhance the satisfaction of both users and service recipients. Additionally, this improvement is crucial for preventing the spread of respiratory diseases, including COVID-19.
4.3 Result from focus group
The focus group discussions on physical environmental factors were conducted with two groups: one comprising patients and their relatives, and the other consisting of medical personnel. Each session lasted approximately 20–30 min. Data analysis and categorization led to the identification of one main theme: factors influencing satisfaction and the prevention of respiratory infectious disease transmission, including COVID-19. This main theme was further divided into three subcategories: ambient environmental factors, building-related factors, and interior design factors. From the interviews, factors contributing to the accumulation and spread of pathogens were identified and categorized into three key themes as follows:
4.3.1 Theme 1: Factors leading to the accumulation and spread of pathogens
4.3.1.1 Interior design factors
These include: Recreational waiting areas, natural elements (real), simulated natural elements, signage and wayfinding and furniture arrangement.
1. Recreational Area–Most users expressed that having designated waiting areas for patients and their relatives outside each department within the OPD building helps reduce congestion in the main waiting area. This, in turn, minimizes the risk of disease transmission in overcrowded spaces, which is a critical factor in the spread of airborne diseases such as COVID-19.
2. Nature–Most users noted that both real and simulated natural elements have both benefits and drawbacks when it comes to promoting health and preventing the accumulation and spread of pathogens. Proper management and maintenance are essential, such as regular cleaning of simulated natural elements and controlling insect vectors in real natural areas, in order to reduce the risk of infection.
3. Directional Sign–Most users agreed that directional signs within the hospital help service users and staff navigate quickly and safely. This reduces the gathering of patients in the same area and helps alleviate congestion. This has a positive effect on preventing the spread of pathogens. However, if the directional signs are not designed for easy cleaning or are placed in areas that are frequently touched, they could become hotspots for pathogen accumulation. This increases the risk of transmission through frequent contact with the signs.
4. Furniture Layout–Everyone agreed that the layout of furniture within the hospital affects the accumulation and spread of pathogens. Properly spaced furniture can help reduce congestion and promote physical distancing.
4.3.2 Theme 2: Space management factors
4.3.2.1 Building factors include
Space Management, Toilet, Area Screening, and Waste Management.
1. Space Management–Everyone agreed that the layout of the space significantly affects the accumulation and spread of pathogens. A well-planned layout that clearly separates different usage areas, such as designating spaces for patients with respiratory symptoms or ensuring sufficiently wide walkways for social distancing, can help reduce congestion, improve ventilation, and minimize the likelihood of disease transmission.
2. Toilet–Most users agreed that the toilets are designed with good ventilation and materials that are easy to clean. However, they suggested that an efficient cleaning system and touchless operation would further reduce the accumulation of pathogens and the risk of disease transmission. For example, implementing sensor-based systems for opening and closing water taps or doors can help minimize contact with potentially contaminated surfaces.
3. Area Screening–Everyone agreed that both OPD buildings have multiple entry points but lack designated screening areas for individuals who may be at risk or showing symptoms of infectious diseases. Suggested measures include temperature checks, ensuring a distance of at least 1 m between patients in waiting or screening areas, the use of face masks, and conducting health assessments and symptom inquiries.
4. Waste Management–Everyone agreed that, currently, infectious waste is not being separated or stored properly, which could lead to the spread of pathogens from the waste to other areas through contact or airborne transmission.
4.3.2.2 Surrounding environment includes lighting, air quality, Acoustics and Ambient air
1. Lighting–Both OPD clinic buildings agreed that the lighting is insufficient, which affects work efficiency and functionality. Additionally, incorporating natural light into the buildings can help kill pathogens.
2. Air quality - Regarding ventilation and cleanliness, both medical staff, patients, and their relatives all agreed that the hospital should have proper air circulation. This includes using both passive ventilation and active ventilation in areas such as corridors, with designs that include openings for airflow. However, within the OPDs, the ventilation system is still inadequate. For example, there is no installation of HEPA (High Efficiency Particulate Air) filters. It is also important to maintain regular cleanliness according to HA (Hospital and Healthcare Standards).
2. Acoustics and Ambient air–Most users noted that excessive noise and a lack of sound control in the hospital environment can cause stress for both patients and staff. Additionally, high humidity levels in the air can promote the growth of mold and bacteria, leading to the accumulation of pathogens in the air, which increases the risk of respiratory infections.
4.4 Theme 3: Respiratory disease prevention measures
Patients, their relatives, and medical personnel indicated that the hospital has different protocols for during and after the COVID-19 pandemic. During the pandemic, the hospital has implemented five prevention measures as follows: (1) Daily Meetings–Regular meetings are held with the infection control team. (2) Use of Face Masks–All patients, their relatives, and medical personnel are required to wear face masks in all areas. (3) Social Distancing–A minimum distance of two m is enforced. (4) Installation of Clear Plastic Dividers–Clear plastic dividers are installed in screening areas, nursing counters, and waiting areas. (5) Cleaning–All areas are cleaned with disinfectants twice a day, and a thorough cleaning is conducted once a month by a professional cleaning company.
The results from the survey and focus group discussions provided in-depth insights into the building’s issues and led to the creation of an initial design draft for the OPD building. The information from the focus group aligned with the preliminary design guidelines, and the suggestions exchanged during the discussion led to a revised layout plan for the hospital. Figure 5 shows the updated layout that has been improved based on this input.
The design of the outpatient departments in both buildings can be divided into five main functional areas as follows.
1. The Waiting Area (Blue) includes the history-taking areas, the waiting areas, and the nurses’ stations.
2. Clinical Area (Purple), including the examination rooms.
3. Support Areas (Light Orange), including the hospital corridors, restrooms, elevators, stairs, and emergency exits.
4. Recreational Area (Yellow), including designated spaces to accommodate patients and their relatives while waiting their turn.
5. Area Screening (Pink), including Entry checkpoints for temperature and symptom screening, Registration and history-taking stations, and Waiting zones designated for screened patients before examination
5 Discussion
This study aimed to examine the physical structure of tertiary hospitals in Thailand in the post-COVID-19 era and to develop design guidelines for improving OPD (Outpatient Department) buildings to help reduce the spread of the COVID-19 virus. In this section, the researcher addresses the research questions as follows:
5.1 Does hospital building design help reduce the spread of COVID-19? Based on site surveys, interviews, and focus group discussions with patients, their relatives, and medical personnel, two main issues related to the physical environment were identified
1. Design Issues: The hospital buildings were not originally designed in accordance with respiratory disease prevention guidelines. Observations revealed a lack of flexibility in building usage, such as multiple entry and exit points without designated screening areas, poor ventilation systems, and improper furniture arrangements. This has had a negative impact on users in the post-COVID-19 period. The OPD building could not be modified or adapted to comply with the guidelines issued by the U.S. Centers for Disease Control and Prevention (CDCP) and the Thai Ministry of Public Health (Ministry of Public Health, 2016; Centers for Disease Control and Prevention (CDC), 2023).
2. Space Management Issues: It was found that the hospital lacked cleanliness standards aligned with infection control measures. Although there was a dedicated team responsible for infection control standards, proper cleaning protocols for COVID-19 prevention were not established. It is crucial to adhere to the guidelines from the Centers for Disease Control and Prevention (CDC) (2023) and the World Health Organization (2022b), which state that hospital spaces should be cleaned regularly at least 2 to 3 times per day, and hand washing stations should be provided at various locations. Additionally, medical personnel, patients, and their relatives expressed that the main issue with hospital visits was the long waiting time and the high number of patients. This contributed to overcrowding within the facility, increasing the risk of disease transmission. This observation aligns with the findings of Atkinson et al. (2021), who reported that hospitals with inadequate cleaning standards had nosocomial infection rates up to 30% higher than the average. Furthermore, patient overcrowding and prolonged waiting times were identified as key risk factors contributing to disease transmission, consistent with the conclusions drawn by (Sng et al., 2021).
5.2 What are the design guidelines for preventing the spread of COVID-19 and promoting wellbeing in tertiary public hospitals?
Interview results indicated that the involvement of key users—patients, their relatives, and medical personnel—in the design process plays a crucial role in developing design that truly meet the needs and is effective in reducing the risk of COVID-19 transmission. Preliminary design recommendations, derived from observations of OPD building spaces and focus group discussions, have been developed into design guidelines for three key areas: OPD waiting areas, clinic spaces, and support areas.
The data collected from this study led to the development of policy recommendations for preventing the spread of respiratory diseases in OPD buildings. These recommendations are categorized into two main areas: hospital management and hospital space design.
(1) Hospital Management
• Implementing technology to manage patient queues, such as an online patient registration system, can significantly benefit medical personnel. It saves time, reduces the number of patients waiting in the area, decreases the risk of infection, and shortens wait times for medical care. Additionally, online patient registration enhances patient data management, allowing for early identification and screening of patients with respiratory infections. Furthermore, it supports the establishment of a contactless check-in system. This recommendation aligns with the findings of Zhang et al. (2020), which indicated that hospitals in China that adopted technology-based queue management systems were able to reduce patient waiting times by over 40% and significantly minimize the risk of person-to-person contact.
• Promoting physical or social distancing of at least two m is a key strategy for enhancing patient and staff safety. Research by Page (2020) and Beggs et al. (2021) supports this concept, emphasizing that maintaining a physical distance of at least 2 m in waiting areas can reduce airborne transmission risk by up to 80%. For hospital design, additional recreational spaces should be provided for patients and their relatives to promote physical distancing in clinic areas and reduce overcrowding in waiting areas. Implementing this will help create a safer environment for everyone in the hospital, instilling confidence in the proposed changes.
(2) Hospital Space Design
• Establish Screening Areas: There should be designated screening areas for patients with respiratory infections at all entry and exit points of the hospital (Centers for Disease Control and Prevention (CDC), 2023; World Health Organization, 2022a).
• Separate Zones: Separate different areas, such as the waiting areas in the OPD building (especially the nurse stations and information desks), to provide efficient patient services and ensure patients can access information quickly. Additionally, distinct areas should be created for clinics and support spaces; the study by Page (2020) and Beggs et al. (2021) found that hospitals that segregated clinic areas from support spaces could reduce staff infection rates by up to 50%. With strict adherence to cleaning protocols.
• Reduce Surface Contact: Use sensors to minimize contact with frequently touched surfaces, such as sensor-controlled lights, automatic doors, and touchless faucets at various points, including hand washing stations. According to The Center for Health Design (2020), touchless devices significantly reduce infection transmission via surfaces.
• Adjust Furniture Layout and Arrangement: Arrange furniture with at least 1.5–2 m Page (2020) and Beggs et al. (2021) highlighted that spaced seating arrangements in waiting areas can reduce the risk of infection by up to 60%. of the distance between each piece. Use symbols or signage to designate safe seating areas. Choose furniture made from materials that are easy to clean and durable against disinfectants, such as metal, plastic, or water-resistant coated materials. Also, clearly define walkways and functional areas with directional signs to minimize the likelihood of people crossing paths.
• Develop Ventilation Systems: This recommendation aligns with the work of Allen and Ibrahim (2020), who emphasized that improving ventilation systems is one of the key factors in reducing the risk of airborne transmission within buildings. Heating, ventilation, air conditioning (HVAC) systems, and Ultraviolet Germicidal Irradiation (UVGI) should be implemented in all OPD clinic areas to enhance airflow in high-traffic spaces. This will also improve the efficiency of the air filtration system (Centers for Disease Control and Prevention (CDC), 2014; 2023).
6 Conclusion
This study provides a clearer understanding of the physical environmental challenges in waiting areas following the COVID-19 pandemic. This section summarizes the findings in response to the study’s objective, which focuses on identifying physical environmental issues within the outpatient department (OPD) at Walailak University Medical Center Hospital. Based on an assessment of the hospital’s physical environment, two fundamental problems were identified as key obstacles that hindered the hospital’s ability to adapt effectively to COVID-19 prevention guidelines.
The first issue is the lack of flexibility in building design. The structure and layout of the hospital do not support the ability to adapt or reconfigure spaces in response to urgent needs or changing circumstances. As a result, the hospital could not modify its facilities to comply effectively with the prevention guidelines issued by the U.S. Centers for Disease Control and Prevention and Thailand’s Ministry of Public Health. This inflexibility also limited space management efforts to control the spread of infectious diseases during high-risk periods.
The second issue is the lack of a systematic approach to space management that supports infection control measures. This is particularly evident in clinic waiting areas, which often experience overcrowding and poorly organized layouts. Such conditions significantly increase the risk of airborne disease transmission. In addition, the ventilation systems in most hospitals were not designed initially to prevent the spread of respiratory infections effectively.
The design guidelines for preventing respiratory infections were developed by systematically analyzing data collected from surveys, questionnaires, and focus group discussions. The findings reveal that user participation in the design process is critical in providing valuable insights that support the development of appropriate and practical solutions. Based on the results, the design recommendations can be categorized into two main approaches as follows:
(1) Improving Hospital Management: This approach focuses on enhancing the efficiency of management systems for preventing respiratory diseases, especially in the post-COVID-19 context. Hospitals need to reduce crowding among patients and visitors by implementing online service systems, enforcing social distancing measures in waiting areas, clearly controlling the number of people allowed in each time slot, and organizing the flow of people entering and exiting the facility. These measures aim to prevent the gathering of individuals in enclosed spaces.
(2) Improving Hospital Interior Design: The physical design should focus on creating an environment that helps reduce the spread of infections. Key recommendations, which we can achieve through our collective efforts, include establishing designated areas for patient screening before service, zoning spaces according to risk levels, minimizing high-touch surfaces that pose infection risks, and designing furniture and ventilation systems to promote proper air circulation and ease of cleaning. All of these factors are essential to enhancing the efficiency and suitability of the hospital’s physical environment.
7 Implications
This research enhances the understanding of designing outpatient department (OPD) buildings that can effectively prevent the spread of respiratory infections. Furthermore, the findings can be applied to the design of hospitals on an international scale. This research emphasizes the importance of user involvement in promoting improvements to the environment. The practical design guidelines summarized from the study to help reduce the spread of respiratory infections are as follows:
• Healthcare Facility Management: Healthcare facilities should prioritize reducing the number of users in the building. On an international level, this can be achieved by using an online patient registration system to promote physical distancing. It is recommended to maintain a distance of at least two meters between individuals.
• Space Design: The design process should consider and adhere to guidelines for respiratory infections, including elevating hygiene standards. Additionally, hospitals should ensure that there is an effective ventilation system for both indoor and outdoor air within the building.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JC: Software, Visualization, Data curation, Resources, Writing – original draft, Project administration, Conceptualization, Investigation, Writing – review and editing, Validation, Methodology, Supervision, Formal Analysis, Funding acquisition. SP: Formal Analysis, Supervision, Resources, Validation, Writing – review and editing, Data curation. TW: Resources, Formal Analysis, Supervision, Validation, Writing – review and editing, Data curation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the New Researcher Development Scheme Grant, Walailak University, Thailand, Grant Number WU67262.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Akanbi, F. A., Oladele, O. A., and Adetunji, O. S. (2017). The impact of physical environment design in hospital waiting areas on patients’ mood and satisfaction. J. Healthc. Des. Manag. 10, 123–131.
Allen, J. G., and Ibrahim, A. M. (2020). Indoor air changes and potential implications for SARS-CoV- 2 transmission. JAMA 324 (20), 2112–2113. doi:10.1001/jama.2021.5053
Amos, D., Au-Yong, C. P., and Musa, Z. N. (2020). Enhancing the role of facilities management in the fight against the COVID-19 (SARS-CoV-2) pandemic in developing countries' public hospitals. J. Facil. Manag. 19 (1), 22–31. doi:10.1108/JFM-06-2020-0034
Atkinson, J., Chartier, Y., Pessoa-Silva, C. L., Jensen, P., Li, Y., and Seto, W. H. (2021). Natural ventilation for infection control in health-care settings. World Health Organization.
Beauchemin, K. M., and Hays, P. (1996). Sunny hospital rooms expedite recovery from severe and refractory depressions. J. Affect. Disord. 40, 49–51. doi:10.1016/0165-0327(96)00040-7
Beggs, C. B., Shepherd, S. J., and Kerr, K. G. (2021). Increasing the ventilation rate in a hospital setting: a simple strategy to reduce the spread of airborne infections. J. Hosp. Infect. 107, 69–76.
Blomkvist, V., Eriksen, C. A., Theorell, T., Ulrich, R., and Rasmanis, G. (2005). Acoustics and psychosocial environment in intensive coronary care. Occup. Environ. Med. 62, 1–3. doi:10.1136/oem.2004.017632
Bryman, A., and Bell, E. (2011). Business research methods. Oxford, United Kingdom: Oxford University Press. Available online at: https://library.lincoln.ac.uk/items/122618 (Accessed August 10, 2024).
Centers for Disease Control and Prevention (CDC) (2014). Introduction to Public Health. In: Public Health 101 Series. Atlanta, GA: U.S. Department of Health and Human Services. Available online at: https://www.cdc.gov/publichealth101/epidemiology.html (Accessed August 20, 2024).
Centers for Disease Control and Prevention (CDC) (2023). Ventilation in building. Available online at: https://archive.cdc.gov/www_cdc_gov/coronavirus/2019-ncov/community/ventilation.html (Accessed August 20, 2024).
Cheung, E. (2020). Wuhan pneumonia: Thailand confirms first case of virus outside China. S. Morning Post.
Corbin, A., and Strauss, J. (2015). Basics of qualitative research. San California, USA: SAGE Publishing.
Douglas, C. H., and Douglas, M. R. (2004). Patient-centered improvements in healthcare built environments: perspectives and design indicators. Health Expect. 7, 264–276.
Erlingsson, C., and Brysiewicz, P. (2017). A hands-on guide to doing content analysis. Afr. J. Emerg. Med. 7 (3), 93–99. doi:10.1016/j.afjem.2017.08.001
Fronczek-Munter, A., and Prugsiganont, S. (2018). “Hospital architecture quality: exploratory observation on three continents,” in The 5th International Conference on Architecture and Built Environment Proceeding, Oslo, Norway (INTEF Academic Press), 156–165.
Geng, S., Chau, H.-W., Yan, S., Zhang, W., and Zhang, C. (2021). Comparative analysis of hospital environments in Australia and China using the space syntax approach. Int. J. Build. Pathol. Adapt. 39 (3), 525–546. doi:10.1108/ijbpa-04-2020-0031
Gilby, A., Blyth, A., and Barlex, M. J. (2006). Guide to post occupancy evaluation. London: Higher Education Funding Council for England, Association of University Directors of Estates.
Guilemany, J. M., Mariño-Sánchez, F. S., Angrill, J., Alobid, I., Centellas, S., Pujols, L., et al. (2011). The importance of smell in patients with bronchiectasis. Respir. Med. 105 (1), 44–49. doi:10.1016/j.rmed.2010.10.019
Gulwadi, G. B., Joseph, A., and Keller, A. B. (2009). Exploring the impact of the physical environment on patient outcomes in ambulatory care settings. HERD Health Environ. Res. Des. J. 2 (2), 21–41. doi:10.1177/193758670900200203
Hamilton, D. K., and Watkins, D. H. (2009). Evidence-based design for multiple building types. Wiley.
Health-care administration (2021). What is the difference between public and private hospital. Available online at: https://www.healthcare-administration-degree.net/faq/what-is-the-difference-between-a-public-and-private-hospital/(Accessed September 3, 2024).
Kevern, J., and Webb, C. (2001). Focus groups as a tool for critical social research in nurse education. Nurse Educ. Today 21 (4), 323–333. doi:10.1054/nedt.2001.0563
Kvande, M., Lykkeslet, E., and Storli, S. L. (2017). ICU nurses and physicians dialogue regarding patients’ clinical status and care options - a focus group study. nternational J. Qual. Stud. Health Well-being 12 (1), 1267346. doi:10.1080/17482631.2016.1267346
Malkin, J. (2008). “Evidence-based design,” in A visual reference to evidence-based design. The Center for Health Design, 2–18.
Mhalla, M. (2020). The impact of novel coronavirus (COVID-19) on the global oil and aviation markets. J. Asian Sci. Res. 10 (2), 96–104. doi:10.18488/journal.2.2020.102.96.104
Ministry of Public Health (2016). Health in Thailand. Available online at: https://muse.jhu.edu/pub/1/article/916341 (Accessed August 18, 2024).
Page, R. (2020). Use beyond usability: integrating user experience design and human factors to improve the usability of a cochlear implant charging system. Des. Health (Abingdon). 4, 122–137. doi:10.1080/24735132.2020.1727693
Pilosof, N. P. (2021). Building for change: comparative case study of hospital architecture. Health Environ. Res. and Des. J. 14, 47–60. doi:10.1177/1937586720927026
Preiser, W. F. E. (1995). Post-occupancy evaluation: how to make buildings work better. Bradford, West Yorkshire: MCB University Press, 13.
Preiser, W. F. E. (2001). “The evolution of post-occupancy evaluation: toward building performance and universal design evaluation,” in Federal Facilities Council Technical Report No. 145, Learning from our buildings: a state-of-the-practice summary of post-occupancy evaluation. Editor L. Stanley (Washington, D.C.: National Academy Press), 9–22.
Prugsiganont, S., and Jensen, P. A. (2019). Identification of space management problems in public hospitals: the case of Maharaj Chiang. Mai Hosp. 37 (7/8), 435–454. doi:10.1108/f-01-2018-0001
Ramanathan, R. (2001). A note on the use of the analytic hierarchy process for environmental impact assessment. J. Environ. Manag. 63 (1), 27–35. doi:10.1006/jema.2001.0455
Saaty, T. L. (1980). The analytic hierarchy process: planning, priority setting, resource allocation. McGraw-Hill.
Saunders, M., Lewis, P., and Thornhill, A. (2016). Research methods for business students. 7th ed. London, United Kingdom: Pearson.
Sng, G. K. H., Tan, M. K., Tay, H. L., Ong, B. C., Gómez, A., Obimpeh, M., et al. (2021). Impact of patient crowding and waiting times on infection transmission in outpatient clinics: a review of current evidence. Int. J. Environ. Res. Public Health 18 (9), 4657. doi:10.3390/ijerph18094657
Soria, A., Galimberti, S., Lapadula, G., Visco, F., Ardini, A., Valsecchi, M. G., et al. (2021). The high volume of patients admitted during the SARS-CoV-2 pandemic has an independent harmful impact on in-hospital mortality from COVID-19. PLoS One 16 (1), e0246170. doi:10.1371/journal.pone.0246170
Thai Health Coding Center (2021). Geographic information system. Available online at: http://thcc.or.th/download/GIS54.pdf September 9, 2024).
Thailand Ministry of Public Health (2020). Sentinel surveillance of COVID-19 in ARI and CAP patients. Available online at: https://ddc.moph.go.th/viralpneumonia/file/g_ari_pneumonia/g_ari_pneumonia_moph.pdf (Accessed August 27, 2024).
The Center for Health Design (2020). Reducing healthcare-associated infections through design. Concord, CA: The Center for Health Design.
Turpin-Brooks, S., and Viccars, G. (2006). The development of robust methods of post occupancy evaluation.
Ulrich, R., Zimring, C., Quan, X., Joseph, A., and Choudhary, R. (2004). “Reduce stress and improve outcomes and IV: improve overall healthcare quality,” in The role of the physical environment in the hospital of the 21st century. Concord, CA: The Center for Health Design, 15–24.
Ulrich, R., Zimring, C., Zhu, X., DuBose, J., Seo, H. B., Choi, Y. S., et al. (2008). A review of the research literature on evidence-based healthcare design. Health Environ. Res. and Des. J. 1, 61–125. doi:10.1177/193758670800100306
Verderber, S., and Refuerzo, B. J. (2006). Innovations in hospital architecture. New York: Routledge.
Waroonkun, T., and Prugsiganont, S. (2022). Preventing the spread of COVID-19 through environmental design in Thai community hospitals. Front. Built Environ. 8. doi:10.3389/fbuil.2022.947211
West, J. (2020). Design in healthcare: the challenge of translation. Des. Health 4 (2), 252–269. doi:10.1080/24735132.2020.1783880
World Health Organization (2022a). COVID-19 weekly epidemiological update. Available online at: https://apps.who.int/iris/handle/10665/355779 (Accessed September 9, 2024).
World Health Organization (2022b). Infection prevention and control. Available online at: https://www.who.int/health-services/infection-prevention-control (Accessed September 11, 2024).
Zhang, Q., Lu, L., and Pan, Y. (2020). Digital health management in public hospitals during the COVID-19 pandemic. BMC Public Health 20, 1358.
Keywords: physical environment, hospital, COVID-19, respiratory disease prevention, design guidelines
Citation: Chotirat J, Prugsiganont van der Hoeven S and Waroonkun T (2025) Design and improvement guidelines to promote wellbeing for patients and their family in government tertiary care hospitals. Front. Built Environ. 11:1615971. doi: 10.3389/fbuil.2025.1615971
Received: 22 April 2025; Accepted: 23 June 2025;
Published: 18 July 2025.
Edited by:
Bjørn Petter Jelle, Norwegian University of Science and Technology, NorwayReviewed by:
Grit Ngowtanasuwan, Mahasarakham University, ThailandHaowei Yao, Zhengzhou University of Light Industry, China
Copyright © 2025 Chotirat, Prugsiganont van der Hoeven and Waroonkun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Supuck Prugsiganont van der Hoeven, c3VwdWNrLnBAY211LmFjLnRo; Tanut Waroonkun, dGFudXQud0BjbXUuYWMudGg=
 Jutamat Chotirat
Jutamat Chotirat Supuck Prugsiganont van der Hoeven
Supuck Prugsiganont van der Hoeven Tanut Waroonkun
Tanut Waroonkun