- 1Department of Neurology, The Second Affiliated Hospital of Nanchang University, Nanchang, China
- 2Institute of Neuroscience, Nanchang University, Nanchang, Jiangxi, China
Loneliness has been reported to be associated with an increased risk of dementia; however, the extent of this relationship remains controversial. This study aimed to assess the strength of the relationship between loneliness and dementia using a meta-analysis approach. PubMed, EMBASE, and China National Knowledge Internet databases were systematically searched for potentially included studies from inception up to 17 February 2022. A meta-analysis was performed using a random-effects model to assess pooled relative risks (RRs) and 95% confidence intervals (CIs). A literature search identified 16 cohort studies (published in 15 articles), among which 4,625 dementia cases and 62,345 individuals were selected for further meta-analysis. Loneliness was associated with an increased risk of Alzheimer’s disease (AD) (RR: 1.72, 95% CI: 1.32–2.23; P < 0.001) and dementia (RR: 1.23, 95% CI: 1.16–1.31; P < 0.00001). However, no significant association between loneliness and risk of mild cognitive impairment (MCI) (RR: 1.34, 95% CI: 0.97–1.87; P = 0.080) or vascular dementia (VaD) (RR: 1.01, 95% CI: 0.51–1.99; P = 0.973) was observed. Results revealed that loneliness might increase the risk of Alzheimer’s disease and dementia. Early interventions that limit loneliness may reduce risk of dementia and Alzheimer’s disease.
Introduction
Dementia is a group of acquired clinical syndromes characterized by the progressive decline in cognition along with psychiatric and behavioral alterations of differing extents. The expected prevalence of the disease in the year 2050 is 152 million (Livingston et al., 2020). The incidence of Alzheimer’s disease (AD) and other types of dementia [mild cognitive impairment (MCI), vascular dementia (VaD), or all-cause dementia] have declined; MCI is a clinical stage on the continuum of cognitive decline between “normal aging” and dementia. It is characterized by impairment in cognition that is not severe enough to require help with activities of daily living (ADLs)/Instrumental activities of daily living (IADLs). Over time, the need for disability, health, and social care among the elderly population has increased (Satizabal et al., 2016). Currently, there is no cure for dementia. Prior studies have identified numerous risk factors for the disease; however, non-modifiable risk factors account for 50–70% of those previously identified (Diamond and Woo, 2014; Kuring et al., 2020). Since our understanding of modifiable risk factors is poor (Yeo et al., 2007; Hudson et al., 2012), further identification of modifiable risk factors is important.
Loneliness is experienced across the lifespan and across cultures. Most adults present transient symptoms of loneliness throughout the course of their lives (Victor et al., 2020; Schutter et al., 2021). Symptoms of loneliness and social isolation overlap; however, loneliness has been shown to be independently associated with health outcomes (Holt-Lunstad et al., 2015; Leigh-Hunt et al., 2017). Additionally, previous systematic reviews have found evidence that poor social relationships (i.e., socially integrated lifestyle, social engagement, and social activities) were associated with an increased risk of dementia (Kuiper et al., 2015; Penninkilampi et al., 2018). Moreover, symptoms of loneliness are particularly severe in individuals with mental illness, and have been associated with recovery delays and poor social functioning. In addition, loneliness has been associated with diabetes, hypertension, cardiovascular diseases, and dementia (Momtaz et al., 2012; Petitte et al., 2015).
A prior meta-analysis determined that loneliness is associated with an increased risk of dementia (Lara et al., 2019); however, several newly published articles were not included in the study (Luchetti et al., 2020; Rafnsson et al., 2020; Sundström et al., 2020; Sutin et al., 2020; Shibata et al., 2021; Freak-Poli et al., 2022; Salinas et al., 2022). Therefore, the strength of the association between loneliness and dementia remains unclear. To determine the extent to which loneliness is associated with dementia, additional assessment is needed. Here, we aimed to comprehensively analyze all available cohort studies to assess the association between loneliness and dementia among individuals of the general population.
Methods
Data sources, search strategy, and selection criteria
The meta-analysis of observational studies in epidemiology guidelines were applied to guide and report this meta-analysis (Stroup et al., 2000). An electronic searches were performed in PubMed, EMBASE, and the China National Knowledge Internet were used to identify eligible studies published from database inception to 17 February 2022. When performing searches, the following keywords were used: “loneliness” and “dementia.” Additional details regarding search strategies used for each database are shown in Supplementary Table 1. The searches were restricted to human studies, with no restrictions placed on the publication language. Citations of relevant publications were also reviewed to determine if they should be included in the meta-analysis. Unpublished data and additional information were obtained by contacting corresponding authors via e-mail. The most recent report was used if multiple studies used the same patient cohort.
Two investigators (LQ and GW) independently performed the literature search and study selection steps. Conflicts between investigators were settled via a group discussion until a consensus was reached. Studies were included if they met the following eligibility criteria: (1) cohort study design; (2) an exposure group experienced loneliness at baseline; (3) control group that experienced non-loneliness at baseline; (4) reported AD, MCI, dementia, or VaD as outcomes post-follow-up; and (5) patients followed-up >1 year.
Data collection and quality assessment
Two investigators (LQ and GW) independently collected the following information: first author’s name, publication year, location, sample size, female proportion, follow-up duration, mean age, or age range, loneliness measurement, reported outcome, number of cases, adjusted factors, and reported effect estimate. The same two investigators assessed the quality of included studies using the Newcastle-Ottawa Scale (NOS), which contains eight items and nine stars, as follows: selection (4 items, which were given a total possible number of 4 stars), comparability (1 item, 2 stars), and outcome (3 items, 3 stars) (Stang, 2010). Studies given 8 or 9 stars were considered to be of high quality. Discrepancies regarding data collection and quality assessment were resolved by a third author (ML) and by referring to the original report.
Statistical analysis
In each study, the relationship between loneliness and dementia risk was assessed via effect estimates and 95% confidence intervals (CIs). Given the cohort study design, hazard ratios were considered equivalent to relative risks (RRs). One article that included data from multiple population-based cohorts, we considered the analysis for each cohort as an independent study and extracted data separately (Freak-Poli et al., 2022). Analyses reporting RRs were maximally adjusted for potential confounders if the studies reported multivariate-adjusted outcome data. τ2 was applied to explore heterogeneity, and I2 was used to assess heterogeneity across included studies. Significant heterogeneity was defined as P < 0.10, as calculated using Cochran’s Q statistical test (Higgins and Thompson, 2002). If significant heterogeneity was not observed, pooled RRs with 95% CIs were calculated using a fixed-effect model, whereas a random-effects model was applied when a significant degree of heterogeneity was observed to take into account underlying variation among included studies (DerSimonian and Laird, 1986). Sensitivity analysis was performed to assess the robustness of pooled conclusions and explore potential sources of heterogeneity. Subgroup analyses were performed based on the following factors: validated loneliness measurement (yes vs. no), depression adjustment (yes vs. no), length of follow-up (≥10 vs. <10 years), geographical area (United States vs. Asian vs. European), and study quality (high vs. low). Publication bias was assessed via a visual inspection of funnel plots and Egger and Begg tests (Begg and Mazumdar, 1994; Egger et al., 1997; Higgins et al., 2003). The “trim and fill” method was applied to adjust for potentially significant publication bias (Duval and Tweedie, 2000). Moreover, population attributable risk (PAR) was calculated when a significant association between loneliness and dementia was observed using the following formula: PAR% = (Pe) (RR − 1)/[(Pe)(RR − 1) + 1] × 100, where the proportion of individuals exposed to loneliness was defined as Pe RR was obtained from the estimated RRs (Benichou, 2001). All reported P-values were two-sided, and those <0.05 were considered significant. Software Review Manager (version 5.3; Cochrane Collaboration, Oxford, UK) and STATA 12.0 (StataCorp, College Station, TX, USA) were used to perform all statistical analyses.
Results
Literature search
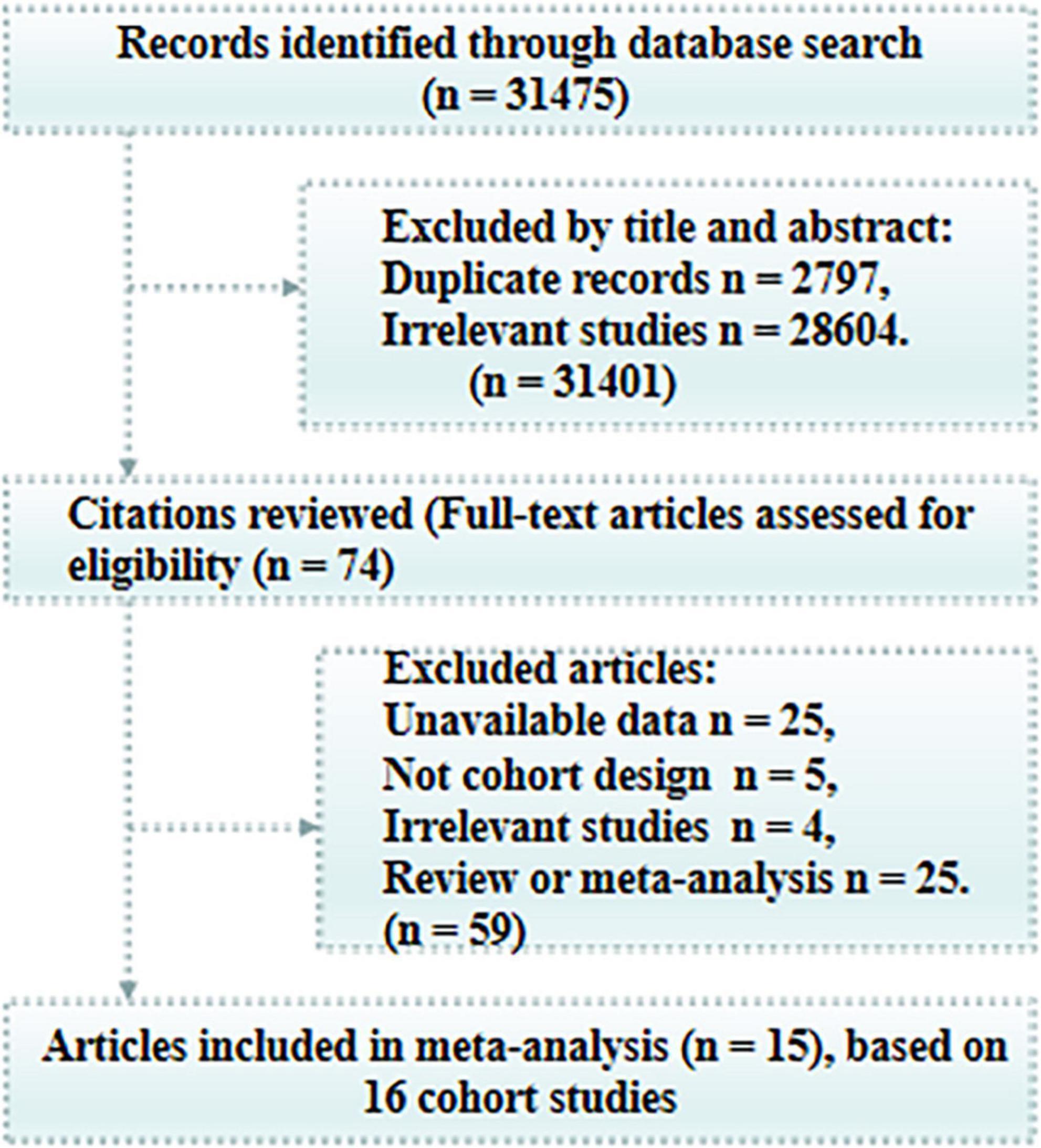
An initial electronic search produced 31,475 potentially relevant articles. Among these, 31,401 articles were excluded due to duplicate records or irrelevance based on a review of titles and abstracts. The remaining 74 potentially eligible articles were retrieved for full-text evaluation, which resulted in the exclusion of 59 due to insufficient data (n = 25), a review or meta-analysis design (n = 25), a non-cohort design (n = 5), or irrelevance (n = 4). Because one article reported the Rotterdam study and the Swedish National study separately (Freak-Poli et al., 2022), we considered the analysis for each cohort as an independent study. Finally, the remaining 16 cohort studies (published in 15 articles) were included in the final analysis (Figure 1; Zhang et al., 1999; Tilvis et al., 2004; Wilson et al., 2007; Lobo et al., 2008; Chen et al., 2011; Holwerda et al., 2014; Rawtaer et al., 2017; Zhou et al., 2018; Luchetti et al., 2020; Rafnsson et al., 2020; Sundström et al., 2020; Sutin et al., 2020; Shibata et al., 2021; Freak-Poli et al., 2022; Salinas et al., 2022).
Study characteristics
Characteristics of articles considered and baseline characteristics individuals included in the analysis are summarized in Supplementary Table 2. Among the 62,345 individuals identified from the 15 articles considered, 4,625 cases were reported. Among the articles considered, three were primarily conducted in the United States (Wilson et al., 2007; Sutin et al., 2020; Salinas et al., 2022), five in Asian countries (China, Japan, and Singapore) (Zhang et al., 1999; Chen et al., 2011; Rawtaer et al., 2017; Zhou et al., 2018; Shibata et al., 2021), and seven in European countries (Tilvis et al., 2004; Lobo et al., 2008; Holwerda et al., 2014; Luchetti et al., 2020; Rafnsson et al., 2020; Sundström et al., 2020; Freak-Poli et al., 2022). The sample size assessed in each article ranged from 650 to 14,411 individuals and the duration of follow-up ranged from 3 to 14 years. Among included articles, the proportion of individuals with dementia ranged from 3.3 to 14.3%, while that of loneliness-associated dementia was approximately 1.5%. Seven articles were considered to be of high quality (Supplementary Table 3; Wilson et al., 2007; Rawtaer et al., 2017; Luchetti et al., 2020; Sundström et al., 2020; Shibata et al., 2021; Freak-Poli et al., 2022; Salinas et al., 2022).
Loneliness and Alzheimer’s disease risk
The association between loneliness and AD risk was reported in three articles, which included 411 AD cases among a total of 3,900 individuals (Zhang et al., 1999; Wilson et al., 2007; Sundström et al., 2020). Among the group, loneliness was associated with an increased risk of AD (RR: 1.72, 95% CI: 1.32–2.23; P < 0.001; Figure 2). Further, a non-significant degree of heterogeneity was observed across articles (P = 0.30, I2 = 18%). No significant publication bias for AD was detected using either Begg (P = 1.000) or Egger (P = 0.503) tests. The PAR of dementia for loneliness in patients with AD was 7%.
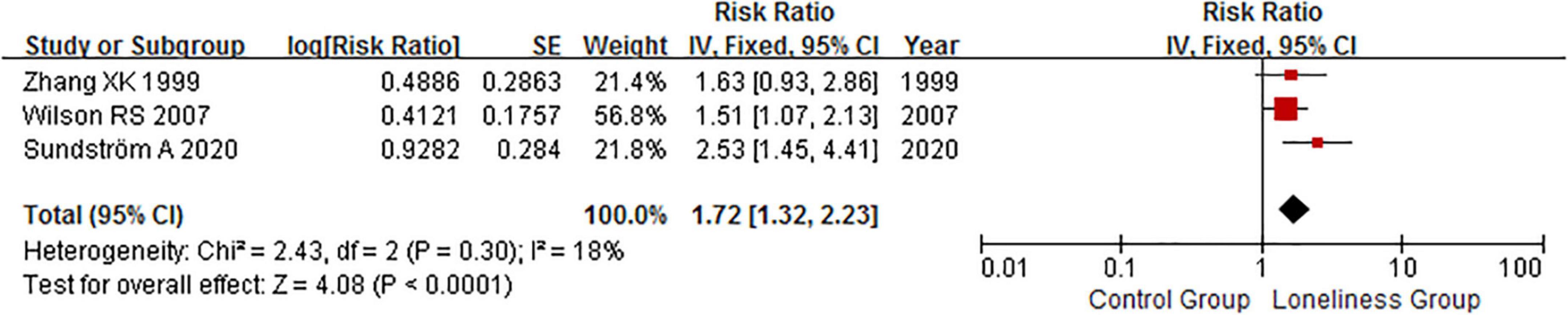
Figure 2. Fixed effects analysis of fully adjusted studies for the association between loneliness and Alzheimer’s disease (AD) risk. The square box in the graph portrays the weight that each study contributed to the analysis. CI, confidence interval; IV, inverse variance; SE, standard error; AD, Alzheimer’s disease.
Loneliness and mild cognitive impairment risk
An association between loneliness and MCI risk was reported in three articles, among which 821 MCI cases were considered among 16,715 individuals (Tilvis et al., 2004; Lobo et al., 2008; Luchetti et al., 2020). No significant association between loneliness and MCI risk was observed (RR: 1.34, 95% CI: 0.97–1.87; P = 0.080; Figure 3). Further, a significant degree of heterogeneity was detected (P = 0.05, I2 = 66%). Publication bias for MCI was not determined to be significant (PBegg = 0.296, PEgger = 0.499).
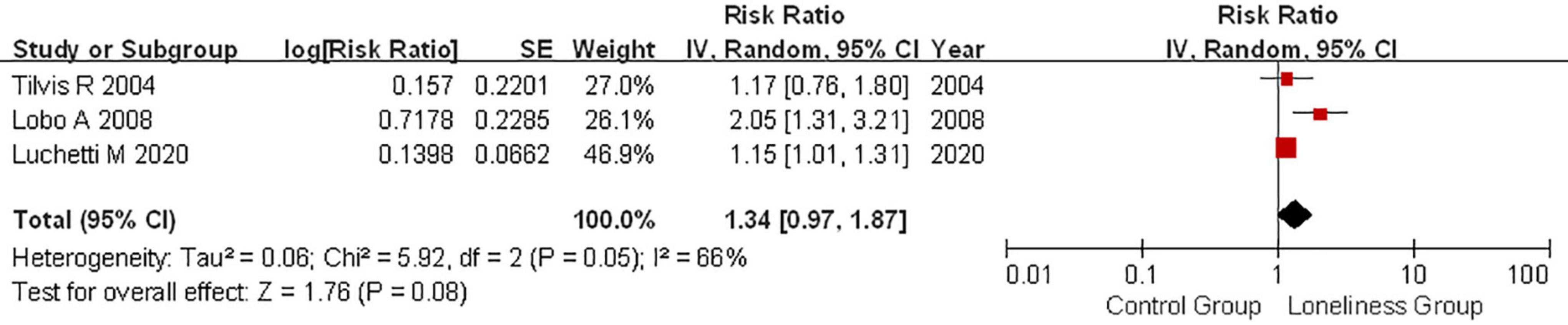
Figure 3. Random effects analysis of fully adjusted studies for the association between loneliness and mild cognitive impairment (MCI) risk. The square box in the graph portrays the weight that each study contributed to the analysis. CI, confidence interval; IV, inverse variance; SE, standard error; MCI, mild cognitive impairment.
Loneliness and dementia risk
The association between loneliness and dementia risk was reported in nine articles, with 3,648 dementia cases reported among 42,034 individuals (Chen et al., 2011; Holwerda et al., 2014; Zhou et al., 2018; Rafnsson et al., 2020; Sundström et al., 2020; Sutin et al., 2020; Shibata et al., 2021; Freak-Poli et al., 2022; Salinas et al., 2022). Notably, loneliness was associated with an increased risk of dementia (RR: 1.23, 95% CI: 1.16–1.31; P < 0.00001; Figure 4). No evidence of heterogeneity across articles (P = 0.27, I2 = 19%) was observed (Supplementary Figure 1). Both the Begg and the Egger test suggested borderline evidence of publication bias (PBegg = 0.074, PEgger = 0.015). Fixed-effects RR corrected for publication bias using the trim and fill method was (RR: 1.21, 95% CI: 1.13–1.29; P < 0.00001) for all articles combined. Correction for potential publication bias therefore did not materially alter the combined risk estimate. The PAR of dementia among those experiencing loneliness was 2%.
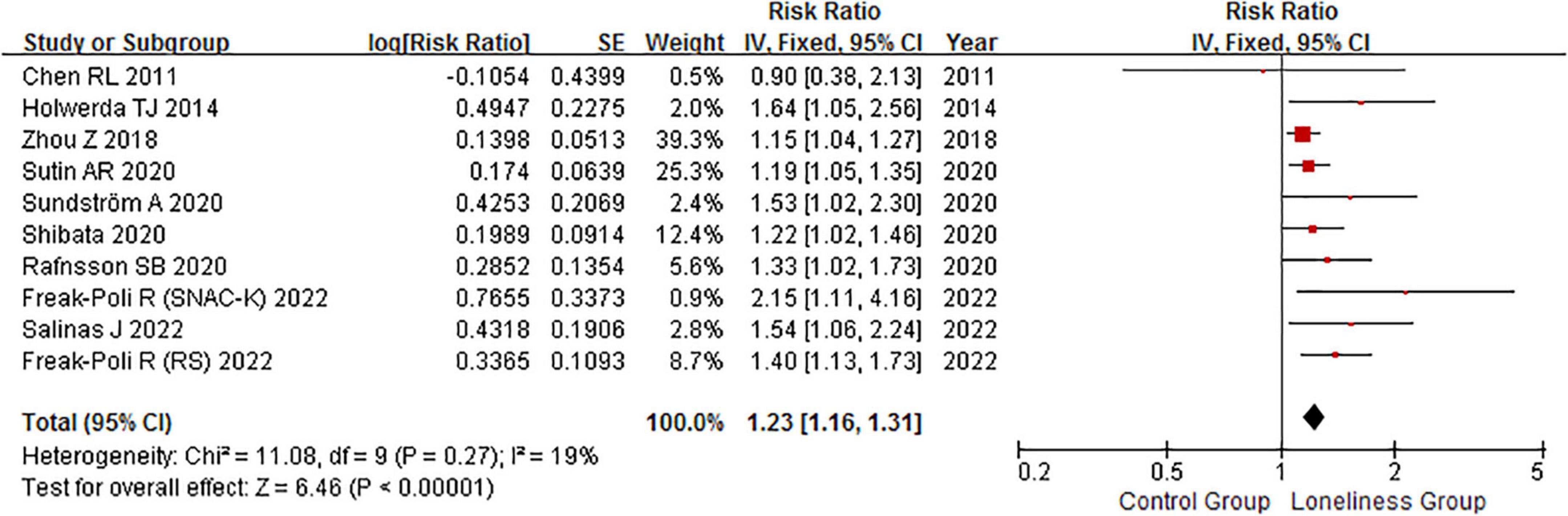
Figure 4. Fixed effects analysis of fully adjusted studies for the association between loneliness and dementia risk. The square box in the graph portrays the weight that each study contributed to the analysis. CI, confidence interval; IV, inverse variance; SE, standard error.
Loneliness and the risk of vascular dementia
One article reported an association between loneliness and VaD, with 157 VaD cases reported among 1,905 included individuals (Sundström et al., 2020). We found no significant association between loneliness and VaD risk (RR: 1.01, 95% CI: 0.51–1.99; P = 0.973).
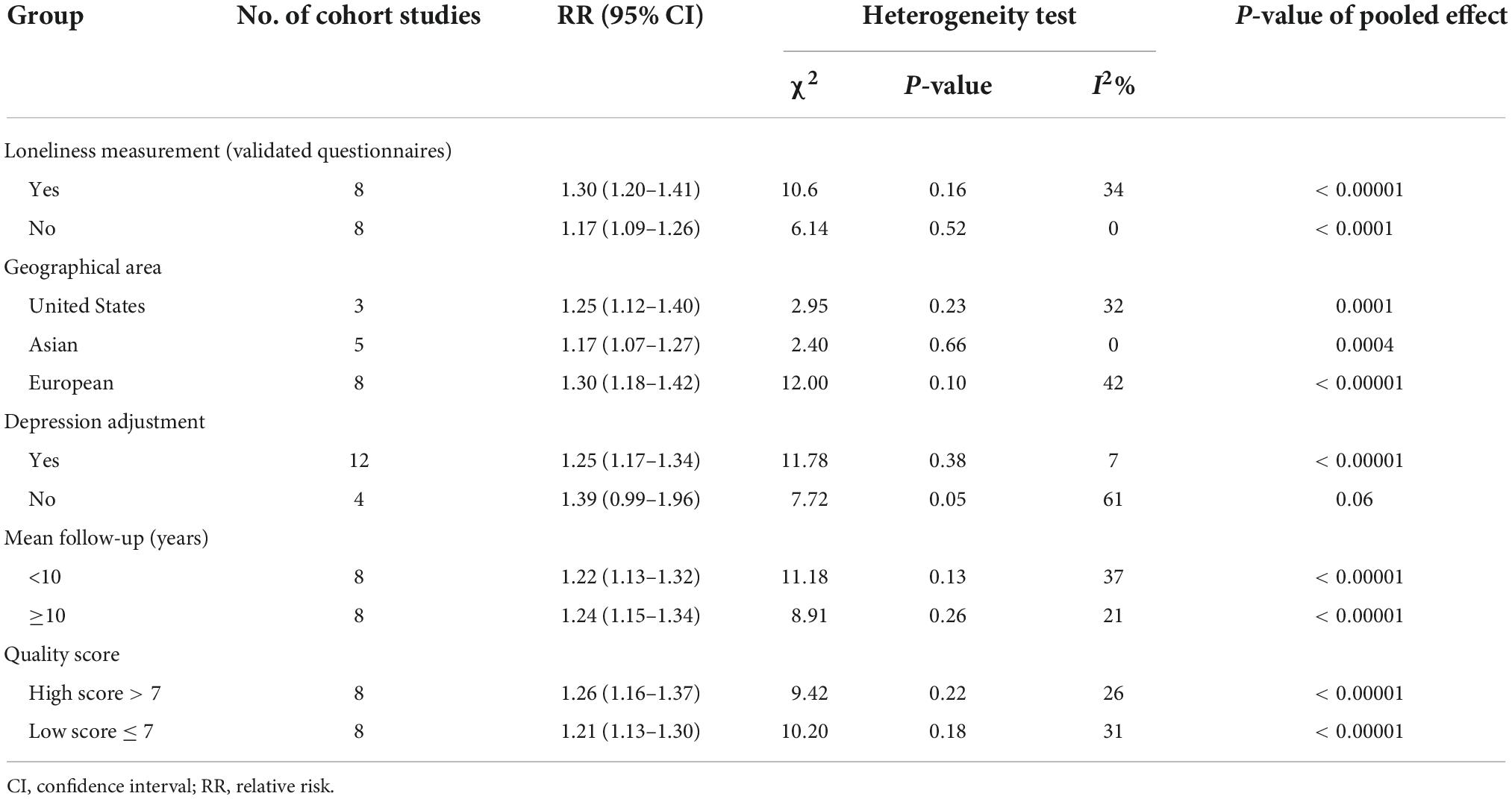
Subgroup and sensitivity analyses
Subgroup analysis of the relationship between loneliness and dementia risk is shown in Table 1. In all subgroups, loneliness was associated with dementia, except within articles that failed to adjust for depressive symptoms (RR: 1.39, 95% CI: 0.99–1.96; P = 0.060; I2 = 61%). Moreover, the strength of the association between loneliness and dementia was greater among articles with the following characteristics: used validated questionnaires, performed in Europe, and had a follow-up duration ≥10.0 years. The strength of the association between loneliness and dementia risk among subgroups was similar when assessed using quality score. Sensitivity analysis indicated that the results of the present meta-analysis were stable after sequentially removing individual articles (data not shown). Pooled RRs for dementia ranged from 1.22 (95% CI: 1.15–1.29, with Freak-Poli et al., excluded) to 1.27 (95% CI: 1.19–1.35; with Zhou et al., excluded).
Discussion
We report that loneliness is associated with an increased risk of AD and dementia, while no significant association between loneliness and MCI risk or VaD was observed. Loneliness has previously been identified as a risk factor for premature mortality (Holt-Lunstad et al., 2015; Schutter et al., 2021), adverse biological parameters (e.g., hypertension), health-risk behaviors (including smoking, physical inactivity, and excess alcohol consumption), physical and mental morbidity, and increased health service use (Hawkley et al., 2009; Shankar et al., 2011; Dyal and Valente, 2015). However, the strength of this relationship between loneliness and dementia remains unclear. The current updated meta-analysis considered 4,625 cases of dementia among 62,345 individuals included in 16 cohort studies. Characteristics of both studies and individuals considered ranged widely.
Numerous studies have reported a potential link between loneliness and dementia risk (Wilson et al., 2007; Lobo et al., 2008; Holwerda et al., 2014; Zhou et al., 2018; Luchetti et al., 2020; Rafnsson et al., 2020; Sundström et al., 2020; Sutin et al., 2020; Shibata et al., 2021; Freak-Poli et al., 2022; Salinas et al., 2022); however, several failed to identify a significant association between loneliness and dementia risk (Zhang et al., 1999; Tilvis et al., 2004; Chen et al., 2011; Rawtaer et al., 2017). An earlier meta-analysis found that loneliness was associated with an increased risk of dementia (Lara et al., 2019), a result that was consistent with a study conducted by Luchetti et al. (2020) and the Singapore Longitudinal Aging Study (Rawtaer et al., 2017) included in a prior meta-analysis were limited to those published by November 2018. Since then, seven additional articles on the topic have been published (Luchetti et al., 2020; Rafnsson et al., 2020; Sundström et al., 2020; Sutin et al., 2020; Shibata et al., 2021; Freak-Poli et al., 2022; Salinas et al., 2022). To clarify the putative association between loneliness and dementia, an additional meta-analysis of relevant articles should be conducted.
Studies have demonstrated that loneliness is significantly related to unhealthy behaviors, which may affect cognition or increase risk of cardiometabolic diseases (Lara et al., 2019). Several plausible mechanisms have been put forward including: cognitive activity and neural reserve decreases when neural responses of loneliness are triggered and brain-derived neurotrophic factor is downregulated (Wilson et al., 2007). Further, studies have shown that genetic mechanisms may link loneliness and dementia (Salinas et al., 2017; Hsiao et al., 2018). Loneliness may increase amyloid burden in the elderly, with those individuals carrying APOE4 displaying altered amyloid-related mechanisms (Donovan et al., 2016; Ge et al., 2018). Loneliness is significantly related to depression risk, indicating that depression may affect cognitive decline and dementia (Cacioppo et al., 2010). Our study revealed that the relationship between loneliness and dementia risk may be affected by adjustment for depressive symptoms. This may be explained by the observation that depressive symptoms and social involvement may affect loneliness, which is significantly associated with dementia risk.
The strengths of this study are as follows: (1) it exclusively included cohort studies, which minimized selection and recall biases; (2) the analysis was based on a large sample size, making study findings more robust than those of any individual study; (3) PAR was calculated so that RR and PAR could be used to assess distributions of risk factors; and (4) all included studies were published after 1999 and included relatively complete data.
Several limitations of this study should be acknowledged. First, loneliness was assessed using various questionnaires; therefore, information bias may have affected findings. Second, loneliness was assessed at baseline, which may have affected the assessment of loneliness severity. Third, loneliness was assessed using questionnaires distributed via postal mail, and the dementia classification of individuals was not available in medical records. Fourth, factors for which data was adjusted varied among studies included in the meta-analysis. This may have affected the assessment of the progression of dementia. Finally, the analysis was based on published articles and pooled data, a study design that is susceptible to publication bias and restricts the analysis of patient details.
Conclusion
This study revealed that loneliness may increase risk of developing both AD and dementia. Early interventions that limit loneliness may reduce risk of AD and dementia.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
ML was the guarantor, conceived, and designed the study. LQ and GW searched the databases and checked these according to the eligible criteria, exclusion criteria, extracted the quantitative data, and wrote the draft of the manuscript. ZT helped develop search strategies. SZ, MY, and JM analyzed the data. All authors contributed in writing, reviewing, or revising the manuscript.
Funding
This study was supported by the Jiangxi Applied Development Special Fund for Health Science and Technology Development (No. 20181BBG78036). The funders had no role in the design of the study, collection, analysis, and interpretation of data, or manuscript writing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnhum.2022.899814/full#supplementary-material
References
Begg, C. B., and Mazumdar, M. (1994). Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–1101.
Benichou, J. (2001). A review of adjusted estimators of attributable risk. Stat. Methods Med. Res. 10, 195–216. doi: 10.1177/096228020101000303
Cacioppo, J. T., Hawkley, L. C., and Thisted, R. A. (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago health, aging, and social relations study. Psychol. Aging 25, 453–463. doi: 10.1037/a0017216
Chen, R., Hu, Z., Wei, L., Ma, Y., Liu, Z., and Copeland, J. R. (2011). Incident dementia in a defined older Chinese population. PLoS One 6:e24817. doi: 10.1371/journal.pone.0024817
DerSimonian, R., and Laird, N. (1986). Meta-analysis in clinical trials. Control. Clin. Trials 7, 177–188. doi: 10.1016/0197-2456(86)90046-2
Diamond, A. G., and Woo, B. K. (2014). Duration of residence and dementia literacy among Chinese Americans. Int. J. Soc. Psychiatry 60, 406–409. doi: 10.1177/0020764013491742
Donovan, N. J., Okereke, O. I., Vannini, P., Amariglio, R. E., Rentz, D. M., Marshall, G. A., et al. (2016). Association of higher cortical amyloid burden with loneliness in cognitively normal older adults. JAMA Psychiatry 73, 1230–1237. doi: 10.1001/jamapsychiatry.2016.2657
Duval, S., and Tweedie, R. (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56, 455–463. doi: 10.1111/j.0006-341x.2000.00455.x
Dyal, S. R., and Valente, T. W. (2015). A systematic review of loneliness and smoking: Small effects, big implications. Subst. Use Misuse 50, 1697–1716. doi: 10.3109/10826084.2015.1027933
Egger, M., Davey Smith, G., Schneider, M., and Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634. doi: 10.1136/bmj.315.7109.629
Freak-Poli, R., Wagemaker, N., Wang, R., Lysen, T. S., Ikram, M. A., Vernooij, M. W., et al. (2022). Loneliness, not social support, is associated with cognitive decline and dementia across two longitudinal population-based cohorts. J. Alzheimers Dis. 85, 295–308. doi: 10.3233/JAD-210330
Ge, T., Sabuncu, M. R., Smoller, J. W., Sperling, R. A., and Mormino, E. C. (2018). Dissociable influences of APOE ε4 and polygenic risk of AD dementia on amyloid and cognition. Neurology 90, e1605–e1612. doi: 10.1212/WNL.0000000000005415
Hawkley, L. C., Thisted, R. A., and Cacioppo, J. T. (2009). Loneliness predicts reduced physical activity: Cross-sectional & longitudinal analyses. Health Psychol. 28, 354–363. doi: 10.1037/a0014400
Higgins, J. P., and Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558. doi: 10.1002/sim.1186
Higgins, J. P., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ 327, 557–560. doi: 10.1136/bmj.327.7414.557
Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., and Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect. Psychol. Sci. 10, 227–237. doi: 10.1177/1745691614568352
Holwerda, T. J., Deeg, D. J., Beekman, A. T., van Tilburg, T. G., Stek, M. L., Jonker, C., et al. (2014). Feelings of loneliness, but not social isolation, predict dementia onset: Results from the Amsterdam study of the elderly (AMSTEL). J. Neurol. Neurosurg. Psychiatry 85, 135–142. doi: 10.1136/jnnp-2012-302755
Hsiao, Y. H., Chang, C. H., and Gean, P. W. (2018). Impact of social relationships on Alzheimer’s memory impairment: Mechanistic studies. J. Biomed. Sci. 25:3. doi: 10.1186/s12929-018-0404-x
Hudson, J. M., Pollux, P. M., Mistry, B., and Hobson, S. (2012). Beliefs about Alzheimer’s disease in Britain. Aging Ment. Health 16, 828–835. doi: 10.1080/13607863.2012.660620
Kuiper, J. S., Zuidersma, M., Oude Voshaar, R. C., Zuidema, S. U., van den Heuvel, E. R., Stolk, R. P., et al. (2015). Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res. Rev. 22, 39–57. doi: 10.1016/j.arr.2015.04.006
Kuring, J. K., Mathias, J. L., and Ward, L. (2020). Risk of dementia in persons who have previously experienced clinically-significant depression, anxiety, or PTSD: A systematic review and meta-analysis. J. Affect. Disord. 274, 247–261. doi: 10.1016/j.jad.2020.05.020
Lara, E., Martín-María, N., De la Torre-Luque, A., Koyanagi, A., Vancampfort, D., Izquierdo, A., et al. (2019). Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Res. Rev. 52, 7–16. doi: 10.1016/j.arr.2019.03.002
Leigh-Hunt, N., Bagguley, D., Bash, K., Turner, V., Turnbull, S., Valtorta, N., et al. (2017). An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 152, 157–171. doi: 10.1016/j.puhe.2017.07.035
Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., et al. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396, 413–446. doi: 10.1016/S0140-6736(20)30367-6
Lobo, A., López-Antón, R., de-la-Cámara, C., Quintanilla, M. A., Campayo, A., and Saz, P. (2008). Non-cognitive psychopathological symptoms associated with incident mild cognitive impairment and dementia, Alzheimer’s type. Neurotox. Res. 14, 263–272. doi: 10.1007/BF03033815
Luchetti, M., Terracciano, A., Aschwanden, D., Lee, J. H., Stephan, Y., and Sutin, A. R. (2020). Loneliness is associated with risk of cognitive impairment in the survey of health, ageing and retirement in Europe. Int. J. Geriatr. Psychiatry 35, 794–801. doi: 10.1002/gps.5304
Momtaz, Y. A., Hamid, T. A., Yusoff, S., Ibrahim, R., Chai, S. T., Yahaya, N., et al. (2012). Loneliness as a risk factor for hypertension in later life. J. Aging Health 24, 696–710. doi: 10.1177/0898264311431305
Penninkilampi, R., Casey, A. N., Singh, M. F., and Brodaty, H. (2018). The association between social engagement, loneliness, and risk of dementia: A systematic review and meta-analysis. J. Alzheimers Dis. 66, 1619–1633. doi: 10.3233/JAD-180439
Petitte, T., Mallow, J., Barnes, E., Petrone, A., Barr, T., and Theeke, L. (2015). A systematic review of loneliness and common chronic physical conditions in adults. Open Psychol. J. 8, 113–132. doi: 10.2174/1874350101508010113
Rafnsson, S. B., Orrell, M., d’Orsi, E., Hogervorst, E., and Steptoe, A. (2020). Loneliness, social integration, and incident dementia over 6 years: Prospective findings from the English longitudinal study of ageing. J. Gerontol. B Psychol. Sci. Soc. Sci. 75, 114–124. doi: 10.1093/geronb/gbx087
Rawtaer, I., Gao, Q., Nyunt, M. S., Feng, L., Chong, M. S., Lim, W. S., et al. (2017). Psychosocial risk and protective factors and incident mild cognitive impairment and dementia in community dwelling elderly: Findings from the Singapore longitudinal ageing study. J. Alzheimers Dis. 57, 603–611. doi: 10.3233/JAD-160862
Salinas, J., Beiser, A., Himali, J. J., Satizabal, C. L., Aparicio, H. J., Weinstein, G., et al. (2017). Associations between social relationship measures, serum brain-derived neurotrophic factor, and risk of stroke and dementia. Alzheimers Dement. 3, 229–237. doi: 10.1016/j.trci.2017.03.001
Salinas, J., Beiser, A. S., Samra, J. K., O’Donnell, A., Donnell, A., DeCarli, C. S., et al. (2022). Association of loneliness with 10-year dementia risk and early markers of vulnerability for neurocognitive decline. Neurology 98, e1337–e1348. doi: 10.1212/WNL.0000000000200039
Satizabal, C. L., Beiser, A. S., Chouraki, V., Chêne, G., Dufouil, C., and Seshadri, S. (2016). Incidence of dementia over three decades in the Framingham heart study. N. Engl. J. Med. 374, 523–532. doi: 10.1056/NEJMoa1504327
Schutter, N., Holwerda, T. J., Comijs, H. C., Naarding, P., Van, R., Dekker, J., et al. (2021). Loneliness, social network size, and mortality in older adults and the role of cortisol. Aging Ment. Health 25, 2246–2254. doi: 10.1080/13607863.2020.1843001
Shankar, A., McMunn, A., Banks, J., and Steptoe, A. (2011). Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 30, 377–385. doi: 10.1037/a0022826
Shibata, M., Ohara, T., Hosoi, M., Hata, J., Yoshida, D., Hirabayashi, N., et al. (2021). Emotional loneliness is associated with a risk of dementia in a general Japanese older population: The Hisayama study. J. Gerontol. B Psychol. Sci. Soc. Sci. 76, 1756–1766. doi: 10.1093/geronb/gbaa196
Stang, A. (2010). Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25, 603–605. doi: 10.1007/s10654-010-9491-z
Stroup, D. F., Berlin, J. A., Morton, S. C., Olkin, I., Williamson, G. D., Rennie, D., et al. (2000). Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283, 2008–2012. doi: 10.1001/jama.283.15.2008
Sundström, A., Adolfsson, A. N., Nordin, M., and Adolfsson, R. (2020). Loneliness increases the risk of all-cause dementia and Alzheimer’s disease. J. Gerontol. B Psychol. Sci. Soc. Sci. 75, 919–926. doi: 10.1093/geronb/gbz139
Sutin, A. R., Stephan, Y., Luchetti, M., and Terracciano, A. (2020). Loneliness and risk of dementia. J. Gerontol. B Psychol. Sci. Soc. Sci. 75, 1414–1422. doi: 10.1093/geronb/gby112
Tilvis, R. S., Kähönen-Väre, M. H., Jolkkonen, J., Valvanne, J., Pitkala, K. H., and Strandberg, T. E. (2004). Predictors of cognitive decline and mortality of aged people over a 10-year period. J. Gerontol. A Biol. Sci. Med. Sci. 59, 268–274. doi: 10.1093/gerona/59.3.m268
Victor, C. R., Rippon, I., Nelis, S. M., Martyr, A., Litherland, R., Pickett, J., et al. (2020). Prevalence and determinants of loneliness in people living with dementia: Findings from the IDEAL programme. Int. J. Geriatr. Psychiatry 35, 851–858. doi: 10.1002/gps.5305
Wilson, R. S., Krueger, K. R., Arnold, S. E., Schneider, J. A., Kelly, J. F., Barnes, L. L., et al. (2007). Loneliness and risk of Alzheimer disease. Arch. Gen. Psychiatry 64, 234–240. doi: 10.1001/archpsyc.64.2.234
Yeo, L. H., Horan, M. A., Jones, M., and Pendleton, N. (2007). Perceptions of risk and prevention of dementia in the healthy elderly. Dement. Geriatr. Cogn. Disord. 23, 368–371. doi: 10.1159/000101338
Zhang, X. K., Li, C. B., Zhang, M. Y., and He, Y. L. (1999). Psychosocial risk factors for Alzheimer’s disease. Chin. Med. J. 79, 335–338.
Keywords: loneliness, meta-analysis, dementia, cohort study, Alzheimer’s disease
Citation: Qiao L, Wang G, Tang Z, Zhou S, Min J, Yin M and Li M (2022) Association between loneliness and dementia risk: A systematic review and meta-analysis of cohort studies. Front. Hum. Neurosci. 16:899814. doi: 10.3389/fnhum.2022.899814
Received: 21 March 2022; Accepted: 16 November 2022;
Published: 01 December 2022.
Edited by:
Julia Christl, LVR Klinik Düsseldorf, GermanyReviewed by:
Klaus Peter Ebmeier, University of Oxford, United KingdomAntonio Guaita, Fondazione Golgi Cenci, Italy
Teruyuki Matsuoka, Kyoto Prefectural University of Medicine, Japan
Copyright © 2022 Qiao, Wang, Tang, Zhou, Min, Yin and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Min Li, bWlubGkyMDEyQHNpbmEuY29t
†These authors have contributed equally to this work
 Luyao Qiao
Luyao Qiao Gege Wang1†
Gege Wang1† Min Li
Min Li