- 1Faculty of Psychotherapy Science, Sigmund Freud Private University, Vienna, Austria
- 2Department of Religious Studies, University of Vienna, Vienna, Austria
- 3Center for Integrative Addiction Research (CIAR), Grüner Kreis Association, Vienna, Austria
- 4Department of Psychiatry and Psychotherapeutic Medicine, Medical University of Graz, Graz, Austria
This focused review integrates theoretical and empirical work from developmental neuroscience, attachment theory, and psychodynamic psychotherapy to reconceptualize addiction as a disorder rooted in disrupted attachment and altered brain function. Drawing on both clinical and research findings, it explores how early relational trauma contributes to dysregulation of stress-response systems and functional changes in brain regions involved in self-awareness, emotion regulation, and reward processing. Particular attention is given to the insular cortex and its role in interoception as it relates to addictive behavior. EEG neurofeedback is introduced as an emerging therapeutic tool, illustrated through a clinical case study that demonstrates how its combination with psychodynamic therapy can foster both neurophysiological regulation and emotional insight. This work supports a view of addiction as a disconnection from bodily and relational signals, rooted in early attachment experiences, and contributes to a more integrative, developmentally informed treatment model.
1 Introduction
Addiction is now widely recognized as a condition emerging from a complex interplay of biological, psychological, and social factors. The World Health Organization’s early definition (1964) remains influential, describing addiction as a state of periodic or chronic intoxication caused by repeated use of natural or synthetic substances, which is harmful to both the individual and society (as cited in Möller et al., 2015). Contemporary perspectives have expanded this definition to encompass behavioral addictions as well. Factors such as substance availability, individual vulnerabilities, and environmental influences-including family dynamics, peer relationships, and life stressors-interact to shape an individual’s trajectory toward substance use and addiction (Volkow et al., 2016).
The idea that addiction may stem from disrupted attachment patterns dates back to Sigmund Freud. Although Freud did not formulate a comprehensive theory of addiction, he observed that removing the substance alone was insufficient for successful treatment (Freud, 1898). His broader conceptualization of sexuality and relational drives aligns with modern psychodynamic and attachment-oriented models, which emphasize the importance of personality structure and developmental history in understanding addiction (Zellner et al., 2011). In line with this, Orford (2001) conceptualized addiction as a form of excessive appetite and behavioral fixation—an intense attachment to an activity that becomes uncontrollable despite adverse consequences. Similarly, Khantzian (2013) described addiction as a maladaptive strategy for emotional self-regulation, reflecting deeper disturbances in personality organization.
Attachment theory, originally developed by Bowlby and Ainsworth (Bretherton, 2013), posits that early relational experiences shape enduring internal working models of self and others. These models influence affect regulation and interpersonal functioning throughout life. Ainsworth’s Strange Situation Test (Ainsworth et al., 2015) identified four attachment patterns: secure, insecure-avoidant, insecure-ambivalent, and disorganized. Disorganized attachment—often linked to early trauma and inconsistent caregiving—is particularly relevant to later psychopathology, including substance use disorders (see Mikulincer and Shaver, 2012 for an in-depth discussion).
2 Addiction as an attachment disorder
In the postscript to Attachment Across the Life Cycle, John Bowlby observed, “Once we postulate the presence within the organism of an attachment behavioral system regarded as the product of evolution and as having protection as its biological function, many of the puzzles that have perplexed students of human relationships are found to be soluble” (Parkes et al., 2006, p. 293). This evolutionary framework supports the proposition that addiction can be conceptualized as an attachment disorder—particularly when viewed through the lens of relational trauma and disrupted affect regulation.
Our empirical findings support this interpretation. In a study conducted within a long-term therapeutic community setting, individuals with substance use disorders (SUD) exhibited elevated levels of insecure attachment and traits associated with borderline personality organization (Hiebler-Ragger et al., 2016). A follow-up study found that while patients with insecure attachment were initially less likely to drop out of therapy, their trust in self and others—an indicator of secure attachment—tended to decline during early treatment (Fuchshuber et al., 2018). This may reflect a transition from initial idealization of the therapeutic environment to a more realistic appraisal, which could facilitate more adaptive therapeutic engagement.
Conversely, other findings revealed a negative association between insecure attachment and both therapy motivation and therapeutic alliance in similar populations (Rübig et al., 2021). Additionally, data from a non-clinical sample showed a negative correlation between disorganized attachment and the use of sedatives and opioids (Fuchshuber et al., 2025b). These mixed results underscore the complex and context-dependent role of attachment in the etiology of addiction and in shaping treatment responsiveness (Fuchshuber and Unterrainer, 2020).
3 A neuro-evolutionary view of attachment and addiction
From a neuro-evolutionary perspective, attachment is understood as a biologically rooted motivational and behavioral system shaped by early interactions with caregivers. This system is closely linked to affect regulation, social bonding, and neurobiological development (Schindler, 2019). Feldman (2017) identified distinct neural circuits that underlie familial, romantic, and platonic attachments, each engaging specific affective and cognitive processes. Our work has been strongly influenced by Jaak Panksepp’s theory of primary emotional systems (Panksepp and Biven, 2012), which include SEEKING, LUST, CARE, ANGER, FEAR, PANIC, and PLAY. These systems originate in subcortical brain structures such as the brainstem and periaqueductal gray (PAG), and they shape more complex emotional experiences—such as empathy, guilt, or shame—that are processed in neocortical regions associated with mentalization and mindfulness.
Although Mac Lean (1990) triune brain model has been criticized for oversimplification (Barratt, 2015), it remains a useful heuristic for conceptualizing the relationships between emotion, personality, and cognition (see Figure 1 for further illustration). In our own studies, we used behavioral data to explore how Big Five personality traits mediate the relationship between primary emotional systems and religious-spiritual well-being. We found that CARE (positively) and ANGER (negatively) predicted spiritual well-being. When personality traits were included as mediators, these effects diminished, while extraversion and agreeableness emerged as significant predictors (Hiebler-Ragger et al., 2018). To address a conceptual gap, we developed a German-language LUST scale and integrated it into our version of the Brief Affective Neuroscience Personality Scales (BANPS–GL; Fuchshuber et al., 2022, 2023).
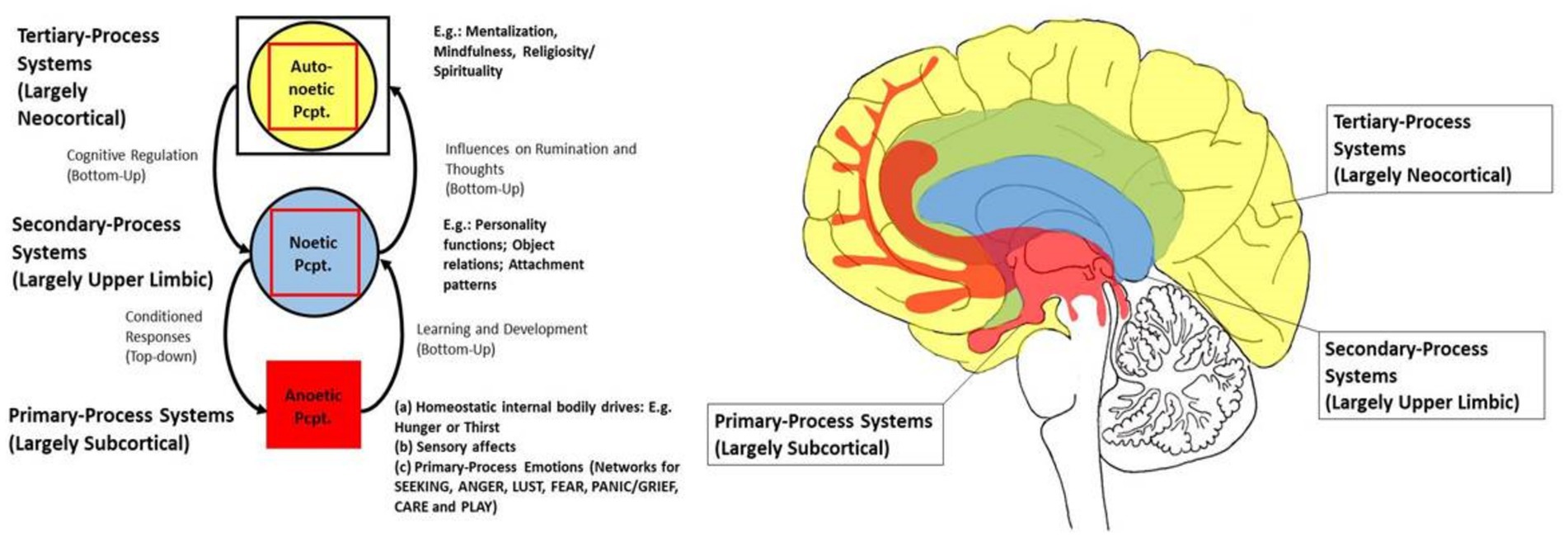
Figure 1. The triune brain model [based on Panksepp and Biven, 2012, Solms and Panksepp, 2012, and Kernberg, 2015]; Original sketch drawn by Jürgen Fuchshuber (slightly adapted; used with kind permission); Pcpt., perception.
Animal and human studies alike show that similar neural circuits are activated during SEEKING and social bonding, particularly involving dopaminergic pathways connecting the amygdala and nucleus accumbens to the prefrontal cortex (Barrett et al., 2013; Coan, 2010; see Figure 2 for further illustration).
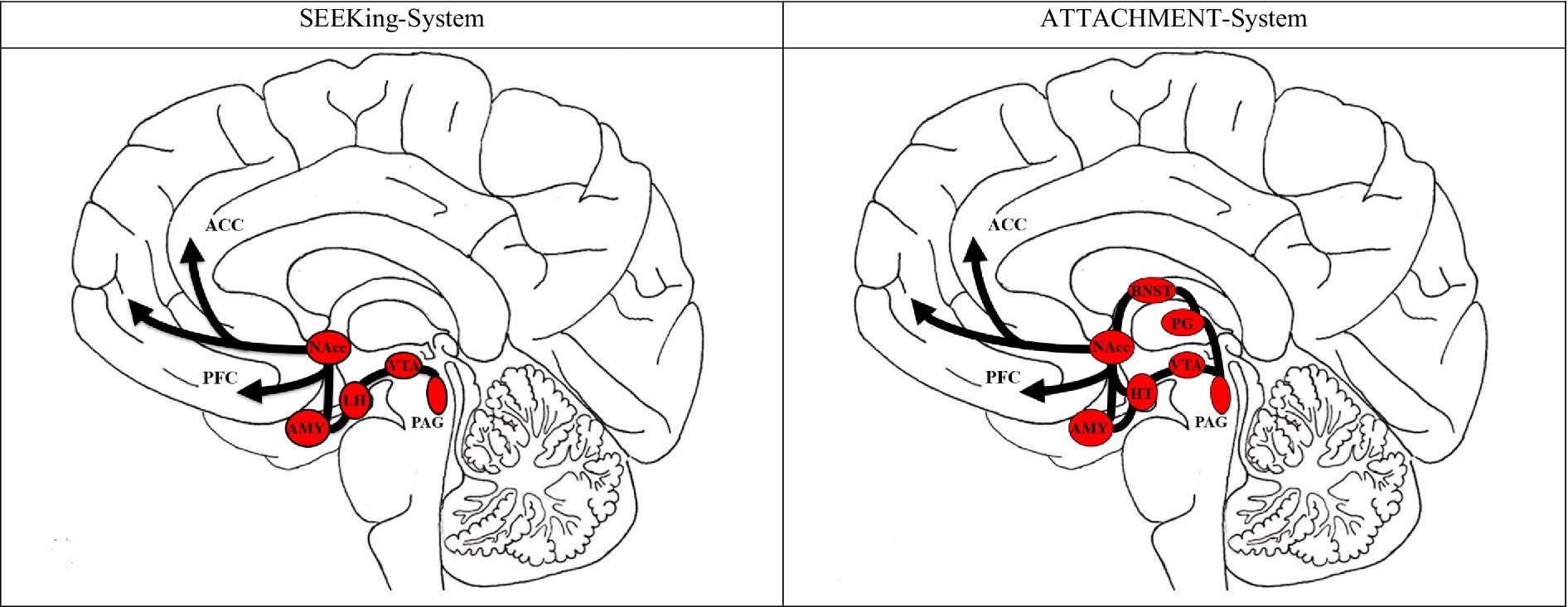
Figure 2. Neural correlates of SEEKing versus Attachment (social bonding) in the brain. ACC, anterior cingulate cortex; PFC, prefrontal cortex; NAcc, nucleus accumbens; AMY, amygydala; LH, left hypothalamus; VTA, ventral tegmental area; PAG, periaqueductal gray; BNST, bed nucleus of the stria terminalis; PG, pineal gland. Original Sketch drawn by Jürgen Fuchshuber; slightly modified; used with kind permission; based on Coan (2010), Panksepp (2008), and Panksepp and Biven (2012).
In our neuroimaging research, patients with poly-drug use disorder (PUD) showed structural brain abnormalities and impairments in attachment and personality organization compared to healthy controls (Unterrainer et al., 2016, 2019). Behavioral difficulties in emotion regulation were consistent across studies, though expected neural correlates were less pronounced. For instance, during an emotion reappraisal task in an fMRI scanner, PUD patients displayed emotional dysregulation, yet anticipated neural activation patterns were attenuated (Hiebler-Ragger et al., 2021). Resting-state fMRI analyses revealed altered connectivity between the default mode network (DMN) and salience network in PUD patients—particularly among those with insecure attachment patterns (Fuchshuber et al., 2025a). These findings suggest a neurobiological basis for impaired affective processing and social cognition in individuals with addiction and attachment disturbances.
We also investigated the role of oxytocin, a neuropeptide implicated in bonding. Using attachment-related stimuli from the Adult Attachment Projective (AAP) system (George and West, 2012), we measured oxytocin responses in PUD patients versus controls (Fuchshuber et al., 2020). While behavioral responses did not differ significantly between groups, oxytocin reactivity was significantly blunted in the addiction group. This suggests reduced physiological sensitivity to attachment cues and highlights a possible neurobiological mechanism underlying impaired relational functioning in addiction. It also raises the question of whether pharmacological substitution therapies might affect the attachment system in ways that hinder interpersonal engagement in treatment.
4 Clinical implications and future perspectives
The conceptualization of addiction as an attachment disorder is exemplified in a case study involving a 19-year-old college student treated with a combined approach of EEG neurofeedback and psychodynamically oriented psychotherapy (Unterrainer et al., 2014). The patient presented with depressive symptoms following a period of polysubstance use. Across 11 treatment sessions, including a follow-up, clinical progress was assessed using the Montgomery-Åsberg Depression Rating Scale (MADRS; Montgomery and Åsberg, 1979), the Brief Psychiatric Rating Scale (BPRS; Overall and Gorham, 1962), and the Beck Depression Inventory (BDI; Beck et al., 1996). These measures showed a clear shift from clinically significant depression to a stable, non-pathological state—confirmed at follow-up.
Neurophysiologically, improvements were mirrored by increased activity in the sensorimotor rhythm (SMR)/theta ratio, highlighting the potential utility of EEG neurofeedback. Equally significant was the strong therapeutic bond formed between the patient and the multidisciplinary treatment team. The team’s diversity—comprising an Austrian addiction therapist, a Taiwanese neurofeedback trainer, and an English neuropsychologist—may have contributed to the development of a meaningful male attachment figure for the patient (see Unterrainer et al., 2013 for further discussion). These results align with other studies from our group demonstrating the effectiveness of EEG neurofeedback in treating addiction (Lackner et al., 2016a; Unterrainer et al., 2013), as well as in the treatment of anorexia nervosa (Lackner et al., 2016b). More broadly, our findings reinforce a growing consensus that addiction is deeply interwoven with disruptions in attachment, emotion regulation, and personality structure (Unterrainer et al., 2018).
Future research should continue to build on this integrative framework by examining neuroplastic changes associated with long-term addiction therapy—particularly within attachment-based psychotherapeutic approaches. Given the established links between insecure attachment and vulnerability to substance use (Fairbairn et al., 2018; Schindler, 2019), and the potential of such therapies to modulate neural circuits involved in reward, stress, and social bonding (Lewis et al., 2020), longitudinal neuroimaging studies are needed. These investigations could illuminate how recovery processes manifest at the neurobiological level, informing the development of more targeted, personalized interventions that address both relational and neurophysiological dimensions of addiction recovery.
Author contributions
H-FU: Writing – original draft, Writing – review & editing.
Funding
The author declares that no financial support was received for the research and/or publication of this article.
Acknowledgments
I am deeply grateful to my former PhD students Dr. Jürgen Fuchshuber and Dr. Michaela Hiebler, without whom this work would not have been possible.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author declares that Gen AI was used in the creation of this manuscript. ChatGBT V4.0 and Deepl Translate was used in order to improve the English language.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ainsworth, M. D. S., Blehar, M. C., Waters, E., and Wall, S. N. (2015). Patterns of attachment: A psychological study of the strange situation. New York, NY: Psychology Press.
Barratt, B. B. (2015). Critical notes on the neuro-evolutionary archaeology of affective systems. Psychoanal. Rev. 102, 183–208. doi: 10.1521/prev.2015.102.2.183
Barrett, F. S., Robins, R. W., and Janata, P. (2013). A brief form of the affective neuroscience personality scales. Psychol. Assess. 25, 826–843. doi: 10.1037/a0032576
Beck, A. T., Steer, R. A., and Brown, G. K. (1996). Beck depression inventory manual. San Antonio, TX: The Psychological Corporation.
Bretherton, I. (2013). “The origins of attachment theory: John Bowlby and Mary Ainsworth” in Attachment theory (London, UK: Routledge), 45–84.
Coan, J. A. (2010). Adult attachment and the brain. J. Soc. Pers. Relat. 27, 210–217. doi: 10.1177/0265407509360900
Fairbairn, C. E., Briley, D. A., Kang, D., Fraley, R.C, Hankin, B.L., and Ariss, T. (2018). A meta-analysis of longitudinal associations between substance use and interpersonal attachment security. Psychological bulletin, 114:532. doi: 10.1037/bul0000141
Feldman, R. (2017). The neurobiology of human attachments. Trends Cogn. Sci. 21, 80–99. doi: 10.1016/j.tics.2016.11.007
Freud, S. (1898). “Sexuality in the Aetiology of the neuroses” in The standard edition of the complete psychological works of Sigmund Freud. ed. J. Strachey, vol. 3 (London: Hogarth Press), 259–285.
Fuchshuber, J., Hiebler-Ragger, M., Ragger, K., Rinner, A., Kapfhammer, H. P., and Unterrainer, H. F. (2018). Increased attachment security is related to early therapy drop-out in substance use disorders. BMC. Res. Notes 11, 141–145. doi: 10.1186/s13104-018-3251-7
Fuchshuber, J., Jauk, E., Hiebler-Ragger, M., and Unterrainer, H. F. (2022). The affective neuroscience of sexuality: development of a LUST scale. Front. Hum. Neurosci. 16:853706. doi: 10.3389/fnhum.2022.853706
Fuchshuber, J., Koschutnig, K., Fink, A., Alexopoulos, J., Löffler-Stastka, H., and Unterrainer, H. F. (2025a). Effects of insecure attachment on fMRI resting state functional connectivity in poly drug use disorder. PLoS One 20:e0318505. doi: 10.1371/journal.pone.0318505
Fuchshuber, J., Löffler-Stastka, H., and Unterrainer, H. F. (2025b). The relationship between attachment types and drug of choice: a cluster analysis. Subst. Use Misuse Submitted.
Fuchshuber, J., Prandstätter, T., Andres, D., Roithmeier, L., Schmautz, B., Freund, A., et al. (2023). The German version of the brief affective neuroscience personality scales including a LUST scale (BANPS–GL). Front. Hum. Neurosci. 17, 1–12. doi: 10.3389/fnhum.2023.1213156
Fuchshuber, J., and Unterrainer, H. F. (2020). Childhood trauma, personality, and substance use disorder: the development of a neuropsychoanalytic addiction model. Front. Psych. 11:531. doi: 10.3389/fpsyt.2020.00531
Fuchshuber, J., Tatzer, J., Hiebler-Ragger, M., Trinkl, F., Kimmerle, A., Rinner, A., et al. (2020). The influence of an attachment-related stimulus on oxytocin reactivity in poly-drug users undergoing maintenance therapy compared to healthy controls. Front. Psychol, 11:460506. doi: 10.3389/fpsyt.2020.460506
George, C., and West, M. L. (2012). The adult attachment projective picture system: Attachment theory and assessment in adults. New York, NY: Guilford Press.
Hiebler-Ragger, M., Fuchshuber, J., Dröscher, H., Vajda, C., Fink, A., and Unterrainer, H. F. (2018). Personality influences the relationship between primary emotions and religious/spiritual well-being. Front. Psychol. 9:370. doi: 10.3389/fpsyg.2018.00370
Hiebler-Ragger, M., Perchtold-Stefan, C. M., Unterrainer, H. F., Fuchshuber, J., Koschutnig, K., Nausner, L., et al. (2021). Lower cognitive reappraisal capacity is related to impairments in attachment and personality structure in poly-drug use: an fMRI study. Brain Imaging Behav. 15, 2187–2198. doi: 10.1007/s11682-020-00414-3
Hiebler-Ragger, M., Unterrainer, H. F., Rinner, A., and Kapfhammer, H. P. (2016). Insecure attachment styles and increased borderline personality organization in substance use disorders. Psychopathology 49, 341–344. doi: 10.1159/000448177
Kernberg, O. F. (2015). Neurobiological correlates of object relations theory: the relationship between neurobiological and psychodynamic development. Int. Forum Psychoanal. 24, 38–46. doi: 10.1080/0803706X.2014.912352
Khantzian, E. J. (2013). Addiction as a self-regulation disorder and the role of self-medication. Addiction 108, 668–669. doi: 10.1111/add.12004
Lackner, N., Unterrainer, H. F., Skliris, D., Shaheen, S., Dunitz-Scheer, M., Wood, G., et al. (2016b). EEG neurofeedback effects in the treatment of adolescent anorexia nervosa. Eat. Disord. 24, 354–374. doi: 10.1080/10640266.2016.1160705
Lackner, N., Unterrainer, H. F., Skliris, D., Wood, G., Wallner-Liebmann, S. J., Neuper, C., et al. (2016a). The effectiveness of visual short-time neurofeedback on brain activity and clinical characteristics in alcohol use disorders: practical issues and results. Clin. EEG Neurosci. 47, 188–195. doi: 10.1177/1550059415605686
Lewis, A. J., Unterrainer, H. F., Galbally, M., and Schindler, A. (2020). Addiction and attachment. Front. Psych. 11:612044. doi: 10.3389/fpsyt.2020.612044
Mac Lean, P. D. (1990). The triune brain in evolution: Role in paleocerebral functions. New York, NY: Springer Science and Business Media.
Mikulincer, M., and Shaver, P. R. (2012). An attachment perspective on psychopathology. World Psychiatry 11, 11–15. doi: 10.1016/j.wpsyc.2012.01.003
Möller, H. J., Laux, G., and Deister, A. (2015). Psychiatry, psychosomatics and psychotherapy. Stuttgart: Thieme.
Montgomery, S. A., and Åsberg, M. (1979). A new depression scale designed to be sensitive to change. Br. J. Psychiatry 134, 382–389. doi: 10.1192/bjp.134.4.382
Orford, J. (2001). Addiction as excessive appetite. Addiction 96, 15–31. doi: 10.1080/09652140020016932
Overall, J. E., and Gorham, D. R. (1962). The brief psychiatric rating scale. Psychological reports, 10, 799–812.
Panksepp, J. (2008). “The affective brain and core consciousness: how does neural activity generate emotional feelings?” in Handbook of emotions. eds. M. Lewis, J. M. Haviland-Jones, and L. F. Barrett. 3rd ed (New York, NY: The Guilford Press), 47–67.
Panksepp, J., and Biven, L. (2012). The archaeology of mind: Neuroevolutionary origins of human emotions. New York, NY: W.W. Norton and Company.
Parkes, C. M., Stevenson-Hinde, J., and Marris, P. (2006). Attachment across the life cycle. London, UK: Routledge.
Rübig, L. L., Fuchshuber, J., Köldorfer, P., Rinner, A., Fink, A., and Unterrainer, H. F. (2021). Attachment and therapeutic alliance in substance use disorders: initial findings for treatment in the therapeutic community. Front. Psych. 12:730876. doi: 10.3389/fpsyt.2021.730876
Schindler, A. (2019). Attachment and substance use disorders—theoretical models, empirical evidence, and implications for treatment. Front. Psych. 10:727. doi: 10.3389/fpsyt.2019.00727
Solms, M., and Panksepp, J. (2012). The “id” knows more than the “Ego” admits: Neuropsychoanalytic and primal consciousness perspectives on the interface between affective and cognitive neuroscience. Brain Sci. 2, 147–175. doi: 10.3390/brainsci2020147
Unterrainer, H. F., Chen, M. L., and Gruzelier, J. H. (2014). EEG-neurofeedback and psychodynamic psychotherapy in a case of adolescent anhedonia with substance misuse: mood/theta relations. Int. J. Psychophysiol. 93, 84–95. doi: 10.1016/j.ijpsycho.2013.03.011
Unterrainer, H. F., Hiebler, M., Ragger, K., Froehlich, L., Koschutnig, K., Schoeggl, H., et al. (2016). White matter integrity in polydrug users in relation to attachment and personality: a controlled diffusion tensor imaging study. Brain Imaging Behav. 10, 1096–1107. doi: 10.1007/s11682-015-9475-4
Unterrainer, H. F., Hiebler-Ragger, M., Koschutnig, K., Fuchshuber, J., Ragger, K., Perchtold, C. M., et al. (2019). Brain structure alterations in poly-drug use: reduced cortical thickness and white matter impairments in regions associated with affective, cognitive, and motor functions. Front. Psych. 10:667. doi: 10.3389/fpsyt.2019.00667
Unterrainer, H. F., Hiebler-Ragger, M., Rogen, L., and Kapfhammer, H. P. (2018). Addiction as an attachment disorder. Nervenarzt 89, 1043–1048. doi: 10.1007/s00115-017-0462-4
Unterrainer, H. F., Lewis, A. J., and Gruzelier, J. H. (2013). EEG-neurofeedback in psychodynamic treatment of substance dependence. Front. Psychol. 4:692. doi: 10.3389/fpsyg.2013.00692
Volkow, N. D., Koob, G. F., and McLellan, A. T. (2016). Neurobiologic advances from the brain disease model of addiction. N. Engl. J. Med. 374, 363–371. doi: 10.1056/NEJMra1511480
Zellner, M. R., Watt, D. F., Solms, M., and Panksepp, J. (2011). Affective neuroscientific and neuropsychoanalytic approaches to two intractable psychiatric problems: why depression feels so bad and what addicts really want. Neurosci. Biobehav. Rev. 35, 2000–2008. doi: 10.1016/j.neubiorev.2011.01.003
Keywords: addiction, attachment, developmental neuroscience, interoception, insular cortex, EEG neurofeedback, psychodynamic therapy, early trauma
Citation: Unterrainer H-F (2025) Addiction, attachment, and the brain: a focused review of empirical findings and future directions. Front. Hum. Neurosci. 19:1625880. doi: 10.3389/fnhum.2025.1625880
Edited by:
Chella Kamarajan, Downstate Health Sciences University, United StatesReviewed by:
Daniela Flores Mosri, Universidad Intercontinental, MexicoCopyright © 2025 Unterrainer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Human-Friedrich Unterrainer, aHVtYW4udW50ZXJyYWluZXJAc2Z1LmFjLmF0
 Human-Friedrich Unterrainer
Human-Friedrich Unterrainer