- 1Department of Critical Care Medicine, Dazhou Central Hospital, Dazhou, Sichuan, China
- 2Department of Interventional Radiology, Dazhou Central Hospital, Dazhou, Sichuan, China
Background: Subarachnoid hemorrhage (SAH) is a devastating cerebrovascular event that leads to high mortality and long-term disability, particularly among adults aged 25–49 years. Elevated systolic blood pressure (SBP) is the leading modifiable risk factor, yet its global burden in this age group has not been systematically assessed.
Methods: We analyzed population-level epidemiological data across 204 countries and territories from 1990 to 2021 to estimate SAH mortality and disability-adjusted life-years (DALYs) attributable to high SBP. Temporal trends were evaluated using estimated annual percentage change (EAPC), and future trajectories to 2050 were projected with autoregressive integrated moving average (ARIMA) models.
Results: Globally, SAH caused 24,908 deaths and 1,373,366 DALYs in 2021 due to high SBP in adults aged 25–49 years. Males had higher rates than females (mortality: 0.78 vs. 0.48 per 100,000; DALYs: 42.4 vs. 27.0 per 100,000), though females experienced steeper declines (EAPC_mortality: −1.78%). The highest burden was in the 45–49 age group (deaths: 9,768; DALYs: 474,092). From 1990 to 2021, high-SDI regions achieved the greatest reductions in mortality (−50.3%) and DALYs (−46.8%), while low-SDI regions saw increases in deaths (+109.5%) and DALYs (+114.7%). Nationally, Zimbabwe and Guatemala showed the sharpest increases in mortality (EAPC: +4.71% and +3.76%), while Sweden and Swiss Confederation achieved the greatest declines (EAPC: −5.5% and −4.9%). Forecasts suggest continued global declines by 2050, but widening disparities by sex, age, and socio-demographic status.
Conclusion: Although the global burden of SAH attributable to high SBP is decreasing, young and middle-aged adults-especially males and those in low-SDI regions-continue to face substantial risks. Targeted hypertension control and region-specific prevention strategies are urgently needed.
Introduction
Subarachnoid hemorrhage (SAH) is a serious and often fatal type of stroke caused by bleeding into the subarachnoid space (Rautalin et al., 2024). Although it represents a relatively small proportion of all stroke cases globally, SAH leads to considerable mortality and disability, particularly among individuals of working age (Haripottawekul et al., 2025; Wyckoff and Hsiang-Yi Chou, 2025). The high case fatality rate and long-term neurological sequelae in survivors make SAH a major contributor to premature death and loss of productive life-years, imposing a significant burden on families, health systems, and societies, especially in low- and middle-income countries (Poliseli et al., 2024).
Among the risk factors for SAH, elevated systolic blood pressure (SBP) is the most important modifiable cause (Eagles et al., 2025). Persistent high SBP increases the risk of aneurysm formation and rupture by promoting structural changes in cerebral vessels (Lin et al., 2023). Despite improvements in hypertension awareness and management in many parts of the world, the prevalence of uncontrolled high SBP remains substantial (GBD 2021 Global Subarachnoid Hemorrhage Risk Factors Collaborators, Rautalin et al., 2025). This is particularly concerning among young and middle-aged adults, who are less likely to be screened or treated for hypertension compared to older adults (Betteridge et al., 2024). The long-term vascular damage associated with early-onset high SBP not only increases the lifetime risk of SAH, but also contributes to other forms of premature cardiovascular disease (Frontera et al., 2010).
In this study, we aimed to describe the global and regional burden of SAH attributable to high SBP among young and middle-aged adults from 1990 to 2021, using data from the Global Burden of Disease (GBD) Study (GBD 2021 Causes of Death Collaborators, 2024). We also sought to examine temporal trends in mortality, incidence, and disability-adjusted life-years (DALYs) related to high SBP in this population. Our findings are intended to provide evidence to support targeted public health interventions to reduce preventable SAH deaths and disability in working-age adults.
Materials and methods
Data sources and study population
This study used data from the GBD Study 2021, coordinated by the Institute for Health Metrics and Evaluation (IHME) (GBD 2021 Causes of Death Collaborators, 2024; GBD 2021 Diseases and Injuries Collaborators, 2024). GBD provides standardized estimates of disease burden attributable to various causes and risk factors across 204 countries and territories, 21 geographical regions, and five Socio-demographic Index (SDI) levels, covering the years 1990–2021 (Zhang et al., 2023). Data were downloaded from the Global Health Data Exchange1 on 25 May 2025. Estimates were based on data from vital registration systems, verbal autopsy, hospital records, claims data, surveys, and published literature, modeled using the DisMod-MR 2.1 Bayesian meta-regression framework (Fan et al., 2022). This analysis focused on adults aged 25–49 years, stratified into 5-year age groups (25–29, 30–34, 35–39, 40–44, 45–49 years) and by sex. Data were analyzed at global, SDI quintile, regional (21 regions), and national (204 countries and territories) levels.
Definition of subarachnoid hemorrhage and high systolic blood pressure
Subarachnoid hemorrhage was defined as bleeding into the subarachnoid space, typically resulting from rupture of an intracranial aneurysm or vascular malformation (Lee et al., 2025). SAH was classified using the following International Classification of Diseases (ICD) codes: ICD-10 I60-I60.9 (non-traumatic SAH), I67.0-I67.1 (cerebral artery dissection and arteriovenous malformations); ICD-9 430-430.9 (non-traumatic SAH), 431.0 (intracranial hemorrhage involving subarachnoid space), and 437.3 (arteriovenous malformations) (Lv et al., 2024). High SBP was defined as SBP ≥ 115 mmHg, with a theoretical minimum risk exposure level (TMREL) of 110–115 mmHg in line with GBD comparative risk assessment standards. The burden attributable to high SBP was calculated as the proportion of SAH burden linked to SBP levels above the TMREL (GBD 2021 Global Subarachnoid Hemorrhage Risk Factors Collaborators, Rautalin et al., 2025).
Statistical analysis
Temporal trends from 1990 to 2021 were assessed using estimated annual percentage change (EAPC). Log-linear regression models were fitted to the natural logarithm of crude incidence, mortality, and DALY rates: ln(rate) = α + β × year + γ; EAPC was calculated as: EAPC = 100 × (eβ−1) (Lv et al., 2024).
A trend was deemed significant if both the EAPC estimate and its 95% confidence interval (CI) were either above or below zero. In addition, autoregressive integrated moving average (ARIMA) models were used to forecast incidence, mortality, and DALYs up to 2050. Model parameters (p, d, q) were selected based on autocorrelation and partial autocorrelation plots and AIC minimization, with model adequacy confirmed by residual diagnostics (Zhang Y. F. et al., 2025).
Results
Global burden and temporal trends of SAH attributable to high SBP
In 2021, there were an estimated 24,908 [95% uncertainty interval (UI) 16,515 to 34,310] deaths globally from SAH attributable to high SBP among adults aged 25–49 years, corresponding to a crude mortality rate of 0.63 (95% UI 0.42 to 0.87) per 100,000 population. This represented a slight increase of 1.72% (95% UI −13.32 to 19.63) in the absolute number of deaths compared with 1990 (Figure 1A and Table 1). The global mortality rate declined more markedly over this period, with an EAPC of −1.44% (95% CI −1.56 to −1.31). Male adults consistently experienced a higher mortality burden compared with females. In 2021, the crude mortality rate among males was 0.78 (95% UI 0.50 to 1.15) per 100,000 population, compared to 0.48 (95% UI 0.32 to 0.66) in females (Figure 1B and Table 1). Although the number of SAH deaths attributable to high SBP in males increased modestly by 6.54% (95% UI −12.15 to 34.36) from 1990 to 2021, the mortality rate declined significantly, with an EAPC of −1.22% (95% CI −1.34 to −1.11). In females, both the number of deaths and the mortality rate decreased, with an EAPC of −1.78% (95% CI −1.93 to −1.62) (Table 1).
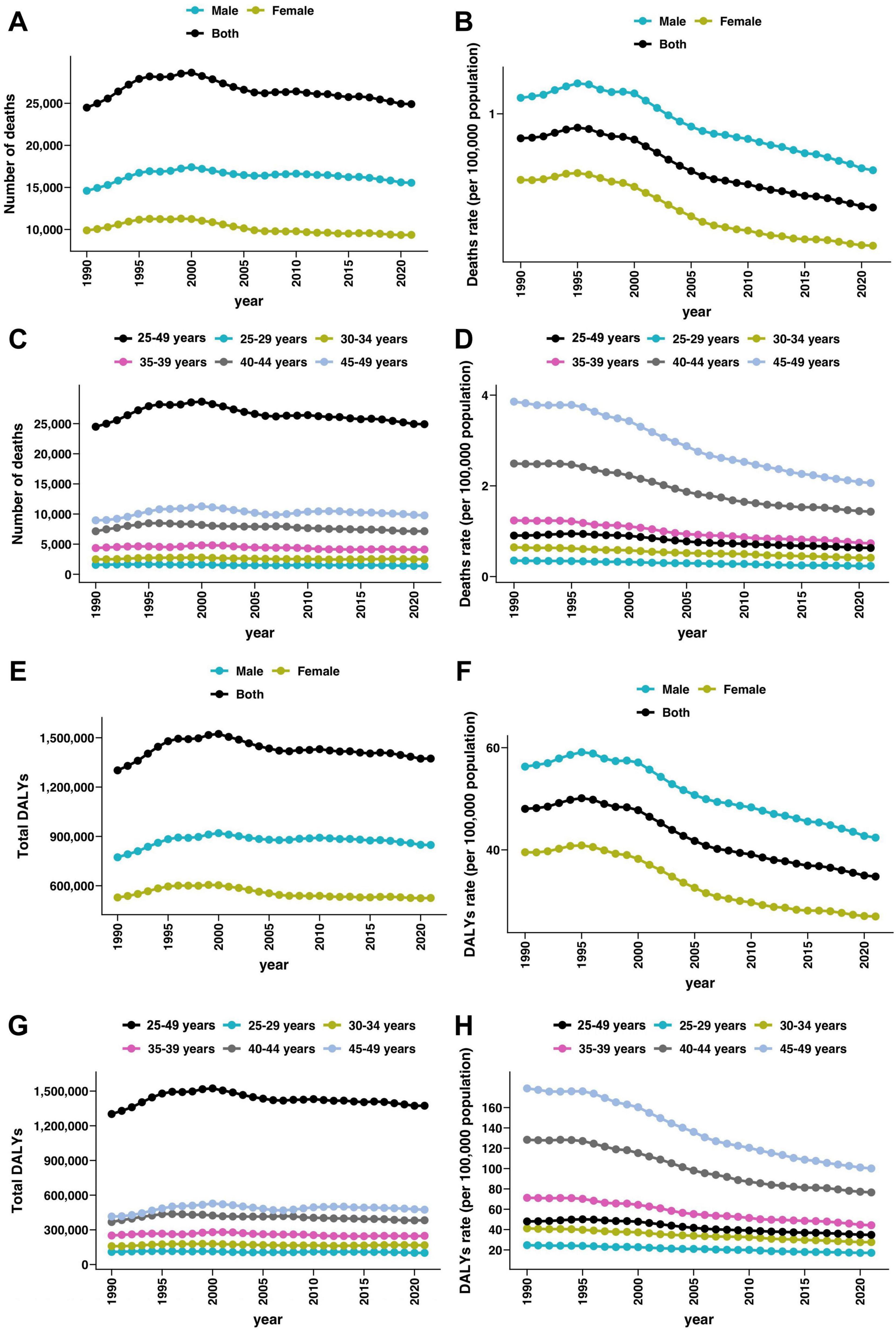
Figure 1. Global trends in subarachnoid hemorrhage deaths and disability-adjusted life years (DALYs) attributable to high systolic blood pressure among young and middle-aged adults from 1990 to 2021. (A,B) Number of deaths and sex-specific death rates (per 100,000 population) due to subarachnoid hemorrhage attributable to high systolic blood pressure over time. (C,D) Number of deaths and age-specific death rates (per 100,000 population) due to subarachnoid hemorrhage attributable to high systolic blood pressure by age group (25–49 years overall and 5-year subgroups) over time. (E,F) Number of DALYs and sex-specific DALYs rate (per 100,000 population) due to subarachnoid hemorrhage attributable to high systolic blood pressure over time. (G,H) Number of DALYs and sex-specific DALYs rate (per 100,000 population) due to subarachnoid hemorrhage attributable to high systolic blood pressure by age group (25–49 years overall and 5-year subgroups) over time.
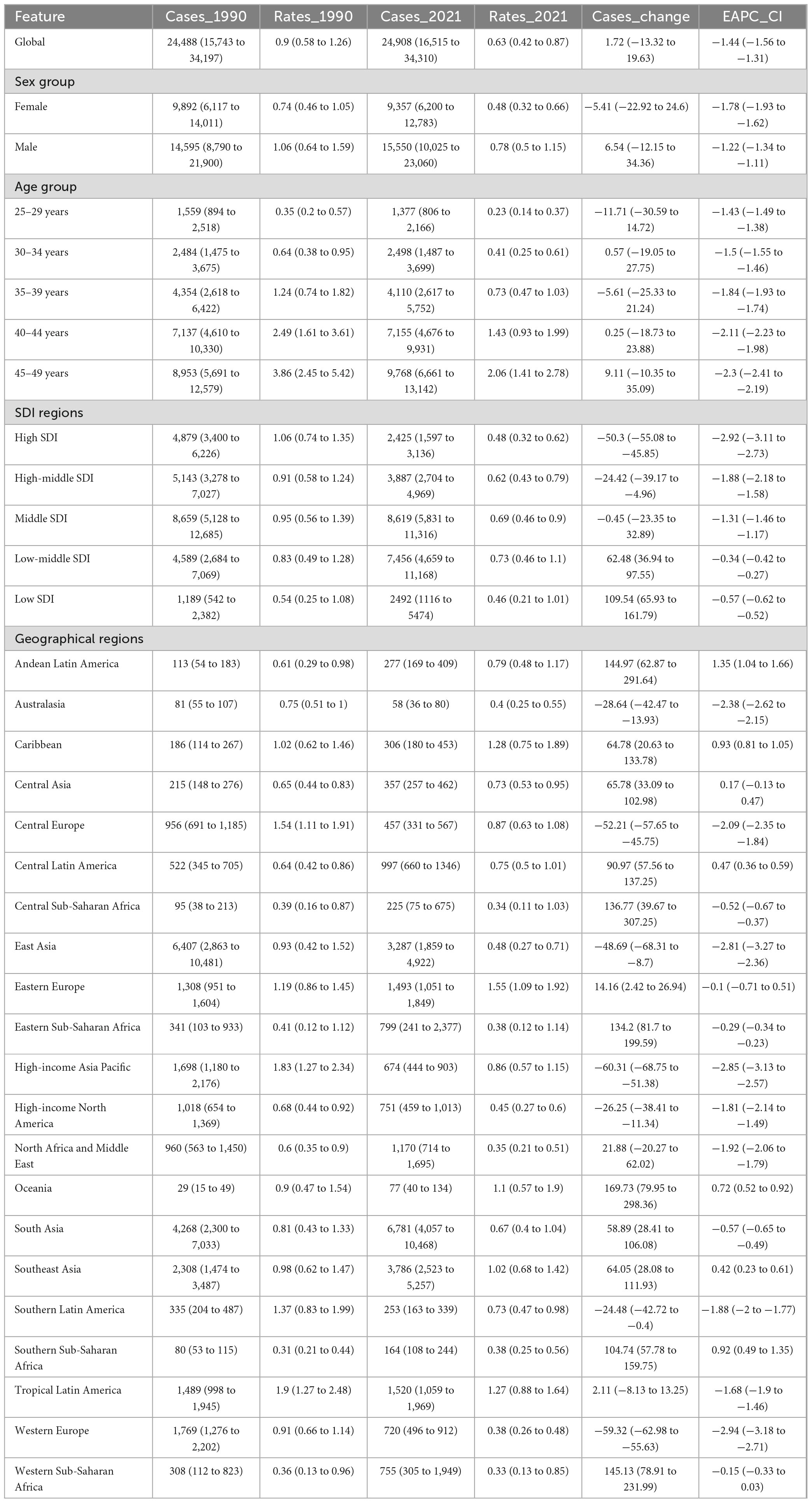
Table 1. Global and regional deaths and trends of subarachnoid hemorrhage attributable to high systolic blood pressure among 25–49 aged from 1990 to 2021.
The global burden of disability, measured by DALYs, followed a similar trend. In 2021, SAH attributable to high SBP accounted for 1,373,366 (95% UI 910,290 to 1,871,996) DALYs globally among adults aged 25–49 years, representing a crude rate of 34.78 (95% UI 23.05 to 47.41) per 100,000 population (Figures 1E, F and Supplementary Table 1). This reflects a slight decrease of 5.5% (95% UI −17.94 to 27.97) in DALYs compared with 1990, when the DALYs were estimated at 1,301,770 (95% UI 844,050 to 1,811,022). The DALY rate declined significantly over the study period, with an EAPC of −1.31% (95% CI −1.42 to −1.19). Again, the burden was higher in males than females. In 2021, the DALY rate in males was 42.4 (95% UI 28.36 to 61.22) per 100,000, compared to 26.97 (95% UI 18.16 to 36.75) in females (Figures 1E, F and Supplementary Table 1). The number of DALYs among males increased by 9.67% (95% UI −7.94 to 35.54) from 1990 to 2021, yet the DALY rate declined with an EAPC of −1.12% (95% CI −1.23 to −1.02). In contrast, females showed a reduction in both DALY number and rate, with an EAPC of −1.59% (95% CI −1.73 to −1.45) (Supplementary Table 1). The temporal trends illustrated a steady decline in both mortality and DALY rates across sexes from 1990 to 2021. The declines were more pronounced among females, while males continued to experience a relatively higher burden throughout the period.
Age-specific patterns and trends
From 1990 to 2021, the global burden of SAH due to high SBP declined across all adult age groups (25–49 years). The 45–49 age group had the highest burden in 2021, with 4,163 deaths (crude mortality rate: 1.77 per 100,000), reflecting a 3.1% increase in deaths but a significant decline in mortality rate (EAPC −2.65%) (Figures 1C, D and Table 1). This group also had the greatest DALY burden (206,858 DALYs, rate: 87.78 per 100,000), with an 8.93% increase in DALYs but a notable rate reduction (EAPC −2.45%) (Figures 1G, H and Supplementary Table 1). The 40–44 age group had 2,698 deaths and 148,972 DALYs in 2021, with mortality and DALY rates declining at EAPCs of −2.48% and −2.28%, respectively (Table 1 and Supplementary Table 1). Among younger adults, the burden was lower but also steadily declined. The 25–29 age group saw a 22.98% decrease in deaths, with mortality and DALY rates dropping significantly (EAPC −1.95% and −1.66%) (Figures 1C, D, G, H). Similarly, the 30–34 and 35–39 age groups experienced declines in mortality and DALY rates at EAPCs of −2.12% to −2.26% (Table 1 and Supplementary Table 1). Although absolute numbers of deaths and DALYs remained highest in older age groups, all age bands saw significant reductions in crude rates, with steeper declines in older adults.
Regional and SDI-level variations
From 1990 to 2021, the mortality and DALY burden of SAH attributable to high SBP showed substantial variation across SDI and geographical regions. High SDI regions achieved the greatest reductions, with deaths decreasing by 50.3% (95% UI −55.08 to −45.85) and DALYs by 46.83% (95% UI −51.74 to −42.42). Mortality and DALY rates in these regions declined from 1.06 to 0.48 and from 55.8 to 27.22 per 100,000, respectively, with EAPCs of −2.92% and −2.69% (Figures 2A–D and Tables 1, 2). High-middle SDI regions also showed marked reductions in deaths (−24.42%, 95% UI −39.17 to −4.96) and DALYs (−20.32, 95% UI −35.04 to −1.13), with EAPCs of −1.88% and −1.67%. Middle SDI regions maintained relatively stable mortality rates (−0.45%, 95% UI −23.35 to 32.89) and DALYs (3.5%, 95% UI −19.32 to 36.39). In contrast, low-middle and low SDI regions experienced substantial increases in both deaths (62.48% and 109.54%) and DALYs (64.92% and 114.77%), though mortality and DALY rates declined slightly (EAPCs −0.34% to −0.57% for mortality, −0.31% to −0.48% for DALYs) (Figures 2A–D and Tables 1, 2).
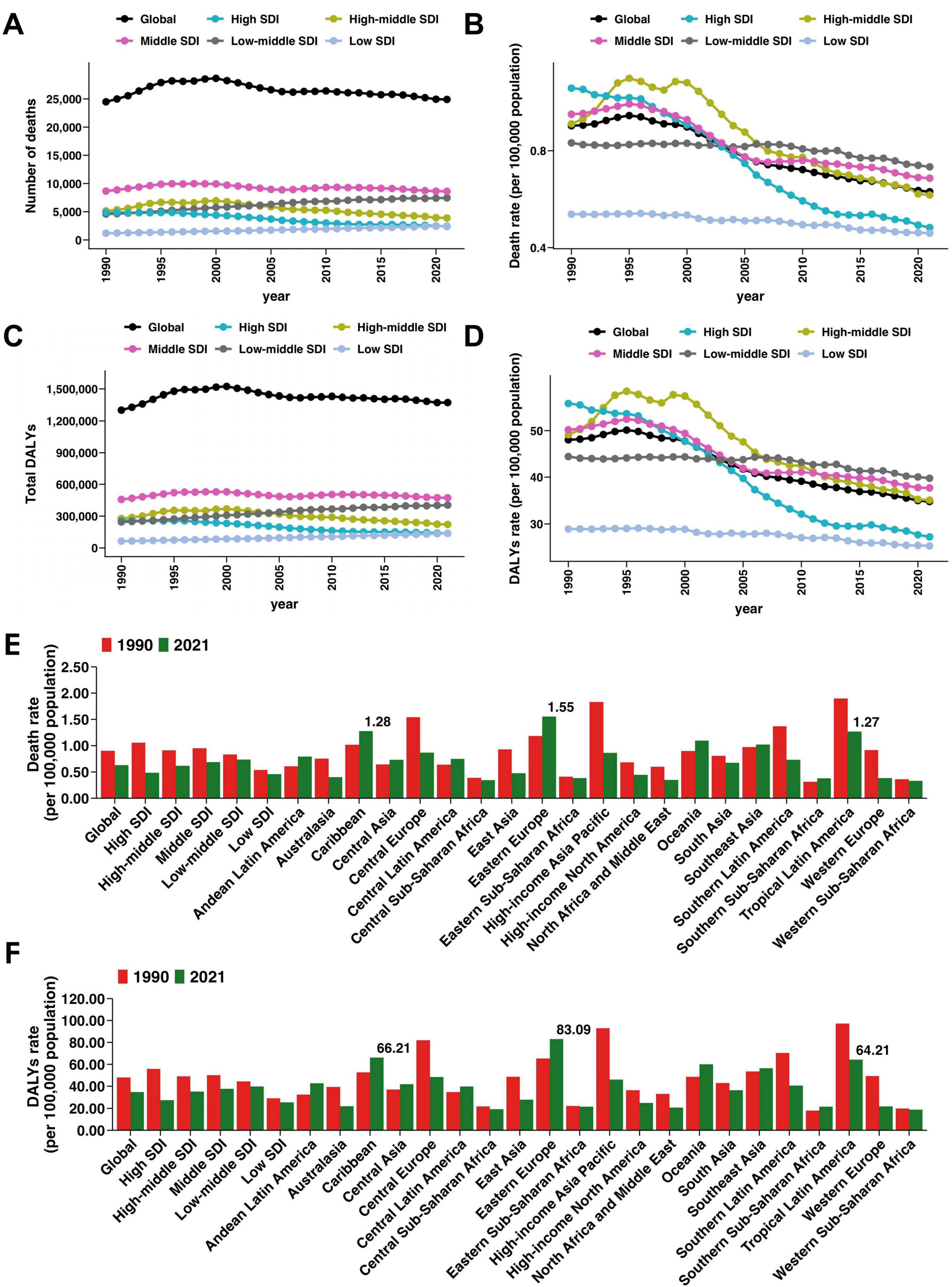
Figure 2. Regional patterns of subarachnoid hemorrhage mortality and disability-adjusted life years (DALYs) attributable to high systolic blood pressure among young and middle-aged adults. (A) Number of deaths by Socio-demographic Index (SDI) region and globally. (B) Death rates (per 100,000 population) over time by SDI region and globally. (C) Total DALYs by SDI region and globally. (D) DALY rates (per 100,000 population) over time by SDI region and globally. (E) Death rates in 1990 and 2021 at the global, SDI, and regional levels. (F) DALY rates in 1990 and 2021 at the global, SDI, and regional levels.
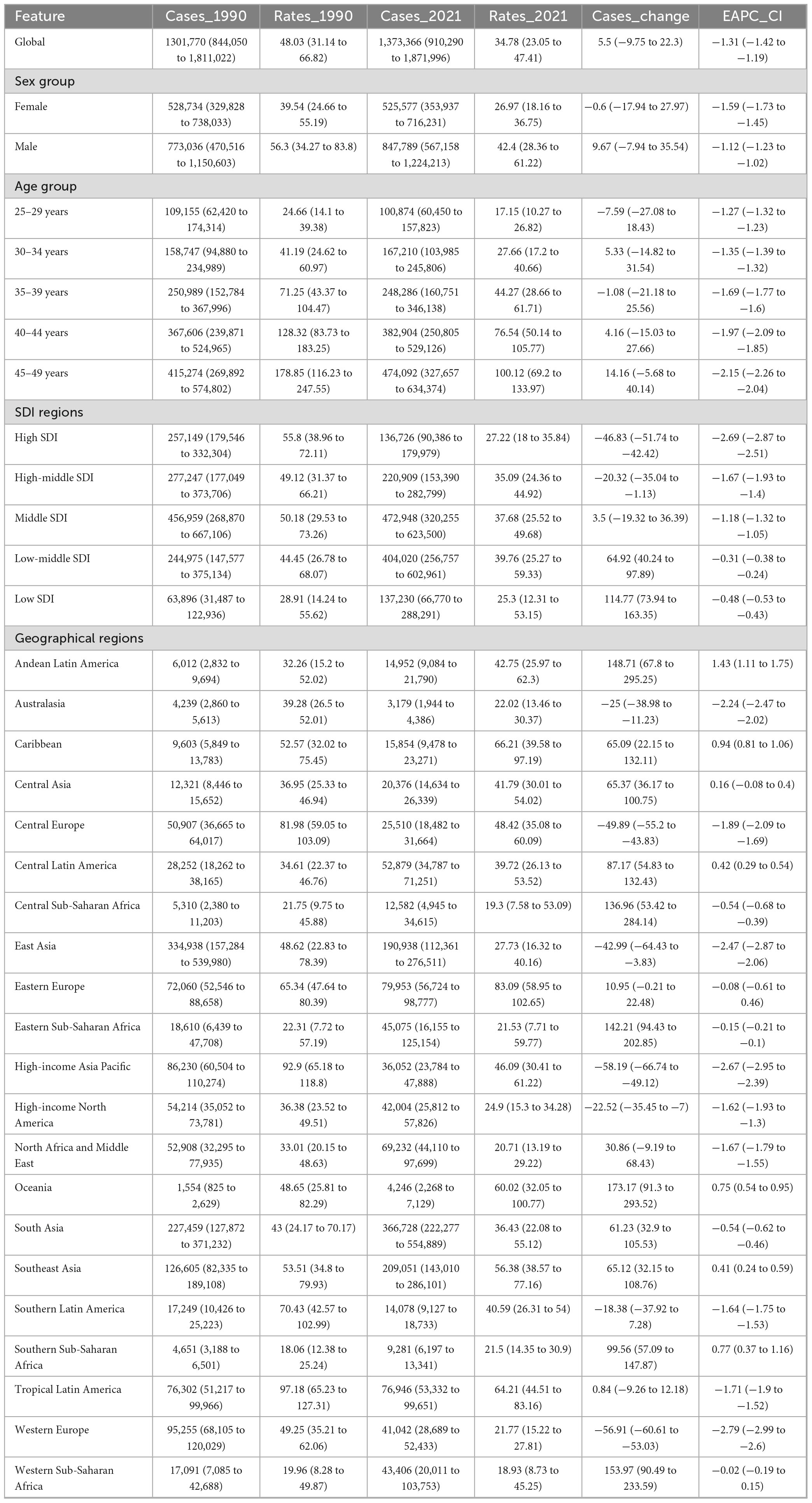
Table 2. Global and regional disability-adjusted life-years (DALYs) and trends of subarachnoid hemorrhage attributable to high systolic blood pressure among 25–49 aged from 1990 to 2021.
Geographically, high-income Asia Pacific, Western Europe, and Central Europe showed the largest reductions. High-income Asia Pacific deaths fell by 60.31% (95% UI −68.75 to −51.38) and DALYs by −58.19% (95% UI −66.74 to −49.12), with mortality and DALY EAPCs of −2.85% and −2.67% (Table 1 and Supplementary Table 1). Western Europe recorded similar trends, with deaths declining by 59.32% and DALYs by 56.91%, and EAPCs of −2.94% and −2.79%. Central Europe saw deaths decrease by 52.21% and DALYs by 49.89%, with mortality and DALY rates falling significantly (EAPC −2.09% and −1.89%) (Table 1 and Supplementary Table 1).
In contrast, regions such as Andean Latin America, the Caribbean, Oceania, and parts of Western Sub-Saharan Africa experienced large increases in both deaths and DALYs. For example, deaths rose by 169.73% in Oceania, 144.97% in the Andean Latin America, and 145.13% in Western Sub-Saharan Africa, accompanied by DALY increases of 173.17%, 148.71%, and 153.97%, respectively (Table 1 and Supplementary Table 1). Several of these regions also showed positive EAPCs in mortality or DALY rates, including Andean Latin America (mortality EAPC 1.35%), the Caribbean (mortality EAPC 0.93%), Oceania (DALY EAPC 0.75%), and Southern Sub-Saharan Africa (0.77%). Central Latin America and Southeast Asia reported increases in deaths and DALYs but relatively stable rates (Figures 2E, F). These patterns highlight persistent and widening disparities in SAH burden attributable to high SBP across global regions.
National burden across 204 countries and territories
From 1990 to 2021, the mortality burden of SAH attributable to high SBP varied across 204 countries. The greatest increases in deaths were observed in Guatemala (529.40%, 95% UI 313.18 to 996.78), Uzbekistan (271.54%, 95% UI 161.55 to 446.59), and Ecuador (227.57%, 95% UI 100.11 to 549.26). In contrast, Slovenia (−74.44%, 95% UI −82.07 to −64.33), Sweden (−80.84%, 95% UI −86.23 to −74.02), and Croatia (−72.03%, 95% UI −79.35 to −61.82) reported the largest declines (Figure 3A and Supplementary Table 2). The highest mortality rates in 2021 were in Nauru (3.53 per 100,000, 95% UI 2.1 to 5.33), Haiti (2.62 per 100,000, 95% UI 1.15 to 4.39), and Vanuatu (2.56 per 100,000, 95% UI 1.35 to 4.42), while the lowest were in Jordan (0.06 per 100,000, 95% UI 0.04 to 0.1), Palestine (0.07 per 100,000, 95% UI 0.04 to 0.1), and Kuwait (0.08 per 100,000, 95% UI 0.05 to 0.01) (Figure 3B and Supplementary Table 2). Lesotho (EAPC 2.95%, 95% CI 2.46 to 3.45) and Guatemala (EAPC 3.76%, 95% CI 3.24 to 4.2) saw the steepest increases, while Sweden (−5.5%, 95% CI −5.75 to −5.25) and Singapore (−4.61%, 95% CI −4.98 to −4.22) achieved the largest reductions (Figure 3C and Supplementary Table 2).
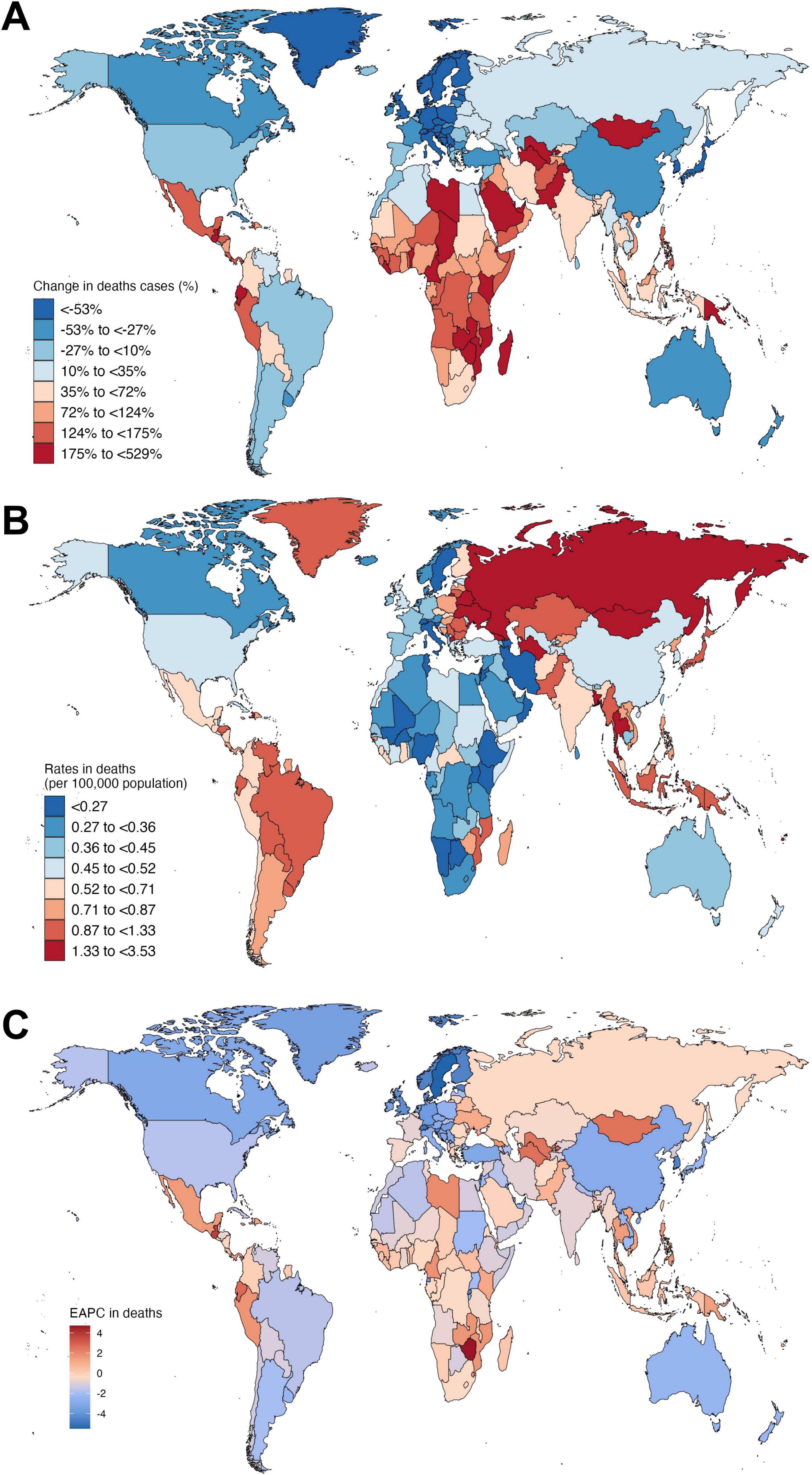
Figure 3. Global distribution of subarachnoid hemorrhage mortality attributable to high systolic blood pressure among young and middle-aged adults in 204 countries. (A) Change in the number of deaths from 1990 to 2021 by country. (B) Death rates (per 100,000 population) by country in 2021. (C) Estimated annual percentage change (EAPC) in death rates from 1990 to 2021 by country.
From 1990 to 2021, SAH DALYs attributable to high SBP also showed large disparities. Guatemala (530.91%, 95% UI 321.09 to 993.11), Uzbekistan (267.52%, 95% UI 168.27 to 433.94), and Ecuador (223.60%, 95% UI 97.49 to 524.61) saw the largest increases, while Sweden (−76.58%, 95% UI −83.00 to −69.30), Estonia (−69.62%, 95% UI −77.14 to −59.91), and Croatia (−68.44%, 95% UI −76.32 to −57.76) reported the greatest declines (Supplementary Figure 1A and Supplementary Table 3). The highest DALY rates in 2021 were in Nauru (194.19 per 100,000, 95% UI 119.09 to 287.52), Vanuatu (142.39 per 100,000, 95% UI 80.55 to 238.57), and Haiti (134.64 per 100,000, 95% UI 60.6 to 223.66), while the lowest were in Jordan (6.33 per 100,000, 95% UI 3.86 to 9.37), Palestine (5.97 per 100,000, 95% UI 3.45 to 8.96), and Kuwait (8.2 per 100,000, 95% UI 5.19 to 11.79). Zimbabwe (EAPC 4.36%, 95% CI 3.53 to 5.19) and Guatemala (EAPC 3.84%, 95% CI 3.32 to 4.36) had the fastest increases, while Sweden (−4.98%, 95% CI −5.17 to −4.78) and Switzerland (−4.51%, 95% CI −4.79 to −4.23) saw the largest declines (Supplementary Figures 1B, C and Supplementary Table 3). These findings highlight growing inequalities in SAH mortality and DALY burden due to high SBP, with many low- and middle-income countries facing alarming increases, while high-income regions have made significant progress.
Correlations between SAH burden and SDI
Globally, trends in SAH deaths attributable to high SBP varied across regions and SDI levels. As shown in Figure 4, there was a significant negative correlation between the EAPC of SAH death rates and SDI in 2021 (ρ = −0.326, P = 0.019), indicating that countries with higher SDI experienced more pronounced declines in mortality (Figure 4A). Similarly, a significant inverse correlation was observed between EAPC and the baseline SAH death rate in 1990 (ρ = −0.249, P < 0.001; Figure 4B), suggesting that countries with higher initial mortality achieved greater reductions over time. The relationship between SAH death rates and SDI followed a non-linear pattern: mortality rates increased with SDI up to approximately 0.65 and then declined as SDI rose further (ρ = 0.289, P < 0.001; Figure 4C), highlighting the disproportionate SAH mortality burden in middle-SDI countries, while many high-SDI regions have achieved substantial reductions. Temporal trends in SAH DALYs due to high SBP from 1990 to 2021 were also significantly associated with SDI levels and baseline burden. The EAPC in DALY rates was negatively correlated with SDI in 2021 (ρ = −0.343, P = 0.014), indicating that higher-SDI countries experienced greater reductions in DALYs (Supplementary Figure 2A). Similarly, a significant inverse association was observed between EAPC and DALY rates in 1990 (ρ = −0.274, P < 0.001; Supplementary Figure 2B), suggesting that regions with higher initial DALY burden achieved more pronounced declines. The relationship between SDI and DALY rates followed a similar non-linear pattern: DALY rates increased with SDI up to approximately 0.65, then declined as SDI continued to improve (ρ = 0.289, P < 0.001; Supplementary Figure 2C), emphasizing the disproportionate DALY burden in middle-SDI regions and the protective effect of higher SDI on SAH outcomes related to high SBP.
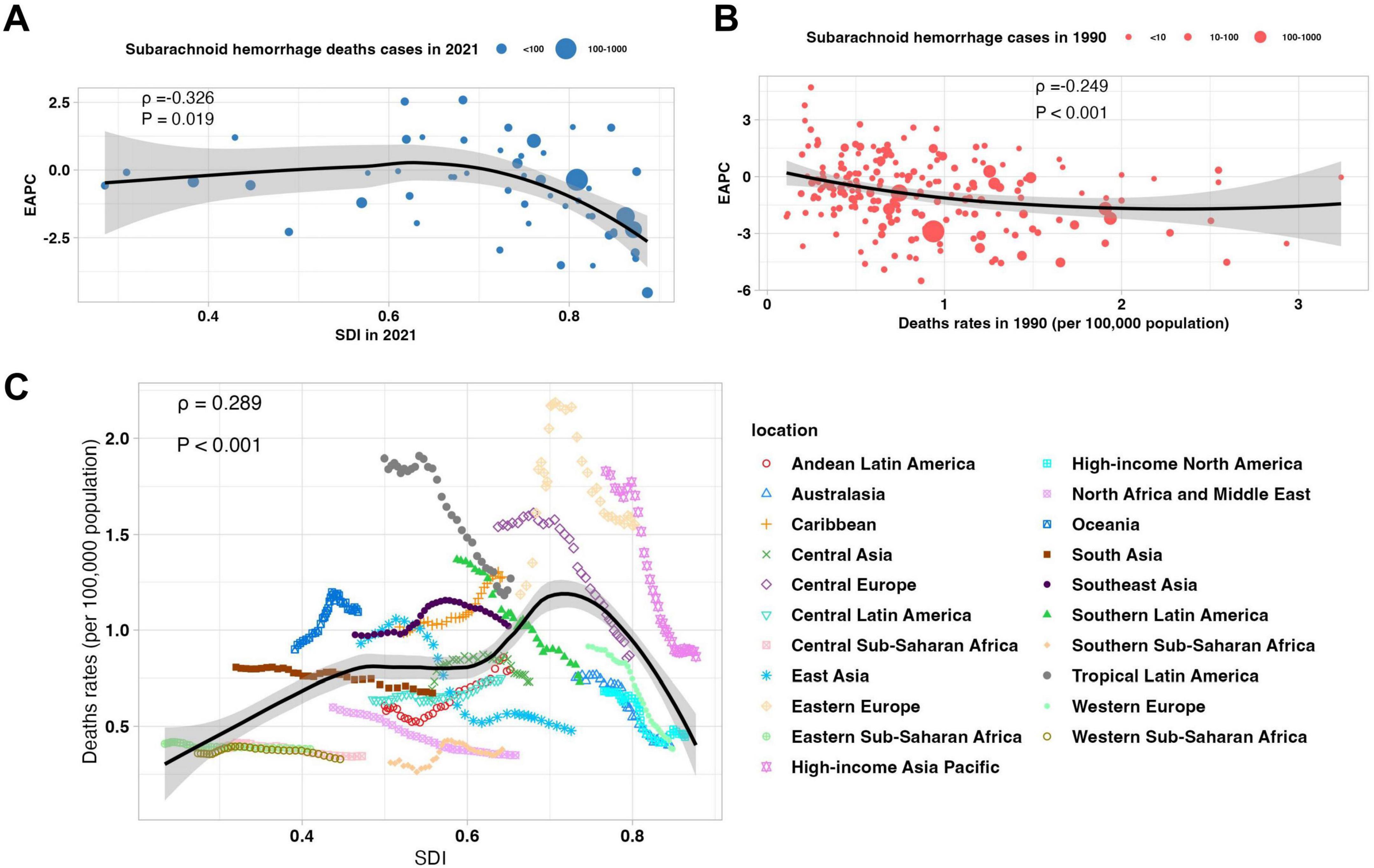
Figure 4. Correlations between subarachnoid hemorrhage mortality attributable to high systolic blood pressure, temporal trends, and socio-demographic development among young and middle-aged adults. (A) Association between the Socio-demographic Index (SDI) in 2021 and the estimated annual percentage change (EAPC) in death rates from 1990 to 2021. (B) Association between death rates in 1990 and EAPC in death rates from 1990 to 2021. (C) Relationship between SDI and death rates from 1990 to 2021 across global regions.
Forecasted trends to 2050
The forecasted trends in SAH deaths attributable to high SBP among individuals aged 25–49 years show continued global declines but substantial variation by sex, age, and region. By sex, SAH death rates in males are projected to plateau at approximately 0.77 (95% UI: 0.38–1.15) per 100,000 by 2050, while females are expected to achieve greater reductions from 0.46 (0.41–0.51) in 2025 to 0.27 (0.06–0.48) in 2050 (Figure 5A and Supplementary Table 4). Age-specific forecasts indicate more pronounced declines in older age groups: for example, deaths in the 45–49 age group are projected to fall from 1.90 (1.69–2.11) in 2025 to 0.54 (−0.21 to 1.29) by 2050. Globally, SAH death rates are expected to remain relatively stable at approximately 0.63 per 100,000 between 2025 and 2050, but with widening uncertainty intervals (2025: 0.56–0.69; 2050: 0.26–0.99) (Figure 5B and Supplementary Table 4). High-SDI regions are forecasted to achieve the greatest reductions, with death rates declining from 0.43 (0.36–0.50) to near-zero levels by 2050 (0.00, −0.30 to 0.31). Middle-SDI regions are projected to maintain rates around 0.67 (0.22–1.12), while low-SDI regions may experience a modest decline from 0.45 (0.43–0.47) to 0.39 (0.32–0.45) (Figure 5C and Supplementary Table 4). These projections highlight sustained progress in reducing SAH mortality linked to high SBP, particularly in high-SDI areas, though disparities across sexes, age groups, and regions are likely to persist.
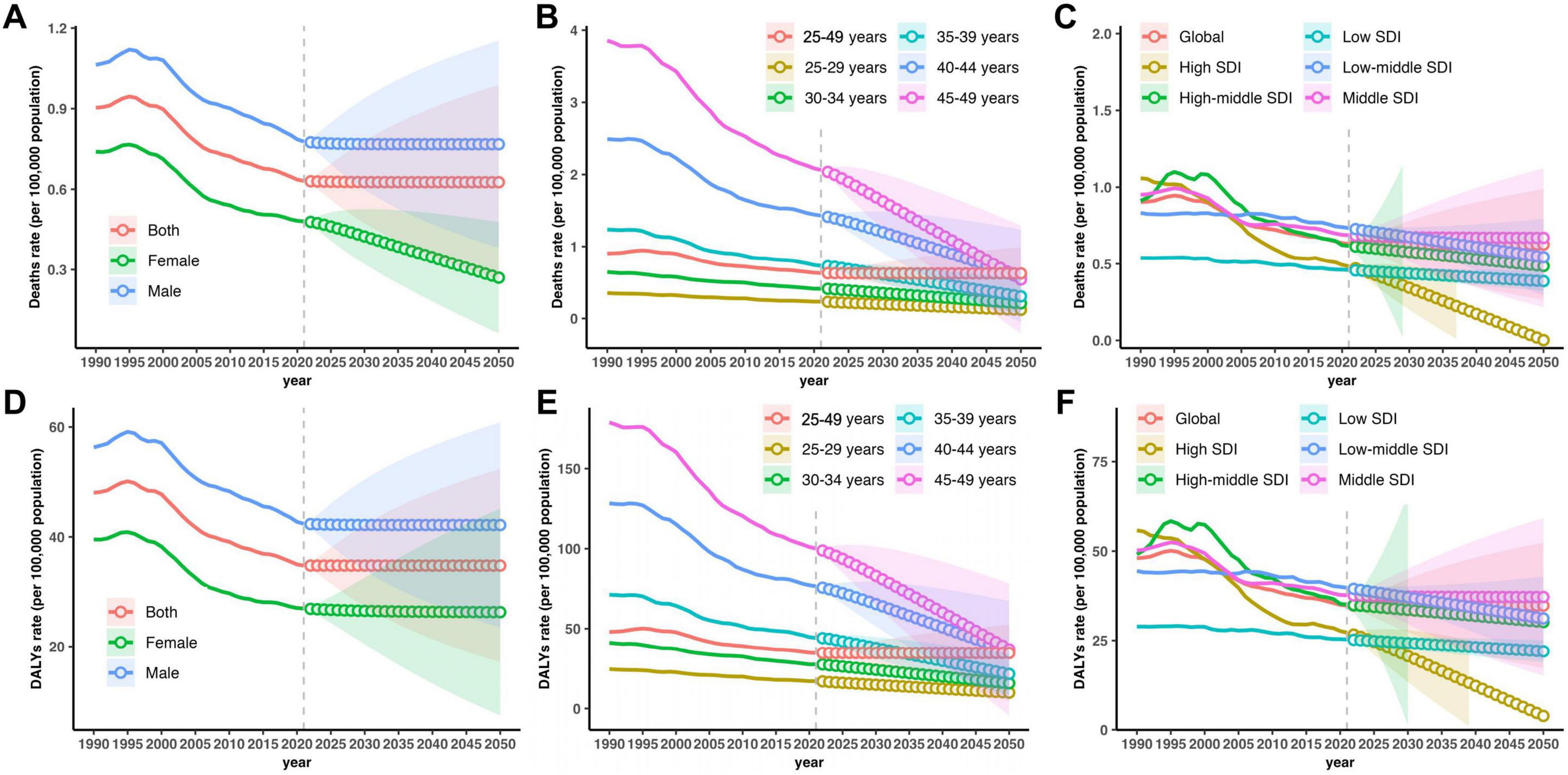
Figure 5. Projected subarachnoid hemorrhage deaths and disability-adjusted life years (DALYs) attributable to high systolic blood pressure among 25–49 years from 1990 to 2050, by sex, age and Socio-demographic Index (SDI) region. (A–C) Trends and projections in deaths rate by sex, age and SDI region. (D–F) Trends and projections in DALYs rate by sex, age and SDI region.
The forecasted trends in SAH DALYs attributable to high SBP among individuals aged 25–49 years suggest a continued global decline, accompanied by persistent disparities by sex, age, and SDI level. By sex, male DALYs are projected to remain relatively stable at 42.16 (23.48–60.84) per 100,000 by 2050, whereas female DALYs may decline slightly from 26.72 (24.35–29.08) in 2025 to 26.30 (7.46–45.13) in 2050 (Figure 5D and Supplementary Table 4). Age-specific projections indicate sharper reductions among older subgroups, with DALYs in the 45–49 age group forecasted to drop from 93.67 (85.08–102.27) to 37.01 (−4.22 to 78.25). Globally, SAH DALY rates are expected to stabilize at around 34.78 per 100,000 between 2025 and 2050, with progressively wider uncertainty intervals (2025: 31.53–38.03; 2050: 17.17–52.38) (Figure 5E and Supplementary Table 4). High-SDI regions are forecasted to achieve the most substantial reductions, from 24.61 (21.09–28.14) to 3.86 (−12.19 to 19.91), while high-middle SDI regions may experience less consistent declines, with DALYs projected at 30.18 (−146.58 to 206.94) by 2050. Middle-SDI and low-middle SDI regions are expected to have modest reductions or stable rates, at 37.19 (15.18–59.19) and 31.20 (19.49–42.90), respectively. Low-SDI regions are projected to see a gradual decline to 21.97 (18.87–25.07) (Figure 5F and Supplementary Table 4). These forecasts underscore global progress in reducing SAH DALYs related to high SBP, particularly in high-SDI settings, while emphasizing the need for targeted strategies to address ongoing inequities.
Discussion
This study provides a comprehensive assessment of global and regional trends in SAH mortality and DALYs attributable to high SBP among adults aged 25–49 years, along with projections to 2050. The findings highlight substantial progress in reducing the burden of SAH associated with elevated SBP, particularly in high-SDI regions, while underscoring persistent disparities across socio-demographic, sex, and age groups.
Moreover, clear sex-specific disparities were observed. Males consistently exhibited higher mortality and DALYs attributable to high SBP-related SAH than females, which may be associated with poorer hypertension control, higher prevalence of smoking and alcohol consumption, and lower healthcare utilization in men. In contrast, the relative decline in female burden may relate to improved awareness and management of blood pressure, as well as protective hormonal factors before menopause. These findings align with previous epidemiological studies reporting sex differences in stroke and SAH outcomes (Franssen et al., 2025; Zhang C. et al., 2025; Zhang J. et al., 2025).
The significant decline in SAH mortality and DALYs in high-SDI regions aligns with decades of investment in hypertension screening, treatment, and stroke care. Prior studies have shown that improved hypertension control, widespread availability of antihypertensive medications, and the establishment of organized stroke systems of care, including aneurysm screening and early surgical or endovascular intervention, have contributed to substantial reductions in SAH mortality in these settings (Boumiza et al., 2021; Nave et al., 2014; Ota and Matsubara, 2021). Moreover, the decline in case fatality rates may reflect advances in neurocritical care and rehabilitation services. Mechanistically, these trends may relate to better control of chronic vascular damage induced by sustained high SBP, including reduced progression of cerebral aneurysms and arterial dissections, both key pathological substrates of SAH (Cayron et al., 2025; Pinsky et al., 2024; Schmidt et al., 2021). Experimental and clinical studies have also suggested that effective SBP management can modulate vessel wall remodeling and decrease the risk of aneurysm rupture by limiting matrix degradation, smooth muscle cell apoptosis, and inflammatory infiltration in cerebral arteries (Chi et al., 2025; Jeong et al., 2025; Lussier et al., 2024).
By contrast, many middle- and low-SDI regions have seen slower progress or even increases in SAH burden. These trends reflect ongoing gaps in hypertension detection, access to affordable care, and population-level prevention strategies. In several of these regions, structural barriers such as weak primary care systems, inadequate health financing, and limited availability of essential medications hinder effective blood pressure management (Papatsoris et al., 2025). Additionally, population transitions toward urbanization, dietary shifts toward high sodium and low potassium intake, and rising prevalence of obesity have further exacerbated hypertension-related risks (Jozwiak et al., 2025; Knowles and Raitt, 2025). Notably, the widening uncertainty intervals in our projections, particularly in middle-SDI settings, highlight the critical importance of strengthening surveillance data quality to better guide policy responses.
Age-specific patterns reveal that SAH burden increases progressively across the 25–49 age range, peaking in the 45–49 group, consistent with the cumulative vascular injury associated with prolonged exposure to elevated SBP. The steeper declines in burden within this age band likely reflect targeted hypertension interventions among older working-age adults, as well as secondary prevention efforts in individuals identified as high risk (Ofori et al., 2024). Looking ahead, the projected continued decline in SAH burden globally—especially in high-SDI regions—is encouraging, yet the persistence of stark disparities underscores the need for intensified efforts in low- and middle-SDI settings. Multifaceted strategies are essential, combining population-level measures (such as salt reduction, promotion of healthy diets, tobacco and alcohol control) with expanded access to hypertension screening, diagnosis, and treatment (Gu et al., 2025). Integration of cardiovascular risk management into universal health coverage and primary care systems represents a key opportunity to address these challenges. Furthermore, emerging evidence on the molecular mechanisms linking SBP to aneurysm pathogenesis—such as the roles of transforming growth factor-β signaling, matrix metalloproteinases, and inflammatory cytokines—highlights the potential for future pharmacological interventions beyond blood pressure control alone (Glass et al., 2014).
Several limitations should be noted. The accuracy of our estimates depends on the quality and availability of primary data, which remain limited in some low-SDI regions. In addition, projections are based on current trends and assume no major disruptions, but future policy shifts, technological innovations, or unforeseen events (e.g., pandemics) could alter trajectories (GBD 2021 Causes of Death Collaborators, 2024; Murray and GBD 2021 Collaborators, 2024). Despite these uncertainties, the study offers valuable insights to inform global and regional strategies aimed at reducing the preventable burden of SAH attributable to high SBP.
Conclusion
In conclusion, despite global declines in SAH mortality and DALYs attributable to high SBP, large disparities remain across sex, age, and SDI levels. These findings highlight the urgent need for equitable hypertension control and strengthened health systems, particularly in low- and middle-SDI regions. Advances in understanding the vascular effects of high SBP and aneurysm pathophysiology may offer new prevention strategies. Focused, data-driven interventions are essential to further reduce premature SAH deaths and disability worldwide.
Data availability statement
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
PC: Conceptualization, Data curation, Methodology, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JC: Investigation, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. JL: Formal analysis, Funding acquisition, Investigation, Project administration, Resources, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnhum.2025.1700918/full#supplementary-material
Abbreviations
SAH, subarachnoid hemorrhage; SBP, systolic blood pressure; DALYs, disability-adjusted life years; EAPC, estimated annual percentage change; ARIMA, autoregressive integrated moving average; SDI, Socio-demographic Index; UI, uncertainty interval; GBD, Global Burden of Disease; IHME, Institute for Health Metrics and Evaluation; TMREL, theoretical minimum risk exposure level; ICD, International Classification of Diseases; AIC, Akaike information criterion.
Footnotes
References
Betteridge, T., Finnis, M., Cohen, J., Delaney, A., Young, P., Udy, A., et al. (2024). Blood pressure management goals in critically ill aneurysmal subarachnoid hemorrhage patients in australia and New Zealand. J. Neurosurg. Anesthesiol. 36, 237–243. doi: 10.1097/ANA.0000000000000926
Boumiza, S., Chahed, K., Tabka, Z., Jacob, M.-P., Norel, X., and Ozen, G. (2021). MMPs and TIMPs levels are correlated with anthropometric parameters, blood pressure, and endothelial function in obesity. Sci. Rep. 11:20052. doi: 10.1038/s41598-021-99577-2
Cayron, A. F., Morel, S., Azam, M., Haemmerli, J., Aoki, T., Bijlenga, P., et al. (2025). Enhanced intracranial aneurysm development in a rat model of polycystic kidney disease. Cardiovasc. Res. 121, 915–928. doi: 10.1093/cvr/cvaf063
Chi, E., Chandrasekara, S., and Keating, D. T. (2025). Severe pulmonary arterial hypertension and cardiogenic shock in acute systemic lupus erythematosus. BMJ Case Rep. 18:e262651. doi: 10.1136/bcr-2024-262651
Eagles, M. E., Veilleux, C., Riva-Cambrin, J., and Macdonald, R. L. (2025). Blood pressure targets after aneurysmal subarachnoid hemorrhage: Is lower better? Neurosurgery doi: 10.1227/neu.0000000000003556 [Online ahead of print].
Fan, K. M., Rimal, J., Zhang, P., and Johnson, N. W. (2022). Stark differences in cancer epidemiological data between GLOBOCAN and GBD: Emphasis on oral cancer and wider implications. EClinicalMedicine 54:101673. doi: 10.1016/j.eclinm.2022.101673
Franssen, M. A., Tjerkstra, M. A., Heijink, M., Rotman, S. A., Verbaan, D., van Bavel, E., et al. (2025). The polyunsaturated fatty acid and oxylipin plasma signature of aneurysmal subarachnoid haemorrhage, case-control study. Neurotherapeutics 5:e00736. doi: 10.1016/j.neurot.2025.e00736
Frontera, J. A., Fernandez, A., Schmidt, J. M., Claassen, J., Wartenberg, K. E., Badjatia, N., et al. (2010). Clinical response to hypertensive hypervolemic therapy and outcome after subarachnoid hemorrhage. Neurosurgery 66, 35–41; discussion 41. doi: 10.1227/01.NEU.0000359530.04529.07
GBD 2021 Causes of Death Collaborators (2024). Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: A systematic analysis for the global burden of disease study 2021. Lancet 403, 2100–2132. doi: 10.1016/S0140-6736(24)00367-2
GBD 2021 Diseases and Injuries Collaborators (2024). Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: A systematic analysis for the global burden of disease study 2021. Lancet 403, 2133–2161. doi: 10.1016/S0140-6736(24)00757-8
GBD 2021 Global Subarachnoid Hemorrhage Risk Factors Collaborators, Rautalin, I., Volovici, V., Stark, B. A., Johnson, C. O., Kaprio, J., et al. (2025). Global, regional, and national burden of nontraumatic subarachnoid hemorrhage: The global burden of disease study 2021. JAMA Neurol. doi: 10.1001/jamaneurol.2025.1522 [Online ahead of print].
Glass, G. E., Murphy, G. F., Esmaeili, A., Lai, L.-M., and Nanchahal, J. (2014). Systematic review of molecular mechanism of action of negative-pressure wound therapy. Br. J. Surg. 101, 1627–1636. doi: 10.1002/bjs.9636
Gu, H., Shi, B., He, H., Yuan, S., Cai, J., Chen, X., et al. (2025). Association between excessive internet use time, internet addiction, and physical-mental multimorbidity among Chinese adolescents: Cross-sectional study. J. Med. Internet Res. 27:e69210. doi: 10.2196/69210
Haripottawekul, A., Barakzai, R., Gonzalez, W., Furie, K. L., Thompson, B. B., and Mahta, A. (2025). Association of external ventricular drain duration and output with cerebral infarct risk in aneurysmal subarachnoid hemorrhage. J. Clin. Neurosci. 133:111059. doi: 10.1016/j.jocn.2025.111059
Jeong, S. Y., Jung, S. C., Roh, Y. H., Kwon, S. U., Kang, D.-W., Kim, J. S., et al. (2025). Serial changes and optimal imaging windows in vessel wall MRI for unruptured intracranial artery dissection. Sci. Rep. 15:21864. doi: 10.1038/s41598-025-05732-4
Jozwiak, M., Cousin, V. L., De Backer, D., Malbrain, M. L. N. G., Monnet, X., Messina, A., et al. (2025). Vasopressin use across shock states: International insights from an international ESICM-endorsed survey: The PRESS survey. Crit. Care 29:273. doi: 10.1186/s13054-025-05505-5
Knowles, C., and Raitt, J. (2025). Blood transfusion – moving from what to how. Scand. J. Trauma Resusc. Emerg. Med. 33:118. doi: 10.1186/s13049-025-01428-w
Lee, H. S., Sohn, M. K., Lee, J., Kim, D. Y., Shin, Y.-I., Oh, G.-J., et al. (2025). Five-year functional outcomes among patients surviving aneurysmal subarachnoid hemorrhage. JAMA Netw. Open 8:e251678. doi: 10.1001/jamanetworkopen.2025.1678
Lin, X., Khalin, I., Harapan, B. N., Terpolilli, N. A., Schwarting, J., and Plesnila, N. (2023). Perivascular macrophages mediate microvasospasms after experimental subarachnoid hemorrhage. Stroke 54, 2126–2134. doi: 10.1161/STROKEAHA.122.042290
Lussier, G., Evans, A. J., Houston, I., Wilsnack, A., Russo, C. M., Vietor, R., et al. (2024). Compact arterial monitoring device use in resuscitative endovascular balloon occlusion of the aorta (REBOA): A simple validation study in swine. Cureus 16:e70789. doi: 10.7759/cureus.70789
Lv, B., Lan, J.-X., Si, Y.-F., Ren, Y.-F., Li, M.-Y., Guo, F.-F., et al. (2024). Epidemiological trends of subarachnoid hemorrhage at global, regional, and national level: A trend analysis study from 1990 to 2021. Mil. Med. Res. 11:46. doi: 10.1186/s40779-024-00551-6
Murray, C. J. L., and GBD 2021 Collaborators (2024). Findings from the global burden of disease study 2021. Lancet 403, 2259–2262. doi: 10.1016/S0140-6736(24)00769-4
Nave, A. H., Mižíková, I., Niess, G., Steenbock, H., Reichenberger, F., Talavera, M. L., et al. (2014). Lysyl oxidases play a causal role in vascular remodeling in clinical and experimental pulmonary arterial hypertension. Arterioscler. Thromb. Vasc. Biol. 34, 1446–1458. doi: 10.1161/ATVBAHA.114.303534
Ofori, M. A., Mensah, D. K., Nizeyimana, I., Jha, N., Zeba, Z., and Roy, S. (2024). High blood pressure and depression among the working population of Ghana: A generalized linear model of the risk factors. Depress. Anxiety 2024, 5261760. doi: 10.1155/2024/5261760
Ota, K., and Matsubara, N. (2021). A case of segmental arterial mediolysis: Hemoperitoneum with hemorrhagic shock due to rupture of a visceral artery aneurysm following subarachnoid hemorrhage. J. Neuroendovasc. Ther. 15, 189–194. doi: 10.5797/jnet.cr.2020-0068
Papatsoris, A., Geavlete, B., Radavoi, G. D., Alameedee, M., Almusafer, M., Ather, M. H., et al. (2025). Management of urinary stones by experts in stone disease (ESD 2025). Arch. Ital. Urol. Androl. 97:14085. doi: 10.4081/aiua.2025.14085
Pinsky, M. R., Gomez, H., Wertz, A., Leonard, J., Dubrawski, A., and Poropatich, R. (2024). Evaluation of a physiologic-driven closed-loop resuscitation algorithm in an animal model of hemorrhagic shock. Crit. Care Med. 52, 1947–1957. doi: 10.1097/CCM.0000000000006297
Poliseli, G. B., Santos, T. A. D., Nunes, H. R., de, C., Victória, C., Zanini, M. A., et al. (2024). Trends in hospitalization and mortality rates associated with subarachnoid hemorrhage and unruptured cerebral aneurysms in Brazil. World Neurosurg. 191, e411–e422. doi: 10.1016/j.wneu.2024.08.149
Rautalin, I. M., Asikainen, A., and Korja, M. (2024). Modifiable risk factors for subarachnoid hemorrhage: Narrative review with an emphasis on common controversies and epidemiologic pitfalls. Neurology 103:e210052. doi: 10.1212/WNL.0000000000210052
Schmidt, K. A., Cromer, G., Burhans, M. S., Kuzma, J. N., Hagman, D. K., Fernando, I., et al. (2021). Impact of low-fat and full-fat dairy foods on fasting lipid profile and blood pressure: Exploratory endpoints of a randomized controlled trial. Am. J. Clin. Nutr. 114, 882–892. doi: 10.1093/ajcn/nqab131
Wyckoff, S., and Hsiang-Yi Chou, S. (2025). High-grade subarachnoid hemorrhage – beyond guidelines. Neurol. Clin. 43, 107–126. doi: 10.1016/j.ncl.2024.07.006
Zhang, Y. F., Li, S.-Z., Wang, S.-W., Mu, D., Chen, X., Zhou, S., et al. (2025). Zoonotic diseases in China: Epidemiological trends, incidence forecasting, and comparative analysis between real-world surveillance data and global burden of disease 2021 estimates. Infect. Dis. Poverty 14:60. doi: 10.1186/s40249-025-01335-3
Zhang, C., Tang, W., Yin, P., Yang, C., Zhao, X., Fang, X., et al. (2025). Sex differences in incidence and risk factors for delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage: A propensity score-matched analysis. J. Am. Heart Assoc. 14:e038952. doi: 10.1161/JAHA.124.038952
Zhang, J., Sun, J., Xu, Y., Jing, H., Zhang, L., and Chen, W. (2025). Different change patterns and sex difference for stroke and its subtypes mortality attributable to tobacco in China from 1990 to 2021. BMC Public Health 25:3189. doi: 10.1186/s12889-025-24336-1
Keywords: subarachnoid hemorrhage, high systolic blood pressure, young adults, global burden, temporal trends
Citation: Chen P, Chen J and Liu J (2025) Rising burden of subarachnoid hemorrhage linked to high systolic blood pressure among young and middle-aged populations: temporal trends and global implication. Front. Hum. Neurosci. 19:1700918. doi: 10.3389/fnhum.2025.1700918
Received: 08 September 2025; Accepted: 13 October 2025;
Published: 30 October 2025.
Edited by:
Hongjian Pu, University of Pittsburgh, United StatesReviewed by:
Weimin Yang, The First Affiliated Hospital of Zhengzhou University, ChinaNicholas Kulaba, Gulu University, Uganda
Copyright © 2025 Chen, Chen and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiazuo Liu, ODk2Nzg0NTQ1QHFxLmNvbQ==
†These authors have contributed equally to this work
 Pengfei Chen
Pengfei Chen Junlin Chen2†
Junlin Chen2†