- 1Neurosurgery Service, Central Virginia Veterans Affairs Health Care System, Richmond, VA, United States
- 2Department of Neurosurgery, Virginia Commonwealth University School of Medicine, Richmond, VA, United States
Introduction: Patient-reported outcomes are widely used to measure surgical success in patients undergoing elective lumbar spine surgery. However, unique goals created by patients may provide a more accurate and individual representation of surgical success. We hypothesize that creation of a patient-derived goal-setting program, and analysis of such goals using an interactive visual dashboard, may provide unique insight into factors important to patients undergoing elective lumbar spine surgery.
Methods: Creation of a visual dashboard was performed with key stakeholders (neurosurgeons, advanced practice providers and informaticists). Patient derived functional and pain goals were set and documented prior to surgery. Goal achievement and surgery satisfaction were collected at primary (6 weeks, 3 months) and secondary (6, 12, ≥12 months postoperatively) endpoints. Schema were created to organize words used in patient-identified goals into specific trends for analysis. Data were analyzed using Chi-square test for statistical significance.
Results: A real-time visual electronic dashboard was successfully implemented, and used throughout the study. A total of 158 patients underwent elective lumbar spine surgery, of which 75 (47%) participated in the goal-setting program. Most patients identified a pain goal of ≥75% reduction (X2 = 32.000, p < 0.001). The most common word used in functional goals was “able.” The most common word used in pain goals was “improvement.” Functional goals were separated into three schemata: “Change Talk,” (60%) “Activity,” (20%) and “Symptoms” (20%). Pain goals were separated into two schemata: “Symptoms” (64%) and “Change Talk” (36%). At 3 months postoperatively, 86% of patients were satisfied with surgery although only 39.1% had achieved their functional goals and 67.9% had achieved their pain goals.
Discussion: The study illustrates the implementation, use and interpretation of a real-time visual dashboard in a unique, patient-derived goal setting program for patients undergoing elective lumbar spine surgery. Patient satisfaction with surgery may not directly correlate with functional and pain goal achievement. Less than half of the eligible total population participated, underscoring the difficulty of long-term compliance. Expanded integration of this program may allow improved understanding of unique factors important topatients, as they undergo elective lumbar spine surgery.
Introduction
Due to the varied and patient-specific impacts that degenerative spine disease and spine surgery can have in a person's life, there is a need to adopt a more individualistic and unique approach to perioperative surgical outcome analysis (1). Currently acceptable methods of measuring surgical success include longitudinal tracking of well-validated and quantifiable scales and patient reported outcomes (PROs). Several studies have demonstrated successful implementation of established PROs into the clinical workflow in both medical and surgical specialties, including head and neck cancer patients, specialty pharmacies, mental health, and spine surgery (2–5).
Analysis and measurement of such measures can be performed using interactive visual electronic dashboards. Successful dashboard creation and integration into the clinical workflow relies on standardization of documentation and data collection, stakeholder engagement, consensus on relevant PROs to use and seeking feedback through multiple reiteration cycles (2, 5). PRO dashboards have been shown to facilitate multidisciplinary communication, improve quality of care delivery, highlight key issues and aid in shared decision making (4, 6, 7).
Although prespecified PRO measures serve as established and validated measurements, they do not always reflect each patient's specific preferences and their personalized goals of surgical care. In our clinic's experience, we have found that patients' Oswestry Disability Index scores did not tend to correlate with patient's subjective assessment of postoperative success. Instead of having providers decide what constitutes a successful procedure by using less-individualistic measures, achieving the patient's specific preferences and goals should be the foundation of surgical success (8–12). Documentation of patient goals for surgery was previously performed by our providers using free-text into the Veterans' Affairs electronic health record (EHR). These entries were not standardized nor completed by all providers and thus it presented challenges by requiring time consuming manual chart reviews for data extraction, analysis and interpretation. The primary goal of this study was to design and implement a patient-derived surgical goal-setting program for veterans undergoing elective lumbar surgery at our medical center. To the best of our knowledge, this approach is the first of its kind to systematically document and track patient-generated goals and preferences for elective spine surgery using a real-time visual dashboard. We secondarily aimed to identify longitudinal trends in postoperative achievement of patient-derived goals, standardize documentation and data collection of patient-derived goals into the electronic health record, and create a visual interactive dashboard for longitudinal tracking.
Materials and equipment
Microsoft PowerBI [Version: 2.131.901.0 64-bit (July 2024), (RRID:SCR_022927)] was used to create an automated dashboard. Microsoft Excel Microsoft Excel for Microsoft 365 MSO (Version 2402 Build 16.0.17328.20550, 32-bit, RRID:SCR_016137) and IBM SPSS Statistics (Version 29.02.0, RRID:SCR_016479, IBM Corporation) were used to analyze descriptive statistics and summarize study sample characteristics. We used Microsoft SQL Server management studio for SQL queries (Version 19.3.4, RRID:SCR_025972).
Methods
Our protocol was reviewed and approved by Central Virginia VA Medical Center Institutional Review Board and was exempt from informed consent due to the quality improvement nature of our study.
Design and test phase
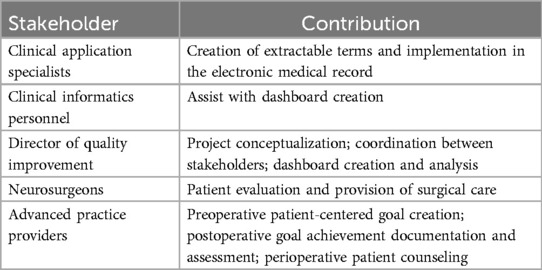
From August 2021 to November 2021, stakeholders (Table 1) were engaged early in the process. Consensus was reached on three key informatic elements, which were then created, tested and incorporated in the Veterans Affairs' Computerized Patient Record System (CPRS) as “health factors”. Three health factors were created: “Functional and Pain Goals”, “Functional and Pain Goals Achievement,” and “Satisfaction with surgery” (Table 2). Note templates were then created in the CPRS. These note templates included drop-down and checkbox style formats as well as an open-text free response box. Drop down and check box menus allowed providers to choose preoperative or postoperative time frame, goal achievement and surgery satisfaction. Open-text boxes allow providers to document patient goals as they are set prior to surgery. The note templates then permitted providers to quickly work with the patient and document his or her responses without leading to significant delay in the clinic visit. Data from the note template responses were then extracted using PowerBI (see “Dashboard creation” below). The processes and steps to develop a patient-derived surgical goal setting dashboard are described in Figure 1.
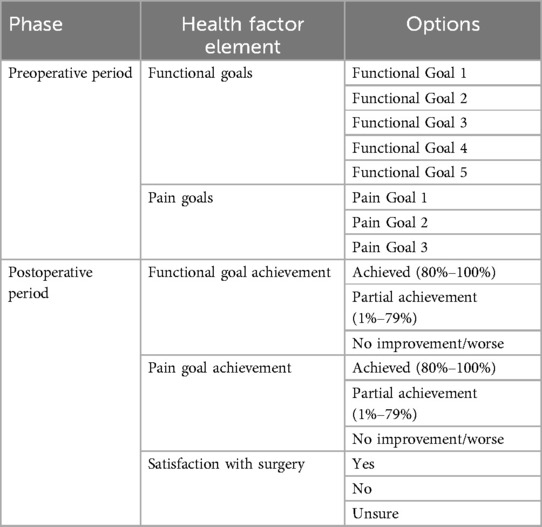
Table 2. Preoperative and postoperative extractable informatics elements and their respective options.
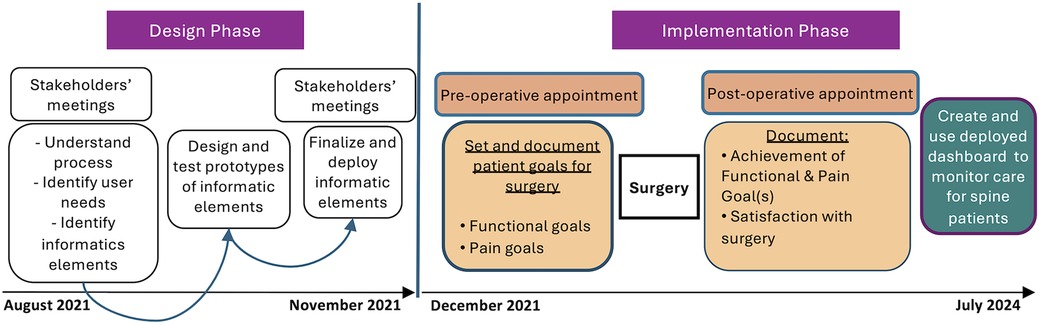
Figure 1. Process of creating and implementing dashboard for tracking patient goals for veterans who have neurosurgery procedures. The Design phase emphasizes the importance of stakeholders’ meetings to understand process and needs of each user, followed by creation and testing of informatics elements that will be incorporated into the EHR. Implementation phase describes the steps for setting and documenting goals for surgery preoperatively, as well as documentation of achievement and satisfaction with surgery. The process ends with creation and deployment of the interactive dashboard to monitor real-time goal tracking and achievement.
Implementation phase
Starting December 2021, patients undergoing elective lumbar spine surgery were asked about the three health factors identified above. Patients were excluded if they were having an emergent lumbar surgical procedure or unable to speak English.
Patients were permitted to self-identify up to 5 separate functional goals and 3 separate pain goals in a free-response fashion. When patients expressed difficulty in identifying specific goals, the clinical care team provided guidance. The goals were discussed verbally, and a quote of each of the patient's goal(s) was documented in the medical record using a standardized template.
Postoperative assessment of functional and pain goals, as well as overall satisfaction with surgery was performed at two routine postoperative visits (6 weeks and 3 months postoperatively). Additional rates for later follow-up appointments were included on a patient-by-patient basis. Data is reported as “n/a” if a patient did not present for a particular time point in the follow up period. Patients self-reported goal achievement rates were defined using a numeric rating scale with the following categories: “Achieved” (80%–100%), “Partial achievement” (1%–79%) or “No improvement/Worse.” Satisfaction with surgery was defined using a 3-point Likert scale: “Yes,” “No,” or “Unsure” (Table 2).
Dashboard creation
An interactive visual dashboard was created using Microsoft PowerBI to automatically harvest the data documented in CPRS note templates. Data in VHA EHR is exported to and stored in VHA's databases daily per VHA IT infrastructure workflows and this data can be extracted using Structured Query Language (SQL) queries. We created SQL queries using Microsoft SQL Server management studio to specifically extract data documented in CPRS note templates' health factors. The SQL queries are then validated and imported into Microsoft PowerBI. Microsoft PowerBI was used to automate the data extraction for the interactive visual dashboard. Data extraction is set to be refreshed daily and clinicians can visualize patient progress in near real-time. Different views (word cloud, functional and pain goals, achievement of goals and satisfaction with surgery) were created to display our findings to our providers. Clinicians can also select different parts of the dashboard and a list and number of patients will be displayed/refresh for each selected tab. Goals, goal achievement rates and satisfaction with surgery rates for each patient at 6 weeks and 3 months postoperatively as well as additional later assessments on a patient-by-patient basis. Our dashboard also facilitated visualization of overall program results, including the aforementioned “health factors”, as well as percentage of patients with preoperative goals documented. Word frequency was calculated and used to create a word cloud. The word cloud provides a visual representation of word frequency and can provide insights on goal patterns desired by patients undergoing lumbar spine surgery. Two separate word clouds using the English language were created to identify the most common words used by patients in describing functional goals and pain goals. Non-specific common words were removed from analysis [to, or, do, my, now, like, be, would, up, and, than, I, 1, 2, 3, a, with, at, to, from, for, by, his, of, on, the, in]. Three or more repeated entries were needed to be included in the word cloud. Schema were then created by two authors (SM, AJC) to organize the words into common frameworks to perform post-hoc analyses. Schema were created to elucidate commonality among goal words used to better understand a framework in which veterans prioritize and create perioperative goals.
Analysis
Microsoft Excel Microsoft® Excel® for Microsoft 365 MSO and IBM SPSS Statistics were used to analyze descriptive statistics and summarize study sample characteristics. Statistical analyses included mean with standard deviation for continuous variables and frequencies with percentages and Chi-square analysis for categorial variables. Fisher exact test was used for comparing categorical variables with n < 10. P < 0.05 was used for significance.
Results
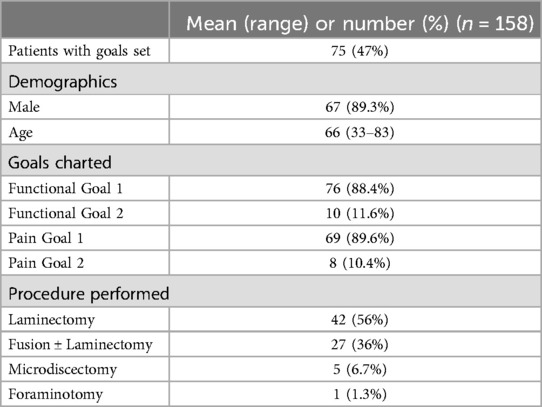
Functional and pain goal documentation
From December 2021 through July 2024, 158 patients underwent elective lumbar spine surgery at our institution. A total of 47% (n = 75) had functional and pain goals documented during the preoperative period (Table 3). Most patients were male (89.3%) and only identified one functional or pain goal; only 11.6% of patients identified 2 functional goals and 10.4% of patients identified 2 pain goals. Laminectomy was the most common procedure performed (56% of all procedures).
Goal identification: word clouds and post-hoc schema analyses
The most common word used in functional goals was “able” (63), followed by “without” (n = 30), “Again” (n = 28), “pain” (n = 27), “leg” (n = 17), “want” (n = 17), “mile” (n = 12) (Figures 2A,B). The most common word used in pain goals was “improvement” (n = 59), followed by “pain” (n = 55), “leg” (n = 42), “back” (n = 15) (Figures 3A,B).
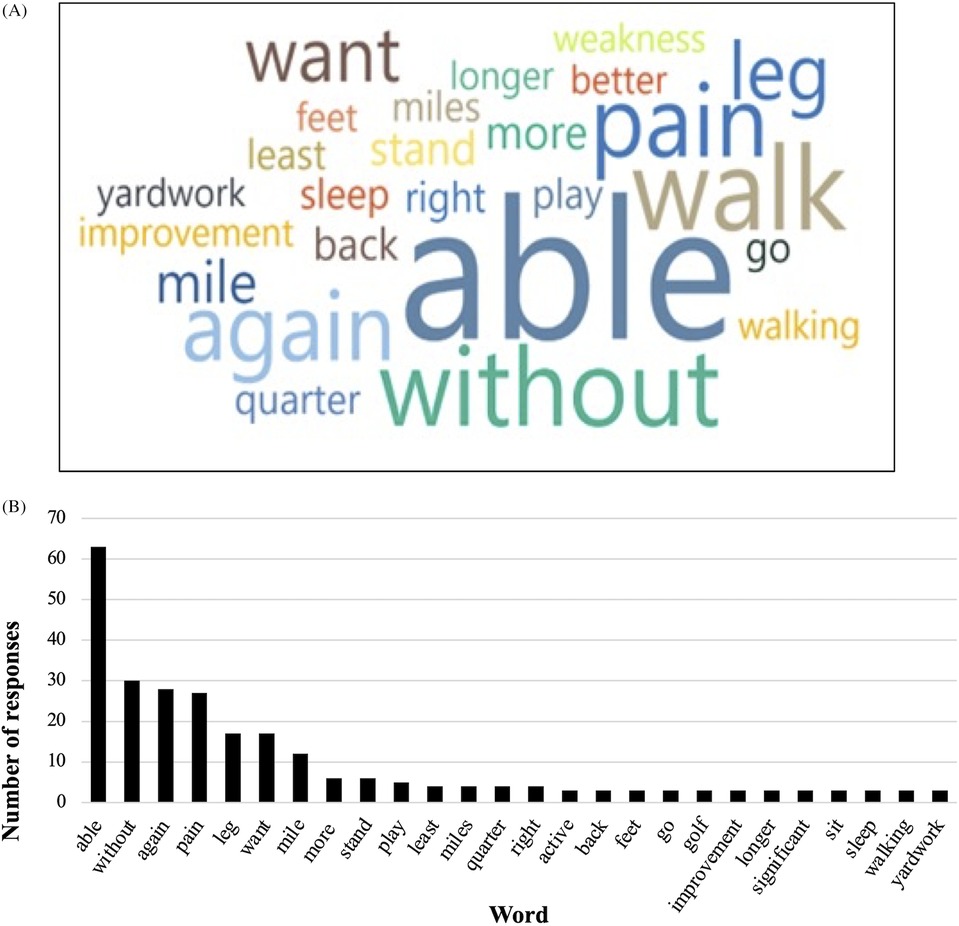
Figure 2. Patient-derived functional goals. (A) Word cloud visual representation of most frequent words used by patients in functional goals. (B) Frequency of each word used by patients in functional goals.
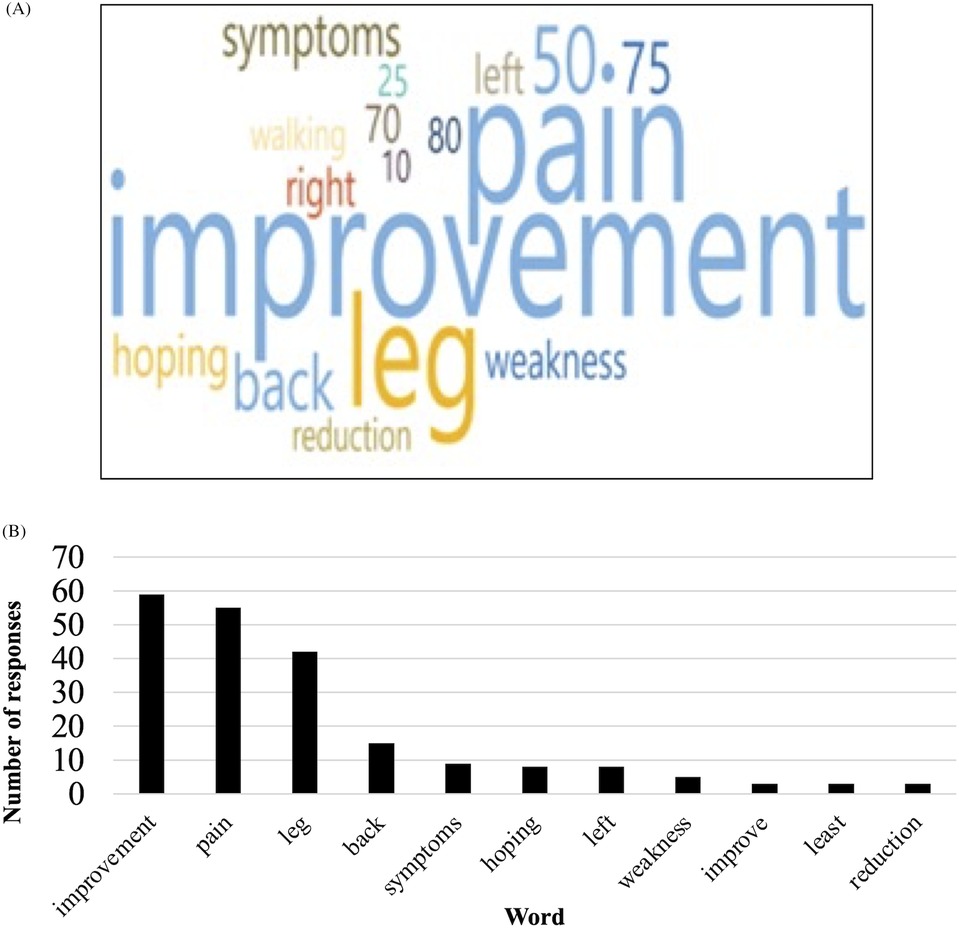
Figure 3. Patient-derived pain goals. (A) Word cloud visual representation of most frequent words used by patients in pain goals. (B) Frequency of each word used by patients in pain goals.
Five numbers, representing the percent improvement patients would like to see in their pain postoperatively, were listed in patients' pain goals: “75” (n = 16), “70” (n = 6), 80 (n = 4), “10” (n = 3), “25” (n = 3) (Figure 4A). There was a statistically significant difference in the incidence of the pain goal percentages identified by patients (X2 = 57.480, p < 0.001). After organizing the identified pain goals into two cohorts, “<75%” (n = 12) and “≥75%,” (n = 20), the difference remained significant (X2 = 32.000, p < 0.001) (Figure 4B).
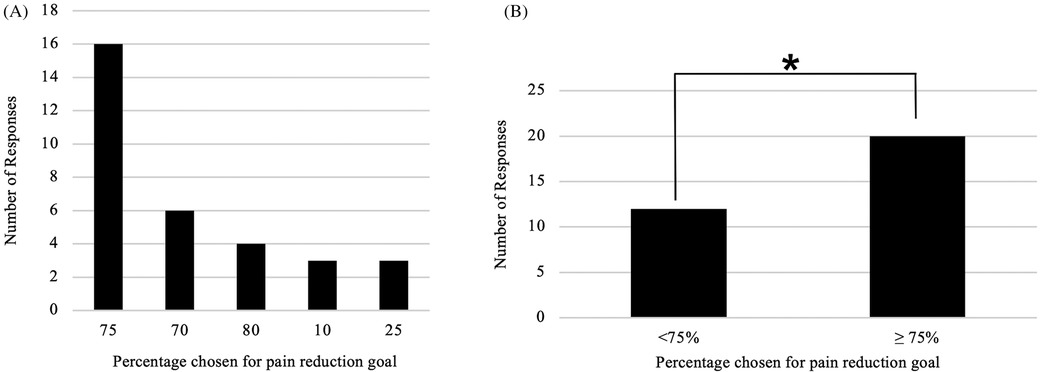
Figure 4. (A) Percentages of desired pain improvement postoperatively chosen by patients. (B) Analysis of <75% and ≥75% desired pain improvement cohorts.
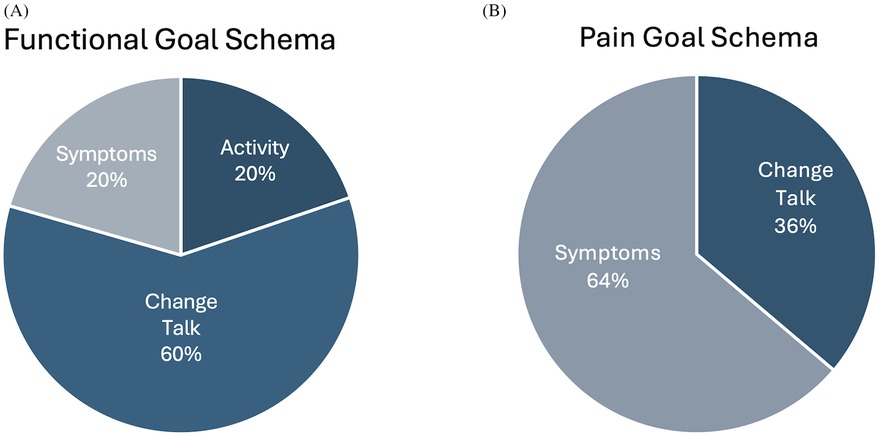
Creation of post-hoc goal schema demonstrated that 60% of functional goal entries were “Change Talk” (defined as “entries” predominantly using words invoking a sense of change or evolution as reviewed by two authors), 20% Activity and 20% Symptoms (Figure 5A). Creation of pain goal schema showed that 64% of entries were Symptoms and 36% of entries were “Change Talk” (Figure 5B).
Goal achievement
Postoperative functional goal achievement was documented for 67 unique patients. At 6 weeks postoperatively, 85% (n = 57) reported their functional goal achievement. Of those 40.4% (n = 23) reported their goal as “Achieved,” 38.6% (n = 22) reported “Partial achievement,” and 21.1.5% (n = 12) reported “No improvement/Worse”. At 3 months postoperatively, 34.5% (n = 23) reported their functional goal achievement. Of those, 39.1% (n = 9) reported “Achieved”, 56.5% (n = 13) reported “Partial Achievement” and 4.4% (n = 1) reported “No improvement/Worse” (Figure 6). At 6 months postoperatively, 49.3% (n = 33) reported their functional goal achievement. Of those, 69.7% (n = 33) reported “Achieved”, 24.2% (n = 8) reported “Partial achievement”, and 6.1% (n = 3) reported “No improvement/worse”. At 12 months postoperatively, 17.9 (n = 12) reported their functional goal achievement. Of those, 83.3% (n = 10) reported “Achieved”, 8.3% (n = 1) reported “Partial achievement”, and 8.3% (n = 1) reported “No improvement/worse”.
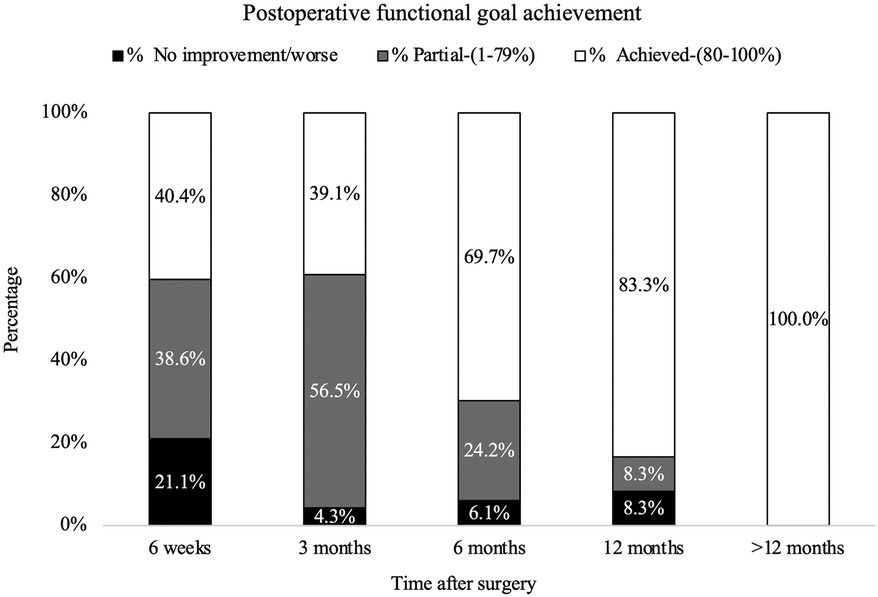
Figure 6. Postoperative functional goal achievement rates at 6 weeks, 3 months, 6 months, 12 months, and >12 months.
At >12 months postoperatively, 1.5% (n = 1) reported their functional goal achievement. Of those, 100% reported “Achieved”, and 0% 0 reported “Partial achievement” or “No improvement/worse” (Figure 6).
Postoperative pain goal achievement was documented for 79 unique patients. At 6 weeks postoperatively 86.7% (n = 65) reported their pain goal achievement. Of those, 63.19% (n = 41) reported “Achieved”, 26.2% (n = 17) report “Partial achievement”, 9.2% (n = 6) reported “No improvement/Worse” and 1.5% reported “Not Applicable”.
At 3 months postoperatively, 37.3% (n = 28) reported their pain goal achievement. Of those, 67.9% (n = 19) reported “Achieved”, 25% (n = 7) reported “Partial achievement” and 3.6% (n = 1) reported “No improvement/worse”, 3.6% (n = 1) reported “Not applicable”. At 6 months postoperatively, 51% (n = 39) reported their pain goal achievement. Of those, 84.6% (n = 33) reported “Achieved”, 5.1% (n = 2) reported “Partial achievement”, 7.7% (n = 3) reported “No improvement/worse”, and 1.5% reported “Not applicable”. At 12 months postoperatively, 21.3% (n = 16) reported their pain goal achievement. Of those, 68.8% (n = 11) reported “Achieved”, 33.5% (n = 5) reported “Partial achievement”, 0% 0 reported “No improvement/worse”. At >12 months postoperatively, 1.3% (n = 1) reported their pain goal achievement. Of those, 100% (n = 1) reported “Achieved”, 0% 0 reported “Partial achievement”, or “No improvement/worse” (Figure 7).
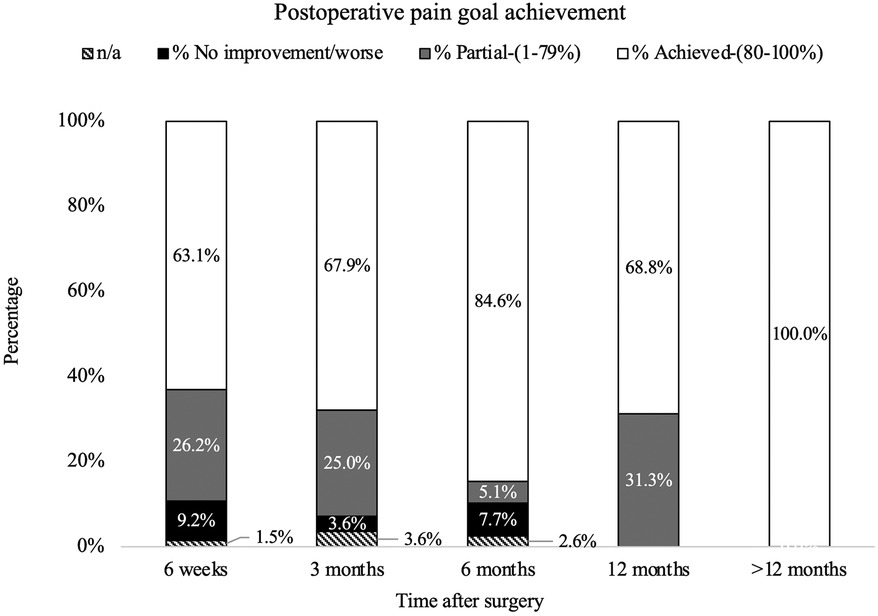
Figure 7. Postoperative pain goal achievement rates at 6 weeks, 3 months, 6 months, 12 months, and >12 months.
Satisfaction with surgery
We collected satisfaction with surgery for 67 unique patients. At 6 weeks postoperatively, 85.1% (n = 57) reported their satisfaction with surgery. Of those, 87.7% (n = 50) responded “Yes”, 8.8% (n = 5) reported “Unsure”, and 3.5% (n = 2) reported “Not satisfied”. At 3 months postoperatively, 32.8% reported their satisfaction with surgery (n = 22). Of those 86.4% (n = 19) reported “Yes”, 13.7% (n = 3) reported “Unsure”, and 0% reported “Not satisfied”. At 6 months postoperatively, 48.3% reported their satisfaction with surgery. Of those, 97% (n = 32) reported “Yes”, 0% reported “Unsure”, and 3% reported “Not satisfied”. At 12 months post-operatively, 17.9% reported their satisfaction with surgery. Of those, 91.7% (n = 11) reported “Yes”, 8.3% (n = 1) reported “Unsure”, and 0% reported “Not satisfied”. At 12 months postoperatively, 100% (n = 1) reported “Yes”, 0% reported “Unsure”, and 0% reported “Not satisfied” (Figure 8).
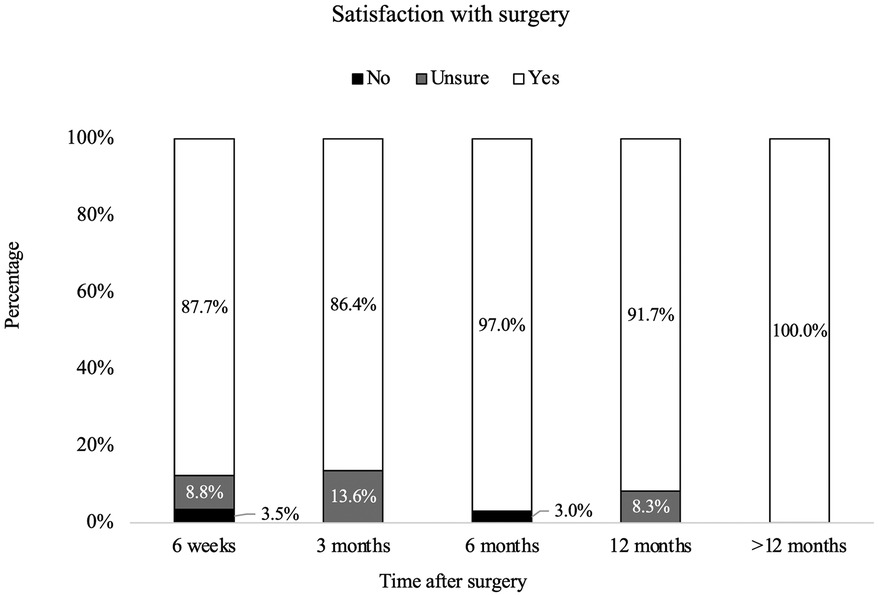
Figure 8. Postoperative operative satisfaction rates at 6 weeks, 3 months, 6 months, 12 months, and >12 months.
Discussion
Our study illustrates the successful design, implementation and post-hoc analysis process of a visual interactive dashboard in the perioperative setting in a veteran population. The program described demonstrates a method to integrate documentation and tracking of patient-derived goals into the clinical workflow for elective spine surgery. Previous studies documented the tracking of validated selected outcome measures that did not account for patient preferences and goals prior to elective surgery.
Visual dashboards have been previously implemented in the clinical setting for other quality improvement initiatives. Such dashboards were successfully created and integrated into clinical care to improve communications and quality of care in head and neck oncology patients (7). Patel et al. highlighted the importance of utilizing stakeholder consultation and engagement to achieve incorporation of clinical outcomes into regular practice for specialty pharmacies within an academic health system (5). Hartzler and colleagues used human-centered design methods to engage stakeholders and successfully develop and implement a visual dashboard that displayed PROs for spine surgery patients (2). Azad et al. successfully integrated quality of life measures such as the Patient Health Questionnaire-9, Oswestry Disability Index, Neck Disability Index, and the Visual Pain Scale into clinical workflow in a tertiary academic health center (3). This group incorporated patient input via a link from the electronic health record (EHR) sent to patients when visits scheduled. Patients were also able to complete questionnaires in clinic either by using a tablet or by manually entered data (via clinic staff) if not done at home. Cronin et al. demonstrated that the creation of a dashboard to collect and display six Patient-Reported Outcomes Measurement Information System health domains is of value for both clinicians and patients (4). Participants perceived the health dashboard positively and felt that a customized assessment portal would improve awareness of their health issues and lead to shared decision making.
Specific to our patient population in the study, documentation of perioperative goals has been previously described in the veteran population using the Goal Attainment Scale (13). We found that it is possible to successfully standardize patient-derived goal collection within the EHR to allow for retrieval of that information without the need for extensive chart review. Organizing the patients' goals into schema allowed investigation of the most common topics listed in patients' goals. Most functional goal entries were classified as “change talk.” This schema classification was used for words or goals invoking a sense of evolution, or change, by two authors (SM, AC) which was found to be a common thread on initial analysis of the words chosen by veterans. Our data therefore suggests that simply experiencing a change from the status quo is more important to patients preoperatively than improving a specific functional activity or symptom. Conversely, specific symptoms (e.g., laterality and anatomic regions) were more commonly identified when describing pain goals, and the use of “change talk” words was less. The data illustrate that patients and providers identify specific pain goals related to anatomic locations they expect to improve with surgery, yet have broader functional goals related to simply becoming more functional overall.
Patients self-identified only five specific percentage goals of pain improvement (which ranged significantly from 10% to 80%), even though patients were free to choose any percentage as a goal. Interestingly, zero patients identified a goal of 100% pain improvement. Creating appropriate preoperative expectations is a key factor in preoperative counseling, and the lack of any patient expecting 100% pain improvement may reflect appropriate perioperative counseling by the surgical team (14). Notably, there is not a standardized preoperative education regimen used in our department which likely reflects the real-world clinical environment at other centers. Conversely, the significantly higher proportion of patients identifying a goal of ≥75% pain improvement compared to <75% pain improvement reflects that most patients who decide to undergo elective lumbar spine surgery expect substantial improvements in their pain postoperatively. These data highlight the balancing act of discussing surgical expectations (in that surgery is neither a “miracle”, nor negligible in benefits and ultimately worthwhile when offered) and comprises the artform of patient selection and preoperative counseling in neurosurgery.
Our data found that postoperative satisfaction scores were generally higher than rates of functional and pain goal achievement. For example, at the initial postoperative visit (6 weeks postoperatively), 87.72% of patients reported being satisfied with surgery but only 40.4% reported functional goal achievement, and 63.1% reported pain goal achievement. Similarly, at 3 months postoperatively, 86.36% reported being satisfied with surgery even though only 39.1% reported achieving their functional goal and 67.9% reported achieving their pain goal. This discordance likely reflects that incompletely understood factors impact a patient's perception of a successful surgery, especially early in the postoperative course. Perhaps patients may perceive a surgery as “successful” if there were no significant complications or if their perioperative inpatient experience was more pleasant than anticipated, independent of achievement of their pain and/or functional goals in the early postoperative course (15). Ultimately, this relationship between patient perception of surgical success and goal achievement merits further investigation.
Pearls and pitfalls of program implementation
We demonstrated that it is possible to successfully standardize and document patient-centric goals of care in a manner that allows for retrieval of that information without the need for extensive chart reviews. Neurosurgeons and advanced practice providers recognized the value of collecting and tracking goals of care to complement clinical data and facilitate patient-centered care. Providers showed strong buy-in, participating in stakeholders' meetings to provide feedback and reported being enthusiastic about having patient-derived outcomes collected. Providers are also able to visualize and use data for quality improvement processes. Each patient's data is recorded in the EHR and can be used during postoperative visits to ascertain progress and realignment of goals.
Some providers reported that data collection was difficult on a consistent basis due to time constraints in a busy clinic setting (with a new patient visit allotted approximately 40 min and a returning patient visit allotted less than 20 min, on average, in our clinic). This may partly explain why we only had data on 48% of elective lumbar spine surgery patients. Anecdotally, the time constraints in the surgical clinic environment are a difficulty faced nearly universally by surgical providers. Perhaps expanding the program to a patient-driven program where answers are collected in the waiting room, either via a paper checklist or electronic, would improve patient participation and decrease provider stress in implementing the project. Patients need provider guidance to ensure reasonable goals are set. Patients who improve after their 6 week or 3-month postoperative appointment do not usually return to our clinic and this can confound the longer-term data.
Limitations
The single-institution nature of our study, as well as the small study population and location at a Veteran's Affairs institution, limits generalizability of our findings to both national and international populations. A potential for bias exists with this study design, as providers were collecting data on their own patients. In addition, providers (not patients) were entering data, which introduces the opportunity for implicit and explicit biases in patient prompting of questions. Approximately half of patients included in the study had goals of care documented at the preoperative visit, which limits our ability to further analyze our results and identify specific patient populations. The participation rate is likely variable due to insensible factors related to patient-provider relationships in the perioperative setting but nonetheless merits further investigation to maximize participation after enrollment. Our dashboard is limited by only incorporating specific health factors identified by the EHR and does not easily incorporate preoperative characteristics in a post-hoc fashion (such as demographic data, diagnosis, previous surgeries or other relevant clinical data). Therefore, more robust comparisons and analyses are limited. A control group (e.g., one who was not offered preoperative goal setting but did have postoperative satisfaction with surgery documented) was not created, as the primary aim of the study was to create the dashboard and understand patient goals, with secondary aims including postoperative patient satisfaction and functional improvement. Nonetheless, this lack of a control limits the assessment of the program in whole in improving patient satisfaction.
We recognize the need to improve workflow integration by developing methods for patients to enter their own surgery goals or to allow for well-trained clinical staff to assist in goal setting at preoperative visits and documentation during postoperative assessments. In the future, it might be possible to share goals of care and achievement with patients in a patient-only dashboard to improve engagement, ownership and agency in their own care (4).
Conclusion
Our study demonstrates automated data extraction of free-text and standardized templated data in the EHR into creation of a separate interactive electronic dashboard. The implementation of the dashboard in the outpatient setting provided our team with an objective tool to track patient-derived surgical goal achievement and surgical satisfaction. Using patient-derived goals, rather than less-specific PROs, provides an opportunity to improve and investigate individualized patient factors. The data presented by the dashboard provides real-time goal tracking which may support future patient care and quality improvement initiatives, such as identifying patient populations or procedures at risk of poor postoperative satisfaction or goal achievement. To this effect, we continue to investigate ways to expand our dashboard dataset via continued stakeholder engagement to identify solutions and eliminate barriers to increase program participation. Our data also highlights the continued work required to successfully implement this program. Although patient participation was only 47% of all eligible patients, continued evolution of the program is ongoing and may permit capture of ideally all eligible patients in an efficient manner.
The overall architecture of our study is widely generalizable, employs commonly available software, and can likely be incorporated with multidisciplinary effort at a range of institutional and organizational levels. Our post-hoc analyses described herein demonstrate the utility of electronic dashboards in quickly identifying and presenting unique trends in selected data. Remarkable potential exists regarding the patient-derived perioperative goal tracking electronic dashboard. With further improvements, such dashboards may offer a seamless and insightful method to continuously present patient quality and satisfaction data in the surgical clinic and ultimately improve patient care.
Data availability statement
The datasets presented in this article are not readily available because of the nature of protected health information presented in this paper. Upon request and with approval of Privacy Officer and Information Security Officer at the Department of Veteran Affairs, the materials created in this work might be made available to interested researchers. Requests to access the datasets should be directed toc2hleW5lLm1hcnRpbkB2YS5nb3Y=.
Ethics statement
The studies involving humans were approved by Central Virginia VA Medical Center Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because of the quality improvement nature of our study.
Author contributions
SM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AC: Conceptualization, Data curation, Formal analysis, Investigation, Software, Validation, Visualization, Writing – review & editing. KJ: Conceptualization, Data curation, Formal analysis, Writing – review & editing. CA: Data curation, Formal analysis, Writing – review & editing. HB: Data curation, Formal analysis, Writing – review & editing. KH: Conceptualization, Data curation, Formal analysis, Project administration, Software, Writing – original draft, Writing – review & editing. KV: Conceptualization, Data curation, Formal analysis, Project administration, Software, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
Authors acknowledge Central Virginia VA Health Care System Clinical Analytics staff for their assistance in creating the visual dashboard. We thank RN Jessica Kaplan on initial development of health care factors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Scheer JK, Keefe M, Lafage V, Kelly MP, Bess S, Burton DC, et al. Importance of patient-reported individualized goals when assessing outcomes for adult spinal deformity (ASD): initial experience with a patient generated index (PGI). Spine J. (2017) 17(10):1397–405. doi: 10.1016/j.spinee.2017.04.013
2. Hartzler AL, Chaudhuri S, Fey BC, Flum DR, Lavallee D. Integrating patient-reported outcomes into spine surgical care through visual dashboards: lessons learned from human-centered design. EGEMS. (2015) 3(2):1133. doi: 10.13063/2327-9214.1133
3. Azad TD, Kalani M, Wolf T, Kearney A, Lee Y, Flannery L, et al. Building an electronic health record integrated quality of life outcomes registry for spine surgery. J Neurosurg Spine. (2016) 24(1):176–85. doi: 10.3171/2015.3.SPINE141127
4. Cronin RM, Conway D, Condon D, Jerome RN, Byrne DW, Harris PA. Patient and healthcare provider views on a patient-reported outcomes portal. J Am Med Inform Assoc. (2018) 25(11):1470–80. doi: 10.1093/jamia/ocy111
5. Patel K, Chim YL, Grant J, Wascher M, Nathanson A, Canfield S. Development and implementation of clinical outcome measures for automated collection within specialty pharmacy practice. J Manag Care Spec Pharm. (2020) 26(7):901–9. doi: 10.18553/jmcp.2020.26.7.901
6. Epstein RM, Street RL. The values and value of patient-centered care. Ann Fam Med. (2011) 9(2):100–3. doi: 10.1370/afm.1239
7. Strachna O, Cohen MA, Allison MM, Pfister DG, Lee NY, Wong RJ, et al. Case study of the integration of electronic patient-reported outcomes as standard of care in a head and neck oncology practice: obstacles and opportunities. Cancer. (2021) 127(3):359–71. doi: 10.1002/cncr.33272
8. Schwartz CE, Ayandeh A, Finkelstein JA. When patients and surgeons disagree about surgical outcome: investigating patient factors and chart note communication. Health Qual Life Outcomes. (2015) 13(1):161. doi: 10.1186/s12955-015-0343-0
9. Matthies N, Keshen S, Lewis S, Webster F, Perruccio AV, Rampersaud YR. An exploratory analysis of spine patients’ preoperative concerns and decision-making process. Spine. (2020) 45(15):1067–72. doi: 10.1097/BRS.0000000000003456
10. Mancuso CA, Duculan R, Cammisa FP, Sama AA, Hughes AP, Lebl DR, et al. Concordance between patients’ and surgeons’ expectations of lumbar surgery. Spine. (2021) 46(4):249–58. doi: 10.1097/BRS.0000000000003775
11. Turcotte J, Kelly M, Lynch K, Pipkin K, Patton C. Patient goal-directed care in an orthopaedic spine specialty clinic. J Am Acad Orthop Surg. (2021) 29(17):e880–7. doi: 10.5435/JAAOS-D-20-01105
12. Deme P, Perera A, Chilakapati S, Stutzman S, Singh R, Eldridge CM, et al. Patient and spine surgeon perceptions on shared decision-making in the treatment of older adults undergoing corrective surgery for adult spinal deformity. Spine. (2022) 47(10):730–6. doi: 10.1097/BRS.0000000000004257
13. Moehl K, Newman D, Perera S, Toto PE, Weiner DK. Validating goal attainment in veterans undergoing decompressive laminectomy: a preliminary study. Pain Med Malden Mass. (2021) 22(4):829–35. doi: 10.1093/pm/pnaa406
14. Rampersaud YR, Canizares M, Perruccio AV, Abraham E, Bailey CS, Christie SD, et al. Fulfillment of patient expectations after spine surgery is critical to patient satisfaction: a cohort study of spine surgery patients. Neurosurgery. (2022) 91(1):173–81. doi: 10.1227/neu.0000000000001981
Keywords: goals of care, lumbar surgery, patient-centered, veteran, spine, quality improvement
Citation: Martin S, Caras AJ, Johnson K, Allen CS, Bradbury HB, Holloway KL and Verma K (2025) Design and implementation of a patient-derived surgical goal setting program for elective lumbar spine surgery. Front. Musculoskelet. Disord. 3:1548472. doi: 10.3389/fmscd.2025.1548472
Received: 19 December 2024; Accepted: 20 June 2025;
Published: 10 July 2025.
Edited by:
Maryse Fortin, Concordia University, CanadaReviewed by:
Yuehui Zhang, Shanghai Jiao Tong University, ChinaQuan Do, Mayo Clinic, United States
Shangjv Gao, Hebei General Hospital, China
Paul Dougherty, Syracuse VA Medical Center, United States
Copyright: © 2025 Martin, Caras, Johnson, Allen, Bradbury, Holloway and Verma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sheyne Martin, U2hleW5lLm1hcnRpbkB2YS5nb3Y=
†These authors have contributed equally to this work and share first authorship
 Sheyne Martin
Sheyne Martin Andrew J. Caras
Andrew J. Caras Kristen Johnson
Kristen Johnson Crystal S. Allen
Crystal S. Allen Heather B. Bradbury
Heather B. Bradbury Kathryn L. Holloway
Kathryn L. Holloway Ketan Verma
Ketan Verma