- 1Department of Orthopaedic Surgery, University of Illinois at Chicago, Chicago, IL, United States
- 2Department of Orthopaedic Surgery, Northshore University Health System, An Affiliate of the University of Chicago Pritzker School of Medicine, Skokie, IL, United States
Introduction: This paper examines the transformative impact of technology on sports medicine, highlighting its current applications and prospects. As advancements continue to emerge, the integration of innovative tools aims to enhance athlete care and improve performance.
Hypothesis and aim: The study's primary objective is to evaluate the effectiveness of diagnostic imaging, wearable devices, motion capture systems, and data analytics in the prevention, diagnosis, and rehabilitation of athletic injuries. Furthermore, it aims to highlight the potential of current sports data collection methods to advance preventive medicine and to leverage virtual simulations to assess injuries and optimize rehabilitation practices.
Methodology: A comprehensive analysis of recent technological advancements in monitoring and data collection is conducted, focusing on their role in preventing injuries related to overuse and fatigue. By leveraging real-time data, these technologies enhance athlete performance and safety.
Conclusion: By highlighting these technological advancements, this study articulates a visionary perspective on the future of sports medicine. It demonstrates how the effective integration of athlete data can elevate treatment protocols, refine prevention strategies, and ultimately enhance athletes' outcomes. The paper also discusses key innovations across biomechanics, wearable technology, advanced diagnostic imaging, rehabilitation technologies, machine learning, and immersive training experiences, underscoring the critical intersection of engineering and sports medicine.
Introduction
Sports injuries pose a significant financial challenge to our healthcare system, and addressing this issue requires a collaborative effort. Youth sports injuries, in particular, have profoundly impacted individuals, families, and the broader healthcare system, resulting in costs that exceed billions of dollars each year. In 2019, the total economic toll of injuries across the United States reached a staggering $4.2 trillion, a figure that captures not only the immediate costs but also the long-term consequences. Of this amount, approximately $327 billion was explicitly allocated to medical care, as highlighted by the Centers for Disease Control and Prevention (CDC). This statistic highlights the substantial resources required to treat injuries and facilitate recovery. A thorough examination by the National Institutes of Health (NIH) sheds light on the financial implications of sport specialization-related injuries, estimating that the United States spends between $0.8 billion and $5.2 billion annually on this pressing issue. This range illustrates the variability in costs depending on the specific sports and types of injuries incurred, emphasizing the need for targeted prevention measures and the importance of collaboration in implementing these measures (1–12).
The field of sports medicine stands at the forefront of significantly impacting athletic performance and improving health through cutting-edge innovation in prevention and treatment. With an increasing emphasis on understanding the mechanisms behind injuries and enhancing rehabilitation, this dynamic area of research is transforming how we approach athlete care (13–16).
Engineering innovation has played a pivotal role in sports analytics, transforming the sports landscape for both amateurs and professionals, as well as institutions and healthcare. To explore the engineering impact on medicine, we examine some of the fundamentals, which include: (a) Biomechanics and Motion Analysis: Understanding the mechanics of human movement plays a crucial role in sports medicine. Innovations in motion capture technology, including high-speed cameras and sensor systems, enable detailed analysis of an athlete's biomechanics. This helps identify improper movement patterns that can lead to injuries and aids in developing effective rehabilitation protocols. (b) Wearable Technology: The integration of wearable devices such as smartwatches, heart rate monitors, and GPS tracking systems has transformed athlete monitoring. These devices collect real-time data on health metrics, performance, and fatigue levels, allowing coaches and medical staff to tailor training regimens and closely monitor athletes’ physical conditions. (c) Diagnostic Imaging Advances: Innovations in imaging techniques, including MRI, CT scans, and ultrasound, enable precise diagnosis and evaluation of sports injuries. Enhanced imaging technologies contribute to better decision-making regarding treatment options and to a better understanding of the extent of injuries. (d) Rehabilitation Technology: Engineering innovations have led to the development of advanced rehabilitation tools, such as robotic exoskeletons, electrical stimulation devices, and virtual reality systems. These technologies facilitate targeted rehabilitation exercises, improve mobility, and accelerate recovery by providing real-time feedback and motivation throughout the process. (e) Data Analytics and Machine Learning: The application of data analytics and machine learning techniques in sports medicine enables the extraction of valuable insights from large datasets collected through various technologies. This analysis can help identify injury trends, optimize training programs, and improve overall athlete performance and safety. (f) Augmented Reality (AR) and Virtual Reality (VR): AR and VR technologies are emerging tools in sports medicine that enhance training and rehabilitation. They enable immersive experiences that simulate real-life scenarios for skill development, providing visual performance feedback that benefits both mental and physical training. (g) Customized Orthotics and Prosthetics: Innovations in materials science and 3D printing technology have revolutionized the design of custom orthotics and prosthetics. These personalized devices enhance comfort, stability, and overall performance for athletes recovering from injuries or those with limb differences. (h) Smart Surfaces and Equipment: The Development of bright training surfaces and equipment that incorporate sensors to monitor performance metrics, environmental conditions, and safety risks can significantly improve training quality and injury prevention strategies (16–19) By focusing on these fundamentals, engineers and researchers in sports medicine can continue to innovate, ensuring that athletes receive the most effective care and support possible.
Additional impactful devices for data collection and athlete monitoring include smart gumshields and exoskeletons. Smart gumshields are engineered to monitor head impacts, helping mitigate concussion risk. In parallel, exoskeletons play a pivotal role in enhancing rehabilitation outcomes by improving both strength and endurance. While these advancements are encouraging, the reality remains that injuries can still occur, highlighting the need for efficient recovery methods. This need is particularly pressing in elite sports scenarios, such as the Olympics, where athletes face tight turnaround times for recovery and performance (20, 21).
Recent innovations in injury prevention and recovery present valuable opportunities for further progress, and include:
1. Cryotherapy Chambers: By employing extreme cold, these chambers effectively speed up muscle recovery and are gaining popularity among elite athletes, including those on Team USA.
2. Hyperbaric Chambers: These chambers promote rapid tissue healing by increasing oxygen levels in the blood, with notable endorsements from top athletes such as Simone Biles and Usain Bolt.
3. Electrotherapy Devices: These technologies stimulate muscle activity and enhance blood flow, providing targeted pain relief that is essential for optimizing athletic performance.
These advancements not only underscore the beneficial fusion of medicine and technology in sports but also add improved safety and performance outcomes for athletes.
This paper aims to investigate the current applications of technology in sports medicine. It will also outline a forward-looking perspective on how integrating video imaging, wearable devices, and sensors can contribute to the development of a comprehensive athlete database. This database has the potential to drive significant advancements in both the prevention and treatment of sports-related injuries.
Methodology and technological highlights
For years, technological advancements have been a key driver of improvements in sports medicine. Diagnostic imaging, including x-rays, magnetic resonance imaging (MRI), computed tomography (CT), and ultrasound, enables physicians to accurately diagnose and evaluate sports-related injuries, such as fractures, ligament tears, muscle strains, and joint problems. Wearable devices such as fitness trackers, smartwatches, and heart rate monitors provide real-time monitoring of vital signs, activity levels, sleep patterns, and performance metrics. Figure 1 shows a soccer player wearing multiple sensing elements and being monitored by several cameras. Motion capture and analysis systems, including high-speed cameras, inertial measurement units (IMUs), and force plates, aid in assessing an athlete's movement patterns, biomechanics, and joint kinetics (22, 23).
While numerous technological advancements have been made in the field over the years, a growing interest in the use of augmented reality (AR) and virtual reality (VR) in sports medicine has emerged. AR and VR can enhance rehabilitation and injury recovery by creating immersive environments that help athletes regain strength, balance, and coordination while performing targeted exercises (24, 25). They can capture an athlete's movements and provide real-time visual feedback, allowing for analysis and correction of movements (see Figure 1). Additionally, VR can create realistic sports scenarios and training environments, allowing athletes to practice their skills in a controlled setting (see Figure 2). Both AR and VR can simulate high-pressure situations and enhance mental skills, such as focus, concentration, and visualization, which are critical for sports performance (26).

Figure 1. This soccer player is using multiple technological devices to improve his game. He wears a VR helmet for simulating game scenarios, a tri-axis accelerometer for biomechanical analysis, a wrist tracker for heart rate and activity tracking, and an ankle accelerometer to measure running mechanics. Cameras are also placed around the training grounds to detect injury risks and monitor player movements.

Figure 2. This image depicts a player using virtual reality (VR) to simulate a football game for training purposes. The player can experience real-match scenarios in an immersive, controlled environment, practicing tactical awareness, decision-making, and positioning against virtual opponents.
AR and VR are increasingly adopted in the healthcare industry as advanced tools to enhance medical education and deliver a cutting-edge learning experience. In the ever-evolving field of healthcare, medical professionals engage in lifelong learning. As medical technology advances rapidly, it has become essential for these professionals to stay abreast of the latest innovations. Technology's role in enhancing medical professionals' learning experience is empowering and motivating. Neglecting to bridge this widening knowledge gap can hinder their ability to deliver high-quality patient care.
Technology's role in injury prevention
Most sports injuries result from overuse and inadequate recovery and rest. Overuse can lead to the wear and tear of muscles, tendons, and joints. Often, athletes and their coaches may be unaware that the probability of an injury occurring is rising because there are no effective methods to measure fatigue. However, teams across various sports are starting to integrate technologies such as smartwatches, wireless integrated circuits, and motion-capture cameras to track the vitals of their athletes, along with using a gyroscope, accelerometer, and blood-oxygen sensor to capture additional parameters (22). This data can be used to monitor an athlete's biomechanical and metabolic status during games or practices (see Figure 3). They can provide potential insights into when an athlete suffers from overuse or fatigue that could lead to an injury (24, 27). Rossi et al. explain that their team collects data from soccer players using a “tight top under their jerseys outfitted with GPS, an accelerometer, a gyroscope, and a digital compass”. (28). Technologies like these enable coaches, trainers, and athletes to more accurately forecast potential injuries (29).

Figure 3. This image illustrates how GPS technology, worn by athletes, enables coaches to track position, speed, distance, and movement patterns in real time during training and matches. This data provides insights into players’ performance, fitness levels, and workload, aiding in the development of personalized training plans and injury prevention.
This technology has expanded its application beyond soccer and is now used in other sports, such as football and baseball. For example, professional football teams increasingly use force plates to measure ground reaction forces and predict injury risk. Research using the Sparta Science force plate has shown a notable decline in musculoskeletal health following the COVID-19 lockdown measures (30). Applying markerless motion capture is an additional AI-driven approach for analyzing sports performance and evaluating injury risk, particularly for baseball pitchers. This technology has demonstrated its efficacy in assessing injury risk for athletes engaged in repetitive overhead throwing (23, 31). Nonetheless, ongoing discussions persist regarding how these technologies can extrapolate injury risk data to other athlete populations (32, 33).
Injury protection in sports requires data collection to be wirelessly filtered, structured, and analyzed to ensure its benefits are realized. The data needs to be processed using data mining, AI, and machine learning algorithms, with feedback from clinical professionals, to accurately assess athletes' health status and provide intelligent recommendations for personalized, well-informed assessment and training methods. It's essential to create a database of models that allows assessment to be performed relatively quickly.
A multitude of factors can significantly influence the effectiveness of a predictive model. At the core of its efficacy lie the quality and quantity of the data used for both training and evaluation. When the data is of poor quality—due to errors, inconsistencies, or biases—or the dataset is insufficient in volume, the result can be a pronounced deviation in the model's accuracy when predicting risks. Moreover, the selection of appropriate features, coupled with meticulous preprocessing and feature engineering, plays a pivotal role in shaping the model's success (see Figure 4). Inadequate or misguided feature selection, as well as subpar processing methods, can severely hamper the model's performance, rendering it less effective in drawing accurate insights.
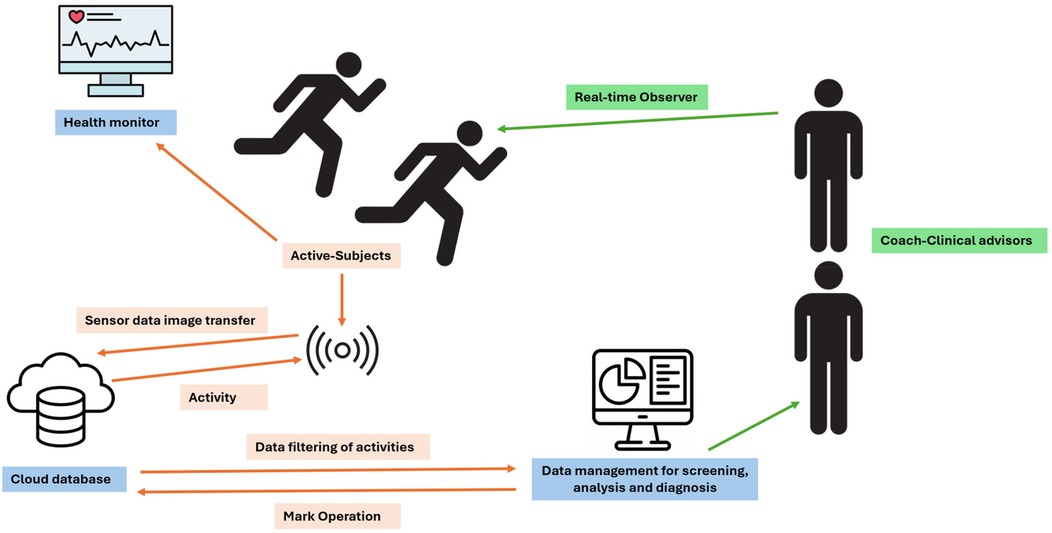
Figure 4. The workflow of a sports-teaching data-collection system that uses wearable devices involves participants wearing devices that track movement data, including posture, exercise duration, frequency, and heart rate. This data is transmitted wirelessly to a central control system for storage and analysis. The monitoring system can provide real-time health feedback. The collected data can be used to provide personalized guidance, help prevent injuries, and improve sports skills and overall health.
In addition, the model's architecture and parameter configurations are crucial determinants of its learning capacity and expressiveness. Opting for a model architecture and fine-tuning parameter settings that align with the task's intricacies and the data's inherent characteristics can substantially enhance the model's overall effectiveness (see Figure 4).
Despite significant advancements in technology and data collection for athletes over the past decade, systematic methods and platforms remain inadequate for fully leveraging that data. However, the importance of personalized treatment plans in sports medicine cannot be overstated. Often, extensive data is collected and stored without being utilized to its maximum potential. This presents an opportunity to apply data science and analytics to harness the collected data and unlock its value effectively. Sensory technology, such as pressure-sensitive insoles that capture foot pressure distribution and gait analysis data, can provide insights into biomechanical abnormalities, identify potential areas of excessive stress or imbalance, and inform decisions regarding injury prevention, footwear selection, and orthotic interventions (34, 35).
Real-time video monitoring of a gymnast's routine during practice can be used to evaluate technique, body positioning, and the risk of overuse injuries (see Figure 5). Reviewing slow-motion videos of a runner's gait can help identify faulty mechanics, such as excessive pronation or asymmetrical movements, which can place undue stress on specific joints or muscles, potentially leading to repetitive strain injuries (36). These technologies facilitate comprehensive data collection, empowering doctors to make evidence-based decisions, develop personalized treatment plans, and enhance overall care in sports medicine.
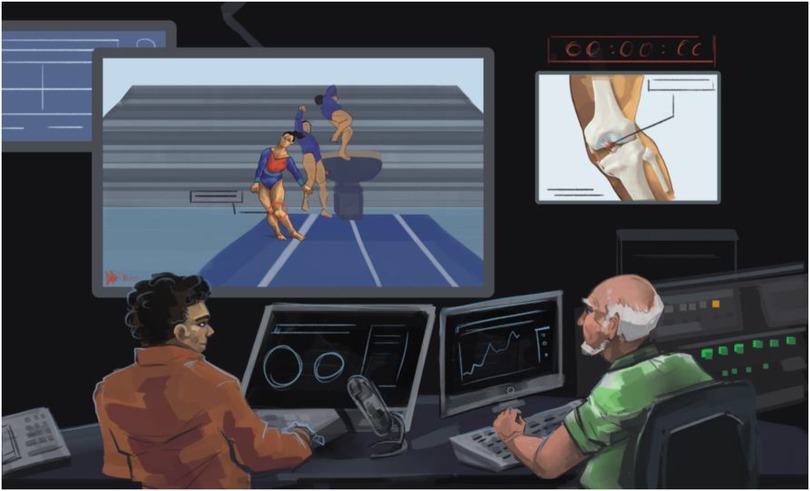
Figure 5. This image illustrates how real-time video monitoring of a gymnast's routine enables coaches to assess technique, body positioning, and potential injuries during practice. Reviewing slow-motion videos of their routines can help identify faulty mechanics, such as excessive pronation or asymmetrical movements, which may lead to repetitive strain injuries by placing undue stress on certain joints and muscles.
Technology's role in surgical planning
Engineering and technology can also potentially improve the experiences and outcomes in the operating room. Orthopedic departments worldwide are implementing Mixed Reality technology and 3D printing to enhance patient outcomes. Verhey et al. describe how virtual reality (VR) can provide residents and fellows with supplemental training in procedures (37, 38). This can help address various concerns, such as closing the gap in experience gained during residency, which is highly dependent on the geographic location of training (i.e., urban hospitals vs. rural clinics) (39). Additionally, it can help mitigate ethical concerns among trainees who gain initial experience outside the operating room, thereby reducing patient risk. As for AR, it has the potential to go one step further. AR can be combined with images and planning to provide individualized patient anatomy and incision locations (25). It also has the added benefit of not requiring ionizing radiation on the patient. To take it even further, there is potential to use Mixed Reality (MR) to provide a more accurate real-world experience through holographic overlays (see Figure 6). It also enables video conferencing for collaboration with colleagues or for offering educational experiences for trainees (39). These technologies are still in development, and teams are beginning to incorporate these practices. As the field of orthopedics continues to advance, it is clear that the integration of technology and engineering will only grow. This integration enables better patient outcomes, reduced healthcare costs, and enhanced planning and educational opportunities for trainees (40).

Figure 6. This image shows surgeons immersed in a 3D, high-fidelity representation of the patient's specific anatomy, enabling them to understand complex structures and relationships better. This advanced visualization enables precise planning, reduces risks, and enhances surgical precision, improving patient outcomes and increasing surgical success.
Technology's role in rehabilitation
When an athlete undergoes rehabilitation following an injury, coaches and trainers must clearly understand how to reintegrate them into practice without increasing the risk of reinjury. Load management has emerged as a popular approach for monitoring an athlete's performance during rehabilitation (41, 42). This method combines objective measurements, such as external workloads (e.g., shots taken, pitches thrown), with subjective factors, such as the athlete's perceived effort level (rate of perceived exertion - RPE). It helps determine the appropriate time for the athlete to return to regular play. While a systematic review has found moderate evidence linking an athlete's training load during rehabilitation to injury, further enhancement of this load management tool requires integrating additional kinematic data (43). This can be accomplished by leveraging wearable technologies, such as accelerometers or motion-tracking devices. Electromagnetic sensors are already being utilized to monitor the kinematics of upper and lower limbs during post-surgery rehabilitation, offering the potential for quantitative evaluation of reinjury risk (44).
Furthermore, there have been suggestions of utilizing algorithms to predict an athlete's risk of injury by analyzing visual data obtained from complex sports movements (45). This represents a more advanced approach. While load management is already a powerful tool, its accuracy and precision can be further improved by analyzing kinematic data from motion-tracking technology.
A vision for the future: opportunities for data integration
Virtual biomechanics
Understanding the biomechanics of different joints is a key component of orthopedic research. In the past, it has been difficult to accurately assess all the forces acting on joints and the surrounding ligaments. Traditionally, cadaveric studies have been used to try to illustrate forces experienced at a joint during different moments of stress (38). More recently, finite element analysis (FEA) has been used to develop a joint model from CT images converted into CAD files. Using FEA, biomechanical experiments have been performed to determine load distribution and joint deformation under specific conditions (40, 46).
A potential pitfall of these experiments is that they do not account for the personalized nature of each athlete, failing to consider the dynamics and contributions of the musculoskeletal structures around the joints and along the limbs. First, many athletes have had previous injuries so that they may be compensating differently under joint stress. Additionally, although different loading conditions can be simulated in the lab using finite element analysis (FEA), each athlete may load their joints differently during movements specific to their sport, and prior injuries and potential surgeries may modify these movements. Several investigators are pursuing a combination of FEA and Multibody Dynamics, which could pave the way for better modeling and simulation of specific exercises.
As demonstrated earlier, a wealth of kinematic data is available for each athlete, thanks to wearable devices and markerless motion capture technologies. Looking ahead, it is possible to collect and seamlessly integrate this data into MBDS and finite element analysis (FEA) models by utilizing patient-specific scans. This data integration can pave the way for using AI in biomechanics experiments explicitly tailored for athletes by replicating an athlete's movements and the resulting joint stresses (see Figure 7). Furthermore, the data can be stratified by sport, position, and prior injuries, enabling more targeted analysis and insights (47).
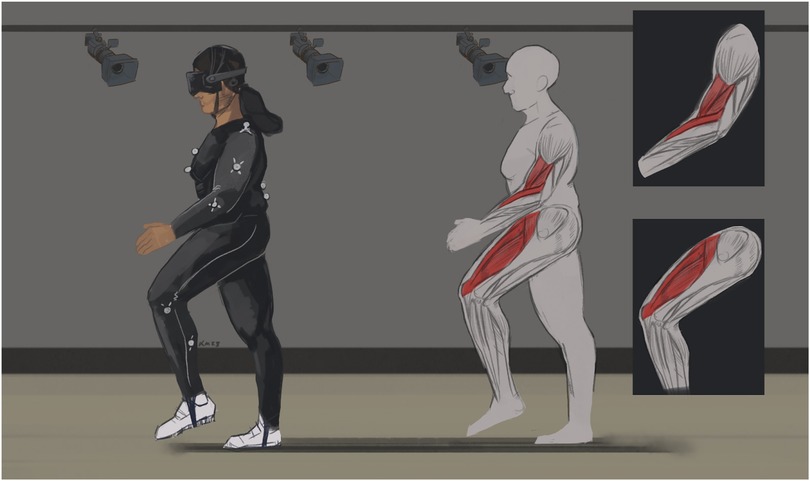
Figure 7. This image exemplifies the synergy between virtual reality (VR) and markerless motion capture in simulating an athlete's distinctive movements and joint stresses. The combination of these technologies enables personalized biomechanics experiments, with the potential to optimize performance and tailor injury-prevention strategies to each athlete's requirements using AI.
Surgery and surgical planning
A similar theme regarding a lack of personalization is found in today's surgical planning. Surgeons typically evaluate patients after an injury, at which point they can suggest surgical intervention. They can employ previously mentioned tools, such as 3D CT scans, to assess the injury and VR to simulate the procedure for a particular patient (48, 49). Despite these advancements, there is currently no efficient method to integrate all the athlete-specific data gathered before and during the injury. This kinematic data is potentially valuable for surgical planning, execution, and future research.
For instance, consider a football player who recently suffered an ACL tear. This player has existing kinematic data capturing their movements during practice and on-field activities, as well as real-time data recorded at the time of injury. If the surgeon could access this data and utilize suitable software to visualize the player's movements, it would provide a more comprehensive understanding of the injury mechanism. Moreover, combining CT images of the player's knee taken before and after the injury with 3D printing technology enables the creation of an almost perfect replica of their ACL. This amalgamation of kinematic and CT image data, accumulated across numerous athlete injuries, holds the potential to develop AI systems that assist with surgical planning and treatment. These systems could identify the most effective approach to ACL repair, leading to a more robust recovery for the athlete.
Rehabilitation and AI
An ACL tear, like the one mentioned in the football player previously, is a devastating injury that typically results in athletes being in recovery for a whole season. Additionally, even after recovery, the athlete often cannot return to their previous level of 100% (27). As the athlete begins the long road to recovery after surgery, trainers, coaches, and medical personnel closely monitor their progress to determine when they are ready to return to play. As discussed previously, return to play is often based on subjective workload measures that are prone to error and may increase the risk of reinjury. Consider a future in which real-time kinematic data from an athlete guides their rehabilitation efforts through gradual increases in workload (26). Again, data on recovery times for many athletes after an ACL tear is used to build a robust AI system that can provide workload recommendations. Past statistics will be used to evaluate when an athlete is at risk of reinjury, providing an objective measure for approval of return to play (27, 50).
The sports medicine industry is experiencing a notable transition towards digital health technologies, driven by increasing demand for real-time, continuous health monitoring and injury diagnostics. The rising incidence of injuries among young athletes, especially in women—such as ACL and ligament ruptures—along with the physical demands of sports and the desire to excel, has amplified the need for remote and ongoing health monitoring.
The emergence of AI-based wearable sensors has enabled the collection, analysis, and transmission of real-time health data to healthcare providers, facilitating informed decision-making and improved patient care. Wearable sensors have become integral to sports medicine, providing clinicians with invaluable data to enhance athlete performance and prevent injuries. By leveraging machine learning (ML) and artificial intelligence (AI) algorithms, these devices analyze key metrics—such as heart rate, movement patterns, and biomechanical data—to provide actionable insights tailored to athletes' physical demands (13, 17–19, 51–60).
In sports medicine, early detection of potential injuries is crucial. Wearable technology can detect subtle changes in biomechanics or physiological responses that may indicate overtraining or the onset of injury, enabling timely interventions. For example, an athlete's fatigue levels or changes in gait can be monitored, prompting a clinician or a coach to adjust training regimens or rehabilitation protocols effectively. Moreover, these sensors enable personalized training programs tailored to each athlete's unique needs, optimizing performance while minimizing injury risk. By bridging the gap between data collection and clinical application, wearable sensors enable sports medicine practitioners to refine recovery protocols and enhance overall athlete health. AI-driven wearable devices champion preventive healthcare, ensuring we no longer wait for injury to strike but instead play an active role in injury prevention through reminders and feedback, thereby fostering a future where timely interventions become the norm rather than the exception.
Wearable health technology has the potential to offer significant benefits, but it also faces several challenges. A major issue is the accuracy of the data these devices collect. Current biosensors are still in development and cannot continuously monitor biological biomarkers effectively. Improvements in sensitivity, selectivity, and accuracy are needed to prevent false alarms and missed health detections, making validation against gold-standard methods crucial. Additionally, privacy and security concerns arise with the collection and transmission of sensitive health data, prompting healthcare providers and manufacturers to implement stringent protections to safeguard patient information (13, 17–19, 51–60).
Implants, 3D printing, and FDA approval
The integration of implants in sports medicine has enhanced treatment options and improved outcomes for athletes with musculoskeletal injuries. With advancements in 3D printing technology, custom-designed implants (see Figure 8) can now be created to match each individual's unique anatomy, resulting in a better fit, improved functionality, and enhanced post-surgical recovery (26). Moreover, the ability to use 3D printing to produce patient-specific surgical guides and instruments has streamlined surgical procedures, increasing their precision and efficiency. However, to ensure the safety and efficacy of these innovations, FDA approval is crucial to their development and commercialization. The journey to FDA approval for implants requires manufacturers to navigate complex regulatory pathways, adhere to quality standards, and provide extensive evidence of the implant's safety and effectiveness. It involves collaboration among medical professionals, engineers, and regulatory experts to meet the rigorous demands set forth by the FDA (61). As a result, athletes and sports medicine practitioners can have confidence in the effectiveness and reliability of these advancements, enabling them to make informed decisions about treatment options and to optimize overall care in sports medicine.

Figure 8. Three-dimensional (3D) printing. Building 3D objects using CAD based on CT and MRI imaging of patients. Implants are then designed and printed to address patient-specific pathologies and ensure a proper fit. Different 3D printing machines are used for polymers and porous metals.
Discussion
The application of technology in sports medicine lags behind advancements in non-medical fields, particularly in the development of artificial intelligence (AI) systems. While progress has been made in data collection through wearable devices, cameras, and other sources, there is still room for improvement. Surgeons have benefited from technological tools, such as 3D imaging and virtual reality (VR), for enhanced surgical planning and decision-making. Furthermore, biomechanics research enables the use of finite element analysis (FEA) with 3D CT scan renderings of athletes. However, there is still a lack of seamless integration of athlete kinematic data, hindering the development of more robust research and surgical planning tools. In the future, AI tools could play a significant role in decision-making for surgery planning and providing precise recommendations for athlete rehabilitation progress. Moreover, there is potential to further individualize the entire process, allowing surgeons and researchers to comprehend the cause of an injury and customize rehabilitation programs by comparing pre- and post-injury kinematic data. Once the connection between data collection and utilization is established, the possibilities for advancing the field of sports medicine become limitless.
Some of the limitations of this paper revolve around the question, “What specific advancements in wearable technology have shown the most promise for preventing sports injuries?” This question is highly relevant to sports medicine. The following points provide further highlights on where we are and what needs to be explored further:
1. Further exploration of advancements in wearable technology is needed, as it is directly linked to injury prevention, making it easier to understand what information is being sought.
2. Manufacturing and sensing technologies drive advancements in wearable technology, aligning well with current trends in sports medicine. Given the rapid development of fitness trackers, bright clothing, and biomechanical sensors, why is this information lacking in sports, and how will this database be shared in the future? To address this critical area of growth in the field, regulations must be in place, and universities, athletics, and industry sponsors must collaborate to achieve a common goal.
3. What specific metrics or features of wearable devices, such as heart rate monitoring, movement analysis, recovery tracking, alarms, frequency and repeatability, performance, and overall health conditions, will be needed? This would deepen the inquiry and yield more nuanced insights into the most effective injury-prevention features.
4. Contextual Considerations may be beneficial to consider how the effectiveness of these advancements varies by type of sport or level of athlete (e.g., amateur vs. professional). This could add depth and applicability to the answers.
5. Encouraging exploration of how wearable technology interacts with training regimens, coaching strategies, and athlete education on injury prevention could lead to a more comprehensive understanding of its impact.
Integrating athlete data across different sports and organizations presents significant challenges but also offers opportunities for innovation in sports medicine. Standardization begins with the establishment of standard metrics for athlete performance and health. This can be achieved by developing universal guidelines that define essential data points — such as heart rate, movement patterns, and fatigue levels — that every organization can adopt regardless of the sport. By leveraging collaborations among governing bodies, sports organizations, and technology developers, a foundational framework can emerge that dictates how data is collected, stored, and shared.
For example, professional bodies in various sports might agree on a set of universally understood performance and injury metrics, creating a common language for data analysis. Such collaboration would facilitate cross-sport comparisons and enable the sharing of insights, leading to enhanced training techniques and improved injury prevention strategies. Additionally, implementing standardized software platforms that integrate data from various wearable technologies would streamline this process, enabling real-time monitoring and analysis.
However, despite these possibilities, several limitations and challenges should be acknowledged, particularly in incorporating augmented reality (AR) and virtual reality (VR) technologies into training and rehabilitation practices. One substantial barrier is the variability in technology adoption across different organizations. While some clubs may have the resources to implement advanced AR and VR systems, others may struggle to afford them, particularly those in lower divisions or minor sports. This disparity can lead to unequal access to innovative training and rehabilitation tools, creating a gap in performance and recovery capabilities.
Moreover, technical challenges exist in effectively integrating AR and VR into existing training regimens. Athletes must be trained to use these technologies and to adapt to new learning and skill-acquisition methods. The effectiveness of simulations can vary depending on an athlete's ability to translate virtual experiences into real-world scenarios, underscoring the need for a thoughtful approach to training methodologies. Additionally, there may be resistance to change among coaches and athletes accustomed to traditional methods and concerned about the reliability and accuracy of data generated by these technologies.
Lastly, the potential for information overload also presents a challenge. As more data is collected, distilling it into actionable insights becomes increasingly complex. Coaches and trainers must be adept at interpreting this information and communicating it effectively to athletes, motivating and educating without overwhelming them.
While establishing standardized data integration across various sports and organizations can enhance athlete care and performance insights, successfully implementing AR and VR technologies in training and rehabilitation requires overcoming significant hurdles in accessibility, adaptability, and data management. Addressing these challenges will be essential for advancing the role of technology in sports medicine.
Conclusion
In conclusion, integrating advanced technologies in sports medicine can potentially transform the landscape of injury prevention, diagnosis, and rehabilitation. Current applications, such as diagnostic imaging, wearable devices, and motion capture systems, have already enhanced our understanding of athletic performance and injury mechanisms, thereby fostering improved treatment strategies. The promising incorporation of augmented reality (AR) and virtual reality (VR) further paves the way for innovative rehabilitation techniques, allowing athletes to engage in immersive training environments that hone their physical and mental skills.
The continuous evolution of data collection and analysis methods will enable a more nuanced understanding of athletes’ needs, promoting personalized prevention and treatment plans. By harnessing technology to monitor fatigue and overuse, we can reduce the incidence of injuries and enhance athlete longevity. As we advance towards a future where athlete data is seamlessly integrated into sports medicine practices, the potential for proactive and informed approaches to athlete care becomes increasingly viable, ultimately optimizing performance and safeguarding athletes' health in an ever-demanding sporting environment.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
FA: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. IP: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
Some of the Pictures were made by Keaton Mullin, conceptualized and drafted by Dr. Farid Amirouche.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bell DR, DiStefano L, Pandya NK, McGuine TA. The public health consequences of sport specialization. J Athl Train. (2019) 54(10):1013–20. doi: 10.4085/1062-6050-521-18
2. Yang J, Phillips G, Xiang H, Allareddy V, Heiden E, Peek-Asa C. Hospitalisations for sport-related concussions in US children aged 5 to 18 years during 2000–2004. Br J Sports Med. (2008) 42(8):664–9. doi: 10.1136/bjsm.2007.040923
3. Nalliah RP, Anderson IM, Lee MK, Rampa S, Allareddy V, Allareddy V. Epidemiology of hospital-based emergency department visits due to sports injuries. Pediatr Emerg Care. (2014) 30(8):511–5. doi: 10.1097/PEC.0000000000000180
4. Knowles SB, Marshall SW, Miller T, Spicer R, Bowling JM, Loomis D, et al. Cost of injuries from a prospective cohort study of North Carolina high school athletes. Inj Prev. (2007) 13(6):416–21. doi: 10.1136/ip.2006.014720
5. Injury costs for high school athletes. US Consumer Product Safety Commission Web site. Available online at: https://cpsc.gov/research–statistics/neiss-injury-data (Accessed April 1, 2017).
6. Bell DR, Lang PJ, Valovich McLeod TC, McCaffrey KA, Zaslow TL, McKay D. Sport specialization is associated with a history of injuries in youth soccer athletes. Athletic Train Sports Health Care. (2018) 10(6):241–6. doi: 10.3928/19425864-20180813-01
7. Roos KG, Marshall SW. Definition and usage of the term “overuse injury” in the US high school and collegiate sport epidemiology literature: a systematic review. Sports Med. (2014) 44(3):405–21. doi: 10.1007/s40279-013-0124-z
8. Soboroff SH, Pappius EM, Komaroff AL. Benefits, risks, and costs of alternative approaches to the evaluation and treatment of severe ankle sprain. Clin Orthop Relat Res. (1984) 183:160–8. doi: 10.1097/00003086-198403000-00026
9. Mather RC, Koenig L, Kocher MS, Dall TM, Gallo P, Scott DJ, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg. (2013) 95(19):1751–9. doi: 10.2106/JBJS.L.01705
10. Gregory. How kids’ sports became a $15 billion industry. Time Magazine Web site. (2017). Available online at: http://time.com/magazine/us/4913681/september-4th-2017-vol-190-no-9-u-s/2017 (Accessed September 14, 2018).
11. Investor survey: parent perspectives on the cost of competitive youth sports. TD Ameritrade Web site. Available online at: https://s1.q4cdn.com/959385532/files/doc_downloads/research/Sports-Parents-Survey-Report_2016.pdf.2016 (Accessed July 27, 2018).
12. Turnbull MR, Gallo TF, Carter HE, Drew M, Toohey LA, Waddington G. Estimating the cost of sports injuries: a scoping review. J Sci Med Sport. (2024) 27(5):307–13. doi: 10.1016/j.jsams.2024.03.001
13. Shajari S, Kuruvinashetti K, Komeili A, Sundararaj U. The emergence of AI-based wearable sensors for digital health technology: a review. Sensors (Basel). (2023) 23(23):9498. doi: 10.3390/s23239498
14. Briganti G, Le Moine O. Artificial intelligence in medicine: today and tomorrow. Front Med. (2020;7:27. doi: 10.3389/fmed.2020.00027
15. Harrer S, Shah P, Antony B, Hu J. Artificial intelligence for clinical trial design. Trends Pharmacol Sci. (2019) 40(8):577–91. doi: 10.1016/j.tips.2019.05.005
16. Phatak AA, Wieland FG, Vempala K, Volkmar F, Memmert D. Artificial intelligence-based body sensor network framework—narrative review: proposing an end-to-end framework using wearable sensors, real-time location systems, and artificial intelligence/machine learning algorithms for data collection, data mining, and knowledge discovery in sports and healthcare. Sports Med Open. (2021) 7(1):79. doi: 10.1186/s40798-021-00372-0
17. Preatoni E, Bergamini E, Fantozzi S, Giraud LI, Orejel Bustos AS, Vannozzi G, et al. The use of wearable sensors for preventing, assessing, and informing recovery from sport-related musculoskeletal injuries: a systematic scoping review. Sensors. (2022) 22(9):3225. doi: 10.3390/s22093225
18. Meena JS, Choi SB, Jung SB, Kim JW. Electronic textiles: new age of wearable technology for healthcare and fitness solutions. Materials Today Bio. (2023) 19:100565. doi: 10.1016/j.mtbio.2023.100565
19. Abhinav V, Basu P, Verma SS, Verma J, Das A, Kumari S, et al. Advancements in wearable and implantable BioMEMS devices: transforming healthcare through technology. Micromachines (Basel). (2025) 16(5):522. doi: 10.3390/mi16050522
20. Drew MK, Raysmith BP, Charlton PC. Injuries impair the chance of successful performance by sportspeople: a systematic review. Br J Sports Med. (2017) 51(16):1209–14. doi: 10.1136/bjsports-2016-096731
21. Walia B, Boudreaux CJ. The cost of players’ injuries to professional sports leagues and other sports organizations. MF. (2021) 47(6):779–88. doi: 10.1108/MF-06-2020-0301
22. Li RT, Kling SR, Salata MJ, Cupp SA, Sheehan J, Voos JE. Wearable performance devices in sports medicine. Sports Health. (2016) 8(1):74–8. doi: 10.1177/1941738115616917
23. Vellios EE, Pinnamaneni S, Camp CL, Dines JS. Technology used in the prevention and treatment of shoulder and elbow injuries in the overhead athlete. Curr Rev Musculoskelet Med. (2020) 13(4):472–8. doi: 10.1007/s12178-020-09645-9
24. Soltani P, Morice AHP. Augmented reality tools for sports education and training. Comput Educ. (2020) 155:103923. doi: 10.1016/j.compedu.2020.103923
25. Azuma R, Baillot Y, Behringer R, Feiner S, Julier S, MacIntyre B. Recent advances in augmented reality. IEEE Comput Grap Appl. (2001) 21(6):34–47. doi: 10.1109/38.963459
26. Negrillo-Cárdenas J, Jiménez-Pérez JR, Feito FR. The role of virtual and augmented reality in orthopedic trauma surgery: from diagnosis to rehabilitation. Comput Methods Programs Biomed. (2020) 191:105407. doi: 10.1016/j.cmpb.2020.105407
27. Asadzadeh A, Samad-Soltani T, Salahzadeh Z, Rezaei-Hachesu P. Effectiveness of virtual reality-based exercise therapy in rehabilitation: a scoping review. Informatics in Medicine Unlocked. (2021) 24:100562. doi: 10.1016/j.imu.2021.100562
28. Rossi A, Pappalardo L, Cintia P, Iaia FM, Fernàndez J, Medina D. Effective injury forecasting in soccer with GPS training data and machine learning. PLoS One. (2018) 13(7):e0201264. doi: 10.1371/journal.pone.0201264
29. Fiscutean A. Data scientists are predicting sports injuries with an algorithm. Nature. (2021) 592(7852):S10–1. doi: 10.1038/d41586-021-00818-1
30. Hewett T, Webster K, Cohen S, Wagner P. 441 Longitudinal Changes in Force Plate Measures are Valid Indicators of Musculoskeletal Health in Professional American Football Players. in: Poster Presentations. London: BMJ Publishing Group Ltd and British Association of Sport and Exercise Medicine (2021). p. A168.3–A169. doi: 10.1136/bjsports-2021-IOC.405
31. Trasolini NA, Nicholson KF, Mylott J, Bullock GS, Hulburt TC, Waterman BR. Biomechanical analysis of the throwing athlete and its impact on return to sport. Arthrosc Sports Med Rehabil. (2022) 4(1):e83–91. doi: 10.1016/j.asmr.2021.09.027
32. Hando BR, Scott WC, Bryant JF, Tchandja JN, Angadi SS. The use of force plate vertical jump scans to identify special warfare trainees at risk for musculoskeletal injury: a large cohort study. Am J Sports Med. (2022) 50(6):1687–94. doi: 10.1177/03635465221083672
33. Hando BR, Scott WC, Bryant JF, Tchandja JN, Scott RM, Angadi SS. Association between markerless motion capture screenings and musculoskeletal injury risk for military trainees: a large cohort and reliability study. Orthop J Sports Med. (2021) 9(10):23259671211041656. doi: 10.1177/23259671211041656
34. Nagano H, Begg RK. Shoe-Insole technology for injury prevention in walking. Sensors. (2018) 18(5):1468. doi: 10.3390/s18051468
35. Crea S, Donati M, De Rossi SMM, Oddo CM, Vitiello N. A wireless, flexible, sensorized insole for gait analysis. Sensors (Basel). (2014) 14(1):1073–93. doi: 10.3390/s140101073
36. Ortiz-Padilla VE, Ramírez-Moreno MA, Presbítero-Espinosa G, Ramírez-Mendoza RA, Lozoya-Santos JDJ. Survey on video-based biomechanics and biometry tools for fracture and injury assessment in sports. Appl Sci. (2022) 12(8):3981. doi: 10.3390/app12083981
37. Goel DP, Lohre R. Value in Healthcare and Education: The Potential of Surgical Training Based on Immersive Virtual Reality. HMPI. (2022) 7(1). Available online at: https://hmpi.org/2021/12/02/value-in-healthcare-and-education-the-potential-of-surgical-training-based-on-immersive-virtual-reality/ (Accessed December 2, 2021).
38. Tsai MD, Hsieh MS, Jou SB. Virtual reality orthopedic surgery simulator. Comput Biol Med. (2001) 31(5):333–51. doi: 10.1016/s0010-4825(01)00014-2
39. Verhey JT, Haglin JM, Verhey EM, Hartigan DE. Virtual, augmented, and mixed reality applications in orthopedic surgery. Robotics Computer Surgery. (2020) 16(2):e2067. doi: 10.1002/rcs.2067
40. Horowitz BT. How AR & VR in Healthcare Enhance Medical Training. HealthTech. Available online at: https://healthtechmagazine.net/article/2022/12/ar-vr-medical-training-2023-perfcon (Accessed December 15, 2022).
41. Impellizzeri FM, Menaspà P, Coutts AJ, Kalkhoven J, Menaspà MJ. Training load and its role in injury prevention, part I: back to the future. J Athl Train. (2020) 55(9):885–92. doi: 10.4085/1062-6050-500-19
42. Schwellnus M, Soligard T, Alonso J-M, Clarsen B, Dijkstra HP, Gabbett TJ, et al. How much is too much? (part 2) international Olympic committee consensus statement on load in sport and risk of illness. Br J Sports Med. (2016) 50(17):1043–52. doi: 10.1136/bjsports-2016-096572
43. Drew MK, Finch CF. The relationship between training load and injury, illness, and soreness: a systematic review of the literature. Sports Med. (2016) 46(6):861–83. doi: 10.1007/s40279-015-0459-8
44. Kuroda Y, Young M, Shoman H, Punnoose A, Norrish AR, Khanduja V. Advanced rehabilitation technology in orthopaedics: a narrative review. Int Orthop. (2021) 45(8):1933–40. doi: 10.1007/s00264-020-04814-4
45. Chen X, Yuan G. Sports injury rehabilitation intervention algorithm based on visual analysis technology. Mob Inform Syst. (2021) 2021:1–8. doi: 10.1155/2021/9993677
46. Moratal D, editor. Finite Element Analysis – From Biomedical Applications to Industrial Developments. London: IntechOpen Limited (2012):510. doi: 10.5772/2552
47. Kanko RM, Laende EK, Davis EM, Selbie WS, Deluzio KJ. Concurrent assessment of gait kinematics using marker-based and markerless motion capture. J Biomech. (2021) 127:110665. doi: 10.1016/j.jbiomech.2021.110665
48. van de Woestijne PC, Bakhuis W, Sadeghi AH, Peek JJ, Taverne YJHJ, Bogers AJJC. 3D Virtual reality imaging of Major aortopulmonary collateral arteries: a novel diagnostic modality. World J Pediatr Congenit Heart Surg. (2021) 12(6):765–72. doi: 10.1177/21501351211045064
49. Opolski MP, Debski A, Borucki BA, Szpak M, Staruch AD, Kepka C, et al. First-in-Man computed tomography-guided percutaneous revascularization of coronary chronic total occlusion using a wearable computer: proof of concept. Can J Cardiol. (2016) 32(6):829.e11–13. doi: 10.1016/j.cjca.2015.08.009
50. Gokeler A, Bisschop M, Myer GD, Benjaminse PU, Dijkstra HGv, Keeken JAMv, et al. Immersive virtual reality improves movement patterns in patients after ACL reconstruction: implications for enhanced criteria-based return-to-sport rehabilitation. Knee Surg Sports Traumatol Arthrosc. (2016) 24(7):2280–6. doi: 10.1007/s00167-014-3374-x
51. Cui J, Du H, Wu X. Data analysis of physical recovery and injury prevention in sports teaching based on wearable devices. Prev Med. (2023) 173:107589. doi: 10.1016/j.ypmed.2023.107589
52. Zhu J. Real-time monitoring for sport and mental health prevention of college student based on a wireless sensor network. Prev Med. (2023) 173:107581. doi: 10.1016/j.ypmed.2023.107581
53. Yang Y. Application of wearable devices based on artificial intelligence sensors in sports human health monitoring. Measure Sens. (2024) 33:101086. doi: 10.1016/j.measen.2024.101086
54. Zhao J, Li G. A combined deep neural network and semi-supervised clustering method for sports injury risk prediction. Alexandria Eng J. (2023) 80:191–201. doi: 10.1016/j.aej.2023.08.048
55. Aroganam G, Manivannan N, Harrison D. Review on wearable technology sensors used in consumer sport applications. Sensors. (2019) 19(9):1983. doi: 10.3390/s19091983
56. Ye S, Feng S, Huang L, Bian S. Recent progress in wearable biosensors: from healthcare monitoring to sports analytics. Biosensors. (2020) 10(12):205. doi: 10.3390/bios10120205
57. Ali SM, Noghanian S, Khan ZU, Alzahrani S, Alharbi S, Alhartomi M, et al. Wearable and flexible sensor devices: recent advances in designs, fabrication methods, and applications. Sensors. (2025) 25(5):1377. doi: 10.3390/s25051377
58. Vo DK, Trinh KTL. Advances in wearable biosensors for healthcare: current trends, applications, and future perspectives. Biosensors. (2024) 14(11):560. doi: 10.3390/bios14110560
59. Mason R, Pearson LT, Barry G, Young F, Lennon O, Godfrey A, et al. Wearables for running gait analysis: a systematic review. Sports Med. (2023) 53(1):241–68. doi: 10.1007/s40279-022-01760-6
60. Adesida Y, Papi E, McGregor AH. Exploring the role of wearable technology in sport kinematics and kinetics: a systematic review. Sensors. (2019) 19(7):1597. doi: 10.3390/s19071597
61. The FDA’s Drug Review Process: Ensuring Drugs Are Safe and Effective. U.S Food and Drug Administration. Available online at: https://www.fda.gov/drugs/information-consumers-and-patients-drugs/fdas-drug-review-process-ensuring-drugs-are-safe-and-effective (Accessed June 19, 2020).
Keywords: sports medicine, rehabilitation, diagnostic imaging, wearable devices, sensors, virtual reality (VR), augmented reality (AR), smart devices
Citation: Amirouche F and Patel I (2025) Advancing sports medicine through technology: some applications and future visions. Front. Musculoskelet. Disord. 3:1609729. doi: 10.3389/fmscd.2025.1609729
Received: 10 April 2025; Accepted: 29 October 2025;
Published: 13 November 2025.
Edited by:
Laikang Yu, Beijing Sport University, ChinaCopyright: © 2025 Amirouche and Patel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Farid Amirouche, ZmFtaXJvdWNoZUBub3J0aHNob3JlLm9yZw==; YW1pcm91Y2hAdWljLmVkdQ==
 Farid Amirouche
Farid Amirouche Ishani Patel1
Ishani Patel1