Abstract
Objective:
In this study, we retrospectively evaluated the efficacy of platelet-rich plasma (PRP) for the treatment of training-induced knee traumatic osteoarthritis (KTOA) by means of a functional scale and MRI cartilage score, and analysed its effects on the improvement of knee function, pain relief and cartilage repair.
Methods:
In this study, 120 patients with training-induced KTOA (screened from 519 cases) were retrospectively analysed from May 2019 to December 2023, and knee function, pain and cartilage repair were evaluated by LKSS, VAS and MRI cartilage scores before and 3 months after treatment, and the statistical methods used were paired t-tests or Wilcoxon tests (P < 0.05).
Results:
Among 120 patients with training-induced KTOA treated with PRP, the Lysholm Knee Score (LKSS) significantly improved from (62.34 ± 18.69) to (81.2 ± 18.20) at 3 months after treatment, and the effective rate was 55.0%; the visual analogue score (VAS) of pain decreased from (5.24 ± 1.57) to (2.66 ± 1.43), and the effective rate of 81.7%; MRI cartilage damage score decreased from (3.24 ± 0.72) to (3.02 ± 0.86), and the effective rate was 36.7%; the differences were statistically significant (P < 0.05).
Conclusion:
KTOA due to PRP therapeutic training improves joint pain and promotes the recovery of knee joint function. Meanwhile, it has a repairing effect on articular cartilage damage.
1 Preface
Knee traumatic osteoarthritis (KTOA) is a secondary osteoarthropathy caused by acute mechanical injury, surgical trauma, load imbalance and chronic overload of the knee joint. Its pathological changes include degenerative lesions of articular cartilage, synovial inflammatory lesions and ossification lesions of the joints, etc. Typical clinical manifestations are pain in the knee joint, accompanied by varying degrees of limping, strangulation, weakness and other activity disorders. It occurs mostly in young adults, high-intensity physical training and other people, with a high incidence and disability rate (1–3). Epidemiological investigations have shown that people with high intensity physical training are at higher risk of lower limb injuries, which has been verified in multinational studies (4). Pain and dysfunction due to KTOA in this population may lead to a significantly increased risk of training interruption and may even have a serious impact on their careers (5).
For the treatment of KTOA, most cases are based on conservative treatments, such as oral or topical medications, rehabilitation training, physical factor therapy, etc. However, these treatments have the shortcomings of slow effect, long period, high cost, etc., which are difficult for patients to adhere to in the long term. With the progress of regenerative medicine, platelet-rich plasma (PRP) technology has developed rapidly and is widely used in clinical practice. Studies have shown that PRP treatment can reduce synovial inflammation, relieve pain, protect cartilage, and potentially promote tissue repair (6, 7). It is less invasive, low-risk and promotes tissue repair, but few studies have reported PRP treatment of training-induced KTOA, so the authors reviewed 519 patients with KTOA who attended the Department of Rehabilitation Medicine of the General Hospital of the Western Theatre of the People's Liberation Army during the period of May 2019 to December 2023, and from them, 120 patients with complete data of KTOA were screened for evaluation of the efficacy of the treatment. It is reported as follows:
2 Information and methods
2.1 General information
This study collected 519 patients who presented with knee pain with activity dysfunction at the Department of Rehabilitation Medicine of the General Hospital of the Western Theatre of the Chinese People's Liberation Army from May 2019 to December 2023, and who were clearly diagnosed with KTOA after physical examination and checkups, and screened a total of 120 cases of KTOA patients with complete information data according to the inclusion and exclusion criteria for analysis The data of 120 eligible KTOA patients were analysed according to the inclusion and exclusion criteria. All patients signed an informed consent form before receiving PRP treatment.
2.1.1 Diagnostic criteria
There are no specific diagnostic criteria for KTOA. Referring to the 2023 edition of the Osteoarthritis Diagnostic and Treatment Guidelines (
8) and the diagnostic value of magnetic resonance for KTOA in the clinic (
9), and combining with the diagnosis and inclusion criteria in the relevant literature, the specific diagnostic criteria are as follows:
① There is a clear history of knee trauma or (and) long-term high-intensity training;
② Having knee pain and weakness for ≥1 month;
③ Limited joint movement, stiffness, relief after activity, stiffness <30 min;
④ There are different degrees of swelling and pressure pain in the knee joint;
⑤ There is bone friction sound;
⑥ MRI suggests that the diagnosis of KTOA is met (including damage to synovium, joint capsule, subchondral bone structure, ligament, meniscus and other parts).
KTOA can be diagnosed if any two of items ①, ⑥ and ②, ③, ④, ⑤ are met.
2.1.2 Inclusion criteria
-
① According to the WHO Age Group Classification Standard, patients aged 18–60 with full civil capacity are selected, and there is no limitation for men and women;
-
② Patients who meet the diagnostic criteria of KTOA and have a disease duration of more than 1 month;
-
③ Patients who have signed the consent form for PRP treatment before treatment and strictly follow the quality control requirements for PRP treatment;
-
④ Patients who have VAS and LKSS scores recorded in the HIS system before PRP treatment and in the 3rd month after the end of PRP treatment course and have MRI imaging results.
2.1.3 Exclusion criteria
-
① Primary knee joint lesions, such as degenerative knee osteoarthritis;
-
② Other secondary knee joint lesions, such as knee joint tumour, gouty arthritis, rheumatoid arthritis, etc;
-
③ Patients who have received other invasive treatments and other additional treatments that may affect this study;
-
④ KTOA patients whose disease course is in the acute stage;
-
⑤ Patients with incomplete information shown in the HIS system, i.e., patients missing any one of VAS, LKSS score and MRI before PRP treatment and at the 3rd month after the end of PRP treatment course.
2.2 Data collection
All the data in this study were collected and organised by the researcher in the HIS system of the Western Theatre General Hospital. The specific data collection process is as follows (Figure 1):
Figure 1
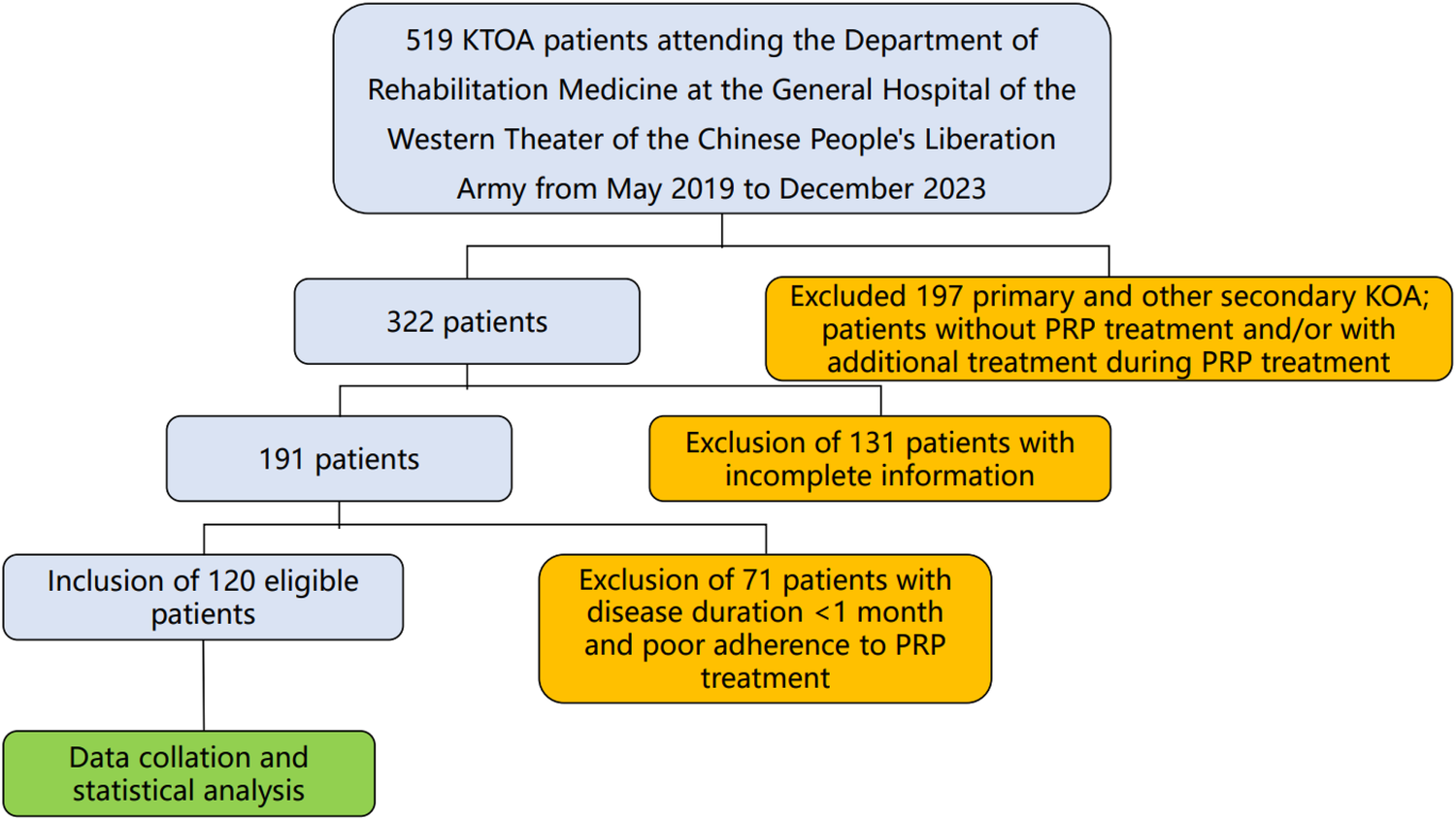
Study of the flow chart.
2.3 PRP preparation and treatment methods
2.3.1 PRP preparation
The preparation of PRP used in this study was completed in the Department of Blood Transfusion Medicine, using a blood component separator to collect and prepare pure platelet-rich plasma (P-PRP) without leukocytes, and applying haematocrit technology to obtain P-PRP products with a platelet concentration of (800–1,000) × 109/L. The PRP products prepared were subjected to quality control and analysis.The prepared PRP products were subjected to quality control analysis, and after qualified, they were placed in a refrigerator at −80° for freeze-thaw storage, and the storage time was ≤6 months.
2.3.2 PRP treatment methods
The triangular area surrounded by the outer edge of the patella, the lower edge of the femur and the upper edge of the tibia is often chosen as the entry point for intra-articular cavity injection.The patient sits with knees bent, disinfects and spreads the towel, and uses a disposable 5 ml syringe to pierce into the joint cavity, and then pumps back to confirm whether it is in the joint cavity and whether there is any accumulation of fluid; if there is no accumulation of fluid, 5 ml of PRP can be extracted and slowly injected into the joint cavity, and if there is any accumulation of fluid, then the accumulation of fluid will be pumped out and then carry out the PRP treatment again. After removing the needle, spot pressure was applied for 1 min, and then passive movement of the knee joint was done for 1 min.Inject once a week for a total of 5 times for 1 course of treatment (see Figure 2).
Figure 2

PRP treatment process.
2.4 Efficacy evaluation
LKSS score, VAS score and MRI articular cartilage damage degree score were collected from 120 patients who met the inclusion criteria for KTOA, and the indicators were evaluated at two time points, i.e., immediately before the start of PRP treatment and at the 3rd month after the end of the PRP treatment course, respectively. The specific evaluation contents are as follows:
2.4.1 Functional evaluation
2.4.1.1 Evaluation of main functional efficacy
Lysholm Knee Function Scoring Scale (LKSS): total score of 100 points, the higher the score, the better the knee function.
The LKSS before and after treatment was evaluated by applying the nimodipine scoring method according to the Guidelines for Clinical Research of New Chinese Medicines (
10). The criteria for determining the efficacy of LKSS were as follows:
Efficacy index: n = (post-treatment score—pre-treatment score)/pre-treatment score × 100%
Clinical recovery: n ≥ 75%;
Apparently effective: 50% ≤ n < 75%;
Effective: 30% ≤ n < 50%;
Ineffective: n < 30%, no clinical change or even aggravation.
2.4.1.2 Secondary function efficacy evaluation
Pain visual analogue score (VAS): a 10 cm scale was taken and patients evaluated their own pain in the affected knee, and the average value was taken from the pain in five different states of patients: lying down, sitting up, standing, walking and running, so as to make the pain evaluation more in line with the actual situation of the patients. A total score of 10 points, the lower the score, suggesting that the pain is less severe.
Criteria for determining the efficacy of VAS (
10):
Effective: more than 70% reduction in score;
Effective: 30%–70% reduction in score;
Ineffective: score reduction of less than 30%, no obvious improvement or even aggravation of clinical symptoms.
2.4.2 Structural evaluation
Magnetic resonance imaging (MRI) scoring of articular cartilage damage: Referring to the WORMS scoring standard published by Peterfy et al. (
11), and combining with the MRI grading of relevant knee cartilage lesions, we choose Recht's standard (
12,
13) to score the degree of articular cartilage damage, and read the films under the T2 compressed fat sequence of the MRI, so as to facilitate the observation of the degree of cartilage damage. The higher the score, the higher the severity of structural damage. The MRI scoring criteria for articular cartilage damage are as follows:
Score 0: Normal articular cartilage with diffuse uniform thinning of the cartilage but smooth surface, i.e., grade 0 (see Figure 3);
Score 1: disappearance of cartilage layered structure, focal signal alteration area in cartilage (including low signal, high and low mixed signal, high signal, high signal combined with bone marrow oedema as mentioned above), and smooth surface of cartilage, i.e., grade 1 (see Figure 4a);
Score 2: The cartilage surface contour is mildly to moderately irregular, and the depth of the cartilage defect is less than 50% of the full thickness, i.e., grade 2 (see Figure 4b);
Score 3: moderate to severe irregularity of the cartilage surface contour, with a depth of cartilage defect that reaches more than 50 per cent of the full thickness of the layer but is not completely detached, i.e., grade 3 (see Figure 4c);
Score 4: full thickness of cartilage defect, exfoliation, exposure of subchondral bone with or without subchondral bone signal changes, i.e., grade 4 (see Figure 4d).
Figure 3
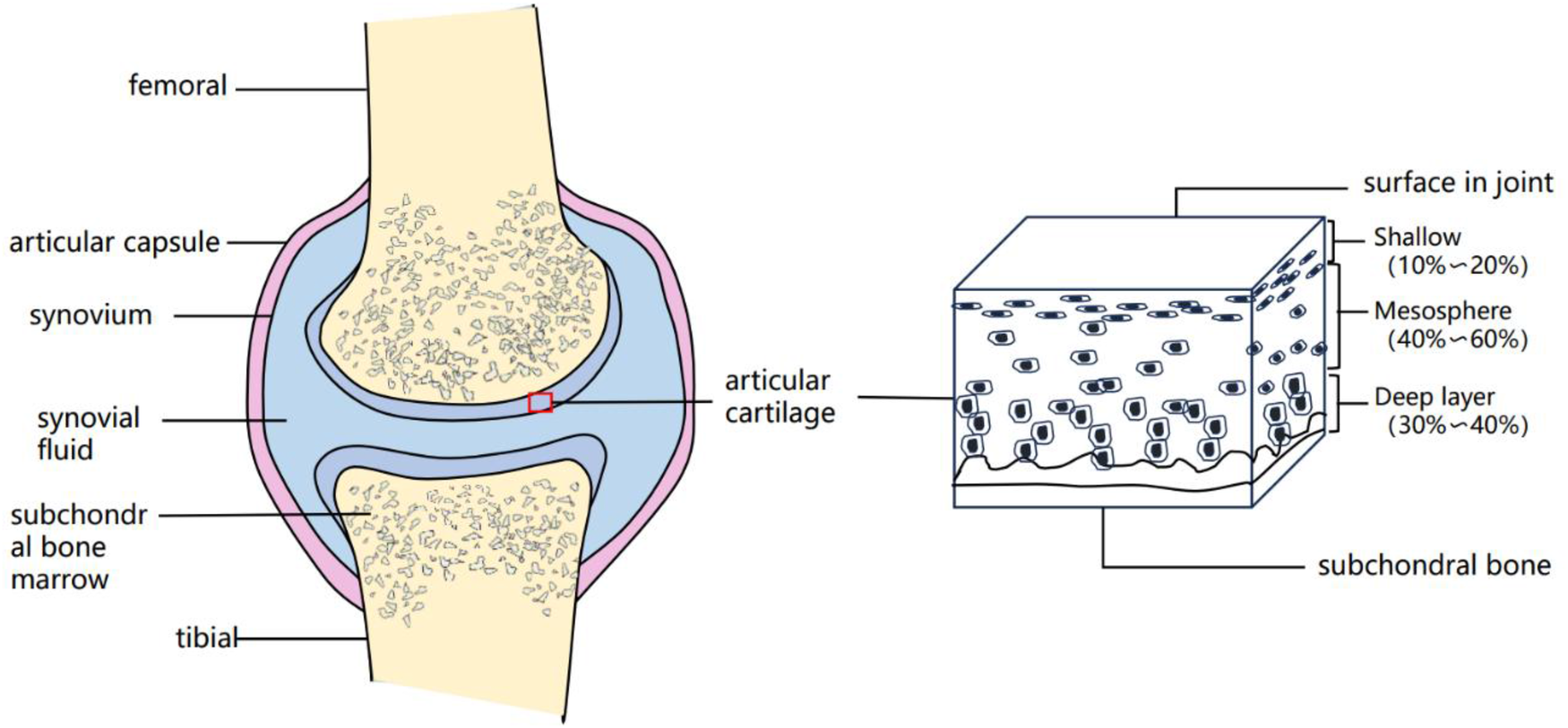
Schematic diagram of the normal knee joint and cartilage.
Figure 4
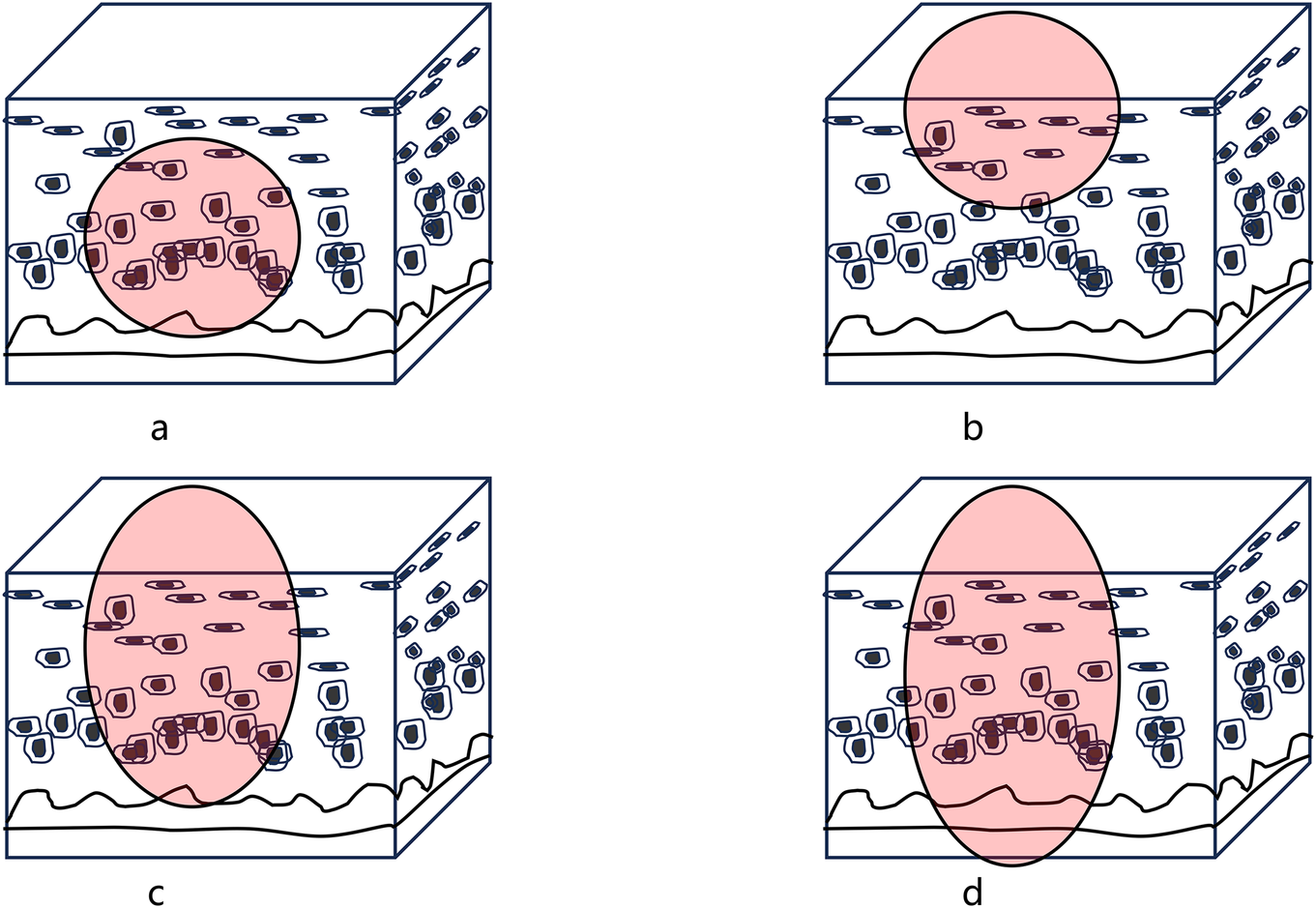
Schematic diagram of cartilage injury grading in MRI. (a) Grade 1: delamination disappears; (b) Grade 2: delamination disappears, involvement of the whole layer <50%; (c) Grade 3: delamination disappears; involvement of the whole layer >50%; deep into the cartilage; (d) Grade 4: delamination disappears; involvement of the whole layer subchondral bone exposure.
Criteria for determining the degree of efficacy of MRI articular cartilage damage:
Effective: a decrease in the articular cartilage score is considered effective.
Ineffective: the score of articular cartilage score is unchanged or increased, which is regarded as ineffective.
2.5 Security evaluation
The safety evaluation index of this trial is the incidence of adverse events. General adverse events of PRP treatment, such as local swelling and pain; serious adverse events include dizziness, headache, nausea, sweating, tachycardia, fainting, and shock. Adverse event rate = number of adverse events divided by total number of cases 100 percent.
2.6 Statistical methods
The data collected were analysed using IBM-SPSS27.0 software. Measurement data before and after treatment were expressed as , and paired-sample t-test was used for before and after treatment comparisons that conformed to normal distribution; Wilcoxon rank-sum test was used for before and after treatment comparisons that didn't conform to normal distribution; the difference was considered statistically significant at P < 0.05.
3 Results
3.1 General information acquisition
In this study, 519 patients with training-induced KTOA who underwent PRP treatment in the Department of Rehabilitation Medicine of the General Hospital of the Western Theatre of Operations from May 2019 to December 2023 were collected, and patients with incomplete data, incomplete follow-up records, other underlying diseases, other additional therapeutic interferences during the period of treatment and patients in the acute phase were excluded, so that a total of 120 patients were finally enrolled in the study as study subjects. Among them, there were 108 males and 12 females; the youngest was 19 years old and the oldest was 55 years old, all of them were in the stage of young and middle-aged; all the patients were in good physical condition, and none of them had any underlying diseases.
3.2 Functional efficacy evaluation
3.2.1 Evaluation of LKSS efficacy
From Table 1 we know that: (1) Comparison of the efficacy evaluation of patients' LKSS scores before and after treatment, the data of the two groups conform to the normal distribution, and the comparison is made using the paired samples t-test; the results show that the t-value = −15.665, P < 0.001, then P < 0.05, the difference is statistically significant (P < 0.05). (2) The patient's LKSS score (62.34 ± 18.69) before treatment and (81.2 ± 18.20) after LKSS treatment, the LKSS score scores improved, suggesting that PRP treatment of KTOA can improve knee joint function.
Table 1
| Pre-treatment | Post-treatment | t值 | P值 | |
|---|---|---|---|---|
| LKSS | 62.34 ± 18.69 | 81.2 ± 18.20 | −15.665 | <0.001 |
Comparison of efficacy in LKSS.
From Table 2, we know that: of the 120 patients, 54 patients, or 45.0%, had ineffective LKSS scores; 39 patients, or 32.5%, had effective LKSS scores; 15 patients, or 12.5%, had effective LKSS scores; and 10 patients, or 10.0%, had cured LKSS scores. The total effective rate was 55.0%.
Table 2
| LKSS efficacy | Null (%) | Validity (%) | Effective (%) | Cure (%) | Effective rate |
|---|---|---|---|---|---|
| Number (n = 120) | 54 (45.0) | 39 (32.5) | 15 (12.5) | 12 (10.0) | 55.0% |
Determination of the efficacy of LKSS.
3.2.2 Evaluation of VAS efficacy
From Table 3 we know that: (1) Comparison of patients' efficacy evaluation before and after VAS treatment, the data of the two groups conform to the normal distribution, and the comparison is made by the paired samples t-test; the results show that the t-value = 17.785, P < 0.001, then P < 0.05, and the difference is statistically significant (P < 0.05). (2) The patients' VAS score (5.24 ± 1.57) before treatment, and VAS score (2.66 ± 1.43) after treatment, the VAS score scores decreased, suggesting that PRP treatment of KTOA can improve pain symptoms.
Table 3
| VAS | Pre-treatment | Post-treatment | t值 | P值 |
|---|---|---|---|---|
| 5.24 ± 1.57 | 2.66 ± 1.43 | 17.785 | <0.001 |
Comparison of efficacy in VAS.
From Table 4, we know that: of the 120 patients, 22 patients, or 18.3%, had ineffective VAS efficacy; 71 patients, or 59.2%, had effective VAS efficacy; and 27 patients, or 22.5%, had significant VAS efficacy. The total effective rate was 81.7%.
Table 4
| VAS efficacy | Null (%) | Validity (%) | Effective (%) | Effective rate |
|---|---|---|---|---|
| Number (n = 120) | 22 (18.3) | 71 (59.2) | 27 (22.5) | 81.7% |
Determination of the efficacy of VAS.
3.3 Evaluation of structural efficacy
3.3.1 Evaluation of the degree of MRI articular cartilage damage
From Table 5 we know that: (1) the efficacy evaluation of the degree of MRI articular cartilage damage before and after the treatment of patients, the data of the two groups do not conform to normal distribution, and the comparison between before and after the treatment is made by Wilcoxon rank sum test; the results show that the Z-value = 3.295, P < 0.001, then P < 0.05, the difference is statistically significant (P < 0.05). (2) The patients' MRI articular cartilage damage degree score (3.24 ± 0.72) before treatment, and MRI articular cartilage damage degree score (3.02 ± 0.86) after treatment, the MRI articular cartilage damage degree score decreased, suggesting that PRP treatment of KTOA can promote cartilage damage repair.
Table 5
| MRI degree of articular cartilage damage | Pre-treatment | Post-treatment | Z值 | P值 |
|---|---|---|---|---|
| 3.24 ± 0.72 | 3.02 ± 0.86 | 3.295 | 0.001 |
Comparison of the effect of MRI on the degree of articular cartilage injury.
From Table 6, we know that: among 120 patients, 76 patients whose efficacy of MRI articular cartilage damage degree score was invalid, accounting for 63.3%; 44 patients whose efficacy of MRI articular cartilage damage degree score was effective, accounting for 36.7%. The total effective rate was 36.7%.
Table 6
| MRI degree of articular cartilage damage | Null (%) | Validity (%) | Effective rate |
|---|---|---|---|
| Number (n = 120) | 76 (63.3) | 44 (36.7) | 36.7% |
Determination of the efficacy of MRI articular cartilage injury.
3.4 Security evaluation
From Table 7, we know that: out of 120 patients, 10 patients (8.3%) had general adverse events and 2 patients (1.7%) had serious adverse events. The incidence of adverse events was 10.0%.
Table 7
| Undesirable incident | General adverse events (%) | Serious adverse event (%) | Adverse event rate |
|---|---|---|---|
| Number (n = 120) | 10 (8.3) | 2 (1.7) | 10.0% |
Statistics of adverse event.
4 Discussion
The incidence of training injuries in China varies greatly from one literature to another, which may be related to many factors such as the wide range of types of training injuries, different training intensities, different study designs and so on (14, 15). Foreign studies have shown (16) that skeletal muscle injuries are the most common among training injuries, and knee training injuries are a common disease, which is basically consistent with the current status of investigation in China.
Existing studies have shown that the pathogenesis of post traumatic osteoarthritis (PTOA) may be related to cartilage degeneration, inflammatory microenvironment, oxidative stress, and mechanical stress alteration (6), and KTOA is a type of traumatic osteoarthritis, from which we hypothesise that there may be a commonality in the pathogenesis of KTOA and PTOA. And PRP is rich in a variety of growth factors, various types of cytokines, such as EGF, PDGF, TGF-α, TGF-β, as well as VEGF and IGF, etc., and these biologically active components play key roles in cell growth, differentiation, synthesis of matrix, as well as regeneration and repair of tissues (17), therefore, these biologically active substances in PRP might play an important role.
For the quality control of PRP products, most of the existing PRP products are applied to the clinic in the form of homemade products, and in most cases the homemade PRPs are not tested for their composition, and the possible platelet concentration is only projected based on estimation, which makes it difficult to ensure the quality control of the composition. In contrast, the PRP products selected for this study were collected and prepared by a blood component separator in the Department of Transfusion Medicine, which controls the platelet concentration through parameter adjustments and uses disposable blood bags for quality control after dispensing, which can ensure that the composition of PRP products meets the needs of clinical treatment and maximises the effectiveness of treatment.
For the choice of PRP treatment protocol, according to the 2022 version of the “Expert Consensus on Autologous Single-Harvested Platelet-Rich Plasma Joint Cavity Injections for Osteoarthritis of the Knee”, it is recommended that the injection volume of PRP treatment should be (4–8) ml/times, and the interval between injections should be 1–2 weeks, and a course of 3–4 injections, and the number of injections can be appropriately increase the number of injections (18). Combined with the fact that most of the patients in this study were more severe, the protocol of 5 ml injection dose in a single single knee, once a week, 5 times a course of treatment was chosen in this study.
Patients with KTOA showed a variety of dysfunctions such as joint pain, joint instability, strangulation, claudication, etc., and in severe cases, even affecting the ability to perform activities of daily living. Therefore, LKSS score is necessary as a functional evaluation index in this study. The results of this study showed that PRP treatment for KTOA was beneficial to improve patients' knee function (P < 0.001), but the LKSS efficacy efficiency was not high (55.0%). For the average KOA patients even with PRP alone the treatment efficiency can reach about 80% (19, 20). The reasons for the difference in functional improvement may be as follows: (1) The LKSS efficacy criterion selected in this study was the nimodipine scoring method, and the LKSS efficacy index of n < 30% was considered ineffective, whereas in some previous studies, an increase in the score was regarded as effective. (2) The low rate of functional improvement in this study may also be related to the insufficient follow-up time of the patients, and it takes some time for PRP treatment to improve knee function. (3) Only patients treated with PRP alone were selected for observation in the design of this study, and it is difficult to attribute the improvement in function to PRP treatment. ④ The subjects of this study were people with high-intensity physical training, whose occupational characteristics may be more likely to cause severe knee trauma; most patients had a history of violent injuries and surgical treatments prior to treatment and may still need to continue training after treatment, as well as some of the patients themselves had a large body mass index and other reasons may have contributed to the poor improvement of knee function. Therefore, this means that we need to perform the necessary analyses of the factors mentioned above.
In terms of the results of the improvement of the degree of MRI articular cartilage damage, the existing relevant studies have not been found to evaluate the efficacy of the Recht criteria, although there is a study in the imaging professional research (21) using the Recht criteria for observational evaluation, but it is different from the purpose of the observation and evaluation that we would like to observe and evaluate, so we can learn from the relevant criteria for evaluation, but we can not compare the effectiveness of the situation with the existing studies. Nevertheless, it does not affect the use of MRI articular cartilage damage score in this study can be used as an objective structural evaluation index for efficacy evaluation. The results may indicate to some extent that PRP is effective in the treatment of KTOA and has the potential to promote tissue repair, although the efficiency was not satisfactory. The reasons affecting the efficacy of PRP may be as follows: (1) some of the patients included in our study had a high degree of damage to articular cartilage and other structures before treatment, and most of the patients in this group had MRI articular cartilage damage scores of 3–4, and PRP had limited ability to repair this kind of damage; (2) some of the patients with pre-treatment MRI articular cartilage damage scores of 2–3 had further MRI damage after treatment and were unable to repair the damaged cartilage; (3) some of the patients with pre-treatment MRI articular cartilage damage scores of 2–3 had further MRI damage after treatment. This may be related to the large body mass index of the patients and the continuation of training after treatment; (3) there is also a part of the patients who have no change in the MRI cartilage damage score before and after treatment, which cannot be excluded from the time of follow-up, and the follow-up time of this study was in the 3rd month after the end of the PRP treatment, which is similar to the time of natural repair of cartilage damage; however, since the patients may have severe damage, the PRP repair ability is limited; (4) there are also some patients who have a score of 2–3 before treatment, and then the MRI cartilage damage score is increased after the treatment. This is similar to the time for natural repair of cartilage damage; however, due to the fact that the patients may have severe cartilage damage, high body mass index, and continued participation in training after treatment, the treatment and repair effects of PRP have not yet been clearly demonstrated during the follow-up period; (5) The improvement in the degree of cartilage damage on MRI was not as good as the improvement in bone marrow oedema and joint effusion, which may be due to the fact that the short-term anti-inflammatory effect of PRP was superior to the effect of tissue repair; (6) Of course, in addition to the reasons mentioned above, we still cannot rule out the possibility that there was no change in the degree of chondral damage scores. Of course, in addition to the above reasons, we still cannot exclude the possibility of errors caused by the level of film readers and differences in equipment presentation.
It is important to acknowledge that there are certain limitations to this study. The most significant limitation is the lack of a control group, which fundamentally limits our ability to draw causal inferences from the results of the study and prevents direct comparisons with untreated or other treated cohorts. First, this design makes our analyses vulnerable to confounding bias, as unmeasured variables (e.g., differences in patient fitness, clinician selection bias, or unrecorded comorbidities) may influence treatment decisions and outcomes. Thus, the favourable outcomes we observed for PRP treatment may have overestimated its true effect in an unselected population. In addition, because all data were obtained from the medical record system of a tertiary care hospital, there may have been selection bias, and our cohort may not have been fully representative of patients treated in the community, thus limiting its generalisability. Therefore, our findings should be interpreted as a valuable treatment rather than conclusive evidence of efficacy. These findings contribute to hypotheses that must be tested in future prospective randomised settings to establish causality and determine the true extent of benefit.
In conclusion, KTOA due to PRP treatment can improve joint pain and promote the recovery of knee joint function. It also has a repairing effect on articular cartilage damage. However, it is necessary for us to sort out and analyse the relevant information that may affect the efficacy as comprehensively as possible, so as to further elucidate the factors that may affect the efficacy of PRP therapy training-induced KTOA, with a view to improving the clinical efficacy of KTOA.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The requirement of ethical approval was waived by Ethics Committee of the General Hospital of the Western Theater of Operations of the Chinese People's Liberation Army for the studies involving humans because The study was a previous data collection, ethical approval obtained. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin because The study was a previous data collection.
Author contributions
CC: Writing – original draft. YH: Data curation, Writing – review & editing. HW: Writing – review & editing, Investigation. ZX: Conceptualization, Writing – review & editing. LW: Writing – review & editing. RP: Writing – review & editing, Supervision. LZ: Resources, Writing – review & editing. ZW: Resources, Methodology, Writing – review & editing. JZ: Writing – review & editing, Resources. WW: Methodology, Supervision, Conceptualization, Writing – original draft, Writing – review & editing. SH: Writing – review & editing, Resources.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Glyn-Jones S Palmer AJR Agricola R Price AJ Vincent TL Weinans H et al Osteoarthritis. Lancet. (2015) 386(9991):376–87. 10.1016/S0140-6736(14)60802-3
2.
Rivera JC Beachler JA . Distraction arthroplasty compared to other cartilage preservation procedures in patients with post-traumatic arthritis. A systematic review. Strateg Trauma Limb Reconstr. (2018) 13(2):61–7. 10.1007/s11751-018-0305-2
3.
Zhao D Yao T Guo Y Mu L Meng X . Clinical study on treating ankle joint traumatic arthritis with external washing of Chinese medicine and sodium hyaluronate injection. Shaanxi Tradit Chin Med. (2018) 39(5):621–4. 10.3969/j.issn.1000-7369.2018.05.024
4.
Müller-Schilling L Gundlach N Böckelmann I Sammito S . Physical fitness as a risk factor for injuries and excessive stress symptoms during basic military training. Int Arch Occup Environ Health. (2019) 92(6):837–41. 10.1007/s00420-019-01423-6
5.
Wu J Li C Huang P Zhou Z Zhao D Jia Z et al Review of prevalences of military training-related injuries in Chinese army. J PLA Med Coll. (2020) 41(12):1236–4, 1246. 10.3969/j.issn.2095-5227.2020.12.015
6.
Chen Z Jun Z Shihong X Chaoyang J Peixin W Yufan Li et al PRP and the treatment of traumatic arthritis. Chem Life. (2023) 43(11):1691–8. 10.13488/j.smhx.20230648
7.
Zhuang W Li T Li Y Zhang Y Gao J Wang X et al The varying clinical effectiveness of single, three and five intraarticular injections of platelet-rich plasma in knee osteoarthritis. J Orthop Surg Res. (2024) 19(1):284. 10.1186/s13018-024-04736-6
8.
Chinese Society of Traditional Chinese Medicine. Osteoarthritis of the knee: a guide to the combination of Chinese and Western medicine (2023 edition). Chin Orthop. (2023) 35(6):1–10. 10.3969/j.issn.1001-6015.2023.06.001
9.
Zhe W . Advantages of MRI in forensic identification of traumatic knee osteoarthritis. (2022) 0(13):90–2. 10.3969/j.issn.1674-9561.mingy202213033
10.
Xiaoyu Z . Guidelines for Clinical Research of New Chinese Medicines. Beijing: China Pharmaceutical Science and Technology Press (2002).
11.
Peterfy CG Guermazi A Zaim S Tirman PFJ Miaux Y White D et al Whole-organ magnetic resonance imaging score (WORMS) of the knee in osteoarthritis. Osteoarthr Cartil. (2004) 12(3):177–90. 10.1016/j.joca.2003.11.003
12.
Recht MP Kramer J Marcelis S Pathria MN Trudell D Haghighi P et al Abnormalities of articular cartilage in the knee: analysis of available MR techniques. Radiology. (1993) 187(2):473–8. 10.1148/radiology.187.2.8475293
13.
Chen Q Yang F . Early evaluation of articular cartilage defects using magnetic resonance imaging in comparison with arthroscopy. China Clin Rehabil. (2005) 9(30):133–5. 10.3321/j.issn:1673-8225.2005.30.063
14.
Pang C Chen ZD Wei B Xu WT Xi HQ . Military training-related abdominal injuries and diseases: common types, prevention and treatment. Chin J Traumatol. (2022) 25(4):187–92. 10.1016/j.cjtee.2022.03.002
15.
Wang P Shi C Chen J Gao X Wang Z Fan Y et al Training methods and evaluation of basketball players' agility quality: a systematic review. Heliyon. (2024) 10(1):e24296. 10.1016/j.heliyon.2024.e24296
16.
Molloy JM Pendergrass TL Lee IE Chervak MC Hauret KG Rhon DI . Musculoskeletal injuries and United States army readiness part I: overview of injuries and their strategic impact. Mil Med. (2020) 185(9–10):e1461–71. 10.1093/milmed/usaa027
17.
Ramaswamy Reddy S Reddy R Babu NC Ashok GN . Stem-cell therapy and platelet-rich plasma in regenerative medicines: a review on pros and cons of the technologies. J Oral Maxillofac Pathol. (2018) 22(3):367. 10.4103/jomfp.JOMFP_93_18
18.
Xiangyan H Qiang Z Ping Z Guiqiu S Jiwu G . Expert consensus on the treatment of knee osteoarthritis with autologous single-minute platelet-rich plasma arthrocentesis. Chin J Blood Transfus. (2022) 35(12):1187–94. 10.13303/j.cjbt.issn.1004-549x.2022.12.001
19.
Ding Z Dong H . Clinical study of platelet-rich plasma combined with triamcinolone acetonide in the treatment of patients with knee osteoarthritis. Chin J Clin Pharmacol. (2023) 39(12):1694–8. 10.13699/j.cnki.1001-6821.2023.12.005
20.
Tan Q Chen RX . Effects of PRP combined with celecoxib treatment on knee function and quality of life in patients with knee osteoarthritis. Contemp Clin J Med. (2023) 36(2):45–6. 10.3969/j.issn.2095-9559.2023.02.26
21.
Xiao P Chen C-f Liang W-b Yuan H-t Tan L-l Shi Y-p . The relationship between bone contusion in the traumatic knee and articular cartilage degenerative injury with 3.0T MRI. Chin J CT MRI. (2019) 17(8):150–2. 10.3969/j.issn.1672-5131.2019.08.045
Summary
Keywords
platelet-rich plasma, knee traumatic osteoarthritis, magnetic resonance imaging, Lysholm score, pain visual analogue score, cartilage repair
Citation
Cheng C, He Y, Wang H, Xiao Z, Wang L, Pang R, Zhu L, Wang Z, Zheng J, Wang W and Huang S (2025) Evaluation of the efficacy of platelet-rich plasma in the treatment of training-induced knee traumatic osteoarthritis: a retrospective study based on a multidimensional quantitative evaluation. Front. Musculoskelet. Disord. 3:1622400. doi: 10.3389/fmscd.2025.1622400
Received
03 May 2025
Accepted
29 August 2025
Published
26 September 2025
Volume
3 - 2025
Edited by
Dalila Scaturro, University of Palermo, Italy
Reviewed by
Wei Yao, Rabpharma, United States
Xu Hong, Heilongjiang Academy of Traditional Chinese Medicine, China
Updates
Copyright
© 2025 Cheng, He, Wang, Xiao, Wang, Pang, Zhu, Wang, Zheng, Wang and Huang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Wenchun Wang wwc1977biology@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.