- 1Syracuse VA Medical Center, United States Department of Veterans Affairs, Syracuse, NY, United States
- 2VA Center for Integrated Healthcare, VA Western New York Healthcare System, Buffalo, NY, United States
Introduction
Chronic lower back pain (CLBP) is a significant public health problem and is one of the leading causes of years lived with disability. It creates a significant burden on both the LBP sufferer and on the healthcare system (1). The costs associated with CLBP are estimated to be approximately $40 billion per year (approximately $2,000/patient/year) (2). There are over 200 different treatment strategies for CLBP, and while all these treatments work some of the time, none of them work all the time thus leaving the treating clinician in a conundrum as to what to do (3). One of the explanations for this lack of responsiveness is the complex nature of the condition. The biopsychosocial (BPS) model of pain recognizes that chronic pain is a complex phenomenon that is unique in everyone (4). CLBP requires a thoughtful and comprehensive approach to management that applies evidence-informed, patient-centered strategies typically through a multimodal approach. However, one of the challenges of a multimodal approach is that it is difficult for one provider to possesses the necessary skills to deliver the care in the most efficient and effective manner. Thus, multidisciplinary teams working in collaboration can enhance the effects of each intervention.
The goal of this commentary is to discuss a novel model of care using two commonly accessed disciplines for chronic pain—chiropractors and behavioral health (BH) providers—which we have called Joining Forces. We will discuss the role of co-management between these two disciplines in delivering an evidence-based management strategy, specifically a biopsychosocial (BPS) management approach. We will discuss the role of manual therapy and/or acupuncture which are commonly performed by chiropractors, in addressing the pathoanatomic and neurological aspects of CLBP while the BH providers emphasize the psychosocial aspects. We will further discuss the potential synergistic effect that may result from each of the disciplines reinforcing the treatment recommendations of the other through a collaborative treatment model. This model not only coordinates care, but also attempts to address some of the contextual factors that can affect prognosis, such as the trust and communication in the patient-practitioner relationship (5).
Background
CLBP traditionally has been based on a pathoanatomic model (PAM), specifically that it originates in the joints, intervertebral discs, muscles and ligaments of the lumbar spine (6). An over emphasis on this PAM has the potential for care which does not follow current practice guidelines. Examples of nonguideline concordant care include overutilization of invasive (e.g., surgery and injections) and non-invasive management strategies (e.g., acupuncture or manual therapy) that can fail to engage patients in self-care strategies and can create passive dependency (7). The BPS model of pain acknowledges that chronic pain includes both pathoanatomic and psychosocial components (8). The recognition of the BPS model of pain resulted in an increased interest in applying psychological interventions to address chronic pain such as Cognitive Behavioral Therapy (CBT), Mindfulness Based Stress Reduction (MBSR), and others (9).
Recent systematic reviews and clinical practice guidelines have demonstrated that both PAM- based interventions and psychological interventions result in mild to moderate improvements in chronic pain and are therefore recommended as management options for CLBP (10). Comparative effectiveness studies have failed to demonstrate that one approach is significantly superior to the other (11). In response to these conclusions there have been some attempts to develop multimodal interventions delivered by the same provider, specifically to train physical therapists to deliver psychologically-informed treatment, such as incorporating cognitive behavioral techniques alongside the PAM based treatments such as manual therapy and/or exercise (12). Unfortunately, this approach to multimodal treatment has also failed to demonstrate superiority over other types of CLBP interventions. A systematic review of 24 studies on psychologically informed physical therapy found that “no clinically significant differences were found for pain and disability between physical, behavioral/psychologically informed, and combined interventions.” (13) A possible explanation for this disappointing finding is that physical and psychologically informed interventions may have similar mechanisms of effect. This possible conclusion is based on trials showing that successful outcomes, even after a PAM based intervention, are often mediated by changes in cognitive and psychological factors (e.g., fear avoidance, catastrophizing, pain self-efficacy, illness beliefs) (14–16). Another possibility is that other important “nonspecific factors” or contextual factors such as clinician support, clinician beliefs, empathy, and ability to motivate and accommodate patients’ treatment preferences and expectations may be common to these seemingly different interventions (5, 17). This assertion is supported by data showing that a positive patient–provider interaction is linked to reduced pain and disability (18). Taken together, it appears that what is needed is an integrated care approach that while truly reflective of the BPS model is less resource intensive than multidisciplinary pain clinics (19), but more encompassing that what a single provider is able to deliver. We suggest that one approach is a care model that would incorporate evidence-based PAM-focused care (such as manual therapy and/or acupuncture) in collaboration and co-management with BH interventions (such as CBT for chronic pain).
Overview of pathoanatomic based interventions
The PAM of chronic lower back pain recognizes the role of anatomic and neurological structures in the experience of pain (20). Many of the invasive procedures developed to address CLBP are based on this model, including spinal injections, radiofrequency ablation and spinal surgery. Many non-invasive procedures also rely on this model including manual therapy and acupuncture. Manual therapy interventions are based on the evidence that there are mechanical, neurological and myofascial contributors to CLBP. There is compelling evidence that intervertebral discs, facet joints, sacroiliac joints and myofascial structures are potential contributors to CLBP (20). These factors are related to degenerative changes in both the disc and facet which result in loss of motion. One of the confounding factors however is that there is not a direct correlation between the extent of anatomic pathology (such as DJD or disc herniations) and the experience of pain (21). One potential explanation for this lack of correlation is that nociception is influenced by local inflammatory changes as well as central nervous system responsiveness (22–24). In addition to the role of articular structures and inflammation, myofascial structures have also been hypothesized to contribute to CLBP. Myofascial pain syndrome (MPS) is common among patients with musculoskeletal pain problems. MPS is a pain condition originating from muscle and surrounding fascia. The exact pathophysiology of MPS is not known, but mechanisms are thought to be similar to the other pathoanatomic factors including mechanical dysfunction, inflammation and central mechanisms (25). In summary, the etiology of CLBP from a pathoanatomic perspective is related to mechanical factors, myofascial pain, inflammation and central mechanisms. However, as recent systematic reviews have elucidated the approaches that are based primarily on a pathoanatomic model have failed to demonstrate consistently predictable durable improvements in CLBP that are superior to other interventions (11, 26).
Manual therapy mechanism
Recent systematic reviews and clinical guidelines support the role of manual therapies such as spinal manipulation in the management of CLBP (10). The mechanisms by which MT is theorized to affect CLBP can be broken down into mechanical and neurological mechanisms. Mechanical effects include the following mechanisms: vertebral position, facet joint space, spinal stiffness and resting muscle thickness (27). Neurological mechanisms of MT include peripheral, segmental spinal, and supraspinal neurological mechanisms occurring with the application of MT, which can be measured directly or indirectly (28). MT is frequently combined with a home exercise program and/or lifestyle recommendations (29). Compliance with these recommendations is sometimes challenging, but when followed it may result in improved pain and function (30). Manual therapy, specifically when delivered by a chiropractor is associated with strong patient satisfaction (31), which is an important contextual factor associated with treatment responsiveness in those with CLBP (5).
Acupuncture mechanism
The mechanisms of acupuncture, like MT include both mechanical (local) effects and central nervous system effects. Mechanistic studies involving animal models support the notion that modulation of various molecules at the brain, spinal cord, and peripheral levels is responsible for the analgesic effects of acupuncture in chronic pain conditions (32). The role of acupuncture in managing pain can be broken into three broad categories: (1) release of neurotransmitters and neuromodulators (such as serotonin and norepinephrine, dynorphin), (2) Modulation of pain signal transmission (descending inhibition, peripheral nerve stimulation, spinal cord modulation or cortical changes), (3) “Other” (inflammation modulation or nonspecific therapeutic effects) (32–35) Acupuncture is also associated often with self-care recommendations (including home exercise programs) and it is also associated with strong patient satisfaction (36).
The role of psycho-social factors in CLBP
One explanation of the failure of PAM-based treatments to result in consistent improvement is that they do not incorporate interventions that address the psycho-social factors associated with CLBP. Although there are multiple depictions of the BPS model of chronic pain, in general, the addition of psychological factors and social (or social-environmental) factors to the PAM is thought to provide a more comprehensive depiction of the many influences that can promote, maintain, or ameliorate pain (See Figure 1). Psychological factors are broad and can include those related to personality, affective states, mental health diagnoses (e.g., depression, anxiety, PTSD), stress, perceived control, self-efficacy, coping style, pain-related attitudes, cognitions, and behaviors. Social factors are equally broad and include but are not limited to interpersonal relationships, social isolation, occupational status, experience of discrimination, financial concerns, and access to healthcare. In general, the presence of more adverse psychological or social factors typically results in increased likelihood of progressing from acute to chronic pain and experiencing worse pain related outcomes (e.g., pain-related disability). While this wide array of factors are more than a single treatment could address, it indicates that there are numerous potential points of intervention for addressing CLBP.
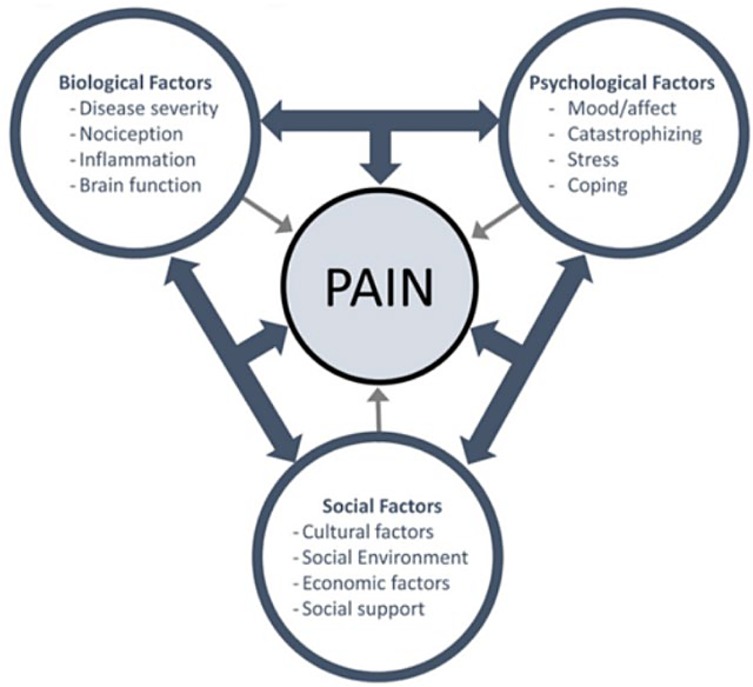
Figure 1. Biopsychosocial model of pain. (Source: https://themtdc.com/have-we-ballsed-up-the-biopsychosocial-model/).
The relationship between psycho-social factors and pain is frequently bi-directional. Depression, for example, is a common co-occurrence with chronic pain and provides an excellent example of why psychological factors are important considerations for treatment of pain. Patients with pre-existing depressive disorders are more likely to develop chronic pain due to an apparent increased vulnerability, and at the same time, chronic pain predicts the development of depression over time. Empirically, it has been demonstrated that chronic pain is more difficult to treat in the presence of depression and other comorbidities (37, 38). Thus, considering the significant role of even a single additional psychosocial factor (i.e., co-morbid depression) expands the PAM-based model to include additional target for therapy (i.e., shared biological and psychological mechanisms) that can improve treatment for pain.
Mechanisms of psychological intervention for CLBP
Psychological intervention for chronic pain has evolved from a strictly behavioral focus, to addressing maladaptive cognitions, emotion regulation, and applying transdiagnostic approaches such as mindfulness, acceptance, and self-compassion. While there is a growing variety of psychological approaches for chronic pain, each with a developing foundation of empirical support, CBT remains the most studied and well-supported psychological intervention for chronic pain, yielding small to moderate improvements in pain and pain-related function (39, 40). The CBT model of chronic pain addresses the chronic pain cycle in which the interplay between the experience of pain and resulting distressing thoughts and feelings perpetuate avoidance and disability (Figure 2).
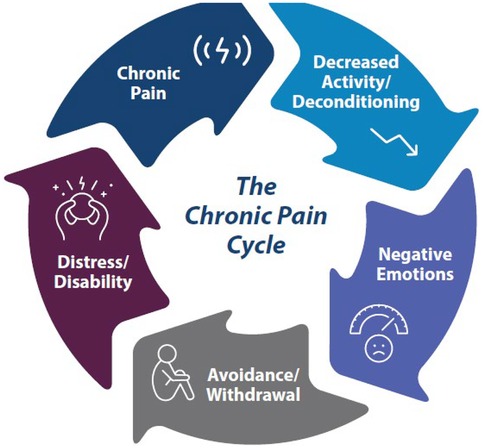
Figure 2. Chronic pain cycle. Beehler et al. (61).
There are several potential mechanisms by which CBT for chronic pain improves pain and related outcomes, but prior work has primarily focused on pain self-efficacy and catastrophizing (41–43). CBT for chronic pain includes psychoeducation, behavioral skills, and cognitive skills designed to address these factors among others. In addition to relaxation training, behavioral activation, and learning to use pacing to re-engage in activities safely, CBT for chronic pain likely impacts pain self-efficacy because it includes elements of effective self-efficacy interventions (e.g., goal setting, use of homework, self-management/self-monitoring) (44). CBT for chronic pain also imparts cognitive coping skills to identify, modify, or replace automatic negative thoughts with more adaptive responses. It is also worth mentioning that CBT, like most psychotherapies, is an approach rooted in the development of a strong therapeutic relationship, and this relationship likely also contributes to improved outcome. CBT can be delivered in different ways: as an individual face-to-face therapy, as a self-administered therapy, which can be done by using materials (i.e., reading books or using the Internet) teaching how to implement CBT without the guidance of a mental health professional; or as a group treatment. The latter is notable, as it confronts social isolation, which is an important aspect in the case of chronic pain. It is well known that interaction with other people is a powerful way of creating a shift out of pain pathways leading to decreased pain perception.
Advantages and disadvantages of each approach
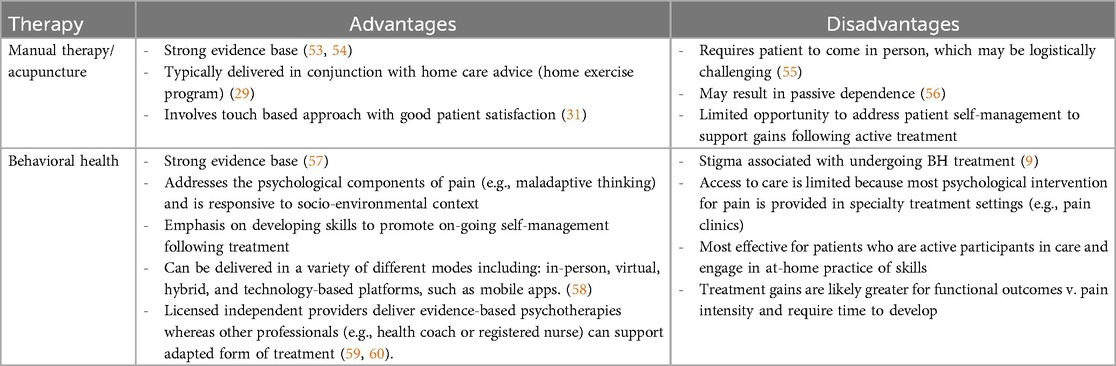
Manual therapy, acupuncture and BH interventions have all been shown to result in improvement in patient outcomes. However, there are advantages and disadvantages to each of them (see Table 1).
Role of co-management
There is a need to design interventions that will address pain from a biopsychosocial perspective, but at the same time be efficient and effective. One model that may be considered is taking two disciplines that are both utilizing evidence-based strategies and combine their care in a pragmatic way. Specifically, if providers are trained in (1) the nature of what the co-managing clinician provides to patients, and (2) methods for efficient interprofessional communication, such as through the electronic medical record (EMR), each clinician could therefore reinforce the treatment and self-management recommendations of the other. This approach based on integration of services has the potential to create a synergistic effect that will be superior to training one provider to deliver both types of intervention (such as the behaviorally informed interventions have done) (13). The proposed novel model that would allow both clinicians to deliver the care that they are most suited to deliver while they encouraged the patient to engage in the behaviors that the other provider has recommended. Below, we provide an overview of Joining Forces, in which a BH provider and a chiropractor could co-manage a patient with CLBP.
Joining Forces model of care
In the Joining Forces model we recommend that as part of basic training, each discipline received education on the management strategies and self-care recommendations that the other provider would deliver in a routine treatment session. Specifically, we would propose a training program that would be co-led by a BH provider and a chiropractor that would be delivered in three 60 min webinars (See Table 2).
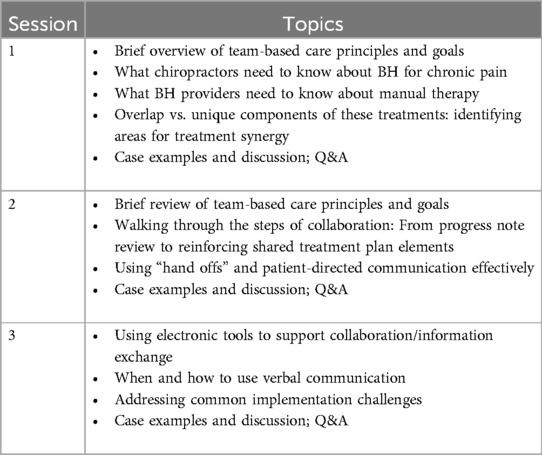
Table 2. Overview of Joining Forces training for chiropractors and BH providers (48).
In these trainings the BH provider would provide education to the chiropractic team on the role of CBT-CP in the management of CLBP, such as pacing, relaxation training, social engagement and others. The chiropractor would educate the BH provider in the mechanisms of manual therapy and acupuncture and discuss the typical self-management strategies that are part of the normal chiropractic encounter including home exercises, postural re-education and lifestyle modifications. In preparation for the encounter, the provider would briefly review the prior progress note from the other service in the EMR. The provider would simply use an “inquire/encourage/communicate” approach. He/she would “inquire” of the patient what the other provider had recommended for a self-management strategy at the previous encounter to begin the conversation and assess the patient's understanding of the self-management skill. They would then encourage (based on their training) the patient to continue with the recommended treatment through the most relevant approach, such as providing positive reinforcement for successful attempts to engage in self-management or briefly discuss barriers to engagement for those who had not attempted to implement a particular skill. The provider would then “communicate” with the other provider through the shared EMR and potentially through a second method (e.g., phone, secure messaging) to highlight anything of particular importance. It should be noted that the training webinars will include opportunities for the providers to give feedback concerning potential barriers or challenges that may be specific to their location such as scheduling issues or space concerns or even potential communication logistics. This will allow for customization of the Joining Forces model for each location and type of setting.
An example of this model would be in the case of a 50-year-old male with chronic lower back pain who also suffers from mild depression. The patient has undergone traditional physical therapy and had a series of medial branch blocks without much success. The patient is referred to the Joining Forces team and evaluated by the chiropractor first and then the clinical psychologist. Each of the providers would put an alert in the electronic medical record for the other provider. Once the patient began treatment, the chiropractor would put in the EMR specific recommendations for self-care that could be reviewed by the clinical psychologist (such as initiation of a walking program or home stretching program). Simultaneously, the clinical psychologist would outline the specific recommendations and homework instructions consistent with CBT for chronic pain (such as diaphragmatic breathing instructions or activity pacing). Each of the providers would then reenforce the recommendations from the other provider by querying the patient about their adherence with the instructions and also encouraging the patient to continue to follow up with the other provider.
Preliminary data
The Joining Forces model is theoretical; however, the two authors of this paper have previous experience that demonstrate the potential feasibility of the model. Dr. Beehler has shown that BH services are underutilized by veterans with chronic pain. A retrospective chart review indicated that veterans with chronic musculoskeletal pain have significantly more encounters than the controls for all forms of care (including chiropractic) except BH care (45). Therefore, the current program may provide an opportunity for chiropractors to encourage engagement with BH. Dr. Dougherty has demonstrated that chiropractors can be trained in the principles of CBT-CP and can deliver these principles reliably. (Dougherty; NCT01894282) A recently published case series demonstrated the potential of co-management of Veterans with chronic musculoskeletal pain between chiropractors and BH providers. This study indicated that all the participating veterans showed functional improvements and improved pain (46). While there remains further work to do in this area, it suggests that it is feasible to have chiropractors reenforcing BH principles to patients with chronic pain.
Proposed methods for implementation of joining forces model
The authors propose the following steps for implementation of the Joining Forces model in an integrated setting, such as the Veterans Health Administration (VHA). The initial step would be to formally develop and test the three 60 min webinars on a sample of both BH and chiropractic providers to determine the acceptability of the training. After incorporating clinician feedback for modifications to improve acceptability, the next step would be to pilot test the training at a single VA facility and perform a prospective cohort study to evaluate the feasibility and preliminary effectiveness of implementing the program. This study would be performed using a mixed methods design to evaluate clinical outcomes and perform qualitative interviews with both the patients and providers. During this process we would identify specific facilitators and barriers impacting the implementation of the model. Using the data from this initial pilot testing we would propose submitting a full scale randomized controlled trial to evaluate clinical effectiveness. The results of the trial can then contribute to a development plan within integrated healthcare settings such as the VHA.
One advantage of this model is that the BH component of the intervention can be delivered in a variety of methods that will be pragmatic and cost effective. The recent development of brief interventions for BH has demonstrated that the traditional model of a long-term commitment for therapy is not necessary for a similar result (47–50). The other advantage of this approach is that the BH component of care can be delivered in a variety of ways that may best meet the needs of the CLBP patient, such as virtual delivery of brief forms of CBT for chronic pain. In addition, the team approach will help to address some of the stigma associated with undergoing BH by reinforcement by a provider who is delivering hands on care, which is associated with high satisfaction. Another advantage of this model of care is that barriers to engaging in self-management (e.g., reluctance to engage in home walking programs) can be directly addressed by the BH provider as examples of how to use CBT skills. Increasing self-care strategies may decrease the risk of provider dependence which can be associated with hands on type treatments (51). Overall the goal of this type of coordinated management strategy is to leverage the skills and strengths of each discipline to create an improved experience for the CLBP sufferer that may have the potential to create a more durable improvement in pain and function.
Conclusion
In summary, we developed Joining Forces to address the limitations of prior combinations of multimodal treatment to date with a feasible intervention that optimizes existing resources. Joining Forces addresses several key factors not adequately addressed previously. First, Joining Forces brings together two evidence-based treatments (chiropractic care and psychological intervention) that are widely accepted in various healthcare settings. Second, this combination is novel in that it brings together a complementary and integrative health approach and conventional BH treatment. Third, these treatments share a patient-centered stance that addresses biopsychosocial factors impacting pain, the contribution of a strong working alliance between patient and provider, and treatment delivery in a similar time period (i.e., ≤12 weeks). Fourth, there is potential synergy between provider-delivered manual therapy strategies that offer timely analgesic effects while the concurrent delivery of psychological intervention that addresses the need for patient activation and skill development supporting long-term self-management. Fifth, concurrent delivery reduces total treatment time (v. sequential treatment) thereby increasing feasibility of uptake. Sixth, capitalizing on usual clinic-based chiropractic care provides an opportunity for meaningful face-to-face interactions and is augmented with delivery of psychological intervention through a patient-centered modality (in person, virtually or through an app).
A recent scoping review on the use of the BPS model in the treatment of patients with CLBP found that although there have been many papers published on this topic, there remains no consensus on the best methodology by which to implement this approach (52). The authors of this review state in their conclusion that: “Healthcare professionals should include patients’ perceptions and social questions on clinical routines once it might be potentially confounding to treatment development. In this context, a multidisciplinary team can be an excellent tool for a broader view of patient care and better use of the model. Another thing to consider is that no single healthcare provider can address all aspects of the model. Thus, implementing educational processes during professional formation and constructing teams that follow the model are ways to improve care.” We have presented a potential model of care for CLBP that utilizes a co-management approach with chiropractors and BH providers that we feel addresses the concerns of this scoping review and presents a model that can be tested in clinical settings such as the VHA where treatment teams include both BH specialists and chiropractors.
Author contributions
PD: Writing – original draft, Writing – review & editing. GB: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The information provided in this study does not represent the views of the Department of Veterans Affairs or the United States Government.
References
1. Ferreira ML, de Luca K, Haile LM, Steinmetz JD, Culbreth GT, Cross M, et al. Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. (2023) 5(6):e316–29. doi: 10.1016/S2665-9913(23)00098-X
2. Chang D, Lui A, Matsoyan A, Safaee MM, Aryan H, Ames C. Comparative review of the socioeconomic burden of lower back pain in the United States and globally. Neurospine. (2024) 21(2):487–501. doi: 10.14245/ns.2448372.186
3. Dougherty P. Can contextual factors improve clarity of the results from clinical trials of low back pain? Lancet Rheumatol. (2024) 6(1):e2–3. doi: 10.1016/S2665-9913(23)00319-3
4. Otero-Ketterer E, Peñacoba-Puente C, Pinheiro-Araujo CF, Valera-Calero JA, Ortega-Santiago R. Biopsychosocial factors for chronicity in individuals with non-specific low back pain: an Umbrella review. Int J Environ Res Public Health. (2022) 19(16):10145. doi: 10.3390/ijerph191610145
5. Sherriff B, Clark C, Killingback C, Newell D. Musculoskeletal Practitioners’ perceptions of contextual factors that may influence chronic low back pain outcomes: a modified delphi study. Chiropr Man Therap. (2023) 31(1):12. doi: 10.1186/s12998-023-00482-4
6. Vardeh D, Mannion RJ, Woolf CJ. Toward a mechanism-based approach to pain diagnosis. J Pain. (2016) 17(9):T50–69. doi: 10.1016/j.jpain.2016.03.001
7. Stevans JM, Delitto A, Khoja SS, Patterson CG, Smith CN, Schneider MJ, et al. Risk factors associated with transition from acute to chronic low back pain in US patients seeking primary care. JAMA Network Open. (2021) 4(2):e2037371. doi: 10.1001/jamanetworkopen.2020.37371
8. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. (1977) 196(4286):129–36. doi: 10.1126/science.847460
9. Darnall BD. Psychological treatment for chronic pain: improving access and integration. Psychol Sci Public Interest. (2021a) 22(2):45–51. doi: 10.1177/15291006211033612
10. Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American college of physicians. Ann Intern Med. (2017) 166(7):514–30. doi: 10.7326/M16-2367
11. Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al. Nonpharmacologic therapies for low back pain: a systematic review for an American college of physicians clinical practice guideline. Ann Intern Med. (2017) 166(7):493–505. doi: 10.7326/M16-2459
12. Keefe FJ, Main CJ, George SZ. Advancing psychologically informed practice for patients with persistent musculoskeletal pain: promise, pitfalls, and solutions. Phys Ther. (2018) 98(5):398–407. doi: 10.1093/ptj/pzy024
13. O’Keeffe M, Purtill H, Kennedy N, Conneely M, Hurley J, O'Sullivan P, et al. Comparative effectiveness of conservative interventions for nonspecific chronic spinal pain: physical, behavioral/psychologically informed, or combined? A systematic review and meta-analysis. J Pain. (2016) 17(7):755–74. doi: 10.1016/j.jpain.2016.01.473
14. Monticone M, Ferrante S, Teli M, Rocca B, Foti C, Lovi A, et al. Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial. Eur Spine J. (2014) 23(1):87–95. doi: 10.1007/s00586-013-2889-z
15. Mannion AF, Junge A, Taimela S, Müntener M, Lorenzo K, Dvorak J. Active therapy for chronic low back pain. Spine. (2001) 26(8):920–29. doi: 10.1097/00007632-200104150-00015
16. Hooff MLv, Spruit M, O’Dowd JK, van Lankveld W, Fairbank JCT, van Limbeek J. Predictive factors for successful clinical outcome 1 year after an intensive combined physical and psychological programme for chronic low back pain. Eur Spine J. (2014) 23(1):102–12. doi: 10.1007/s00586-013-2844-z
17. Foster NE, Hill JC, Hay EM. Subgrouping patients with low back pain in primary care: are we getting any better at it? Man Ther. (2011) 16(1):3–8. doi: 10.1016/j.math.2010.05.013
18. Hall AM, Ferreira PH, Maher CG, Latimer J, Ferreira ML. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Phys Ther. (2010) 90(8):1099–110. doi: 10.2522/ptj.20090245
19. Chowdhury AR, Graham PL, Schofield D, Cunich M, Nicholas M. Cost-effectiveness of multidisciplinary interventions for chronic low back pain. Clin J Pain. (2022) 38(3):197–207. doi: 10.1097/AJP.0000000000001009
20. Ford JJ, Hahne AJ. Pathoanatomy and classification of low back disorders. Man Ther. (2013) 18(2):165–68. doi: 10.1016/j.math.2012.05.007
21. Oei MW, Evens AL, Bhatt AA, Garner HW. Imaging of the aging spine. Radiol Clin North Am. (2022) 60(4):629–40. doi: 10.1016/j.rcl.2022.03.006
22. Pinto EM, Neves JR, Laranjeira M, Reis J. The importance of inflammatory biomarkers in non-specific acute and chronic low back pain: a systematic review. Eur Spine J. (2023) 32(9):3230–44. doi: 10.1007/s00586-023-07717-1
23. Li W, Gong Y, Liu J, Guo Y, Tang H, Qin S, et al. Peripheral and central pathological mechanisms of chronic low back pain: a narrative review. J Pain Res Vol. (2021) 14:1483–94. doi: 10.2147/JPR.S306280
24. Fitzcharles M-A, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Häuser W. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. (2021) 397(10289):2098–110. doi: 10.1016/S0140-6736(21)00392-5
25. Lluch E, Nijs J, De Kooning M, Van Dyck D, Vanderstraeten R, Struyf F, et al. Prevalence, incidence, localization, and pathophysiology of myofascial trigger points in patients with spinal pain: a systematic literature review. J Manipulative Physiol Ther. (2015) 38(8):587–600. doi: 10.1016/j.jmpt.2015.08.004
26. Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. (2018) 391(10137):2356–67. doi: 10.1016/S0140-6736(18)30480-X
27. Young KJ, Leboeuf-Yde C, Gorrell L, Bergström C, Evans DW, Axén I, et al. Mechanisms of manipulation: a systematic review of the literature on immediate anatomical structural or positional changes in response to manually delivered high-velocity, low-amplitude spinal manipulation. Chiropr Man Therap. (2024) 32(1):28. doi: 10.1186/s12998-024-00549-w
28. Keter DL, Bialosky JE, Brochetti K, Courtney CA, Funabashi M, Karas S, et al. The mechanisms of manual therapy: a living review of systematic, narrative, and scoping reviews. PLoS One. (2025) 20(3):e0319586. doi: 10.1371/journal.pone.0319586
29. Blanco-Giménez P, Vicente-Mampel J, Gargallo P, Baraja-Vegas L, Bautista IJ, Ros-Bernal F, et al. Clinical relevance of combined treatment with exercise in patients with chronic low back pain: a randomized controlled trial. Sci Rep. (2024) 14(1):17042. doi: 10.1038/s41598-024-68192-2
30. Beinart NA, Goodchild CE, Weinman JA, Ayis S, Godfrey EL. Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: a systematic review. Spine J. (2013) 13(12):1940–50. doi: 10.1016/j.spinee.2013.08.027
31. Newell D, Holmes MM. Patient experience and satisfaction with chiropractic care: a systematic review. J Patient Exp. (2024) 11:1–21. doi: 10.1177/23743735241302992
32. Yin C, Buchheit TE, Park JJ. Acupuncture for chronic pain. Curr Opin Anaesthesiol. (2017) 30(5):583–92. doi: 10.1097/ACO.0000000000000501
33. Fan Z, Dou B, Wang J, Wu Y, Du S, Li J, et al. Effects and mechanisms of acupuncture analgesia mediated by afferent nerves in acupoint microenvironments. Front Neurosci. (2024) 17:1–11. doi: 10.3389/fnins.2023.1239839
34. Sun M-z, Wang X, Li Y-c, Liu Y-h, Yu Y, Ren L-j, et al. Effects of acupuncture needle modification on acupuncture analgesia. J Integr Med. (2025) 23(1):66–78. doi: 10.1016/j.joim.2024.11.007
35. Zhao Z-Q. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol. (2008) 85(4):355–75. doi: 10.1016/j.pneurobio.2008.05.004
36. Cheshire A, Polley M, Peters D, Ridge D. Patient outcomes and experiences of an acupuncture and self-care service for persistent low back pain in the NHS: a mixed methods approach. BMC Complement Altern Med. (2013) 13(1):300. doi: 10.1186/1472-6882-13-300
37. Thielke SM, Fan M-Y, Sullivan M, Unützer J. Pain limits the effectiveness of collaborative care for depression. Am J Geriatr Psychiatry. (2007) 15(8):699–707. doi: 10.1097/JGP.0b013e3180325a2d
38. DeVeaugh-Geiss AM, West SL, Miller WC, Sleath B, Gaynes BN, Kroenke K. The adverse effects of comorbid pain on depression outcomes in primary care patients: results from the artist trial. Pain Med. (2010) 11(5):732–41. doi: 10.1111/j.1526-4637.2010.00830.x
39. Driscoll MA, Edwards RR, Becker WC, Kaptchuk TJ, Kerns RD. Psychological interventions for the treatment of chronic pain in adults. Psychol Sci Public Interest. (2021) 22(2):52–95. doi: 10.1177/15291006211008157
40. Williams ACdC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. (2012) 11:1–98. doi: 10.1002/14651858.CD007407.pub3
41. Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive–behavioral therapy for chronic pain. Pain. (2007) 127(3):276–86. doi: 10.1016/j.pain.2006.09.005
42. Burns JW, Day MA, Thorn BE. Is reduction in pain catastrophizing a therapeutic mechanism specific to cognitive-behavioral therapy for chronic pain? Transl Behav Med. (2012) 2(1):22–9. doi: 10.1007/s13142-011-0086-3
43. Burns JW, Nielson WR, Jensen MP, Heapy A, Czlapinski R, Kerns RD. Specific and general therapeutic mechanisms in cognitive behavioral treatment of chronic pain. J Consult Clin Psychol. (2015) 83(1):1–11. doi: 10.1037/a0037208
44. Marks R, Allegrante JP. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: implications for health education practice (part II). Health Promot Pract. (2005) 6(2):148–56. doi: 10.1177/1524839904266792
45. Beehler GP, Rodrigues AE, Mercurio-Riley D, Dunn AS. Primary care utilization among veterans with chronic musculoskeletal pain: a retrospective chart review. Pain Med. (2013) 14(7):1021–31. doi: 10.1111/pme.12126
46. Daniels CJ, Anderson DR, Cupler ZA. Coordination of care between chiropractic and behavioral health practitioners within the US department of veterans affairs health care system: a report of 3 patients with pain and mental health symptoms. J Chiropr Med. (2022) 21(1):1–8. doi: 10.1016/j.jcm.2022.01.002
47. Beehler GP, Loughran TA, King PR, Dollar KM, Murphy JL, Kearney LK, et al. Patients’ perspectives of brief cognitive behavioral therapy for chronic pain: treatment satisfaction, perceived utility, and global assessment of change. Fam Syst Health. (2021) 39(2):351–57. doi: 10.1037/fsh0000606
48. Beehler GP, Verile M, Conrad M, Moskal D. Brief behavioral intervention for chronic pain in integrated primary care: what are we waiting for? Fam Syst Health. (2024) 42(2):151–56. doi: 10.1037/fsh0000899
49. Funderburk JS, Shepardson RL, Wray J, Acker J, Beehler GP, Possemato K, et al. Behavioral medicine interventions for adult primary care settings: a review. Fam Syst Health. (2018) 36(3):368–99. doi: 10.1037/fsh0000333
50. Darnall BD. Brief interventions for chronic pain: approaches and evidence. Curr Opin Psychol. (2025) 62:101978. doi: 10.1016/j.copsyc.2024.101978
51. Vining RD, Shannon ZK, Salsbury SA, Corber L, Minkalis AL, Goertz CM. Development of a clinical decision aid for chiropractic management of common conditions causing low back pain in veterans: results of a consensus process. J Manipulative Physiol Ther. (2019) 42(9):677–93. doi: 10.1016/j.jmpt.2019.03.009
52. Almeida VC, Pereira LCD, Machado S, dos Santos Maciel LY, de Farias Neto JP, de Santana Filho VJ. The use of a biopsychosocial model in the treatment of patients with chronic. Patient Educ Couns. (2024) 121:108117. doi: 10.1016/j.pec.2023.108117
53. Mu J, Furlan AD, Lam WY, Hsu MY, Ning Z, Lao L. Acupuncture for chronic nonspecific low back pain. Cochrane Database Syst Rev. (2020) 2020:12. doi: 10.1002/14651858.CD013814
54. Rubinstein SM, de Zoete A, van Middelkoop M, Assendelft WJJ, de Boer MR, van Tulder MW. Benefits and Harms of spinal manipulative therapy for the treatment of chronic low back pain: systematic review and meta-analysis of randomised controlled trials. Br Med J. (2019) 689:l689. doi: 10.1136/bmj.l689
55. Roseen EJ, Joyce C, Winbush S, Pavco-Luttschwager N, Morone NE, Saper RB, et al. Primary care barriers and facilitators to nonpharmacologic treatments for low back pain: a qualitative pilot study. PM&R. (2024):1–12. doi: 10.1002/pmrj.13183
56. Rhon DI, Deyle GD. Manual therapy: always a passive treatment? J Orthop Sports Phys Ther. (2021) 51(10):474–77. doi: 10.2519/jospt.2021.10330
57. Ho EK-Y, Chen L, Simic M, Ashton-James CE, Comachio J, Wang DXM, et al. Psychological interventions for chronic, non-specific low back pain: systematic review with network meta-analysis. Br Med J. (2022) 376:e067718. doi: 10.1136/bmj-2021-067718
58. Moreno-Ligero M, Moral-Munoz JA, Salazar A, Failde I. MHealth intervention for improving pain, quality of life, and functional disability in patients with chronic pain: systematic review. JMIR Mhealth Uhealth. (2023) 11:e40844. doi: 10.2196/40844
59. Barnet-Hepples T, Dario A, Oliveira J, Maher C, Tiedemann A, Amorim A. Health coaching improves physical activity, disability and pain in adults with chronic non-cancer pain: a systematic review. J Physiother. (2024) 70(2):115–23. doi: 10.1016/j.jphys.2024.01.001
60. Arnold T, Haubrick KK, Klasko-Foster LB, Rogers BG, Barnett A, Ramirez- Sanchez NA, et al. Acceptance and commitment therapy informed behavioral health interventions delivered by non-mental health professionals: a systematic review. J Contextual Behav Sci. (2022) 24:185–96. doi: 10.1016/j.jcbs.2022.05.005
Keywords: chronic lower back pain, chiropractic, behavioral health, biopsychosocial (BPS) model, multimodal care
Citation: Dougherty P and Beehler G (2025) Biopsychosocial management of chronic lower back pain: the role of manual therapy and behavioral health co-management. Front. Musculoskelet. Disord. 3:1646096. doi: 10.3389/fmscd.2025.1646096
Received: 12 June 2025; Accepted: 15 July 2025;
Published: 1 August 2025.
Edited by:
Maryse Fortin, Concordia University, CanadaReviewed by:
Yuehui Zhang, Shanghai Jiao Tong University, ChinaCopyright: © 2025 Dougherty and Beehler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paul Dougherty, cGF1bC5kb3VnaGVydHlAdmEuZ292
 Paul Dougherty
Paul Dougherty Gregory Beehler
Gregory Beehler