- 1Department of Neurosurgery, 21 September University for Medical and Applied Sciences, Sana’a, Yemen
- 2Department of Neurosurgery, Sana’a university, Sana’a, Yemen
Background: Musculoskeletal disorders, particularly cervical and low back pain (CLBP), are leading causes of disability worldwide. However, evidence from conflict-affected and low-resource regions such as Yemen remains scarce. This study aimed to determine the prevalence, associated risk factors, and radiological patterns of CLBP among women attending a tertiary hospital in Sana'a, Yemen.
Methods: A hospital-based cross-sectional study was conducted among 470 adult female patients at Al-Gumhori Teaching Hospital, Sana'a, from January to March 2025. Participants completed structured questionnaires covering sociodemographic characteristics, lifestyle behaviors, psychological stress, and musculoskeletal symptoms. CLBP was defined according to European Guidelines as non-traumatic spinal pain persisting ≥12 weeks. Radiological assessments (x-ray and MRI) were performed in clinically indicated cases. Multivariable logistic regression identified independent factors associated with CLBP.
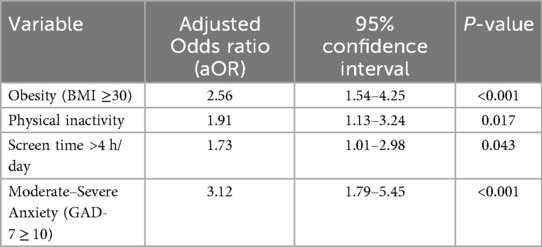
Results: The prevalence of cervical and/or low back pain was 69.4% (95% CI: 65.2–73.3). Independent factors associated with CLBP included obesity (aOR = 2.56; 95% CI: 1.54–4.25), physical inactivity (aOR = 1.91; 95% CI: 1.13–3.24), prolonged screen time >4 h/day (aOR = 1.73; 95% CI: 1.01–2.98), and moderate-to-severe anxiety symptoms (aOR = 3.12; 95% CI: 1.79–5.45). Radiological findings revealed cervical muscle spasm in 62%, vertebral osteophytosis in 33%, and lumbar disc prolapse in 28%.
Conclusion: CLBP is highly prevalent among Yemeni women, with multiple modifiable risk factors linked to lifestyle and psychological distress. Targeted, integrated public health strategies are urgently needed to reduce musculoskeletal disability among women in conflict-affected regions.
1 Introduction
Musculoskeletal disorders (MSDs) are among the most common causes of chronic disability globally, particularly affecting women in low-resource and conflict-affected settings. Cervical and low back pain (CLBP) contribute substantially to years lived with disability and lost productivity. Despite extensive research in developed countries, data from conflict zones such as Yemen remain scarce.
The ongoing humanitarian crisis in Yemen has intensified psychosocial stress, disrupted healthcare access, and altered daily activity patterns—factors that may amplify musculoskeletal burden. Women in Yemen, often balancing physical labor with caregiving responsibilities, are especially vulnerable to both physical strain and emotional stress.
This study aimed to estimate the prevalence of CLBP among women in Sana'a, identify associated sociodemographic, lifestyle, and psychological factors, and assess radiological findings to provide evidence for preventive and therapeutic interventions.
2 Methods
2.1 Study design and setting
A hospital-based cross-sectional study was conducted at Al-Gumhori Teaching Hospital, one of the largest tertiary referral centers in Sana'a, Yemen, between January 1 and March 30, 2025.
2.2 Ethical approval
Ethical clearance was obtained from the Institutional Review Board of 21 September University for Medical and Applied Sciences (IRB Approval No: 100001644). Written informed consent was obtained from all participants.
2.3 Participants
Eligible participants were female patients aged ≥18 years attending outpatient clinics for non-emergency complaints.
2.3.1 Exclusion criteria
• Recent spinal or major trauma
• Diagnosed spinal tumors or infections
• Neurological deficits suggesting systemic pathology
2.4 Sampling
A systematic convenience sampling approach was applied to recruit consecutive eligible women during the study period until the target sample size (n = 470) was reached. This hospital receives referrals from multiple districts, making the sample representative of the urban female population in conflict-affected Sana'a.
2.5 Measurement and definitions
Data were collected via structured face-to-face interviews using a validated questionnaire covering:
• Sociodemographics: age, marital status, education, occupation
• Anthropometrics: height, weight, BMI (classified per WHO)
• Lifestyle: physical activity, sedentary time, daily screen use
• Psychological stress: assessed by GAD-7 scale (categorized as none <5, mild 5–9, moderate–severe ≥10)
• Musculoskeletal pain: assessed by Visual Analog Scale (VAS) and duration ≥12 weeks
2.6 Radiological evaluation
Plain x-rays were performed for all participants presenting with moderate-to-severe or chronic pain (>3 months). MRI was ordered for those with neurological symptoms or red flags. All imaging was interpreted by a senior radiologist blinded to clinical data, following standardized diagnostic criteria for osteophytosis, disc prolapse, and muscle spasm.
2.7 Statistical analysis
Data were analyzed using SPSS version 26.
• Descriptive statistics summarized participant characteristics.
• Univariate associations were tested using chi-square and t-tests.
• Variables with p < 0.10 were included in a multivariable logistic regression model.
• Model fit was verified using the Hosmer–Lemeshow test (p > 0.05 indicates good fit), and multicollinearity was checked (VIF < 2).
• A p-value < 0.05 was considered statistically significant.
3 Results
3.1 Participant characteristics
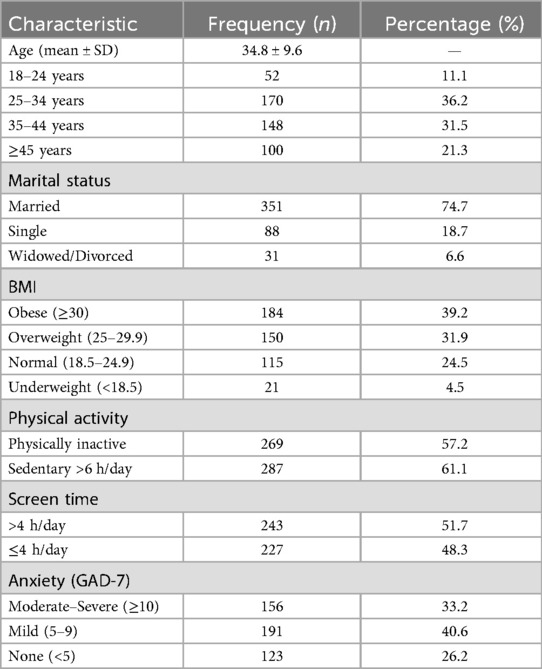
A total of 470 women were included (mean age 34.8 ± 9.6 years). Sociodemographic and behavioral characteristics are shown below.
3.1.1 Analytical comment
Most participants were overweight or obese, physically inactive, and had high daily screen exposure. One-third demonstrated moderate-to-severe anxiety symptoms, indicating a high psychosocial burden among women in this population.
3.2 Prevalence and risk factors
The overall prevalence of cervical and/or low back pain was 69.4% (95% CI: 65.2–73.3) (see Tables 1, 2).
• Cervical pain only: 29.1%
• Lumbar pain only: 24.7%
• Both sites: 15.6%
3.2.1 Analytical comment
Anxiety and obesity showed the strongest associations with CLBP, suggesting a biopsychosocial interaction where both mental and physical factors contribute significantly to pain persistence.
3.3 Radiological findings (n = 420)
• Cervical muscle spasm: 62%
• Vertebral osteophytosis: 33%
• Lumbar disc prolapse: 28%
• Normal imaging: 12%
3.3.1 Analytical comment
Radiological abnormalities confirmed the clinical diagnosis in most cases. The predominance of muscular spasm highlights chronic strain rather than acute injury as the primary mechanism.
4 Discussion
This study provides important evidence on the high prevalence and multifactorial nature of cervical and low back pain (CLBP) among women in conflict-affected Yemen. The overall prevalence of 69.4% observed in this study aligns with regional estimates from low- and middle-income countries in the Middle East and North Africa (MENA), where musculoskeletal disorders (MSDs) represent a growing cause of disability (1). The findings confirm that women in fragile contexts experience a disproportionate burden of musculoskeletal pain due to combined physical, psychosocial, and socioeconomic pressures.
Our results identified obesity, physical inactivity, prolonged screen time, and anxiety as significant correlates of CLBP. These associations reflect a biopsychosocial model in which both physical and psychological determinants contribute to chronic pain persistence. Similar risk factors were reported in Syrian and Iraqi studies, where obesity and anxiety symptoms were independently linked with chronic spinal pain (2–4). Furthermore, comparable epidemiological patterns have been documented in recent analyses of musculoskeletal conditions across the Middle East, highlighting sedentary lifestyles, poor ergonomics, and stress exposure as shared contributors (1, 5).
Conflict-related disruptions play an essential role in shaping these risk profiles. Evidence from Syria demonstrates that ongoing conflict limits healthcare access, reduces physical activity, and heightens psychological distress—factors that collectively increase chronic pain prevalence [2,4]. Among displaced and refugee populations, chronic pain syndromes are further aggravated by prolonged stress, inadequate rehabilitation, and restricted access to pain management services (6). Yemen shares these contextual vulnerabilities, where healthcare infrastructure damage and economic instability likely exacerbate musculoskeletal morbidity among women.
The strong link between anxiety and CLBP observed in this study is consistent with prior research demonstrating that psychological distress amplifies both pain perception and disability (7). Chronic stress may alter central pain processing pathways, leading to increased muscular tension and prolonged recovery times. This underscores the need to incorporate mental health assessment and stress management strategies into musculoskeletal care programs in conflict-affected regions.
Radiological findings in this study—particularly cervical muscle spasm and vertebral osteophytosis—support the predominance of chronic strain rather than acute trauma as the underlying mechanism of pain. Similar radiological patterns have been described in studies from low-resource environments, where occupational load, domestic labor, and inadequate postural ergonomics are common (4, 5). Addressing these factors through ergonomic education and workplace awareness campaigns may substantially reduce musculoskeletal pain incidence.
Despite its valuable insights, this study has several limitations. The cross-sectional design restricts causal inference, and being single-center may limit generalizability beyond urban women in Sana'a. Selective imaging could have biased radiological prevalence estimates. Additionally, self-reported behavioral and psychological data are prone to recall bias. Nevertheless, the combination of clinical assessment, imaging, and psychological screening enhances the internal validity of the findings.
In summary, the present study adds to the limited body of literature on musculoskeletal pain in conflict-affected settings and emphasizes the interplay between physical, mental, and environmental determinants of health. Integrating public health interventions targeting physical activity, ergonomic behavior, weight management, and psychological resilience could substantially mitigate the musculoskeletal burden among women in Yemen and comparable regions.
5 Conclusion
Cervical and low back pain are highly prevalent and disabling among women in Yemen, driven by modifiable lifestyle and psychological factors. Integrated, gender-sensitive public health strategies addressing physical inactivity, ergonomic habits, and mental well-being are essential to mitigate the burden of musculoskeletal pain in conflict-affected settings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
This study was conducted in accordance with the ethical standards of the Declaration of Helsinki. Ethical approval was obtained from the Institutional Review Board (IRB) of 21 September University for Medical and Applied Sciences, Sana'a, Yemen (Approval No: [100001644]). Written informed consent was obtained from all participants prior to enrollment.
Author contributions
HM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MB: Funding acquisition, Writing – review & editing.
Funding
The author(s) declare no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors thank the participants and the Radiology Department staff at Al-Gumhori Teaching Hospital for their cooperation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Al-Ajlouni YA, Al Ta’ani O, Mushasha R, Lee JL, Capoor J, Kapadia MR, et al. The burden of musculoskeletal disorders in the Middle East: and North Africa (MENA) region: a longitudinal analysis from the global burden of disease dataset 1990–2019. BMC Musculoskelet Disord. (2023) 24(1):439. doi: 10.1186/s12891-023-06556-x
2. Zakaria W, Ibrahim Y. Rheumatic diseases amidst conflict in northwest Syria: unveiling health challenges and implications. Avicenna J Med. (2024) 14(02):115–22. doi: 10.1055/s-0044-1786826
3. Khadour FA, Khadour YA, Alhatem W, Albarroush D, Halwani AZ, Goirge MM, et al. Risk factors of chronic low back pain among Syrian patients: across-sectional study. BMC Neurol. (2025) 25(1):146. doi: 10.1186/s12883-025-04158-9
4. Al-Bakri SHM, Al-Shuwaili SJ, Ataimish HHJ. The prevalence and risk factors of lower back pain among adult populations in Iraq. Rom J Rheumatol. (2024) 33:11–4. doi: 10.37897/RJR.2024.1.4
5. Behairy M, Odeh S, Alsourani J, Talic M, Alnachef S, Qazi S, et al. Prevalence of lower back pain (LBP) and its associated risk factors among Alfaisal University medical students in Riyadh, Saudi Arabia: a cross-sectional study. Healthcare. (2025) 13:1490. doi: 10.3390/healthcare13131490
6. Standnes MB, Haukenes I, Lunde A, Diaz E. Chronic pain and use of painkillers, healthcare services and long-term impairment among Syrian refugees. BMC Public Health. (2024) 24(1):2815. doi: 10.1186/s12889-024-20266-6
7. Gerdle B, Dragioti E, Rivano Fischer M, Ringqvist Å. Pain intensity and psychological distress show different associations with interference and lack of life control: a clinical registry-based cohort study of >40,000 chronic pain patients from SQRP. Front Pain Res (Lausanne). (2023) 4:1093002. doi: 10.3389/fpain.2023.1093002
Keywords: cervical pain, low back pain, Yemen, musculoskeletal disorders, radiology, women's health, public health
Citation: Muafa HM and Balkam MA (2025) The hidden burden of cervical and low back pain among women in conflict-affected Yemen. Front. Musculoskelet. Disord. 3:1673096. doi: 10.3389/fmscd.2025.1673096
Received: 25 July 2025; Accepted: 6 November 2025;
Published: 13 November 2025.
Edited by:
Oleksandr P Romanchuk, Lesya Ukrainka Volyn National University, UkraineReviewed by:
Elias Alberto Bedoya Marrugo, Fundación Universitaria Tecnológico de Comfenalco (COMFENALCO), ColombiaKrupa Tank, RK University, India
Copyright: © 2025 Muafa and Balkam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hussein Mussa Muafa, aC5tLm11YWZhQDIxdW1hcy5lZHUueWU=
 Hussein Mussa Muafa
Hussein Mussa Muafa Malika Abdu Balkam2
Malika Abdu Balkam2