- 1Department of Biological Sciences, Rutgers University, Newark, NJ, United States
- 2Department of Chemical Biology, Ernest Mario School of Pharmacy, Rutgers University, Piscataway, NJ, United States
- 3Rutgers Cancer Institute of New Jersey, New Brunswick, NJ, United States
- 4Department of Pathology, Princeton Medical Center, Plainsboro, NJ, United States
Paneth cells are residents of the intestinal epithelium. Abnormal appearance of Paneth cells has been widely documented in non-intestinal tissues within the digestive tract and even observed in non-gastrointestinal organs. Although metaplastic Paneth cells are part of the overarching pathology of intestinal metaplasia (IM), only a fraction of intestinal metaplastic lesions contain Paneth cells. We survey literature documenting metaplastic Paneth cells to gain insights into mechanism underlying their etiologic development as well as their potential relevance to human health. A synthesized view from this study suggests that the emergence of metaplastic Paneth cells at extra-intestinal mucosal sites likely represents a protective, anti-bacterial, and inflammatory response evoked by an altered microbial activity.
Introduction
Paneth cells are a group of mature intestinal epithelial cells present in humans and other mammals. They are primarily localized at the base of the crypts of Lieberkühn in the small intestine. These cells were first described by Schwalbe (1872) and later fully characterized by Josef Paneth (1888). Normal Paneth cells differentiate from intestinal stem cells and live for about 60 days (Ireland et al., 2005). Paneth cells can be found in human cecum and ascending colon but are extremely rare in human distal colon and are absent in rodent colonic epithelium (Tanaka et al., 2001). Conventional histological examination identifies Paneth cells as large columnar epithelial cells with characteristic eosinophilic secretory granules densely packed in the cytoplasm. In addition to secretion of growth factors (e.g., Wnt and EGF ligands) (Clevers and Bevins, 2013) to maintain the intestinal stem cell niche (Clevers and Bevins, 2013), Paneth cells secrete numerous antimicrobial peptides (e.g., α-defensins, lysozyme, Reg3A, etc.) (Bevins and Salzman, 2011) to regulate mucosal immune response.
Loss or reduction of Paneth cells are found in ileal Crohn’s disease (Wehkamp et al., 2005; Perminow et al., 2010; Adolph et al., 2013), intestinal ischemia (Grootjans et al., 2011), necrotizing enterocolitis (McElroy et al., 2013), pathogenic bacterial infection (Zhang et al., 2012; Conway et al., 2013; White et al., 2017), and graft vs. host disease (Fishbein et al., 2008; Levine et al., 2013; Kroemer et al., 2016). In contrast, abnormal appearance of Paneth cells in other parts of the gastrointestinal and extra-gastrointestinal region is referred to as Paneth cell metaplasia (PCM). Abundant appearance of Paneth cells in the human distal colons have been extensively documented in literatures published on ulcerative colitis (Tanaka et al., 2001; Bedini et al., 2014; Simmonds et al., 2014), Crohn’s disease (Tanaka et al., 2001; Simmonds et al., 2014), and colonic tubular adenoma (Symonds, 1974; Wada et al., 2005; Shi, 2007; Wehkamp and Stange, 2010; Wang et al., 2011a; Mahon et al., 2016). Although these Paneth cell alterations are frequently associated with chronic inflammation, the molecular mechanism and significance of Paneth cell-related pathologies are poorly understood.
Intestinal metaplasia (IM) represents a gastrointestinal pathological condition and is defined as an abnormal presence of intestinal epithelial cells in non-intestinal tissues. Although not all IM contain Paneth cells, metaplastic Paneth cells have been widely reported in diseased upper alimentary tissues such as Barrett’s esophagus (BE) (Chen et al., 2015), chronic gastritis (Montero and Loizaga, 1971; Lewin et al., 1976; Rubio et al., 1987; Deveci and Deveci, 2004; Shen et al., 2005), and Brunner’s gland (Coutinho et al., 1996). Surprisingly, rare metaplastic Paneth cells were even observed in other gastrointestinal and non-gastrointestinal tissues (Symonds, 1974; Tanaka et al., 2001; Mitsuhashi et al., 2005; Puiman et al., 2011; Gassler, 2017). In addition to briefly summarizing the well-studied PCM in the left colon, which represents a hallmark change in idiopathic inflammatory bowel disease (IBD), this review will analyze literature on metaplastic Paneth cells in upper gastrointestinal or non-gastrointestinal tissues, an area of research that has received little attention. We noted a potential correlation between bacterial activity and the etiologic development of metaplastic Paneth cells within these extra-intestinal mucosal niche.
Metaplastic Paneth Cells in Colon and Its Disease Relevance
Paneth cells are normally present in proximal (right and transverse) colons in human but are extremely rare in the distal (left) colon. Detection of Paneth cells in the left colon were referred to as PCM, and documented in many IBD studies (Lewin, 1969; Bansal et al., 1984; Ajioka et al., 2005; Simmonds et al., 2014). In addition, PCM in other colonic inflammation conditions such as diverticulitis (Sandow and Whitehead, 1979) and radiation colitis (Watanabe, 1978) had also been reported. However, the histogenesis of colonic PCM is not fully understood. Metaplastic Paneth cells in IBD colon were usually found in crypt regions and morphologically identical to normal Paneth cells that reside in the small intestines (Cunliffe et al., 2001). Immuno-histochemical studies indicated that colonic metaplastic Paneth cells expressed antimicrobial peptides: lysozyme (Klockars et al., 1977), sPLA2 (Haapamaki et al., 1997), and α-defensins (Cunliffe et al., 2001). Normal colonic mucosa does not express human alpha defensin 5 (HD5; antimicrobial protein produced by Paneth cells). However, HD5 was detected in colonic crypts of IBD patients’ samples, consistent with the occurrence of PCM (Cunliffe et al., 2001).
By reporting significantly higher PCM incidences in the distal colon of IBD patients compared to non-IBD and control patients, Tanaka et al. (2001) proposed an association of colonic Paneth cells with IBD. Regression analysis suggested that repair and regeneration might be the most potent stimuli causing PCM (Tanaka et al., 2001). Moreover, Paneth cells can sense commensal microbiota (Vaishnava et al., 2008) and shape the microbiome (Salzman et al., 2010) to maintain the intestinal homeostasis. Therefore, the presence of PCM could be an adaptive response to protect the damaged colonic epithelium against bacterial invasion. Additionally, Wehkamp et al. (2007) suggested that the antibacterial peptides produced by Paneth cells might counteract bacterial attack as an “on-demand” mechanism.
The detection of Paneth cells in colorectal adenomas was reported as early as 1967 (Gibbs, 1967) and the reported frequencies of such detection varied from 0.2 to 39% in different studies (Bansal et al., 1984; Wada et al., 1994, 2005; Joo et al., 2009; Pai et al., 2013; Mahon et al., 2016). Furthermore, Paneth cells not only produce antimicrobial components but also constitute an important epithelial niche for small intestinal stem cells by producing epithelial growth factor (EGF), transforming growth factor (TGF-α), Wnt3, and Notch ligands (Sato et al., 2011). The IBD patients have an increased risk to develop inflammation-associated colon cancer. Additionally, during repair and regeneration of damaged epithelium in IBD patients, there might be an increased chance of mutation accumulation (cyclic hit model, described in later paragraphs), and the metaplastic Paneth cells may contribute to accelerated epithelial tumorigenesis by providing stem cell growth factor to tumor cells (Chen and Huang, 2014).
Metaplastic Paneth Cells in Gastric Mucosa and Its Disease Relevance
Intestinal metaplasia in human stomach was first reported by Morson (1955) and later recognized as a precursor for gastric cancer in various studies (Morson, 1955; Ming et al., 1967; Matsukura et al., 1979; Segura and Montero, 1983; Shimada et al., 1987). Kawachi et al. (1976) used Tes Tape method to characterize IM by disaccharidase visualization and classified the lesions into two types. In type I IM, also known as the complete IM, goblet cells, Paneth cells, as well as enterocyte enzymes, including sucrase, maltase, trehalase and alkaline phosphatase were present. In type II, the incomplete form of IM, trehalase, alkaline phosphatase, and Paneth cells were absent. Thus, complete metaplasia partially resembles small intestinal epithelium containing Paneth cells whereas incomplete metaplasia resembles colonic epithelium lacking Paneth cells. In their study, out of 96 samples of IM, 57% showed type I IM with the presence of Paneth cells, while 43% were type II lacking Paneth cells (Kawachi et al., 1976).
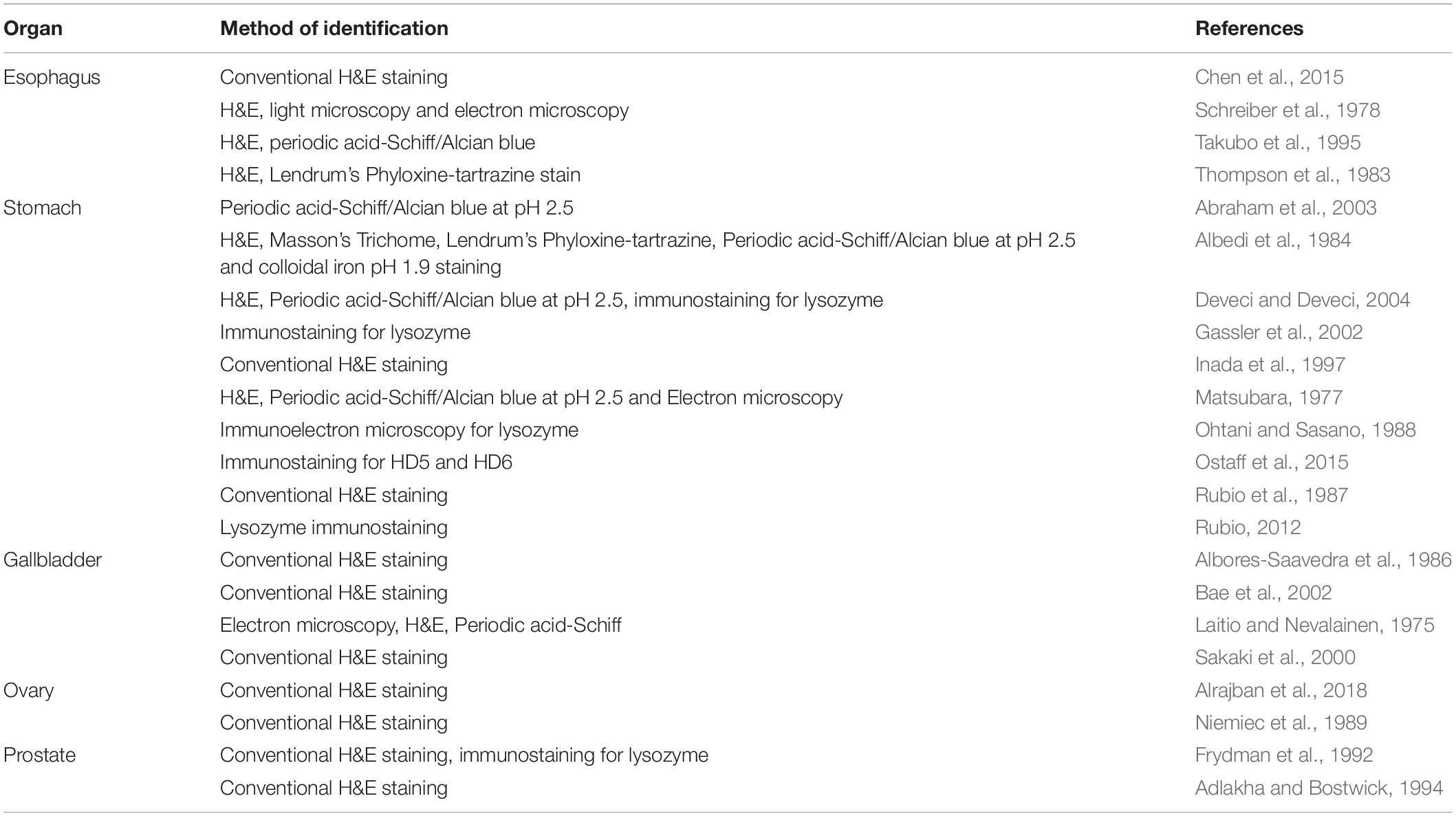
By using various staining procedures (Table 1), Albedi et al. (1984) reported that immature Paneth cells were present in less differentiated IM. Other authors also confirmed the presence of PCM by immunostaining for PSTI (Pancreatic secretory trypsin inhibitor) (Kazal et al., 1948; Bohe et al., 1986, 1987), lysozyme (Heitz and Wegmann, 1980), and human defensin 5 (Shen et al., 2005). Additionally, Paneth-like cells were reported in gastric adenomas and carcinomas (Heitz and Wegmann, 1980; Ito et al., 1986; Caruso et al., 1989; Rubio, 1989). Although some of these tumors exhibited aggressiveness (Ohtani and Sasano, 1988), the prognostic value of these Paneth-like cells for gastric carcinoma remain unclear.
Inada et al. (1997) further classified gastric IM on the basis of differentiation status into two major classes (i) gastric and intestinal (GI) mixed type; and (ii) solely intestinal (I) type. Six subclasses were further established for the mixed GI type. In this study, they observed the presence and absence of Paneth cells in IM at almost the same incidence rate i.e., 15 and 17%, respectively in fundic mucosa. The incidences of intestinal subtypes with Paneth cells were 17% in fundic and 19% in pyloric mucosa, respectively. The incidences of GI(Su-Pa+) subtypes which are characterized as showing presence of Paneth cells (Pa) and absence of surface mucous cells (Su) were 11% in fundic and 14% in pyloric mucosa (Inada et al., 1997). Within these metaplastic lesions, the presence of Paneth cells near the proliferative zone and the large intracellular granules suggested that these cells were neither chief cells nor pyloric gland cells (Inada et al., 1997).
Matsubara performed morphological characterizations of Paneth cells and reported that Paneth cells in normal small intestinal epithelia contained more phagolysosomes in lower cytoplasm compared to Paneth cells found in IM (Matsubara, 1977). This represented one of the earliest attempts to distinguish intestinal resident cells vs. metaplastic Paneth cells. Gassler et al. (2002) later reported that the expression of calnexin was inversely related to secretory lysozyme in Paneth cells of normal intestinal mucosa but became directly correlated to lysozyme in metaplastic Paneth cells in gastric mucosa. They further identified the expression of proliferative marker Ki67 in metaplastic Paneth cells but not in Paneth cells of normal small intestines. These studies suggested that metaplastic Paneth cells may behave differently from normal Paneth cells (Gassler et al., 2002). However, detailed information at the molecular level is currently absent to distinguish normal from metaplastic Paneth cells.
Most human gastric cancers arise after long-term Helicobacter pylori infection via progression of metaplastic changes, first named by Correa (Correa, 1992; Correa and Shiao, 1994; Uemura et al., 2001) with the first metaplastic change that increases risk for progression to cancer being atrophic gastritis, involving loss of acid secreting parietal cells with concomitant pseudopyloric metaplasia (aka SPEM, discussed below) of the remaining cells. Some authors believe IM is a requisite step after atrophy (Correa’s hypothesis), whereas others like David Graham (Graham et al., 2019) have suggested IM is more of a reparative lesion, not directly related to carcinogenesis, and atrophy is the more diagnostic risk factor (El-Zimaity et al., 2002). In gastric atrophy, caused by long-term H. pylori colonization, mature chief cells that are present at the base of glands are replaced by (metaplastic) cell types that co-express both the chief cell marker and markers of normal mucus-secreting cells residing in the gland neck, such as Trefoil Factor 2, TFF2 (spasmolytic polypeptide). This type of metaplasia was also known as spasmolytic polypeptide-expressing metaplasia (SPEM) or pseudopyloric metaplasia due to the lack of mature chief and parietal cells, resembling antrum or pyloric epithelium (Goldenring et al., 2011; Saenz and Mills, 2018). During SPEM, the differentiated cells change their fate to a regenerative state by first shutting down the mTORC1 signaling followed by expression of progenitor markers to reactivate mTORC1. This process was named as paligenosis (Jin and Mills, 2018; Willet et al., 2018). In mouse models, SPEM emerged in chronically inflamed stomach and clearly proceeded to give rise to gastric cancer (Fox et al., 1996). Inflammation due to infection or other insults increases paligenotic events. This continuous process of paligenosis increases the risk of accumulation of mutations leading to emergence of a neoplastic or dysplastic clone. This phenomenon was called “cyclical hit model” (Burclaff and Mills, 2018; Saenz and Mills, 2018; Jin and Mills, 2019). Although there is no study that has explicitly studied how Paneth cells originated during the process of metaplasia, a recent study by Leushacke et al. (2017) showed LGR5+ subpopulation of chief cells co-expressed intestinal stem cell and Wnt markers in advanced intestinal type tumors in the corpus. Therefore, metaplastic Paneth cells could be part of the program of IM, the origin of which may relate to infection and inflammation but remain poorly understood.
Although the relevance of metaplastic Paneth cells during gastric mucosal pathogenesis are not clear, the characteristic production of antimicrobial peptides by Paneth cells suggested that the metaplasia might be an adaptive response to bacterial infection. Paneth cells secrete defensins and lysozyme shown to reduce the colonization of H. pylori in the stomach (Tanabe et al., 2008). Interestingly, mucosal areas with IM or with pseudo-pyloric metaplasia showed a lack of H. pylori, suggesting presence of Paneth cells in the metaplastic mucosa may be an adaptation against bacterial infection (Rubio, 2015). Gastric atrophy is characterized by the loss of chief and parietal cells and during infection this atrophy progresses from antrum to corpus (Kimura et al., 1996; Shichijo et al., 2015). As H. pylori infection is associated with IM and a higher risk of cancer, attempts were made to reduce the infection (Fukase et al., 2008; Ogura et al., 2008; Sakitani et al., 2011; Shichijo et al., 2016). Some studies reported that IM did not seem alleviated even after eradication of H. pylori infection, suggesting the potentially irreversible nature of IM (Wang et al., 2011b; Kodama et al., 2012; Mera et al., 2018). However, other studies showed that eradication of H. pylori somewhat reduced the IM (Correa et al., 2000; Zullo et al., 2000; Kong et al., 2014). In addition, Paneth cell antimicrobial peptides, especially human defensin 5 and 6, were recently found upregulated in gastric mucosa of heavy alcohol users (Ostaff et al., 2015). Thus, IM in gastric mucosa might also be caused by non-bacterial factors such as excessive alcohol use, retrograde bile reflux, aspirin, and anti-inflammatory drugs (Webb et al., 1996; Bresalier, 1998). However, these changes may also indirectly alter the gastric colonization of H. pylori or other bacterial species. More studies are required to elucidate these causal relationships.
Metaplastic Paneth Cells in Esophageal Mucosa and Disease Relevance
The presence of Paneth cells in BE was first described by Schreiber et al. (1978), when metaplastic Paneth cells similar to intestinal resident Paneth cells were detected in BE biopsy samples from 4 patients. BE is characterized by a single layer of columnar epithelium replacing the native multi-layered stratified squamous epithelium of distal esophagus. BE is considered as a form of protective adaption from chronic insults, secondary to gastroesophageal reflux disease (Burgess et al., 1971; Naef et al., 1975; Ozzello et al., 1977), and the precursor to most esophageal adenocarcinomas. This esophageal disorder is pathologically manifested by the presence of multiple intestinal epithelial cell lineages including Paneth cells and enteroendocrine cells along with gastric cells (Boulton et al., 2003).
Later, Thompson et al. (1983) exhibited the presence of Paneth cells in 50% of the esophagogastrectomy samples of Barrett’s metaplasia and specimens with adenocarcinoma at the gastroesophageal junction. No difference in sex ratio or age range was observed among the samples associated with or without metaplasia. Compared to earlier studies using biopsy samples, sampling error was minimized in this study using esophagogastrectomy. Moreover, various experimental approaches including scanning electron microscopy, specimen radiography, and dissecting microscopy along with regular histochemical techniques were used in this study in comparison to earlier studies that mainly relied on histologic analysis.
In the last decade, immunostaining for various antimicrobial peptides was used to identify Paneth cells. Shen et al. (2005) reported human defensin 5 immunostaining as a tool for identification of IM in BE as well as in gastric IM. Under normal conditions, human defensin 5 is present in intestinal Paneth cells, and is generally confined to the small intestinal epithelium. However, the expression of defensin 5 was also observed in IM. The frequency of human defensin 5 staining was higher in gastric IM compared to BE. This difference was attributed to higher H. pyloric infection in stomach compared to esophagus (Shen et al., 2005).
Rubio also reported the presence of PCM in BE by detecting expression of lysozyme and other Paneth cell-specific antimicrobial proteins (Rubio, 2012). In a recent study, Chen et al. (2015) conducted a large study on 757 esophageal biopsy specimens, and reported that 31% of this cohort with IM contained metaplastic Paneth cells. These results were in accordance with previous reports showing a similar frequency of PCM in BE (Schreiber et al., 1978; Thompson et al., 1983; Takubo et al., 1995). Moreover, the highest incidence of PCM in BE was observed in indefinite dysplasia and low grade dysplasia samples. Additionally, in their follow-up study, they showed PCM was associated with reduced disease regression and suggested it as a potential marker for identification of severe disease (Chen et al., 2015). Moreover, presence of metaplastic Paneth cell products such as antimicrobial peptides may accelerate the cascade of BE by altering the expression of E-cadherin, thereby reducing the cell-cell interaction (Nomura et al., 2013).
Similar to gastric IM, BE was also viewed as an adaptation following chronic inflammation or injury to the esophageal epithelium. Bile acid was reported as one of the major contributor to the development of BE in animal models (Clark et al., 1994; Quante et al., 2012). Patients with gastroesophageal reflux disease often received proton pump inhibitors, which could cause reduced gastric acid secretion leading to bacterial overgrowth in BE. Additionally, it was reported that BE biopsies were highly associated with presence of bacteria compared to esophageal biopsies without BE (Osias et al., 2004). Two different types of microbiome were observed in esophageal biopsies: type I was dominated by genus Streptococcus and present with phenotypically normal esophagus; and type II contained Gram-negative anaerobes that were correlated with BE (Yang et al., 2009). Other studies also reported the presence of residential bacterial population in gastroesophageal reflux disease and BE. One study showed the presence of Bacteroidetes, Firmicutes, Proteobacteria, and Actinobacteria (Pei et al., 2005), while the other reported 46 bacterial species including high levels of Campylobacter consisus and Campylobacter rectus (Macfarlane et al., 2007). Liu et al. (2013) also observed Firmicutes, Proteobacteria, Bacteroides, Fusobacterium, and Actinobacter in 6 cases of BE. These studies suggested a potential rational toward a self defense mechanism against pathogenic bacteria. Therefore, presence of metaplastic Paneth-like cells in these lesions may represent an adaptive antibacterial response by the infected mucosa. However, besides an antibacterial role, defensins were also proposed to reduce E-cadherin in esophageal epithelium to possibly accelerate the BE pathogenesis (Nomura et al., 2013).
Appearance of Paneth Cells in Other Gastrointestinal and Non-gastrointestinal Organs
Intestinal metaplasia has also been observed in several other gastrointestinal tissues. Although IM in gallbladder is very rare, complete IM was reported in gallbladder as early as 1967 (Jarvi and Lauren, 1967). Laitio and Nevalainen (1975) studied 100 gallbladders following cholecystectomies to remove gallstones. One specimen showed the presence of Paneth cells. Electron microscopy of this sample showed Paneth cells in columnar shape with apical cytoplasm occupied by secretory granules and well-developed Golgi apparatus. Later, Albores-Saavedra et al. (1986) reported that 3 out of 49 gallbladder samples showed the presence of Paneth cells. The presence of similar morphology in the IM in gallbladder to those in the stomach suggested that gastric and gallbladder epithelia have the same potential to differentiate into similar cell lineages. Although the IM of gallbladder containing Paneth cells was suspected to be associated with carcinoma development, the presence of higher immunoreactivity of lysozyme in non-dysplastic mucosa than in carcinoma did not support the hypothesis. Furthermore, the frequency of observing Paneth cells was found to be lowest in gallbladder cancer tissues compared to non-neoplastic mucosa, suggesting an inverse correlation of PCM to gallbladder cancer (Yamamoto et al., 1989). This observation was consistent with a recent comprehensive case-control study of 1,900 colorectal adenomas showing metaplastic Paneth cells in distal colorectal adenomas were inversely associated with synchronous advanced adenoma and carcinoma (Mahon et al., 2016). Sakaki et al. (2000) observed a case of gallbladder adenocarcinoma with extensive PCM.
Moreover, PCM was also observed in intestinal type cholangiocarcinoma associated with hepatolithiasis in large hepatic bile duct (Bae et al., 2002). Abnormal cholesterol and bile acid metabolism and secretion are common pathophysiological defects in gallbladder-related diseases. The presence of metaplastic Paneth cells in these diseases could be attributed to the presence of bacterial community. Bile-acid metabolism was reported to be regulated by the gut microbiome, thus the role of microbiota in disease cannot be overruled (Abeysuriya et al., 2008; Wang et al., 2009; Sayin et al., 2013). Similarly, the presence of microbiota in lithogenic bile could also promote inflammation and gall stones (White et al., 2006; Capoor et al., 2008; Sekirov et al., 2010) and microbiota association with gallstones was well reported (Kaufman et al., 1989; Lee et al., 1999; Maurer et al., 2005; Saltykova et al., 2016). Additionally, various microbes have also been isolated from bile in patients with cholesterol stones (Stewart et al., 1987; Cull and Beck, 1988; Darko and Archampong, 1994). Although, no study has established a direct correlation of PCM and the presence of bacteria in gallbladder related diseases, existing studies showed the presence of bacterial communities in lithogenic bile (Abeysuriya et al., 2008) and metaplastic Paneth cells in gallbladder with gallstones (Laitio and Nevalainen, 1975). Therefore, the presence of Paneth cells could be a protective mechanism against the pathogenic bacteria in lithogenic bile.
Alrajban et al. (2018) reported the first PCM in Krukenberg tumors, which represents 1–2% of ovarian tumors and are characterized by the presence of metastatic adenocarcinoma cells. A poorly differentiated carcinoma was observed to contain a mixture of signet ring malignant cells with eosinophilic cytoplasm characteristic of PCM. PCM was also observed in the lining of urethral diverticulum (Niemiec et al., 1989), a condition in which a variable sized pouch is formed. The E. coli was the most common organism among other enteric gram-negative bacteria isolated from urethral diverticulum patients (Ljungqvist et al., 2007; Greiman et al., 2019). Since urethral diverticulum is connected to the urethra and filled during urination, the metaplastic change in urethral lining could be due to exposure to irritants like bacterial colonization and retained urine. Thus, the metaplastic Paneth cells could again be an anti-bacterial response in this scenario. The reported presence of Paneth cells in neovaginitis (van der Sluis et al., 2016) might suggest a similar adaptive response to combat bacterial presence.
Intestinal metaplasia has been described in both benign and malignant prostate glands following estrogen therapy (Bainborough, 1952; Maung et al., 1988). Paneth cell-like metaplasia of prostate gland was first reported by Frydman et al. (1992). Adlakha and Bostwick later reported that these Paneth cell-like changes resembled intestinal Paneth cells by light microscopy. However, they lacked lysozyme immunoreactivity, and retained many prostate markers. Since these Paneth-like cells were positive for neuroendocrine markers, they were called “neuroendocrine cells with large eosinophilic granules” (Adlakha and Bostwick, 1994). PCM was also found in epididymis disorders (Nevalainen et al., 2001; Nistal et al., 2007). Together, these Paneth-like cells may represent transformed normal or neoplastic prostate cells.
The association of infection and inflammation had been investigated in many prostate cancer studies. In a recent study, Shrestha et al. (2018) showed that urine samples of patients with biopsy-proven prostate cancer had increased bacterial clusters frequently associated with other urogenital infections such as prostatitis and bacterial vaginosis (Massari et al., 2019). Additionally, a recent study testing prostatic fluid from prostate cancer and non-prostate cancer patients showed the presence of microbes in both samples, but revealed a difference in microbial species (Ma et al., 2019). Similarly, the presence of microbiota within tumoral, peritumoral and non-tumoral prostate tissue has also been reported (Cavarretta et al., 2017). Thus, whether emergence of Paneth like cells in prostate pathology represented another form of protective mechanism against bacteria may require future investigation.
Closing Remarks
The mucosa of the gastrointestinal tract is continuously challenged by various micro-environmental factors ranging from pathogenic and opportunistic bacteria, and their products, to harsh secretions with digestive properties. In turn, human body has developed defense mechanisms like peristalsis, continuous revival of lining epithelium, and production of antimicrobial peptides, such as those secreted by the Paneth cells. The ectopic expression and secretion of these antimicrobial peptides in non-intestinal mucosa where they are normally absent illustrates a robust tissue plasticity in adaptation to infection and injury. Future studies are necessary to delineate the responsible microbial signaling pathways that invoke such unusual cellular metaplasia. The impact of these widely emerged metaplastic Paneth cells on the progression of inflammatory diseases and cancers warrants in-depth investigation such as using Paneth cell lineage tracing approaches (Yu et al., 2018).
Author Contributions
RS, IB, LZ and NG conceptualized the manuscript. RS and NG drafted the manuscript. IB and LZ edited the manuscript.
Funding
This work was supported by the National Institutes of Health (NIH) grants (DK102934, AT010243, and DK119198), National Science Foundation grants (NSF/BIO/IDBR 1353890 and 1952823), and an ACS Scholar Award (RSG-15-060-01-TBE) to NG.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Abeysuriya, V., Deen, K. I., Wijesuriya, T., and Salgado, S. S. (2008). Microbiology of gallbladder bile in uncomplicated symptomatic cholelithiasis. Hepatobiliary Pancreat. Dis. Int. 7, 633–637.
Abraham, S. C., Park, S. J., Lee, J. H., Mugartegui, L., and Wu, T. T. (2003). Genetic alterations in gastric adenomas of intestinal and foveolar phenotypes. Mod. Pathol. 16, 786–795. doi: 10.1097/01.mp.0000080349.37658.5e
Adlakha, H., and Bostwick, D. G. (1994). Paneth cell-like change in prostatic adenocarcinoma represents neuroendocrine differentiation: report of 30 cases. Hum. Pathol. 25, 135–139. doi: 10.1016/0046-8177(94)90268-2
Adolph, T. E., Tomczak, M. F., Niederreiter, L., Ko, H. J., Bock, J., and Martinez-Naves, E. (2013). Paneth cells as a site of origin for intestinal inflammation. Nature 503, 272–276.
Ajioka, Y., Nishikura, K., and Watanabe, G. (2005). [Pathomorphology of ulcerative colitis]. Nihon Rinsho 63, 763–769.
Albedi, F. M., Lorenzetti, E., Contini, M., and Nardi, F. (1984). Immature Paneth cells in intestinal metaplasia of gastric mucosa. Appl. Pathol. 2, 43–48.
Albores-Saavedra, J., Nadji, M., Henson, D. E., Ziegels-Weissman, J., and Mones, J. M. (1986). Intestinal metaplasia of the gallbladder: a morphologic and immunocytochemical study. Hum. Pathol. 17, 614–620. doi: 10.1016/s0046-8177(86)80134-4
Alrajban, W. A., Khubrani, R. A., Almalki, M. S., Almassri, A., and Alrikabi, A. C. (2018). Extensive Paneth cell metaplasia in an ovarian Krukenberg tumor: report of an unusual case and literature review. J. Surg. Case Rep. 2018:rjy323.
Bae, J. Y., Park, Y. N., Nakanuma, Y., Lee, W. J., Kim, J. Y., and Park, C. (2002). Intestinal type cholangiocarcinoma of intrahepatic large bile duct associated with hepatolithiasis–a new histologic subtype for further investigation. Hepatogastroenterology 49, 628–630.
Bainborough, A. R. (1952). Squamous metaplasia of prostate following estrogen therapy. J. Urol. 68, 329–336. doi: 10.1016/s0022-5347(17)68202-8
Bansal, M., Fenoglio, C. M., Robboy, S. J., and King, D. W. (1984). Are metaplasias in colorectal adenomas truly metaplasias? Am. J. Pathol. 115, 253–265.
Bedini, O. A., Naves, A., San Miguel, P., Quispe, A., and Guida, C. (2014). [Metaplasic Paneth cells in ulcerative colitis]. Acta Gastroenterol. Latinoam. 44, 285–289.
Bevins, C. L., and Salzman, N. H. (2011). Paneth cells, antimicrobial peptides and maintenance of intestinal homeostasis. Nat. Rev. Microbiol. 9, 356–368. doi: 10.1038/nrmicro2546
Bohe, M., Borgstrom, A., Lindstrom, C., and Ohlsson, K. (1986). Pancreatic endoproteases and pancreatic secretory trypsin inhibitor immunoreactivity in human Paneth cells. J. Clin. Pathol. 39, 786–793. doi: 10.1136/jcp.39.7.786
Bohe, M., Lindstrom, C. G., and Ohlsson, K. (1987). Varying occurrence of gastroduodenal immunoreactive pancreatic secretory trypsin inhibitor. J. Clin. Pathol. 40, 1345–1348. doi: 10.1136/jcp.40.11.1345
Boulton, R. A., Usselmann, B., Mohammed, I., and Jankowski, J. (2003). Barrett’s esophagus: environmental influences in the progression of dysplasia. World J. Surg. 27, 1014–1017. doi: 10.1007/s00268-003-7054-0
Bresalier, R. S. (1998). Helicobacter pylori and gastric cancer: a not so simple association. Gastroenterology 114, 408–409. doi: 10.1016/s0016-5085(98)70495-0
Burclaff, J., and Mills, J. C. (2018). Plasticity of differentiated cells in wound repair and tumorigenesis, part II: skin and intestine. Dis. Model Mech. 11:dmm035071. doi: 10.1242/dmm.035071
Burgess, J. N., Payne, W. S., Andersen, H. A., Weiland, L. H., and Carlson, H. C. (1971). Barrett esophagus: the columnar-epithelial-lined lower esophagus. Mayo Clin. Proc. 46, 728–734.
Capoor, M. R., Rajni, D. N., Khanna, G., Krishna, S. V., Chintamani, M. S., and Aggarwal, P. (2008). Microflora of bile aspirates in patients with acute cholecystitis with or without cholelithiasis: a tropical experience. Braz. J. Infect. Dis. 12, 222–225.
Caruso, R. A., La Spada, F., Casablanca, G., and Rigoli, L. (1989). Lysozyme and mucins in gastric adenomas. J. Clin. Pathol. 42, 827–833. doi: 10.1136/jcp.42.8.827
Cavarretta, I., Ferrarese, R., Cazzaniga, W., Saita, D., Luciano, R., Ceresola, E. R., et al. (2017). The microbiome of the prostate tumor microenvironment. Eur. Urol. 72, 625–631.
Chen, S., and Huang, E. H. (2014). The colon cancer stem cell microenvironment holds keys to future cancer therapy. J. Gastrointest. Surg. 18, 1040–1048. doi: 10.1007/s11605-014-2497-1
Chen, W., Frankel, W. L., Cronley, K. M., Yu, L., Zhou, X., and Yearsley, M. M. (2015). Significance of Paneth cell metaplasia in Barrett esophagus: a morphologic and clinicopathologic study. Am. J. Clin. Pathol. 143, 665–671. doi: 10.1309/ajcpvujmcvbc9pkm
Clark, G. W., Smyrk, T. C., Mirvish, S. S., Anselmino, M., Yamashita, Y., Hinder, R. A., et al. (1994). Effect of gastroduodenal juice and dietary fat on the development of Barrett’s esophagus and esophageal neoplasia: an experimental rat model. Ann. Surg. Oncol. 1, 252–261. doi: 10.1007/bf02303531
Clevers, H. C., and Bevins, C. L. (2013). Paneth cells: maestros of the small intestinal crypts. Annu. Rev. Physiol. 75, 289–311. doi: 10.1146/annurev-physiol-030212-183744
Conway, K. L., Kuballa, P., Song, J. H., Patel, K. K., Castoreno, A. B., Yilmaz, O. H., et al. (2013). Atg16l1 is required for autophagy in intestinal epithelial cells and protection of mice from Salmonella infection. Gastroenterology 145, 1347–1357. doi: 10.1053/j.gastro.2013.08.035
Correa, P. (1992). Human gastric carcinogenesis: a multistep and multifactorial process–First American cancer society award lecture on cancer epidemiology and prevention. Cancer Res. 52, 6735–6740.
Correa, P., Fontham, E. T., Bravo, J. C., Bravo, L. E., Ruiz, B., Zarama, G., et al. (2000). Chemoprevention of gastric dysplasia: randomized trial of antioxidant supplements and anti-Helicobacter pylori therapy. J. Natl. Cancer Inst. 92, 1881–1888. doi: 10.1093/jnci/92.23.1881
Correa, P., and Shiao, Y. H. (1994). Phenotypic and genotypic events in gastric carcinogenesis. Cancer Res. 54, 1941s–1943s.
Coutinho, H. B., Robalinho, T. I., Coutinho, V. B., Amorin, A. M., Almeida, J. R., Filho, J. T., et al. (1996). Immunocytochemical demonstration that human duodenal Brunner’s glands may participate in intestinal defence. J. Anat. 189(Pt 1), 193–197.
Cull, D. L., and Beck, D. E. (1988). Routine bile cultures during elective cholecystectomy. South Med. J. 81, 1358–1360. doi: 10.1097/00007611-198811000-00006
Cunliffe, R. N., Rose, F. R., Keyte, J., Abberley, L., Chan, W. C., and Mahida, Y. R. (2001). Human defensin 5 is stored in precursor form in normal Paneth cells and is expressed by some villous epithelial cells and by metaplastic Paneth cells in the colon in inflammatory bowel disease. Gut 48, 176–185. doi: 10.1136/gut.48.2.176
Darko, R., and Archampong, E. Q. (1994). The microflora of bile in Ghanaians. West Afr. J. Med. 13, 113–115.
Deveci, M. S., and Deveci, G. (2004). Altered distribution of metaplastic Paneth, gastrin and pancreatic acinar cells in atrophic gastritic mucosa with endocrine cell lesions. Tohoku J. Exp. Med. 202, 13–22. doi: 10.1620/tjem.202.13
El-Zimaity, H. M., Ota, H., Graham, D. Y., Akamatsu, T., and Katsuyama, T. (2002). Patterns of gastric atrophy in intestinal type gastric carcinoma. Cancer 94, 1428–1436. doi: 10.1002/cncr.10375
Fishbein, T., Novitskiy, G., Mishra, L., Matsumoto, C., Kaufman, S., Goyal, S., et al. (2008). NOD2-expressing bone marrow-derived cells appear to regulate epithelial innate immunity of the transplanted human small intestine. Gut 57, 323–330. doi: 10.1136/gut.2007.133322
Fox, J. G., Li, X., Cahill, R. J., Andrutis, K., Rustgi, A. K., Odze, R., et al. (1996). Hypertrophic gastropathy in Helicobacter felis-infected wild-type C57BL/6 mice and p53 hemizygous transgenic mice. Gastroenterology 110, 155–166. doi: 10.1053/gast.1996.v110.pm8536852
Frydman, C. P., Bleiweiss, I. J., Unger, P. D., Gordon, R. E., and Brazenas, N. V. (1992). Paneth cell-like metaplasia of the prostate gland. Arch. Pathol. Lab Med. 116, 274–276.
Fukase, K., Kato, M., Kikuchi, S., Inoue, K., Uemura, N., Okamoto, S., et al. (2008). Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet 372, 392–397. doi: 10.1016/s0140-6736(08)61159-9
Gassler, N. (2017). Paneth cells in intestinal physiology and pathophysiology. World J. Gastrointest. Pathophysiol. 8, 150–160. doi: 10.4291/wjgp.v8.i4.150
Gassler, N., Schnolzer, M., Rohr, C., Helmke, B., Kartenbeck, J., Grunewald, S., et al. (2002). Expression of calnexin reflects paneth cell differentiation and function. Lab. Invest. 82, 1647–1659. doi: 10.1097/01.lab.0000041709.42598.4a
Gibbs, N. M. (1967). Incidence and significance of argentaffin and paneth cells in some tumours of the large intestine. J. Clin. Pathol. 20, 826–831. doi: 10.1136/jcp.20.6.826
Goldenring, J. R., Nam, K. T., and Mills, J. C. (2011). The origin of pre-neoplastic metaplasia in the stomach: chief cells emerge from the Mist. Exp. Cell Res. 317, 2759–2764. doi: 10.1016/j.yexcr.2011.08.017
Graham, D. Y., Rugge, M., and Genta, R. M. (2019). Diagnosis: gastric intestinal metaplasia - what to do next? Curr. Opin. Gastroenterol. 35, 535–543. doi: 10.1097/mog.0000000000000576
Greiman, A. K., Rolef, J., and Rovner, E. S. (2019). Urethral diverticulum: a systematic review. Arab J. Urol. 17, 49–57. doi: 10.1080/2090598x.2019.1589748
Grootjans, J., Hodin, C. M., De Haan, J. J., Derikx, J. P., Rouschop, K. M., Verheyen, F. K., et al. (2011). Level of activation of the unfolded protein response correlates with Paneth cell apoptosis in human small intestine exposed to ischemia/reperfusion. Gastroenterology 140, 529–539.e3. doi: 10.1053/j.gastro.2010.10.040
Haapamaki, M. M., Gronroos, J. M., Nurmi, H., Alanen, K., Kallajoki, M., and Nevalainen, T. J. (1997). Gene expression of group II phospholipase A2 in intestine in ulcerative colitis. Gut 40, 95–101. doi: 10.1136/gut.40.1.95
Heitz, P. U., and Wegmann, W. (1980). Identification of neoplastic Paneth cells in an adenocarcinoma of the stomach using lysozyme as a marker, and electron microscopy. Virchows Arch. A Pathol. Anat. Histol. 386, 107–116. doi: 10.1007/bf00432648
Inada, K., Nakanishi, H., Fujimitsu, Y., Shimizu, N., Ichinose, M., Miki, K., et al. (1997). Gastric and intestinal mixed and solely intestinal types of intestinal metaplasia in the human stomach. Pathol. Int. 47, 831–841. doi: 10.1111/j.1440-1827.1997.tb03714.x
Ireland, H., Houghton, C., Howard, L., and Winton, D. J. (2005). Cellular inheritance of a Cre-activated reporter gene to determine Paneth cell longevity in the murine small intestine. Dev. Dyn. 233, 1332–1336. doi: 10.1002/dvdy.20446
Ito, H., Hata, J., Yokozaki, H., Nakatani, H., Oda, N., and Tahara, E. (1986). Tubular adenoma of the human stomach. An immunohistochemical analysis of gut hormones, serotonin, carcinoembryonic antigen, secretory component, and lysozyme. Cancer 58, 2264–2272. doi: 10.1002/1097-0142(19861115)58:10<2264::aid-cncr2820581018>3.0.co;2-f
Jarvi, O., and Lauren, P. K. (1967). Intestinal metaplasia in the mucosa of the gallbladder and common bile duct with additional observations on pancreas heterotopy. Ann. Med. Exp. Biol. Fenn. 45, 213–223.
Jin, R. U., and Mills, J. C. (2018). Are gastric and esophageal metaplasia relatives? The case for Barrett’s stemming from SPEM. Dig. Dis. Sci. 63, 2028–2041. doi: 10.1007/s10620-018-5150-0
Jin, R. U., and Mills, J. C. (2019). The cyclical hit model: how paligenosis might establish the mutational landscape in Barrett’s esophagus and esophageal adenocarcinoma. Curr. Opin. Gastroenterol. [Epub ahead of print].
Joo, M., Shahsafaei, A., and Odze, R. D. (2009). Paneth cell differentiation in colonic epithelial neoplasms: evidence for the role of the Apc/beta-catenin/Tcf pathway. Hum. Pathol. 40, 872–880. doi: 10.1016/j.humpath.2008.12.003
Kaufman, H. S., Magnuson, T. H., Lillemoe, K. D., Frasca, P., and Pitt, H. A. (1989). The role of bacteria in gallbladder and common duct stone formation. Ann. Surg. 209, 584–591;discussion591–582.
Kawachi, T., Kurisu, M., Numanyu, N., Sasajima, K., and Sano, T. (1976). Precancerous changes in the stomach. Cancer Res. 36, 2673–2677.
Kazal, L. A., Spicer, D. S., and Brahinsky, R. A. (1948). Isolation of a crystalline trypsin inhibitor-anticoagulant protein from pancreas. J. Am. Chem. Soc. 70, 3034–3040. doi: 10.1021/ja01189a060
Kimura, K., Satoh, K., Ido, K., Taniguchi, Y., Takimoto, T., and Takemoto, T. (1996). Gastritis in the Japanese stomach. Scand. J. Gastroenterol. Suppl. 214, 17–20; discussion 21–23.
Klockars, M., Reitamo, S., Reitamo, J. J., and Moller, C. (1977). Immunohistochemical identification of lysozyme in intestinal lesions in ulcerative colitis and Crohn’s disease. Gut 18, 377–381. doi: 10.1136/gut.18.5.377
Kodama, M., Murakami, K., Okimoto, T., Sato, R., Uchida, M., Abe, T., et al. (2012). Ten-year prospective follow-up of histological changes at five points on the gastric mucosa as recommended by the updated Sydney system after Helicobacter pylori eradication. J. Gastroenterol. 47, 394–403. doi: 10.1007/s00535-011-0504-9
Kong, Y. J., Yi, H. G., Dai, J. C., and Wei, M. X. (2014). Histological changes of gastric mucosa after Helicobacter pylori eradication: a systematic review and meta-analysis. World J. Gastroenterol. 20, 5903–5911.
Kroemer, A., Elsabbagh, A. M., Matsumoto, C. S., Zasloff, M., and Fishbein, T. M. (2016). The microbiome and its implications in intestinal transplantation. Curr. Opin. Organ Transplant. 21, 135–139. doi: 10.1097/mot.0000000000000278
Laitio, M., and Nevalainen, J. (1975). An electron microscopic study of intestinal metaplasia in human gallbladder. Beitr. Pathol. 155, 297–308. doi: 10.1016/s0005-8165(75)80123-5
Lee, D. K., Tarr, P. I., Haigh, W. G., and Lee, S. P. (1999). Bacterial DNA in mixed cholesterol gallstones. Am. J. Gastroenterol. 94, 3502–3506. doi: 10.1111/j.1572-0241.1999.01614.x
Leushacke, M., Tan, S. H., Wong, A., Swathi, Y., Hajamohideen, A., Tan, L. T., et al. (2017). Lgr5-expressing chief cells drive epithelial regeneration and cancer in the oxyntic stomach. Nat. Cell Biol. 19, 774–786. doi: 10.1038/ncb3541
Levine, J. E., Huber, E., Hammer, S. T., Harris, A. C., Greenson, J. K., Braun, T. M., et al. (2013). Low Paneth cell numbers at onset of gastrointestinal graft-versus-host disease identify patients at high risk for nonrelapse mortality. Blood 122, 1505–1509. doi: 10.1182/blood-2013-02-485813
Lewin, K. J., Dowling, F., Wright, J. P., and Taylor, K. B. (1976). Gastric morphology and serum gastrin levels in pernicious anaemia. Gut 17, 551–560. doi: 10.1136/gut.17.7.551
Liu, N., Ando, T., Ishiguro, K., Maeda, O., Watanabe, O., Funasaka, K., et al. (2013). Characterization of bacterial biota in the distal esophagus of Japanese patients with reflux esophagitis and Barrett’s esophagus. BMC Infect. Dis. 13:130. doi: 10.1186/1471-2334-13-130
Ljungqvist, L., Peeker, R., and Fall, M. (2007). Female urethral diverticulum: 26-year followup of a large series. J. Urol. 177, 219–224; discussion 224.
Ma, X., Chi, C., Fan, L., Dong, B., Shao, X., Xie, S., et al. (2019). The microbiome of prostate fluid is associated with prostate cancer. Front. Microbiol. 10:1664. doi: 10.3389/fmicb.2019.01664
Macfarlane, S., Furrie, E., Macfarlane, G. T., and Dillon, J. F. (2007). Microbial colonization of the upper gastrointestinal tract in patients with Barrett’s esophagus. Clin. Infect. Dis. 45, 29–38. doi: 10.1086/518578
Mahon, M., Xu, J., Yi, X., Liu, X., Gao, N., and Zhang, L. (2016). Paneth cell in adenomas of the distal colorectum is inversely associated with synchronous advanced adenoma and carcinoma. Sci. Rep. 6:26129.
Massari, F., Mollica, V., Di Nunno, V., Gatto, L., Santoni, M., Scarpelli, M., et al. (2019). The human microbiota and prostate cancer: friend or foe? Cancers 11:E459.
Matsubara, F. (1977). Morphological study of the Paneth cell. Paneth cells in intestinal metaplasia of the stomach and duodenum of man. Acta Pathol. Jpn. 27, 677–695. doi: 10.1111/j.1440-1827.1977.tb00185.x
Matsukura, N., Kawachi, T., Sugimura, T., Nakadate, M., and Hirota, T. (1979). Induction of intestinal metaplasia and carcinoma in the glandular stomach of rats by N-alkyl-N’-nitro-N-nitrosoguanidines. Gan 70, 181–185.
Maung, R., Kelly, J. K., and Grace, D. A. (1988). Intestinal metaplasia and dysplasia of prostatic urethra secondary to stricture. Urology 32, 361–363. doi: 10.1016/0090-4295(88)90246-4
Maurer, K. J., Ihrig, M. M., Rogers, A. B., Ng, V., Bouchard, G., Leonard, M. R., et al. (2005). Identification of cholelithogenic enterohepatic Helicobacter species and their role in murine cholesterol gallstone formation. Gastroenterology 128, 1023–1033. doi: 10.1053/j.gastro.2005.01.008
McElroy, S. J., Underwood, M. A., and Sherman, M. P. (2013). Paneth cells and necrotizing enterocolitis: a novel hypothesis for disease pathogenesis. Neonatology 103, 10–20. doi: 10.1159/000342340
Mera, R. M., Bravo, L. E., Camargo, M. C., Bravo, J. C., Delgado, A. G., Romero-Gallo, J., et al. (2018). Dynamics of Helicobacter pylori infection as a determinant of progression of gastric precancerous lesions: 16-year follow-up of an eradication trial. Gut 67, 1239–1246. doi: 10.1136/gutjnl-2016-311685
Ming, S. C., Goldman, H., and Freiman, D. G. (1967). Intestinal metaplasia and histogenesis of carcinoma in human stomach. Light and electron microscopic study. Cancer 20, 1418–1429. doi: 10.1002/1097-0142(196709)20:9<1418::aid-cncr2820200908>3.0.co;2-z
Mitsuhashi, J., Mikami, T., Saigenji, K., and Okayasu, I. (2005). Significant correlation of morphological remodeling in ulcerative colitis with disease duration and between elevated p53 and p21 expression in rectal mucosa and neoplastic development. Pathol. Int. 55, 113–121. doi: 10.1111/j.1440-1827.2005.01802.x
Montero, C., and Loizaga, J. M. (1971). Disulphide groups in Paneth cell granules of enteoid metaplasia in chronic gastritis. Histochem. J. 3, 399–402. doi: 10.1007/bf01005022
Morson, B. C. (1955). Carcinoma arising from areas of intestinal metaplasia in the gastric mucosa. Br. J. Cancer 9, 377–385. doi: 10.1038/bjc.1955.36
Naef, A. P., Savary, M., and Ozzello, L. (1975). Columnar-lined lower esophagus: an acquired lesion with malignant predisposition. Report on 140 cases of Barrett’s esophagus with 12 adenocarcinomas. J. Thorac. Cardiovasc. Surg. 70, 826–835. doi: 10.1016/s0022-5223(19)39666-7
Nevalainen, T. J., Shah, V. I., De Peralta-Venturina, M., and Amin, M. B. (2001). Absence of group II phospholipase A2, a Paneth cell marker, from the epididymis. APMIS 109, 295–298. doi: 10.1034/j.1600-0463.2001.d01-123.x
Niemiec, T. R., Mercer, L. J., Stephens, J. K., and Hajj, S. N. (1989). Unusual urethral diverticulum lined by colonic epithelium with Paneth cell metaplasia. Am. J. Obstet. Gynecol. 160, 186–188. doi: 10.1016/0002-9378(89)90116-6
Nistal, M., Marino-Enriquez, A., and De Miguel, M. P. (2007). Granular changes (Paneth cell-like) in epididymal epithelial cells are lysosomal in nature and are not markers of obstruction. Histopathology 50, 944–947. doi: 10.1111/j.1365-2559.2007.02690.x
Nomura, Y., Tanabe, H., Moriichi, K., Igawa, S., Ando, K., Ueno, N., et al. (2013). Reduction of E-cadherin by human defensin-5 in esophageal squamous cells. Biochem. Biophys. Res. Commun. 439, 71–77. doi: 10.1016/j.bbrc.2013.08.026
Ogura, K., Hirata, Y., Yanai, A., Shibata, W., Ohmae, T., Mitsuno, Y., et al. (2008). The effect of Helicobacter pylori eradication on reducing the incidence of gastric cancer. J. Clin. Gastroenterol. 42, 279–283.
Ohtani, H., and Sasano, N. (1988). Ultrastructural immunolocalization of lysozyme in paneth-like cells in undifferentiated (gastric)-type carcinoma of the stomach. Acta Pathol. Jpn. 38, 861–871. doi: 10.1111/j.1440-1827.1988.tb02358.x
Osias, G. L., Bromer, M. Q., Thomas, R. M., Friedel, D., Miller, L. S., Suh, B., et al. (2004). Esophageal bacteria and Barrett’s esophagus: a preliminary report. Dig. Dis. Sci. 49, 228–236.
Ostaff, M. J., Schafer, C., Courth, L., Stebe, S. R., Ott, G., Stange, E. F., et al. (2015). Chronic heavy alcohol use is associated with upregulated paneth cell antimicrobials in gastric mucosa. Clin. Transl. Gastroenterol. 6:e103. doi: 10.1038/ctg.2015.26
Ozzello, L., Savary, M., and Roethlisberger, B. (1977). Columnar mucosa of the distal esophagus in patients with gastroesophageal reflux. Pathol. Annu. 12(Pt 1), 41–86.
Pai, R. K., Rybicki, L. A., Goldblum, J. R., Shen, B., Xiao, S. Y., and Liu, X. (2013). Paneth cells in colonic adenomas: association with male sex and adenoma burden. Am. J. Surg. Pathol. 37, 98–103. doi: 10.1097/pas.0b013e318267b02e
Paneth, J. (1888). Ueber die secernirenden zellen des dunndarm-epithels. Arch. Mikrosk. Anat. 31, 113–191. doi: 10.1007/bf02955706
Pei, Z., Yang, L., Peek, R. M. Jr., Levine, S. M., Pride, D. T., and Blaser, M. J. (2005). Bacterial biota in reflux esophagitis and Barrett’s esophagus. World J. Gastroenterol. 11, 7277–7283.
Perminow, G., Beisner, J., Koslowski, M., Lyckander, L. G., Stange, E., Vatn, M. H., et al. (2010). Defective paneth cell-mediated host defense in pediatric ileal Crohn’s disease. Am. J. Gastroenterol. 105, 452–459. doi: 10.1038/ajg.2009.643
Puiman, P. J., Burger-Van Paassen, N., Schaart, M. W., De Bruijn, A. C., De Krijger, R. R., Tibboel, D., et al. (2011). Paneth cell hyperplasia and metaplasia in necrotizing enterocolitis. Pediatr. Res. 69, 217–223. doi: 10.1203/pdr.0b013e3182092a9a
Quante, M., Bhagat, G., Abrams, J. A., Marache, F., Good, P., Lee, M. D., et al. (2012). Bile acid and inflammation activate gastric cardia stem cells in a mouse model of Barrett-like metaplasia. Cancer Cell 21, 36–51. doi: 10.1016/j.ccr.2011.12.004
Rubio, C. A. (1989). Paneth cell adenoma of the stomach. Am. J. Surg. Pathol. 13, 325–328. doi: 10.1097/00000478-198904000-00008
Rubio, C. A. (2012). Lysozyme is up-regulated in columnar-lined Barrett’s mucosa: a possible natural defence mechanism against Barrett’s esophagus-associated pathogenic bacteria. Anticancer Res. 32, 5115–5119.
Rubio, C. A. (2015). Increased production of lysozyme associated with bacterial proliferation in Barrett’s Esophagitis, Chronic Gastritis, Gluten-induced Atrophic duodenitis (celiac disease), lymphocytic colitis, collagenous colitis, ulcerative colitis and Crohn’s colitis. Anticancer Res. 35, 6365–6372.
Rubio, C. A., Kato, Y., Sugano, H., and Kitagawa, T. (1987). Intestinal metaplasia of the stomach in Swedish and Japanese patients without ulcers or carcinoma. Jpn. J. Cancer Res. 78, 467–472.
Saenz, J. B., and Mills, J. C. (2018). Acid and the basis for cellular plasticity and reprogramming in gastric repair and cancer. Nat. Rev. Gastroenterol. Hepatol. 15, 257–273. doi: 10.1038/nrgastro.2018.5
Sakaki, M., Hirokawa, M., Sano, T., Horiguchi, H., Wakatsuki, S., and Ogata, S. (2000). Gallbladder adenocarcinoma with florid neuroendocrine cell nests and extensive paneth cell metaplasia. Endocr. Pathol. 11, 365–371.
Sakitani, K., Hirata, Y., Watabe, H., Yamada, A., Sugimoto, T., Yamaji, Y., et al. (2011). Gastric cancer risk according to the distribution of intestinal metaplasia and neutrophil infiltration. J. Gastroenterol. Hepatol. 26, 1570–1575. doi: 10.1111/j.1440-1746.2011.06767.x
Saltykova, I. V., Petrov, V. A., Logacheva, M. D., Ivanova, P. G., Merzlikin, N. V., Sazonov, A. E., et al. (2016). Biliary microbiota, gallstone disease and infection with Opisthorchis felineus. PLoS Negl. Trop. Dis. 10:e0004809. doi: 10.1371/journal.pntd.0004809
Salzman, N. H., Hung, K., Haribhai, D., Chu, H., Karlsson-Sjoberg, J., Amir, E., et al. (2010). Enteric defensins are essential regulators of intestinal microbial ecology. Nat. Immunol. 11, 76–83.
Sato, T., Van Es, J. H., Snippert, H. J., Stange, D. E., Vries, R. G., Van Den Born, M., et al. (2011). Paneth cells constitute the niche for Lgr5 stem cells in intestinal crypts. Nature 469, 415–418. doi: 10.1038/nature09637
Sayin, S. I., Wahlstrom, A., Felin, J., Jantti, S., Marschall, H. U., Bamberg, K., et al. (2013). Gut microbiota regulates bile acid metabolism by reducing the levels of tauro-beta-muricholic acid, a naturally occurring FXR antagonist. Cell Metab. 17, 225–235. doi: 10.1016/j.cmet.2013.01.003
Schreiber, D. S., Apstein, M., and Hermos, J. A. (1978). Paneth cells in Barrett’s esophagus. Gastroenterology 74, 1302–1304. doi: 10.1016/0016-5085(78)90711-4
Schwalbe, G. (1872). Beitrage zur kenntnis der drusen in den darmwandungen insbesondere der Brunner’schen drusen. Arch. Mikr. Anat. 8, 92–139.
Segura, D. I., and Montero, C. (1983). Histochemical characterization of different types of intestinal metaplasia in gastric mucosa. Cancer 52, 498–503. doi: 10.1002/1097-0142(19830801)52:3<498::aid-cncr2820520320>3.0.co;2-8
Sekirov, I., Russell, S. L., Antunes, L. C., and Finlay, B. B. (2010). Gut microbiota in health and disease. Physiol. Rev. 90, 859–904.
Shen, B., Porter, E. M., Reynoso, E., Shen, C., Ghosh, D., Connor, J. T., et al. (2005). Human defensin 5 expression in intestinal metaplasia of the upper gastrointestinal tract. J. Clin. Pathol. 58, 687–694. doi: 10.1136/jcp.2004.022426
Shi, J. (2007). Defensins and Paneth cells in inflammatory bowel disease. Inflamm. Bowel Dis. 13, 1284–1292. doi: 10.1002/ibd.20197
Shichijo, S., Hirata, Y., Niikura, R., Hayakawa, Y., Yamada, A., Ushiku, T., et al. (2016). Histologic intestinal metaplasia and endoscopic atrophy are predictors of gastric cancer development after Helicobacter pylori eradication. Gastrointest. Endosc. 84, 618–624. doi: 10.1016/j.gie.2016.03.791
Shichijo, S., Hirata, Y., Sakitani, K., Yamamoto, S., Serizawa, T., Niikura, R., et al. (2015). Distribution of intestinal metaplasia as a predictor of gastric cancer development. J. Gastroenterol. Hepatol. 30, 1260–1264. doi: 10.1111/jgh.12946
Shimada, S., Maeno, M., Misumi, A., Takano, S., and Akagi, M. (1987). Antigen reversion of glycogen phosphorylase isoenzyme in carcinoma and proliferative zone of intestinal metaplasia of the human stomach. An immunohistochemical study. Gastroenterology 93, 35–40. doi: 10.1016/0016-5085(87)90310-6
Shrestha, E., White, J. R., Yu, S. H., Kulac, I., Ertunc, O., De Marzo, A. M., et al. (2018). Profiling the urinary microbiome in men with positive versus negative biopsies for prostate cancer. J. Urol. 199, 161–171. doi: 10.1016/j.juro.2017.08.001
Simmonds, N., Furman, M., Karanika, E., Phillips, A., and Bates, A. W. (2014). Paneth cell metaplasia in newly diagnosed inflammatory bowel disease in children. BMC Gastroenterol. 14:93. doi: 10.1186/1471-230X-14-93
Stewart, L., Smith, A. L., Pellegrini, C. A., Motson, R. W., and Way, L. W. (1987). Pigment gallstones form as a composite of bacterial microcolonies and pigment solids. Ann. Surg. 206, 242–250. doi: 10.1097/00000658-198709000-00002
Symonds, D. A. (1974). Paneth cell metaplasia in diseases of the colon and rectum. Arch. Pathol. 97, 343–347.
Takubo, K., Nixon, J. M., and Jass, J. R. (1995). Ducts of esophageal glands proper and paneth cells in Barrett’s esophagus: frequency in biopsy specimens. Pathology 27, 315–317. doi: 10.1080/00313029500169213
Tanabe, H., Sato, T., Watari, J., Maemoto, A., Fujiya, M., Kono, T., et al. (2008). Functional role of metaplastic paneth cell defensins in Helicobacter pylori-infected stomach. Helicobacter 13, 370–379. doi: 10.1111/j.1523-5378.2008.00621.x
Tanaka, M., Saito, H., Kusumi, T., Fukuda, S., Shimoyama, T., Sasaki, Y., et al. (2001). Spatial distribution and histogenesis of colorectal Paneth cell metaplasia in idiopathic inflammatory bowel disease. J. Gastroenterol. Hepatol. 16, 1353–1359. doi: 10.1046/j.1440-1746.2001.02629.x
Thompson, J. J., Zinsser, K. R., and Enterline, H. T. (1983). Barrett’s metaplasia and adenocarcinoma of the esophagus and gastroesophageal junction. Hum. Pathol. 14, 42–61. doi: 10.1016/s0046-8177(83)80045-8
Uemura, N., Okamoto, S., Yamamoto, S., Matsumura, N., Yamaguchi, S., Yamakido, M., et al. (2001). Helicobacter pylori infection and the development of gastric cancer. N. Engl. J. Med. 345, 784–789.
Vaishnava, S., Behrendt, C. L., Ismail, A. S., Eckmann, L., and Hooper, L. V. (2008). Paneth cells directly sense gut commensals and maintain homeostasis at the intestinal host-microbial interface. Proc. Natl. Acad. Sci. U.S.A. 105, 20858–20863. doi: 10.1073/pnas.0808723105
van der Sluis, W. B., Neefjes-Borst, E. A., Bouman, M. B., Meijerink, W. J., De Boer, N. K., Mullender, M. G., et al. (2016). Morphological spectrum of neovaginitis in autologous sigmoid transplant patients. Histopathology 68, 1004–1012. doi: 10.1111/his.12894
Wada, R., Kuwabara, N., and Suda, K. (1994). Incidence of Paneth cells in colorectal adenomas of Japanese descendants in Hawaii. J. Gastroenterol. Hepatol. 9, 286–288. doi: 10.1111/j.1440-1746.1994.tb01727.x
Wada, R., Yamaguchi, T., and Tadokoro, K. (2005). Colonic Paneth cell metaplasia is pre-neoplastic condition of colonic cancer or not? J. Carcinog. 4:5.
Wang, D., Peregrina, K., Dhima, E., Lin, E. Y., Mariadason, J. M., and Augenlicht, L. H. (2011a). Paneth cell marker expression in intestinal villi and colon crypts characterizes dietary induced risk for mouse sporadic intestinal cancer. Proc. Natl. Acad. Sci. U.S.A. 108, 10272–10277. doi: 10.1073/pnas.1017668108
Wang, D. Q., Cohen, D. E., and Carey, M. C. (2009). Biliary lipids and cholesterol gallstone disease. J. Lipid Res. 50(Suppl.), S406–S411.
Wang, J., Xu, L., Shi, R., Huang, X., Li, S. W., Huang, Z., et al. (2011b). Gastric atrophy and intestinal metaplasia before and after Helicobacter pylori eradication: a meta-analysis. Digestion 83, 253–260. doi: 10.1159/000280318
Watanabe, H. (1978). Experimentally induced intestinal metaplasia in Wistar rats by X-ray irradiation. Gastroenterology 75, 796–799. doi: 10.1016/0016-5085(78)90460-2
Webb, P. M., Yu, M. C., Forman, D., Henderson, B. E., Newell, D. G., Yuan, J. M., et al. (1996). An apparent lack of association between Helicobacter pylori infection and risk of gastric cancer in China. Int. J. Cancer 67, 603–607. doi: 10.1002/(sici)1097-0215(19960904)67:5<603::aid-ijc2>3.0.co;2-y
Wehkamp, J., Salzman, N. H., Porter, E., Nuding, S., Weichenthal, M., Petras, R. E., et al. (2005). Reduced Paneth cell alpha-defensins in ileal Crohn’s disease. Proc. Natl. Acad. Sci. U.S.A. 102, 18129–18134.
Wehkamp, J., Schmid, M., and Stange, E. F. (2007). Defensins and other antimicrobial peptides in inflammatory bowel disease. Curr. Opin. Gastroenterol. 23, 370–378. doi: 10.1097/mog.0b013e328136c580
White, J. R., Gong, H., Pope, B., Schlievert, P., and Mcelroy, S. J. (2017). Paneth-cell-disruption-induced necrotizing enterocolitis in mice requires live bacteria and occurs independently of TLR4 signaling. Dis. Model Mech. 10, 727–736. doi: 10.1242/dmm.028589
White, J. S., Hoper, M., Parks, R. W., Clements, W. D., and Diamond, T. (2006). Patterns of bacterial translocation in experimental biliary obstruction. J. Surg. Res. 132, 80–84. doi: 10.1016/j.jss.2005.07.026
Willet, S. G., Lewis, M. A., Miao, Z. F., Liu, D., Radyk, M. D., Cunningham, R. L., et al. (2018). Regenerative proliferation of differentiated cells by mTORC1-dependent paligenosis. EMBO J. 37:e98311.
Yamamoto, M., Nakajo, S., and Tahara, E. (1989). Dysplasia of the gallbladder. Its histogenesis and correlation to gallbladder adenocarcinoma. Pathol. Res. Pract. 185, 454–460.
Yang, L., Lu, X., Nossa, C. W., Francois, F., Peek, R. M., and Pei, Z. (2009). Inflammation and intestinal metaplasia of the distal esophagus are associated with alterations in the microbiome. Gastroenterology 137, 588–597. doi: 10.1053/j.gastro.2009.04.046
Yu, S., Tong, K., Zhao, Y., Balasubramanian, I., Yap, G. S., Ferraris, R. P., et al. (2018). Paneth cell multipotency induced by notch activation following injury. Cell Stem Cell 23, 46–59. doi: 10.1016/j.stem.2018.05.002
Zhang, C., Sherman, M. P., Prince, L. S., Bader, D., Weitkamp, J. H., Slaughter, J. C., et al. (2012). Paneth cell ablation in the presence of Klebsiella pneumoniae induces necrotizing enterocolitis (NEC)-like injury in the small intestine of immature mice. Dis. Model Mech. 5, 522–532. doi: 10.1242/dmm.009001
Keywords: Paneth cells, Paneth cell metaplasia, microbiome, intestinal metaplasia, gastritis, Barrett’s esophagus
Citation: Singh R, Balasubramanian I, Zhang L and Gao N (2020) Metaplastic Paneth Cells in Extra-Intestinal Mucosal Niche Indicate a Link to Microbiome and Inflammation. Front. Physiol. 11:280. doi: 10.3389/fphys.2020.00280
Received: 09 December 2019; Accepted: 12 March 2020;
Published: 31 March 2020.
Edited by:
Monika Jakubowska, Jagiellonian University, PolandReviewed by:
Eduard Stange, Robert Bosch Hospital, GermanyJason C. Mills, Washington University in St. Louis, United States
Copyright © 2020 Singh, Balasubramanian, Zhang and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nan Gao, bmdhb0BydXRnZXJzLmVkdQ==
 Rajbir Singh
Rajbir Singh Iyshwarya Balasubramanian
Iyshwarya Balasubramanian Lanjing Zhang
Lanjing Zhang Nan Gao
Nan Gao