- 1Clinical Research Center, The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou, China
- 2The Second Clinical Medical College, Guangzhou University of Chinese Medicine, Guangzhou, China
- 3Division of Preventive Cardiology, Department of Cardiovascular Medicine, Mayo Clinic and Foundation, Rochester, MN, United States
- 4Department of Cardiology, The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou, China
- 5Department of Scientific Research, The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou, China
Objective: Baduanjin is a traditional Chinese exercise and serves as an alternative to conventional cardiac rehabilitation in China. In this study, we compare the cardiopulmonary and hemodynamic responses of Baduanjin to those of cycle ergometer exercise in chronic heart failure patients.
Methods: For this cross-sectional study design, following baseline data collection, participants underwent a series of tests including impedance cardiography (ICG) and a maximal cardiopulmonary exercise test (CPET) to determine peak exercise capacity. Participants then engaged in 9-min of Baduanjin exercise. The average oxygen consumption (EqualVO2) during Baduanjin was calculated. Participants then engaged 9 min of constant-load cycling at 60 rpm at an intensity which elicited the EqualVO2. Cardiopulmonary and hemodynamic data were measured continuously during both Baduanjin and cycling exercise.
Results: A total of 30 participants were included. Although Baduanjin and cycling exercise showed similar VO2 levels (8.2 ± 1.3 vs. 8.4 ± 1.4, p = 0.339, respectively), there was a bimodal distribution during Baduanjin exercise compared to a unimodal distribution during cycling exercise. Compared to conventional cycling, Baduanjin demonstrated lower respiratory burden which is associated with greater ventilatory efficiency as evidenced by lower respiratory rate values (p = 0.003), minute ventilation (p < 0.001), end-tidal carbon dioxide pressure (p < 0.001), and minute ventilation to carbon dioxide production ratio (p < 0.001). In terms of hemodynamic response, Baduanjin is demonstrated significantly lower cardiac output (p = 0.017) and elevated arterial-venous oxygen difference (p = 0.036).
Conclusion: Our study offers novel insight into the cardiopulmonary and hemodynamic differences between Baduanjin and cycling when performed at consistent intensity levels. Baduanjin demonstrates an intermittent intensity pattern and increased peripheral oxygen utilization, which is attributed to more pronounced muscle activation. Furthermore, Baduanjin has been linked to a reduction in both cardiac and respiratory burdens.
1 Introduction
Comprehensive exercise-based cardiac rehabilitation (CR) is a Class 1A recommend therapy for patients with chronic heart failure (HF) (Pelliccia et al., 2020; McDonagh et al., 2023; Ponikowski et al., 2016). Patients with HF who engage in exercise based CR demonstrate improved quality of life, reduced hospitalization, and lower mortality rates (Molloy et al., 2024-03; Bozkurt et al., 2021). However, these CR programs are underutilized, with participation rates ranging from 10% to 30% worldwide (Beatty et al., 2023; Ozemek and Squires, 2021; Balady et al., 2011; Grace et al., 2008-10; Sanderson et al., 2003). In China, primary barriers to participation in CR have been identified and include resource scarcity and limited healthcare funding (Zhang et al., 2023; Zhang et al.). Therefore, solutions to improving CR uptake HF patients must be tailored to these barriers. In addition to overcoming the above noted barriers, resource-adapted CR programs must be sensitive to the cultural context in which they are embedded.
Commonly accepted as beneficial to one’s health, traditional Chinese exercise is a form of exercise embedded within communities throughout different regions of mainland China for nearly sixteen centuries (Wang et al., 2016; Health Qigong Management Center, 2003). Thus, this equipment-free exercise may be ideal for hospitals with limited resources (Sun, 2015), as well as patients, because it can be practiced at home, reducing barriers such as weather, transportation, and cost (Deka et al., 2017; Conraads et al., 2012). Baduanjin, translated as “eight silken movements”, is one form of traditional Chinese exercise which has been practiced for over 1,000 years. It is characterized by slow movements (physical training) synchronized with meditation (mindfulness-based training) and regulated breathing (respiratory training) to achieve a harmonious flow of energy (qi) in the body (Zou et al., 2017). Baduanjin is easy to learn, with minimal physical or cognitive demands, as it only entails eight simple movements based on traditional Chinese medicine theory. Moreover, it is an adaptable form of exercise that can be practiced in any location, at any time, without any special equipment, and requires minimal time investment (Chen et al., 2022). Hence, it is easily incorporated into daily routines and could easily be integrated into a comprehensive CR program.
Moderate intensity continuous aerobic exercise is the most widely researched type of exercise in CR and has been shown to be efficient, safe, and well-tolerated by patients with HF (Molloy et al., 2024-03). Historically, Baduanjin has been considered light-intensity exercise, regardless of the individual’s physical fitness. In contrast, our group has recently demonstrated that Baduanjin exercise falls within the moderate intensity aerobic exercise classification, based on the percent of measured oxygen consumption (VO2), particularly for deconditioned patients such as those with HF (Chen et al., 2020). However, to date there is a lack of evidence comparing Baduanjin with conventional moderate intensity aerobic exercise such as cycle ergometer exercise, among CHF patients. This highlights a key knowledge gap for referring physicians. Therefore, the purpose of this study was to 1) compare the cardiopulmonary responses between Baduanjin and cycle ergometer exercise; and 2) compare the hemodynamic responses between Baduanjin and cycle ergometer exercise, in patients with CHF.
2 Methods
2.1 Participants
We utilized a cross-sectional design to recruit patients from the chronic disease management cohort at the Heart Failure Center at Guangdong Provincial Hospital of Chinese Medicine, between June 2023 and January 2024. Eligible participants included stable heart failure patients aged 18–85 years, classified as New York Heart Association (NYHA) class II or III, who had practiced Baduanjin for at least 3 months. The exclusion criteria for the trial included conditions that contraindicate exercise testing. Inclusion and exclusion criteria details are listed in Supplementary S1.
2.2 Data collection
2.2.1 Procedures, equipment, and requirements
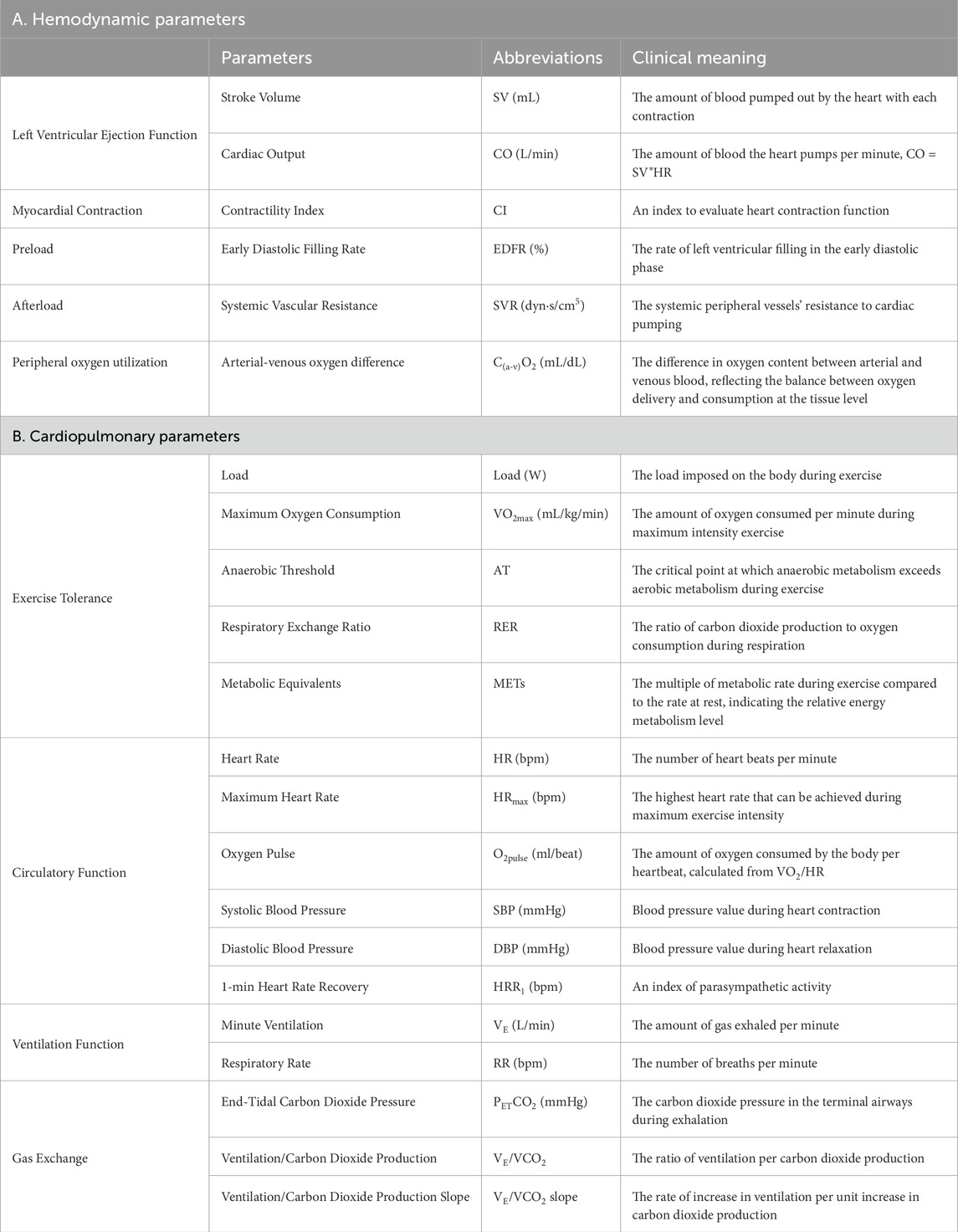
Our study was conducted in the CR department at the Heart Failure Center at Guangdong Provincial Hospital of Chinese Medicine. The main process of this study included three steps (Figure 1). First, after collecting the baseline information (i.e., medical history, physical examination, anthropometric measurements, and echocardiograph data), we conducted a maximal cardiopulmonary exercise test to determine individual maximal exercise capacity (e.g., VO2 peak). Second, we conducted a real-time monitoring test of cardiopulmonary and hemodynamic metrics during Baduanjin exercise. Third, we conducted a real-time monitoring test of the same cardiopulmonary and hemodynamic metrics during cycle ergometer exercise. Details of data collection were listed in Supplementary S2. All of the hemodynamic data collected and constructed by PhysioFlow are listed below with their clinical meanings listed in Table 1.
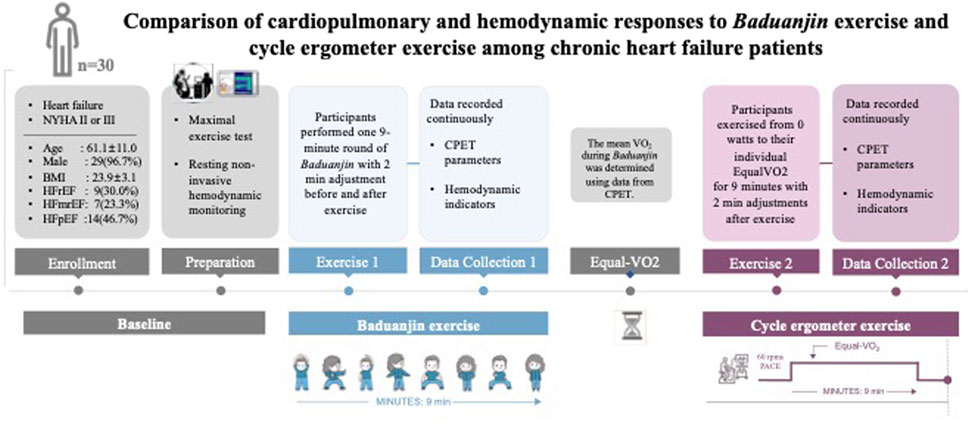
Figure 1. Study procedures Legends: NYHA, New York Heart Association; BMI, body mass index; HFrEF, heart failure with reduced ejection fraction; HFmrEF, heart failure with middle ranged ejection fraction; HFpEF, heart failure with perceived ejection fraction; VO2, volume of Oxygen; EqualVO2, the average oxygen consumption; CPET, cardiopulmonary exercise testing.
2.3 Statistical analysis
We adopted statistical analyses similar to those described in our previous work (Chen et al., 2020). Data from the maximal exercise test as well as the average cardiorespiratory and hemodynamic parameters obtained during Baduanjin exercise and cycle ergometer exercise were summarized as mean and standard deviation (SD). The mean VO2 and HR collected during Baduanjin exercise and cycle ergometer exercise were compared to individual maximum exercise capacity measured during the cardiopulmonary exercise test and reported as a percentage (expressed as %VO2max and %HRmax). In order to categorize the exercise intensity, we referred to a position statement on exercise intensity terminology (Norton et al., 2010). Moreover, in order to explore the cardiopulmonary response patterns throughout the session, all cardiopulmonary parameters were summarized at 10-s intervals as mean ± SD, and plotted over time. All statistical procedures were performed with SPSS (version 18.0, Chicago, IL, USA).
3 Results
3.1 Participant characteristics
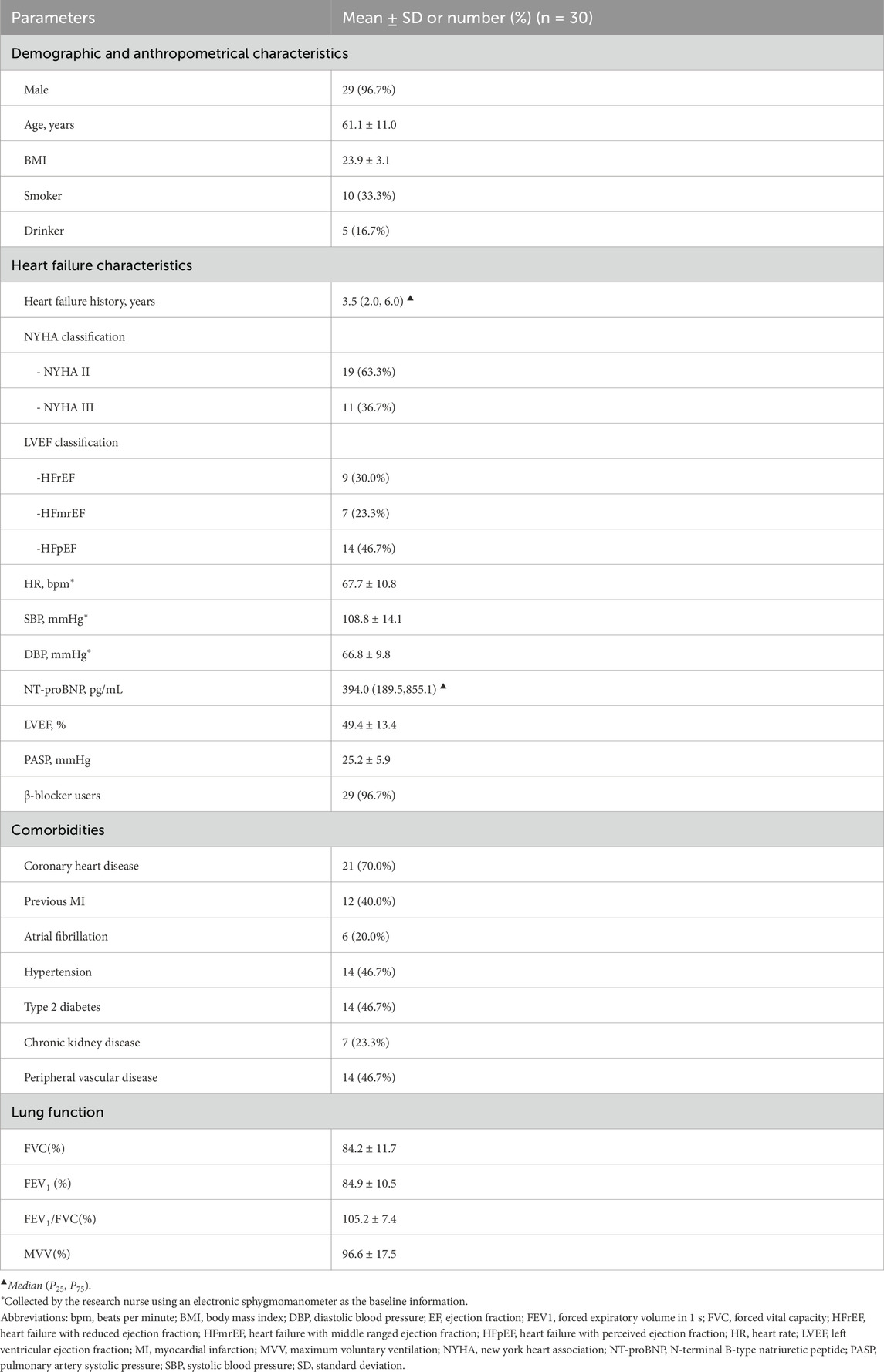
The participants (n = 30, 29 male and 1 female, ages 61.1 ± 11.0 years) had a clinical history of heart failure for a median of 3.5 years and were classified as either New York Heart Association (NYHA) II (n = 19, 63.3%) or NYHA III (n = 11, 36.7%). The mean left ventricular ejection fraction (LVEF) was 49.4% ± 13.4%, and they were either with reduced LVEF (HFrEF, n = 9, 30.0%), middle ranged LVEF (HFmrEF, n = 7, 23.3%), or preserved LVEF n (HFpEF, n = 14, 46.7%). In addition, 96.7% of the participants (n = 29) had been taking β-blockers. Spirometry showed that 66.7% (n = 20) of participants had normal lung function; and 26.7% (n = 8), 3.3% (n = 1), and 3.3% (n = 1) showed restrictive, obstructive, and mixed pulmonary ventilatory dysfunction, respectively. Details on demographic and anthropometry characteristics, medical history, heart failure status, and comorbidities are presented in Table 2.
3.2 Results of maximum exercise tests and resting hemodynamic status
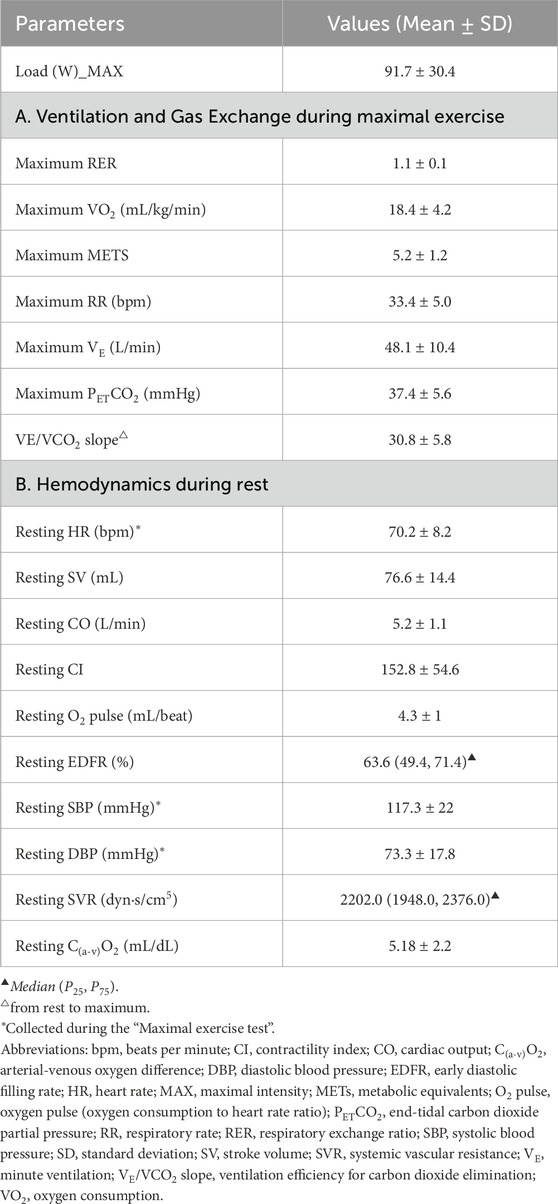
As shown in Table 3, the results of the maximum exercise test revealed that the average RER of the 30 participants was 1.1 ± 0.1. All participants stopped testing due to leg muscle fatigue. VT was detected in all cases. Participants had an impaired exercise capacity with a mean VO2max of 18.4 ± 4.2 mL/kg/min and demonstrated an elevated VE/VCO2 slope (30.8 ± 5.8).
The results of hemodynamic assessment indicated that this sample exhibited normal resting SV at 76.6 ± 14.4 mL, CO at 5.2 ± 1.1 L/min, C(a-v)O2 at 5.18 ± 2.2 mL/dL, and SVR with a median of 2,202.0 dyn∙s/cm5. Additional details regarding hemodynamic indices are presented in Table 3.
3.3 Comparison of the average cardiopulmonary and hemodynamic responses between Baduanjin exercise and cycle ergometer exercise
For the average cardiopulmonary responses (Table 4), the intensity of the two exercises are similar. During exercise, the average VO2 during Baduanjin was 44.6% of VO2max compared to 45.7% of VO2max during cycling with no statistically significant difference between the two groups (8.2 ± 1.3 vs. 8.4 ± 1.4, p = 0.339, respectively; Table 4). For ventilatory and metabolic measures, Baduanjin demonstrated significantly lower RR, VE, PETCO2, and VE/VCO2 (all P < 0.001), compared to the cycling exercise (Table 4).
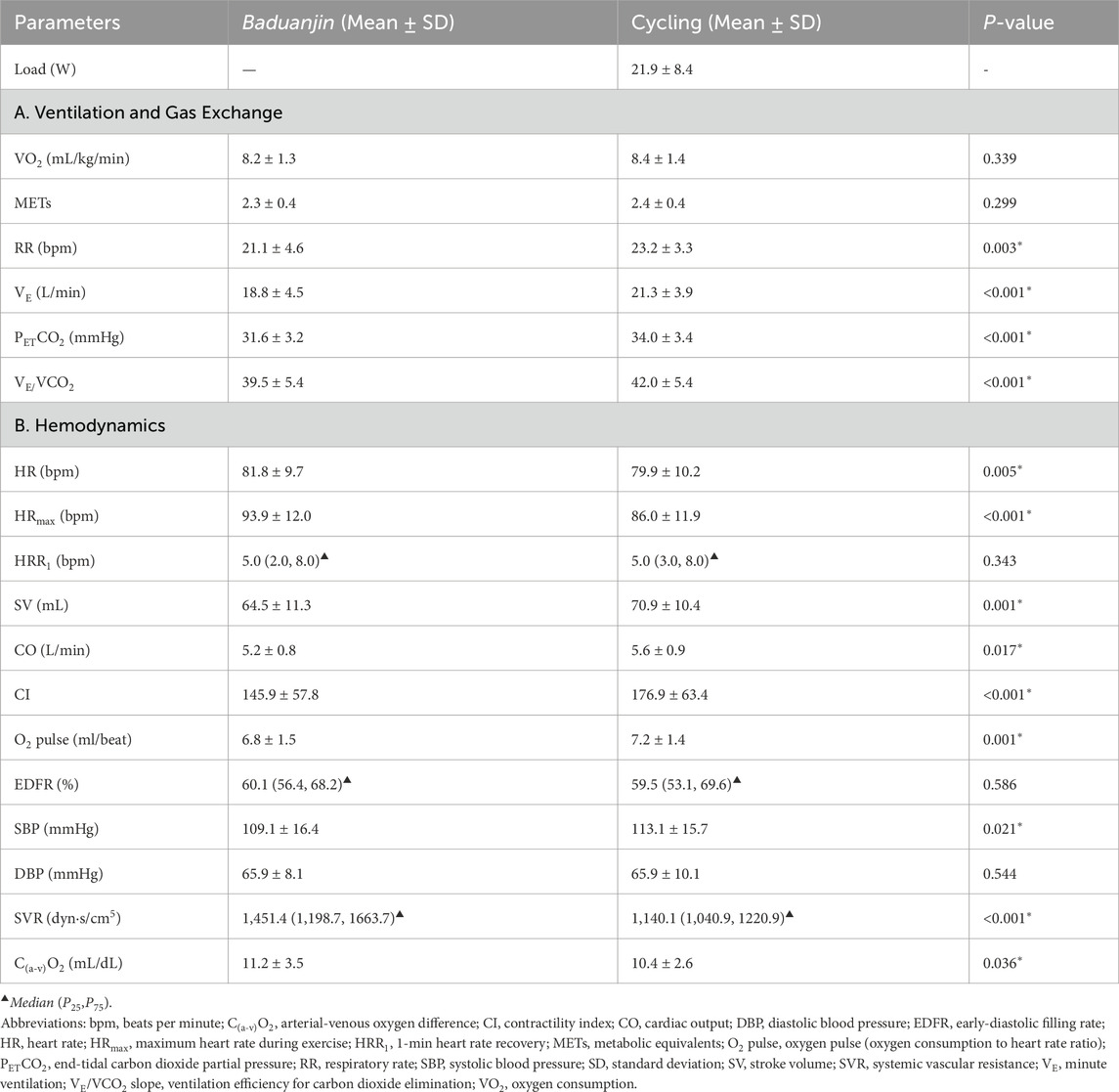
Table 4. Comparison of cardiopulmonary and hemodynamic responses to Baduanjin exercise or cycle exercise.
For the average hemodynamic responses (Table 4), the average HR during Baduanjin exercise was significantly higher when compared to cycling (Table 4). Similarly, the peak heart rate during Baduanjin was significantly higher than during cycle exercise (93.9 bpm versus 86.0 bpm, P < 0.001, Table 4). Furthermore, our data indicate that SBP was significantly lower during Baduanjin compared to cycling while DBP was not different between the two activities (Table 4). In addition, the average SV and CO during Baduanjin exercise (SV: 64.5 ± 11.3 mL, CO: 5.2 ± 0.8 L/min) were both significantly lower than cycle exercise (SV: 70.9 ± 10.4 mL, P = 0.001; CO: 5.6 ± 0.9 L/min, P = 0.017). Moreover, significantly higher C(a-v)O2 (P = 0.036) and SVR (P = 0.036) were found during Baduanjin exercise than during cycle exercise.
3.4 Comparison of the real-time cardiopulmonary and hemodynamic responses between Baduanjin exercise and cycle ergometer exercise
The VO2 responses are shown in Figures 2a,b. The VO2 response curve of the cycle exercise is smooth with no obvious peaks. After the cycle ergometer exercise reached moderate intensity in the second minute, it leveled off and remained at moderate intensity. However, the fluctuations in VO2 during the Baduanjin exercise are greater than those during the cycle exercise. The VO2 responses exhibited a bimodal distribution during Baduanjin. The VO2 increased during the first 3 min when a hemi-squat posture was involved (second posture), followed by a small drop in VO2 after the transition to third posture. The intensity reached the second peak at the seventh minute during an additional two hemi-squat postures (fifth and seventh). It then dropped to the baseline during the resting phase. Overall, the absolute VO2 response remained under the VT (Figure 2a) and the %VO2max response remained within the moderate-intensity range (Figure 2b).
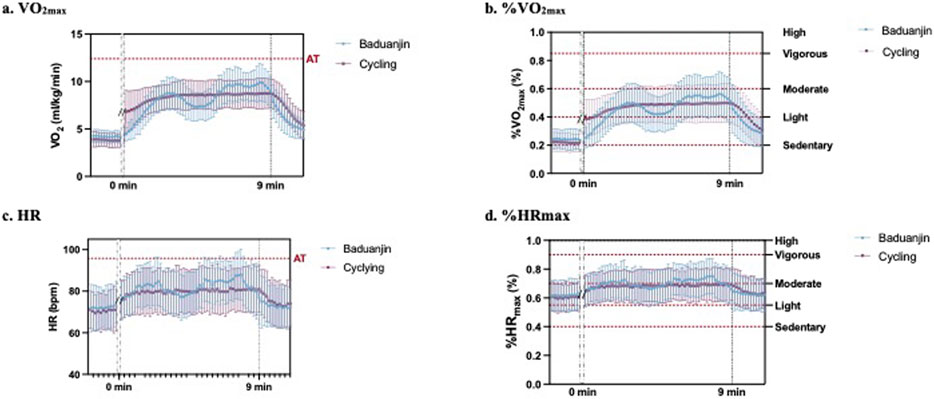
Figure 2. Comparison of the real-time cardiopulmonary responses of (a) VO2max, (b) %VO2max, (c) HR, and (d) %HRmax between Baduanjin exercise and cycle ergometer exercise.
The HR responses are shown in Figures 2c,d. Similar to the VO2 response, the HR response was smooth during cycle exercise and exhibited a bimodal distribution with smaller magnitudes during Baduanjin (Figures 2c,d). Overall, the absolute HR response remained under the equivalent HR for the VT (Figure 2c) and the %HRmax response remained within the moderate-intensity range (Figure 2d).
Figure 3 shows the participants’ ventilatory responses, including respiratory rate (Figure 3a), VE (Figure 3b), PETCO2 (Figure 3c), and VE/VCO2 (Figure 3d), during Baduanjin and cycling exercise. All three response lines from Baduanjin were lower than those from cycling.
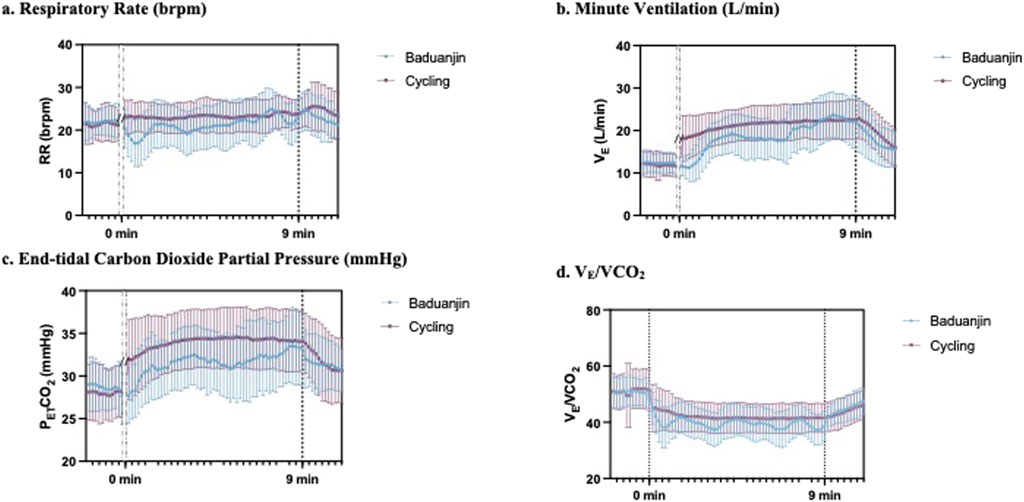
Figure 3. Comparison of the real-time pulmonary responses of (a) respiratory rate, (b) minute ventilation, (c) end-tidal carbon dioxide partial pressure, and (d) VE/VCO2 between Baduanjin exercise and cycle ergometer exercise.
Figure 4 illustrates the real-time hemodynamic responses during Baduanjin and cycle exercise. Overall, during cycling, hemodynamics initially increased from a low value and then stabilized, while Baduanjin’s SV and CO response lines showed fluctuations with time and movement changes. Compared to cycle exercise, the SV and CO response were both lower during Baduanjin (Figures 4a,b), while the C(a-v)O2 and SVR response was higher during Baduanjin (Figures 4c,d).
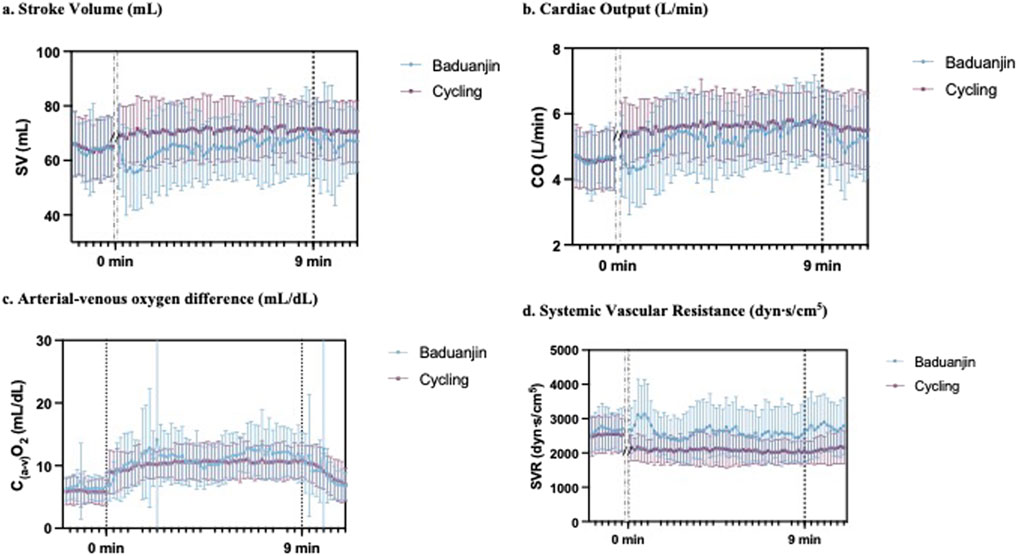
Figure 4. Comparison of the real-time hemodynamic responses of (a) stroke volume, (b) cardiac output, (c) arterial-venous oxygen difference, and (d) systemic vascular resistance between Baduanjin exercise and cycle ergometer exercise.
4 Discussion
This is the first study to compare chronic heart failure patients’ cardiopulmonary and hemodynamic responses to Baduanjin exercise to their responses to constant-load moderate intensity cycle exercise. The intensity of both exercise modalities was calibrated according to VO2, resulting in comparable average VO2 for each modality. In terms of the cardiopulmonary response, Baduanjin exercise is characterized by a bimodal distribution of VO2 responses as well as a lower respiratory burden, which is associated with greater ventilatory efficiency compared to conventional cycling. In terms of hemodynamic response, Baduanjin is demonstrated significantly lower cardiac output and elevated arterial-venous oxygen difference. These cardiopulmonary and hemodynamic responses to Baduanjin may be attributed to a higher degree of muscle engagement compared to cycle ergometer exercise.
The strength of this study lies in its comparison of the cardiopulmonary and hemodynamic differences between Baduanjin exercise and cycle exercise during matched intensity levels. Our study suggests that Baduanjin is a moderate-intensity aerobic exercise suitable for CHF patients, similar to our prior findings (Chen et al., 2020). However, there is a lack of research on real-time physiological responses comparing these two exercise modalities. When studying the cardiopulmonary and hemodynamic responses to different exercises, maintaining a consistent intensity level is crucial (Taylor et al., 2021). In a previous study, exercise intensity was matched based on heart rate response (Gary et al., 2019), while in this study, mean VO2 during Baduanjin exercise was used for match intensity. As such, there was no significant difference in average VO2 between the two modes of exercise. This suggests that VO2 as a parameter is a good tool for balancing determining exercise intensity as complexities may arise when using HR due to the HR-modulating effect of pharmacotherapies commonly prescribed for CHF patients, such as β-blockers.
While average VO2 levels were comparable between the two modes of exercise, distinct differences emerged in the intensity response curves. Cycle exercise plateaued in intensity due to a consistent power output, whereas Baduanjin exhibited an intermittent pattern with notable fluctuations, leading to a bimodal response curve. The bimodal VO2 response observed during Baduanjin exercise is a reflection of the unique characteristics of this traditional Chinese practice, likely attributed to its structured sequence of movements with varying intensities. The presence of two VO2 peaks corresponds to movements involving semi-squat postures, indicating that Baduanjin offers a distinctive form of moderate-intensity intermittent training. Moderate-intensity intermittent physical activity has been shown to be associated with improved executive function in older adults (MacDonald et al., 2024). Furthermore, a systematic review demonstrated that following training, moderate-intensity intermittent training results in greater reductions in fat mass, as well as improved performance on functional tests for elderly women, compared to moderate-intensity continuous training (Coswig et al., 2020/02). Therefore, Baduanjin exercise may be particularly suitable for heart failure patients with impaired executive function or functional performance, as well as for those aiming to achieve fat loss.
Baduanjin exercise imposes a lower respiratory burden by enhancing ventilatory efficiency compared to conventional cycle exercise. Similarly, a meta-analysis has also demonstrated that Baduanjin improves ventilatory efficiency (Zou et al., 2017). Patients with CHF typically exhibit an exaggerated ventilatory response for a given metabolic demand during exercise (Dubé et al., 2016-09). Our study’s findings indicate that during Baduanjin exercise, the respiratory rate is lower than that observed during cycle exercise at the same intensity, suggesting a more stable exercise-induced respiratory response during Baduanjin. This can be particularly advantageous for individuals with heart failure working to improve exercise endurance. In addition, our study show that both VE and VE/VCO2 were lower during Baduanjin exercise, compared to cycle exercise. VE quantifies the total volume of gas inhaled or exhaled per minute and is influenced by respiratory rate and tidal volume. The VE/VCO2 ratio indicates the proportion of ventilation relative to carbon dioxide production. The observed decrease in VE and VE/VCO2 during Baduanjin exercise suggests that less ventilation is needed for the same amount of carbon dioxide production. This indicates a higher efficiency for gas exchange per breath compared to cycle exercise. Baduanjin exercise involves movements that elongate respiratory muscles, enhance thoracic compliance and mobility, reduce respiratory center stimulation, and reduce exertional dyspnea (Xie et al., 2022). Additionally, it incorporates respiratory muscle and breathing training to increase respiratory muscle strength and endurance, decrease mechanical loads such as chest wall stiffness, and facilitate deeper, slower breathing for improved gas exchange efficiency.
Baduanjin exercise imposes a lower cardiac demand with increased peripheral oxygen utilization, compared to cycling. Our results demonstrate a significantly lower CO response during Baduanjin compared with cycling. This reduction in CO, which represents the volume of blood the heart pumps per minute, suggests that Baduanjin imposes less cardiac demand than cycling. Moreover, applying the Fick principle, the C(a-v)O2 was significantly higher during Baduanjin exercise when compared to the cycling. The C(a-v)O2., which quantifies the oxygen concentration disparity between arterial and venous blood post-circulation through active muscle, indicates the efficiency with which peripheral organs, tissues, and cells extract oxygen from the mitochondria. Thus, patients engaged in Baduanjin exercise may experience improved peripheral oxygen extraction, potentially due to the engagement of multiple muscle groups characteristic of this form of exercise.
Baduanjin has been recognized for its comprehensive muscle training program which targets both the upper and lower extremities. In contrast to cycle exercise, which involves simple movements with less muscle mass engagement, Baduanjin incorporates a diverse range of movements that engage muscles throughout the body. For instance, postures such as the horse-riding stance in Postures 2, 5, and 7 can be likened to targeted quadriceps training, effectively strengthening the thigh muscles. Additionally, dynamic movements involving the forearms and fists in Postures 1, 2, 3, and 7 provide comprehensive upper extremity training, enhancing strength and coordination in the arms and hands. Furthermore, Baduanjin emphasizes high-impact and weight-bearing exercises, as illustrated in Posture 8 where practitioners push upward from their toes and land forcefully on their feet. Thus, this holistic approach to physical conditioning extends beyond the focus on lower body muscle endurance typically associated with cycle exercise. However, our current data do not allow us to distinguish perfusion changes specifically in the upper or lower extremities. The higher SVR observed during Baduanjin compared to that during cycle ergometer exercise may suggest greater muscular engagement, further evidenced by high C(a-v)O2. Previous research demonstrated that a single bout of resistance training elevates systemic peripheral resistance (Wakeham et al., 2025a; Wakeham et al., 2025b; Dawson et al., 1985; Miles et al., 1987). Therefore, the engagement of multiple muscle groups in Baduanjin contributes to its therapeutic benefits, particularly in expanding practitioners’ functional capacity and overall muscle strength (Esposito et al., 2011).
4.1 Study limitations
As with any study, this study has potential limitations. Firstly, the sample size was small and we were unable to perform a sample size calculation, as we did not find adequate data for our research question and study design a priori. Although the number of participants was low, the within-subject repeats narrowed the estimates’ confidence intervals. Secondly, the interpretability and generalizability of the results are limited by the analyzed population’s clinical characteristics; our study population included mainly NYHA II CHF patients, and only one female. Therefore, our findings are specific to the population studied. Thirdly, our research employed a non-invasive technique known as ICG, which offers benefits for patients. However, ICG also has limitations regarding specific hemodynamic measurements (such as volume and contractility) that need to be estimated or recalculated. Fourthly, it is crucial to recognize that Baduanjin exercise encompasses elements of strength training and balance training in addition to endurance exercise training. This multifaceted nature sets Baduanjin apart from endurance cycling, which primarily focuses on cardiovascular endurance. As such, the unique combination of strength, balance, and endurance components in Baduanjin requires careful consideration when interpreting the results and comparing it to other forms of exercise. Fifth, this study was specifically designed to observe the gas and hemodynamic changes during the two types of exercise. We did not measure the changes in peak VO2 or VO2 at the first ventilatory threshold following the two types of exercise in this study. However, these parameters are crucial for reflecting improvements in endurance capacity (Christou et al., 2024). Comparing these two parameters would be valuable for further elucidating the differences between the two exercises.
5 Conclusion
Our study offers novel insight into the cardiopulmonary and hemodynamic differences between Baduanjin and cycle ergometer exercise when performed at consistent intensity levels. Unlike the steady intensity of cycle exercise, Baduanjin exhibits an intermittent intensity pattern which is the result of more prominent muscle activation during various postures. Additionally, Baduanjin is associated with superior improvement in oxygen respiratory efficiency and increased peripheral oxygen utilization, which is crucial to CHF patients’ health. Furthermore, Baduanjin reduces cardiac and respiratory burden, providing a more comfortable exercise experience. From the clinical perspective, the practice’s ease-of-use and flexibility regarding time commitment and space requirements make it an attractive option for cardiac rehabilitation programs. Given these advantages, Baduanjin would be particularly effective for inclusion in cardiac rehabilitation programs for CHF patients in China, where it is widely practiced and culturally familiar.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The research protocol was approved by the Ethics Committee at Guangdong Provincial Hospital of Chinese Medicine under ethical approval number YF2023-119-01. Prior to participation, each subject received an oral explanation of the study and provided written and verbal informed consent.
Author contributions
XC: Conceptualization, Data curation, Formal Analysis, Methodology, Project administration, Writing – original draft, Writing – review and editing. XH: Data curation, Formal Analysis, Writing – original draft, Writing – review and editing. TO: Writing – review and editing. YQ: Data curation, Writing – review and editing. HZ: Writing – review and editing. ZW: Writing – review and editing. HC: Funding acquisition, Writing – review and editing. WL: Funding acquisition, Writing – review and editing. WJ: Conceptualization, Methodology, Project administration, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Science and Technology Major Project on Prevention and Treatment of Cancer, Cardiovascular and Cerebrovascular, Respiratory and Metabolic Diseases (grant number 2024ZD0522003); and the Clinical Research Funding of Traditional Chinese Medicine Science and Technology (Project 1010) (grant number YN10101910). Guangzhou Basic and Applied Basic Research Foundation (grant number 2024A03J0739).
Acknowledgments
The authors wish to thank their research assistant Yunxiang Fan from the Department of Cardiology of Guangdong Provincial Hospital of Chinese Medicine for assistance with collecting data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2025.1620785/full#supplementary-material
References
Balady G. J., Ades P. A., Bittner V. A., Franklin B. A., Gordon N. F., Thomas R. J., et al. (2011). Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation 124 (25), 2951–2960. doi:10.1161/CIR.0b013e31823b21e2
Beatty A. L., Beckie T. M., Dodson J., Goldstein C. M., Hughes J. W., Kraus W. E., et al. (2023). A New era in cardiac rehabilitation delivery: research gaps, questions, strategies, and Priorities. Circulation 147 (3), 254–266. doi:10.1161/circulationaha.122.061046
Bozkurt B., Fonarow G. C., Goldberg L. R., Guglin M., Josephson R. A., Forman D. E., et al. (2021). Cardiac rehabilitation for patients With Heart Failure: JACC Expert Panel. J. Am. Coll. Cardiol. 77 (11), 1454–1469. doi:10.1016/j.jacc.2021.01.030
Chen X., Marrone G., Olson T. P., Lundborg C. S., Zhu H., Wen Z., et al. (2020). Intensity level and cardiorespiratory responses to Baduanjin exercise in patients with chronic heart failure. Esc. Heart Fail. 7 (6), 3782–3791. doi:10.1002/ehf2.12959
Chen X., Jiang W., Salazar M., Zhu H., Wen Z., Chen X., et al. (2022). Traditional Baduanjin exercise through the eyes of patients with chronic heart failure: a qualitative content analysis study. Front. Cardiovasc Med. 9, 1049036. doi:10.3389/fcvm.2022.1049036
Christou G. A., Christou M. A., Davos C. H., Markozannes G., Christou K. A., Mantzoukas S., et al. (2024). Ergophysiological evaluation of heart failure patients with reduced ejection fraction undergoing exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Hell. J. Cardiol. 77, 106–119. doi:10.1016/j.hjc.2024.01.004
Conraads V. M., Deaton C., Piotrowicz E., Santaularia N., Tierney S., Piepoli M. F., et al. (2012). Adherence of heart failure patients to exercise: barriers and possible solutions: a position statement of the study group on exercise training in heart failure of the heart failure association of the European Society of cardiology. Eur. J. heart Fail. 14 (5), 451–458. doi:10.1093/eurjhf/hfs048
Coswig V. S., Barbalho M., Raiol R., Del Vecchio F. B., Ramirez-Campillo R., Gentil P. (2020). Effects of high vs moderate-intensity intermittent training on functionality, resting heart rate and blood pressure of elderly women. J. Transl. Med. 18 (1), 88. doi:10.1186/s12967-020-02261-8
Dawson E. A., Green D. J., Cable N. T., Thijssen D. H. (1985). Effects of acute exercise on flow-mediated dilatation in healthy humans. J. Appl. Physiol. 115 (11), 1589–1598. doi:10.1152/japplphysiol.00450.2013
Deka P., Pozehl B., Williams M. A., Yates B. (2017). Adherence to recommended exercise guidelines in patients with heart failure. Heart Fail Rev. 22 (1), 41–53. doi:10.1007/s10741-016-9584-1
Dubé B.-P., Agostoni P., Laveneziana P. (2016). Exertional dyspnoea in chronic heart failure: the role of the lung and respiratory mechanical factors. Eur. Respir. Rev. Official J. Eur. Respir. Soc. 25 (141), 317–332. doi:10.1183/16000617.0048-2016
Esposito F., Reese V., Shabetai R., Wagner P. D., Richardson R. S. (2011). Isolated quadriceps training increases maximal exercise capacity in chronic heart failure: the role of skeletal muscle convective and diffusive oxygen transport. J. Am. Coll. Cardiol. 58 (13), 1353–1362. doi:10.1016/j.jacc.2011.06.025
Gary M. A., Henning A. L., McFarlin B. K. (2019). Metabolic and cardiovascular responses on a novel, Whole body exercise Device compared to a cycle ergometer. Int. J. Exerc. Sci. 12 (2), 1206–1215. doi:10.70252/KICB9258
Grace S. L., Gravely-Witte S., Brual J., Monette G., Suskin N., Higginson L., et al. (2008). Contribution of patient and physician factors to cardiac rehabilitation enrollment: a prospective multilevel study. Eur. J. Cardiovasc. Prev. Rehabilitation Official J. Eur. Soc. Cardiol. Work. Groups Epidemiol. and Prev. Cardiac Rehabilitation Exerc. Physiology 15 (5), 548–556. doi:10.1097/HJR.0b013e328305df05
Health Qigong Management Center (2003). Health Qigong management center of general administration of Sport of China: health Qigong-Baduanjin.
MacDonald E., Morrison E. G., Shivgulam M. E., Pellerine L. P., Kimmerly D. S., Bray N. W., et al. (2024). Moderate intensity intermittent lifestyle physical activity is associated with better executive function in older adults. Front. Sports Act. Living 6, 1393214. doi:10.3389/fspor.2024.1393214
McDonagh T. A., Metra M., Adamo M., Gardner R. S., Baumbach A., Böhm M., et al. (2023). 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 44 (37), 3627–3639. doi:10.1093/eurheartj/ehad195
Miles D. S., Owens J. J., Golden J. C., Gotshall R. W. (1987). Central and peripheral hemodynamics during maximal leg extension exercise. Eur. J. Appl. Physiol. Occup. Physiol. 56 (1), 12–17. doi:10.1007/bf00696369
Molloy C., Long L., Mordi I. R., Bridges C., Sagar V. A., Davies E. J., et al. (2024). Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst. Rev. 3 (3), CD003331. doi:10.1002/14651858.CD003331.pub6
Norton K., Norton L., Sadgrove D. (2010). Position statement on physical activity and exercise intensity terminology. J. Sci. Med. sport 13 (5), 496–502. doi:10.1016/j.jsams.2009.09.008
Ozemek C., Squires R. W. (2021). Enrollment and Adherence to early Outpatient and Maintenance cardiac rehabilitation programs. J. Cardiopulm. Rehabil. Prev. 41 (6), 367–374. doi:10.1097/hcr.0000000000000645
Pelliccia A., Sharma S., Gati S., Bäck M., Börjesson M., Caselli S., et al. (2020). ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 42 (1), 17–96. doi:10.1093/eurheartj/ehaa605
Ponikowski P., Voors A. A., Anker S. D., Bueno H., Cleland J. G. F., Coats A. J. S., et al. (2016). 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. heart Fail. 18 (8), 891–975. doi:10.1002/ejhf.592
Sanderson B. K., Phillips M. M., Gerald L., DiLillo V., Bittner V. (2003). Factors associated with the failure of patients to complete cardiac rehabilitation for medical and nonmedical reasons. J. Cardiopulm. Rehabilitation 23 (4), 281–289. doi:10.1097/00008483-200307000-00005
Sun X. G. (2015). Rehabilitation practice patterns for patients with heart failure: the Asian perspective. Heart Fail. Clin. 11 (1), 95–104. doi:10.1016/j.hfc.2014.09.001
Taylor J. L., Bonikowske A. R., Olson T. P. (2021). Optimizing Outcomes in cardiac rehabilitation: the Importance of exercise intensity. Front. Cardiovasc. Med. 8, 734278. doi:10.3389/fcvm.2021.734278
Wakeham D. J., Pierce G. L., Heffernan K. S. (2025a). Effect of acute resistance exercise and resistance exercise training on Central Pulsatile hemodynamics and Large artery stiffness: Part II. Pulse (Basel) 13 (1), 45–61. doi:10.1159/000543314
Wakeham D. J., Pierce G. L., Heffernan K. S. (2025b). Effect of acute resistance exercise and resistance exercise training on Central Pulsatile hemodynamics and Large artery stiffness: Part I. Pulse (Basel) 13 (1), 31–44. doi:10.1159/000543313
Wang X. Q., Pi Y. L., Chen P. J., Liu Y., Wang R., Li X., et al. (2016). Traditional Chinese exercise for cardiovascular diseases: systematic review and meta-analysis of Randomized Controlled trials. J. Am. Heart Assoc. 5 (3), e002562. doi:10.1161/jaha.115.002562
Xie Q., Xiao M., Huang J. (2022). The efficacy and physiological mechanisms of Baduanjin on dyspnea and exercise limitation in patients with COPD [in Chinese]. Massage Rehabilitation Med. 13 (22), 46–50. doi:10.19787/j.issn.1008-1879.2022.22.012
Zhang Z., Pack Q., Squires R. W., Lopez-Jimenez F., Yu L., Thomas R. J. (2016). Availability and characteristics of cardiac rehabilitation programmes in China. Heart Asia 8 (2), 9–12. doi:10.1136/heartasia-2016-010758
Zhang S., Ding R., Chen S., Meng X., Jianchao L., Wang D. W., et al. (2023). Availability and trend of dissemination of cardiac rehabilitation in China: report from the multicenter national registration platform between 2012 and 2021. Front. Cardiovasc Med. 10, 1210068. doi:10.3389/fcvm.2023.1210068
Zou L., SasaKi J. E., Wang H., Xiao Z., Fang Q., Zhang M. (2017). A systematic review and meta-analysis Baduanjin Qigong for health benefits: Randomized Controlled trials. Evidence-based complementary Altern. Med. eCAM 2017, 4548706. doi:10.1155/2017/4548706
Glossary
CHF chronic heart failure
ICG impedance cardiography
CPET cardiopulmonary exercise testing
NYHA New York Heart Association
EqualVO2 the average oxygen consumption
VO2 volume of oxygen
VE minute ventilation
CO cardiac output
EBCR exercise-based cardiac rehabilitation
HF heart failure
HR heart rate
SV stroke volume
CI contractility index
EDFR diastolic filling rate
SVR systemic vascular resistance
VO2max maximum oxygen consumption
RER respiratory exchange ratio
METs metabolic equivalents
HRmax maximum heart rate
O2pulse oxygen pulse
SBP systolic blood pressure
DBP diastolic blood pressure
HRR1 minute heart rate recovery
RR respiratory rate
PETCO2 end-tidal carbon dioxide pressure
VE/VCO2 ventilation/carbon dioxide production
VE/VCO2slope ventilation/carbon dioxide production slope
VT ventilatory threshold
AT anaerobic threshold
VCO2 volume of carbon dioxide
LVEF left ventricular ejection fraction
SD standard deviation
C(a-v)O2 elevated arterial-venous oxygen difference
BMI body mass index
bpm beats per minute
NT-proBNP N-terminal B-type natriuretic peptide
PASP pulmonary artery systolic pressure
MI myocardial infarction
MAX maximal intensity
O2pulse oxygen pulse (oxygen consumption to heart rate ratio)
FEV1 forced expiratory volume in 1 s
FVC forced vital capacity
MVV maximum voluntary ventilation
Keywords: chronic heart failure, Baduanjin, cycle ergometer exercise, cardiopulmonary response, hemodynamic response
Citation: Chen X, Hu X, Olson TP, Qiu Y, Zhu H, Wen Z, Cai H, Lu W and Jiang W (2025) Cardiopulmonary and hemodynamic responses to Baduanjin exercise and cycle ergometer exercise among chronic heart failure patients: a comparison. Front. Physiol. 16:1620785. doi: 10.3389/fphys.2025.1620785
Received: 30 April 2025; Accepted: 25 August 2025;
Published: 18 September 2025.
Edited by:
Guoxin Ni, First Affiliated Hospital of Xiamen University, ChinaReviewed by:
Georgios A. Christou, University of Ioannina, GreeceQian Luo, Sichuan University, China
Copyright © 2025 Chen, Hu, Olson, Qiu, Zhu, Wen, Cai, Lu and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weihui Lu, d2VpaHVpLmx1QGd6dWNtLmVkdS5jbg==; Wei Jiang, ZHJqaWFuZ3dlaUAxMjYuY29t
†These authors have contributed equally to this work
 Xiankun Chen
Xiankun Chen Xiaoyue Hu
Xiaoyue Hu Thomas P. Olson
Thomas P. Olson Yaqi Qiu
Yaqi Qiu Huiying Zhu
Huiying Zhu Zehuai Wen
Zehuai Wen Huayang Cai
Huayang Cai Weihui Lu
Weihui Lu Wei Jiang
Wei Jiang