- 1Department of Anorectal Surgery, Yancheng TCM Hospital Affiliated to Nanjing University of Chinese Medicine, Yancheng, China
- 2Department of Gastroenterology, Yancheng NO.1 People’s Hospital, Yancheng, China
Background and aims: Crohn’s disease (CD) exhibits escalating incidence in China, particularly in coastal regions undergoing rapid industrialization. We aim to investigate the epidemiological characteristics of CD and identify factors influencing diagnostic delay in the Yancheng region of China.
Methods: A cross-sectional analysis was conducted on CD patients from two tertiary medical centers (Yancheng TCM Hospital Affiliated to Nanjing University of Chinese Medicine and Yancheng No.1 People’s Hospital) between October 2021 and October 2024. We calculated crude prevalence and incidence rates, and performed logistic regression analyses to identify predictors of diagnostic delay.
Results: Among 200 enrolled CD patients (male-to-female ratio: 2.07:1), the crude prevalence and incidence rates were 17.48/100,000 and 2.3/100,000, respectively. Diagnostic delay occurred in 48% (96/200) of cases, with a median delay duration of 23 months (IQR: 12–48; maximum: 300 months). Multivariate analysis identified advanced age at diagnosis as an independent risk factor for delay (OR = 1.035, 95% CI: 1.010–1.060, P = 0.005), while abdominal pain served as a protective factor (OR = 2.088, 95% CI: 1.136–3.838, P = 0.018). Diagnostic delay duration correlated positively with age at diagnosis (r = 0.302, P = 0.003) and frequency of refrigerated food consumption (r = 0.219, P = 0.032). No significant associations were observed between delay duration and complications such as intestinal obstruction, perforation, or surgical intervention (P > 0.05).
Conclusion: The Yancheng region exhibits higher CD prevalence and incidence rates compared to national averages, with pronounced diagnostic delays. These findings highlight the need for targeted interventions to improve early diagnosis and mitigate healthcare burdens.
1 Introduction
Crohn’s disease (CD), a chronic idiopathic inflammatory bowel disorder affecting the entire gastrointestinal tract (predominantly the terminal ileum and proximal colon), exhibits marked global epidemiological heterogeneity. CD pathogenesis arises from multifactorial interactions involving impaired intestinal barrier function, dysregulation of both innate and adaptive immune responses, and alterations in gut microbial ecology. These interconnected pathological mechanisms collectively drive the characteristic chronic transmural inflammation observed in this condition (Roda et al., 2020). While Australia reports the highest incidence (29.3 per 105 person-years) and Europe/Canada demonstrate prevalence peaks (322.0 and 319.0 per 105, respectively) (Ng et al., 2017), Asia is experiencing an accelerating epidemiological transition. Rapidly rising CD rates in this region are hypothesized to reflect lifestyle shifts, dietary modifications, and environmental exposures (GBD, 2017 Inflammatory Bowel Disea se Collaborators, 2020). In China, national incidence surged from 0.46/105 (2010-2013) (Cui and Yuan, 2018) to 0.71/105 in urban areas by 2016 (Xu et al., 2023), underscoring evolving disease dynamics. Notably, China’s vast geographical diversity—encompassing distinct climate zones, socioeconomic gradients, and genetic/environmental interactions—drives heterogeneous epidemiological patterns (Cui and Yuan, 2018). Current CD research predominantly focuses on metropolitan hubs (Shanghai, Guangzhou, Wuhan) and high-prevalence provinces (Guangdong, Zhejiang, Taiwan) (Xu et al., 2023; Wang et al., 2013; Ng et al., 2016; Chen et al., 2025), leaving coastal-industrial regions like Yancheng critically underrepresented. Situated in Jiangsu Province within the Yangtze River Delta, Yancheng exemplifies unique coastal-industrial characteristics: high humidity, seafood-rich diets, rapid industrialization, and documented water quality concerns. These factors may synergistically modulate CD risk, yet systematic epidemiological data remain absent. This study pursues dual objectives: 1) to delineate CD epidemiological profiles in Yancheng, addressing critical data gaps for coastal China; 2) to identify determinants of diagnostic delay, a pervasive issue compromising therapeutic efficacy. Prolonged diagnostic intervals correlate with reduced quality of life, delayed biologic initiation, and irreversible bowel damage. Early use of biologics reduces CD-related surgery rates and the risk of hormone dependence (Lujan et al., 2024). Concurrently, early post-diagnosis initiation of biologic agents has been evidenced to reduce cumulative healthcare expenditures while mitigating long-term healthcare resource utilization (Ungaro et al., 2024). Consequently, this study incorporates a focused investigation into diagnostic delay, analyzing region-specific risk factors. We aim to inform targeted prevention strategies and optimize clinical management.
2 Methods
This study protocol received ethical clearance from the Ethics Committee of Yancheng TCM Hospital Affiliated to Nanjing University of Chinese Medicine (Approval No. KY241101) in November 2024. Following rigorous evaluation by two board-certified inflammatory bowel disease (IBD) specialists and acquisition of informed consent, 200 confirmed CD patients were retrospectively enrolled in this cohort study. The sample size required for this epidemiological study was calculated using the standard formula for prevalence surveys:
Where: Z1−α/2 = Z-value for the desired confidence level, p = Expected prevalence of Crohn’s disease, d = Margin of error, Deff = Design effect accounting for cluster sampling.
Utilizing demographic data derived from the Yancheng Population Census, we calculated disease frequency metrics as follows:
Prevalence was computed as the proportion of individuals with existing cases relative to the permanent resident population at a specified reference date:
Incidence was defined as the number of newly confirmed cases occurring during the observation period divided by the at-risk population:
Diagnostic delay was defined as time period (in months) from first symptoms to CD diagnosis (Schoepfer et al., 2013).
2.1 Patient recruitment
Given the centralized healthcare-seeking pattern of CD patients in Yancheng, where a large proportion of regional cases are managed at two tertiary centers (Yancheng Affiliated Hospital of Nanjing University of Chinese Medicine and Yancheng NO.1 People’s Hospital), we consecutively enrolled all confirmed CD patients attending these institutions from October 2021 to October 2024. Diagnosis was validated through Chinese clinical practice guideline on the management of Crohn’s disease or ECCO Guidelines on the Prevention, Diagnosis, and Management of Infections in Inflammatory Bowel Disease (Inflammatory Bowel Disease Group et al., 2024; Kucharzik et al., 2021). Exclusion criteria comprised incomplete clinical documentation, cognitive impairment affecting consent capacity, concurrent participation in interventional trials or Withdrawal of informed consent. Control subjects were systematically recruited from the same clinical settings, with comprehensive exclusion criteria encompassing inflammatory bowel disease (Crohn’s disease or ulcerative colitis), autoimmune disorders (e.g., rheumatoid arthritis, systemic lupus erythematosus), gastrointestinal malignancies, and other forms of colitis (including infectious, ischemic, or microscopic colitis).
2.2 Data collection
Referring to the relevant literature (Xu et al., 2023), we formulated the “Yancheng Region Crohn’s Disease Questionnaire” to register the clinical data of patients in Yancheng region in detail, including demographic information (age, gender, occupation, residential area, education level, etc.), disease characteristics (Symptom duration, Montreal classification, therapeutic interventions, complication profiles, etc.), as well as potentially influencing factors (family history, smoking, diet, history of antibiotic use, gastrointestinal infections, pharmacological history, parasitic infections, measles, rubella and mumps, etc.).
2.3 Statistical analysis
All analyses were conducted using SPSS Statistics 27.0 (IBM Corp.). Continuous variables underwent normality assessment via Shapiro-Wilk tests, supplemented by visual inspection of histograms and Q-Q plots. Normally distributed data were expressed as mean ± standard deviation (SD) and analyzed using independent t-tests (two-group comparisons) or one-way ANOVA (multi-group comparisons). Non-parametric variables were reported as median (interquartile range, IQR) with Mann-Whitney U tests for between-group analyses. Categorical variables were presented as frequencies (%) and compared via χ2 or Fisher’s exact tests. Multivariate logistic regression analyses were implemented to identify independent determinants of Crohn’s disease development and diagnostic delay. Variables demonstrating preliminary associations (P ≤ 0.05) in univariate screening were incorporated into the logistic regression models, with computation of odds ratios (ORs) and corresponding 95% confidence intervals (95% CIs). Spearman’s rank correlation coefficients (r) quantified temporal relationships between diagnostic delay duration and clinical covariates, with Bonferroni correction applied for multiple comparisons. Statistical significance thresholds were defined as P < 0.05 (two-tailed) and P < 0.01 (high significance).
3 Results
3.1 Incidence and prevalence of CD in Yancheng
Based on municipal demographic data (resident population: 7.1 million), Yancheng exhibited a crude CD prevalence of 17.48 cases per 100,000 population, with an annual incidence rate of 2.30/100,000 in 2024.
3.2 Demographic profile of the CD cohort
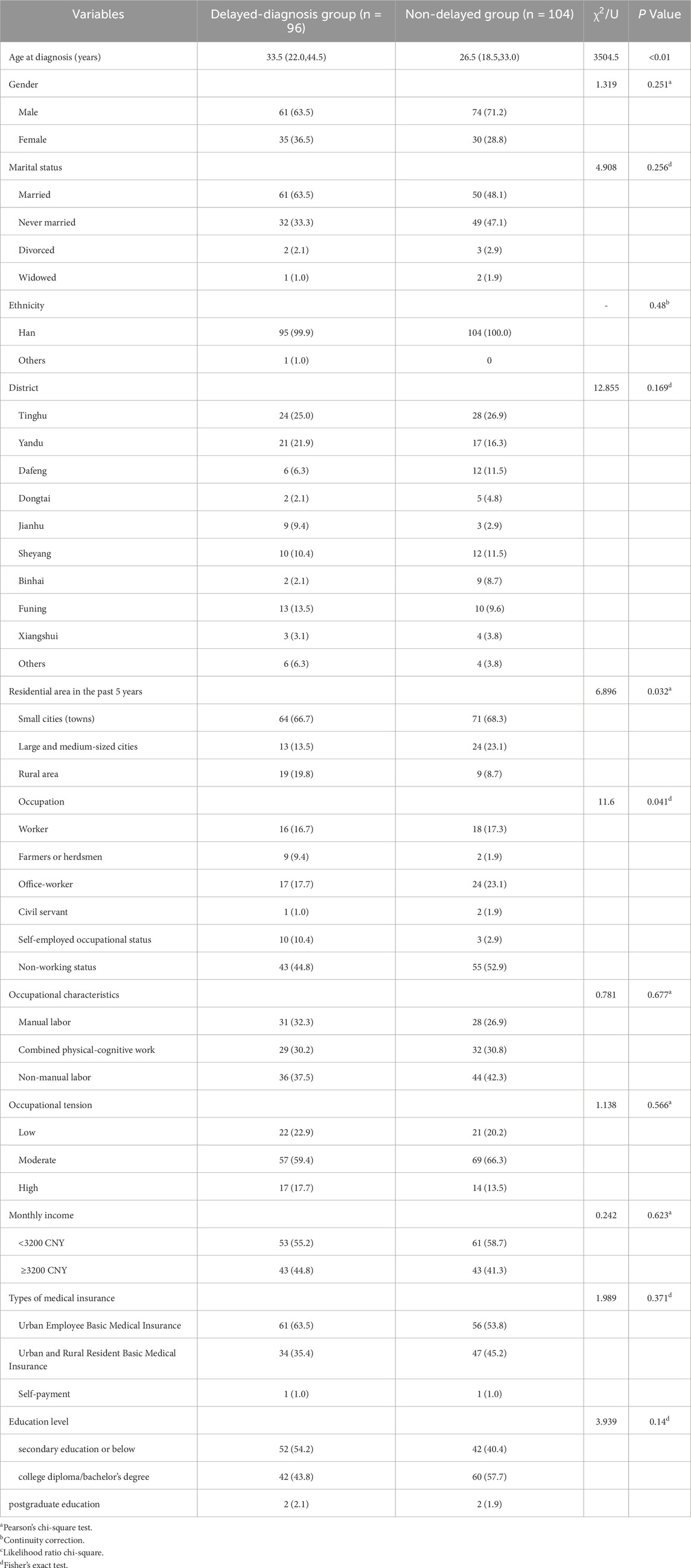
This study enrolled 200 patients with CD, excluding 14% of screened cases. The cohort comprised predominantly male patients (male-to-female ratio: 2.07:1) with a median diagnosis age of 29 years (IQR 20–39; range 12–80, exhibiting a unimodal age distribution peaking at 20–29 years overall, though sex-specific disparities were observed (male peak: 20–29 years vs. female peak: 30–39 years; Figure 1). Geospatial analysis revealed concentrated case distribution in Tinghu District (26.0%, n = 52) and minimal representation in Xiangshui County (3.5%, n = 7; Figure 2). The cohort predominantly comprised Han Chinese (99.5%), married individuals (55.5%, n = 111), and residents of small cities (towns) (67.5%, n = 135). Socioeconomically, 47.0% (n = 94) had secondary education or below, 57.0% (n = 114) reported monthly incomes below 3 200 CNY, and 58.5% (n = 117) were covered by urban employee basic medical insurance. Occupational profiling identified non-working status (retirees/homemakers/unemployed) in 49.0% (n = 98), with white-collar workers comprising 40.0% (n = 80) and moderate occupational intensity reported by 63.0% (n = 126) (Table 1).
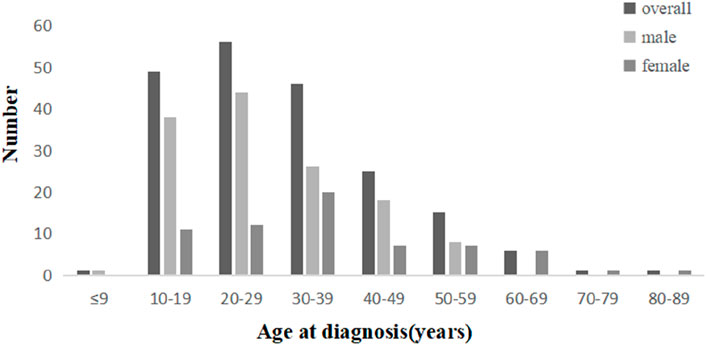
Figure 1. Distribution of age at diagnosis of CD patients in Yancheng region. Bar graph showing the number of medical diagnoses across different age groups divided by gender: overall, male, and female. Ages range from under 9 to 80–89 years. The highest number of diagnoses occurs in the 10–19 and 20–29 age ranges. Sex-specific disparities were observed (male peak: 20–29 years vs. female peak: 30–39 years.
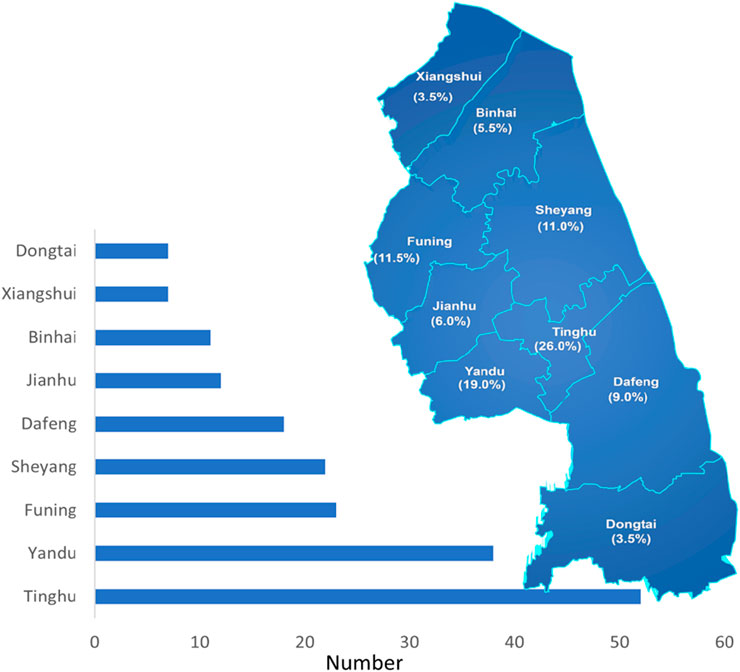
Figure 2. Distribution of CD patients in Yancheng region. Map of a region divided into labeled areas, each with percentages. Tinghu has the highest percentage at 26.0%, followed by Yandu at 19.0%, and Xiangshui has the lowest percentage at 3.5%.
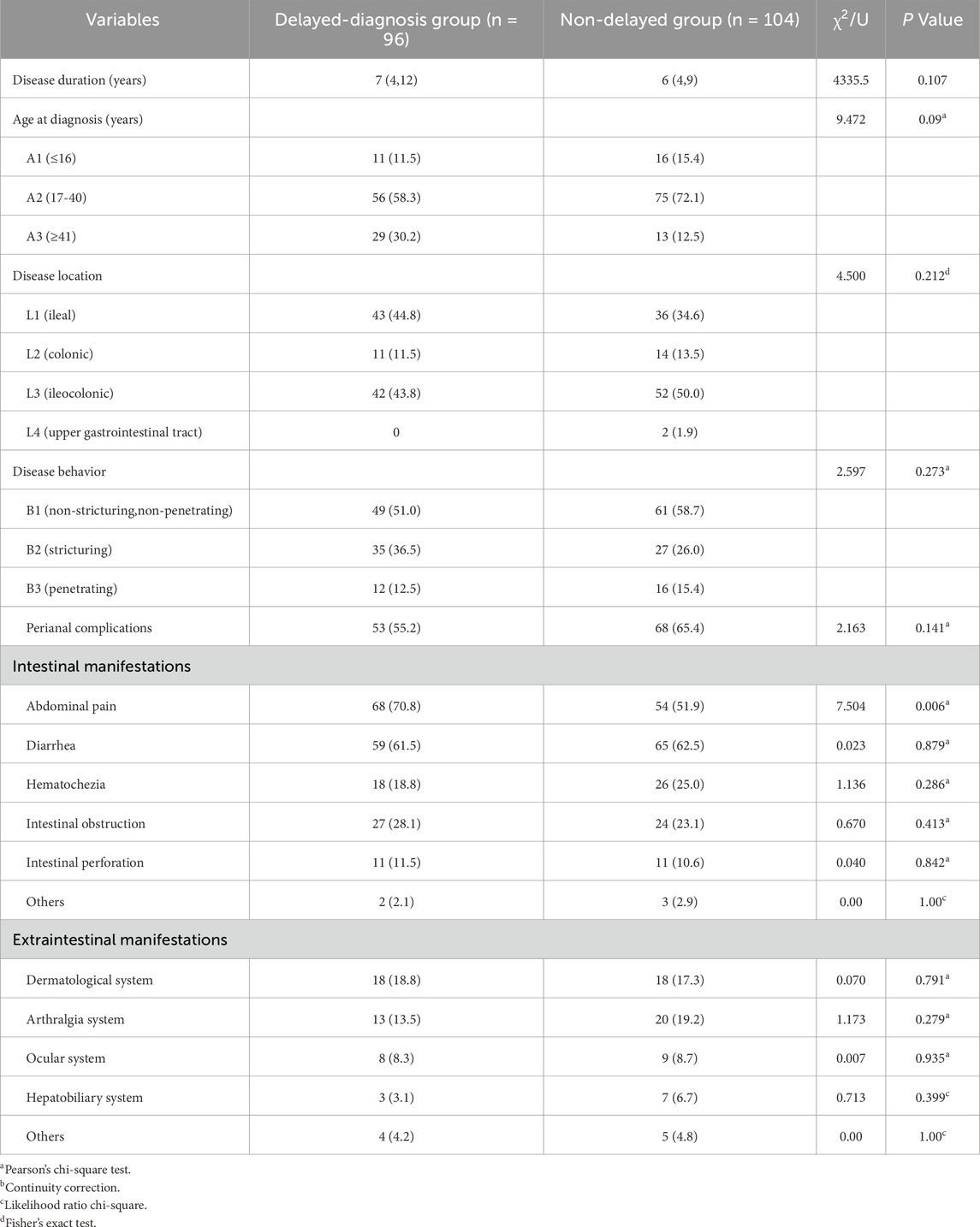
3.3 Clinical characteristics and disease phenotypes
The cohort comprised 200 CD patients with a median disease duration of 6 years (IQR 4–10), predominantly presenting with intestinal manifestations (n = 176, 88.0%), including abdominal pain (n = 122), diarrhea (n = 124), hematochezia (n = 44), intestinal obstruction (n = 51), and perforation (n = 22). Extraintestinal manifestations affected 40.0% (n = 80) of patients, involving dermatological (n = 36), arthralgia (n = 33), ocular (n = 17), and hepatobiliary systems (n = 10). Disease localization followed Montreal classification: ileal (L1: 39.5%, n = 79), colonic (L2: 12.5%, n = 25), ileocolonic (L3: 47.0%, n = 94), and upper gastrointestinal involvement (L4: 11.5%, n = 23). Disease behavior was non-stricturing, non-penetrating (B1: 55.0%, n = 110), stricturing (B2: 31.0%, n = 62), or penetrating (B3: 14.0%, n = 28), with perianal complications documented in 60.5% (n = 121) of cases (Table 2).
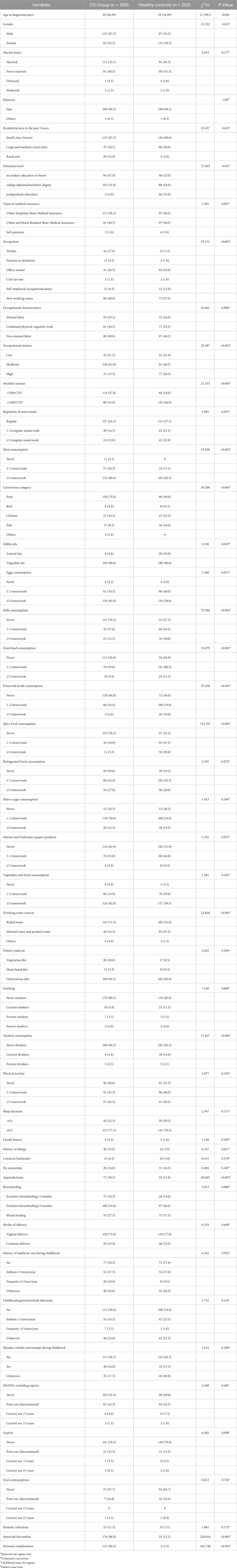
3.4 Treatment patterns and therapeutic interventions
Among the 200 CD patients analyzed, biologic agents constituted the predominant therapeutic strategy (n = 178, 89.0%), followed by surgical intervention (n = 50, 25.0%) and conventional therapies including 5-Aminosalicylic acid (5-ASA), corticosteroids, or immunosuppressants (n = 40, 20.0%), with multiple treatment modalities employed in progressive cases (Table 3).
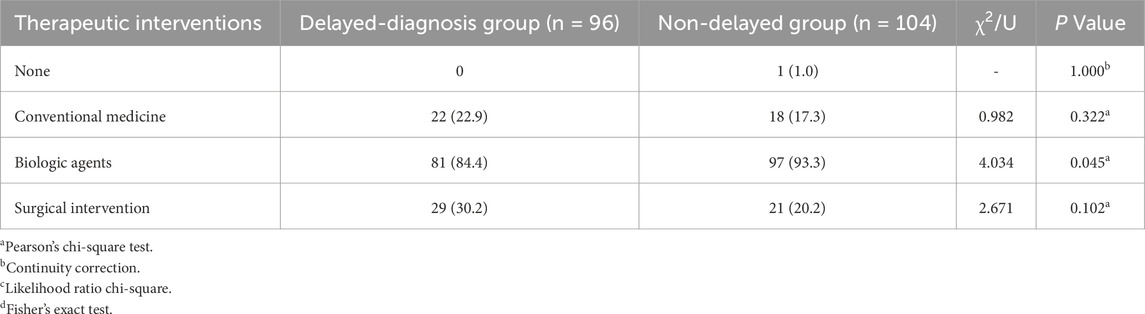
3.5 Multivariable determinants of Crohn’s disease risk in coastal China
In this case-control study comprising 200 CD cases and 200 matched controls, univariate analysis identified 20 significant determinants of CD development, spanning sociodemographic factors (gender, recent residential area [past 5 years], education level, occupation, occupational characteristics, occupational stress levels, monthly income), dietary patterns (meat consumption frequency/types, edible oil classes, milk intake, fried/preserved/spicy food consumption, drinking water sources), lifestyle exposures (alcohol consumption), clinical history (history of allergy, appendectomy), and disease-specific features (intestinal symptoms, perianal complications), as detailed in Table 4. Multivariable logistic regression adjusted for age and genetic confounders identified intestinal symptoms (OR = 44.807, 95%CI: 22.346-89.842), perianal complications (OR = 147.701, 95%CI:42.037-518.952), appendectomy (OR = 5.199, 95%CI: 2.927-9.233), history of allergy (OR = 3.801, 95%CI: 1.660-8.703),and rural residence history (OR = 7.273, 95%CI: 1.873-28.244) as independent risk determinants, while protective associations emerged across sociodemographic (female gender, higher education, office-worker, self-employed occupational status, non-working status, occupations devoid of physical exertion, elevated income) and dietary domains (milk consumption, chicken/fish intake, preserved foods, moderate fried/spicy food intake, alcohol consumption) (Figure 3).
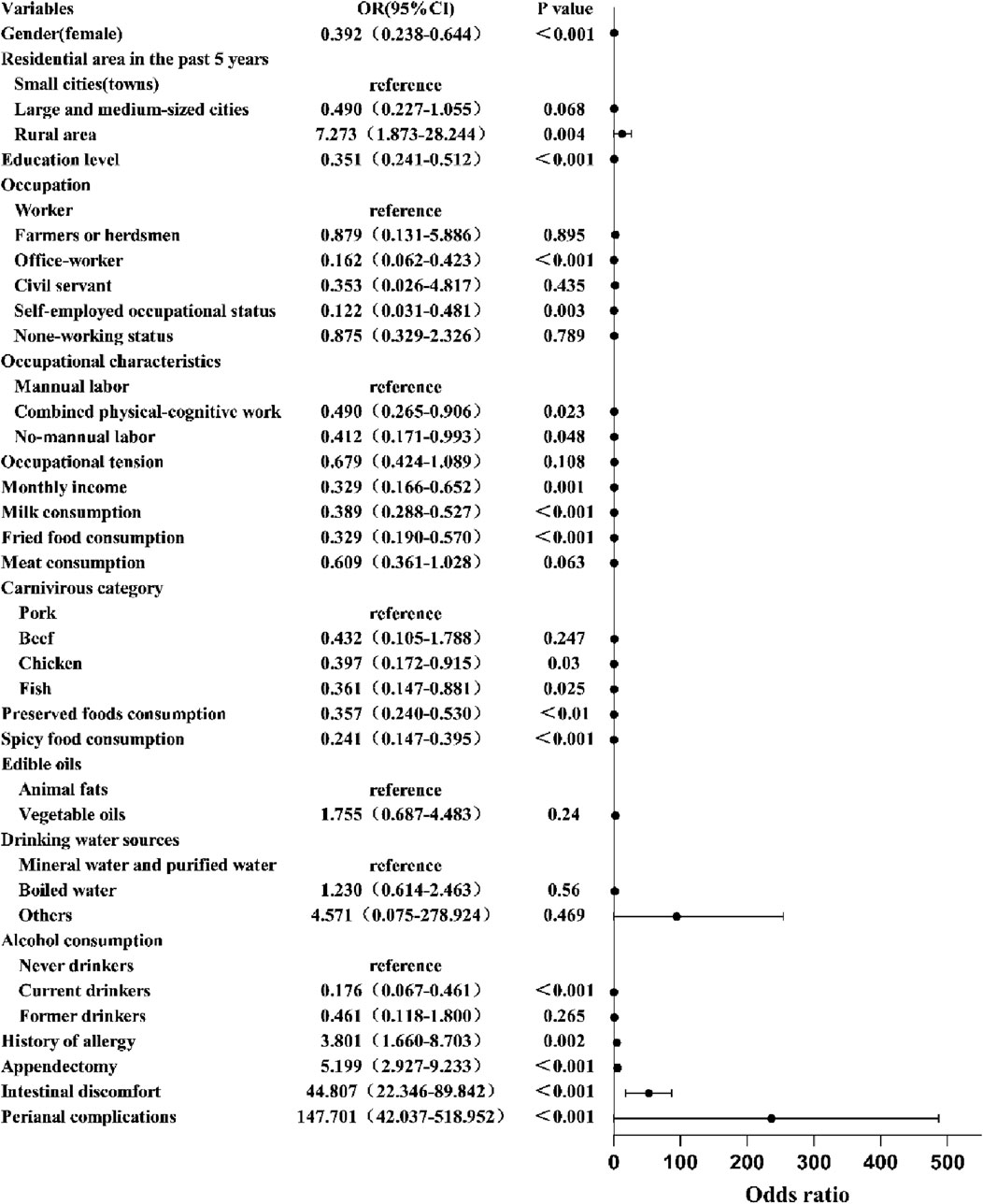
Figure 3. Multivariable analysis of factors influencing Crohn’s disease pathogenesis. The forest plot displays odds ratios (OR) and confidence intervals (CI) for various variables affecting an unspecified outcome. Significant associations, marked by dots and horizontal lines, show factors like gender, education level, and conditions like intestinal discomfort and perianal complications are highly significant (p < 0.001).
3.6 Diagnostic delay
3.6.1 Determinants of diagnostic delay in Crohn’s disease
In this cohort of 200 CD patients, diagnostic delay (median duration: 23 months, IQR 12–48) occurred in 48.0% (n = 96). Univariate screening identified advanced age at diagnosis, recent residential area (past 5 years), and absence of abdominal pain as significant predictors of delayed diagnosis (Tables 1, 2). Multivariable logistic regression confirmed advanced age at diagnosis as an independent risk factor (OR = 1.035 per additional year, 95% CI: 1.010–1.060, P = 0.005), while abdominal pain exhibited protective effects against diagnostic delay (OR = 2.088, 95% CI: 1.136–3.838, P = 0.018), suggesting symptom-driven diagnostic acceleration in symptomatic presentations (Figure 4).
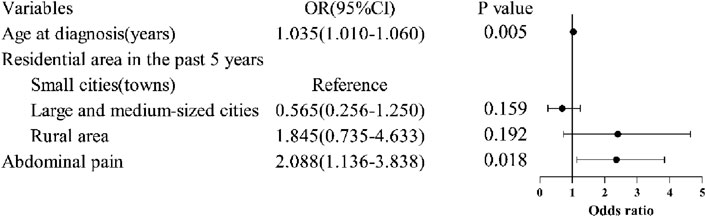
Figure 4. Multivariable analysis of factors influencing diagnostic delay in Crohn’s disease. Multivariable logistic regression confirmed advanced age at diagnosis as an independent risk factor, while abdominal pain exhibited protective effects against diagnostic delay.
3.6.2 Temporal correlates of diagnostic delay in Crohn’s disease
Spearman’s rank correlation analysis revealed significant positive associations between diagnostic delay duration and both advanced age at diagnosis (r = 0.302, P = 0.003) and frequent consumption of refrigerated foods (r = 0.219, P = 0.032), while educational attainment and other dietary behaviors showed no statistically meaningful correlations (Figure 5).
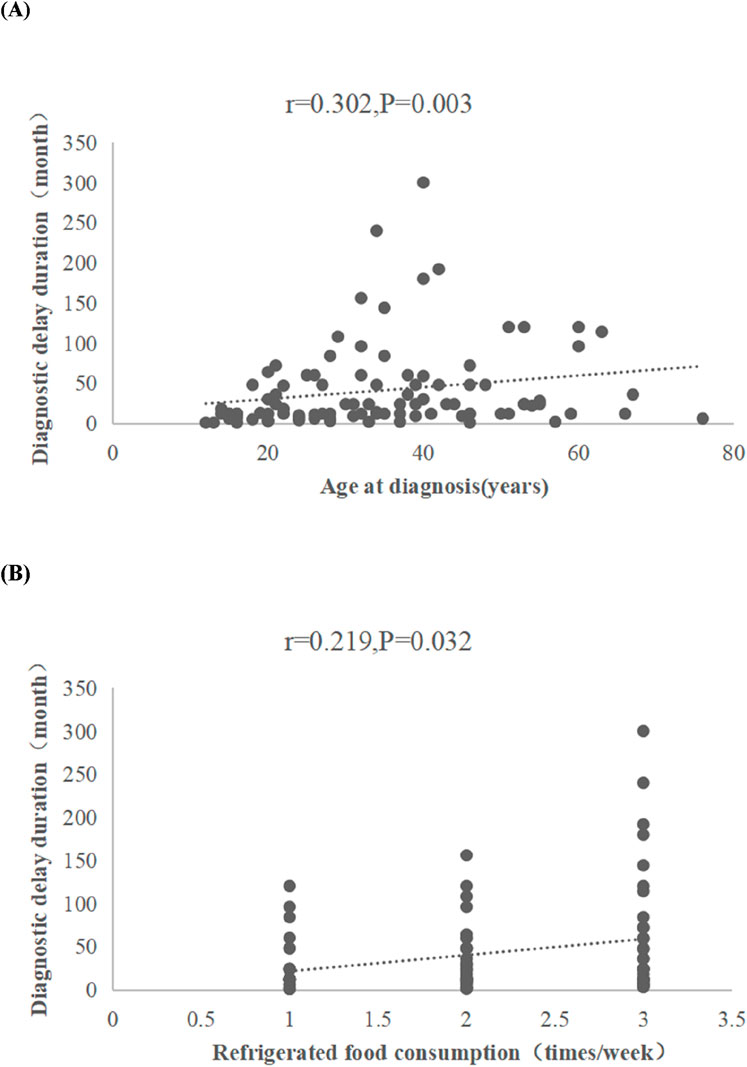
Figure 5. Spearman’s rank correlation analysis between diagnostic delay duration and relevant variables. Scatter plots show correlations related to diagnostic delay duration. (A) This scatter plot graphs age at diagnosis against diagnostic delay, demonstrating a significant positive correlation. (B) This scatter plot graphs refrigerated food consumption frequency against diagnostic delay, demonstrating a positive correlation.
3.6.3 Univariate logistic regression analysis of intestinal obstruction, perforation, and surgical intervention
Univariate logistic regression analysis demonstrated no statistically significant associations between diagnostic delay duration and complications including intestinal obstruction (OR = 1.12, 95% CI: 0.89–1.41), perforation (OR = 0.97, 95% CI: 0.72–1.30), or surgical intervention rates (OR = 1.08, 95% CI: 0.93–1.25), with all comparisons exceeding the α = 0.05 threshold (Table 5).
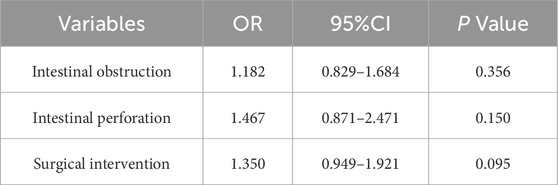
Table 5. Univariate logistic regression analysis of intestinal obstruction, perforation, and surgical intervention.
4 Discussion
Crohn’s disease (CD), a chronic idiopathic inflammatory bowel disorder, exhibits rising incidence in China, though epidemiological data remain scarce in coastal regions. This study reports a crude CD prevalence of 17.48/105 and incidence of 2.30/105 in Yancheng, a coastal city—substantially higher than rates in Hong Kong SAR (1.25/100,000) (Ng et al., 2013), Guangdong Province (1.09/100,000) (Zeng et al., 2013), Taiwan region (0.81/100,000) (Kuo et al., 2024), Wuhan City (0.51/100,000) (Jiang et al., 2007), Chengdu City (0.14/100,000),Xi’an City (0.07/100,000 (Ng et al., 2013), yet below Western benchmarks (Australia: 29.3/105; Canada: 319.0/105) (Ng et al., 2017). This epidemiological pattern suggests coastal regions may constitute disease hotspots influenced by distinct environmental determinants.
The cohort demonstrated male predominance (M:F = 2.07:1), and median diagnosis age of 29 years (IQR 20–39). This demographic profile aligns with global epidemiological patterns of CD in terms of gender distribution and age-stratified incidence. The observed male preponderance may be mediated through sex-specific environmental exposures and differential sex hormone profiles (Tshikudi et al., 2025). The study cohort demonstrated geographical clustering in Tinghu District (26.0% vs. 3.5% in Xiangshui County), likely reflecting imbalances between healthcare resources and economic development. Disease phenotypes aligned with global patterns: ileocolonic involvement (L3:47.0%), non-stricturing, non-penetrating disease behavior (B1:55.0%), and frequent perianal complications (60.5%). Epidemiological studies have demonstrated that CD patients with concomitant perianal complications exhibit 3- to 4-fold elevated incidence and prevalence rates compared to the general population (H Everhov et al., 2025). Biologic therapy predominance (89.0%) underscores treatment intensification trends, while simultaneously indicating potential enrollment bias toward patients with more severe disease phenotypes or treatment-refractory profiles.
The culinary profile of Yancheng region is characterized by a high-sodium and capsaicin-rich dietary regimen, with preserved foods—including traditional fermented sausages and estuarine mud snails (bullacta exarata)—occupying a prominent nutritional niche due to their organoleptic distinctiveness and superior preservation properties under humid subtropical conditions. Contrary to established dietary risks (Papadimitriou et al., 2025), multivariable analysis identified protective associations for milk (OR = 0.389), fried food (OR = 0.329), preserved foods (OR = 0.357), alcohol consumption (OR = 0.176) and spicy intake (OR = 0.241). These paradoxical findings may reflect reverse causation: post-diagnosis dietary modifications (e.g., self-imposed elimination diet (Tingting et al., 2022)), which may distort retrospective exposure assessments. Mechanistically plausible hypotheses exist, including the potential protective effects of probiotics in dairy products and mucosal adaptation to dietary spices. Notably, seafood showed null associations, potentially obscured by similar behavioral adjustments. Female sex, lower occupational physical demands, higher educational attainment, and elevated socioeconomic status conferred additional protection, potentially mediated by enhanced health literacy and proactive healthcare-seeking behaviors. Animal-derived proteins from fish and poultry, as key components of the Mediterranean diet, provide essential amino acids, vitamin B12, and bioavailable heme iron. Their consumption is inversely associated with Crohn’s disease (CD) incidence, potentially mediated through maintaining metabolic homeostasis and preserving muscle mass (Guasch-Ferré and Willett, 2021). The observed dietary paradoxes likely reflect reverse causation bias introduced by post-diagnosis dietary modifications, underscoring the necessity for large-scale prospective cohorts with longitudinal dietary monitoring to disentangle true etiological relationships from behavioral adaptations. Rural residency was identified as an independent risk factor for CD, with exposure pathways likely mediated through environmental contaminants in water supplies, barriers to healthcare access, and insufficient health awareness. Our cohort analysis demonstrates a significantly elevated risk of Crohn’s disease among atopic individuals (OR = 3.801, 95%CI:1.660-8.703), consistent with other study (Virta et al., 2013) Shared environmental-immunogenetic mechanisms underlie both allergic diseases and IBD. Mast cells serve as key effector cells in allergic responses, where allergen-specific IgE crosslinking triggers degranulation and release of histamine/leukotrienes. Critically, these pro-inflammatory mediators similarly contribute to Crohn’s disease pathogenesis (Kanchan et al., 2021). While an epidemiological link between appendectomy and subsequent CD diagnosis was observed, this finding is likely confounded by diagnostic misclassification. The considerable clinical mimicry of incipient CD and acute appendicitis often results in erroneous appendectomies prior to definitive IBD diagnosis. Early-onset intestinal symptoms and perianal complications may serve as clinical harbingers of elevated Crohn’s disease risk. It is reported that up to 30% of CD patients present with perianal complications at diagnosis, while up to 17% exhibit isolated perianal pathology preceding formal diagnosis (Eglinton et al., 2012). Consequently, vigilance for underlying Crohn’s disease is warranted in patients presenting with isolated perianal pathology, enabling timely diagnostic confirmation and reducing therapeutic delays.
Therapeutic efficacy during CD’s early “window of opportunity” is critically compromised by diagnostic delays. In anti-tumor necrosis factor (TNF) therapy efficacy trials, a substantial proportion of patients exhibit primary nonresponse, potentially attributable to prolonged diagnostic delays and subsequent irreversible intestinal architectural damage (Spencer et al., 2002). However, diagnostic delay during Crohn’s disease management has garnered increasing research attention, primarily categorized into patient-dependent delay and healthcare system-related delay. Diagnostic delays plagued 48% of cases (median 23 months) in this study, substantially exceeding the median durations reported in other countries (e.g., France: 5 months (Nahon et al., 2016), Switzerland: 9 months (Schoepfer et al., 2013), United States: 9.5 months (Furfaro et al., 2014)). Multivariable analysis identified advanced age at diagnosis (OR = 1.035) as an independent risk factor for diagnostic delay due to atypical presentations mimicking ischemic/medication-induced colitis (Jia-ming and Hong, 2018). Notably, patients with late-onset disease exhibit a significantly elevated risk of adverse clinical outcomes (Singh et al., 2024). Yancheng’s diagnostic delay prevalence reflects systemic healthcare disparities and inadequate diagnostic infrastructure (limited fecal calprotectin/microbiome testing). The current distribution of IBD specialists in China remains suboptimal, with clinicians predominantly concentrated in developed regions, resulting in a critical shortage of specialized personnel in primary care hospitals. According to data from the China Crohn’s and Colitis Foundation (CCCF), the Yancheng region has only six IBD-certified gastroenterologists, with four at Yancheng NO.1 People’s Hospital and two at Yancheng TCM Hospital. These systemic deficiencies mirror broader challenges in China’s IBD care cascade. Urgent reforms—specialist training programs, tiered referral networks, and point-of-care biomarker deployment—are imperative to mitigate complication risks in late-onset CD populations. Contrastingly, abdominal pain (OR = 2.088) emerged as a protective determinant, potentially mediated through severe pain-induced prompt medical consultation that expedited diagnostic confirmation.
Spearman’s analysis demonstrated significant positive associations between diagnostic delay duration and both age at diagnosis (r = 0.302, P = 0.003) and frequency of refrigerated food consumption (r = 0.219, P = 0.032), suggesting that advanced age and frequent refrigerated dietary exposures may elevate risks of delayed diagnosis. The latter association may be linked to intestinal dysbiosis induced by prolonged consumption of refrigerated food (e.g., leftover dishes, cold beverages) or exacerbation of mucosal damage from thermal stress due to low-temperature exposure, necessitating validation of these mechanistic pathways through prospective studies. Under the cold-chain hypothesis, advancements in industrial and domestic refrigeration have led to frequent human exposure to psychrotrophic bacteria capable of proliferating in chilled environments. Notably, Yersinia species may exacerbate enteric inflammation in genetically susceptible individuals. However, given their typically low pathogenicity, the reported infection rates remain disproportionately low relative to exposure prevalence, potentially resulting in diagnostic delays (Hugot et al., 2021). Chinese cohorts reveal protective effects against CD in households without refrigerators (Shi et al., 2008), reinforcing temperature-dependent microbial dysbiosis as a plausible mechanism. Furthermore, diagnostic delay duration demonstrates significant associations with exacerbated intestinal architectural damage, increased necessity for CD-related surgical interventions, and elevated risks of adverse long-term prognostic outcomes (Schoepfer et al., 2013; Jia et al., 2018). Not with standing the absence of statistically significant associations between diagnostic delay and risks of intestinal obstruction, intestinal perforation, or surgical intervention in univariate analyses within this cohort, these null findings may be attributable to limitations in statistical power or residual confounding. Subsequent investigations with expanded sample sizes are warranted to clarify these relationships.
The substantial epidemiological burden of Crohn’s disease in coastal Yancheng—marked by elevated incidence rates and protracted diagnostic delays—underscores the urgency of region-specific prevention strategies. While our findings illuminate novel environmental-dietary interactions and healthcare system vulnerabilities, validation through population-based cohorts remains imperative to address coastal China’s epidemiological data gap. Priority interventions must establish multidisciplinary task forces integrating fecal biomarker screening, specialist telemedicine networks, and community-based cold-chain food safety initiatives, particularly targeting aging populations and high-risk dietary patterns. Concurrently, national IBD registries should be expanded to monitor delayed diagnosis consequences on long-term disability-adjusted life years (DALYs), ensuring equitable resource allocation across rapidly developing regions.
5 Limitations
This hospital-based retrospective design inherently carries selection bias, limiting generalizability to population-level CD epidemiology in coastal China. The findings primarily reflect CD incidence patterns within the Yancheng region. Recall bias in dietary/lifestyle assessments—particularly regarding pre-diagnosis exposures—and unmeasured environmental confounders (industrial pollutants, waterborne contaminants) may distort observed associations. Besides, changes in relevant indicators during disease progression may have some impact on observed outcomes such as treatment modalities. Furthermore, the lack of granular treatment data (biologic dosing schedules, concomitant immunomodulators) and longitudinal outcome measures precludes analysis of therapeutic durability and complication trajectories. This study primarily provides a descriptive analysis of region-specific epidemiological characteristics of CD, without delving into underlying pathological mechanisms; its preliminary nature warrants further in-depth investigation. These limitations necessitate future validation through prospective population-based cohorts integrating multi-omics profiling (metagenomics, metabolomics) with geospatial environmental monitoring to elucidate coastal CD pathogenesis.
6 Conclusion
The Yancheng region exhibits higher CD prevalence and incidence rates compared to national averages, with pronounced diagnostic delays. These findings highlight the need for targeted interventions to improve early diagnosis and mitigate healthcare burdens.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Yancheng TCM Hospital Affiliated to Nanjing University of Chinese Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
SJ: Writing – original draft, Formal Analysis, Data curation, Investigation. MZ: Investigation, Formal Analysis, Writing – original draft. ZZ: Resources, Validation, Investigation, Writing – original draft. YH: Writing – original draft, Investigation, Resources. LW: Investigation, Writing – original draft, Formal Analysis. SX: Supervision, Conceptualization, Writing – review and editing, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Jiangsu Provincal Chinese Medicine Science and Technology Development Program Project (MS2021071) and Postgraduate Research and Practice Innovation Program of Jiangsu Province (SJCX24_1032).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Chen Y. Y., Huang C. W., Chou J. W., Yen H. H. (2025). Epidemiology and temporal trends of IBD in central Taiwan. J. Crohns and Colitis 19, i2205–i2206. doi:10.1093/ecco-jcc/jjae190.1391
Cui G., Yuan A. (2018). A systematic review of epidemiology and risk factors associated with Chinese inflammatory bowel disease. Front. Med. 5, 183. doi:10.3389/fmed.2018.00183
Eglinton T. W., Barclay M. L., Gearry R. B., Frizelle F. A. (2012). The spectrum of perianal crohn's disease in a population-based cohort. Dis. Colon Rectum 55 (7), 773–777. doi:10.1097/DCR.0b013e31825228b0
Furfaro F., Sciurti R., Bezzio C., Dell'Era A., Ardizzone S., de Franchis R., et al. (2014). P617 Impact of diagnostic delay on clinical outcome of Crohn's disease (CD). J. Crohns and Colitis 8 (Suppl. ment_1), S327–S327. doi:10.1016/S1590-8658(14)60202-4
GBD 2017 Inflammatory Bowel Disease Collaborators (2020). The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. lancet Gastroenterology and hepatology 5 (1), 17–30. doi:10.1016/s2468-1253(19)30333-4
Guasch-Ferré M., Willett W. C. (2021). The Mediterranean diet and health: a comprehensive overview. J. Intern Med. 290 (3), 549–566. doi:10.1111/joim.13333
H Everhov Å., Eberhardson M., Söderling J., Nordenvall C., Halfvarson J., Ludvigsson J. F., et al. (2025). Cumulative incidence and prevalence of perianal diseases in patients with inflammatory bowel disease and in the population: a nationwide Swedish study. Scand. J. gastroenterology 60 (4), 349–354. doi:10.1080/00365521.2025.2476669
Hugot J. P., Dumay A., Barreau F., Meinzer U. (2021). Crohn's Disease: is the cold chain Hypothesis still hot?. J. Crohn's and colitis 15 (4), 678–686. doi:10.1093/ecco-jcc/jjaa192
Inflammatory Bowel Disease Group, Chinese Society of Gastroenterology, Chinese Medical Association (2024). Inflammatory Bowel Disease Quality Control Center of China. Chinese clinical practice guideline on the management of Crohn's disease(2023, Guangzhou). Chin. J. Inflamm. Bowel Dis. 8, 2–32. (in Chinese). doi:10.3760/cma.j.cn311367-20240109-00010
Jia X. M., Zhang J. X., Deng H., Guo Y. M., Tian S., Dong W. G. (2018). Effects of diagnostic delay on early disease of Crohn's disease (in Chinese). Chin. J. Pract. Intern. Med. 38 (3), 177–179. doi:10.3760/cma.j.issn.0254-1432.2018.05.005
Jia-ming Q., Hong Y. (2018). Special concerns for the specific populations with inflammatory bowel disease (in Chinese). Chin. J. Pract. Intern. Med. 38 (03), 177–179. doi:10.19538/j.nk2018030101
Jiang L., Xia B., Li J., Ye M., Deng C., Ding Y., et al. (2007). Risk factors for ulcerative colitis in a Chinese population: an age-matched and sex-matched case-control study. J. Clin. gastroenterology 41 (3), 280–284. doi:10.1097/01.mcg.0000225644.75651.f1
Kanchan K., Clay S., Irizar H., Bunyavanich S., Mathias R. A. (2021). Current insights into the genetics of food allergy. J. Allergy Clin. Immunol. 147 (1), 15–28. doi:10.1016/j.jaci.2020.10.039
Kucharzik T., Ellul P., Greuter T., Rahier J. F., Verstockt B., Abreu C., et al. (2021). ECCO Guidelines on the prevention, diagnosis, and management of infections in inflammatory bowel disease. J. Crohn's and colitis 15 (6), 879–913. doi:10.1093/ecco-jcc/jjab052
Kuo C. J., Lin C. Y., Le P. H., Kuo Y. W., Hsu C. M., Lai M. W., et al. (2024). Temporal Trends of Inflammatory Bowel Diseases in Taiwan from 2016 to 2020: a Population-Based Study. Dig. Dis. Sci. 69 (9), 3172–3179. doi:10.1007/s10620-024-08518-2
Lujan R., Buchuk R., Focht G., Yogev D., Greenfeld S., Ben-Tov A., et al. (2024). Early initiation of biologics and disease outcomes in adults and children with inflammatory bowel diseases: results from the Epidemiology Group of the nationwide Israeli inflammatory bowel disease research Nucleus cohort. Gastroenterology 166 (5), 815–825.e22. doi:10.1053/j.gastro.2024.01.041
Nahon S., Lahmek P., Paupard T., Lesgourgues B., Chaussade S., Peyrin-Biroulet L., et al. (2016). Diagnostic delay is associated with a greater risk of early surgery in a French cohort of Crohn's Disease patients. Dig. Dis. Sci. 61 (11), 3278–3284. doi:10.1007/s10620-016-4189-z
Ng S. C., Tang W., Ching J. Y., Wong M., Chow C. M., Hui A. J., et al. (2013). Incidence and phenotype of inflammatory bowel disease based on results from the Asia-Pacific Crohn's and colitis epidemiology study. Gastroenterology 145 (1), 158–165.e2. doi:10.1053/j.gastro.2013.04.007
Ng W. K., Wong S. H., Ng S. C. (2016). Changing epidemiological trends of inflammatory bowel disease in Asia. Intestinal Res. 14 (2), 111–119. doi:10.5217/ir.2016.14.2.111
Ng , Shi H. Y., Hamidi N., Underwood F. E., Tang W., Benchimol E. I., et al. (2017). Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet London, Engl. 390 (10114), 2769–2778. doi:10.1016/s0140-6736(17)32448-0
Papadimitriou K., Deligiannidou G. E., Voulgaridou G., Giaginis C., Papadopoulou S. K. (2025). Nutritional habits in Crohn's Disease onset and management. Nutrients 17 (3), 559. doi:10.3390/nu17030559
Roda G., Chien Ng S., Kotze P. G., Argollo M., Panaccione R., Spinelli A., et al. (2020). Crohn's disease. Nat. Rev. Dis. Prim. 6 (1), 22. doi:10.1038/s41572-020-0156-2
Schoepfer A. M., Dehlavi M. A., Fournier N., Safroneeva E., Straumann A., Pittet V., et al. (2013). Diagnostic delay in Crohn's disease is associated with a complicated disease course and increased operation rate. Am. J. gastroenterology 108 (11), 1744–1754. quiz 1754. doi:10.1038/ajg.2013.248
Shi X., Zheng J., Guo Z., Chen F., Wang Z.(2008). Correlated pathogenetic factors of Crohn’s disease: a case-control study (in Chinese). Chin. J. Gastroenterology 13 (5), 293–296.
Singh S., Poulsen G. J., Bisgaard T. H., Bonfils L., Jess T. (2024). Epidemiology of elderly onset IBD: a nationwide population-based cohort Study. Clin. gastroenterology hepatology official Clin. Pract. J. Am. Gastroenterological Assoc. 23, 1204–1215.e11. doi:10.1016/j.cgh.2024.08.011
Spencer D. M., Veldman G. M., Banerjee S., Willis J., Levine A. D. (2002). Distinct inflammatory mechanisms mediate early versus late colitis in mice. Gastroenterology 122 (1), 94–105. doi:10.1053/gast.2002.30308
Tingting Y., Wenjing T., Wenjing X., Guihua X. J. C. J. o. G. (2022). Progress of research on dietary restriction behavior and its influencing factors in patients with inflammatory bowel disease (in Chinese). Chin. J. Gastroenterology, 439–443.
Tshikudi D. M., Bernstein C. N., Mishra S., Ghia J. E., Armstrong H. K. (2025). Influence of biological sex in inflammatory bowel diseases. Nat. Rev. Gastroenterology and hepatology 22, 415–437. doi:10.1038/s41575-025-01038-y
Ungaro R. C., Naegeli A. N., Choong C. K., Shan M., Zheng X. S., Hunter G. T., et al. (2024). Early use of biologics reduces healthcare costs in Crohn's Disease: results from a United States population-based cohort. Dig. Dis. Sci. 69 (1), 45–55. doi:10.1007/s10620-023-07906-4
Virta L. J., Ashorn M., Kolho K. L. (2013). Cow's milk allergy, asthma, and pediatric IBD. J. Pediatr. Gastroenterol. Nutr. 56 (6), 649–651. doi:10.1097/MPG.0b013e318285e9d8
Wang X. Q., Zhang Y., Xu C. D., Jiang L. R., Huang Y., Du H. M., et al. (2013). Inflammatory bowel disease in Chinese children: a multicenter analysis over a decade from Shanghai. Inflamm. bowel Dis. 19 (2), 423–428. doi:10.1097/MIB.0b013e318286f9f2
Xu L., He B., Sun Y., Li J., Shen P., Hu L., et al. (2023). Incidence of inflammatory bowel disease in urban China: a nationwide population-based Study. Clin. gastroenterology hepatology official Clin. Pract. J. Am. Gastroenterological Assoc. 21 (13), 3379–3386.e29. doi:10.1016/j.cgh.2023.08.013
Keywords: Crohn’s disease, epidemiology, diagnostic delay, China, Yancheng
Citation: Jin S, Zhang M, Zhou Z, Hao Y, Wang L and Xu S (2025) Crohn’s disease in coastal China: epidemiological profile and determinants of diagnostic delay in the Yancheng cohort. Front. Physiol. 16:1643597. doi: 10.3389/fphys.2025.1643597
Received: 11 June 2025; Accepted: 04 August 2025;
Published: 25 August 2025.
Edited by:
George Grant, Independent Researcher, Aberdeen, United KingdomReviewed by:
Yi Li, Nanjing University of Aero, ChinaChen Pan, Zhongshan Hospital of Traditional Chinese Medicine, China
Copyright © 2025 Jin, Zhang, Zhou, Hao, Wang and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Su Xu, eHN0Y204MUAxMjYuY29t
 Shengnan Jin
Shengnan Jin Maozhen Zhang1
Maozhen Zhang1