- 1Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 2Department of Orthopedics and Traumatology, Longhua Hospital Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 3Shanghai Geriatric Institute of Chinese Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 4Department of Respiratory Medicine, Longhua Hospital Shanghai University of Traditional Chinese Medicine, Shanghai, China
Background: Post-COVID-19 syndrome (PCS) describes a constellation of persistent or new symptoms lasting beyond the acute phase of SARS-CoV-2 infection. Emerging evidence suggests that exercise is a cost-effective and accessible intervention that may enhance pulmonary function, improve cardiopulmonary circulation, regulate emotional status, and alleviate symptoms of PCS. However, robust evidence supporting the efficacy of exercise therapy in PCS remains limited. This systematic review and meta-analysis aimed to elucidate the therapeutic potential of exercise therapy in PCS.
Method: A search of the PubMed, Embase, Web of Science, and Ovid databases up to March 25, 2025 yielded 33 randomized controlled trials (with 2,895 participants) for meta-analysis.
Result: The results showed that exercise therapy significantly improved the multi-dimensional outcomes of patients with PCS. Bayesian network meta-analysis indicated that the combination of aerobic exercise and respiratory muscle training had the best effect on lung function. Multimodal exercise significantly improved the results of the six-minute walk test, the dyspnea score, and peak oxygen uptake. Mental Health and Mental Component Summary scores improved significantly in the group that received exercise therapy (P<0.01).
Conclusion: The results of this meta-analysis confirm that exercise can significantly improve quality of life and the emotional state of patients with PCS. They also provide evidence for a treatment strategy in patients with post-COVID-19 sequelae.
Systematic Review registration: https://www.crd.york.ac.uk/PROSPERO/#myprospero, identifier CRD420251034187.
Introduction
Post-COVID-19 syndrome (PCS) is a multisystem disorder in which a subset of patients develop persistent or new symptoms following the acute phase of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. These symptoms manifest as organ dysfunction that cannot be explained by alternative diagnoses and often involve protracted fatigue, cardiopulmonary compromise, and neurocognitive impairment (Pierce et al., 2022; Yong, 2021; Ceban et al., 2022). SARS-CoV-2 is classified as a coronavirus because its surface protrudes like a crown. In most cases, its symptoms are similar to those of the common cold, namely, coughing and fever. Severely ill patients present with typical respiratory symptoms, including severe breathing difficulties, hypoxemia, and acute respiratory distress syndrome, which may progress to a systemic inflammatory storm and even to sepsis or shock (Yuce et al., 2021). In the post-acute phase following resolution of symptoms or during a prolonged period of immunocompromise, individuals may experience a persistent or novel constellation of symptoms, including fatigue and malaise, palpitations and chest pain, anorexia and diarrhea, anxiety and depression, cognitive decline and memory impairment, and concurrent symptom clusters. The incidence of PCS ranges from 10% to 35%, being more common among the older adult with chronic underlying diseases and in individuals with weakened immune systems. There is some evidence to suggest that PCS is more common in women (Yong, 2021; Majumder and Minko, 2021).
In the absence of any specific diagnostic criteria, PCS is usually diagnosed based on the medical history and after exclusion of other conditions. There is no cure for this syndrome, and most of the treatments are symptomatic, such as drug therapy to relieve airway obstruction, alleviate pain, and combat anxiety. Behavioral cognitive therapy improves “brain fog,” cognitive impairment, and memory loss. Other non-pharmacological therapies may also be used for symptomatic relief (Habas et al., 2020; Kevadiya et al., 2021; Bamji, 2021). Exercise therapy, which includes aerobic exercise (AE), resistance training (RT), and respiratory muscle training (RMT), is a conservative, simple, and cost-effective treatment with several advantages, including a choice between a wide range of exercises and methods and exercises of varying intensity. Exercise is an important component of rehabilitation medicine, and our previous research has confirmed that it can significantly improve symptoms in patients with lumbar disc herniation and enhance their quality of life (Du et al., 2025). In a clinical cohort study, Tucker et al. found that exercise therapy reduced the incidence of cardiovascular disease, improved cardiopulmonary function, and enhanced the self-protection ability of the heart (Tucker et al., 2022). Smart et al. demonstrated that resistance exercise can enhance cardiopulmonary function, muscle mass, and functional capacity in healthy older adult individuals aged over 60 years. Furthermore, AE has been shown to significantly improve cognitive flexibility, working memory, and inhibitory control in healthy middle-aged and older adult (Ye et al., 2024). The combination of multiple exercise therapies may make the clinical effect more significant (Smart et al., 2022). Exercise therapy has not only brought about improvements in both organic and functional diseases, but also made contributions to the management of psychiatric disorders (Abdullahi et al., 2024). A cohort study by Harvey et al. found that regular exercise protected against symptoms of depression (Harvey et al., 2018), while Herring and Meyer found that RT and RMT could alleviate anxiety (Herring and Meyer, 2024).
There is still no systematic summary of its validity and accuracy in PCS. And traditional pairwise meta-analyses could not adequately compare different exercise modalities simultaneously, thus we employed a Bayesian network meta-analysis to integrate direct and indirect evidence across interventions. Therefore, this meta-analysis was performed to evaluate the clinical efficacy of exercise therapy in patients with PCS and its auxiliary role as a non-pharmacological treatment. Our analysis of three exercise methods (AE, RT and RMT) confirmed their feasibility and safety in multiple rehabilitation treatment models.
Materials and methods
Search strategy
The PubMed, Embase, Web of Science, and Ovid databases were searched through to 25 March 2025 for relevant clinical studies. This research is registered on PROSPERO (CRD420251034187).
Eligibility criteria
Studies were eligible for inclusion in the meta-analysis if they were randomized controlled clinical trials, the disease under investigation was PCS, the main intervention was exercise therapy, outcomes were described, and the publication language was English. No changes to the drug regimen during the month before the intervention or during the intervention were permitted. Furthermore, no restrictions were set for comparison countries. Eligible studies were required to include specific outcome indicators, such as lung function, peak oxygen uptake (VO2), and the modified Medical Research Council (mMRC) score, for evaluation of the effectiveness of exercise therapy in PCS. Figure 1 shows the process used to select studies for inclusion in the meta-analysis. Any differences were resolved by discussion until consensus was reached. No grey literature search was conducted because our focus was limited to peer-reviewed randomized controlled trials to ensure data quality and consistency. The detailed search strategy is shown in Table 1.
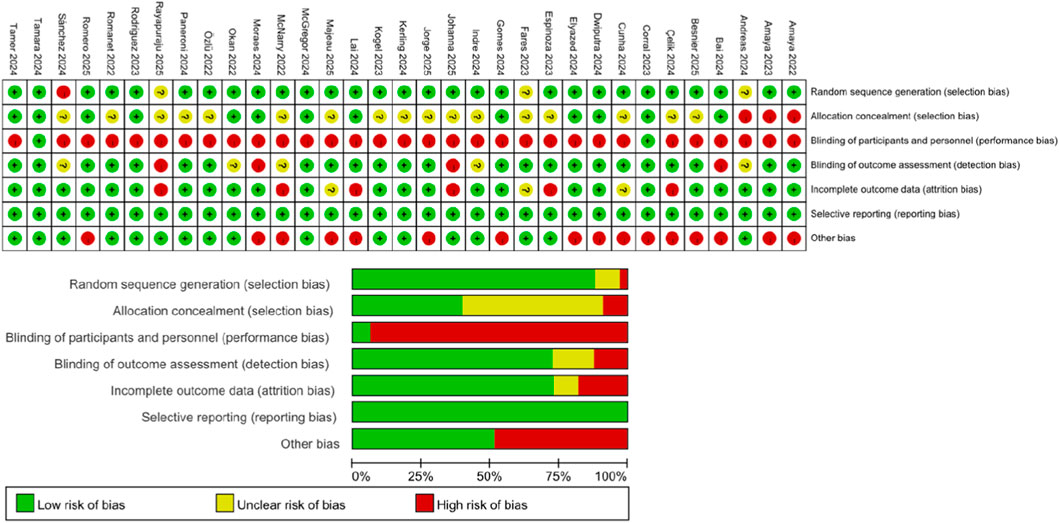
Risk of bias assessment
Two researchers independently evaluated the methodological quality of the included randomized controlled trials based on the Cochrane risk of bias criteria and classified each quality item as low risk, high risk, or uncertain risk. The seven items of bias in each trial evaluation included randomized sequence generation, allocation concealment, subject and personnel blinding, outcome assessment blinding, incomplete outcome data, selective reporting, and other biases.
Extraction of data
The reviewers extracted the following information from the included studies: authors, publication year, trial design, type of intervention, number of study participants, age and sex distribution, and study outcome indicators. If there were multiple subgroup outcomes under the same outcome measure in the study, we handled them using the sub-combination and union formula. For subgroups that performed multiple exercises (e.g., AE and core training), the inverse variance weighting method was used for merging. Subgroup data were merged by combining subgroup A (sample size N1, mean M1, standard deviation SD1) and subgroup B (N2, M2, SD2). If there were multiple subgroups of data that needed to be merged, the following formula was used:
First, the data for two of the subgroups were merged, after which the data obtained were merged with data for the third subgroup. Any differences in opinion among the reviewers were resolved by consensus or by consultation with a third-party reviewer.
Data analysis and statistical methodology
The data were analyzed using Review Manager 5.4. Continuous data are summarized as the mean difference, which was the 95% confidence interval (CI). Heterogeneity was evaluated using the I2 test. In accordance with the recommendation in version 5.1.0 of the Cochrane Handbook, we defined I2 as follows: <25%, mild heterogeneity; 25%–50%, moderate heterogeneity; and >50%, severe heterogeneity. We used a random effects model when heterogeneity was >50% and a fixed effects model when it was ≤50%. For studies with high heterogeneity, we used Stata14 software for the sensitivity analysis to evaluate the stability of the results. When the number of studies of the same indicator was sufficient, we performed a network meta-analysis using the Bayesian method and the GeMTC package in R 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria). This analytical framework is helpful for comparing the results obtained by various research groups and enhancing our understanding of the effectiveness of various intervention measures.
This study protocol was prospectively registered on PROSPERO (CRD420251034187).
Results
Literature screening
As shown in Figure 1, the database generated 418 unique records, 148 of which were excluded for being duplicates. After application of the screening criteria, a further 200 studies were excluded, leaving 70 potentially relevant studies. Thirty-six of these studies were found to have missing data and were excluded, as was one study in young children, leaving 33 studies for inclusion in the meta-analysis (Del Corral et al., 2025; Romanet et al., 2022; Rodriguez-Blanco et al., 2023; de Moraes Sirydakis et al., 2024; Sánchez Milá et al., 2024; Rayapuraju et al., 2025; Paneroni et al., 2024; Lai et al., 2024; Okan et al., 2022; Elyazed et al., 2024; Jorge et al., 2025; Kerling et al., 2024; McNarry et al., 2022; Sánchez-Romero et al., 2025; Bileviciute-Ljungar et al., 2024; McGregor et al., 2024; Gaudreau-Majeau et al., 2025; Sick et al., 2025; Abo Elyazed et al., 2024; Bai et al., 2024; Özlü et al., 2022; Kogel et al., 2023; Dwiputra et al., 2024; Gomes Dos Santos et al., 2024; Çelik et al., 2024; Espinoza-Bravo et al., 2023; Cunha et al., 2024; Besnier et al., 2025; del Corral et al., 2023; Fares et al., 2023; Jimeno-Almazan et al., 2022; Jimeno-Almazan et al., 2023; Barz et al., 2024).
Characteristics of the included studies
Supplementary Table S1 shows the characteristics of the 33 included studies (involving 2,895 participants). All were published between 2022 and 2025. Two reviewers summarized the intervention methods used in the studies as follows: none (no exercise therapy); AE (aerobic exercise, such as jogging); RMT (respiratory muscle training); or RT (resistance training).
Risk of bias assessment
In the dimensions of random sequence generation (selection bias) and selective reporting (reporting bias), about 80% of the studies were found to be low risk, reflecting standardization of the randomization process and outcome reporting. Most studies did not report allocation concealment measures and were classified as risk uncertain. With regard to participant and personnel blinding, most studies were assessed as high risk because of the inability to blind the intervention (exercise therapy). The blinding methods used for assessment of outcomes were differentiated. Most studies assessed objective indicators (such as pulmonary function tests) in a blinded manner, so they were considered to be low risk for bias. However, some studies used subjective indicators and were deemed to be high risk because they did not clarify the blinding method (red). Incomplete outcomes data are marked in red because of the high rate of loss to follow-up. Some studies were considered high risk because of an imbalance of baseline characteristics or an inadequate sample size (Figure 2).
Meta-analysis
Pulmonary function
Using a Bayesian network, we compared the effects of AE, RMT, AE + RMT, AE + RT, AE + RMT + RT, and no exercise therapy intervention on lung function (forced expiratory volume in 1 s [FEV1]/forced vital capacity [FVC]) in patients with PCS. The leverage plot (Supplementary Figure S1) shows that the studies were distributed within the curve, indicating good convergence of the Bayesian model. The surface under the cumulative ranking curve values indicated that the intervention was effective, supported treatment with higher scores, and suggested better FEV1/FVC outcomes (Supplementary Figure S2). The top three treatments were AE + RMT (97.62%), AE (76.33%), and RMT (40.62%). The results for the league table (Supplementary Table S2) and the forest plot (Figure 3) indicated that AE + RMT was more effective than the other treatments except for AE, while AE was more effective than no exercise therapy. The network geometry included five nodes representing interventions (None, AE, RMT, AE + RMT, AE + RT, AE + RMT + RT). Edges connecting nodes indicate direct comparisons available in the included RCTs (Supplementary Figure S1). The network was well connected with good model convergence.

Figure 3. Forest plot showing the results of network meta-analysis of pulmonary function. FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
Peak VO2
Peak VO2 represents the highest oxygen uptake over a 30-s interval attained during a particular test. Seven of the included studies used peak VO2 as an outcome measure. After exclusion of the 2024 study by Kerling et al. (2024), which showed large differences in peak VO2 at baseline, we compared the effects of exercise versus non-exercise interventions on the severity of symptoms of PCS in the remaining six randomized controlled trials. The forest plot showed that the experimental group had a statistically significant reduction in peak VO2 when compared with the control group (Z = 3.02, P = 0.003) and I2 = 0%, suggesting that exercise intervention could effectively improve lung function in patients with PCS (Supplementary Figure S3).
Six-minute walk test
Ten studies were included. As shown in Supplementary Figure S8, we divided these studies into two subgroups for analysis. The first subgroup compared the difference in efficacy between exercise intervention and non-exercise intervention. Four studies that compared the difference between AE + RMT + RT and non-exercise intervention were extracted as the second subgroup. The forest plot showed that the experimental group had a statistically significant advantage in terms of improvement in the 6MWT distance when compared with the control group (Z = 6.13, P < 0.00001) (Supplementary Figure S4). Considering the high heterogeneity (I2 = 83%), we performed a sensitivity analysis (Supplementary Figure S5), the result for which was relatively robust. For the second subgroup, we found that AE + RMT + RT was more effective than no exercise intervention in the control group (Z = 14.26, P < 0.00001) with I2 = 0%, suggesting that the combination intervention of AE + RMT + RT could effectively improve mobility in patients with PCS.
Modified medical research council score
The mMRC is used to assess the severity of dyspnea. Six studies were included (Supplementary Figure S10). The forest plot showed that the mMRC score was significant better in the experimental group than in the control group (Z = 2.88, P = 0.004) with I2 = 95% (Supplementary Figure S6). Considering the high heterogeneity, we conducted a sensitivity analysis, the results of which suggested that the outcome was relatively robust (Supplementary Figure S7), indicating that exercise therapy can effectively improve dyspnea in patients with PCS.
Mental health
Mental health was assessed using the Mental Health (MH) and Mental Component Summary (MCS) tools, both of which are derived from the SF-36 and SF-12. Five studies used MH and five used the MCS as outcome indicators (Supplementary Figures S8, S9). Psychological status was found to be significantly better in the experimental group than in the control group (MH, Z = 2.63, P = 0.008, I2 = 0%; MCS, Z = 4.09, P < 0.0001, I2 = 10%), suggesting that exercise intervention can effectively improve the mental health status of patients with PCS.
Discussion
The most common symptom of PCS is fatigue, accompanied by dyspnea and chest pain. Other symptoms include cognitive impairment, palpitations, autonomic dysfunction, joint pain, and muscle pain (Tsuji et al., 2022; Cao et al., 2022; Shafqat et al., 2024; van Doremalen et al., 2020). Mental health is affected when the body is under stress, with many reports of patients under physical stress developing symptoms of anxiety and depression. Moreover, SARS-CoV-2 has a greater ability for immune escape, which may lead to more lasting impairment of the immune system.
The fatigue associated with PCS may be related to blocking of signal transduction as a result of chronic inflammatory invasion. However, a cross-sectional analysis found no significant association between proinflammatory markers and chronic fatigue in most cases. It is possible that a combination of central, peripheral, and psychological factors are involved in the development of post-COVID-19 fatigue. Damage to olfactory neurons leads to increased resistance to drainage of cerebrospinal fluid through the lamina cribrosa, which may contribute to fatigue in patients with PCS. Prolonged exposure to inflammation and cell-mediated immunity leads to decreased metabolism in the frontal lobe and cerebellum, which may also lead to fatigue. Recent studies have shown that long-term social isolation can exacerbate anxiety and depression and promote aging, as can negative psychological and social factors. Finally, peripheral factors, such as direct infection leading to muscle damage, weakness, and muscle fiber and neural-related inflammation, may exacerbate fatigue (Cao et al., 2022; Shafqat et al., 2024; Mehandru and Merad, 2022; Scharf and Anaya, 2023).
Dyspnea is also a common symptom of PCS. Pulmonary dysfunction, indicated by abnormalities in pulmonary function, can still be observed at 1 month after discharge in patients hospitalized with COVID-19 (Carfi et al., 2020; Mandal et al., 2021; Halpin et al., 2021). A cohort study found that many patients with COVID-19 had cardiac involvement, persistent myocardial inflammation, and elevated serum troponin levels 71 days after diagnosis (Carfi et al., 2020; Puntmann et al., 2020). The main reason for the cardiac involvement is that the ACE2 receptor is strongly expressed in the human heart, providing a direct route for SARS-CoV-2 infection (Perez-Bermejo et al., 2020).
A similar study found that cognitive scores at 3 months after discharge were significantly lower, similar in 40% of patients to those with moderate traumatic brain injury, and similar in 26% of cases to those in patients with mild Alzheimer’s disease. This finding may be related to long-term social isolation. The COVID-19 epidemic has had a negative impact on people’s mental health. During recovery from the acute infection, people may develop longer-term psychiatric symptoms, including post-traumatic stress disorder, depression, anxiety, and obsessive-compulsive symptoms, which seriously impede recovery from PCS. People with dementia become more depressed, anxious, agitated, and lonely (Velayudhan et al., 2020). This may be related to invasion of the virus into neurons within the central nervous system, producing neuroinflammation and chronic degenerative changes. SARS-CoV-2 may also affect the permeability of the blood-brain barrier, allowing peripheral cytokines and other blood-derived foreign bodies to enter the central nervous system and exacerbate neuroinflammation (Romero-Sanchez et al., 2020).
A scientifically designed exercise program can be used to prevent, treat, or promote rehabilitation in patients with a variety of diseases. Exercise is widely used in the management of chronic disease and rehabilitation of sports injuries and to improve mental health. Exercise therapy includes AE, respiratory exercise, and resistance exercise and has been confirmed to aid recovery from illness. Initially, it was used mainly in patients recovering from conditions affecting the bones and joints, limbs, spine, and nervous system. In-depth studies have found that exercise therapy is an effective intervention for many diseases affecting the internal organs, and there is ample evidence of improvement in patients with psychiatric conditions. In terms of immune regulation, moderate exercise can upregulate the activity of natural killer cells, neutrophils, and macrophages and improve the detection and clearance of viruses. Studies have found that regular exercise reduces the risk of respiratory infections by 40%–50% (Nieman et al., 2011). AE can promote the proliferation of T cells (especially CD4+ Th1 cells) and memory B cells, which may accelerate the specific immune response to SARS-CoV-2. Long-term resistance exercise can reduce levels of inflammatory markers, such as IL-6 and tumor necrosis factor-alpha, which is an important way to alleviate the “cytokine storm” caused by COVID-19 (Kishimoto and Kang, 2022). Various exercises can improve antioxidant capacity, reduce levels of reactive oxygen species, and increase expression of malondialdehyde to varying degrees. It can also promote mitochondrial biosynthesis and improve energy metabolism disorders caused by COVID-19 (Varda et al., 2022). Considering that ACE2 is a viral receptor, some investigators have hypothesized that exercise may reduce viral invasion by regulating the expression and distribution of ACE2. Animal studies have also shown that exercise upregulates the circulating soluble form of ACE2 or competitively inhibits viral binding (Driggin et al., 2020). Recent aging-related phenotypes have incorporated psychosocial isolation, with patients who have PCS having more or less reduced social contact, which greatly slows disease recovery and increases mental distress. Respiratory exercise can reduce cortisol, increase β-endorphins, regulate immunity through the hypothalamic–pituitary–adrenal axis, and alleviate the suppression of immunity by COVID-19-related emotional stress (Pizzorno, 2023). AE can also promote the release of endorphins and serotonin, improve the patient’s mental health, restore a sense of control over the body, and reduce “fear of disease” (de Oliveira et al., 2022).
Limitations
The results of this meta-analysis of the existing literature underscore the effectiveness of exercise therapy in patients recovering from COVID-19. However, which type of exercise is most effective and its exact content have not been clarified, and whether there is a difference in effect between long-term exercise and short-term exercise has not been explored. Another problem worth considering is the lack of consistency in the evaluation criteria used. These criteria vary according to the type of exercise, which is an impediment to further research in this area. Potential publication bias cannot be completely excluded, as most included studies were small-scale and published in peer-reviewed journals. We found that most of the relevant studies in SportDiscus database were already included in the four databases we explored. However, this database better reflects the professionalism of exercise therapy, so we will take full account of its content in future research to explore the advantages of exercise therapy. In addition, long-term follow-up data were lacking, and there was variability in the definitions of PCS and outcome measures across studies.
Prospects
In the future, we will explore the effect of exercise therapy on the course of PCS further in the hope of formulating consistent evaluation criteria and developing an efficient method for assessment of cognitive function, emotional state, physical function, cardiopulmonary status, and quality of life in these patients. The ultimate goal will be to identify the best treatment strategy and explore the effects of combined exercise based on multimodal intervention.
Conclusion
The severity of the symptoms of COVID-19 are lessening with the passage of time but still cannot be ignored. The existing treatments are symptomatic only, and there is no cure for this illness. Therefore, patients need to engage with other rehabilitation strategies. Exercise is becoming increasingly popular as a convenient and effective treatment. Using a seven-item data scale, we have confirmed that exercise therapy can significantly improve lung function, physical activity status, and emotional status in patients with PCS. Combined with the existing evidence, we believe that exercise is a safe and effective treatment for these patients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
SD: Resources, Project administration, Software, Formal Analysis, Investigation, Data curation, Visualization, Writing – original draft, Conceptualization, Validation, Writing – review and editing, Methodology, Supervision, Funding acquisition. ZC: Software, Investigation, Resources, Funding acquisition, Writing – review and editing, Writing – original draft, Formal Analysis, Visualization, Validation, Methodology, Data curation, Supervision, Project administration, Conceptualization. XX: Validation, Writing – original draft, Resources, Funding acquisition, Writing – review and editing, Methodology, Conceptualization. TL: Methodology, Validation, Formal Analysis, Data curation, Supervision, Writing – original draft, Writing – review and editing. JY: Investigation, Conceptualization, Funding acquisition, Methodology, Writing – review and editing, Resources, Writing – original draft.
Funding
The authors declare that financial support was received for the research and/or publication of this article. The study was supported by the Science and Technology Development Project of Shanghai University of Traditional Chinese Medicine in 2023 (23KFW18); Shanghai University of Traditional Chinese Medicine Emergency Research Project on Omicron infection with COVID-19 in 2022 (2022YJ-12); Pudong New Area Famous Traditional Chinese Medicine Studio Construction Project (PDZY-2025-0715).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2025.1656713/full#supplementary-material
References
Abdullahi A., Wong T. W., Ng S. S. (2024). Understanding the mechanisms of disease modifying effects of aerobic exercise in people with alzheimer's disease. Ageing Research Reviews 94, 102202. doi:10.1016/j.arr.2024.102202
Abo Elyazed T. I., El-Moneim Abd El-Hakim A. A., Saleh O. I., Fadel Sonbol M. M., Assad Eid H., Moazen E., et al. (2024). Diaphragmatic strengthening exercises for patients with post COVID-19 condition after mild-to-moderate acute COVID-19 infection: a randomized controlled study. J. Rehabilitation Med. 56, jrm25491. doi:10.2340/jrm.v56.25491
Bai B., Xu M., Zhou H., Liao Y., Liu F., Liu Y., et al. (2024). Effects of aerobic training on cardiopulmonary fitness in patients with long COVID-19: a randomized controlled trial. Randomized Control. Trial 25 (1), 649. doi:10.1186/s13063-024-08473-3
Bamji A. N. (2021). Infection with SARS-CoV-2 is not the same as covid-19. Bmj 374. doi:10.1136/bmj.n1896
Barz A., Berger J., Speicher M., Morsch A., Wanjek M., Rissland J., et al. (2024). Effects of a symptom-titrated exercise program on fatigue and quality of life in people with post-COVID condition - a randomized controlled trial. Sci. Rep. 14 (1), 30511. doi:10.1038/s41598-024-82584-4
Besnier F., Malo J., Mohammadi H., Clavet S., Klai C., Martin N., et al. (2025). Effects of cardiopulmonary rehabilitation on cardiorespiratory fitness and clinical symptom burden in long COVID. Am. J. Phys. Med. and Rehabilitation 104 (2), 163–171. doi:10.1097/PHM.0000000000002559
Bileviciute-Ljungar I., Norrefalk J. R., Borg K. (2024). Improved functioning and activity according to the international classification of functioning and disability after multidisciplinary telerehabilitation for Post-COVID-19 Condition-A randomized control Study. J. Clin. Med. 13 (4), 970. doi:10.3390/jcm13040970
Cao X., Li W., Wang T., Ran D., Davalos V., Planas-Serra L., et al. (2022). Accelerated biological aging in COVID-19 patients. Nat. Communications 13 (1), 2135. doi:10.1038/s41467-022-29801-8
Carfi A., Bernabei R., Landi F., Against C-P-Acsg G. (2020). Persistent symptoms in patients after Acute COVID-19. Jama 324 (6), 603–605. doi:10.1001/jama.2020.12603
Ceban F., Ling S., Lui L. M. W., Lee Y., Gill H., Teopiz K. M., et al. (2022). Fatigue and cognitive impairment in Post-COVID-19 Syndrome: a systematic review and meta-analysis. Brain, Behavior, Immunity 101, 93–135. doi:10.1016/j.bbi.2021.12.020
Çelik Z., Kafa N., Güzel N. A., Köktürk N. (2024). The effects of physical activity tele-counseling intervention on physical activity, functional performance, and quality of life in post-COVID-19 conditions: a randomized controlled trial. Expert Rev. Respir. Med. 18 (5), 321–331. doi:10.1080/17476348.2024.2363862
Cunha A. C. R., Silva J. C., Garcês C. P., Magnabosco Sisconeto T., Rezende Nascimento J. L., Luiza Amaral A. (2024). Online and face-to-face mat pilates training for long COVID-19 patients: a randomized controlled trial on health outcomes. Int. J. Environ. Res. and Public Health Electronic Resour. 21 (10), 1385. doi:10.3390/ijerph21101385
de Moraes Sirydakis M. E., Danielevicz A., de Melo P. U. G., Bregalda J., Constantini M. I., Pelliciari G., et al. (2024). Improving quality of life, sleep and mental health through multicomponent training versus Brazilian recommendations of physical activity in post-COVID-19 patients: core-study–a randomized controlled trial. Ment. Health Phys. Activity 27. doi:10.1016/j.mhpa.2024.100615
de Oliveira L. R. S., Machado F. S. M., Rocha-Dias I., Cod E. M., De Sousa R. A. L., Cassilhas R. C. (2022). An overview of the molecular and physiological antidepressant mechanisms of physical exercise in animal models of depression. Mol. Biology Reports 49 (6), 4965–4975. doi:10.1007/s11033-022-07156-z
del Corral T., Fabero-Garrido R., Plaza-Manzano G., Fernández-de-las-Peñas C., Navarro-Santana M., López-de-Uralde-Villanueva I. (2023). Home-based respiratory muscle training on quality of life and exercise tolerance in long-term post-COVID-19: randomized controlled trial. Ann. Phys. Rehabilitation Med. 66 (1), 101709. doi:10.1016/j.rehab.2022.101709
Del Corral T., Fabero-Garrido R., Plaza-Manzano G., Izquierdo-García J., López-Sáez M., García-García R., et al. (2025). Effect of respiratory rehabilitation on quality of life in individuals with post-COVID-19 symptoms: a randomised controlled trial. Ann. Phys. and Rehabilitation Med. 68 (1), 101920. doi:10.1016/j.rehab.2024.101920
Driggin E., Madhavan M. V., Bikdeli B., Chuich T., Laracy J., Biondi-Zoccai G., et al. (2020). Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J. Am. Coll. Cardiol. 75 (18), 2352–2371. doi:10.1016/j.jacc.2020.03.031
Du S., Cui Z., Peng S., Wu J., Xu J., Mo W., et al. (2025). Clinical efficacy of exercise therapy for lumbar disc herniation: a systematic review and meta-analysis of randomized controlled trials. Front. Med. (Lausanne) 12, 1531637. doi:10.3389/fmed.2025.1531637
Dwiputra B., Ambari A. M., Triangto K., Supriami K., Kesuma T. W., Zuhdi N., et al. (2024). The home-based breathing and chest mobility exercise improves cardiorespiratory functional capacity in long COVID with cardiovascular comorbidities: a randomized study. BMC Cardiovasc. Disord. 24 (1), 574. doi:10.1186/s12872-024-04196-0
Elyazed T. I. A., Alsharawy L. A., Salem S. E., Helmy N. A., El-Hakim AAEMA (2024). Effect of home-based pulmonary rehabilitation on exercise capacity in post COVID-19 patients: a randomized controlled trail. J. NeuroEngineering Rehabilitation 21 (1), 40. doi:10.1186/s12984-024-01340-x
Espinoza-Bravo C., Arnal-Gómez A., Martínez-Arnau F. M., Núñez-Cortés R., Hernández-Guillén D., Flor-Rufino C. (2023). Effectiveness of functional or aerobic exercise combined with breathing techniques in telerehabilitation for patients with long COVID: a randomized controlled trial. Phys. Ther. 103 (11), 04. doi:10.1093/ptj/pzad118
Fares H. M., Elsary A. Y., Elrefaey B. H., Ghanem A. A. M., Fares E. M., Farhat E. S. (2023). Effect of pulmonary rehabilitation program on post hospitalization severe COVID-19 patients (experimental study). Article. J. Popul. Ther. Clin. Pharmacol. 30 (7), e133–e140. doi:10.47750/jptcp.2023.30.07.016
Gaudreau-Majeau F., Gagnon C., Djedaa S. C., Bérubé B., Malo J., Iglesies-Grau J., et al. (2025). Cardiopulmonary rehabilitation's influence on cognitive functions, psychological state, and sleep quality in long COVID-19 patients: a randomized controlled trial. Neuropsychol. Rehabil. 35 (2), 345–361. doi:10.1080/09602011.2024.2338613
Gomes Dos Santos E. G., Vieira da Costa K., Cordeiro de Souza I. T., Victor Dos Santos Felix J., Furtado Brandão C. B., Michelle de Souza Fernandes V., et al. (2024). Effects of a cardiopulmonary rehabilitation protocol on functional capacity, dyspnea, fatigue, and body composition in individuals with post-COVID-19 syndrome: a randomized controlled trial. Physiother. Res. Int. 29 (2), e2086. doi:10.1002/pri.2086
Habas K., Nganwuchu C., Shahzad F., Gopalan R., Haque M., Rahman S., et al. (2020). Resolution of coronavirus disease 2019 (COVID-19). Expert Review Anti-infective Therapy 18 (12), 1201–1211. doi:10.1080/14787210.2020.1797487
Halpin S. J., McIvor C., Whyatt G., Adams A., Harvey O., McLean L., et al. (2021). Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J. Medical Virology 93 (2), 1013–1022. doi:10.1002/jmv.26368
Harvey S. B., Overland S., Hatch S. L., Wessely S., Mykletun A., Hotopf M. (2018). Exercise and the prevention of depression: results of the HUNT cohort Study. Am. Journal Psychiatry 175 (1), 28–36. doi:10.1176/appi.ajp.2017.16111223
Herring M. P., Meyer J. D. (2024). Resistance exercise for anxiety and depression: efficacy and plausible mechanisms. Trends Molecular Medicine 30 (3), 204–206. doi:10.1016/j.molmed.2023.11.016
Jimeno-Almazan A., Franco-Lopez F., Buendia-Romero A., Martínez-Cava A., Sánchez-Agar J. A., Sánchez-Alcaraz Martínez B. J., et al. (2022). Rehabilitation for post-COVID-19 condition through a supervised exercise intervention: a randomized controlled trial. Scand. J. Med. and Sci. SPORTS 32 (12), 1791–1801. doi:10.1111/sms.14240
Jimeno-Almazan A., Buendia-Romero A., Martinez-Cava A., Franco-López F., Sánchez-Alcaraz B. J., Courel-Ibáñez J., et al. (2023). Effects of a concurrent training, respiratory muscle exercise, and self-management recommendations on recovery from post-COVID-19 conditions: the RECOVE trial. J. Appl. Physiology 134 (1), 95–104. doi:10.1152/japplphysiol.00489.2022
Jorge M. S. G., Nepomuceno P., Schneider R. H., Wibelinger L. M. (2025). Eight weeks of Pilates Method improves physical fitness and sleep quality of individuals with post-COVID-19 syndrome: a randomized clinical trial blinded. J. Bodyw. and Mov. Ther. 41, 238–245. doi:10.1016/j.jbmt.2024.11.037
Kerling A., Beyer S., Dirks M., Scharbau M., Hennemann A. K., Dopfer-Jablonka A., et al. (2024). Effects of a randomized-controlled and online-supported physical activity intervention on exercise capacity, fatigue and health related quality of life in patients with post-COVID-19 syndrome. BMC Sports Sci. Med. Rehabilitation 16 (1), 33. doi:10.1186/s13102-024-00817-5
Kevadiya B. D., Machhi J., Herskovitz J., Oleynikov M. D., Blomberg W. R., Bajwa N., et al. (2021). Diagnostics for SARS-CoV-2 infections. Nat. Materials 20 (5), 593–605. doi:10.1038/s41563-020-00906-z
Kishimoto T., Kang S. (2022). IL-6 revisited: from rheumatoid arthritis to CAR T cell therapy and COVID-19. Annu. Review Immunology 40, 323–348. doi:10.1146/annurev-immunol-101220-023458
Kogel A., Machatschek M., Scharschmidt R., Wollny C., Lordick F., Ghanem M., et al. (2023). Physical exercise as a treatment for persisting symptoms post covid infection. Eur. Heart J. 44. doi:10.1093/eurheartj/ehad655.2398
Lai C.-Y., Lin C.-H., Chao T.-C., Lin C.-H., Chang C.-C., Huang C.-Y., et al. (2024). Effectiveness of a 12-week telerehabilitation training in people with long COVID: a randomized controlled trial. Ann. Phys. Rehabilitation Med. 67 (5), 101853. doi:10.1016/j.rehab.2024.101853
Majumder J., Minko T. (2021). Recent developments on therapeutic and diagnostic approaches for COVID-19. AAPS Journal 23 (1), 14. doi:10.1208/s12248-020-00532-2
Mandal S., Barnett J., Brill S. E., Brown J. S., Denneny E. K., Hare S. S., et al. (2021). Long-COVID': a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax 76 (4), 396–398. doi:10.1136/thoraxjnl-2020-215818
McGregor G., Sandhu H., Bruce J., Sheehan B., McWilliams D., Yeung J., et al. (2024). Clinical effectiveness of an online supervised group physical and mental health rehabilitation programme for adults with post-covid-19 condition (REGAIN study): Multicentre randomised controlled trial. Randomized Control. Trial Multicent. Study. BMJ. 384, e076506. doi:10.1136/bmj-2023-076506
McNarry M. A., Berg R. M. G., Shelley J., Hudson J., Saynor Z. L., Duckers J., et al. (2022). Inspiratory muscle training enhances recovery post-COVID-19: a randomised controlled trial. Eur. Respir. J. 60 (4), 2103101. doi:10.1183/13993003.03101-2021
Mehandru S., Merad M. (2022). Pathological sequelae of long-haul COVID. Nat. Immunology 23 (2), 194–202. doi:10.1038/s41590-021-01104-y
Nieman D. C., Henson D. A., Austin M. D., Sha W. (2011). Upper respiratory tract infection is reduced in physically fit and active adults. Br. Journal Sports Medicine 45 (12), 987–992. doi:10.1136/bjsm.2010.077875
Okan F., Okan S., Duran Yücesoy F. (2022). Evaluating the efficiency of breathing exercises via telemedicine in Post-Covid-19 patients: randomized controlled study. Clin. Nursing Research 31 (5), 771–781. doi:10.1177/10547738221097241
Özlü A., Yaman F., Leblebicier M. A., Özkaya D. B. (2022). Efficacy of a home exercise program on balance, kinesiophobia, pain and quality of life in post-COVID-19 patients: efficacy of a home exercise program in post COVID. Article. Ann. Clin. Anal. Med. 13 (5), 563–567. doi:10.4328/ACAM.21033
Paneroni M., Scalvini S., Perger E., Zampogna E., Govetto S., Oliva F. M., et al. (2024). Home-based exercise program for people with residual disability following hospitalization for COVID-19: randomized control trial. Ann. Phys. Rehabilitation Med. 67 (2), 101815. doi:10.1016/j.rehab.2023.101815
Perez-Bermejo J. A., Kang S., Rockwood S. J., Simoneau C. R., Joy D. A., Ramadoss G. N., et al. (2020). SARS-CoV-2 infection of human iPSC-derived cardiac cells predicts novel cytopathic features in hearts of COVID-19 patients. bioRxiv The Preprint Server Biology. doi:10.1101/2020.08.25.265561
Pierce J. D., Shen Q., Cintron S. A., Hiebert J. B. (2022). Post-COVID-19 syndrome. Nurs. Research 71 (2), 164–174. doi:10.1097/NNR.0000000000000565
Pizzorno J. (2023). What have we learned about preventing and treating COVID-19? Part 1: physical strategies, natural health products, and lifestyle. Integr. Medicine 22 (1), 8–13.
Puntmann V. O., Carerj M. L., Wieters I., Fahim M., Arendt C., Hoffmann J., et al. (2020). Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiology 5 (11), 1265–1273. doi:10.1001/jamacardio.2020.3557
Rayapuraju A., Mohamed E., Upadhyay P., Orui H., Pratt M., Friedopfer S., et al. (2025) “Yogic breathing and guided meditation practices address the mental fear associated with breathing,” in Fostering a sense of self-stability among long COVID patients: a mixed methods Study.
Rodriguez-Blanco C., Bernal-Utrera C., Anarte-Lazo E., Gonzalez-Gerez J. J., Saavedra-Hernandez M. (2023). A 14-Day therapeutic exercise telerehabilitation protocol of physiotherapy is effective in non-hospitalized Post-COVID-19 conditions: a randomized controlled trial. J. Clin. Med. 12 (3), 776. doi:10.3390/jcm12030776
Romanet C., Wormser J., Fels A., Lucas P., Prudat C., Sacco E. (2022). Effectiveness of endurance training rehabilitation after hospitalisation in intensive care for COVID-19 related acute respiratory distress syndrome on dyspnoea (RECOVER): a randomised controlled, open-label multicentre trial.
Romero-Sanchez C. M., Diaz-Maroto I., Fernandez-Diaz E., Sánchez-Larsen Á., Layos-Romero A., García-García J., et al. (2020). Neurologic manifestations in hospitalized patients with COVID-19: the ALBACOVID registry. Neurology 95 (8), e1060–e1070. doi:10.1212/WNL.0000000000009937
Sánchez Milá Z., Rodríguez Sanz D., Martín Nieto A., Jiménez Lobo A., Ramos Hernández M., Campón Chekroun A., et al. (2024). Effects of a respiratory and neurological rehabilitation treatment plan in post Covid-19 affected university students. Chronic Respir. Dis. 21. doi:10.1177/14799731241255967
Sánchez-Romero E. A., García-Barredo-Restegui T., Martínez-Rolando L., Villafañe J. H., Galán-Fraguas A., Jurado-Molina R., et al. (2025). Addressing post-COVID-19 musculoskeletal symptoms through pulmonary rehabilitation with an evidence-based eHealth education tool: preliminary results from a pilot randomized controlled clinical trial. Medicine 104 (10), e41583. doi:10.1097/MD.0000000000041583
Scharf R. E., Anaya J. M. (2023). Post-COVID syndrome in Adults-An overview. Viruses 15 (3), 675. doi:10.3390/v15030675
Shafqat A., Masters M. C., Tripathi U., Tchkonia T., Kirkland J. L., Hashmi S. K. (2024). Long COVID as a disease of accelerated biological aging: an opportunity to translate geroscience interventions. Ageing Research Reviews 99, 102400. doi:10.1016/j.arr.2024.102400
Sick J., Steinbacher V., Kotnik D., König F., Recking T., Bengsch D., et al. (2025). Exercise rehabilitation in post COVID-19 patients: a randomized controlled trial of different training modalities. Eur. J. Phys. Rehabilitation Med. 61 (1), 130–140. doi:10.23736/S1973-9087.24.08487-9
Smart T. F. F., Doleman B., Hatt J., Paul M., Toft S., Lund J. N., et al. (2022). The role of resistance exercise training for improving cardiorespiratory fitness in healthy elderly: a systematic review and meta-analysis. Age Ageing 51 (6), afac143. doi:10.1093/ageing/afac143
Tsuji S., Minami S., Hashimoto R., Konishi Y., Suzuki T., Kondo T., et al. (2022). SARS-CoV-2 infection triggers paracrine senescence and leads to a sustained senescence-associated inflammatory response. Nat. Aging 2 (2), 115–124. doi:10.1038/s43587-022-00170-7
Tucker W. J., Fegers-Wustrow I., Halle M., Haykowsky M. J., Chung E. H., Kovacic J. C. (2022). Exercise for primary and secondary prevention of cardiovascular disease: JACC focus seminar 1/4. J. Am. Coll. Cardiol. 80 (11), 1091–1106. doi:10.1016/j.jacc.2022.07.004
van Doremalen N., Bushmaker T., Morris D. H., Holbrook M. G., Gamble A., Williamson B. N., et al. (2020). Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. Journal Medicine 382 (16), 1564–1567. doi:10.1056/NEJMc2004973
Vardakas P., Skaperda Z., Tekos F., Kouretas D. (2022). ROS and COVID. Antioxidants 11 (2), 339. doi:10.3390/antiox11020339
Velayudhan L., Aarsland D., Ballard C. (2020). Mental health of people living with dementia in care homes during COVID-19 pandemic. Int. Psychogeriatrics 32 (10), 1253–1254. doi:10.1017/S1041610220001088
Ye M., Song T., Xia H., Hou Y., Chen A. (2024). Effects of aerobic exercise on executive function of healthy middle-aged and elderly: a systematic review and meta-analysis. Int. Journal Nursing Studies 160, 104912. doi:10.1016/j.ijnurstu.2024.104912
Yong S. J. (2021). Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect. Diseases 53 (10), 737–754. doi:10.1080/23744235.2021.1924397
Keywords: post-COVID syndrome, exercise therapy, clinical trials, netword meta-analysis, PCS
Citation: Du S, Cui Z, Xu X, Liu T and Ye J (2025) Clinical efficacy of exercise in the treatment of post-COVID-19 syndrome: a systematic review and network meta-analysis. Front. Physiol. 16:1656713. doi: 10.3389/fphys.2025.1656713
Received: 02 July 2025; Accepted: 20 November 2025;
Published: 18 December 2025.
Edited by:
Hassane Zouhal, University of Rennes 2 – Upper Brittany, FranceReviewed by:
Robson Chacon Castoldi, North University of Paraná, BrazilShiv Kumar Mudgal, All India Institute of Medical Sciences, Deoghar (AIIMS Deoghar), India
Copyright © 2025 Du, Cui, Xu, Liu and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Ye, eWVqaWUxOTc3QDEyNi5jb20=; Te Liu, bGl1dGUxOTc5QHNodXRjbS5lZHUuY24=; Xiangqian Xu, bGgyOTQ5QHNodXRjbS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Shaojie Du
Shaojie Du Zeyu Cui1,3†
Zeyu Cui1,3† Te Liu
Te Liu Jie Ye
Jie Ye