- 1Effective Care Research Unit, Department of Obstetrics and Gynaecology, Nnamdi Azikiwe University, Awka, Nigeria
- 2Department of Obstetrics and Gynaecology, Nnamdi Azikiwe University Teaching Hospital, Nnewi, Anambra State, Nigeria
- 3Department of Paediatrics, Nnamdi Azikiwe University, Awka, Nigeria
- 4Department of Paediatrics, Nnamdi Azikiwe University Teaching Hospital, Nnewi, Anambra State, Nigeria
- 5Department of Obstetrics and Gynecology, Kelina Hospital, Lagos, Nigeria
- 6Department of Pharmacology, Calcutta Institute of Pharmaceutical Technology & AHS, Howarah,-West Bengal, India
Editorial on the Research Topic
HIV/HBV and/or HCV infections and hepatotoxicity in pregnant and non-pregnant women
Introduction
Viral infections such as human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV) remain major public health concerns globally, especially among women of reproductive age (1). Pregnancy introduces unique immunological and physiological changes that may influence the course of these infections, their management, and associated complications, including hepatotoxicity (1–3). This editorial unifies key findings from multiple studies to highlight how these infections intersect with maternal and non-maternal health outcomes, spanning pregnancy complications, treatment challenges, and innovative testing strategies in low-resource settings. The all-encompassing goal is to provide an interconnected understanding of how these infections impact women's health and identify gaps for future research and policy interventions.
The need for integrated focus on HIV, HBV, and HCV in women
While previous studies has individually examined HIV, HBV, or HCV (4–6), few studies address their overlapping burden or combined implications for hepatotoxicity, especially across pregnant and non-pregnant populations (7–10). The four studies in this research topic illustrated in Table 1, collectively demonstrate that viral co-infections and associated liver complications require integrated screening, prevention, and treatment approaches. In all, they reinforce the necessity of linking maternal health interventions with broader women's health strategies.
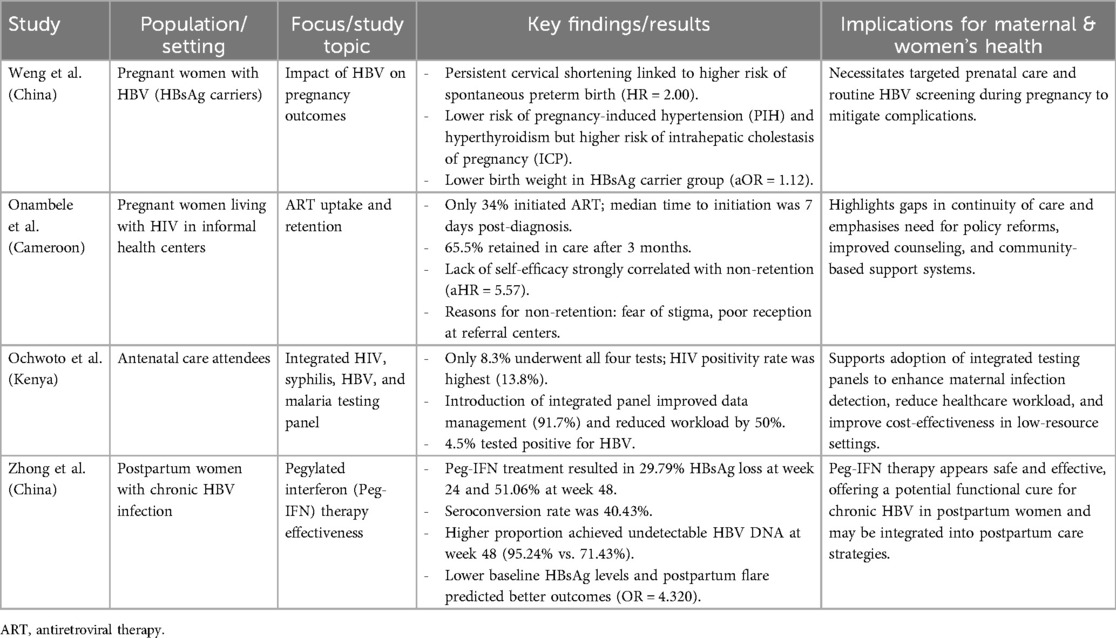
Table 1. Summary of key findings from research studies on HIV, HBV, and HCV infections and hepatotoxicity in women.
Hepatitis B virus and pregnancy complications
The study by Weng et al. investigates how hepatitis B surface antigen (HBsAg) carriage affects pregnancy outcomes. This retrospective cohort study in Shenzhen, China, shows that HBsAg-positive women have lower risks of some complications, such as pregnancy-induced hypertension (PIH) and hyperthyroidism, but face higher risks of intrahepatic cholestasis of pregnancy (ICP) and delivering low birth weight infants. These findings emphasise the complex interplay between HBV and maternal health, highlighting the importance of risk-stratified prenatal care and ongoing screening.
HIV management in informal health centers
Onambele et al.'s study examines the low uptake and retention of antiretroviral therapy (ART) among pregnant women living with HIV in informal health centers (IHCs) in Cameroon. Despite growing access to HIV screening, only 34% of women initiated ART, and retention after three months was 65.5%. This reinforces systemic gaps in continuity of care, pointing to the urgent need for policy interventions, enhanced counseling, and strengthened linkages between informal and formal healthcare settings.
Integrating HIV, syphilis, HBV, and malaria testing in Kenya
Ochwoto et al. evaluated a four-test antenatal care (ANC) panel in Kenya, covering HIV, syphilis, HBV, and malaria. Their findings reveal how integrated testing significantly improved detection rates and streamlined service delivery, reducing healthcare worker burden while enhancing cost-effectiveness. This model demonstrates potential scalability for low- and middle-income countries seeking comprehensive maternal infection screening.
Pegylated interferon treatment for hepatitis B in postpartum women
Lastly, Zhong et al.'s exploratory study highlights pegylated interferon alpha-2b (Peg-IFN) as a promising treatment for postpartum women with chronic HBV infection. The treatment achieved a 51.06% HBsAg loss rate and 40.43% HBsAg seroconversion rate after 48 weeks, with no serious adverse events. These results suggest that postpartum women may particularly benefit from Peg-IFN therapy due to immune reconstitution after pregnancy, offering a viable pathway toward functional cure.
Conclusion
Together, these studies provide a comprehensive view of how HIV, HBV, and HCV infections intersect with hepatotoxicity and maternal outcomes in diverse settings. The unifying theme is the urgent need for integrated care approaches, of combining screening, prevention, and treatment, to address the complex burden of these infections across both pregnant and non-pregnant women. Strengthening health systems, bridging gaps between informal and formal care, and implementing cost-effective, mountable interventions are critical to improving outcomes and reducing disparities in low-resource settings. Future research must also explore long-term effects of maternal infections on both mothers and infants to inform sustained global health strategies.
Table 1 shows the summary of key findings from research studies.
The table summarises the main results related to HBV on pregnancy outcomes, ART uptake and retention in Cameroon, integrated testing in Kenya, and Peg-IFN treatment for HBV in postpartum women.
Author contributions
GE: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. CO: Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. EI: Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SF: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Eleje GU, Loto OM, Usman HA, Onubogu CU, Fiebai PO, Akaba GO, et al. A systematic review and meta-analysis of the prevalence of triplex infections (combined human immunodeficiency virus, hepatitis B virus, and hepatitis C virus) among pregnant women in Nigeria. Obstet Gynecol Int. (2023) 2023:3551297. doi: 10.1155/2023/3551297
2. Ugwu EO, Eleje GU, Ugwu AO, Nwagha UI, Ikechebelu JI, Umeh UA, et al. Antivirals for prevention of hepatitis B virus mother-to-child transmission in human immunodeficiency virus positive pregnant women co-infected with hepatitis B virus. Cochrane Database Syst Rev. (2023) 6(6):CD013653. doi: 10.1002/14651858.CD013653.pub2
3. Eleje GU, Onubogu CU, Fiebai PO, Mbachu II, Akaba GO, Loto OM, et al. Mother-to-child transmission of human immunodeficiency virus, hepatitis B virus and hepatitis C virus among pregnant women with single, dual or triplex infections of human immunodeficiency virus, hepatitis B virus and hepatitis C virus in Nigeria: a systematic review and meta-analysis. SAGE Open Med. (2022) 10:20503121221095411. doi: 10.1177/20503121221095411
4. Eleje GU, Akaba GO, Mbachu II, Rabiu A, Loto OM, Usman HA, et al. Pregnant women’s hepatitis B vaccination coverage in Nigeria: a national pilot cross-sectional study. Ther Adv Vaccines Immunother. (2021) 9:25151355211032595. doi: 10.1177/25151355211032595
5. Eleje GU, Rabiu A, Mbachu II, Akaba GO, Loto OM, Usman HA, et al. Awareness and prevalence of hepatitis C virus infection among pregnant women in Nigeria: a national pilot cross-sectional study. Womens Health (Lond). (2021) 17:17455065211031718. doi: 10.1177/17455065211031718
6. Chukwuanukwu RC, Eleje GU, Menkiti FE, Ikpeze GC, Mbachu CN, Obiegbu NP, et al. Intermittent preventive treatment, malaria, HIV, hepatitis and pregnancy outcomes in Nigerian women: a cross-sectional study in two healthcare facilities. BMC Pregnancy Childbirth. (2025) 25(1):809. doi: 10.1186/s12884-025-07943-z
7. Eleje GU, Mbachu II, Ogwaluonye UC, Kalu SO, Onubogu CU, Nweje SI, et al. Prevalence, seroconversion and mother-to-child transmission of dual and triplex infections of HIV, hepatitis B and C viruses among pregnant women in Nigeria: study protocol. Reprod Health. (2020) 17(1):144. doi: 10.1186/s12978-020-00995-8
8. Eke AC, Eleje GU, Eke UA, Xia Y, Liu J. Hepatitis B immunoglobulin during pregnancy for prevention of mother-to-child transmission of hepatitis B virus. Cochrane Database Syst Rev. (2017) 2(2):CD008545. doi: 10.1002/14651858.CD008545.pub2
9. Eleje GU, Usman HA, Onubogu CU, Fiebai PO, Akaba GO, Rabiu A, et al. Seroprevalence, seroconversion, and mother-to-child transmission of dual and triplex infections of HIV, HBV, and HCV among Nigerian obstetric population: a national multicentre prospective cohort study. Antivir Ther. (2025) 30(2):13596535251333259. doi: 10.1177/13596535251333259
10. Tesfaye S, Abebaw T, Bizualem E, Mehabie D, Alelign A. Seroprevalence of hepatitis B and C and HIV infections and associated risk factors among pregnant women attending antenatal care unit at simada hospital, south gondar zone, northwest Ethiopia. Biomed Res Int. (2025) 2025:6895237. doi: 10.1155/bmri/6895237
Keywords: co-infections, vaccination coverage, antiviral treatments, mother-to-child transmission (MTCT), HBsAg-positive
Citation: Eleje GU, Onubogu CU, Igbodike EP and Firdous SM (2025) Editorial: HIV/HBV and/or HCV infections and hepatotoxicity in pregnant and non-pregnant women. Front. Reprod. Health 7:1538380. doi: 10.3389/frph.2025.1538380
Received: 2 December 2024; Accepted: 5 August 2025;
Published: 22 August 2025.
Edited and Reviewed by: Gasim Ibrahim Gasim, Gauteng Department of Health, South Africa
Copyright: © 2025 Eleje, Onubogu, Igbodike and Firdous. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: George Uchenna Eleje, Z2VvcmdlbDIxQHlhaG9vLmNvbQ==
 George Uchenna Eleje
George Uchenna Eleje Chinyere Ukamaka Onubogu
Chinyere Ukamaka Onubogu Emeka Philip Igbodike
Emeka Philip Igbodike Sayeed Mohammed Firdous
Sayeed Mohammed Firdous