- 1School of Medicine, University of Pittsburgh, Pittsburgh, PA, United States
- 2Clinical and Translational Science Institute University of Pittsburgh, Pittsburgh, PA, United States
- 3Department of Obstetrics, Gynecology and Reproductive Sciences, UPMC Magee-Womens Hospital, Pittsburgh, PA, United States
- 4Magee-Womens Research Institute, Pittsburgh, PA, United States
Introduction: Disparities in pregnancy care exist in the United States, with limited data on access to specialized postpartum care for patients with complicated perineal lacerations. Our objective was to assess for disparities in access to a postpartum pelvic floor healing clinic following vaginal delivery. We hypothesized an underrepresentation of patients from more resource-deprived neighborhoods and those with longer travel times to the specialized clinic.
Methods: This is a retrospective cohort study comparing sociodemographic variables from a historical cohort of patients with third- and fourth-degree lacerations following vaginal delivery to a cohort of patients evaluated in a postpartum pelvic floor healing clinic. The primary outcome involved the comparison of the neighborhood area deprivation index between groups. The secondary outcomes included median household income, driving time, and distance to the hospital.
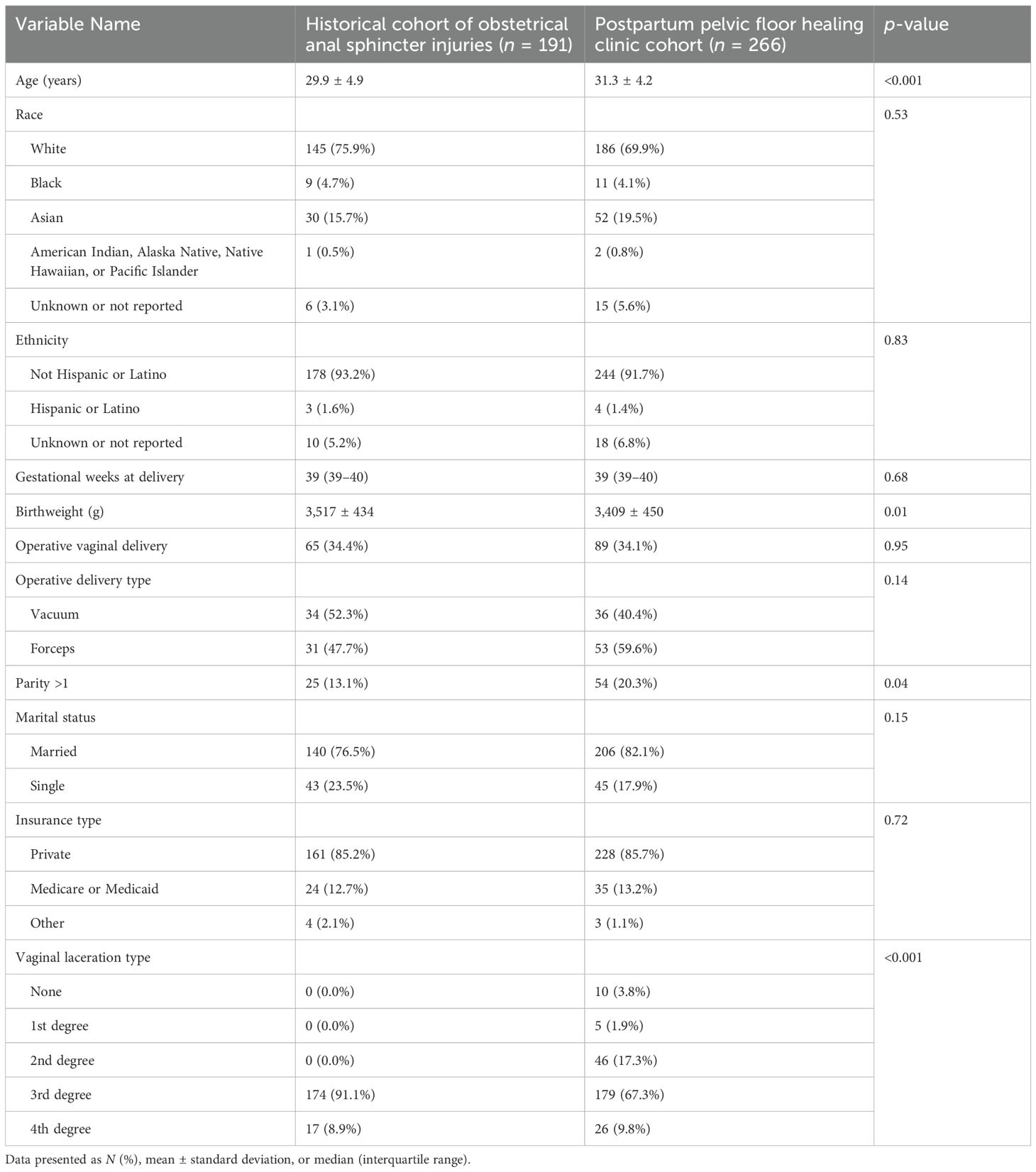
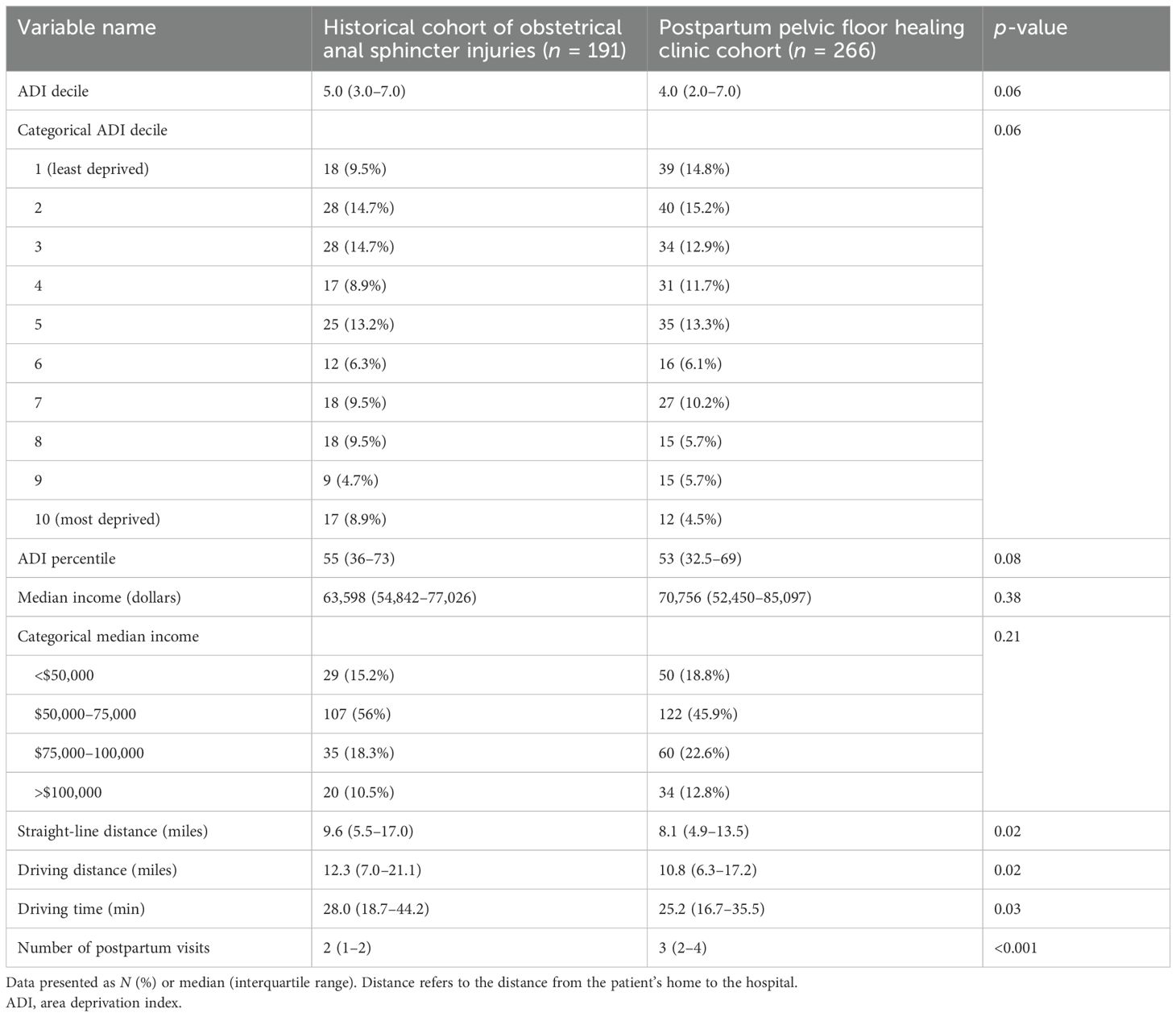
Results: Patients seen in the postpartum pelvic floor healing clinic were older (31.3 vs. 29.9 years, p < 0.01) and more likely to be multiparous (20.3% vs. 13.1%, p = 0.04). Race, ethnicity, and operative vaginal delivery were similar between groups. Patients from the postpartum pelvic floor healing clinic had more postpartum visits [3 (IQR 2–4) vs. 2 (IQR 1–2) visits, p < 0.01]. There was no significant difference in median neighborhood area deprivation indices [4 (IQR 2–7) vs. 5 (IQR 3–7), p = 0.06]. Fewer patients from the most resource-deprived neighborhoods were seen in the postpartum pelvic floor healing clinic, though this was not statistically significant (4.5% vs. 8.9%, p = 0.06). There were no significant differences in median household income or driving distance to the hospital between groups.
Conclusions: Access to a specialized postpartum pelvic floor healing clinic at our institution appears equitable across several sociodemographic factors.
1 Introduction
Vaginal delivery is the most common cause of perineal trauma, and approximately 70%–80% of patients undergoing vaginal childbirth will experience a laceration or tear to the vagina or perineum. Furthermore, 2%–6% of patients experience more complex third- or fourth-degree tears, also known as obstetric anal sphincter injuries (OASIs) (1, 2). OASIs are associated with an increased risk of complications including wound breakdown, infection, anal sphincter incontinence, pain, and pelvic floor dysfunction (3). Additionally, OASIs pose significant psychological stress to patients (4). Thus, there has been heightened emphasis on the importance of early postpartum follow-up and close monitoring of individuals who have experienced OASIs (5–7). As such, a specialized postpartum pelvic floor healing clinic (PPFHC) was established at our institution to provide the necessary and complex care required for patients with OASIs.
In the United States, there are ongoing disparities in maternal healthcare ranging from inadequate access to maternal mortality (8–10). There has been an increase in the number of publications assessing how neighborhood-level disparities relate to access to healthcare and healthcare disparities (11–13), and there are now multiple tools to help quantify and understand this relationship (14–19). With our current knowledge of existing and pervasive inequities in the care of pregnant and postpartum patients, it is possible that disparities might also exist in postpartum care for patients who experience OASIs. There are very limited data assessing access to specialized, focused postpartum care for patients who have experienced an OASI or who have other postpartum pelvic floor concerns (20).
The purpose of this study was to evaluate disparities in and potential barriers to accessing care in a PPFHC utilizing a historical cohort for comparison of sociodemographic factors. We hypothesized that patients from more resource-deprived neighborhoods with higher area deprivation indices (ADI) would be less represented within a specialty PPFHC patient population compared to a historical cohort of OASIs.
2 Materials and methods
We performed a retrospective comparative cohort study of two pre-existing datasets, which were both chosen as convenience samples from a large academic hospital. The first dataset was a pre-PPFHC historical cohort of all OASIs from December 2019 to January 2021 before the institutional creation of the specialized PPFHC clinic. These patients experienced an OASI at that time of vaginal delivery and received routine postpartum care from a physician, nurse midwife, or advanced practice provider within their primary obstetric provider group. Patients in this cohort had been identified by documentation of either a third- or fourth-degree perineal laceration in the delivery records. Demographic, delivery, and postpartum data were subsequently abstracted from the electronic medical record.
The second dataset consisted of all patients who were evaluated in a specialized PPFHC for evaluation after a vaginal delivery from July 2021 to July 2022. The PPFHC is a specialized clinic staffed by board-certified urogynecologists. Patients are referred to the PPFHC at the discretion of their primary obstetric provider for postpartum care of OASIs, other complex obstetrical lacerations, or postpartum pelvic floor disorders including but not limited to wound healing issues, urinary and anal incontinence, and pain. Patients in this cohort were identified if they had been evaluated in the PPFHC. Demographic, delivery, and postpartum data were subsequently abstracted from the electronic medical record. For both cohorts, patients were excluded if their electronic health records were missing address data or if they resided in a state outside our normal referral base which includes Pennsylvania, Ohio, and West Virginia.
Our primary outcome involved the area deprivation index (ADI) (Neighborhood Atlas, University of Wisconsin), in which higher decile neighborhoods are considered more resource-deprived (21, 22). Patient addresses and zip codes were entered into the ADI database for Pennsylvania, West Virginia, and Ohio, and both state decile and national percentile rankings were recorded. If we assume equitable access to care, then sociodemographic factors, including the ADI of patients in the PPFHC, should be similar to those in the historical cohort. However, we hypothesized that there would be disparities in access to care in the PPFHC. Moreover, we hypothesized that the neighborhood ADI would be lower (less resource-deprived) among the PPFHC and patients from more resource-deprived neighborhoods would be underrepresented in the PPFHC compared to the historical cohort.
The secondary outcomes included the median household income (2020 American Community Survey, U.S. Census Bureau), for which patient zip codes were cross-referenced to their corresponding zip code tabulation areas. This identifier was then queried in the American Community Survey to collect median household income for that location. We also assessed driving distance (miles) and driving time (min) to the hospital (ArcMap GIS, ESRI, Redlands, California). The straight-line distance was calculated by ArcMap GIS, where the destination location was the coordinates for the PPFHC and the origin location was each patient’s address. Driving distance and time were also calculated with this software using the same coordinates, with driving time based on the driving route used for the driving distance. We also assessed the patient’s age, race, ethnicity, marital status, and insurance type. Any identified disparity is also a potential barrier to care, and thus by assessing disparities in the above sociodemographic primary and secondary outcomes, we are also assessing potential barriers to care.
Continuous variables were analyzed with independent t-tests or Mann–Whitney U tests, and categorical variables were analyzed by chi-square or Fisher’s exact tests using the SPSS statistical software (Version 28; IBM, Armonk, NY). To control for baseline differences between groups, we performed multivariable linear regression for continuous variables and logistic regression analyses for binary variables. Secondary to data skewness, the driving distance variable was log-transformed for the linear regression model. As this was a convenience sample from two previously collected datasets, no a-priori sample size calculation was performed. The University of Pittsburgh Institutional Review Board approved this research with a waiver of informed consent.
3 Results
There were 191 patients in the pre-PPFHC cohort and 263 patients in the PPFHC cohort (Table 1). Patients in the PPFHC cohort were older (31.3 vs. 29.9 years, p < 0.01) and more likely to be multiparous (20.3% vs. 13.1%, p = 0.04) than the historical cohort. There were no differences in race, ethnicity, insurance type, marital status, or gestational age at delivery between cohorts (Table 1). The historical cohort had a greater proportion of OASI owing to the data collected within the existing database and the broader referral patterns for the PPFHC; however, the rates of operative vaginal deliveries were similar between groups. Patients in the PPFHC cohort had significantly more postpartum visits than pre-PPFHC patients [median 3 (IQR 2–4) vs. 2 (IQR 1–2) visits, p = 0.01] (Table 2).
In the analysis of patient ADIs, no statistically significant difference was found between cohorts (Table 2). There were non-significant trends toward lower (less deprived) ADI values in the PPFHC; similarly, fewer patients from more deprived neighborhoods were seen in the PPFHC compared to the historical cohort (Table 2). Half as many patients from the most deprived neighborhoods (highest ADI decile) were seen in the PPFHC cohort compared to the pre-PPFHC cohort (4.5% vs. 8.9%, Table 2). On multivariable linear regression for ADI controlling for age, marital status, and obstetrical laceration type, our findings were unchanged: ADI was not significantly different between the PPFHC and historical pre-PPFHC cohorts (B = −0.19, 95% CI −0.70 to 0.31, p = 0.46). Lastly, we dichotomized the ADI deciles into least deprived (deciles 1–6) and most deprived (deciles 7–10) and re-ran our statistical analyses with a multivariable logistic regression, which did not change our results with no significant difference in dichotomized ADI between cohorts (OR 0.82, 95% CI 0.51 to 1.32, p = 0.42).
Patients in the PPFHC cohort lived closer to the hospital by a straight-line distance of 1.52 miles [pre-PPFHC: 8.08 (IQR 4.90–13.45) vs. 9.60 (IQR 5.48–16.96) miles, p = 0.02]. Driving distance was also significantly shorter in the PPFHC cohort [10.8 (IQR 6.3–17.2) vs. 12.3 (IQR 6.9–21.1) miles, p = 0.02]. Similarly, the associated driving time was significantly shorter for the PPFHC cohort [25.2 (IQR 16.7–35.5) vs. 27.96 (IQR 18.7–44.2) min, p = 0.03]. After performing a multivariable linear regression controlling for patient age, driving distance was no longer significantly different between groups (B = 0.13, 95% CI −0.03 to 0.29, p = 0.10).
4 Discussion
There were no significant differences in neighborhood ADI, median income, driving distance, race, ethnicity, or insurance type among patients seen in a specialized PPFHC compared to a historical cohort of OASIs. Our data are reassuring and suggest that patients who are at increased risk for postpartum pelvic floor disorders are able to access care in a PPFHC, regardless of these sociodemographic and socioeconomic factors. While not statistically significant, trends in our data suggest that access to care in the PPFHC may be more difficult for patients from more resource-deprived neighborhoods, and we should continue to monitor access for these populations.
The recommended postoperative care of OASIs includes early and close follow-up (23). Owing to both the short-term and long-term risks associated with OASIs, many institutions have moved to a model that offers a dedicated clinic setting for the follow-up of complex obstetrical lacerations (7). These dedicated pelvic floor clinics have been associated with high patient satisfaction (24) and provide an opportunity for early identification and treatment of postpartum pelvic floor disorders. However, there are limited data assessing patient access to this specialized type of care (25). Our results are reassuring in that there were no sociodemographic differences among patients who accessed the PPFHC compared to a historical cohort of women with higher-order obstetrical lacerations. Importantly, there were no differences in racial or ethnic proportions between the two cohorts. This is an important finding given the disproportionate disparities that Black women in the US face throughout obstetrical care, labor, and delivery (26).
As specialized postpartum pelvic floor healing clinics continue to emerge, it is important to pay attention to equitable access to care. While this seems intuitive, we do not want to recreate inequities that have long persisted in maternal healthcare (25–27). While our results are reassuring, non-significant trends in our data suggest that we need to monitor access for patients from more resource-deprived neighborhoods to ensure they continue to receive the postpartum pelvic floor care that is necessary. Other specialized pelvic floor healing clinics in the United States may use these data as a model to track access to care and assess whether care in similar clinics around the country is equitable. Lastly, while not significant on regression modeling, patients who lived farther from the hospital were underrepresented in the PPFHC cohort on unadjusted analyses. Potential solutions to overcome distance as a potential barrier to care may include telehealth visits with the ability to securely submit photos through the medical record if wound concerns exist. Another potential solution is offering services at satellite office locations closer to patient communities. While not studied specifically as part of this research, we have found that patients will often schedule PPFHC appointments in outreach locations closer to their homes (farther from the hospital of delivery) when this option is available.
We demonstrate that patients who attended the PPFHC had significantly more postpartum visits than the historical cohort of OASIs. Prior data demonstrate that, overall, only half of mothers attend a postpartum visit (27). While this may not be clinically impactful for patients with lesser-degree obstetrical lacerations, patients with OASIs should receive closer follow-up (7). A dedicated PPFHC may be a way to encourage adequate follow-up for a patient population at high risk for a variety of postpartum pelvic floor disorders.
The current study represents data from one institution, and it is important that providers who offer specialized postpartum pelvic floor care also assess their own patient populations to identify potential inequities and barriers to access to care. An area to monitor is our identified trend toward patients from more resource-deprived areas being less represented among the PPFHC cohort. Though not significant, this suggests that there is potential to miss a critical population should additional barriers arise and are not adequately identified and addressed. Future research in postpartum care clinics should assess equitable access or potential disparities in different geographic areas and in larger patient populations.
The strengths of our study include data from a large institution that evaluates and treats patients from both urban and rural settings, making our results generalizable to the greater population. We also have a historical cohort of OASIs available, which represents a patient population at increased risk of postpartum pelvic floor concerns and can thus be used for comparison to the PPFHC, which represents a patient population with a similarly increased risk of postpartum pelvic floor disorders (7). By using a historical cohort, we remove the possibility of bias related to patient choice or differing referral patterns between groups, as the historical cohort did not have the option to attend or be referred to a PPFHC. Additionally, we utilized software that provides tangible estimates for socioeconomic status to the best of our abilities given our retrospective data.
Our study has important limitations. The two patient cohorts differ in that the historical cohort consisted solely of OASIs, whereas the PPFHC cohort also had a small proportion of non-OASI patients. However, the majority of patients (77%) in the PPFHC had OASIs; thus, both groups remain comparable and represent patients at an increased risk of postpartum pelvic floor complications and disorders. We also recognize that while our study evaluates area deprivation index, time, distance, and median household income, there are several other sociodemographic variables that can contribute to a patient’s ability to access care including but not limited to employment, education level, and housing. Additionally, we demonstrate a non-significant trend, suggesting that access to a postpartum pelvic floor healing clinic may be more difficult for patients from more resource-deprived neighborhoods. Thus, it is possible that with a larger sample size, a significant difference might emerge, supporting similar studies among larger patient populations. The generalizability of our study is also limited given the use of a historical cohort and the data were derived from a single center. Our inclusion and assessment of driving time was predicated on the assumption that every patient has access to a car. However, we know that this is not the case, and we were not able to assess accessibility to transportation or public transportation routes, which would impact access. Additionally, the ArcGIS software used for calculating distance and time of travel to the clinic assumes a singular route, when in reality, there are several possible routes. Lastly, we have a small number of Black patients in our cohort, and thus, it is difficult to draw conclusions regarding racial inequities from our data. Prior data demonstrate that OASIs occur less frequently in Black patients, and thus, our small number of Black patients is consistent with prior research (28).
Data availability statement
The raw data supporting the conclusions of this article can be made available by the authors after discussion and with a data usage agreement.
Ethics statement
This study was approved by the University of Pittsburgh Institutional Review Board. This study was conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the exempt status granted by the Institutional Review Board.
Author contributions
AS: Writing – original draft, Writing – review & editing. LW: Writing – original draft, Writing – review & editing. RD: Writing – original draft, Writing – review & editing. PM: Writing – original draft, Writing – review & editing. LG: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Statistical analyses for this project were supported by the National Institutes of Health through Grant Number UL1TR001857.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rogers RG, Leeman LM, Borders N, Qualls C, Fullilove AM, Teaf D, et al. Contribution of the second stage of labour to pelvic floor dysfunction: a prospective cohort comparison of nulliparous women. Bjog. (2014) 121:1145–54. doi: 10.1111/bjo.2014.121.issue-9
2. Vale de Castro Monteiro M, Pereira GM, Aguiar RA, Azevedo RL, Correia-Junior MD, Reis ZS. Risk factors for severe obstetric perineal lacerations. Int Urogynecol J. (2016) 27:61–7. doi: 10.1007/s00192-015-2795-5
3. Dudding TC, Vaizey CJ, Kamm MA. Obstetric anal sphincter injury: incidence, risk factors, and management. Ann Surg. (2008) 247:224–37. doi: 10.1097/SLA.0b013e318142cdf4
4. Iles D, Khan R, Naidoo K, Kearney R, Myers J, Reid F. The impact of anal sphincter injury on perceived body image. Eur J Obstet Gynecol Reprod Biol. (2017) 212:140–3. doi: 10.1016/j.ejogrb.2017.03.024
5. Mathé M, Valancogne G, Atallah A, Sciard C, Doret M, Gaucherand P, et al. Early pelvic floor muscle training after obstetrical anal sphincter injuries for the reduction of anal incontinence. Eur J Obstet Gynecol Reprod Biol. (2016) 199:201–6. doi: 10.1016/j.ejogrb.2016.01.025
6. Lewicky-Gaupp C, Mueller MG, Collins SA, Tavathia M, Geynisman-Tan J, Kenton KS. Early secondary repair of obstetric anal sphincter injury breakdown: contemporary surgical techniques and experiences from a peripartum subspecialty clinic. Female Pelvic Med Reconstr Surg. (2021) 27:e333–5. doi: 10.1097/SPV.0000000000000921
7. Hickman LC, Propst K, Swenson CW, Lewicky-Gaupp C. Subspecialty care for peripartum pelvic floor disorders. Am J Obstet Gynecol. (2020) 223:709–14. doi: 10.1016/j.ajog.2020.08.015
8. Chinn JJ, Eisenberg E, Artis Dickerson S, King RB, Chakhtoura N, Lim IAL, et al. Maternal mortality in the United States: research gaps, opportunities, and priorities. Am J Obstet Gynecol. (2020) 223:486–492.e486. doi: 10.1016/j.ajog.2020.07.021
9. Howell EA. Reducing disparities in severe maternal morbidity and mortality. Clin Obstet Gynecol. (2018) 61:387–99. doi: 10.1097/GRF.0000000000000349
10. Ozimek JA, Kilpatrick SJ. Maternal mortality in the twenty-first century. Obstet Gynecol Clin North Am. (2018) 45:175–86. doi: 10.1016/j.ogc.2018.01.004
11. Adams EK, Kramer MR, Joski PJ, Coloske M, Dunlop AL. Examination of the Black-White racial disparity in severe maternal morbidity among Georgia deliveries, 2016 to 2020. AJOG Glob Rep. (2024) 4:100303. doi: 10.1016/j.xagr.2023.100303
12. Foley MK, Djerboua M, Kushner T, Biondi MJ, Feld JJ, Terrault NA, et al. Maternal neighbourhood-level social determinants of health and their association with paediatric hepatitis C screening among children exposed to hepatitis C in pregnancy. Paediatr Perinat Epidemiol. (2024) 38(2):152–60. doi: 10.1111/ppe.13042
13. Meiman J, Grobman WA, Haas DM, Yee LM, Wu J, McNeil B, et al. Association of neighborhood socioeconomic disadvantage and postpartum readmission. Obstet Gynecol. (2023) 141:967–70. doi: 10.1097/AOG.0000000000005151
14. Yee LM, Silver RM, Haas DM, Parry S, Mercer BM, Iams J, et al. Quality of periconceptional dietary intake and maternal and neonatal outcomes. Am J Obstet Gynecol. (2020) 223:121.e121–121.e128. doi: 10.1016/j.ajog.2020.01.042
15. Moroni EA, Bustos SS, Mehta M, Munoz-Valencia A, Douglas NKO, Bustos VP, et al. Disparities in access to postmastectomy breast reconstruction: does living in a specific ZIP code determine the patient’s reconstructive journey? Ann Plast Surg. (2022) 88:S279–s283. doi: 10.1097/SAP.0000000000003195
16. Maroko AR, Doan TM, Arno PS, Hubel M, Yi S, Viola D. Integrating social determinants of health with treatment and prevention: A new tool to assess local area deprivation. Prev Chronic Dis. (2016) 13:E128. doi: 10.5888/pcd13.160221
17. Arora KS, Ascha M, Wilkinson B, Verbus E, Montague M, Morris J, et al. Association between neighborhood disadvantage and fulfillment of desired postpartum sterilization. BMC Public Health. (2020) 20:1440. doi: 10.1186/s12889-020-09540-5
18. Cabacungan ET, Ngui EM, McGinley EL. Racial/ethnic disparities in maternal morbidities: a statewide study of labor and delivery hospitalizations in Wisconsin. Matern Child Health J. (2012) 16:1455–67. doi: 10.1007/s10995-011-0914-6
19. Kind AJ, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. (2014) 161:765–74. doi: 10.7326/M13-2946
20. Messer LC, Laraia BA, Kaufman JS, Eyster J, Holzman C, Culhane J, et al. The development of a standardized neighborhood deprivation index. J Urban Health. (2006) 83:1041–62. doi: 10.1007/s11524-006-9094-x
21. Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible - the neighborhood atlas. N Engl J Med. (2018) 378:2456–8. doi: 10.1056/NEJMp1802313
22. University of Wisconsin School of Medicine and Public Health. 2021 Area Deprivation Index v4.0 (2023). Available online at: https://www.neighborhoodatlas.medicine.wisc.edu/ (Accessed June 1, 2024).
23. ACOG Practice Bulletin No. 198. Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. (2018) 132:e87–e102. doi: 10.1097/AOG.0000000000002841
24. Mowers EMB, Durst R, Giugale L. High patient satisfaction with postpartum pelvic floor healing clinic. In: Urogynecology (Phila) (2023) 29(10S):S41–S256.
25. Brincat C, Crosby E, McLeod A, Fenner DE. Experiences during the first four years of a postpartum perineal clinic in the USA. Int J Gynaecol Obstet. (2015) 128:68–71. doi: 10.1016/j.ijgo.2014.07.026
26. Guendelman S, Thornton D, Gould J, Hosang N. Obstetric complications during labor and delivery: assessing ethnic differences in California. Womens Health Issues. (2006) 16:189–97. doi: 10.1016/j.whi.2005.12.004
27. Thiel de Bocanegra H, Braughton M, Bradsberry M, Howell M, Logan J, Schwarz EB. Racial and ethnic disparities in postpartum care and contraception in California’s Medicaid program. Am J Obstet Gynecol. (2017) 217:47.e41–7. doi: 10.1016/j.ajog.2017.02.040
Keywords: area deprivation index, access to care, postpartum, health equity, median income, disparities, perineal laceration, obstetric anal sphincter injuries
Citation: Singh-Varma A, Wang L, Durst R, Moalli PA and Giugale LE (2025) Assessing access to care in a postpartum pelvic floor healing clinic. Front. Urol. 5:1548341. doi: 10.3389/fruro.2025.1548341
Received: 19 December 2024; Accepted: 25 March 2025;
Published: 16 April 2025.
Edited by:
Bilal Chughtai, Northwell Health, United StatesReviewed by:
Rui Viana, Fernando Pessoa Foundation, PortugalPaola Vasquez, Murdoch University, Australia
Copyright © 2025 Singh-Varma, Wang, Durst, Moalli and Giugale. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lauren E. Giugale, Z2l1Z2FsZWxlQHVwbWMuZWR1
 Anya Singh-Varma
Anya Singh-Varma Li Wang2
Li Wang2 Pamela A. Moalli
Pamela A. Moalli