- Department of Urology, Duke University School of Medicine, Durham, NC, United States
Objectives: Patients with a poorly functioning kidney, defined as less than 20% differential renal function, have historically been considered poor candidates for ipsilateral ureteral reconstruction for stricture. To determine if renal function can be safely preserved in poorly functioning kidneys with ureteral stricture, we evaluated patient outcomes following ureteral reconstruction.
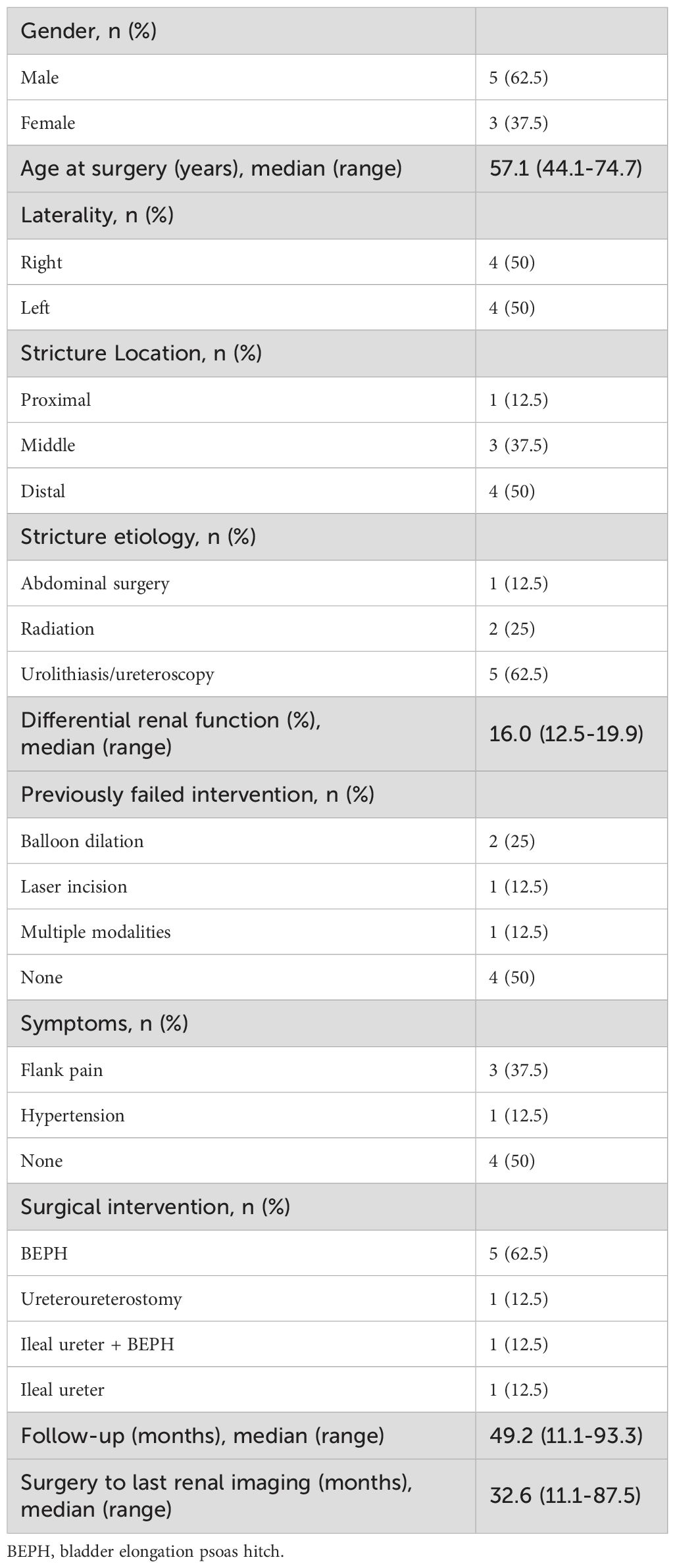
Methods: We conducted a review of 114 adult patients who underwent ureteral reconstructive surgery at our institution between 2013 and 2023. Patients with poorly functioning ipsilateral kidneys were identified by a preoperative renal scan (MAG3 renogram). Variables of interest included patient characteristics, peri/postoperative outcomes, resolution of hydronephrosis, pre/postoperative renal function, and preservation of renal parenchyma.
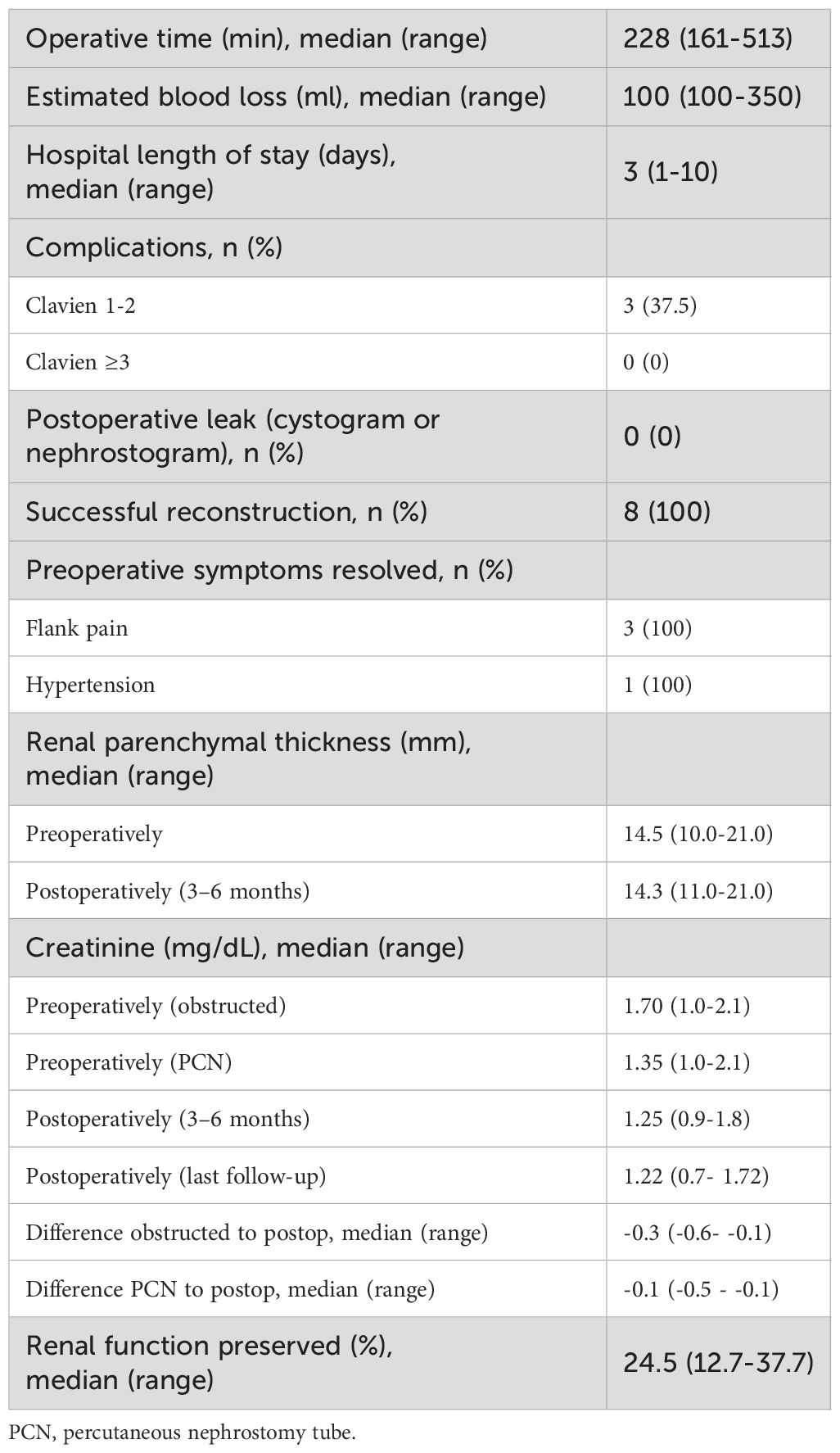
Results: Of the 8 patients meeting inclusion criteria, 5 underwent bladder elongation psoas hitch (BEPH), 1 ileal ureter, 1 ileal ureter with BEPH, and 1 ureteroureterostomy. Median preoperative differential renal function was 16.0% with a median preoperative serum creatinine (sCr) of 1.70 mg/dL before decompression and 1.35mg/dL after percutaneous nephrostomy tube (PCN) placement. Preoperative median average renal parenchyma thickness (RPT) was 14.5mm. At 6-month follow-up, median sCr and RPT were preserved at 1.25mg/dL (p= 0.084) and 14.3 mm (p=0.41), respectively. At median follow-up of 49.2 months, all patients had a successful repair, defined as no reinsertion of stent/PCN, resolution of hydronephrosis, and no return to the operating room for revision or nephrectomy. Median sCr at last follow-up showed sustained improvement at 1.22 (p=0.0097).
Conclusions: Reconstruction can be successful for obstructed kidneys with less than 20% differential function and may be considered prior to nephrectomy.
Introduction
Benign ureteral stricture is a relatively rare but potentially devastating disease that can result from urolithiasis, trauma, ischemia, radiation, infection, retroperitoneal fibrosis, iatrogenic causes, or be idiopathic in nature (1). These often present with flank pain but can also remain asymptomatic. The most feared consequence of chronic ureteral obstructions is irreversible renal injury, although urinary tract infections (UTI), hematuria, stone disease, proteinuria, chronic pain, and hypertension may also develop (2, 3). Ideally, strictures are identified early and definitively managed with surgical intervention before permanent damage to kidney function occurs.
Before intervention, 99mTc-mercaptoacetyltriglycine diuretic renography (MAG3 renal scan) is typically obtained if there is a concern for functional loss of the affected kidney (e.g. parenchymal loss on prior diagnostic imaging). In adults, kidneys with a differential renal function (DRF) of<15-20% have traditionally been considered unsalvageable, and nephrectomy has been recommended (3, 4). Endoscopic intervention was shown to be more likely to fail in poorly functioning kidneys by Wolf et al. in 1997 (5), and has been discouraged when DRF is<25% (3, 6). These historical precedents have led to nephrectomy being considered the de facto standard of care in patients with poorly functioning kidneys in this scenario.
With an aging global population and increasing incidence/prevalence of chronic kidney disease, our group now emphasizes maximal renal unit preservation whenever possible (7). This led us to challenge the classic dogma that poorly functioning kidneys are poor candidates for reconstruction. We hypothesize that reconstructive surgery for ureteral strictures in kidneys with less than 20% differential function is safe and successful. Herein, we report our group’s outcomes of ureteral reconstruction in patients with poorly functioning ipsilateral kidneys.
Materials and methods
Patient selection
We completed chart reviews of patients who underwent ureteral reconstruction for non-ureteropelvic junction (UPJ) ureteral stricture at our institution between 2013 and 2023. We defined the poorly functioning kidney as a renal unit on the ipsilateral side as the ureteral stricture/obstruction. DRF is established with preoperative MAG3 renal scans and defined for this study as less than 20% ipsilateral function. All patients who underwent ureteral reconstruction with an ipsilateral poorly functioning kidney and had completed a minimum of 6 months of follow-up were consecutively included. Our facility’s institutional review board (IRB) deemed this study to be exempt (IRB Number: Pro00109096).
Medical/surgical management and follow-up
Prior to surgical intervention for ureteral stricture, our standardized institutional protocol includes: assessment of renal function with a MAG3 renal scan, placement of a percutaneous nephrostomy (PCN) (if not present at the time of referral) with removal of any pre-existing ureteral stent to allow ureteral rest, performance of an antegrade nephrostogram (AN) after 4 to 6 weeks of ureteral rest, review of previously completed renal imaging [ultrasound (US) or computed tomography of the abdomen and pelvis (CT)], and a comprehensive conversation of treatment options (8). Typically, the shared decision-making conversation with patients who have an ipsilateral poorly functioning kidney (defined as<20% DRF on MAG3 renal scan) covers all appropriate surgical intervention for the size and location of stricture, conservative management with chronic PCN/ureteral stent, observation alone, or nephrectomy.
If reconstructive surgery is chosen, patients leave the operating room (OR) with a urethral catheter, ureteral stent, and capped PCN. If the bladder was utilized in the repair, follow-up begins at 10 days with an x-ray cystogram and urethral catheter removal (e.g. ureteral reimplantation bladder elongation psoas hitch (BEPH) and ileal ureter). Catheters are otherwise removed prior to discharge. At 4–6 weeks, AN is repeated and the ureteral stent is removed. After an additional week, AN is again repeated with PCN removal if the ureter is patent and intact. At 6 months post-operation, the patient is seen for symptom review, physical examination, renal function testing, and renal ultrasound. Patients with a history of radiation follow the same care pathway. If the recovery has proceeded without complication, periodic monitoring of renal function and renal imaging can continue with the patient’s primary care provider. Repeat MAG3 renal scans are rarely clinically indicated.
Data collection and analysis
We recorded patient demographics, resolution of hydronephrosis, need for additional intervention, pre/postoperative renal function, postoperative complications, and preservation of renal parenchyma on imaging. If multiple renal function tests or imaging studies were available, the results nearest to the patient’s initial urology evaluation or follow-up for a given time point were used. Postoperative development or progression of hypertension, flank pain, and recurrent UTI were also recorded. Successful treatment is defined as meeting all the following criteria: no reinsertion of stent/PCN, resolution of hydronephrosis, stability of decompressed renal function, and no return to the OR for revision or nephrectomy by most recent follow-up. The resolution of hydronephrosis was evaluated on both post-operative imaging at 6-month follow-up and the most recent available renal imaging. Most recent follow-up is considered any provider encounter with renal function testing.
Renal function preserved (RFP) is defined as the difference between postoperative estimated glomerular filtration rate (GFR) and obstructed GFR (prior to PCN placement), divided by obstructed GFR, and is reported as a percentage (). For example, if a patient with an obstructed kidney has a GFR of 50 ml/min, then undergoes reconstruction rather than nephrectomy and has a documented improvement in GFR to 60 ml/min, RFP would be 20%. To assess the potential effect of compensation by the contralateral (unaffected) kidney, a predicted new baseline glomerular filtration rate (NBGFR) was calculated for each patient using the formula . Similar calculations have been described in the nephrectomy literature and are often used in preoperative counseling prior to nephrectomy for malignancy (9).
In conjunction with serum renal function markers (creatinine and GFR), average renal parenchymal thickness (RPT) was measured as a correlate to the function of the renal unit (9–11). Renal volume was not used as it is distorted by preoperative hydronephrosis. RPT measurements were made using the method described by Roger et al. (12) For consistent comparison across the cohort, RPT was measured on preoperative imaging and follow-up imaging at 6-month follow-up. Both US and CT imaging were used for measurements (often only US is obtained postoperatively, while CT imaging more commonly diagnosed the ureteral obstruction), which correlate well enough for this purpose (11).
Statistical analysis
Statistics were calculated using the Paired T test (two-tailed) and Wilcoxon Signed Rank Test (WSRT). A value of p<0.05 is defined as significant. The two tests agreed on significance unless stated within the text.
Results
Between 2013 and 2023, 114 patients underwent ureteral reconstruction for non-UPJ ureteral stricture at our institution. Of these, 8 patients had a preoperative MAG3 renal scan showing<20% ipsilateral renal function. Median follow-up was 49.2 months (range: 11.1-93.3 months). All of the patients had follow-up greater than six months; therefore none were excluded from analysis. Patient characteristics are described in Table 1. The median DRF of the affected kidney was 16.0% (range: 12.5-19.9%). Half of the cohort failed at least one intervention prior to referral to our center, with 1 patient undergoing both balloon dilation and laser incision and 1 patient undergoing 3 balloon dilations. BEPH was the most common intervention (n=5, 62.5%). All surgeries were performed open.
Perioperative and postoperative outcomes are outlined in Table 2. Operative times were highly varied (range: 161–513 minutes), with longer procedures associated with operations requiring multiple interventions (ileal ureter with BEPH, 513 minutes; BEPH with abdominal perineal resection, 503 minutes). Reported complications included ileus (n=2, both in patients requiring ileal ureter) and UTI (n=1). No patients required invasive intervention or return to the OR in the postoperative period.
Upon follow-up, no patients were found to have a leak on cystogram or nephrostogram, and all urethral catheters/PCNs were removed on schedule. Prior to reconstruction, 3 patients complained of preoperative flank pain, and 1 demonstrated obstruction-associated hypertension. Postoperatively, all three had resolution of their pain and the hypertension normalized. No patients developed new-onset postoperative flank pain, hypertension, recurrent UTI, or proteinuria.
RPT was similar before intervention and at 6-month follow-up at 14.5 mm (range: 10.0-21.0 mm) and 14.3 mm (range:11.0-21.0mm), respectively (p= 0.41). The most recent imaging available was completed at a median 32.1 months (range: 11.0-86.3 months) postoperatively. All patients had a successful reconstruction (as defined above).
Serum creatinine (sCr) trends are illustrated in Figure 1. Prior to reconstruction, renal function improved following PCN placement from a median sCr 1.70 mg/dL (range 1.0-2.1mg/dL) to 1.35 mg/dL (range: 1.0-2.1) (p=0.076). After reconstruction, the median sCr at 6-month follow-up improved to 1.25 mg/dL (range: 0.9-1.8mg/dL) and 1.22 mg/dL (range: 0.7-1.72mg/dL) at the most recent follow-up [p= 0.084, significant on WSRT and 0.0097, respectively (post-PCN sCr compared to follow-up sCr)]. Improvement in sCr between obstructed levels and 6-month follow-up was statistically significant (p= 0.0018). Overall, median RFP was 24.5% (range: 12.7-37.7%), when calculated using GFR at 6-month follow-up. GFR at last follow-up was a median 10.6 ml/min higher (median 24.1% greater) than the predicted NBGFR if nephrectomy was chosen instead of reconstruction (p=0.013).
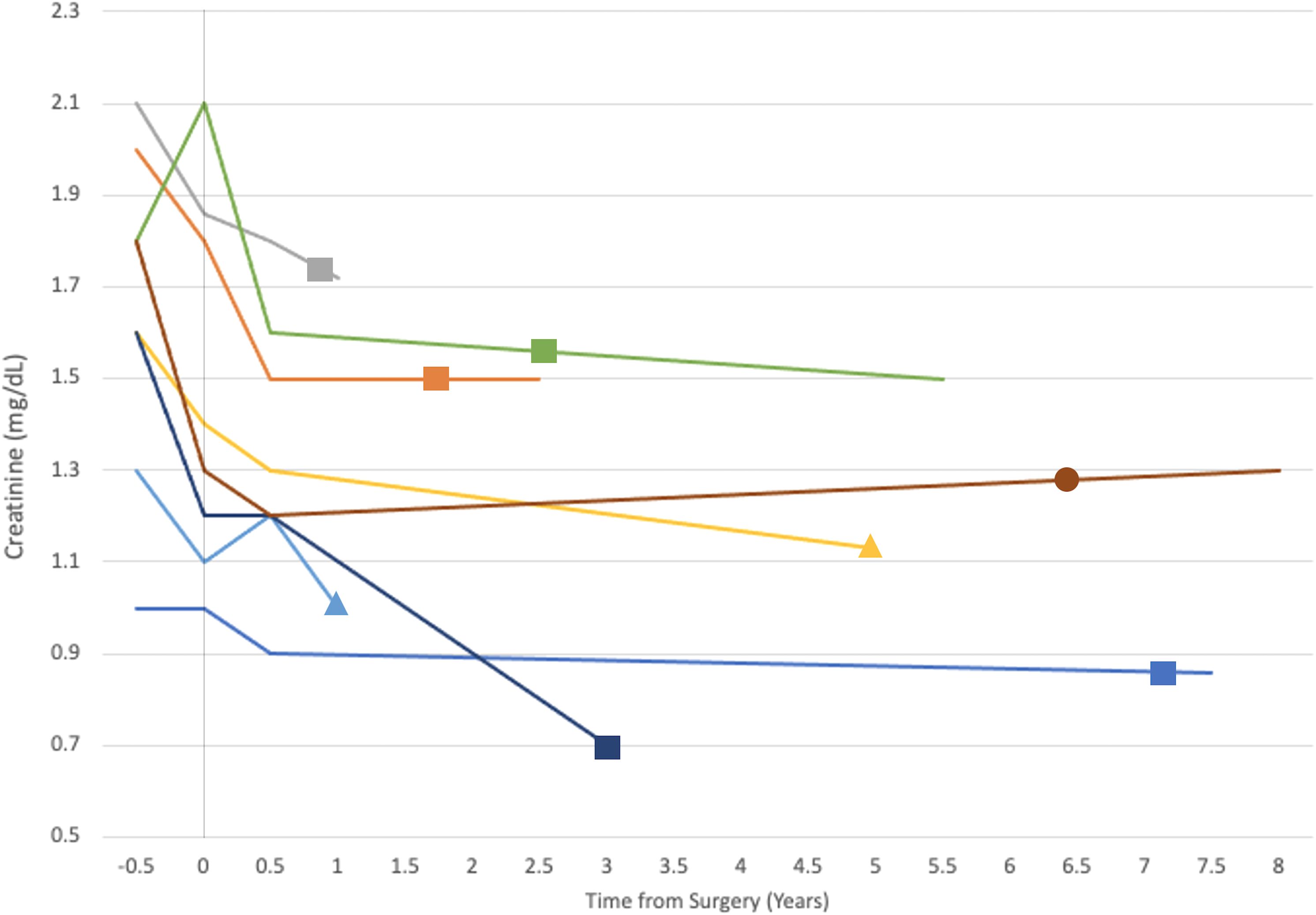
Figure 1. The evolution of creatinine (y-axis) over time (x-axis) in years with 0 on the x-axis marking the time of surgery. Each line represents a single patient and terminates at the time of their last follow-up. Shapes appear on each patient’s line at the time of their most recent renal imaging. Shape type correlates with the surgical intervention undergone by the associate patient: square, bladder elongation psoas hitch (BEPH); triangle, ileal ureter/ileal ureter with BEPH; circle, ureteroureterostomy.
Discussion
Attempts to challenge the dogma in adult clinical urology that ureteral obstruction in kidneys with decreased function is best addressed with extirpative surgery have exclusively evaluated UPJ obstruction. This topic has been more thoroughly assessed in pediatric populations, with many studies favoring renal preservation (13–15). A systematic review of pyeloplasty for UPJ obstruction in adults with poorly functioning kidneys showed notable improvement in obstructive symptoms without a clear trend in postoperative renal function across available studies (3 of the 9 included studies showed a statistically significant improvement in renal function, while the others did not show a significant change) (16). Some contemporary examples support higher failure rates of reconstruction in poorly functioning kidneys as originally described by Wolf et al. (5, 17) While no literature is available on the rates of treatment utilization, most poorly functioning kidneys with ureteral stricture are managed with nephrectomy or decompression without attempt at repair. Neither the American Urologic Association nor the European Association of Urology guidelines address this specific scenario. “Poorly functioning kidney” is heterogeneously defined in the literature as less than 10 to 30% differential function. 20% is frequently chosen within this range by UPJ reconstruction investigators and was adopted for this investigation (3, 16). To our knowledge, this is the first report to evaluate the outcomes of ureteral reconstruction for strictures distal to the UPJ in poorly functioning kidneys.
Rising rates of chronic kidney disease (CKD) (incidence increased globally by 88.76% from 1990 to 2016) make nephron-preserving surgical techniques more important than ever before (7). This becomes even more pertinent when considering specific patient populations, including those with cancer, whose treatment options may depend on their GFR. Moreover, renal insufficiency is associated with worse overall survival in patients with solid tumors (18). Urologists have already embraced changes to the surgical standard of care to promote renal preservation. When feasible, partial nephrectomy is a preferred treatment option over radical nephrectomy for this purpose (19). It is imperative to determine if total renal function can be preserved by ureteral reconstruction, even if the ipsilateral kidney contributes<20%.
The incidence of ureteral stricture distal to the UPJ is unknown, but it is generally understood that UPJ obstruction is a more prevalent pathology (3, 4). Pyeloplasty is widely accepted as the gold standard for UPJ obstruction treatment, while management of more distal strictures is less clearly defined and sometimes more technically challenging (20). Given these differences, it is understandable that there is more available literature discussing the management of UPJ obstruction in poorly functioning kidneys (4, 15, 21). It is also likely that few poorly functioning kidneys are being chosen for reconstruction given the widely accepted view that nephrectomy is the preferred treatment (these rates have not been described). Most graduating urology trainees in the United States feel comfortable performing a nephrectomy but may be less experienced with complex ureteral reconstruction (22). In a health system with a shortage of reconstructive urologists, it can be assumed that few kidneys with<20% DRF and ipsilateral ureteral stricture undergo an attempt at reconstruction (23).
Although a distinct disease process from ureteral strictures distal to the UPJ, contemporary literature supports renal preservation in poorly functioning kidneys with UPJ obstruction (14–16, 24). For example, Nishi et al. showed that median improvement in split renal function following pyeloplasty for UPJ obstruction in kidneys with<20% DRF was 24.0% at 6 months and 38.3% at 12 months follow-up (13 of 15 patients in this cohort were adults) (4). Nascimento et al. demonstrated stable renal function following pyeloplasty in kidneys with<15% DRF in a cohort of 15 adult patients (21). While these results would suggest favorable outcomes of ureteral reconstruction for strictures distal to the UPJ in poorly functioning kidneys, they cannot be directly extrapolated.
Despite this cohort’s size, it reveals a statistically and clinically relevant improvement in renal function following ureteral reconstruction. All patients had improved or stable renal function at median follow-up of 49.2 months when compared to the time of their surgery (when decompressed with PCN). The comparison between obstructed renal function and postoperative renal function may be of higher importance. Physiologically, it can be speculated that renal function in a patient with a unilateral chronically, completely obstructed kidney would be similar post-nephrectomy. Median total RFP, which represents the relative change between obstructed and reconstructed total renal function, is 24.5% in this cohort. In other words, if these patients were treated with nephrectomy rather than reconstruction, the predicted median total renal function would be 24.5% lower than the observed postoperative levels.
As observed in patients after nephrectomy, a portion of the improvements in total renal function following ureteral reconstruction could theoretically result from compensation of the contralateral kidney (9, 25). Postoperative MAG3 renograms can evaluate for this confounding factor. The study by Nishi et al. did evaluate pre/postoperative DRF and showed a significant increase in DRF of the affected kidney (as described above) (4). Their findings support the assertion that the reconstructed kidney is contributing to the improvement in overall renal function in a meaningful way. In lieu of postoperative radionuclide imaging in this cohort, analysis of the change in RPT was completed. RPT has been shown to linearly correlate with loss of renal function and CKD (9, 10, 26). It was predicted that stability of RPT in the affected kidney would indicate stability of function, whereas declining RPT would suggest progressive atrophy. No significant change in RPT was noted in this study (median RPT 14.5mm preoperatively and 14.3mm postoperatively). Therefore, it is probable that the affected kidneys continue to have at least a stable DRF. Average RPT varies by region, age, height, weight, and laterality (27). To our knowledge, there are no generalizable reference values for RPT in the literature- significance was only given to individual patients’ RPT trend.
A predicted NBGFR was calculated for each patient to further discern if the reconstructed poorly functioning kidney was contributing to the global renal function independently of contralateral compensation. This NBGFR represents the patients’ expected renal function if their strictures were treated with nephrectomy instead of reconstruction (9). Consistent with the RFP calculations, the cohorts observed GFR was a median 24.1% greater than the predicted NBGFR, which represents a clinically significant difference in renal function. Again, this comparison suggests that a meaningful percentage of total renal function can be preserved with reconstruction of poorly functioning kidneys.
Stability of renal function was of primary interest, but quality of life factors should not be overlooked. Reconstructive surgery offered patients symptom improvement from flank pain (n=3) and hypertension (n=1). All patients were PCN and ureteral stent-free following definitive surgical management, both of which have been shown to have a detrimental impact on lifestyle, but were not specifically evaluated in this study (28).
This study has several limitations inherent to its small sample size and retrospective design. While this is a report on a small patient cohort it is important to remember that for uncommon diseases and rare conditions, case series and reports still contribute significant value to the literature (29). Each individual intervention in this cohort was not uniform amongst all patients making direct comparison somewhat difficult. Treatment choice for ureteral stricture is nuanced and ureteral stricture reconstruction in poorly functioning kidneys is rare, which makes the organization of a sizable or homogenous cohort difficult. Selection bias is inherent to retrospective studies; patients with a larger number of comorbidities or those requiring more difficult reconstructions may have undergone conservative management or nephrectomy outside of our healthcare system without referral. In this case, our cohort would comprise better surgical candidates who would be expected to have preferable outcomes. Given our experience, we do not believe that a randomized controlled trial would be possible. However, a multi-institutional case-control study would offer higher quality evidence to support the efficacy of reconstruction of kidneys with<20% DRF and should represent the next step of future research. The findings described here may not single-handedly change the current treatment paradigm, but they do demonstrate that ureteral reconstruction in poorly functioning kidneys can be completed safely and successfully.
In conclusion, upper urinary tract reconstruction was safe and successful for obstructed kidneys with less than 20% split function within this small patient series. While more robust investigation is indicated, we recommend abandoning the dogma of nephrectomy alone for these patients to maximize the preservation of renal function.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Duke University institutional review board (#Pro00109096). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because deidentified retrospective review of patient outcomes was deemed to be exempt.
Author contributions
LG: Data curation, Investigation, Visualization, Methodology, Conceptualization, Validation, Writing – original draft, Formal analysis, Writing – review & editing. KS: Data curation, Formal analysis, Methodology, Writing – review & editing, Investigation, Conceptualization. MS: Data curation, Investigation, Writing – review & editing. AL: Investigation, Writing – review & editing, Data curation. ACL: Resources, Writing – review & editing, Supervision. AP: Formal analysis, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
ACL: Speaker, consultant, and preceptor for Coloplast Corporation and Boston Scientific Corporation. AP: Speaker, consultant, and researcher for Boston Scientific Corporation.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be constructed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tyritzis SI and Wiklund NP. Ureteral strictures revisited … trying to see the light at the end of the tunnel: a comprehensive review. J Endourol. (2015) 29:124–36. doi: 10.1089/end.2014.0522
2. Riehle RA Jr. and Vaughan ED Jr. Renin participation in hypertension associated with unilateral hydronephrosis. J Urol. (1981) 126:243–6. doi: 10.1016/s0022-5347(17)54461-4
4. Nishi M, Matsumoto K, Fujita T, and Iwamura M. Improvement in renal function and symptoms of patients treated with laparoscopic pyeloplasty for ureteropelvic junction obstruction with less than 20% Split renal function. J Endourol. (2016) 30:1214–8. doi: 10.1089/end.2016.0553
5. Wolf JS Jr., Elashry OM, and Clayman RV. Long-term results of endoureterotomy for benign ureteral and ureteroenteric strictures. J Urol. (1997) 158:759–64. doi: 10.1097/00005392-199709000-00016
6. Wieder JA. Pocket guide to urology United States J wieder medical. (2021) 441. Oakland, CA: J. Wieder Medica.
7. Xie Y, Bowe B, Mokdad AH, Xian H, Yan Y, Li T, et al. Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. (2018) 94:567–81. doi: 10.1016/j.kint.2018.04.011
8. Lee Z, Lee M, Lee R, Koster H, Cheng N, Siev M, et al. Ureteral rest is associated with improved outcomes in patients undergoing robotic ureteral reconstruction of proximal and middle ureteral strictures. Urology. (2021) 152:160–6. doi: 10.1016/j.urology.2021.01.058
9. Lewis K, Maina EN, Lopez CM, Rathi N, Attawettayanon W, Kazama A, et al. Limitations of parenchymal volume analysis for estimating split renal function and new baseline glomerular filtration rate after radical nephrectomy. J Urol. (2024) 211:775–83. doi: 10.1097/ju.0000000000003903
10. Bargman JM and Skorecki KL. Chronic kidney disease. In: Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL, and Loscalzo J, editors. Harrison’s principles of internal medicine, vol. 20e . McGraw-Hill Education, New York, NY (2018).
11. Braconnier P, Piskunowicz M, Vakilzadeh N, Müller M-E, Zürcher E, Burnier M, et al. How reliable is renal ultrasound to measure renal length and volume in patients with chronic kidney disease compared with magnetic resonance imaging? Acta Radiologica. (2020) 61:117–27. doi: 10.1177/0284185119847680
12. Roger SD, Beale AM, Cattell WR, and Webb JA. What is the value of measuring renal parenchymal thickness before renal biopsy? Clin Radiol. (1994) 49:45–9. doi: 10.1016/s0009-9260(05)82913-7
13. Gupta DK, Chandrasekharam VV, Srinivas M, and Bajpai M. Percutaneous nephrostomy in children with ureteropelvic junction obstruction and poor renal function. Urology. (2001) 57:547–50. doi: 10.1016/s0090-4295(00)01046-3
14. Aziz MA, Hossain AZ, Banu T, Karim MS, Islam N, Sultana H, et al. In hydronephrosis less than 10% kidney function is not an indication for nephrectomy in children. Eur J Pediatr Surg. (2002) 12:304–7. doi: 10.1055/s-2002-35956
15. Lone YA, Samujh R, Bhattacharya A, and Kanojia RP. Outcome of poorly functioning kidneys secondary to PUJO preserved by pyeloplast. J Pediatr Surg. (2017) 52:578–81. doi: 10.1016/j.jpedsurg.2016.11.039
16. Freitas PFS, Barbosa J, Andrade HS, Arap MA, Mitre AI, Nahas WC, et al. Pyeloplasty in adults with ureteropelvic junction obstruction in poorly functioning kidneys: A systematic review. Urology. (2021) 156:e66–73. doi: 10.1016/j.urology.2021.05.017
17. Grimsby GM, Jacobs MA, and Gargollo PC. Success of laparoscopic robot-assisted approaches to ureteropelvic junction obstruction based on preoperative renal function. J Endourol. (2015) 29:874–7. doi: 10.1089/end.2014.0876
18. Launay-Vacher V, Janus N, and Deray G. Renal insufficiency and cancer treatments. ESMO Open. (2016) 1:e000091. doi: 10.1136/esmoopen-2016-000091
19. Tan H-J, Norton EC, Ye Z, Hafez KS, Gore JL, and Miller DC. Long-term survival following partial vs radical nephrectomy among older patients with early-stage kidney cancer. JAMA. (2012) 307:1629–35. doi: 10.1001/jama.2012.475
20. Abboudi H, Ahmed K, Royle J, Khan MS, Dasgupta P, and N’Dow J. Ureteric injury: a challenging condition to diagnose and manage. Nat Rev Urol. (2013) 10:108–15. doi: 10.1038/nrurol.2012.254
21. Nascimento B, Andrade HS, Miranda EP, Barbosa J, Moscardi PR, Arap MA, et al. Laparoscopic pyeloplasty as an alternative to nephrectomy in adults with poorly functioning kidneys due to ureteropelvic junction obstruction. Int Urol Nephrol. (2021) 53:269–73. doi: 10.1007/s11255-020-02626-4
22. Okhunov Z, Safiullah S, Patel R, Juncal S, Garland H, Khajeh NR, et al. Evaluation of urology residency training and perceived resident abilities in the United States. J Surg Educ. (2019) 76:936–48. doi: 10.1016/j.jsurg.2019.02.002
23. Santucci RA. The reconstructive urology work force: present and future. Transl Androl Urol. (2014) 3:205–8. doi: 10.3978/j.issn.2223-4683.2014.04.08
24. Zhang S, Zhang Q, Ji C, Zhao X, Liu G, Zhang S, et al. Improved split renal function after percutaneous nephrostomy in young adults with severe hydronephrosis due to ureteropelvic junction obstruction. J Urol. (2015) 193:191–5. doi: 10.1016/j.juro.2014.07.005
25. Garg AX, Muirhead N, Knoll G, Yang RC, Prasad GV, Thiessen-Philbrook H, et al. Proteinuria and reduced kidney function in living kidney donors: A systematic review, meta-analysis, and meta-regression. Kidney Int. (2006) 70:1801–10. doi: 10.1038/sj.ki.5001819
26. Kodikara I, Gamage DTK, Nanayakkara G, and Ilayperuma I. Diagnostic performance of renal ultrasonography in detecting chronic kidney disease of various severity. Asian BioMed (Res Rev News). (2020) 14:195–202. doi: 10.1515/abm-2020-0028
27. Eze C, Okoye J, and Agwu K. Normative ultrasound values of renal parenchymal thickness among adults in Enugu, South-East Nigeria. Afr Health Sci. (2014) 14:689–97. doi: 10.4314/ahs.v14i3.27
28. Shoshany O, Erlich T, Golan S, Kleinmann N, Baniel J, Rosenzweig B, et al. Ureteric stent versus percutaneous nephrostomy for acute ureteral obstruction - clinical outcome and quality of life: a bi-center prospective study. BMC Urol. (2019) 19:79. doi: 10.1186/s12894-019-0510-4
Keywords: ureteral stricture, reconstruction, renal function, dogma, stricture disease
Citation: Grimaud LW, Sury K, Salvino M, Livingston A, Lentz AC and Peterson AC (2025) Ureteral reconstruction is safe and successful in poorly functioning kidneys. Front. Urol. 5:1593307. doi: 10.3389/fruro.2025.1593307
Received: 13 March 2025; Accepted: 07 August 2025;
Published: 09 September 2025.
Edited by:
Simone Morra, Federico II University Hospital, ItalyReviewed by:
Nicola Pavan, University of Palermo, ItalyMatthew Dunn, University of California, Los Angeles, United States
Copyright © 2025 Grimaud, Sury, Salvino, Livingston, Lentz and Peterson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Logan W. Grimaud, bG9nYW4uZ3JpbWF1ZEBkdWtlLmVkdQ==
 Logan W. Grimaud
Logan W. Grimaud Kiran Sury
Kiran Sury Andrew C. Peterson
Andrew C. Peterson