- 1Department of Midwifery, College of Health Sciences, Woldia University, Woldia, Ethiopia
- 2College of Medicine and Health Sciences, School of Nursing and Midwifery, Wollo University, Dessie, Ethiopia
- 3Department of Midwifery, School of Nursing and Midwifery, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Background: Prenatal ultrasound (US) is essential in antenatal care worldwide and offers significant benefits for maternal and neonatal health. It should be a standard procedure in low- income countries. However, its utilization remains poor in nations such as Ethiopia.
Objective: This study aimed to assess the use of prenatal ultrasound and associated factors among pregnant women who attended antenatal care in South Wollo Zone Public Hospitals, Northeast Ethiopia, in 2023.
Method: An institution-based cross-sectional study was conducted among 590 pregnant women from December 30, 2022, to February 28, 2023, in selected South Wollo Zone Public Hospitals. The data were coded, cleaned, and entered into Epi-Data version 4.6 and subsequently exported to SPSS version 26 for analysis. The strength of the association between the dependent and independent variables was presented as odds ratios (ORs) at a 95% confidence interval (95% CI), with a P-value of less than 0.05 according to multivariable logistic regression.
Results: The prevalence of prenatal ultrasound utilization was 62.8% [95% CI: 58.7%–66.8%]. The significant factors associated with utilization included urban residency (AOR = 4.82, 95% CI: 2.99–8.03), mothers’ knowledge (AOR = 7.36, 95% CI: 4.06–13.32), educational status above primary (AOR = 2.10, 95% CI: 1.09–4.05), medical illness (AOR = 3.03, 95% CI: 1.64–5.59), government employment (AOR = 4.05, 95% CI: 1.70–9.64), and private employment (AOR = 2.34, 95% CI: 1.58–7.05).
Conclusion: The proportion of patients who underwent prenatal ultrasound was lower than the WHO recommendation. The factors most significantly associated with ultrasound utilization were women's knowledge, urban residency, educational status, medical illness, and occupation. Therefore, the author recommended for health care providers educating mothers on the purposes of obstetric ultrasound and including a prenatal ultrasound screening as part of antenatal care is needed.
1 Introduction
Medical imaging is indispensable for medical practice today. Obstetric ultrasound is a harmless, inexpensive, and noninvasive imaging modality that helps to scan a pregnant mother's abdominal and pelvic cavity with high-frequency sound waves and delivers a real-time images of the fetus to parents (1). Diagnostic ultrasound is recognized as a safe, effective, and highly flexible imaging modality capable of providing clinically relevant information about most parts of the body rapidly and cost-effectively. Prenatal ultrasound utilization is an integral part of antenatal care worldwide (2).
The International Federation of Gynecology and Obstetrics (FIGO) recommends two ultrasound examination services for all pregnant women (3). Similarly, in 2016, the World Health Organization (WHO) recognized the benefits of offering at least one antenatal ultrasound scanning service, before 24 weeks of gestation for all pregnant women (4).
Ultrasound has been used to diagnose obstructed labor, non-cephalic presentation, single or multiple pregnancy, incomplete miscarriage, molar pregnancy, ectopic pregnancy, fetal abnormality, intrauterine growth restriction and placenta previa (5, 6). Although the degree of diagnostic accuracy may vary depending on when pregnant women present themselves for an ultrasound exam (7). Applications of ultrasound also extend to abdominal, musculoskeletal, cardiac, renal, pulmonary, trauma and soft tissue and vascular conditions (7–9).
A study shown that a minimum of three screening tests should be performed during pregnancy. The first should be performed at the fetal age of 10–14 weeks to detect abnormalities and pathological conditions in early pregnancy. The second one has to be performed between the fetal ages of 18 and 22 weeks to assess detailed fetal anatomy and rate of development. The third should be performed between the fetal age of 30 and 34 weeks to assess fetal anatomy, rate of development, placentation and circulation (10). In low-income countries where there is a lack of machines and qualified sonographers, high-risk conditions during pregnancy might be undetected until delivery. Information generated on maternal, fetal and placental conditions using ultrasound imaging enhances the diagnosis and management of life-threatening conditions (9, 10).
Ultrasound in antenatal care (ANC) is crucial for assessing maternal health, pregnancy progression and fetal development (11). In developed countries such as Vietnam and India, the prevalence of ultrasound scans during ANC is high, averaging 6.6 scans per 8 visits (12). Another study conducted in Vietnam revealed that, women scans 8–10 times throughout pregnancy (13). In low- and middle-income countries (LMICs), the prevalence of ANC is approximately 24% (14). In sub-Saharan Africa, utilization rates are 30% in urban areas and 6.9% in rural areas, significantly below WHO recommendations (15). A study in Ethiopia showed first-trimester scan rates of 5.2%, 3.7%, and 8.1% for the Amhara, Oromia, and SNNP regions, respectively, with second-trimester scans of 22.2%, 26.6%, and 48.6% respectively. Only one in six eligible women received a scan, which is much lower than the WHO's recommendation of at least one scan before 24 weeks of gestation (16).
Maternal and neonatal morbidity and mortality are critical health indicators (12). Globally, in 2017, an estimated 295,000 women died due to pregnancy and childbirth, 99% of whom died in LMICs where ANC quality is low (16, 17). It has also been reported that up to 37% of patients are potentially misdiagnosed. All the above could be reduced by incorporating U/S services in their care (12, 14, 16). In the Philippines, providing ultrasound during prenatal visits reduced maternal and neonatal deaths by 6.3% and 26.1%, respectively, and was cost-effective (18). Although antenatal ultrasound use did not affect mortality measures, there is evidence suggesting that ultrasound can confirm and improve patient management for both obstetric and non-obstetric conditions. A recent cluster-randomized trial found that use of ultrasound in rural health centers did not impact antenatal care attendance, facility delivery, maternal mortality, neonatal mortality and stillbirths (19). In contrary, a study conducted in three regions of Ethiopia found that introducing ultrasound services at the primary health care level, by mid-level health professionals, led to an increase in both antenatal and postnatal care utilization (20).
The use of ultrasound in developing countries is limited by several factors, such as culture, religion, illiteracy, attitude, accessibility and the high cost of ultrasound equipment; the fee of using ultrasound in a private clinic; the lack of trained sonographers or physicians; and the skill required to perform the examinations (15). Studies have suggested that the long interval between visits from 32 to 36 weeks could result in non-detection of intrauterine growth restriction and other problems that could arise and cause foetal death in the third trimester (21, 22). Moreover, poor utilization of ultrasound has indicated a high prevalence of adverse perinatal outcomes, such as ectopic pregnancies, abortions, congenital anomalies, fetal death, and increased maternal and neonatal morbidity and mortality (23). A systematic review in Ethiopia revealed a high incidence of neural tube defects (63.3% per 10,000), which contributes increased abortion rates (7, 24).
Ethiopia is working to improve maternal health care quality, reduce morbidity and mortality, and achieve sustainable development goals (16). The Ethiopian Ministry of Health aims to provide at least one ultrasound scan for all pregnant women before 24 weeks of gestation (25). The USAID Transform: Primary Health Care Activity provides 100 ultrasound machines to health centers and trains206 mid-level providers in ultrasound use (26).
Despite these efforts, maternal and neonatal morbidity and mortality remain high due to poor utilization of prenatal ultrasound scans (16). This study addresses new variables, such as maternal knowledge and attitudes toward obstetric ultrasound utilization, which previous studies did not cover. As far as my search is concerned, no published studies have assessed the proportion of prenatal ultrasound utilization in the South Wollo Zone. Therefore, this study aimed to determine the prevalence and associated factors of prenatal ultrasound among pregnant women attending ANC in South Wollo Zone Public Hospitals.
2 Methods and materials
2.1 Study design, area and period
A hospital based cross-sectional study was conducted at the South Wollo Zone Public Health Institution from December to February 2023. The town is found in the southern Wollo zone, southeastern Ethiopia, and is approximately 401 km away from Addis Ababa, the capital city of Ethiopia. The zone comprises 14 governmental hospitals (one comprehensive specialized hospital, four general hospitals, and nine primary hospitals) and four private hospitals. There are also 119 health centers and 450 health posts in the zone. All public and private hospitals provide all types of obstetric care including antenatal care, ultrasound services and outpatient and inpatient services. According to South Wollo Zone Health Bureau reports, the estimated number of antenatal admissions in South Wollo Zone Public Hospitals is 1800 women per month. The financial coverage of ANC services in Ethiopia is cost free and limited by the state. According to the 2017 Central Statistical Agency (CSA) of Ethiopia, the total estimated population of the South Wollo Zone is 3,086,132 from which these women accounts for almost half of the entire population. The language spoken in the zone was mainly Amharic.
2.2 Study design
An institution-based cross-sectional study was conducted.
2.3 Source population
All pregnant women were receiving antenatal care in South Wollo Zone Public Hospitals.
2.4 Study population
All pregnant women were receiving antenatal care at selected South Wollo Zone Public Hospitals during the data collection period.
2.5 Inclusion criteria
All pregnant women who attended antenatal care and who had been living for at least 6 months in the southern Wollo zone were included.
2.6 Exclusion criteria
Pregnant women who were severely ill and unable to communicate during the data collection period.
2.7 Sample size determination
The sample size was calculated based on a single population proportion formula using the following assumptions. The use of prenatal ultrasound.
Taken p = 50%.
where n is the minimum sample size needed, p is the estimated proportion of prenatal ultrasound utilization, z is the standard value of the confidence level of α = 95% and d = 0.05 is the margin of error between the sample and the population.
For this study, p = 60.7%, since a study was performed in Jimma, Oromia Region, in Ethiopia on the proportion of prenatal ultrasound utilization (19).
Since we used two-stage sampling procedures and then multiplied by deff or 1.5, which is almost equal to 536, by adding a 10% nonresponse rate, the final sample size became 590.
2.8 Sampling techniques and procedure
There are fourteen public hospitals in the South Wollo Zone. Of these, five public hospitals were selected randomly by the lottery method. The allocation of the samples to the hospitals was performed proportionally based on the average number of clients who received antenatal care at each hospital in the most recent 3-month report of each health facility. Study participants were selected at each facility by systematic random sampling techniques. The participants were selected in the order in which they came to health facilities. Participant card numbers were used to systematically select participants in every Kth, interval taking K = N/n = 974/590 = 1.65 ≈ 2. The first sample was selected randomly and then samples were taken every Kth interval until the required sample size was obtained. (where N is the source population taken from the Zone Health Bureau Three-month Antenatal Care Report of five selected hospitals and n is the sample size for this study (as shown in Figure 1).
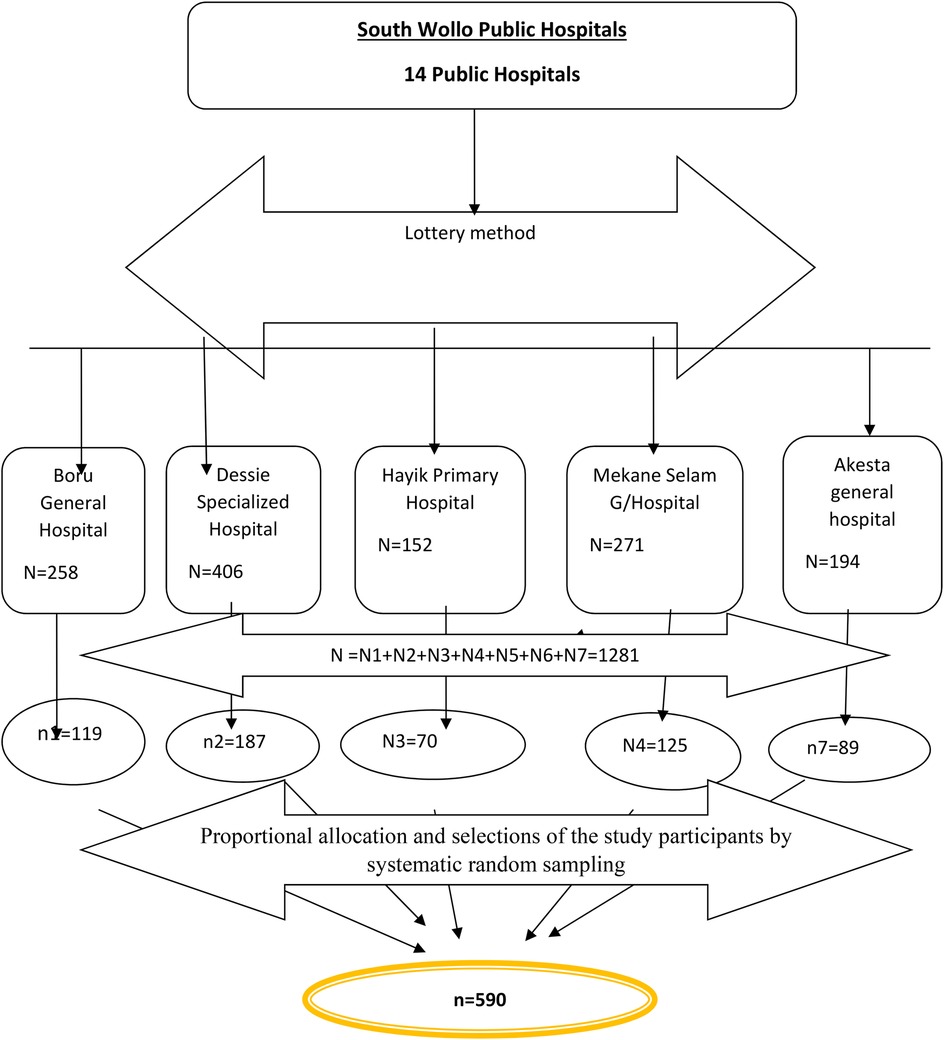
Figure 1. Schematic representation of sampling procedure for prenatal ultrasound utilization and associated factors among women who attending ANC in South Wollo Zone Public Hospitals, North-east, Ethiopia, 2023.
2.9 Dependent Variables
Proportion of prenatal ultrasound utilization
2.10 Independent variables
• Sociodemographic factors: Maternal age, residence, ethnicity, marital status, monthly income, religion, educational level of the mother, and husband's education
• The obstetric factors: included parity, gravidity, history of abortion, history of ectopic pregnancy, history of recent congenital anomaly, illness experienced in recent pregnancy, and twin pregnancy
• Maternal factors: maternal knowledge of obstetric ultrasound findings and maternal attitudes toward obstetric ultrasound findings.
2.11 Operational definitions
Obstetric ultrasound utilization: In this study, the utilization of ultrasound by pregnant women was defined as obtaining ultrasound services at least once during a recent pregnancy (27).
Knowledge of obstetric ultrasound: Respondents who answered more than or equal to 6 questions (50%) of knowledge-related questions correctly provided were considered to have good knowledge. Those who answered fewer than 6 questions (<50%) were considered to have poor knowledge of obstetric ultrasound utilization (28).
Attitude toward obstetric ultrasound: The respondents whose responses “agree” to >50% of the questions regarding the attitude provided are categorized as having a good attitude toward obstetric ultrasound, whereas those whose responses “agree” to <50% disagree to the majority of questions are considered those with poor attitudes toward obstetric ultrasound (28, 29).
2.12 Data collections tool and procedures
The data were collected using semi structured interviewer-administered questionnaires. The questionnaire was prepared by reviewing different published literature and adapted to the objective of this study (25, 30–32), but knowledge and attitude assessment questionnaires were adopted from one study (28). The questionnaires were modified to suit the local conditions and it consisted of sections related to Socio-demographic characteristics, obstetric factors, maternal knowledge about obstetric ultrasound factors, and maternal attitudes towards obstetric ultrasound factors.
Five data collectors with BSc degrees in midwifery with two supervisors were recruited. The data collectors undertook face-to-face interviews using a semi structured and pretested Amharic questionnaire. Internal consistency/reliability of the item was checked by computing Cronbach's alpha. The value of Cronbach's alpha for knowledge assessment was 0.96 and attitude was 0.82.
2.13 Data quality control
The questionnaire was initially prepared in English. The English version was translated to the Amharic local language and translated back to English to ensure internal consistency by language experts. The quality of the data was ensured during collection, coding, entry, and analysis. Before the data were collected, one day of training and orientation were given to the data collectors and supervisors. Follow-up was also performed during the data collection. Moreover, the questionnaires were pretested on 29 participants (5% of the sample) at Woldia Hospital 15 days before the data collection to ensure the clarity, wording, and logical sequence of the questions. The necessary modifications were made. In addition, the supervisors and principal investigator supervised the whole activity of the data collection process and checked the completed questionnaires every day for completeness, and correctness, and necessary corrections were made in a timely manner.
2.14 Data processing and analysis
The data were edited and cleaned for inconsistencies by using Epidemiologic Data (Epid-data) 4.6 version software and then subjected to Statistical Package for Social Science version (SPSS) 26 (manufactured in April 2019; Armonk, Nework, United States) for data analysis. Descriptive statistics such as frequencies and cross-tabulations were performed. Graphical presentations such as pie charts were used to present the findings of the study. The information was presented in tables and figures. Bivariable and multivariable logistic regression analyses were performed to determine the associations between outcome and explanatory variables. Variables with a P-value <0.25 in the Bivariate analysis were used as the cutoff points for eligibility in the multivariate logistic regression model.
An effort was made to assess whether the necessary assumptions for the application of multivariable logistic regression were fulfilled. In this regard, the Hosmer and Lemeshow goodness-of-fit test yielded a large p value (p > 0.05) and the result was 0.589. Multicollinearity was checked to determine the linear correlation among the independent variables by using the variance inflation factor (VIF), Tolerance test and standard error. Variables with an inflation factor >10, standard error >2 and tolerance <0.1 were excluded from the multivariable analysis. The confounding effect were also checked.
Variables without collinearity were entered into a multivariable model. Only variables with a p value <0.05 were included in the final model. Finally, the AOR and, 95% CI were considered associated factors for utilizing prenatal obstetric ultrasound.
3 Results
3.1 Sociodemographic characteristics of the respondents
A total of 562 pregnant women participated in this study, for a response rate of 95.3%. The mean age of the study participants was 29.93 (SD ± 5.53) years, with a minimum of 18 years and a maximum of 45 years.
Three hundred twenty-four (56.2%) patients were living in urban areas. The majority of the respondents (70.3%) were married, and 296 (52.7%) of the respondents were housewives. The educational level of the respondents varied from illiterate to above a college diploma, with the majority (48.2%) being illiterate, as shown in Table 1.
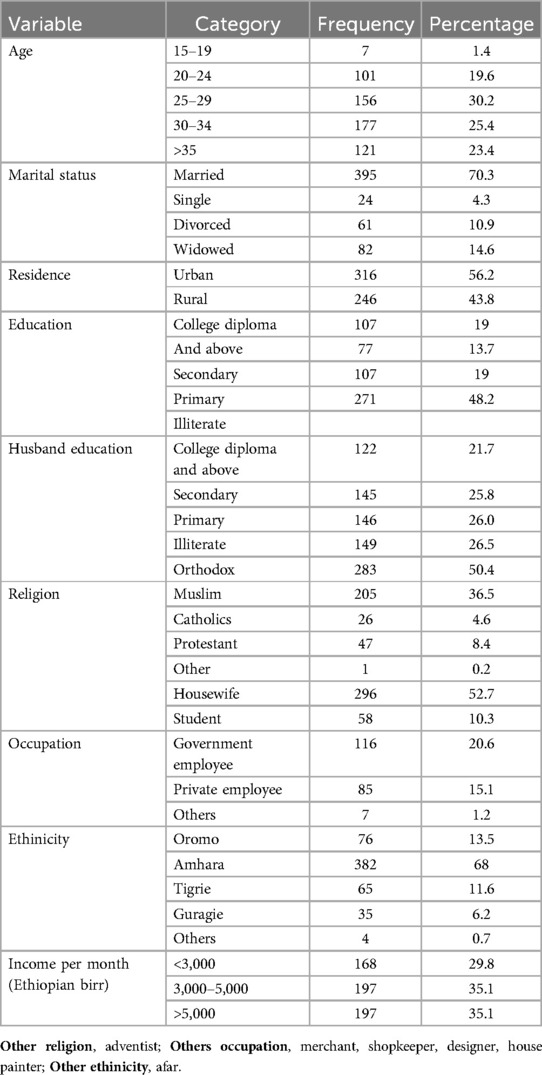
Table 1. Sociodemographic history of pregnant mothers who attended ANC in selected South Wollo Zone Public Hospitals, Ethiopia, 2023 (n = 562).
3.2 Obstetric and maternal health service characteristics of pregnant women in selected South Wollo zone hospitals in Northeast Ethiopia, 2023
Four-hundred-ninety-nine (88.8%) of the respondents were multigravida, five hundred thirty nine (95.9%) initiated antenatal visits after six months, and 379 (67.4%) had four or more antenatal visits. One hundred seventy-four (31.0%) of the respondents had a pregnancy that experienced medical illness while one hundred fifty-four (27.4%) mothers had a pregnancy ended in abortion. Ninety-eight (17.4%) of the mothers delivered congenital anomalies (Table 2).
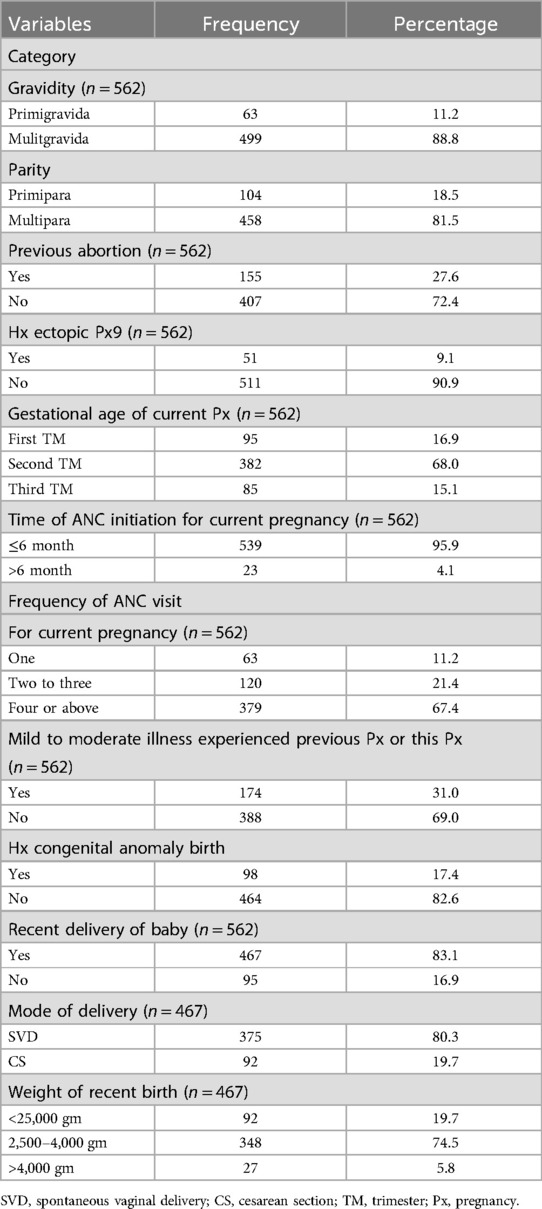
Table 2. Obstetric history of pregnant women who attended ANC in selected Southern Wollo Zone Public Hospitals, Ethiopia, 2023.
The most reported component of knowledge reported by participants was helping to estimate gestational age which was reported by approximately 412 (73.3%) mothers. Estimating fetal weight was the second most reported importance of ultrasound, with 397 (70.6%) reporting it. The least common component of knowledge regarding obstetric ultrasound was determining the cord and placental position which was reported by only 310 (55.2%) particpants (Table 3).
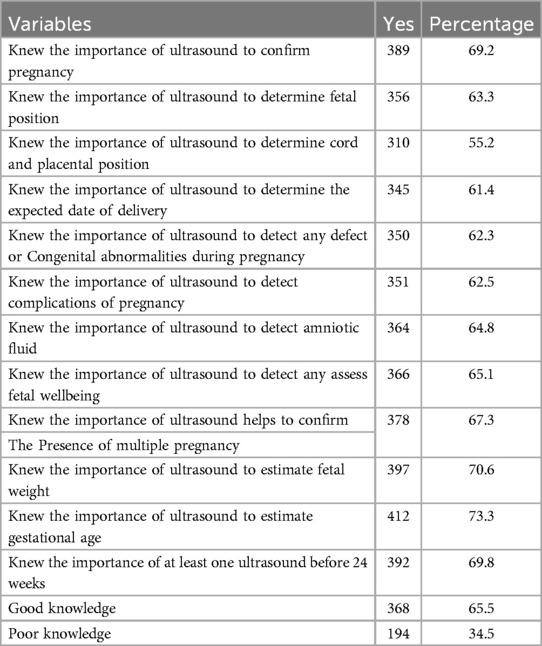
Table 3. Knowledge component on obstetric ultrasound among pregnant women who attended ANC in selected South Wollo Zone Public Hospitals, Ethiopia, 2023.
In this study, of 562 pregnant women, 368 (65.5%) had good knowledge of obstetrics ultrasound, while the remaining (194.34.5%) had poor knowledge of obstetric ultrasound. This indicates that more than half of the respondents were knowledgeable about the actual importance and effectiveness of obstetric ultrasound. The remaining women may to have a low rate of use of obstetric ultrasound or hinder women from being examined by ultrasound even in an emergency even though prenatal scanning improves pregnancy outcomes (as shown in Figure 2).
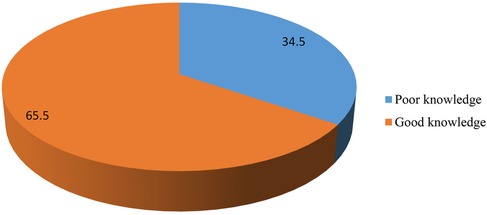
Figure 2. Knowledge of obstetric ultrasound finding among pregnant women attending ANC in selected South Wollo Zone Public Hospitals, 2023.
The most frequently mentioned component attitudes regarding obstetric ultrasound were “educating others about obstetric ultrasound is necessary”and“perceived that ultrasound is an essential investigation during pregnancy” (459; 81.7%). The second most mentioned component was “terminating a pregnancy if sex is other than you prefer,” where 437 (77.8%) respondents did not believe that terminating a pregnancy based on sex was the right decision (Table 4).
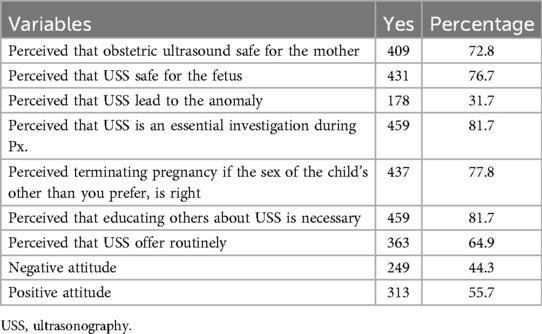
Table 4. Attitudes of pregnant women on obstetric ultrasound among pregnant women who attended ANC in selected South Wollo Zone Public Hospitals, Ethiopia, 2023.
Out of 562 pregnant women, more than half (313, 55.7%) had a positive attitude toward obstetric ultrasound, while the remaining (249, 44.3%) had a negative attitude toward obstetric ultrasound. This indicated that nearly half of the women had a negative attitude toward prenatal ultrasound scanning. A negative attitude toward prenatal ultrasound scanning indicated that she was not willing to be scanned by obstetric ultrasound, which may have had a negative impact on the outcomes of pregnancy and motherhood (Figure 3).

Figure 3. Overall attitudes among women who attended ANC in selected South Wollo Zone Public Hospitals, Ethiopia, 2023.
3.3 Prenatal ultrasound utilization
Three hundred fifty-three (62.8%) respondents used prenatal ultrasound at least once during pregnancy, of whom 221 (62.5%) utilized it before 24 weeks of gestation and the remaining 122 (34.6) utilized it after 24 weeks of gestation. Nearly half, (51.3%) of the women requested the scan by themselves whereas 145 (41.1%) of the respondents were requested by clinicians (Table 5).
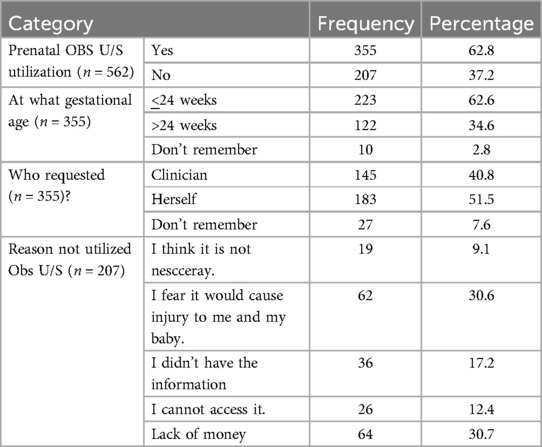
Table 5. Questions related to prenatal ultrasound utilization among pregnant women who attended ANC in the South Wollo Zone in the northeast region of Ethiopia, 2023.
3.4 Factor associated with the use of prenatal obstetric ultrasound
According to our bivariate logistic regression, fifteen variables were associated with the use of prenatal obstetric ultrasound: education status, husband's education status, residence, occupation, gravidity, parity, previous abortion, congenital anomaly delivery, the timing of ANC initiation, the frequency of ANC visits, recent delivery of baby, mode of delivery, recent birth weight delivery, knowledge of the woman and attitudes about the woman.
Respondents whose educational status was above college and diploma were nearly six times more likely to use prenatal ultrasound than did those with no formal education [crude odds ratio (COR) = 6.45; 95% CI: 3.56–11.72]. Similarly, pregnant women whose occupation was a government employee were more likely to utilize obstetric ultrasound than were those whose occupation was a housewife (COR = 7.99; 95% CI: 4.22–15.15).
However, according to our multivariate logistic regression analysis, only five variables were significantly associated with the use of obstetric ultrasound such as women's education status, women's knowledge, residence, occupation, and medical illness during pregnancy.
The odds of utilizing prenatal ultrasound among pregnant women who reside in urban areas were nearly five times greater than those who reside in rural areas, [adjusted odds ratio (AOR) = 4.82; 95% CI: 2.99–8.03]. Those respondents who encountered medical illness during pregnancy were nearly three times more likely to utilize prenatal ultrasound than were their counterparts (AOR = 3.03; 95% CI: 1.64–5.59). Similarly, women who had good knowledge of prenatal obstetric ultrasound were nearly seven times more likely to utilize prenatal ultrasound than were those who had poor knowledge (AOR = 7.32; 95% CI: 4.07–13.33) (see details in Table 6).
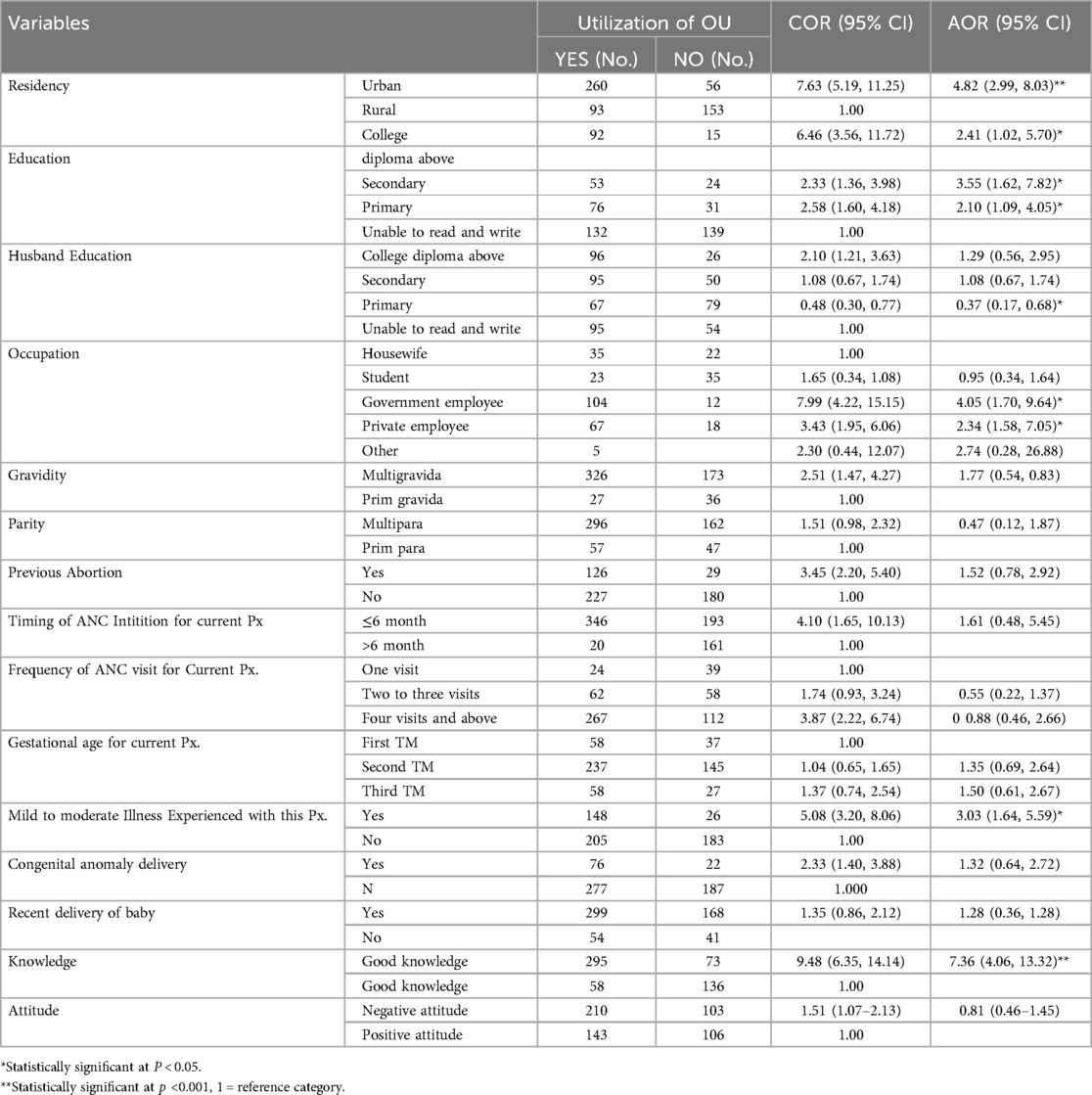
Table 6. Result of multivariate binary logistic regression analysis of factors associated with prenatal ultrasound utilization among pregnant women who attended ANC in selected South Wollo Zone Public Hospitals, Ethiopia, 2023.
4 Discussion
This study was designed to assess the proportion of pregnant women utilizing prenatal ultrasound and associated factors mong those attending ANC in five public hospitals of South Wollo Zone. The proportion of prenatal ultrasound utilization in this study was 62.8% [95% CI: (58.7%–66.8%)]. This result was in line with the findings of prenatal ultrasound utilization described in Jimma Zone public hospitals in Ethiopia, which reported a 60.7% (33). This result was also consistent with the findings recorded in southeastern Nigeria, which were58.7% (34). However, the result of the current study were lower than tthose obtained in Uganda (35) and accordance with the local government Zaria, Kaduna State, northern Nigeria where the proportion of patients utilizing ultrasound was 83.5% (36).
These finding were also lower than those of a cluster rondomized study conducted in Eastern China (96.1%) (37). This variation may be due to socioeconomic factors, the propensity to use services and geographical differences between Ethiopia and Eastern China. The next step might be to focuses on both urban and rural pregnant women as China's study included only rural pregnant women. Moreover, the discrepancy might be due to variations in access to use services, barriers to use services, health service systems, and health policy programs.
In contrast, the percentages of patients in the current study was greater than that in a study conducted in Kenya (49.7%) (38). The difference may be atributed to variations in health policy strategies for child and maternal health care between Ethiopia and Kenya.
The findings of this study showed that there was a strong association between women's knowledge of prenatal obstetric ultrasound and prenatal ultrasound utilization. Pregnant women who had good knowledge were 7.36 times more likely to utilize prenatal ultrasound than pregnant women who had poor knowledge. This result was consistent with the findings recorded in Jimma, Ethiopia (21,33), and in different countries, e.g., a peri-urban health center in Uganda (35) and the main referral hospital, in Sokoto, Nigeria (27). Pregnant women with good obstetric ultrasound knowledge have a positive attitude toward obstetric ultrasound scans. The findings of this study align with research conducted in Gedeo Zone, Ethiopia (39). This indicates that increased awareness of obstetric ultrasound enhances its utilization. This, in turn, facilitates early detection and management of obstetric complications, ultimately contributing to reduced perinatal mortality. Greater knowledge fosters confidence in ultrasound's role in predicting pregnancy outcomes, whereas misconceptions may discourage its use. Obstetric ultrasound has become a critical tool in obstetrics, and its benefits have undeniably contributed to improved pregnancy outcomes (39–41). Therefore, ensuring that all antenatal women receive obstetric ultrasound scans is essential for the prevention and management of obstetric complications, ultimately leading to improved pregnancy outcomes, as recommended by the World Health Organization (WHO). To bridge gaps in knowledge and accessibility, obstetric care providers should integrate routine ultrasound assessments into maternity services while promoting education on its benefits, particularly for rural women with limited access. Strengthening maternal health policies and integrating educational interventions into antenatal care programs could further enhance uptake of ultrasound utilization, contributing to better maternal and neonatal outcomes across the countries.
In this study, pregnant mothers who reside in urban areas were more likely to utilize obstetric ultrasound than mothers who reside in rural areas (AOR = 4.82; 95% at CI: 2.99–8.03). This is probably due to the greater accessibility of information and awareness about prenatal ultrasound in urban areas than in rural areas and the variation in the distance of health facilities. Multiple sources of information about prenatal ultrasound data are obtained through television (TV) programs, private clinics, etc., for urban women rather than for rural pregnant women. Another reason may be the limited expansion of infrastructure in the rural areas compared to urban areas. These findings are in line with, other findings conducted in dilla (29). Therefore, the South Wollo Zone Health Office, in collaboration with nongovernmental organizations (NGOs), should prioritize the expansion and enhancement of healthcare services in rural areas through a multifaceted approach. This includes the construction of well-equipped health centers, the deployment of adequately trained healthcare professionals, the implementation of telemedicine services, and the introduction of mobile health units to extend services to remote communities. Furthermore, advocating for policies that ensure the equitable distribution of healthcare resources, including the provision of prenatal ultrasound services, across rural regions is essential for closing the urban-rural healthcare gap.
Medical illness during pregnancy was the third explanatory variable that was significantly associated with the use of prenatal ultrasound. Pregnant mothers who had medical illness during pregnancy were 3.03 times more likely to utilize prenatal ultrasound than were those who were free of illness during pregnancy. Similarly, a study from Canada, showed that medical illness during pregnancy was significantly associated with the use of prenatal ultrasound (42). This might be because of the perceived fear of losing their pregnancy and the complications associated with it. The authors suggest that policymakers and guideline developer's consider incorporating more frequent ultrasound scans into the antenatal care schedule for pregnant women with medical conditions, as this strategy can help mitigate concerns about pregnancy loss and related complications. Further more women with history of pregnancy loss or anomaly detection might feel that their pregnancy loss related to poor utiliztions of ultrasound services. Another study in India showed that medical conditions such as abdominal problems and urinary tract infections (UTIs) were among the most common conditions (12, 31). A possible explanation might be that abdominal pain and urinary tract infection during pregnancy may lead to frequent antenatal visits and subsequently greater opportunities for ultrasound scans. The more patients visit a health facility with complaints during pregnancy, the more scans they obtain.
In this study, occupation was also a predictor variable that was significantly associated with the use of prenatal ultrasound. The pregnant women whose occupations were government or private were 4.06 and 3.34 times more likely to utilize obstetric ultrasound, respectively, than were those whose occupations were housewives respectively. Similarly, in China, occupation was significantly associated with the use of prenatal ultrasound (12, 37). In contrast to these findings, a study performed in Nigeria reported that occupation does not affect the utilization of prenatal ultrasound (27). This may be explained by the differences in sociodemographic background and economic status the two countries. In this study, the educational level of the women was another predictor variable associated with the utilization of prenatal ultrasound. An education level above the primary level was significantly associated with prenatal ultrasound utilization with (OR = 2.10; 95% at CI: 1.09–4.05). This study proved that mothers with a high level of education had more requests for ultrasound scans, possibly because their awareness of pregnancy complications is greater than that of mothers with low education levels. Furthermore, families with high socioeconomic status had better access to sonography and did not mind financial factors, as previous studies have also supported these findings (29, 43).
Similar findings were obtained in a study conducted in Jimma (Ethiopia), in which individuals whose educational level was above primary level were more likely to undergo obstetric ultrasound than their counterparts were (33). This may be explained by the fact that the educational status of the pregnant mother increases, and exposure to pieces of information may also increase. Discussing and disseminating of this issue may become more common among educated pregnant women than among those younger primary school. The level of education tends to influence the methods by which women obtain and analyze information about ultrasound.
5 Strengths and limitations of the study
This research addressed pregnant women in different areas, both urban and rural by considering hospitals where antenatal flow is highest in all areas. The first study area in particular is the major strength of this study. Regarding the limitations of the current study, the literature on prenatal ultrasound utilization was limited, so discussing the findings of the study was difficult. While the study was designed as an institution-based cross-sectional study, it did not include women who received antenatal care at a private clinic. Moreover, The limitation of this study is, it is impossible to make causal inferences due to the cross-sectional nature of the study.
6 Conclusions
According to the current findings, the proportion of prenatal ultrasounds utilized was 62.8%, but the prevalence prenatal ultrasounds was still much lower than that recommended by FIGO and WHO, which suggest that all pregnancies should undergo a minimum of two scans throughout pregnancy. The educational status of the pregnant woman, occupations, knowledge, urban residency, and medical illness during pregnancy were significantly associated with the use of prenatal ultrasound. Therefore, the authors recommended for health care providers to educating mothers on the purposes of obstetric ultrasound and including a prenatal ultrasound screening as part of antenatal care is needed.
7 Recommendation
In light of these findings, the following recommendations are proposed:
The authors recommended for health care providers to educating mothers on the purposes of obstetric ultrasound and including a prenatal ultrasound screening as part of antenatal care is needed.
The authors suggest that policymakers and guideline developers consider incorporating more frequent ultrasound scans into the antenatal care schedule for pregnant women with medical conditions, as this strategy can help mitigate concerns about pregnancy loss and related complications
Authors recommended strengthening maternal health policies and integrating educational interventions into antenatal care programs could further enhance uptake of ultrasound utilization, contributing to better maternal and neonatal outcomes across the countries.
The south wollo zone health office, in collaboration with NGOs, should prioritize expanding rural healthcare services and task health extension workers with educating rural women about the importance of obstetric ultrasound as part of their routine duties.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethical clearance was obtained from the Institutional Health Research Ethics Review Committee (IHRERC) of Wollo University College of Medicine and Health Sciences. An official letter was sent to South Wollo public hospitals from Southern Health Bearuea before data collection was started. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft. SY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Software, Validation, Visualization, Writing – review & editing. TE: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft. AY: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft. CM: Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
This study is part of the first author's Master of Science in Clinical Midwifery thesis with the College of Medicine and Health Sciences at Wollo University, Ethiopia. First, we would like to express our gratefulness to Woldia University for providing us with full sponsorship for our research thesis. Second, we would like to acknowledge the staff of all South Wollo Public Hospitals for their cooperation by providing all the necessary baseline information which was important for this study. Finally, we would like to extend our appreciation to Wollo University, College of Medicine, and health science librarians and internet center coordinators for their support and assistance in obtaining important materials to develop this research proposal, data collectors, supervisors, and all the participants during data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2025.1547547/full#supplementary-material
Abbreviations
ANC, antenatal care; AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; LMIC, low and middle income country; O/U, obstetric ultrasound; OR, odds ratio; U/S, ultrasound; USAID, united states agency for international development; WHO, World Health Organization.
References
2. Simó S, Zúñiga L, Izquierdo MT, Rodrigo MF. Effects of ultrasound on anxiety and psychosocial adaptation to pregnancy. Arch Women’s Ment Health. (2019) 22:511–8. doi: 10.1007/s00737-018-0918-y
3. Figo Working Group on Best Practice in Maternal-Fetal Medicine, International Federation of Gynecology and Obstetrics. Best practice in maternal-fetal medicine. Int J Gynaecol Obstet. (2015) 128(1):80–2. doi: 10.1016/j.ijgo.2014.10.011
4. World Health Organization. Intrapartum Care for a Positive Childbirth Experience. Geneva: World Health Organization (2018).
5. Harris RD, Marks WM. Compact ultrasound for improving maternal and perinatal care in low-resource settings: review of the potential benefits, implementation challenges, and public health issues. J Ultrasound Med. (2009) 28(8):1067–76. doi: 10.7863/jum.2009.28.8.1067
6. Kozuki N. Epidemiology, diagnosis, and care-seeking related to risk factors for intrapartum-related fetal and neonatal death in rural Nepal (Doctoral dissertation). Johns Hopkins University, Baltimore, MD, United States (2016).
7. Stanton K, Mwanri L. Global maternal and child health outcomes: the role of obstetric ultrasound in low resource settings. J Prev Med. (2013) 1(3):22–9. doi: 10.12691/jpm-1-3-3
8. Sippel S, Muruganandan K, Levine A, Shah S. Use of ultrasound in the developing world. Int J Emerg Med. (2011) 4:1–11. doi: 10.1186/1865-1380-4-72
9. Shah SP, Johnston V, Allotey P, Mulholland K, Markovic M. Impact of the introduction of ultrasound services in a limited resource setting: rural Rwanda 2008. BMC Int Health Hum Rights. (2009) 9:1–6. doi: 10.1186/1472-698X-9-4
10. Papp Z, Fekete T. The evolving role of ultrasound in obstetrics/gynecology practice. Int J Gynaecol Obstet. (2003) 82(3):339–46. doi: 10.1016/S0020-7292(03)00224-8
11. Salomon LJ, Alfirevic Z, Berghella V, Bilardo C, Hernandez-Andrade E, Johnsen SL, et al. Practice guidelines for performance of the routine mid-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol. (2011) 37(1):116–26. doi: 10.1002/uog.8831
12. Phutke G, Laux T, Jain P, Jain Y. Ultrasound in rural India: a failure of the best intentions. Indian J Med Ethics. (2018) 18:1–7.
13. McBride B, Kane S, O'Neil J, Nguyen LT. The best healthcare (commodity) available (for purchase): provider-induced demand for obstetric ultrasonography among ethnic minority women in rural northern Vietnam. AJOG Global Rep. (2024) 4(3):100375. doi: 10.1016/j.xagr.2024.100375
14. Shah S, Noble VE, Umulisa I, Dushimiyimana JMV, Bukhman G, Mukherjee J, et al. Development of an ultrasound training curriculum in a limited resource international setting: successes and challenges of ultrasound training in rural Rwanda. Int J Emerg Med. (2008) 1:193–6. doi: 10.1007/s12245-008-0053-z
15. Wanyonyi SZ, Mariara C, Vinayak S, Stones W. Opportunities and challenges in realizing universal access to obstetric ultrasound in sub-Saharan Africa. Ultrasound Int Open. (2017) 3(02):E52–9. doi: 10.1055/s-0043-103948
16. Abawollo HS, Tsegaye ZT, Desta BF, Beshir IA, Mengesha BT, Guteta AA, et al. Contribution of portable obstetric ultrasound service innovation in averting maternal and neonatal morbidities and mortalities at semi-urban health centers of Ethiopia: a retrospective facility-based study. BMC Pregnancy Childbirth. (2022) 22(1):368. doi: 10.1186/s12884-022-04703-1
17. World Health Organization. Health in 2015: from MDGs, millennium development goals to SDGs, sustainable development goals. (2015).
18. Dalmacion GV, Reyles RT, Habana AE, Cruz LMV, Chua MC, Ngo AT, et al. Handheld ultrasound to avert maternal and neonatal deaths in 2 regions of the Philippines: an iBuntis® intervention study. BMC Pregnancy Childbirth. (2018) 18:1–8. doi: 10.1186/s12884-018-1658-8
19. Mcclure E, Goldenberg R, Swanson D, Saleem S, Esamai F, Garces A, et al. 3: routine antenatal ultrasound in low/middle income countries: a cluster randomized trial. Am J Obstet Gynecol. (2017) 216(1):S3.
20. Abawollo HS, Argaw MD, Tsegaye ZT, Beshir IA, Guteta AA, Heyi AF, et al. Institutionalization of limited obstetric ultrasound leading to increased antenatal, skilled delivery, and postnatal service utilization in three regions of Ethiopia: a pre-post study. PLoS One. (2023) 18(2):e0281626. doi: 10.1371/journal.pone.0281626
21. Vogel JP, Habib NA, Souza JP, Gülmezoglu AM, Dowswell T, Carroli G, et al. Antenatal care packages with reduced visits and perinatal mortality: a secondary analysis of the WHO antenatal care trial. Reprod Health. (2013) 10:1–7. doi: 10.1186/1742-4755-10-19
22. Hofmeyr GJ, Hodnett ED. Antenatal care packages with reduced visits and perinatal mortality: a secondary analysis of the WHO antenatal care trial-comentary: routine antenatal visits for healthy pregnant women do make a difference. Reprod Health. (2013) 10:1–2. doi: 10.1186/1742-4755-10-20
23. Ekott MI, Edet E, Ovwigho U, Ameh S, Udo A, Akinwunmi F, et al. Acceptability of focused antenatal care by antenatal clinic attendees in Obio Cottage Hospital, Port Harcourt, Nigeria. Res J Women’s Health. (2017) 4(1):2. doi: 10.7243/2054-9865-4-1
24. Bitew ZW, Worku T, Alebel A, Alemu A. Magnitude and associated factors of neural tube defects in Ethiopia: a systematic review and meta-analysis. Glob Pediatr Health. (2020) 7:2333794X20939423. doi: 10.1177/2333794X20939423
25. Argaw MD, Abawollo HS, Tsegaye ZT, Beshir IA, Damte HD, Mengesha BT, et al. Experiences of midwives on vscan limited obstetric ultrasound use: a qualitative exploratory study. BMC Pregnancy Childbirth. (2022) 22(1):196. doi: 10.1186/s12884-022-04523-3
27. Oche OM, Umar AS, Raji MO, Kaoje AU, Godwin G, Ango JT, et al. Knowledge of the use and indications for obstetric ultrasound scan among women attending a main referral hospital, Sokoto, Nigeria. Res Obstet Gynecol. (2013) 2(5):55–62. doi: 10.5923/j.rog.20130205.01
28. Abduljabbar HS, Jabal NAB, Hussain FA, Alqabbaa RM, Marwani FA, Alghamdi SA, et al. Knowledge, attitudes and practice about obstetric ultrasonography among women attending a university hospital: a cross-sectional study. Open J Obstet Gynecol. (2020) 10(12):1763–75. doi: 10.4236/ojog.2020.10120159
29. Haile ZW, Gurmu AG. Knowledge, attitude, barriers, and associated factors of obstetric ultrasound among pregnant women in public hospitals, Ethiopia, 2022: a cross-sectional study. J Ultrasound. (2024) 27(1):31–40. doi: 10.1007/s40477-023-00783-7
30. Flores AH, Kassamali S, Won GY, Stein JC, Reynolds T. Frequency of utilisation of ultrasound in the diagnosis of ectopic pregnancy in sub-Saharan Africa countries: a systematic review. Afr J Emerg Med. (2015) 5(1):31–6. doi: 10.1016/j.afjem.2014.08.001
31. Adams SJ, Yao S, Mondal P, Lim H, Mendez I, Babyn P. Sociodemographic and geographic disparities in obstetrical ultrasound imaging utilization: a population-based study. Acad Radiol. (2022) 29(5):650–62. doi: 10.1016/j.acra.2021.07.012
32. Jarahi L, Mahmoudi R, Yazd MV, Ghodsi H, Ramezani M, Omranzadeh A. Association of sociodemographic, obstetric, and attitudinal factors with prenatal ultrasound in Mashhad, Iran. J Child Sci. (2021) 11(1):e222–6. doi: 10.1055/s-0041-1733872
33. Yetwale A, Kabeto T, Biyazin T, Fenta B. Prenatal ultrasound utilization and its associated factors among pregnant women in Jimma town public health institutions, Ethiopia. Health Serv Res Manag Epidemiol. (2022) 9:23333928221085881. doi: 10.1177/23333928221085881
34. Ikeako L, Ezegwui HU, Onwudiwe E, Enwereji JO. Attitude of expectant mothers on the use of ultrasound in pregnancy in a tertiary institution in South East of Nigeria. Ann Med Health Sci Res. (2014) 4(6):949–53.25506492
35. Gonzaga MA, Kiguli-Malwadde E, Businge F, Byanyima RK. Utilisation of obstetric sonography at a peri-urban health centre in Uganda. Pan Afr Med J. (2010) 7:24.21918711
36. Galadanci H, Künzel W, Shittu O, Zinser R, Gruhl M, Adams S. Obstetric quality assurance to reduce maternal and fetal mortality in Kano and Kaduna State hospitals in Nigeria. Int J Gynaecol Obstet. (2011) 114(1):23–8. doi: 10.1016/j.ijgo.2011.02.005
37. Huang K, Umar N, Litaker D, Schaarschmidt M-L, Peitsch WK, Schmieder A, et al. Utilization of antenatal ultrasound scan and implications for caesarean section: a cross-sectional study in rural Eastern China. BMC Health Serv Res. (2012) 12:1–10. doi: 10.1186/1472-6963-12-93
38. Matiang’i M, Joosse K, Ngunju P, Kiilu C, Harkx R, Hangelbroek M, et al. Barriers and enablers that influence utilization of ultrasound screening services among antenatal women in Kajiado and Kisii counties Kenya. Open J Clin Diagn. (2021) 11(1):1–17. doi: 10.4236/ojcd.2021.111001
39. Molla W, Mengistu N, Wudneh A. Pregnant women’s knowledge, attitude, and associated factors toward obstetric ultrasound in public hospitals, Ethiopia, 2021: multi-centered cross-sectional study. Women’s Health. (2022) 18:17455057221091357. doi: 10.1177/17455057221091357
40. Tunçalp Ö, Pena-Rosas JP, Lawrie T, Bucagu M, Oladapo OT, Portela A, Metin Gülmezoglu A. WHO recommendations on antenatal care for a positive pregnancy experience-going beyond survival. Bjog. (2017) 124(6):860–2. doi: 10.1111/1471-0528.14599
41. Shidhaye PR, Giri P, Nagaonkar S. Study of knowledge and attitude regarding prenatal diagnostic techniques act among the pregnant women at a tertiary care teaching hospital in Mumbai. J Educ Health Promot. (2012) 1(1):36. doi: 10.4103/2277-9531.102049
42. Abdullah P, Landy CK, McCague H, Macpherson A, Tamim H. Factors associated with the timing of the first prenatal ultrasound in Canada. BMC Pregnancy Childbirth. (2019) 19:1–14. doi: 10.1186/s12884-019-2309-4
Keywords: antenatal care, obstetric ultrasound, prenatal, pregnant women, utilization
Citation: Susu B, Temesgen K, Ayalew S, Yibeltal S, Emagneneh T, Yesuf A and Mulugeta C (2025) Prenatal ultrasound utilization and associated factors among pregnant women attending antenatal care in south Wollo zone public hospitals, north east, Ethiopia, 2023. Front. Digit. Health 7:1547547. doi: 10.3389/fdgth.2025.1547547
Received: 18 December 2024; Accepted: 8 April 2025;
Published: 28 April 2025.
Edited by:
Björn Wolfgang Schuller, Imperial College London, United KingdomReviewed by:
Francisco Maria Calisto, University of Lisbon, PortugalRafiat Anokwuru, University of Pretoria, South Africa
Copyright: © 2025 Susu, Temesgen, Ayalew, Yibeltal, Emagneneh, Yesuf and Mulugeta. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Belay Susu, c3VzdWJlbGF5MTlAZ21haWwuY29t
 Belay Susu
Belay Susu Kibir Temesgen
Kibir Temesgen Sindu Ayalew2
Sindu Ayalew2 Selam Yibeltal
Selam Yibeltal Tadele Emagneneh
Tadele Emagneneh Adem Yesuf
Adem Yesuf Chalie Mulugeta
Chalie Mulugeta