- 1Department of Otolaryngology–Head & Neck Surgery, University of Toronto, Toronto, ON, Canada
- 2Undergraduate Department of Psychology, University of Toronto, Toronto, ON, Canada
- 3Institute of Health Policy, Management and Evaluation, Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
- 4Division of General Surgery, Department of Surgery, University of Toronto, Toronto, ON, Canada
Background: Outpatient thyroid surgery is gaining popularity as it can reduce length of hospital stay, decrease costs of care, and increase patient satisfaction. There remains a significant variation in the use of this practice including a perceived knowledge gap with regards to the safety of outpatient thyroidectomies and how to go about implementing standardized institutional protocols to ensure safe same-day discharge. This review summarizes the information available on the subject based on existing published studies and guidelines.
Methods: This is a scoping review of the literature focused on the safety, efficacy and patient satisfaction associated with outpatient thyroidectomies. The review also summarizes and editorializes the most recent American Thyroid Association guidelines.
Results: In total, 11 studies were included in the analysis: 6 studies were retrospective analyses, 3 were retrospective reviews of prospective data, and 2 were prospective studies. The relative contraindications to outpatient thyroidectomy have been highlighted, including: complex medical conditions, anticipated difficult surgical dissection, patients on anticoagulation, lack of home support, and patient anxiety toward an outpatient procedure. Utilizing these identified features, an outpatient protocol has been proposed.
Conclusion: The salient features regarding patient safety and selection criteria and how to develop a protocol implementing ambulatory thyroidectomies have been identified and reviewed. In conclusion, outpatient thyroidectomy is safe, associated with high patient satisfaction and decreased health costs when rigorous institutional protocols are established and implemented. Successful outpatient thyroidectomies require standardized preoperative selection, clear discharge criteria and instructions, and interprofessional collaboration between the surgeon, anesthetist and same-day nursing staff.
Introduction
Background
The American Thyroid Association (ATA) has recently released an interdisciplinary consensus statement with regards to outpatient thyroidectomies. They investigated the peri-operative factors that optimize safe performance of ambulatory thyroidectomies (1). Traditionally, thyroidectomies were an inpatient procedure for close monitoring of potential post-operative complications, however, increasingly, outpatient thyroidectomy has been adopted albeit with large variations in practice (2). The primary objective of this article is to provide a scoping review and rationale for the feasibility and safety of outpatient thyroidectomies, the patient-selection factors required for safe outpatient thyroidectomy, and the implementation of hospital programs that make outpatient thyroidectomies practicable.
Thyroidectomy Complications
Thyroidectomy is a relatively low risk procedure; however, the potential post-operative complications include: symptomatic hypocalcemia due to parathyroid gland injury, airway compromise secondary to cervical hematoma, and recurrent laryngeal nerve injury (3, 4). The incidence of these complications is quite low (5–10).
Intraoperative injury to the parathyroid glands can result in post-operative hypoparathyroidism and, consequently, symptomatic hypocalcemia. A single 1-hour post-thyroidectomy parathyroid hormone level has been validated to risk stratify patients into low-risk and high-risk groups for developing post-operative symptomatic hypocalcemia (11–16). Early calcium and vitamin D supplementation for patients in the high-risk category can effectively prevent symptomatic hypocalcemia (17). Outpatient bloodwork and close follow up is preferred by patients over inpatient management (18). In the age of integrated electronic patient care, surgeons can follow serum calcium values upon discharge and adjust calcium supplementation accordingly. As such, hypocalcemia is rarely a reason to avoid outpatient thyroidectomy given (1) our ability to predict it and (2) our ability to manage it with oral supplementation and with close ambulatory follow up.
There is also the risk for paresis or paralysis of the recurrent laryngeal nerve. Hospital admission for suspected unilateral recurrent nerve injury is not required as the majority of patients tolerate recurrent laryngeal nerve injury well. These injuries are often transient. In approximately 50% patients there is full return of function within the first 6 months (19). Furthermore, if concern for recurrent laryngeal nerve injury arises intra-operatively, intra-operative nerve monitoring and a post-operative nasopharyngoscopy examination can confirm the movement of the vocal cords. Expectant management and patient education with regards to swallowing precautions can be provided accordingly if vocal cord paralysis is noted (9, 18). Bilateral vocal cord paresis is extremely rare, often predicted based on intra-operative findings and nerve monitoring.
Lastly, the most feared complication of thyroid surgery is the risk of a post-operative hematoma resulting in airway compromise; however, recent literature quotes post-thyroidectomy hematoma rates of 0.25%-1.0%. Furthermore, 40-50% of hematomas are reported to occur within 6 hours post-operatively, and less than 10% occur beyond the first 24 hours (20–23). Thus, with mandated set length-of-time for observation, rapidly-progressive arterial hematomas are unlikely to occur after a patient is discharged home. After propensity score matching was used to match patients who were discharged on postoperative day 0 and those discharged on postoperative days 1 or 2, a retrospective study analyzing 10, 502 patients who underwent thyroidectomies found that there was no difference in hematoma rates requiring intervention for patients who were discharged same-day versus those who were admitted overnight - for patients who suffered a hematoma requiring further intervention, such as drainage, operation, or tracheostomy, in both crude rates (0.8% vs 0.5%, P = .16) and adjusted odds (OR 1.81, 95% CI 0.81–4.31) for those discharged POD0 and POD1-2, respectively (24). Retrospectively-evaluated patient-factors associated with post-operative hematoma have contributed to a predictive scoring system intended to identify patients at higher risk for this complication (3, 19–21, 25–27). With the implementation of predictive risk-stratification, and established discharge protocols, these patients are flagged for hematoma evaluation prior to discharge, which mitigates the risk of airway obstruction. Ultimately, the surgeon must judge the adequacy of hemostasis at the end of the operation to decide whether same-day discharge is appropriate.
Same Day Surgery
The rationale for pursuing outpatient thyroidectomy is founded on the fact that thyroidectomies are often well-tolerated by patients (28). Potential post-operative complications can be risk-stratified prior to same-day discharge, and appropriate intervention and follow-up can be implemented accordingly. The aforementioned post-operative complications can be identified and observed prior to discharge. With regards to the risk of post-operative hematomas, more than half will occur within the initial 6-hour post-operative period – which is still within the window of same-day surgery observation as most centers observe patients for 8-12 hours prior to discharge (29, 30). This is further exemplified in the literature that demonstrates no increased incidence of complications that might have been prevented by a prolonged postoperative inpatient stay (31). High volume centers have reported good outcomes with even shorter hospital stays of less than 3 hours’ postoperative observation (8). Thus, in experienced hands, outpatient thyroidectomies are safe. Clear discharge instructions and reasons to return to the emergency department mitigate the risk of later occurring complications.
Patient Satisfaction and Cost Effectiveness
Outpatient thyroidectomies are valued by patients who prefer post-operative recovery from the comfort of their homes. Studies investigating patient satisfaction with same-day thyroidectomies boast response rates over 80% with high patient satisfaction (26). Patient preference and security in outpatient thyroidectomies were also measured by Sahmkow et al. (32) and reported average scores of 9.3/10 (10 being highest satisfaction and security). They thus concluded that the majority of patients felt safe to leave the hospital after their operation. Clear communication between healthcare providers and their patients prior to discharge was correlated with positive questionnaire responses and no reported displeasure for early discharge (10, 32–36). Given these findings, it is evident that patients have a preference towards post-operative recovery at their own comfort and convenience with clear instructions on reasons to return to the hospital to ensure their safety (10, 36–39).
Outpatient thyroidectomies have been gaining desirability on an institutional level as they are cost-effective and demonstrate conservation of scarce resources (2). In a cost analysis study conducted by Terris et al, it was found that healthcare cost for outpatients was significantly lower than inpatients on average – highlighting a cost reduction of approximately $2,500 USD per patient (10, 40, 41). Thus, in the appropriately-selected patient, outpatient thyroidectomies have been shown to not only optimize perioperative patient experiences but have also demonstrated cost savings.
Methods
A scoping review study design was employed to examine the full breadth of knowledge with regards to the safety of outpatient thyroidectomies across study designs; as well as, identify gaps in knowledge to inform future research directions and hospital protocol implementation.
A scoping review – aimed to map the research surrounding the literature on outpatient thyroidectomies - was conducted in line with the framework of Arksey and O’Malley (42). The following databases were searched from inception through the Ovid search interface: Medline (1946 – April 20, 2021), Embase (1947 – April 20, 2021), and PsycINFO (1809 – April 20, 202). The searching process followed the Cochrane Handbook (43) and the Cochrane Methodological Expectations of Cochrane Intervention Reviews (MECIR) (44) for conducting the search, the PRISMA guideline for reporting the search (45), and the PRESS guideline for peer reviewing the search strategies (46).
Inclusion criteria comprised randomized controlled trials (RCTs), and observational studies. All English language full-text articles conducted on humans were included regardless of the age of participants. The study outcomes of interest pertained to the criteria employed to determine eligibility for outpatient thyroidectomy.
Data extraction was performed using a unique form created specifically for the purposes of this review. For each included study, study design, eligibility criteria for outpatient thyroidectomy and contraindications for outpatient thyroidectomy were extracted.
Results
Search Results
In total, 11 studies were identified and used for this scoping narrative review. In terms of study design, 6 studies were retrospective analyses, 3 were retrospective reviews of prospective data, and 2 were prospective studies.
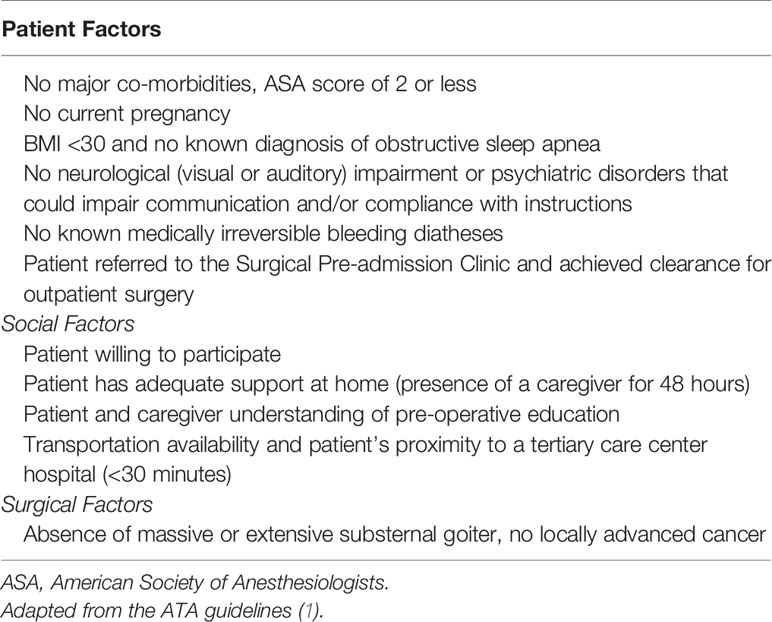
We aimed to analyze the both the patient factors and tumor characteristics that these studies used to determine their eligibility criteria for a patient’s fitness for outpatient thyroidectomy. The results of which can be found in Table 1.
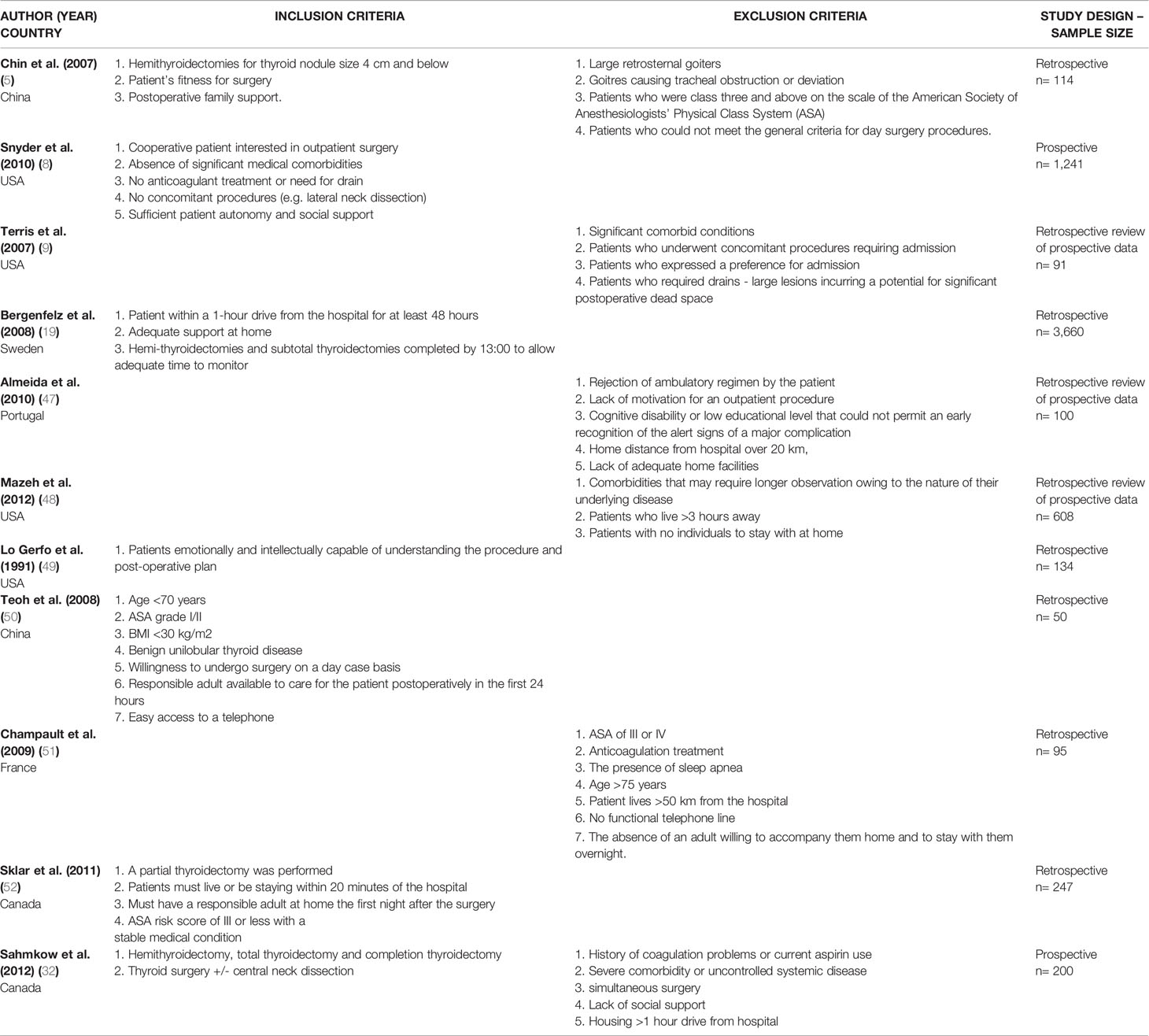
Table 1 An overview of the literature analyzing patient characteristics amenable to outpatient thyroidectomy.
Required Patient Characteristics for Outpatient Thyroidectomy
There were three main themes that emerged from the literature with regards to patient characteristics that make them suitable for outpatient thyroidectomy: fitness for surgery, hospital accessibility and social support. With regards to fitness for surgery, two of the included studies used the American Society of Anesthesiologists’ (ASA) Physical Class System to determine a cut-off. The ASA score is determined by pre-anesthetic medical co-morbidities. An ASA score of II or below indicates a patient with mild systemic disease (53). One study indicated a criterion of ASA risk score of III or less with a stable medical condition (52), while the other indicated an ASA score of I/II (50). The other three studies that indicated fitness for surgery as a criterion for outpatient thyroidectomy did not set standardized specifications; but rather, cited “absence of significant medical comorbidities” and “patient’s fitness for surgery” as criteria (5, 8, 32). The second consideration that emerged was patient accessibility. Three studies outlined defined a time cut-off for hospital accessibility (19, 32, 52), and a third required that patients have access to a telephone (50). Lastly, six studies made mention of adequate home support as a requirement for outpatient thyroidectomy (5, 8, 19, 32, 50, 52).
Patient Characteristics Contraindicated for Outpatient Thyroidectomy
Patient comorbidities were the greatest prohibitor for an outpatient thyroidectomy. Two studies noted an ASA score of III or above as a contraindication for outpatient surgery (5, 51). Other studies reported broader criteria with regards to a patient’s comorbidities precluding them from outpatient thyroidectomy (47, 48). Lastly, social support (48, 51) and distance from hospital (47, 48, 51) were again noted as important factors in stratifying patients’ eligibility for outpatient thyroidectomy. Similarly, a recent retrospective review of thyroidectomies through the American College of Surgeons National Surgical Quality Improvement Program found that patients with dyspnea (at rest or with exertion), a bleeding disorder (including active anticoagulation), or undergoing dialysis were to be excluded from outpatient procedures (54).
Tumor Characteristics Contraindicated to Outpatient Thyroidectomy
Only one study incorporated tumor characteristics in their exclusion criteria for outpatient thyroidectomy. Chin et al. excluded patients with (a) large retrosternal goiters and (b) goiters causing tracheal obstruction or deviation, from eligibility for outpatient thyroidectomy (5). Furthermore, Terris et al. excluded patients who underwent larger resections as they incurred a potential for significant postoperative dead space which required drain insertion and an admission (9).
Tumor Characteristics Amenable to Outpatient Thyroidectomy
Six of the included studies identified the final pathologic diagnosis of patients undergoing outpatient thyroidectomy (7–10, 48, 52). Furthermore, a recent meta-analysis concluded that malignant pathology was identified in 322 outpatient thyroidectomy cases (23%) (55). In contrast, one of the included study’s criterion required benign unilobular thyroid disease for outpatient thyroidectomy consideration (50); another study only included hemithyroidectomies with a set cut-off of thyroid nodule size 4 cm and below, regardless of pathology, for consideration of outpatient thyroidectomy (5). With regards to concomitant procedures, Snyder et al. and Sahmkow et al. included patients undergoing procedures such as central neck dissections and parathyroidectomies for consideration of outpatient thyroidectomy. Their studies also included patients undergoing hemithyroidectomies, subtotal thyroidectomies, total thyroidectomies and completion thyroidectomies (8, 32). Lastly, a recent retrospective review also concluded that lesser estimated intraoperative blood loss was also amenable to same-day discharge as it likely signified a less extensive operation (56).
Discussion
Post-operative discharge planning after thyroidectomy is not one size fits all. It depends on experienced clinical judgment that takes into account the underlying health of the patient, extensiveness and difficulty of the anticipated thyroidectomy, risk for postoperative bleeding, and other patient characteristics (8). The ATA released their statement on outpatient thyroidectomies – its indications, contraindications, and discharge criteria – in 2013 (1). Figure 1 outlines the contraindications to outpatient thyroidectomies as defined by the ATA (1); furthermore, their criteria set to facilitate safe discharge after same-day thyroidectomy is outlined in Figure 2. The recommendations from the ATA and the papers reviewed above can be summarized into three broad categories that need to be satisfied to facilitate safe outpatient thyroidectomy: pre-operative patient comorbidity, social support, and extent of thyroid disease and its resection (1).
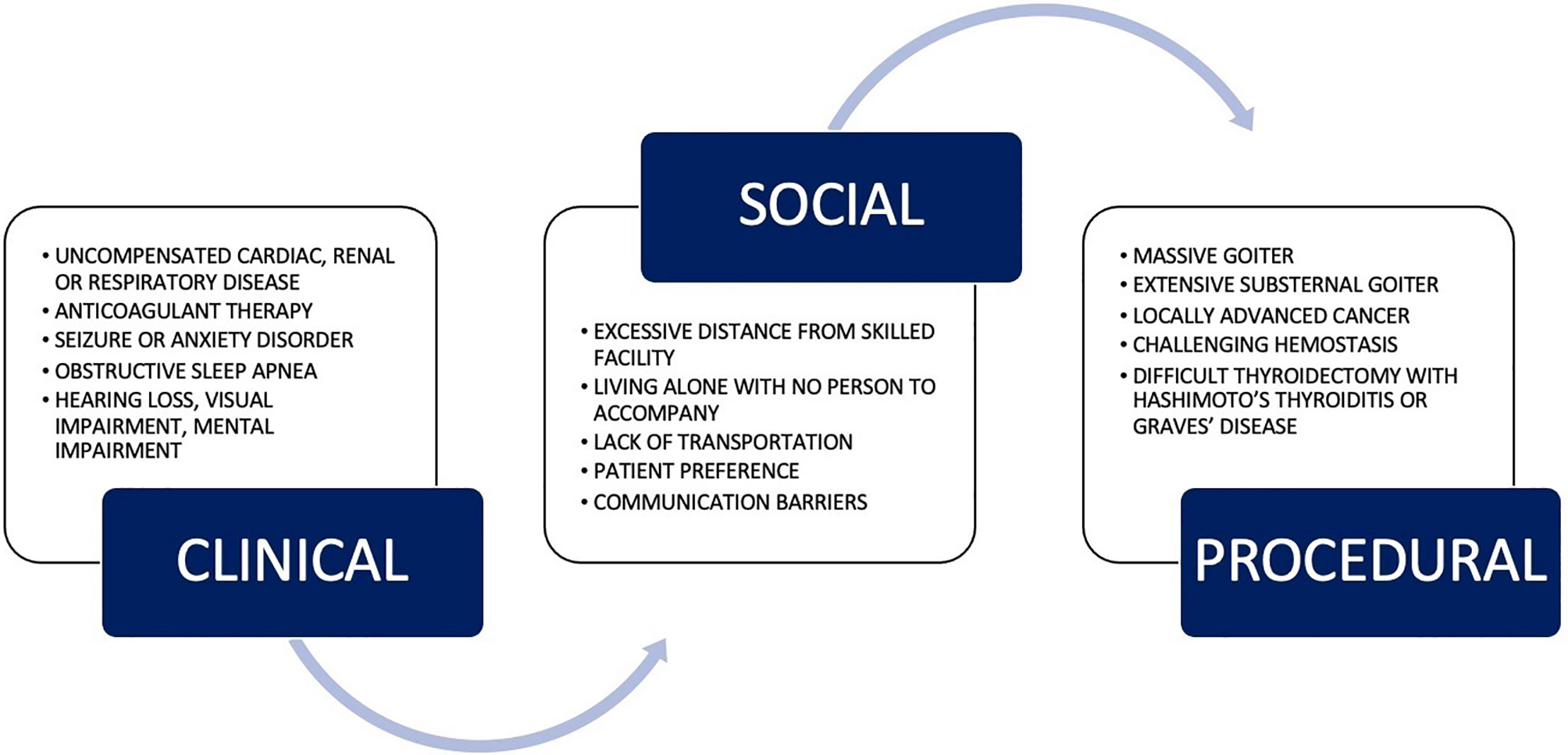
Figure 1 Relative contraindications to outpatient thyroidectomy as outlined by American Thyroid Association. Adapted from the ATA guidelines (1).
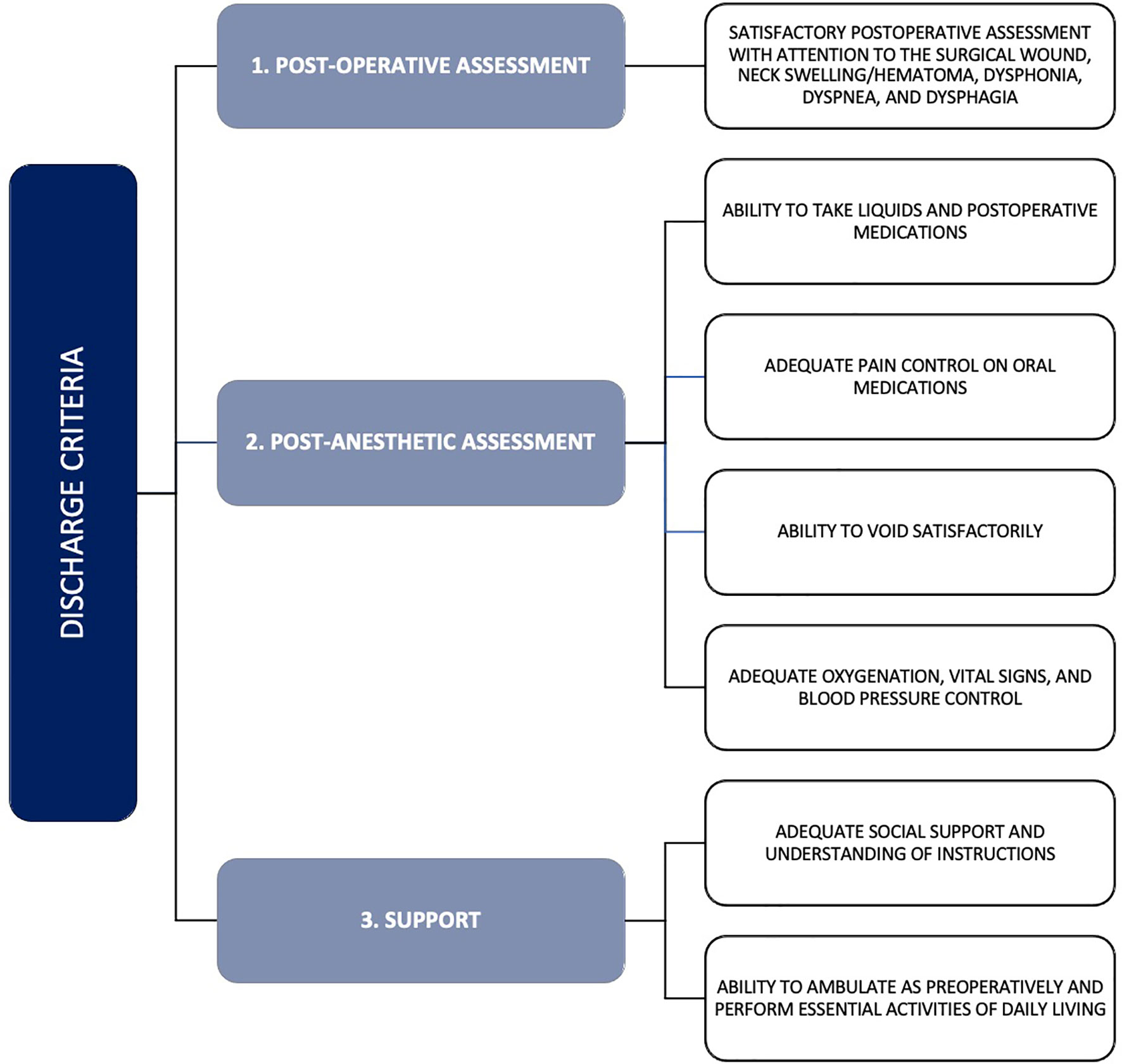
Figure 2 Discharge criteria for outpatient thyroidectomy as outlined by the American Thyroid Association. Adapted from the ATA guidelines (1).
Successful outpatient thyroidectomies require rigorous pre-operative selection, discharge criteria and instructions, and interprofessional collaboration between the surgeon, anesthetist and same-day nursing staff. Experienced clinical judgment – that takes into account the underlying comorbidities of a patient, anesthetic technique employed, difficulty of the anticipated thyroidectomy, and risk for postoperative bleeding – is necessary to identify patients suitable for outpatient thyroidectomies. We have established that careful patient selection is essential when deciding whether a patient can be managed as an outpatient. Meticulous hospital structures and organization are integral to successful outpatient thyroidectomies. As noted by Stavrakis and colleagues, increased surgeon experience with thyroidectomy leads to improved postoperative results and lower complication rates (57), this suggests that outpatient thyroidectomy should likely be performed at high volume institutions and by high volume surgeons. Engaging surgical, anesthetic, and administrative stakeholders is pivotal in implementing novel hospital program which facilitates outpatient thyroid surgery as its execution requires sufficient resources and collaboration.
As alluded to by the ATA, appropriate patient selection for ambulatory thyroidectomies requires meticulous implementation of standardized protocol in the preoperative, intraoperative, and postoperative phases of thyroidectomies.
Preoperative Patient Selection
To ensure appropriate patient selection for ambulatory thyroid surgery, patients should be required to present to a preoperative clinic visit or telehealth visit. Eligibility criteria for outpatient thyroidectomy is outlined in Table 2 (1). The eligibility criteria are to be reviewed by an anesthesiologist and a registered nurse. Of note, there was variability in the acceptable ASA score cut-off for patient consideration for outpatient thyroidectomy. Previous literature has demonstrated that there is a lack of interrater reliability in the assignment of ASA scores (58). The hypothesized contributing factors behind this is multifactorial, including: anesthetist performance evaluation, resource allocation, and financial reimbursement. As such, we have opted to take a more conservative approach and chose an ASA score of 2 or below in the proposed eligibility criteria.
Intraoperative Considerations
Intraoperative considerations involve surgical and anesthetic collaboration. From the anesthetic perspective, it is integral that efforts are made to reduce post-operative nausea and vomiting. This is facilitated by reducing the use of perioperative opioids, and the routine administration of non-sedating anti-emetics (59). Furthermore, total intravenous anesthesia is preferred over volatile agents for same-day thyroidectomies as it carries a lower incidence of post-operative nausea and vomiting (60). For analgesia, the surgeon preference is to avoid non-steroidal anti-inflammatory drugs (NSAIDs) to minimize potential bleeding risk (61). Routine administration of acetaminophen as first-line analgesia is encouraged. Interestingly, recent literature has shown that the use of NSAIDs does not increase the risk of cervical bleeding after thyroid and parathyroid surgery. This may have an impact on future post-operative analgesia choices (62). From a surgical perspective, the focus is on visualizing the recurrent laryngeal nerve and utilizing intraoperative neuromonitoring in more complex cases, local analgesia, and hemostasis. It is suggested to utilize intra-operative nerve monitoring or stimulation for recurrent laryngeal nerve integrity confirmation for more complex surgical cases – as is the case with large goiters and completion thyroidectomies (63, 64). Furthermore, intra-operative nerve monitoring can provide real-time feedback with regards to the depth of anesthetic (65); which also has important implications on post-operative nausea and vomiting (66). The routine administration of long-acting local analgesic incision infiltration and cervical block for optimal postoperative pain management is recommended, as is the use of intraoperative hemostatic agents. Cervical blocks have also been shown to be a helpful adjunct to general anesthesia and reduce postoperative use of narcotics for pain (67, 68). This is invaluable in reducing the outpatient opioid prescription burden for these patients.
Post-Operative Protocol
After surgery, patients should be observed and monitored for 4-8 hours. Same-day surgery nursing staff should be specifically alerted to monitor for potential airway, bleeding, or wound management concerns. Furthermore, parathyroid hormone (PTH) and calcium levels must be drawn for total or completion thyroid surgery in the post-anesthetic care unit to assess for potential hypocalcemia prior to discharge. Discharge eligibility is to be determined by a standardized set of discharge criteria that ensures no evidence of bleeding, swelling, dyspnea, dysphagia, or dysphonia in addition to the usual criteria. Most importantly, clear discharge instructions, and reasons to return to the emergency department, must be provided to the patient and their caregiver to mitigate the risk of later-onset complications. Furthermore, for patients who live further away, an admission may be mitigated through encouraging overnight stay at a nearby hotel (9).
The benefits of outpatient thyroidectomy are well established in the literature; however, maintaining patient safety remains the primary goal when triaging patients for fitness of ambulatory thyroidectomy (33, 34). Thus, before adopting new hospital practices we must assure ourselves that we can maintain patient safety. Our proposed protocol ensures patient safety, satisfaction and provides thorough patient education for post-operative recovery.
Conclusion
The research surrounding the safety of outpatient thyroidectomies continues to mount with ongoing refinements in selection criteria. Outpatient thyroidectomy, in experienced hands, is safe and is associated with high patient satisfaction and decreased health costs (3, 8). High-volume endocrine surgery centers should consider adopting ambulatory thyroidectomies for the appropriately-selected patient. Suitable patient selection is integral for successful outpatient thyroidectomy. A thorough review of the literature regarding the considerations for ensuring the safety of outpatient thyroidectomies has been provided while incorporating key points from the recent ATA guidelines. Lastly, a proposed protocol integrating important perioperative considerations for ambulatory thyroidectomies has been provided. The authors acknowledge the time commitment and numerous hospital considerations with regards to the implementation of new procedural protocol; however, this is an opportunity to increase safe outpatient thyroidectomies which ultimately better serves our healthcare system and our patients.
Author Contributions
JP carried out the study, analyzed the dataset, and drafted the manuscript. EB participated in the design of the study and drafted the manuscript. CN, JDP, KH, JF, and AC revised the manuscript and provided expertise feedback. AE participated in the design of the study, contributed to the conception of the study, and revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Terris DJ, Snyder S, Carneiro-Pla D, Inabnet WB 3rd, Kandil E, Orloff L, et al. American Thyroid Association Statement on Outpatient Thyroidectomy. Thyroid (2013) 23(10):1193–202. doi: 10.1089/thy.2013.0049
2. Tuggle CT, Roman S, Udelsman R, Sosa JA. Same-Day Thyroidectomy: A Review of Practice Patterns and Outcomes for 1,168 Procedures in New York State. Ann Surg Oncol (2011) 18(4):1035–40. doi: 10.1245/s10434-010-1398-0
3. Rosato L, Avenia N, Bernante P, De Palma M, Gulino G, Nasi PG, et al. Complications of Thyroid Surgery: Analysis of a Multicentric Study on 14,934 Patients Operated on in Italy Over 5 Years. World J Surg (2004) 28(3):271–6. doi: 10.1007/s00268-003-6903-1
4. Dralle H, Sekulla C, Lorenz K, Grond S, Irmscher B. Ambulatory and Brief Inpatient Thyroid Gland and Parathyroid Gland Surgery. Chirurg (2004) 75(2):131–43. doi: 10.1007/s00104-003-0775-7
5. Chin CW, Loh KS, Tan KS. Ambulatory Thyroid Surgery: An Audit of Safety and Outcomes. Singapore Med J (2007) 48(8):720–4.
6. Hall BL, Hirbe M, Yan Y, Khuri SF, Henderson WG, Hamilton BH. Thyroid and Parathyroid Operations in Veterans Affairs and Selected University Medical Centers: Results of the Patient Safety in Surgery Study. J Am Coll Surg (2007) 204(6):1222–34. doi: 10.1016/j.jamcollsurg.2007.02.073
7. Seybt MW, Terris DJ. Outpatient Thyroidectomy: Experience in Over 200 Patients. Laryngoscope (2010) 120(5):959–63. doi: 10.1002/lary.20866
8. Snyder SK, Hamid KS, Roberson CR, Rai SS, Bossen AC, Luh JH, et al. Outpatient Thyroidectomy Is Safe and Reasonable: Experience With More Than 1,000 Planned Outpatient Procedures. J Am Coll Surg (2010) 210(5):575–82, 82-4. doi: 10.1016/j.jamcollsurg.2009.12.037
9. Terris DJ, Moister B, Seybt MW, Gourin CG, Chin E. Outpatient Thyroid Surgery is Safe and Desirable. Otolaryngol Head Neck Surg (2007) 136(4):556–9. doi: 10.1016/j.otohns.2006.09.024
10. Trottier DC, Barron P, Moonje V, Tadros S. Outpatient Thyroid Surgery: Should Patients be Discharged on the Day of Their Procedures? Can J Surg (2009) 52(3):182–6.
11. Wong C, Price S, Scott-Coombes D. Hypocalcaemia and Parathyroid Hormone Assay Following Total Thyroidectomy: Predicting the Future. World J Surg (2006) 30(5):825–32. doi: 10.1007/s00268-005-0478-y
12. Islam S, Al Maqbali T, Howe D, Campbell J. Hypocalcaemia Following Total Thyroidectomy: Early Post-Operative Parathyroid Hormone Assay as a Risk Stratification and Management Tool. J Laryngol Otol (2014) 128(3):274–8. doi: 10.1017/S0022215113002600
13. Adams J, Andersen P, Everts E, Cohen J. Early Postoperative Calcium Levels as Predictors of Hypocalcemia. Laryngoscope (1998) 108(12):1829–31. doi: 10.1097/00005537-199812000-00012
14. Higgins KM, Mandell DL, Govindaraj S, Genden EM, Mechanick JI, Bergman DA, et al. The Role of Intraoperative Rapid Parathyroid Hormone Monitoring for Predicting Thyroidectomy-Related Hypocalcemia. Arch Otolaryngol Head Neck Surg (2004) 130(1):63–7. doi: 10.1001/archotol.130.1.63
15. Le TN, Kerr PD, Sutherland DE, Lambert P. Validation of 1-Hour Post-Thyroidectomy Parathyroid Hormone Level in Predicting Hypocalcemia. J Otolaryngol Head Neck Surg (2014) 43:5. doi: 10.1186/s40463-014-0042-6
16. Vescan A, Witterick I, Freeman J. Parathyroid Hormone as a Predictor of Hypocalcemia After Thyroidectomy. Laryngoscope (2005) 115(12):2105–8. doi: 10.1097/01.MLG.0000181504.69230.87
17. Moore FD Jr. Oral Calcium Supplements to Enhance Early Hospital Discharge After Bilateral Surgical Treatment of the Thyroid Gland or Exploration of the Parathyroid Glands. J Am Coll Surg (1994) 178(1):11–6.
18. Materazzi G, Dionigi G, Berti P, Rago R, Frustaci G, Docimo G, et al. One-Day Thyroid Surgery: Retrospective Analysis of Safety and Patient Satisfaction on a Consecutive Series of 1,571 Cases Over a Three-Year Period. Eur Surg Res (2007) 39(3):182–8. doi: 10.1159/000100904
19. Bergenfelz A, Jansson S, Kristoffersson A, Martensson H, Reihner E, Wallin G, et al. Complications to Thyroid Surgery: Results as Reported in a Database From a Multicenter Audit Comprising 3,660 Patients. Langenbecks Arch Surg (2008) 393(5):667–73. doi: 10.1007/s00423-008-0366-7
20. Burkey SH, van Heerden JA, Thompson GB, Grant CS, Schleck CD, Farley DR. Reexploration for Symptomatic Hematomas After Cervical Exploration. Surgery (2001) 130(6):914–20. doi: 10.1067/msy.2001.118384
21. Leyre P, Desurmont T, Lacoste L, Odasso C, Bouche G, Beaulieu A, et al. Does the Risk of Compressive Hematoma After Thyroidectomy Authorize 1-Day Surgery? Langenbecks Arch Surg (2008) 393(5):733–7. doi: 10.1007/s00423-008-0362-y
22. Lang BH, Yih PC, Lo CY. A Review of Risk Factors and Timing for Postoperative Hematoma After Thyroidectomy: Is Outpatient Thyroidectomy Really Safe? World J Surg (2012) 36(10):2497–502. doi: 10.1007/s00268-012-1682-1
23. Schwartz AE, Clark OH, Ituarte P, Lo Gerfo P. Therapeutic Controversy: Thyroid Surgery–the Choice. J Clin Endocrinol Metab (1998) 83(4):1097–105. doi: 10.1210/jcem.83.4.4740-1
24. Hu QL, Livhits MJ, Ko CY, Yeh MW. Same-Day Discharge is Not Associated With Increased Readmissions or Complications After Thyroid Operations. Surgery (2020) 167(1):117–23. doi: 10.1016/j.surg.2019.06.054
25. Godballe C, Madsen AR, Pedersen HB, Sorensen CH, Pedersen U, Frisch T, et al. Post-Thyroidectomy Hemorrhage: A National Study of Patients Treated at the Danish Departments of ENT Head and Neck Surgery. Eur Arch Otorhinolaryngol (2009) 266(12):1945–52. doi: 10.1007/s00405-009-0949-0
26. Ozbas S, Kocak S, Aydintug S, Cakmak A, Demirkiran MA, Wishart GC. Comparison of the Complications of Subtotal, Near Total and Total Thyroidectomy in the Surgical Management of Multinodular Goitre. Endocr J (2005) 52(2):199–205. doi: 10.1507/endocrj.52.199
27. Zambudio AR, Rodriguez J, Riquelme J, Soria T, Canteras M, Parrilla P. Prospective Study of Postoperative Complications After Total Thyroidectomy for Multinodular Goiters by Surgeons With Experience in Endocrine Surgery. Ann Surg (2004) 240(1):18–25. doi: 10.1097/01.sla.0000129357.58265.3c
28. Khavanin N, Mlodinow A, Kim JY, Ver Halen JP, Antony AK, Samant S. Assessing Safety and Outcomes in Outpatient Versus Inpatient Thyroidectomy Using the NSQIP: A Propensity Score Matched Analysis of 16,370 Patients. Ann Surg Oncol (2015) 22(2):429–36. doi: 10.1245/s10434-014-3785-4
29. Steckler RM. Outpatient Thyroidectomy: A Feasibility Study. Am J Surg (1986) 152(4):417–9. doi: 10.1016/0002-9610(86)90315-6
30. Bergamaschi R, Becouarn G, Ronceray J, Arnaud JP. Morbidity of Thyroid Surgery. Am J Surg (1998) 176(1):71–5. doi: 10.1016/S0002-9610(98)00099-3
31. Meltzer C, Klau M, Gurushanthaiah D, Tsai J, Meng D, Radler L, et al. Safety of Outpatient Thyroid and Parathyroid Surgery: A Propensity Score-Matched Study. Otolaryngol Head Neck Surg (2016) 154(5):789–96. doi: 10.1177/0194599816636842
32. Sahmkow SI, Audet N, Nadeau S, Camire M, Beaudoin D. Outpatient Thyroidectomy: Safety and Patients’ Satisfaction. J Otolaryngol Head Neck Surg (2012) 41(Suppl 1):S1–12.
33. Dionigi G, Rovera F, Carrafiello G, Boni L, Dionigi R. Ambulatory Thyroid Surgery: Need for Stricter Patient Selection Criteria. Int J Surg (2008) 6(Suppl 1):S19–21. doi: 10.1016/j.ijsu.2008.12.026
34. Spanknebel K, Chabot JA, DiGiorgi M, Cheung K, Curty J, Allendorf J, et al. Thyroidectomy Using Monitored Local or Conventional General Anesthesia: An Analysis of Outpatient Surgery, Outcome and Cost in 1,194 Consecutive Cases. World J Surg (2006) 30(5):813–24. doi: 10.1007/s00268-005-0384-3
35. Aldrete JA. Modifications to the Postanesthesia Score for Use in Ambulatory Surgery. J Perianesth Nurs (1998) 13(3):148–55. doi: 10.1016/S1089-9472(98)80044-0
36. Lacroix C, Potard G, Clodic C, Mornet E, Valette G, Marianowski R. Outpatient Hemithyroidectomy. Eur Ann Otorhinolaryngol Head Neck Dis (2014) 131(1):21–6. doi: 10.1016/j.anorl.2013.01.005
37. Mowschenson PM, Hodin RA. Outpatient Thyroid and Parathyroid Surgery: A Prospective Study of Feasibility, Safety, and Costs. Surgery (1995) 118(6):1051–3; discussion 3-4. doi: 10.1016/S0039-6060(05)80113-8
38. Samson PS, Reyes FR, Saludares WN, Angeles RP, Francisco RA, Tagorda ER Jr. Outpatient Thyroidectomy. Am J Surg (1997) 173(6):499–503. doi: 10.1016/S0002-9610(97)00019-6
39. Hopkins B, Steward D. Outpatient Thyroid Surgery and the Advances Making it Possible. Curr Opin Otolaryngol Head Neck Surg (2009) 17(2):95–9. doi: 10.1097/MOO.0b013e328325a512
40. Sun GH, DeMonner S, Davis MM. Epidemiological and Economic Trends in Inpatient and Outpatient Thyroidectomy in the United States, 1996-2006. Thyroid (2013) 23(6):727–33. doi: 10.1089/thy.2012.0218
41. Balentine CJ, Sippel RS. Outpatient Thyroidectomy: Is it Safe? Surg Oncol Clin N Am (2016) 25(1):61–75. doi: 10.1016/j.soc.2015.08.003
42. Arksey H OML. Scoping Studies: Towards a Methodological Framework. Int J Soc Res Method (2005) 8:19–32. doi: 10.1080/1364557032000119616
43. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [Updated March 2011]. Cochrane Collab (2011).
44. Higgins JPT, Lasserson T, Chandler J, Tovey D, Churchill R. Methodological Expectations of Cochrane Intervention Reviews. (2016) 105.
45. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. J Clin Epidemiol (2009) 62(10):1006–12. doi: 10.1016/j.jclinepi.2009.06.005
46. McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol (2016) 75:40–6. doi: 10.1016/j.jclinepi.2016.01.021
47. Almeida C, Campos M, Leal T, Alves L, Lemos P. Outpatient Hemi- Thyroidectomy: Is it Safe? Ambulatory Surg (2010) 16:17–9.
48. Mazeh H, Khan Q, Schneider DF, Schaefer S, Sippel RS, Chen H. Same-Day Thyroidectomy Program: Eligibility and Safety Evaluation. Surgery (2012) 152(6):1133–41. doi: 10.1016/j.surg.2012.08.033
49. Lo Gerfo P, Gates R, Gazetas P. Outpatient and Short-Stay Thyroid Surgery. Head Neck (1991) 13(2):97–101. doi: 10.1002/hed.2880130203
50. Teoh AY, Tang YC, Leong HT. Feasibility Study of Day Case Thyroidectomy. ANZ J Surg (2008) 78(10):864–6. doi: 10.1111/j.1445-2197.2008.04681.x
51. Champault A, Vons C, Zilberman S, Labaille T, Brosseau S, Franco D. How to Perform a Thyroidectomy in an Outpatient Setting. Langenbecks Arch Surg (2009) 394(5):897–902. doi: 10.1007/s00423-009-0527-3
52. Sklar M, Ali MJ, Solomon P. Outpatient Thyroid Surgery in a Toronto Community Hospital. J Otolaryngol Head Neck Surg (2011) 40(6):458–61.
53. Abouleish AE, Vinta SR, Shabot SM, Patel NV, Hurwitz EE, Krishnamurthy P, et al. Improving Agreement of ASA Physical Status Class Between Pre-Anesthesia Screening and Day of Surgery by Adding Institutional-Specific and ASA-Approved Examples: A Quality Improvement Project. Perioper Med (Lond) (2020) 9(1):34. doi: 10.1186/s13741-020-00162-4
54. McLaughlin EJ, Brant JA, Bur AM, Fischer JP, Chen J, Cannady SB, et al. Safety of Outpatient Thyroidectomy: Review of the American College of Surgeons National Surgical Quality Improvement Program. Laryngoscope (2018) 128(5):1249–54. doi: 10.1002/lary.26934
55. Khadra H, Mohamed S, Hauch A, Carter J, Hu T, Kandil E. Safety of Same-Day Thyroidectomy: Meta-Analysis and Systematic Review. Gland Surg (2017) 6(4):292–301. doi: 10.21037/gs.2017.01.05
56. Reinhart HA, Snyder SK, Stafford SV, Wagner VE, Graham CW, Bortz MD, et al. Same Day Discharge After Thyroidectomy Is Safe and Effective. Surgery (2018) 164(4):887–94. doi: 10.1016/j.surg.2018.06.019
57. Stavrakis AI, Ituarte PH, Ko CY, Yeh MW. Surgeon Volume as a Predictor of Outcomes in Inpatient and Outpatient Endocrine Surgery. Surgery (2007) 142(6):887–99; discussion -99. doi: 10.1016/j.surg.2007.09.003
58. Aronson WL, McAuliffe MS, Miller K. Variability in the American Society of Anesthesiologists Physical Status Classification Scale. AANA J (2003) 71(4):265–74.
59. Shaikh SI, Nagarekha D, Hegade G, Marutheesh M. Postoperative Nausea and Vomiting: A Simple Yet Complex Problem. Anesth Essays Res (2016) 10(3):388–96. doi: 10.4103/0259-1162.179310
60. Bacuzzi A, Dionigi G, Del Bosco A, Cantone G, Sansone T, Di Losa E, et al. Anaesthesia for Thyroid Surgery: Perioperative Management. Int J Surg (2008) 6 Suppl 1:S82–5. doi: 10.1016/j.ijsu.2008.12.013
61. Sheth KR, Bernthal NM, Ho HS, Bergese SD, Apfel CC, Stoicea N, et al. Perioperative Bleeding and Non-Steroidal Anti-Inflammatory Drugs: An Evidence-Based Literature Review, and Current Clinical Appraisal. Med (Baltimore) (2020) 99(31):e20042. doi: 10.1097/MD.0000000000020042
62. Basto ER, Waintrop C, Mourey FD, Landru JP, Eurin BG, Jacob LP. Intravenous Ketoprofen in Thyroid and Parathyroid Surgery. Anesth Analg (2001) 92(4):1052–7. doi: 10.1097/00000539-200104000-00047
63. Hermann M, Hellebart C, Freissmuth M. Neuromonitoring in Thyroid Surgery: Prospective Evaluation of Intraoperative Electrophysiological Responses for the Prediction of Recurrent Laryngeal Nerve Injury. Ann Surg (2004) 240(1):9–17. doi: 10.1097/01.sla.0000132260.34503.02
64. Calo PG, Pisano G, Medas F, Pittau MR, Gordini L, Demontis R, et al. Identification Alone Versus Intraoperative Neuromonitoring of the Recurrent Laryngeal Nerve During Thyroid Surgery: Experience of 2034 Consecutive Patients. J Otolaryngol Head Neck Surg (2014) 43:16. doi: 10.1186/1916-0216-43-16
65. Chang PY, Wu CW, Chen HY, Chen HC, Cheng KI, Lu IC, et al. Influence of Intravenous Anesthetics on Neuromonitoring of the Recurrent Laryngeal Nerve During Thyroid Surgery. Kaohsiung J Med Sci (2014) 30(10):499–503. doi: 10.1016/j.kjms.2014.05.009
66. Sahni N, Anand LK, Gombar K, Gombar S. Effect of Intraoperative Depth of Anesthesia on Postoperative Pain and Analgesic Requirement: A Randomized Prospective Observer Blinded Study. J Anaesthesiol Clin Pharmacol (2012) 28(2):266–7. doi: 10.4103/0970-9185.94920
67. Suh YJ, Kim YS, In JH, Joo JD, Jeon YS, Kim HK. Comparison of Analgesic Efficacy Between Bilateral Superficial and Combined (Superficial and Deep) Cervical Plexus Block Administered Before Thyroid Surgery. Eur J Anaesthesiol (2009) 26(12):1043–7. doi: 10.1097/EJA.0b013e32832d6913
Keywords: thyroidectomy, endocrine surgery, ambulatory surgery, de-escalation, same-day discharge, outpatient procedures
Citation: Philteos J, Baran E, Noel CW, Pasternak JD, Higgins KM, Freeman JL, Chiodo A and Eskander A (2021) Feasibility and Safety of Outpatient Thyroidectomy: A Narrative Scoping Review. Front. Endocrinol. 12:717427. doi: 10.3389/fendo.2021.717427
Received: 30 May 2021; Accepted: 13 July 2021;
Published: 28 July 2021.
Edited by:
Dario Giuffrida, Mediterranean Institute of Oncology (IOM), ItalyReviewed by:
Masha Livhits, UCLA David Geffen School of Medicine, United StatesSimona Censi, University of Padua, Italy
Copyright © 2021 Philteos, Baran, Noel, Pasternak, Higgins, Freeman, Chiodo and Eskander. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antoine Eskander, Antoine.eskander@mail.utoronto.ca
 Justine Philteos
Justine Philteos Elif Baran2
Elif Baran2 Jesse D. Pasternak
Jesse D. Pasternak