- 1National Center for PTSD, Behavioral Science Division, Boston, MA, United States
- 2Department of Psychiatry, Chobanian & Avedisian School of Medicine, Boston University, Boston, MA, United States
- 3Department of Psychiatry, Weill Cornell Medicine, New York, NY, United States
- 4Eunice Kennedy Shriver Center, University of Massachusetts Chan Medical School, Worcester, MA, United States
- 5Departments of Psychiatry, Pediatrics, and Obstetrics & Gynecology, University of Massachusetts Chan Medical School, Worcester, MA, United States
Editorial on the Research Topic
Bridging the knowledge gap: mental health, substance use disorders, and mortality in women
Mental health conditions and substance use disorders (SUDs) among women represent one of the most pressing global health challenges of our time. Women are nearly twice as likely as men to experience major depression (1) and have significantly higher lifetime risk of anxiety disorders (2, 3). Trauma-related disorders, including PTSD, also disproportionately affect women, often in the context of sex-based violence and adverse social determinants (2). Women with SUD face unique biological vulnerabilities and social barriers, developing complications more rapidly than men and experiencing stigma, caregiving burdens, and treatment access inequities (4–6). Despite this elevated burden, research and interventions have too often neglected women's specific biological, social, and cultural contexts. Historically, women—particularly those who are pregnant, postpartum, or from marginalized groups—have been excluded from clinical research, leaving critical gaps in understanding mechanisms, risk factors, and effective interventions (7, 8).
This research topic brings together a diverse set of contributions addressing these knowledge gaps. These articles advance our understanding of how women's mental health and SUDs intersect with morbidity and mortality, while highlighting innovative solutions ranging from community-driven interventions to health systems integration and big-data approaches.
Expanding conceptual frameworks for women's mental health
Friedhoff and colleagues underscore the importance of integrating the concept of matrescence—the developmental transition into motherhood—into perinatal psychiatry (Friedhoff et al.). They highlight how maternal mental health cannot be reduced to pathology alone; instead, it should be understood as a holistic transformation encompassing biological, social, cultural, and existential domains. This perspective challenges existing nosology, which often stigmatizes perinatal women while failing to capture their lived experiences. Their call echoes a broader theme of this issue: the need to center women's voices in shaping mental healthcare systems.
Skommer and Gunesh extend this agenda by examining the intersection of autism spectrum disorder (ASD), menstruation, and mental health (Skommer and Gunesh). Their scoping review reveals how women and gender-diverse individuals with ASD face unique vulnerabilities at reproductive transitions such as menarche and menopause—periods often overlooked in both ASD and women's health research. By framing menstruation within a biopsychosocial model, they highlight structural neglect and call for inclusive, sex-sensitive approaches that link neurodevelopmental and reproductive health.
Biological, social, and structural determinants of risk
A core focus of this issue is understanding how structural inequities amplify women's risk for poor health outcomes. Martinez-Gonzalez and Santiago document the stark disparities in access to evidence-based treatment for opioid use disorder (OUD) among Hispanic pregnant individuals (Martinez-Gonzalez and Santiago). Despite the safety and efficacy of medications for OUD, systemic inequities in prescribing practices and retention place this population at elevated risk for overdose, maternal mortality, and adverse neonatal outcomes. Their perspective highlights the urgency of culturally tailored interventions that dismantle stigma, expand harm reduction, and integrate perinatal addiction care into mainstream health systems.
Yang and colleagues add further nuance by identifying psychosocial and biological contributors to mental health comorbidities in women with polycystic ovary syndrome (PCOS; Yang et al.). In a large clinical sample, they report alarmingly high rates of depression (47.7%) and anxiety (39.9%) in women with PCOS. The authors propose that these high rates may in part be driven by sleep disruptions and daytime dysfunction. These findings highlight a potential bidirectional pathway between reproductive endocrinology and mental health, emphasizing the need for comprehensive screening and integrated treatment strategies. Figure 1 illustrates a conceptual framework mapping how biological, social, and healthcare determinants (“Inputs”) shape women's mental health and substance use conditions (“Conditions”), and how interventions (“Outputs”) translate into improved health and equity (“End goals”).
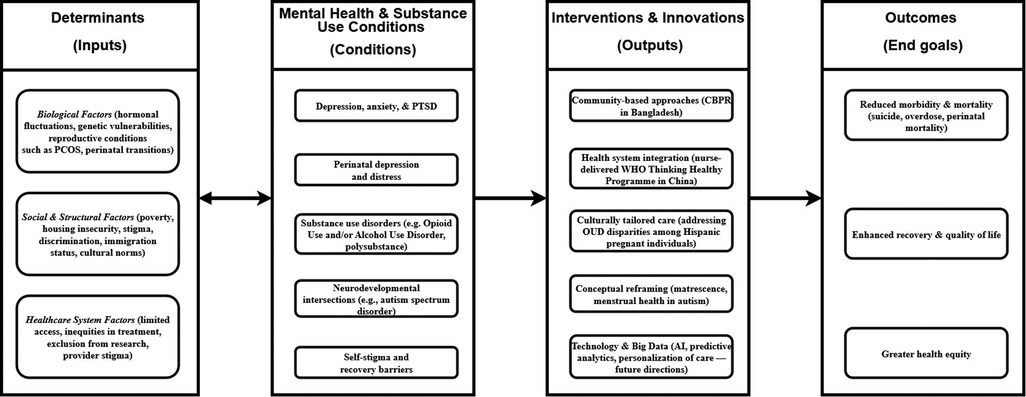
Figure 1. Conceptual framework linking determinants, mental health/SUD conditions, interventions, and outcomes for women. Inputs (biological, social, and healthcare system determinants) contribute to the development and exacerbation of conditions (i.e., mental health and substance use). Outputs (interventions such as community-based care, health system integration, and conceptual reframing) lead to improved end goals: reduced morbidity and mortality, enhanced recovery, and greater health equity.
Innovation in interventions
Two contributions demonstrate how innovative delivery models can expand access to effective interventions. Nisar and colleagues piloted integration of the World Health Organization's Thinking Healthy Programme [a cognitive-behavioral therapy (CBT)–based intervention for perinatal depression] into routine antenatal care in China (Nisaret al.). Delivered by nurses within hospital-based pregnancy schools, authors found that the intervention was feasible, acceptable, and associated with reductions in depressive and anxiety symptoms. Their work exemplifies task-shifting and health system integration as scalable approaches to closing the massive treatment gap for perinatal depression globally.
Complementing this, Afreen and colleagues showcase the promise of community-based participatory research (CBPR) in rural Bangladesh (Afreen et al.). By engaging women, community health workers, and local technology hubs, they developed strategies to improve mental health literacy and challenge stigmatization. Their model not only empowers women to advocate for their health but also leverages local infrastructure for sustainable solutions—illustrating the power of bottom-up approaches in resource-limited settings.
Stigma, recovery, and sex differences
Finally, Leon-Morales and colleagues work on “self-stigma”, sex, and personal recovery in psychotic spectrum disorders extends our understanding of how sex mediates recovery pathways. The authors report that, for women, greater “self-stigma” is associated with diminished hope, confidence, and symptom control, whereas in men, alienation paradoxically correlated with higher orientation toward success. These sex-differentiated findings underscore the need for recovery-oriented interventions that are sensitive to sex-based experiences of stigma.
Toward a future of sex-sensitive, inclusive, and data-driven care
Across these diverse contributions, several unifying themes emerge: (a) Centering Women's Lived Experience: Whether through matrescence, menstrual health, or stigma in psychosis, these studies call for theoretical and clinical frameworks that reflect women's lived experiences and realities rather than pathologize them; (b) Addressing Inequities: From rural Bangladesh to Hispanic perinatal populations in the U.S., disparities in access to care remain profound, requiring structural reforms and culturally responsive models; (c) Integrating Biological and Psychosocial Determinants: Research on PCOS and perinatal depression demonstrates how reproductive biology, sleep, and social context interact to shape morbidity and mortality risks; (d) Scaling Effective Interventions: Nurse-delivered CBT and CBPR-based literacy initiatives illustrate feasible, sustainable models for addressing the treatment gap in both high- and low-resource settings; (e) Harnessing Innovation: Future directions must leverage big data, machine learning, and interdisciplinary collaboration to personalize interventions and identify modifiable risk factors at scale.
Together, the contributions in this issue expand the frontiers of women's mental health research and care. They chart a path toward a future where interventions are not only evidence-based but also sex-sensitive, culturally grounded, and equitably delivered. Addressing women's mental health and substance use is not peripheral to global health—it is central to reducing morbidity and mortality and to advancing health equity worldwide.
Author contributions
AM: Visualization, Writing – review & editing, Writing – original draft. LS: Writing – original draft, Writing – review & editing. SK: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. (2017) 4(2):146–58. doi: 10.1016/S2215-0366(16)30263-2
2. McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. (2011) 45(8):1027–35. doi: 10.1016/j.jpsychires.2011.03.006
3. Altemus M, Sarvaiya N, Epperson CN. Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol. (2014) 35(3):320–30. doi: 10.1016/j.yfrne.2014.05.004
4. Tuchman E. Women and addiction: the importance of gender issues in substance abuse research. J Addict Dis. (2010) 29(2):127–38. doi: 10.1080/10550881003684582
5. Mandavia AD, Banducci AN, Simpson TL, Marx BP, Hawn SE, Hyde J, et al. Sex differences in suicide, lethal means, and years of potential life lost among veterans with substance use disorder. Women’s Health Issues. (2025) 35(3):196–204. doi: 10.1016/j.whi.2025.02.002
6. SAMHSA. Treatment Improvement Protocol (TIP) 51: Addressing the Specific Needs of Women for Treatment of Substance use Disorders. Rockville, MD: Substance Abuse and Mental Health Services Administration (2020). https://library.samhsa.gov/sites/default/files/pep20-06-04-002.pdf (Accessed September 09, 2025).
7. Shankar M, Gülmezoglu AM, Vogel JP, Goudar SS, McDougall A, Somannavar MS, et al. Eliminating gender bias in biomedical research requires fair inclusion of pregnant women and gender diverse people. Commun Med. (2024) 4(1):211. doi: 10.1038/s43856-024-00629-1
Keywords: womens health, social detereminants, mortality, substance use disorder, mental illness & social determinants
Citation: Mandavia AD, Susser LC and Kim S (2025) Editorial: Bridging the knowledge gap: mental health, substance use disorders, and mortality in women. Front. Glob. Women's Health 6:1721670. doi: 10.3389/fgwh.2025.1721670
Received: 9 October 2025; Accepted: 27 October 2025;
Published: 21 November 2025.
Edited and Reviewed by: Jayashri Kulkarni, Monash University, Australia
Copyright: © 2025 Mandavia, Susser and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amar D. Mandavia, YW1hci5tYW5kYXZpYUB2YS5nb3Y=
 Amar D. Mandavia
Amar D. Mandavia Leah C. Susser
Leah C. Susser Sohye Kim
Sohye Kim