- Centre for Neglected Tropical Diseases, Department of Tropical Disease Biology, Liverpool School of Tropical Medicine, Liverpool, United Kingdom
Introduction
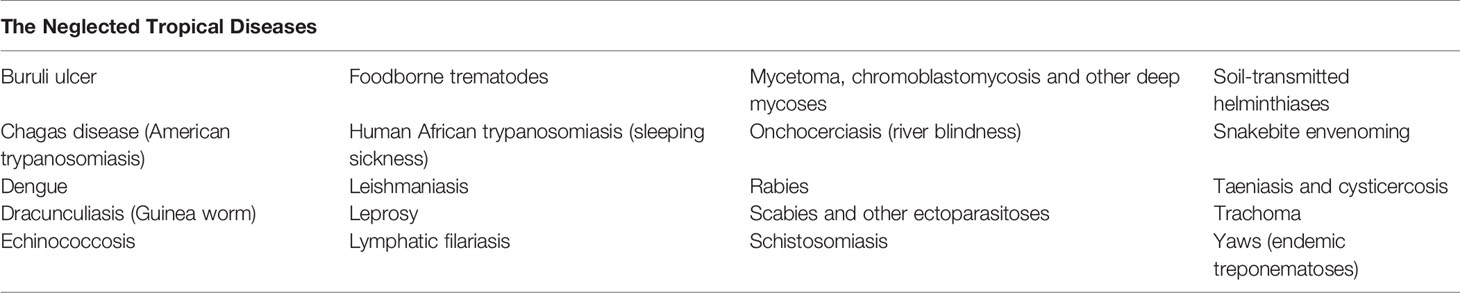
Neglected tropical diseases (NTDs) are a diverse group of 20 communicable diseases that prevail in 149 tropical and subtropical countries (1) (Table 1). They are identified as “neglected” because they persist predominantly in the poorest and the most marginalized populations living without adequate sanitation and in close contact with infectious vectors and domestic animals and livestock. NTDs are also neglected in terms of investment in R&D to the extent provided to HIV, malaria and TB. Over one billion people from the world’s most disadvantaged and poorest communities suffer from at least one NTD, which can significantly impact upon their physical and mental health. NTDs are markers, agents and drivers of poverty (2).
A New NTD Road Map
The launch of Frontiers in Tropical Diseases coincides with the official launch in January 2021 of a new road map for Neglected Tropical Diseases (NTDs) for 2021−2030 - Ending the neglect to attain the Sustainable Development Goals: a road map for neglected tropical diseases 2021–2030 (3). The new roadmap replaces the previous roadmap launched in 2012, which in spite of the substantial progress made across several NTDs, suffered from being over ambitious with many targets unfulfilled by 2020. Thankfully the new roadmap is greatly improved with more detail and finesse generated by broader engagement and consultation with NTD stakeholders, national programme managers and academia. It reflects and is framed by the growing commitment to achieving sustainable development goals (SDGs) and universal health coverage. It acknowledges how fragile and vulnerable programmes are to political instability, conflict, migration, climate change, epidemics/pandemics and anti-microbial resistance as barriers to achieving the goals laid out in the roadmap.
The new road map seeks to promote a paradigm shift in the way NTDs are addressed by; 1) moving away from process driven targets to measures of the impact on public health, 2) replacing vertical and siloed disease specific programmes with holistic cross-cutting approaches integrated into national health systems with a people and community centred focus, and 3) to transfer programme ownership away from partner support and reliance on donor funding to country ownership with NTDs integrated into national health plans and budgets.
The overarching goals for 2021-2030 decade are:
● To reduce by 90% the number of people requiring treatment for NTDs
● To eliminate at least one NTD in 100 countries
● To eradicate two diseases (dracunculiasis and yaws)
● To reduce by 75% the disability-adjusted life years (DALYs) related to NTDs
Most importantly, from the perspective of a new academic journal the new roadmap fully embraces the need for “research and innovation as fundamental enablers for programmatic progress for all NTDs”. It includes summaries of the gaps in the tools and processes required for each of the 20 diseases with a “traffic light” coded table, which includes a realistic representation of amber and red requirements highlighting the broad range of research and innovation needed to achieve these goals.
NTD Research and Innovation
There are many new examples of where innovative scientific approaches are providing new and more effective tools and understanding to improve and strengthen existing strategies. After being previously excluded from many programmatic approaches, vector control tools are re-emerging to add novel approaches to NTD control. Examples include the introduction of Wolbachia infected Aedes aegypti, which render the mosquitos refractory to arboviral transmission leading to a 77% reduction in dengue incidence in community trials in Indonesia carried out under the umbrella of the “World Mosquito Programme” (4). Another example is the deployment of vector control as an adjunct strategy to case detection and treatment for the control of Gambian human African trypanosomiasis thanks to the development of “Tiny Targets” - cost-effective traps for the tsetse fly vector (5).
Another remarkable success story is the Guinea Worm Eradication Programme. Even without any drug, vaccine or diagnostic, highly effective public health measures including access to safe drinking water, education, surveillance and copepod control has led to the incidence of human Dracunculus medinensis declining from 3.6 million cases in the 1980’s to 53 cases in 2019 (6). One of only two NTDs targeted for eradication, the programme has encountered an entirely unexpected challenge in the “last mile”. The parasite so frustratingly close to being eradicated from humans appears to have expanded into zoonotic animal reservoirs including, dogs, cats and baboons, with genomic analysis supporting a common origin of animal and human parasite populations (7). This together with the extreme challenges of surveillance in countries blighted by civil unrest and insecurity and the strict criteria for eradication demanded by the International Commission for the Certification of Dracunculus Eradication, questions whether Guinea worm eradication is still achievable and further re-enforces the need for research and innovation right up until the end.
The expansion of the guinea worm life-cycle to include zoonotic hosts re-enforces the concept of multi-sectorial engagement to bring the relevant expertise in to meet the challenges that NTD diseases face. Schistosomiasis is another example where hybridisation between human and cattle parasites has radically changed the traditional view of the parasites epidemiology, with a fundamental impact on the effectiveness of current strategies used to control urogenital schistosomiasis (8). Hybridization within and between species can accelerate parasite evolution, expand host-range, increase transmission and virulence potential and alter responsiveness to drug treatment (9) – all of which could impact on the NTD roadmap targets for existing control and elimination strategies.
Leave No One Behind
NTDs are stigmatized, can be disabling and often inhibit individuals from being or feeling able to care for themselves or their families - all of which promote poverty on a global scale (10). Individuals living in remote areas with limited access to effective health care are most vulnerable to NTDs and their consequences, such as malnutrition, anaemia, serious or permanent morbidity and associated disability, illness and death. New research approaches applied to NTDs have uncovered the significant mental health impact these diseases can inflict. The use of narrative and intersectional analysis by Dr. Laura Dean (11) and her team illustrates the terrible consequences of onchocerciasis on people that, for one reason or another, have been excluded from the control programme, leading to ostracization and suicidal thoughts due to their blindness and being a burden on their carers (See Box 1, 11). These people have been “left behind” to face the traumatic and devastating impact of these diseases alone. This work has emphasised how important it is for NTD programmes to address the psychosocial distress and mental health conditions (such as depression or anxiety) that these people and their families face, which should now be embedded in the strategies of NTD programme implementors (12).
Box 1. Jon and Hannah’s story of suffering from onchocerciasis1.
Jon’s story (abridged):
Jon is a 46 years old school-teacher from Liberia. He established a school in his community during Liberia’s conflict to educate children in his community in the absence of government schools at the time. Jon kept a diary of his experience of suffering from onchocerciasis on his wall in chalk.
● In 1985 he first experienced severe itching and was treated with Banocide (diethylcarbamazine) at the local hospital
● In 1990, the itching returned, but during the conflict accessing medicine was difficult
● In 2005 Jon sought help for his illness - his first trip to the hospital failed to provide any help
● He next accessed traditional medicine to manage the itching
● In 2012 he visited a larger hospital and was mis-diagnosed with glaucoma and cataract and given medication to reduce his blood pressure. The itching continued.
● When the Mectizan donation programme visited his community he was wrongly charged for the medicine
● By now his vision was becoming impaired and he found it difficult to read his diary on the wall
● “I feel hurt when I open it (his eyes). I can see no writing. Hmm I can see no writing”
● Since this last entry to his diary on the wall Jon’s wife left and took his children to another community
● He can no longer fix his leaking roof and often sleeps on wet ground and faces difficulty finding food
● “I just sit down the whole day. You alone and you know what it means”
Jon described his last chalk marking and going blind as the end of his journey as he now felt isolated and alone. Jon no longer teaches in the school, which he acknowledges affects him and the community. As we move toward onchocerciasis elimination in many contexts, it is vital that people like Jon are not left behind and that this isn’t the end of their story.
Hannah’s story (abridged):
In 1989, Hannah was successful at school and had ambitions to be a doctor. In 1991, as a teenager, she experienced severe itching and her eyes watered in direct light.
● Due to the ongoing conflict in Liberia her mother sought health care in Guinea and the Ivory Coast (Cote d’Ivoire) from traditional medicine.
● Returning to Liberia health care from the hospital was too expensive
● In 1994, Hannah woke to find she could no longer see her parents
● “I can’t see, I can’t see, [I] was looking all around for things from beside [me], [I] was looking for something to just finish [my] life.”
● Since 1994 Hannah described how “men will come and tell me they will help me, but after a period of time, they leave”
● Hannah gave birth to four children but had to send them to her sister as she and her mother struggle for food
● Hannah’s mother has become her primary carer, which led Hannah to feel a liability to her mother “who will take care of me when my mother dies”
● Hannah struggles to access sanitation and clean water due to her blindness
● Hannah’s mother had to give up farm work and her job as a traditional mid-wife to care for her daughter
● Her mother was unable to go to church “[I] can’t go there [to church] to leave her… [I] can’t go nowhere to leave her...for that reason she just decided to be glue to her.”
● When asked why, she explained “because Hannah always saying she will kill herself. So, [I am] afraid maybe if [I] go out, she may come and take something to harm herself. So, for that reason [I] don’t want to go far from her.”
● Hannah and her mother struggle for food and rely on donations from people in their community
Hannah’s story highlights the impact that disability caused by onchocerciasis can have on an individual, but also on other members of the household. The impact on Hannah, her mother and children, presents a need for holistic support interventions for people who are living with the clinical manifestations of onchocerciasis, such as skin disease and blindness, to ensure their psychological, social and physical support needs are met. It is only if these things are provided that we will ensure that no-one is left behind in managing the impacts of onchocerciasis.
Neglected Needs
Some areas of research that are embedded in all other infectious disease fields have traditionally been neglected by the NTD community. One example being the development of resistance to NTD drugs, which many programmes are exclusively reliant upon. In contrast to insecticides, malaria, HIV, TB, anti-microbial resistance and veterinary anti-parasitic drugs, where resistance management is integrated into their respective treatment strategies - resistance to NTD drugs is rarely acknowledged as a risk. There is currently no systematic screening or monitoring and evaluation for resistance development in NTD programmes. This is all the more remarkable considering many of the mass-drug administration approaches, several of which rely on a single drug, are likely to promote resistance. The NTD community needs to embrace the concept urgently and accept that any organism placed under selective pressure will evolve. Thankfully a number of academic consortia, such as the Consortium for Anthelminthic Resistance and Susceptibility (13) and Starworms (Stop Anthelmintic Resistant Worms) (14) are turning their attention to this neglected need, which will hopefully lead to resistance management being incorporated into programme strategies, to protect the legacy of existing NTD drugs and promote the translation of new drugs, where needed.
Another neglected need is in NTD diagnostics, a critical gap identified by the new roadmap (3). Diagnostics have received poor investment and prioritisation within NTD programmatic planning, which compromise the ability to monitor and evaluate programme progress, validation of programmatic endpoints, resistance management, surveillance and impact on health. Of the four priorities areas identified in the roadmap (diagnostics, monitoring and evaluation, access and logistics, advocacy and funding), diagnostics is the area in most need of research and innovation with 18 (out of 20) NTDs listing diagnostics as requiring critical action to meet the 2030 targets (3). In an attempt to address this neglected need WHO have established a Diagnostic Technical Advisory Group (DTAG) (15). In the face of limited resources one of the first tasks was to prioritize the NTDs most in need of diagnostic development, which brought the list down to 14 from the 18 listed in the roadmap (15). The establishment of the DTAG is a welcome first step to raise the profile and coordinate the NTD communities approaches and activities to overcome the challenges of NTD diagnostic development. However, without concerted lobbying and advocacy to turn around the lack of investment and funding to discover, develop and translate new diagnostic tools these challenges will continue to threaten the ability to meet the 2030 targets across the majority of NTDs.
Translation of Research and Innovation
Translating the outputs of NTD research discovery and development remains a barrier to the timely testing and implementation of new products and approaches. A disproportionately low level of investment in funding for translational research and access to the regulatory expertise for product development further impact on translational research progress. Product Development Partnerships have been established with a focus on NTDs including DNDi2, FIND3 and funders with dedicated NTD investment portfolios including the Bill & Melinda Gates Foundation4 and G-HIT5 among others. DNDi and FIND have been successful in meeting their targets, with new treatments for human African trypanosomiasis (HAT), visceral leishmaniasis and Chagas disease and new diagnostics for HAT and other kinetoplastids (16). Much of the early success came from “low-hanging fruit” from re-purposed drugs and combinations (17), but the current capacity of product portfolios, pipelines, timeframes and a restricted focus on selected NTDs2–5, falls well short of the gap needs analysis included in the NTD road map. Increased capacity and a broader diversity will be required to meet the translational requirements for the roadmap targets to be achieved.
Conclusion
This Speciality Grand Challenge is a personal perspective of a few of the key challenges faced by the NTD community and some examples of how the academic NTD community have responded with innovation and research to address these challenges. There are plenty of other challenges, many of which are highlighted in the needs gap analysis in the new NTD roadmap - and others will arise as we travel toward these targets and goals. The aim of the NTD section of Frontiers in Tropical Diseases is to provide an academic forum for the critical evaluation and promotion of research and innovation as fundamental enablers for programmatic progress for all Neglected Tropical Diseases.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
- ^ Written informed consent was obtained from the participants and the names used are pseudonyms (11).
- ^ https://dndi.org/research-development/portfolio/
- ^ https://www.finddx.org/ntd/
- ^ https://www.gatesfoundation.org/what-we-do/global-health/neglected-tropical-diseases
- ^ https://www.ghitfund.org/investment/portfolio/
References
1. World Health Organisation. Control of Neglected Tropical Diseases (2021). Available at: https://www.who.int/teams/control-of-neglected-tropical-diseases (Accessed February 12, 2021).
2. Molyneux DH, Asamoa-Bah A, Fenwick A, Savioli L, Hotez P. The history of the neglected tropical disease movement. Trans R Soc Trop Med Hyg (2021) 115(2):169–75. doi: 10.1093/trstmh/trab015
3. World Health Organisation. Ending the neglect to attain the Sustainable Development Goals – A road map for neglected tropical diseases 2021–2030 (2021). Available at: https://www.who.int/neglected_diseases/WHONTD-roadmap-2030/en/ (Accessed February 12, 2021).
4. Indriani C, Tantowijoyo W, Rancès E, Andari B, Prabowo E, Yusdi D, et al. Reduced dengue incidence following deployments of Wolbachia-infected Aedes aegypti in Yogyakarta, Indonesia: a quasi-experimental trial using controlled interrupted time series analysis. Gates Open Res (2020) 4:50. doi: 10.12688/gatesopenres.13122.1
5. Tirados I, Esterhuizen J, Kovacic V, Mangwiro TNC, Vale GA, Hastings I, et al. Tsetse Control and Gambian Sleeping Sickness; Implications for Control Strategy. PLoS Negl Trop Dis (2015) 9(8):e0003822. doi: 10.1371/journal.pntd.0003822
6. Molyneux DH, Eberhard ML, Cleaveland S, Addey R, Guiguemdé RT, Kumar A, et al. Certifying Guinea worm eradication: current challenges. Lancet (2020) 396(10265):1857–60. doi: 10.1016/S0140-6736(20)32553-8
7. Durrant C, Thiele EA, Holroyd N, Doyle SR, Sallé G, Tracey A, et al. Population genomic evidence that human and animal infections in Africa come from the same populations of Dracunculus medinensis. PLoS Negl Trop Dis (2020) 14(11):e0008623. doi: 10.1371/journal.pntd.0008623
8. Stothard JR, Kayuni SA, Al-Harbi MH, Musaya J, Webster BL. Future schistosome hybridizations: Will all Schistosoma haematobium hybrids please stand-up! PLoS Negl Trop Dis (2020) 14(7):e0008201. doi: 10.1371/journal.pntd.0008201
9. King KC, Stelkens RB, Webster JP, Smith DF, Brockhurst MA. Hybridization in Parasites: Consequences for Adaptive Evolution, Pathogenesis, and Public Health in a Changing World. PLoS Pathog (2015) 11(9):e1005098. doi: 10.1371/journal.ppat.1005098
10. Kuper H. Disability, mental health, stigma and discrimination and neglected tropical diseases. Trans R Soc Trop Med Hyg (2021) 115(2):145–6. doi: 10.1093/trstmh/traa160
12. Dixon R, Lar L, Dean L. Neglect in the Numbers: leaving no voice behind in disease elimination. Correspondence. Lancet Global Health (2020) 9(1):e22. doi: 10.1016/S2214-109X(20)30453-8
13. Kotze AC, Gilleard JS, Doyle SR, Prichard RK. Challenges and opportunities for the adoption of molecular diagnostics for anthelmintic resistance. Int J Parasitol Drugs Drug Resist (2020) 14:264–73. doi: 10.1016/j.ijpddr.2020.11.005
14. Vlaminck J, Cools P, Albonico M, Ame S, Chanthapaseuth T, Viengxay V, et al. Piloting a surveillance system to monitor the global patterns of drug efficacy and the emergence of anthelmintic resistance in soil-transmitted helminth control programs: a Starworms study protocol. Gates Open Res (2020) 10:4:28. doi: 10.12688/gatesopenres.13115.1
15. Souza AA, Ducker C, Argaw D, King JD, Solomon AW, Biamonte MA, et al. Diagnostics and the neglected tropical diseases roadmap: setting the agenda for 2030. Trans R Soc Trop Med Hyg (2020) 9:115(2):129–35. doi: 10.1093/trstmh/traa118
16. Boulton I, Meredith S, Mertenskoetter T, Glaue F. Evaluation of the Product Development Partnerships funding activities. Report. (2013). Publisher is Department for International Development, UK government Available at: https://assets.publishing.service.gov.uk/media/57a0897140f0b649740000b0/,Evaluation_of_the_Product_Development_Partnerships_funding_activities.pdf.
Keywords: neglected tropical diseases, leave no one behind, resistance, diagnostics, translational research
Citation: Taylor MJ (2021) Specialty Grand Challenge: Embracing the Need for Research and Innovation as Fundamental Enablers for Programmatic Progress for All Neglected Tropical Diseases. Front. Trop. Dis 2:669726. doi: 10.3389/fitd.2021.669726
Received: 19 February 2021; Accepted: 04 March 2021;
Published: 19 March 2021.
Edited and reviewed by: Jeremy Foster, New England Biolabs, United States
Copyright © 2021 Taylor. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mark J. Taylor, Mark.Taylor@lstmed.ac.uk
 Mark J. Taylor
Mark J. Taylor