- 1Santa Lucia Foundation, Rome, Italy
- 2Multidisciplinary Department of Medicine for Surgery and Orthodontics, University of Campania Luigi Vanvitelli, Naples, Italy
- 3Department of Industrial Engineering, University of Naples Federico II, Naples, Italy
- 4Department of Anesthesia and Intensive Care Therapy, Military General Hospital, Rome, Italy
- 5Department of Mental and Physical Health and Preventive Medicine, University of Campania Luigi Vanvitelli, Naples, Italy
After the global spread of a severe acute respiratory syndrome caused by a coronavirus (SARS-CoV-2), factors that influence viral diffusion have gained great attention. Human-to-human transmission mainly occurs through droplets, but viral RNA clearance in different biological fluids in coronavirus disease 2019 (COVID-19) remains unclear. We aimed to correlate the presence and the relevant temporal patterns of SARS-CoV-2 viral RNA in biological specimens (stool, urine, blood, and tears) of the transmission with clinical/epidemiological features in patients with COVID-19. We focused on the time window between the positivity of reverse transcriptase-polymerase chain reaction (RT-PCR) tests from different specimens. We used the Mantel–Cox log rank test to verify the differences in terms of viral shedding duration, while we employed the Mann–Whitney U-test for subgroup analysis. This review protocol was registered with PROSPERO number: CRD42020183629. We identified 147 studies; we included 55 (1,348 patients) for epidemiological analysis, of which we included 37 (364 patients) for statistical analysis. The most frequently used specimens other than respiratory tract swabs were stool samples (or anal/rectal swabs), with a positivity rate of 48.8%, followed by urine samples, with a positivity rate of 16.4%; blood samples showed a positivity rate of 17.5%. We found that fecal positivity duration (median 19 days) was significantly (p < 0.001) longer than respiratory tract positivity (median 14 days). Limited data are available about the other specimens. In conclusion, medical and social communities must pay close attention to negativization criteria for COVID-19, because patients could have longer alternative viral shedding.
Introduction
At the end of the 2019, a novel coronavirus was isolated from patients with pneumonia in Hubei province, China; it was named the 2019 novel coronavirus (2019-nCoV), and the related severe acute respiratory syndrome was referred to as SARS-CoV-2 (1). On January 30, 2020, the World Health Organization (WHO) announced that the new emerging coronavirus pneumonia epidemic constituted a public health emergency of international concern (2). On March 11, 2020, due to the exponential increase in the number of reported cases and the high number of deaths (3), WHO's General Director announced that the novel coronavirus disease (COVID-19) may be defined as a pandemic.
The main sources of infection are SARS-CoV-2-infected patients, who produce a large quantity of the virus in the upper respiratory tract during a prodromal period and clinical manifestations. However, many factors play a crucial role in augmenting diffusion, such as the presence of asymptomatic carriers, the incubation period of the disease (usually ranging from 1 to 14 days, and even up to 24 days), and the mild clinical symptoms during the first disease period, with infected subjects still having an active life (4, 5).
Our understanding of SARS-CoV-2 human-to-human transmission is still evolving; currently, we know that it mainly occurs through air droplets. However, feces may be another potential route of transmission (6). Nosocomial transmission is a severe problem, given the susceptible condition of inpatients, so any action should be taken to minimize the risk of transmission. Notably, there is no indication regarding the danger of biological fluids from a patient with a negative pharyngeal swab. This could become a major problem if he or she is admitted to a post-acute hospital ward or to any sanitary structure with lower healthcare assistance or when he or she is discharged into the community, as demonstrated by a recent review on gastrointestinal symptoms (7). Subjects with positive viral RNA excretion need to be isolated; however, the persistence and clearance of viral RNA in different biological fluids remains unclear. Thus, as the clearance of viral RNA from patients' stool is delayed compared with that from oropharyngeal swabs, it is important to detect the viral RNA in feces during the convalescence phase to provide guidance to patients about contact limitations and even to manage drug administration (i.e., avoiding immunosuppressant drugs such as glucocorticoids).
In this context, our study, inspired by the needs expressed by physicians in post-acute settings, aimed to systematically review the existing data on novel coronavirus viral shedding. We reviewed, referring to the recommended diagnostic criteria: (i) the incidence of viral RNA in biological specimens (urine, stool, blood, and tears); (ii) the persistence of viral shedding and the correlation between the presence of viral RNA in the respiratory tract and in feces; and (iii) the correlation between persistent viral shedding in the post-acute phase with disease severity.
Methods
Search Strategy and Selection Criteria
For our systematic review and meta-analysis, we followed PRISMA guidelines (8). We searched for data on confirmed COVID-19 patients' viral shedding reported in any kind of study (case report/series, cohort studies, case-control studies, or randomized control trials) with available data in English, published until May 5, 2020. Two authors (G.M. and A.P.) independently and synchronously searched PubMed, EMBASE, and Web of Science up to May 5, 2020, in order to identify all studies documenting modalities of SARS-CoV-2 viral shedding in patients with a confirmed diagnosis of COVID-19.
The search terms were “2019-nCoV,” “SARS-CoV-2,” “novel coronavirus,” or “COVID-19” combined with “viral shedding” and/or “feces,” “stool,” “feces,” “urine,” “blood,” or “tears.” We found additional studies by carefully searching the reference lists of the identified works. Titles and abstracts were screened, and two authors (G.M. and A.P.) independently reviewed full-text papers. Exclusion criteria were studies not written in English, not reporting specimens other than respiratory tract swabs, duplicates, or not matching the inclusion criteria and/or the topic of the review (for this last criterion, in case of disagreement between the two above authors, an independent reviewer stepped in, namely D.D.).
We obtained data about the sites of studies, sample sizes, patient demographics, analyzed clinical samples, disease duration, and viral shedding duration through different routes. We then focused on the time window between the positivity of reverse transcriptase-polymerase chain reaction (RT-PCR) tests from different specimens. In particular, we considered the duration of sample positivity for SARS-CoV-2 from the onset of symptoms or, for asymptomatic patients, from the first positive result until the last available positive testing. We considered respiratory samples (throat swabs, nasopharyngeal swabs, oral swabs, sputum, or saliva) to be a hallmark of COVID-19 diagnosis, while we compared the other specimens' duration of positivity to the respiratory one. We collected specific data about single patients when available. When possible, we asked corresponding authors for missing data in order to collect wider information. When we could not obtain single patient data, we took pooled data.
Data Analysis
M.I. performed all statistical analyses using Statistical Package for Social Science (SPSS) 25.0. Continuous variables are expressed as median (interquartile range) or mean (± standard deviation), according to their normality test results (verified through the Shapiro–Wilk test). In order to overcome the possible heterogeneity within and between studies, M.I. performed the analyses on a pooled database containing data from each patient enrolled in the studies that provided single subject data and not using aggregated measures. M.I. used the Mantel–Cox log rank test to verify the differences in terms of viral shedding duration, while M.I. used the Mann–Whitney U-test for subgroup analysis. Moreover, we assessed the quality of the selected studies using the Newcastle–Ottawa Scale (9). We registered our review on PROSPERO (registration number: CRD42020183629).
Results
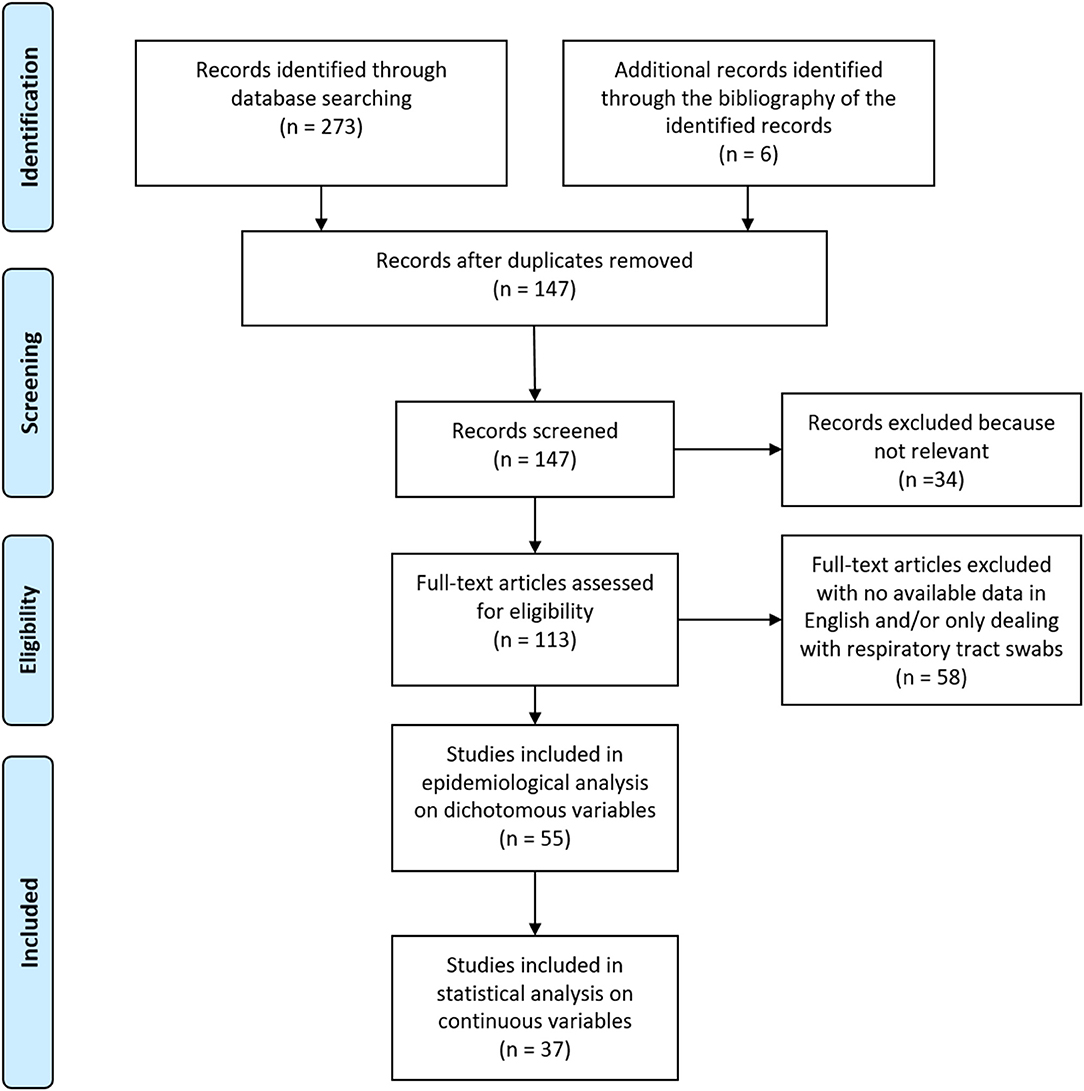
The results of our search are shown in the PRISMA flow-chart depicted in Figure 1. After removal of duplicates and documents assessed as not eligible for our purposes, we found 113 papers. Of these, we included 55 studies in the present review for epidemiological analysis on group data and dichotomous variables; 37 of these reported continuous values and could be included in our quantitative analysis on single patients' data.
The detailed data of the 55 selected studies are available in Table 1. All the selected articles used RT-PCR for viral RNA detection (10–64). A few of them (32, 41, 42, 63) added viral cultures, viral isolation, or next generation sequencing (NGS). The total number of patients was 1,348 (1–132 for each article), with an age range from 17 days to 96 years. Of 1,219 patients for whom we found information about gender, 593 were female (48.6%). Most of the studies (78.2%) were conducted in China, while the others were from Asia (two from Korea, two from Singapore, one from Taiwan, and one from Lebanon), Europe (two from Italy, one from France, and one from Germany), and the United States of America (two). Almost all studies (52 out of 55) were assessed as high quality, showing Newcastle–Ottawa Scale scores ≥7 (9).
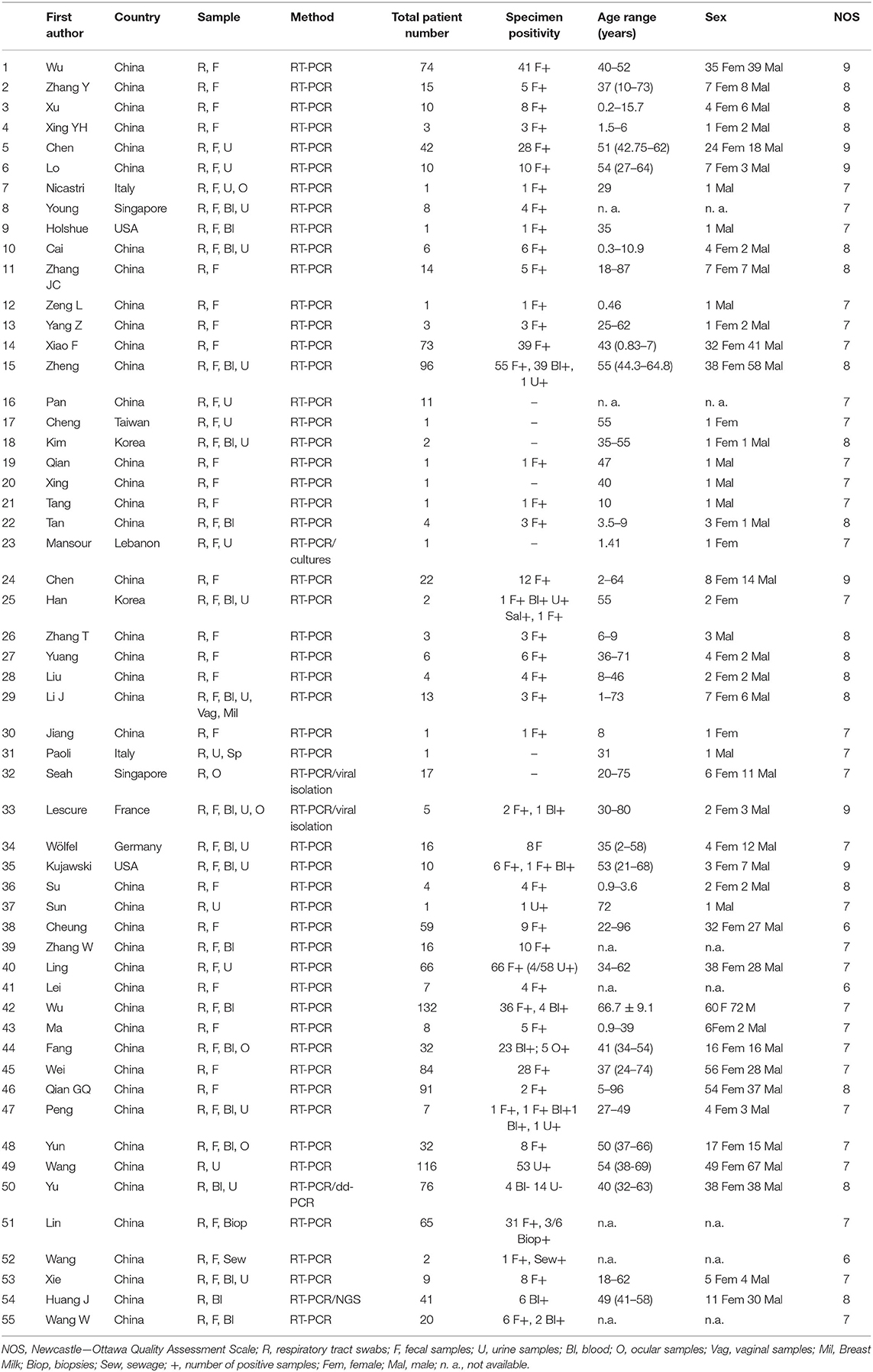
As shown in Figure 2, the most frequently used specimens other than respiratory tract swabs were stool samples (or anal/rectal swabs). Indeed, 50 articles examined fecal samples, with a positivity rate of 48.8% (490 out of 1,005 patients). Moreover, 22 articles examined urine samples, with a positivity rate of 16.4% (60 out of 366 patients), while blood samples showed in 20 articles a positivity rate of 17.5% (80 out of 456 patients). Finally, five articles considered ocular samples (tears or conjunctival swabs), with a positivity rate of 7.7% (5/65 patients). However, most of these studies did not report the duration data of each tested patient. One study (16) examined the semen of only one patient, with a negative result, while another study (38) looked for coronavirus RNA in the breast milk of a breastfeeding woman, also with a negative result. Another study (60) added the virus search on gastrointestinal tract biopsies (with three positive results out of six biopsies). Wang and colleagues (62) analyzed sewage and identified SARS-CoV-2 RNA.
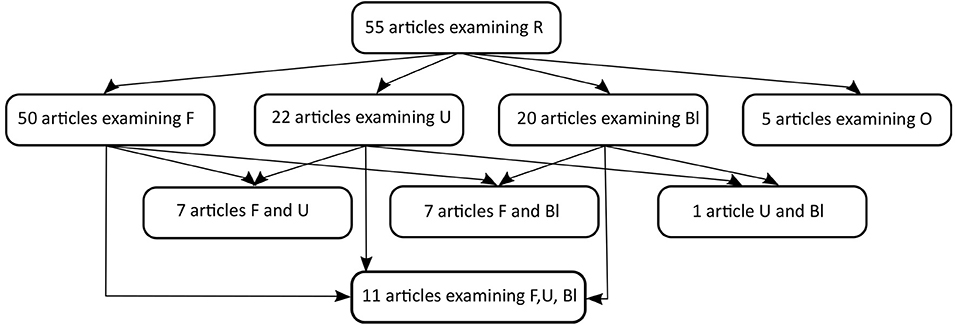
Figure 2. Flow diagram of the specimens considered in the 55 selected articles (R, respiratory tract; F, feces; U, urine; Bl, Blood; O, ocular samples). We want to clarify that two of the F and Bl, one of the F, U, Bl and one of the F and U even consider ocular samples.
From 37 studies (including 364 patients) reporting the duration of both R+ (respiratory tract swab positivity) and F+ (fecal sample positivity) for each patient (9–45), we pooled data for statistical analysis. Although these studies included 364 patients, R+ and F+ duration data were only available for 215 individuals, plus 11 patients for whom only the difference between F+ and R+ had been reported. The median R+ duration was 14 days [interquartile range (IQR) 12 days], whereas that of F+ was 19 days (IQR 14 days). The Shapiro–Wilk test highlighted that both R+ and F+ were not normally distributed (p < 0.001). For this reason, we used the Wilcoxon test to compare the lengths of positivity; there was a statistically significant difference (p < 0.001, n = 215). There was a significant correlation between the duration of R+ and F+ (Spearman correlation coefficient R = 0.507, p < 0.001). The Mantel–Cox log rank showed a statistically significant difference between F+ and R+ trends (χ2 = 31.6, p < 0.001; Figure 3). Of the 226 patients with both R+ and F+, 27 patients (11.9%) had the same duration for both routes of viral shedding, 55 (24.3%) had a longer R+ duration, and the remaining 144 (63.7%) showed a longer F+ duration.
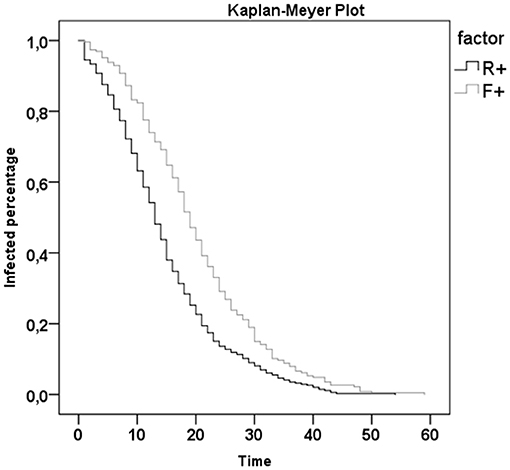
Figure 3. Kaplan-Meyer Plot of R+ (respiratory tract swab positivity) and F+ (fecal sample positivity) duration.
Moreover, there were statistically significant differences between severe and not severe [as defined by the American Thoracic Society and Infectious Disease Society of America guidelines for community acquired pneumonia (65)] patients in terms of R+ duration (p < 0.001, Mann–Whitney U-test, n = 309), F+ duration (p = 0.010, n = 184), and their difference (p < 0.001, n = 182). Interestingly, for the most severe subjects, R+ and F+ durations were not statistically different from each other (p = 0.496, Wilcoxon test, n = 69), whereas for less severely affected patients, there was a statistically significant difference (p < 0.001, n = 112; Figure 4).
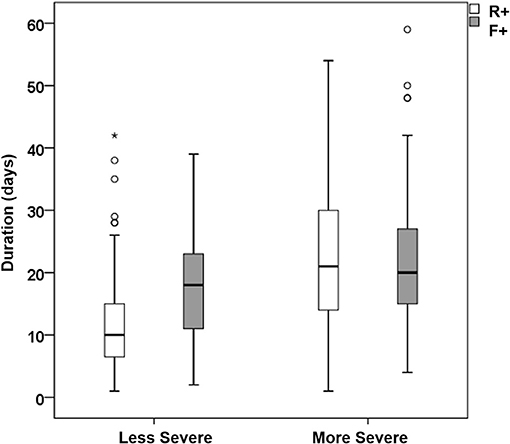
Figure 4. Box-whiskers plot with median and quartile values for the duration of R+ (white boxes) and F+ (gray boxes) of less (left) and more (right) severe patients (circles and stars indicate patients out of the 95% confidence interval).
There were age data available for 105 subjects, 41 of whom were children (age <18 years old), 38 of whom showed mild symptoms (according to the literature). For this reason, we compared the data of these 38 children with those of adults with mild symptoms for whom age data were available (n = 48). We did not find significant age-related differences in terms of R+ (median 8 days, IQR 9 days in children vs. median 10 days, IQR 11 days in adults; p = 0.121) or F+ (median 22 days, IQR 12 days in children vs. median 18 days, IQR 12 days in adults; p = 0.058). However, the difference between F+ and R+ was significantly longer in children than in adults (median 12 days, IQR 12 days in children vs. median 5 days, IQR 11 days in adults; p = 0.001).
Statistical analysis about the duration of other specimen positivity (blood, urine, and ocular samples) was not possible, due to the reduced sample size of available data. Indeed, single patient data about blood sample positivity were reported only in three studies (24, 34, 42), and urinary sample positivity duration was available for one single case study (34). There were no available data on other specimens for single patients.
Finally, digestive symptoms were available for 42 patients, but all from the same study (14). For this reason, it was not possible to perform a meta-analysis on these symptoms.
Discussion
The available data confirm the presence of viral RNA in several biological specimens (stool, urine, blood, and tears), but with very different positivity rates. Our results confirm concerns initially identified by Zhang and colleagues in their pioneering work (48). These concerns are related to modalities of dealing with people considered recovered after COVID-19 infection, without considering the persistent viral shedding in their biological specimens other than those collected in the respiratory tract. Not keeping them isolated or not taking the appropriate precautions could markedly increase the risk for virus spreading during the post-acute phase. Indeed, the present work confirms, on a wider basis than previous studies (364 patients), the significant prolonged viral shedding through feces. Although our aim was to also analyze other specimens, most of the analyzed studies only reported respiratory tract and fecal data. Our results revealed that the prolonged positivity of viral RNA excretion was statistically significant, particularly in patients with less severe disease, although digestive symptoms had only been anecdotally reported in previous review studies (14). This outcome may depend on the inclusion/exclusion search criteria of our review. Other reviews have focused on gastrointestinal symptoms and reported a higher prevalence in more severe patients (46, 65). Our findings suggest the importance of screening the viral positivity of patients' stool even after negative results of their respiratory tract swabs. Therefore, prolonging the contact precautions both at home or in the post-acute environment for all post-COVID-19 patients seems to be advisable. The Kaplan–Meyer plot (Figure 3) would suggest prolonging the precautions for about 10 days. Moreover, as suggested by Yeo et al. (66), it is important to clarify the possibility of fecal-oral transmission for SARS-CoV-2, as already confirmed for other coronaviruses (67). In addition, a recent review by Cheung (47) investigated the correlation between fecal viral shedding duration and enteric symptoms. Finally, we analyzed the correlation between viral RNA excretion in feces and the disease severity. The longer duration of viral shedding in feces was statistically significant for less affected patients, and especially for children, a population in which the severity of COVID-19 was lower, as has been widely reported in literature.
The main limitation of this work is related to the fact that most of the studies detected viral RNA and not live viral shedding. So far, the exact correlation between RNA viral shedding and infectious viral shedding is not known, although live SAR-CoV-2 viruses have been isolated in different specimens including stool (68). We identified four other limitations: (1) despite our aim to analyze viral shedding in specimens other than respiratory swabs, most of the data were limited to feces; (2) specimens collected in different areas of the same body tract are considered a single type of sample; (3) we analyzed all data available in the publications about positivity rates and viral RNA shedding duration, but we must consider possible biases in the previous publications, for which only part of the data had been published by the authors (publication bias); and (4) the duration of infection might depend on the criteria related to the diagnosis of infection and to those for defining the negativization of a patient (with one or two consecutive negative tests) potentially related to different tracts (nasal or fecal swab tests) and different symptoms (respiratory or digestive).
Conclusions
In conclusion, on the basis of our results, medical and social communities must pay close attention to patients who present COVID-19 with mild or no symptoms, because our results suggest they could represent individuals with longer alternative viral shedding, even after a negativized pharyngeal swab. Therefore, appropriate management of the patient flow between an intensive care unit (ICU) and post-ICU departments (i.e., post-acute units) should be carefully considered by implementing risk management that is also related to alternative viral shedding.
Data Availability Statement
All datasets generated for this study are included in the article/supplementary material.
Author Contributions
GM and AP performed the literature search and wrote the first draft of the report, with input from DC. TC assessed the quality of the selected studies. DD, VV, AS, PC, FG, GI, and SP reviewed the draft and expanded the clinical implications. MI performed the statistical analysis and had full access to all the data in the study. All authors contributed to the article and approved the submitted version.
Funding
This review has been supported by the Santa Lucia Foundation and the Italian Ministry of Healthcare (Current Research Line). The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. doi: 10.1056/NEJMoa2001017
2. WHO. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19. (2020). Available online at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 (accessed on May 10, 2020)
3. Iosa M, Paolucci S, Morone G. Covid-19: a dynamic analysis of fatality risk in Italy. Front Med. (2020) 7:185. doi: 10.3389/fmed.2020.00185
4. Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. (2020) 382:1177–9. doi: 10.1056/NEJMc2001737
5. Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. (2020) 382:970–1. doi: 10.1056/NEJMc2001468
6. Gu J, Han B, Wang J, COVID-19: gastrointestinal manifestations and potential fecal–oral transmission. Gastroenterology. (2020) 158:1518–19. doi: 10.1053/j.gastro.2020.02.054
7. Tu H, Tu S, Gao S, Shao A, Sheng J. The epidemiological and clinical features of COVID-19 and lessons from this global infectious public health event. J Infect. (2020) 81:1–9. doi: 10.1016/j.jinf.2020.04.011
8. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
9. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
10. Wu Y, Guo C, Tang L, Hong Z, Zhou J, Dong X, et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol. (2020) 5:434–5. doi: 10.1016/S2468-1253(20)30083-2
11. Yongchen Z, Shen H, Wang X, Shi X, Li Y, Yan J, et al. Different longitudinal patterns of nucleic acid and serology testing results based on disease severity of COVID-19 patients. Emerg Microbes Infect. (2020) 9:833–6. doi: 10.1080/22221751.2020.1756699
12. Xu Y, Li X, Zhu B, Liang H, Fang C, Gong Y, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. (2020) 26:502–5. doi: 10.1038/s41591-020-0817-4
13. Xing YH, Ni W, Wu Q, Li WJ, Li GJ, Wang WD, et al. Prolonged viral shedding in feces of pediatric patients with coronavirus disease 2019. J Microbiol Immunol Infect. (2020) 53:473–80. doi: 10.1016/j.jmii.2020.03.021
14. Chen Y, Chen L, Deng Q, Zhang G, Wu K, Ni L, et al. The presence of SARS-CoV-2 RNA in feces of COVID-19 patients. J Med Virol. (2020) 92:833–40. doi: 10.1002/jmv.25825
15. Lo IL, Lio CF, Cheong HH, Lei CI, Cheong TH, Zhong X, et al. Evaluation of SARS-CoV-2 RNA shedding in clinical specimens and clinical characteristics of 10 patients with COVID-19 in Macau. Int J Biol Sci. (2020) 16:1698–707. doi: 10.7150/ijbs.45357
16. Nicastri E, D'Abramo A, Faggioni G, De Santis R, Mariano A, Lepore L, et al. Coronavirus disease (COVID-19) in a paucisymptomatic patient: epidemiological and clinical challenge in settings with limited community transmission. Euro Surveill. (2020) 25:2000230. doi: 10.2807/1560-7917.ES.2020.25.11.2000230
17. Young BE, Ong SWX, Kalimuddin S, Low JG, Tan SY, Loh J, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. (2020) 323:1488–94. doi: 10.1001/jama.2020.3204
18. Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. (2020) 382:929–36. doi: 10.1056/NEJMoa2001191
19. Cai J, Xu J, Lin D, Xu L, Qu Z, Zhang Y, et al. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis. (2020). doi: 10.1093/cid/ciaa198. [Epub ahead of print].
20. Zhang J, Wang S, Xue Y. Fecal specimen diagnosis 2019 novel coronavirus–infected pneumonia. J Med Virol. (2020) 92:680–2. doi: 10.1002/jmv.25742
21. Zeng LK, Tao XW, Yuan WH, Wang J, Liu X, Liu ZS. First case of neonate infected with novel coronavirus pneumonia in China. Zhonghua Er Ke Za Zhi. (2020) 58:E009. doi: 10.3760/cma.j.issn.0578-1310.2020.0009
22. Yang Z, Li G, Dai X, Liu G, Li G, Jie Y. Three cases of novel coronavirus pneumonia with viral nucleic acids still positive in stool after throat swab detection turned negative. Chin J Dig. (2020) 40:E002. doi: 10.3760/cma.j.issn.0254-1432.2020.0002
23. Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. (2020) 158:1831–3.e3. doi: 10.1053/j.gastro.2020.02.055
24. Zheng S, Fan J, Yu F, Feng B, Lou B, Zou Q, et al. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: retrospective cohort study. BMJ. (2020) 369:m1443. doi: 10.1136/bmj.m1443
25. Pan Y, Zhang D, Yang P, Poon LL, Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis. (2020) 20:411–2. doi: 10.1016/S1473-3099(20)30113-4
26. Cheng SC, Chang YC, Chiang YLF, Chien YC, Cheng M, Yang CH, et al. First case of Coronavirus Disease 2019 (COVID-19) pneumonia in Taiwan. J Formos Med Assoc. (2020) 119:747–51. doi: 10.1016/j.jfma.2020.02.007
27. Kim JY, Ko JH, Kim Y, Kim YJ, Kim JM, Chung YS, et al. Viral load kinetics of SARS-CoV-2 infection in first two patients in Korea. J Korean Med Sci. (2020) 35:e86. doi: 10.3346/jkms.2020.35.e86
28. Qian GQ, Chen XQ, Lv DF, Ma AHY, Wang LP, Yang NB, et al. Duration of SARS-CoV-2 viral shedding during COVID-19 infection. Infect Dis. (2020) 52:511–12. doi: 10.1080/23744235.2020.1748705
29. Xing Y, Mo P, Xiao Y, Zhang Y, Wang F. Post-discharge surveillance and positive virus detection in two medical staff recovered from coronavirus disease 2019 (COVID-19), China, January to February 2020. Euro Surveill. (2020) 25:2000191. doi: 10.2807/1560-7917.ES.2020.25.10.2000191
30. Tang A, Tong ZD, Wang HL, Dai YX, Li KF, Liu JN. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg Infect Dis. (2020) 26:1337–9. doi: 10.3201/eid2606.20.0301
31. Tan YP, Tan BY, Pan J, Wu J, Zeng SZ, Wei HY. Epidemiologic and clinical characteristics of 10 children with coronavirus disease 2019 in Changsha, China. J Clin Virol. (2020) 127:104353. doi: 10.1016/j.jcv.2020.104353
32. Mansour A, Atoui R, Kamal Kanso RM, Fares Y, Fares J. First case of an Infant with COVID-19 in the middle east. Cureus. (2020) 12:e7520. doi: 10.7759/cureus.7520
33. Chen C, Gao G, Xu Y, Pu L, Wang Q, Wang L, et al. SARS-CoV-2–positive sputum and feces after conversion of pharyngeal samples in patients with COVID-19. Ann Intern Med. (2020) 172:832–4. doi: 10.7326/M20-0991
34. Han MS, Seong MW, Heo EY, Park JH, Kim N, Shin S, et al. Sequential analysis of viral load in a neonate and her mother infected with SARS-CoV-2. Clin Infect Dis. (2020). doi: 10.1093/cid/ciaa447. [Epub ahead of print].
35. Zhang T, Cui X, Zhao X, Wang J, Zheng J, Zheng G, et al. Detectable SARS-CoV-2 viral RNA in feces of three children during recovery period of COVID-19 pneumonia. J Med Virol. (2020) 92:909–14. doi: 10.1002/jmv.25795
36. Wang N, Ou X. Caution should be exercised for the detection of SARS-CoV-2, especially in the elderly. J Med Virol. (2020). doi: 10.1002/jmv.25796. [Epub ahead of print].
37. Liu J, Xiao Y, Shen Y, Shi C, Chen Y, Shi P, et al. Detection of SARS-CoV-2 by RT-PCR in anal from patients who have recovered from coronavirus disease 2019. J Med Virol. (2020). doi: 10.1002/jmv.25875. [Epub ahead of print].
38. Li Y, Hu Y, Yu Y, Zhang X, Li B, Wu J, et al. Positive result of Sars-Cov-2 in faeces and sputum from discharged patient with COVID-19 in Yiwu, China. J Med Virol. (2020). doi: 10.1002/jmv.25905. [Epub ahead of print].
39. Jiang X, Luo M, Zou Z, Wang X, Chen C, Qiu J. Asymptomatic SARS-CoV-2 infected case with viral detection positive in stool but negative in nasopharyngeal samples lasts for 42 days. J Med Virol. (2020). doi: 10.1002/jmv.25941. [Epub ahead of print].
40. Paoli D, Pallotti F, Colangelo S, Basilico F, Mazzuti L, Turriziani O, et al. Study of SARS-CoV-2 in semen and urine samples of a volunteer with positive naso-pharyngeal swab. J Endocrinol Invest. (2020). doi: 10.1007/s40618-020-01261-1. [Epub ahead of print].
41. Jun ISY, Anderson DE, Kang AEZ, Wang LF, Rao P, Young BE, et al. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) patients. Ophthalmology. (2020) 127:977–79. doi: 10.1016/j.ophtha.2020.03.026
42. Lescure FX, Bouadma L, Nguyen D, Parisey M, Wicky PH, Behillil S, et al. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect Dis. (2020) 20:697–706. doi: 10.1016/S1473-3099(20)30200-0
43. Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. (2020) 581:465–69. doi: 10.1038/s41586-020-2196-x
44. Kujawski SA, Wong KK, Collins JP, Epstein L, Killerby ME, Midgley CM, et al. Clinical and virologic characteristics of the first 12 patients with coronavirus disease 2019 (COVID-19) in the United States. Nat Med. (2020) 26:861–68. doi: 10.1038/s41591-020-0877-5
45. Su L, Ma X, Yu H, Zhang Z, Bian P, Han Y, et al. The different clinical characteristics of corona virus disease cases between children and their families in China–the character of children with COVID-19. Emerg Microbes Infect. (2020) 9:707–13. doi: 10.1080/22221751.2020.1744483
46. Sun J, Zhu A, Li H, Zheng K, Zhuang Z, Chen Z, et al. Isolation of Infectious SARS-CoV-2 from Urine of a COVID-19 Patient. Emerg Microbes Infect. (2020) 9:991–93. doi: 10.1080/22221751.2020.1760144
47. Cheung KS, Hung IF, Chan PP, Lung KC, Tso E, Liu R, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from the Hong Kong cohort and systematic review and meta-analysis. Gastroenterology. (2020). 159:81–95. doi: 10.1053/j.gastro.2020.03.065
48. Zhang W, Du RH, Li B, Zheng XS, Yang XL, Hu B, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. (2020) 9:386–9. doi: 10.1080/22221751.2020.1729071
49. Ling Y, Xu SB, Lin YX, Tian D, Zhu ZQ, Dai FH, et al. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J. (2020) 133:1039–43. doi: 10.1097/CM9.0000000000000774
50. Lei Z, Cao H, Jie Y, Huang Z, Guo X, Chen J, et al. A cross-sectional comparison of epidemiological and clinical features of patients with coronavirus disease (COVID-19) in Wuhan and outside Wuhan, China. Travel Med Infect Dis. (2020) 35:101664. doi: 10.1016/j.tmaid.2020.101664
51. Wu J, Liu J, Li S, Peng Z, Xiao Z, Wang X, et al. Detection and analysis of nucleic acid in various biological samples of COVID-19 patients. Travel Med Infect Dis. (2020). doi: 10.1016/j.tmaid.2020.101673. [Epub ahead of print].
52. Ma X, Su L, Zhang Y, Zhang X, Gai Z, Zhang Z. Do children need a longer time to shed SARS-CoV-2 in stool than adults? J Microbiol Immunol Infect. (2020) 53:373–76. doi: 10.1016/j.jmii.2020.03.010
53. Fang Z, Zhang Y, Hang C, Ai J, Li S, Zhang W. Comparisons of viral shedding time of SARS-CoV-2 of different samples in ICU and non-ICU patients. J Infect. (2020) 81:147–78. doi: 10.1016/j.jinf.2020.03.013
54. Wei XS, Wang X, Niu YR, Ye LL, Peng WB, Wang ZH, et al. Diarrhea is associated with prolonged symptoms and viral carriage in COVID-19. Clin Gastroenterol Hepatol. (2020) 18:1753–1759.e2. doi: 10.1016/j.cgh.2020.04.030
55. Qian GQ, Yang NB, Ding F, Ma AHY, Wang ZY, Shen YF, et al. Epidemiologic and clinical characteristics of 91 hospitalized patients with COVID-19 in Zhejiang, China: a retrospective, multi-centre case series. QJM. (2020) 113:474–81. doi: 10.1093/qjmed/hcaa089
56. Peng L, Liu J, Xu W, Luo Q, Deng K, Lin B, et al. SARS-CoV-2 can be detected in urine, blood, anal swabs, and oropharyngeal swabs specimens. J Med Virol. (2020). doi: 10.1002/jmv.25936. [Epub ahead of print].
57. Yun H, Sun Z. Wu J, Tang A, Hu M, Xiang Z. Laboratory data analysis of novel coronavirus (COVID-19) screening in 2510 patients. Clin Chim Acta. (2020) 507:94–7. doi: 10.1016/j.cca.2020.04.018
58. Wang L, Li X, Chen H, Yan S, Li D, Li Y, et al. Coronavirus disease 19 infection does not result in acute kidney injury: an analysis of 116 hospitalized patients from Wuhan, China. Am J Nephrol. (2020) 51:343–8. doi: 10.1159/000507471
59. Yu F, Yan L, Wang N, Yang S, Wang L, Tang Y, et al. Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients. Clin Infect Dis. (2020) 71:793–98. doi: 10.1093/cid/ciaa345
60. Lin L, Jiang X, Zhang Z, Huang S, Zhang Z, Fang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. (2020) 69:997–1001. doi: 10.1136/gutjnl-2020-321013
61. Xie C, Jiang L, Huang G, Pu H, Gong B, Lin H, et al. Comparison of different samples for 2019 novel coronavirus detection by nucleic acid amplification tests. Int J Infect Dis. (2020) 93:264–67. doi: 10.1016/j.ijid.2020.02.050
62. Wang J, Feng H, Zhang S, Ni Z, Ni L, Chen Y, et al. SARS-CoV-2 RNA detection of hospital isolation wards hygiene monitoring during the Coronavirus Disease 2019 outbreak in a Chinese hospital. Int J Infect Dis. (2020) 94:103–106. doi: 10.1016/j.ijid.2020.04.024
63. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
64. Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. (2020). doi: 10.1001/jama.2020.3786. [Epub ahead of print].
65. Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. (2019) 200:e45–67. doi: 10.1164/rccm.201908-1581ST
66. Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. (2020) 5:335–7. doi: 10.1016/S2468-1253(20)30048-0
67. Ding S, Liang TJ. Is SARS-CoV-2 also an enteric pathogen with potential fecal-oral transmission: a COVID-19 virological and clinical review. Gastroenterology. (2020) 159:53–61. doi: 10.1053/j.gastro.2020.04.052
Keywords: viral shedding, COVID-19, SARS-CoV-2, stool, post-acute phase
Citation: Morone G, Palomba A, Iosa M, Caporaso T, De Angelis D, Venturiero V, Savo A, Coiro P, Carbone D, Gimigliano F, Iolascon G and Paolucci S (2020) Incidence and Persistence of Viral Shedding in COVID-19 Post-acute Patients With Negativized Pharyngeal Swab: A Systematic Review. Front. Med. 7:562. doi: 10.3389/fmed.2020.00562
Received: 03 June 2020; Accepted: 10 August 2020;
Published: 28 August 2020.
Edited by:
Zhongheng Zhang, Sir Run Run Shaw Hospital, ChinaReviewed by:
Yanfei Shen, Zhejiang Hospital, ChinaJing Yuan, Children's Hospital of Capital Institute of Pediatrics, China
Copyright © 2020 Morone, Palomba, Iosa, Caporaso, De Angelis, Venturiero, Savo, Coiro, Carbone, Gimigliano, Iolascon and Paolucci. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marco Iosa, bS5pb3NhQGhzYW50YWx1Y2lhLml0
†These authors have contributed equally to this work
 Giovanni Morone
Giovanni Morone Angela Palomba
Angela Palomba Marco Iosa
Marco Iosa Teodorico Caporaso
Teodorico Caporaso Domenico De Angelis1
Domenico De Angelis1 Stefano Paolucci
Stefano Paolucci