- 1Monash Nursing and Midwifery, Faculty of Medicine, Nursing and Health Sciences, Monash University, Melbourne, VIC, Australia
- 2Monash Partners Academic Health Science Centre, Clayton, VIC, Australia
- 3Monash Health, Clayton, VIC, Australia
- 4School of Nursing and Midwifery, Deakin University, Melbourne, VIC, Australia
Coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was identified in China in December 2019 and became a pandemic in a short period of time. While most infected people might have mild symptoms, older people and people with chronic illnesses may develop acute respiratory distress syndrome (ARDS). Patients with ARDS with worsening hypoxemia require prone positioning to improve the respiratory mechanics and oxygenation. Intubated patients may stay in a prone position up to 12–16 h, increasing the risk of pressure injury (PI). Frequent skin inspections and PI risk assessment in COVID-19 patients will be challenging due to hospital infection control measures aimed to reduce the risk for health professionals. In this perspective article, we summarize the best practice recommendations for prevention of PI in SARS-CoV-2-infected ARDS patients in prone positioning. Prior to positioning patients in prone position, the main recommendations are to (1) conduct a skin assessment, (2) use pressure redistribution devices, (3) select an appropriate mattress or an overlay, (4) ensure that the endotracheal tube securing device is removed and the endotracheal tube is secured with tapes, (5) use a liquid film-forming protective dressing, and (6) lubricate the eyes and tape them closed. Once a patient is in prone position, it is recommended to (1) use the swimmer's position, (2) reposition the patient every 2 h, and (3) keep the skin clean. When the patient is repositioned to supine position, healthcare professionals are advised to (1) assess the pressure points and (2) promote early mobilization.
Introduction
Coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was identified in China in December 2019 and rapidly became a pandemic (1, 2). While most infected people have mild symptoms, older people and people with chronic illnesses may become critically ill and develop viral pneumonia and acute respiratory distress syndrome (ARDS) (3–5), requiring admission to an intensive care unit (ICU) (6). The pathophysiology of SARS-CoV-2 ARDS differs from that of the typical ARDS (7). The pathophysiological mechanism of COVID-19-related ARDS is pulmonary micro-thrombosis (8). The results of lung and skin biopsy of critically ill SARS-CoV-2-infected patients demonstrated generalized thrombotic microvascular injury (7). SARS-CoV-2 infection results in cytokine storm and a local and systemic inflammatory response syndrome leading to macro- and microthrombosis (8, 9). The three factors of Virchow's triad—reduced blood flow, endothelial injury, and hypercoagulability—increase the risk of thrombosis in severe COVID-19 patients (8).
Most ICU-admitted COVID-19 patients need non-invasive ventilation, a non-rebreathing mask, and prone positioning to increase oxygen delivery (10) as well as high-flow nasal oxygen through specialized nasal cannula in negative-pressure rooms (11). Up to 5% of COVID-19 patients with ARDS may require endotracheal intubation (12, 13). In general, patients with ARDS of any etiology with worsening hypoxemia (PaO2:FiO2 < 100–150 mmHg, FiO2 ≥ 0.6, PEEP ≥ 10 cm of water, and tidal volume of 6 ml/kg of predicted body weight) require prone positioning to improve the respiratory mechanics, improve oxygenation, and offload the weight of the heart (14, 15). When applied early (usually 12 to 24 h after the initiation of mechanical ventilation) with other lung-protective strategies and adopted for a prolonged period, the prone position is associated with reduced mortality, particularly in patients with severe hypoxemia (16–18).
Prone positioning was reported in the management of ARDS in critically ill patients with severe acute respiratory syndrome (SARS) (19) and Middle East respiratory syndrome (MERS) (20) coronavirus infections and is used to manage ARDS in COVID-19 patients (12). Initially, it was found to be effective in one small-scale study of 52 critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China (21), with further anecdotal evidence from day-to-day clinical practice in ICU. A recent small-scale study (22) on the use of prone positioning in non-intubated patients with COVID-19 and hypoxemic acute respiratory failure in Turkey, managed outside the ICU, reported that oxygenation increased in only a quarter of patients and was not sustained in half of those after resupination. Self-proning of COVID-19 patients is increasingly used in several countries and has become a standard treatment in the management of ARDS patients with hypoxia (23). With some precautions, prone positioning is used in the management of COVID-19-related ARDS in pregnant women (24). A case report from Japan suggests that, although prone positioning may mitigate hypoxemia, its role in reducing mortality in COVID-19 patients with ARDS is unclear, particularly in patients with a secondary superinfection (25), which is often associated with sepsis, shock, and multiple organ failure (26).
The intubated patients may remain in a prone position up to 16 h per day, alternating with 8 h in supine position (27). Prone positioning increases the risk of developing hospital-acquired pressure injury (HAPI) (16, 28), and this risk is higher when compared to the supine position (29). A Wuhan study reported that the mean hospital stay of COVID-19 patients with pneumonia was 22 days (5); prolonged ICU admission (30) and increased hospital stay (31) are independent risk factors for the development of HAPI.
While the studies reporting HAPI incidence in COVID-19 ARDS patients have not yet been published, individual case reports have reported that patients cared in prone position are at risk of developing multiple severe device-related PI on their face, requiring a consultation and an intervention by plastic surgeons (32). Furthermore, diarrhea is a common gastrointestinal feature in COVID-19 patients (33, 34), and in addition to other risk factors, such as immobility and reduced perfusion, diarrhea may contribute to the development of incontinence-associated dermatitis and a pressure injury in the sacral area (35). This risk is even higher in older patients with COVID-19 ARDS and requires immediate attention (36).
Repositioning and pressure relief are important strategies to reduce the risk (37). However, clinical experience reports the need to involve up to seven people to reposition the intubated patient. Frequent skin inspections and risk assessment in COVID-19 patients could be challenging due to hospital infection control measures aimed to reduce the risk for health professionals working in ICU (11, 38).
In general, there is a global health professional knowledge deficit on PI prevention, with early detection (39–45) and standard preventive interventions recommended in clinical practice guidelines not fully implemented (46) in the context of COVID-19 clinical care. Health professionals may lack awareness of pressure points typical for patients in prone position and may have misconceptions related to the specific equipment required for prone positioning (47). In this perspective article, we summarize the best recommendations for the prevention of PI in SARS-CoV-2-infected ARDS patients in prone position.
Prone Position: Pressure Injury Prevention
The latest version of Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline, International Version (37) acknowledges evidence derived from one low-quality study (29), indicating that prone positioning is associated with a higher incidence of HAPI compared with supine positioning. The reported incidence of HAPI is said to be 5 to 15% as derived from low- and moderate-quality studies (48–50). The main recommendation is to avoid the extended use of prone positioning unless required for the management of a medical condition ((37), p. 126). However, COVID-19 ARDS management requires prone positioning for extended periods of time, and therefore, using appropriate support surfaces and pillows and patient repositioning as soon as feasible are key preventive strategies recommended by the guidelines (37). Facial pillows and chest padding can be used to redistribute pressure. The main pressure points in the prone position are the forehead, chin, cheeks, shoulder (anterior), elbow, chest (breasts), genitalia (particularly male), anterior pelvic bones (iliac crests and ischium), knees (patella), dorsal feet and toes, and nose (if positioned incorrectly), which should be inspected as soon as feasible ((37), p. 139), especially if supplies of personal protective equipment are limited.
According to the guidelines ((37), p. 126), the implementation strategies for HAPI prevention in the prone position include the following:
1) Use of pressure redistribution support surface or positioning devices to offload pressure points on the face and the body,
2) Checking for uneven pressure redistribution, focusing on main pressure points unique to prone position, and positioning of medical devices,
3) Use of additional PI preventive strategies, including prophylactic silicone dressings over the bony prominences and under medical devices,
4) Assessing the face and body areas in the main pressure points at each rotation.
A recent review (51) of PI prevention in non-COVID-19 patients, placed in prone position, reported that the main preventive strategies include (1) conducting a skin assessment before proning and following repositioning to the supine position, (2) keeping the skin clean and moisturized, (3) repositioning to offload pressure points on the face and the body, (4) use of positioning devices, and (5) application of dressings, such as hydrocolloids, transparent film, and silicone, to decrease facial skin breakdown (51). Practical suggestions provided by Wounds International (52) include the need to (1) protect bony prominences on the front of the body prior to prone positioning, (2) lubricate the eyes and tape them closed, (3) select an appropriate mattress or an overlay, (4) ensure that the endotracheal tube securing devices are removed—the endotracheal tube should be secured with tapes with the help of a respiratory therapist, (5) ensure the use of liquid film-forming dressing such as SKIN-PREP to decrease trauma on removal, and (6) place the patient's face in swimmer's position when prone, i.e., turn the face to the side toward a flexed arm and put the other arm behind the patient. The swimmer's position allows movement of the head and the endotracheal tube (and a nasogastric tube) at the same time, which should be done every 2 h.
We have summarized the main points of PI prevention in patients in prone position in the infographic (Figure 1).
Finally, considering the pathophysiology of SARS-CoV-2 in relation to severe thrombosis (7, 8), patient repositioning as well as early mobilization should be prioritized. Specific guidelines with detailed instructions on how to prepare patients in prone position for care and how to reposition in the supine position are available for intensive care units (15, 53).
The patient's position and the duration in prone position need to be well-documented. Repositioning of unconscious patients into a prone position should be conducted by a team of at least four health professionals, following individual hospital policies, standard safety practices (37), and COVID-19 occupational safety guidelines. PI management relies on team work (37), and the assistance of other team members may be required (54), which should be arranged according to the risk mitigation strategies for health professionals (55).
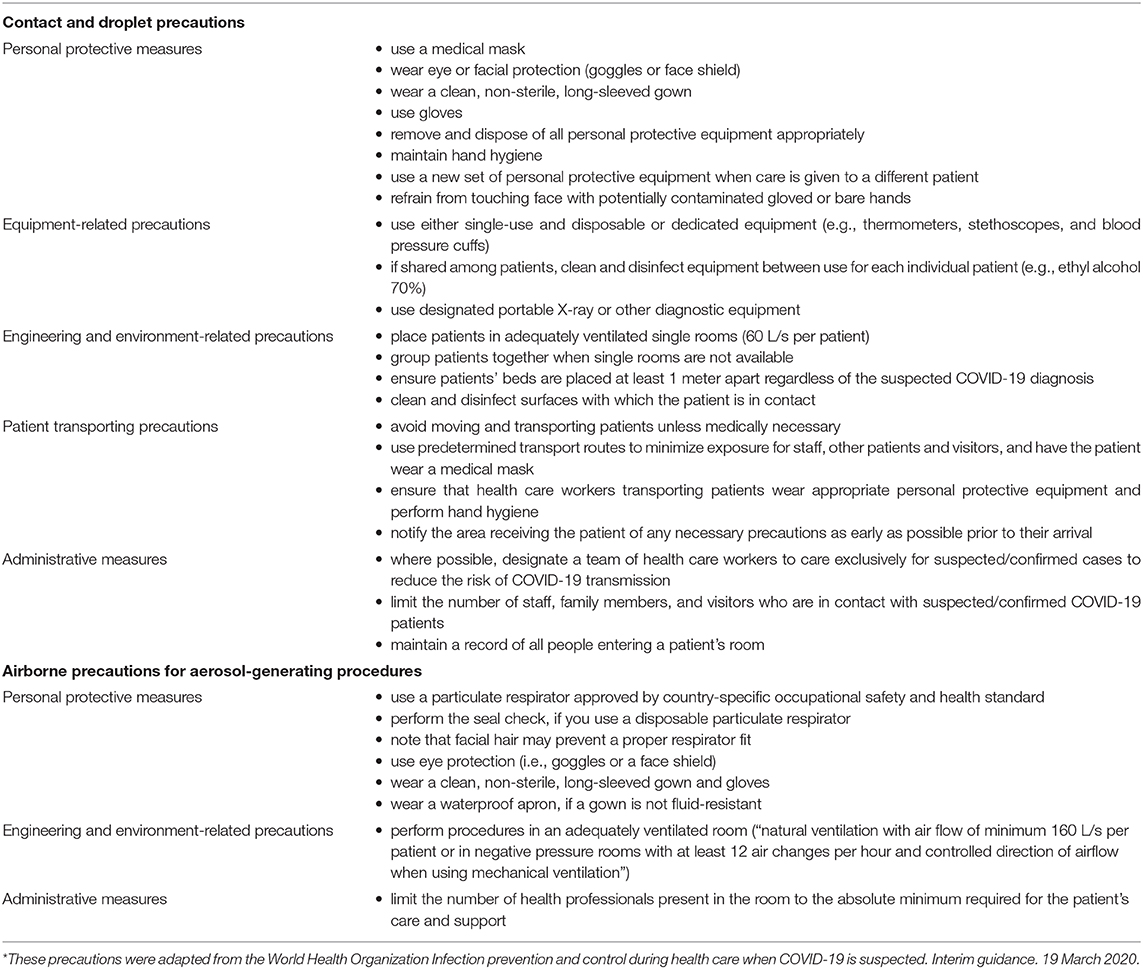
The main routes of occupational SARS-Cov-2 transmission for health professionals include droplets, airborne transmission, especially during invasive respiratory procedures, and contact transmission (26). In addition to standard measures, health professionals should apply contact and droplet precautions and airborne precautions for aerosol-generating procedures to mitigate the risk of SARS-Cov-2 transmission (56). The main risk mitigation strategies for health professionals (Table 1) include the need to be trained in fastidiously applying, wearing, and removing personal protective equipment, which prevents droplets, contact, and airborne transmission; to perform aerosol-generating procedures in a well-ventilated environment, preferably in a negative-pressure room; to allocate a team of healthcare workers to care exclusively for suspected/confirmed cases; and to limit the number of healthcare workers present in the room to the absolute minimum required for the patient's care and support (56).
Discussion
Prone positioning may be effective in the management of SARS-CoV-2 ARDS (10), although this position is associated with an increased risk of HAPI (28). HAPI is a well-known indicator of the quality of care in acute settings (57). Patient influx coupled with a shortage of nursing staff and related caregiver fatigue may influence the quality of care. Preventable PI in acute care can interfere with the patients' recovery, can increase hospital stay, and may contribute to death from PI complications, such us osteomyelitis and sepsis (58). Stages III and IV PI are frequently colonized with methicillin-resistant Staphylococcus aureus (59) and multi-resistant Gram-negative bacilli (60), which increase the risk of bacteremia (58) and associated mortality (61). We have discussed the main recommendations for PI prevention in COVID-related ARDS patients in prone position from the latest version of Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline, International Version (37) and included practical suggestions from the field. In summary, they include specific recommendations for the preparatory stage, care in prone position, and care after repositioning in supine position.
Prior to positioning patients in prone position, the main recommendations are to (1) conduct a skin assessment, (2) use pressure redistribution devices to offload pressure from bony prominences, (3) select an appropriate mattress or an overlay, (4) ensure that the endotracheal tube securing device is removed and that the endotracheal tube is secured with tapes, (5) use a liquid film-forming protective dressing, and (6) lubricate the eyes and tape them closed.
Once the patient is prone, it is recommended to (1) use the “swimmer's position,” i.e., turn the face on the side toward a flexed arm and put the other arm behind the patient, (2) reposition the patient every 2 h, i.e., turn the patient's face to the left and lift the left arm if their face was positioned to the right and their right hand was extended, and (3) keep the skin clean.
When the patient is repositioned to supine position, health care professionals are advised to (1) assess the pressure points and (2) promote early mobilization.
The management of PIs is costly to health systems (62–67). Studies show that PI prevention is more cost-effective than treatment (68). Prevention of HAPI in COVID-19 patients would help to avoid additional financial burden to an increasingly drained health system (69–71), particularly in countries significantly impacted by the COVID-19 outbreak (72). In order to preserve healthcare resources and to ensure adequate hospital capacity for the management of COVID-19 patients, many countries have deferred elective surgeries (73–77) and extended elective surgery waiting time. When the restrictions on elective surgeries are lifted, a sizable proportion of hospital beds might be occupied by COVID-19 patients requiring HAPI care if the preventive practices were suboptimal, given that patients with HAPIs have longer adjusted length of hospital stay (63). In addition to health system costs, there are extreme human costs associated with PI development (66), which further strengthens the importance of prevention of HAPIs in COVID-19 patients. Finally, the predicted second wave of COVID-19 cases (78), the lack of evidence on acquired immunity after COVID-19, and the risk of potential re-infection (79) in the absence of a COVID-19 vaccine (80) may result in increased hospital admissions, highlighting the need to speed up quality improvement in this field.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
VT and LT conducted the literature search and drafted the manuscript with support and guidance from CW, AJ, and HT. VT designed the infographic. All the authors critically reviewed and contributed to the individual parts of the manuscript and approved the final version.
Funding
The preparation of this article was supported by the Australian Government Department of Health Medical Research Future Fund.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors acknowledge the preprint of this article deposited in the OSF Preprints repository (78). All infographic images were licensed under the Creative Commons licenses. Walking is licensed under CC0 1.0, https://creativecommons.org/licenses/cc0/1.0/. Osha-facemask-blue.svg by j4p4n is licensed under CC0 1.0, http://creativecommons.org/ publicdomain/zero/1.0/deed.en. SARS-CoV-2 (Wikimedia colors).svg by Geraki is licensed under CC BY-SA 4.0, https://creativecommons.org/licenses/by-sa/4.0. Intensive Care—The Noun Project.svg by undefined is licensed under CC0 1.0, http://creativecommons.org/publicdomain/zero/1.0/deed.en. Prone position1.gif by Saltanat Ebli is licensed under CCO 1.0, https://creativecommons.org/publicdomain/zero/1.0/deed.en. Patient lies with stomach on the bed. Abdomen can be raised off the bed by Saltanat Ebli, CCO 1.0, https://creativecommons.org/publicdomain/zero/1.0/deed.en. 符号; creator: not available, CCO 1.0, https://creativecommons.org/publicdomain/zero/1.0/deed.en. Therapy; creator: not available, CCO 1.0, https://creativecommons.org/publicdomain/zero/1.0/deed.en.
References
1. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. (2020) 395:470–3. doi: 10.1016/S0140-6736(20)30185-9
2. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
3. Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032
4. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. doi: 10.1001/jama.2020.1585
5. Liu X, Zhou H, Zhou Y, Wu X, Zhao Y, Lu Y, et al. Risk factors associated with disease severity and length of hospital stay in COVID-19 patients. J Infect. (2020) 81:e95–7. doi: 10.1016/j.jinf.2020.04.008
6. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. (2020) 323:1545–6. doi: 10.1001/jama.2020.4031
7. Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. (2020) 220:1–13. doi: 10.1016/j.trsl.2020.04.007
8. Joly BS, Siguret V, Veyradier A. Understanding pathophysiology of hemostasis disorders in critically ill patients with COVID-19. Intensive Care Med. (2020) 46:1603–6. doi: 10.1007/s00134-020-06088-1
9. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. (2020) 395:1033. doi: 10.1016/S0140-6736(20)30628-0
10. Dondorp AM, Hayat M, Aryal D, Beane A, Schultz MJ. Respiratory support in novel coronavirus disease (COVID-19) patients, with a focus on resource-limited settings. Am J Trop Med Hyg. (2020) 102:1191–7. doi: 10.4269/ajtmh.20-0283
11. Odor PM, Neun M, Bampoe S, Clark S, Heaton D, Hoogenboom EM, et al. Anaesthesia and COVID-19: infection control. Br J Anaesth. (2020) 125:16–24. doi: 10.1016/j.bja.2020.03.025
12. Phua J, Weng L, Ling L, Egi M, Lim C-M, Divatia JV, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. (2020) 8:P506–17. doi: 10.1016/S2213-2600(20)30161-2
13. Meng L, Qiu H, Wan L, Ai Y, Xue Z, Guo Q, et al. Intubation and ventilation amid the COVID-19 outbreak: Wuhan's experience. Anesthesiology. (2020) 132:1317–32. doi: 10.1097/ALN.0000000000003296
14. Gattinoni L, Taccone P, Carlesso E, Marini JJ. Prone position in acute respiratory distress syndrome. Rationale, indications, and limits. Am J Resp Crit Care Med. (2013) 188:1286–93. doi: 10.1164/rccm.201308-1532CI
15. Burrell A, McLean L, Jones A, DiCocco K, Luff T. Prone Positioning for Hypoxic Respiratory Failure in ICU. Guideline. Melbourne, VIC: Alfred Health (2018).
16. Munshi L, Del Sorbo L, Adhikari NKJ, Hodgson CL, Wunsch H, Meade MO, et al. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thoracic Soc. (2017) 14:S280–8. doi: 10.1513/AnnalsATS.201704-343OT
17. Bloomfield R, Noble DW, Sudlow A. Prone position for acute respiratory failure in adults. Cochrane Database Syst Rev. (2015) 2015:CD008095. doi: 10.1002/14651858.CD008095.pub2
18. Sud S, Friedrich JO, Taccone P, Polli F, Adhikari NKJ, Latini R, et al. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta-analysis. Intensive Care Med. (2010) 36:585–99. doi: 10.1007/s00134-009-1748-1
19. Joynt GM, Editorial A. Severe Acute Respiratory Syndrome (SARS). Mech Ventilat. (2008) 61–6. doi: 10.1016/B978-0-7216-0186-1.50011-9
20. Al-Dorzi HM, Alsolamy S, Arabi YM. Critically ill patients with Middle East respiratory syndrome coronavirus infection. Crit Care. (2016) 20:65. doi: 10.1186/s13054-016-1234-4
21. Yang X, Yu Y, Xu J, Shu H, Xia Ja, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. (2020) 8:475–81. doi: 10.1016/S2213-2600(20)30079-5
22. Elharrar X, Trigui Y, Dols A-M, Touchon F, Martinez S, Prud'homme E, et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA. (2020) 323:2336–8. doi: 10.1001/jama.2020.8255
23. Caputo ND, Strayer RJ, Levitan R. Early self-proning in awake, non-intubated patients in the emergency department: a single ed's experience during the COVID-19 pandemic. Acad Emerg Med. (2020) 27:375–8. doi: 10.1111/acem.13994
24. Tolcher MC, McKinney JR, Eppes CS, Muigai D, Shamshirsaz A, Guntupalli KK, et al. Prone positioning for pregnant women with hypoxemia due to coronavirus disease 2019 (COVID-19). Obstetr Gynecol. (2020) 136:259–61. doi: 10.1097/AOG.0000000000004012
25. Miyamoto K, Yonemitsu T, Tanaka R, Nakashima T, Shibata M, Funahashi R, et al. Protracted course of coronavirus disease with severe acute respiratory distress syndrome: a case report. Acute Med Surg. (2020) 7:e521. doi: 10.1002/ams2.521
26. Bouadma L, Lescure F-X, Lucet J-C, Yazdanpanah Y, Timsit J-F. Severe SARS-CoV-2 infections: practical considerations and management strategy for intensivists. Intensive Care Med. (2020) 46:579–82. doi: 10.1007/s00134-020-05967-x
27. Scholten EL, Beitler JR, Prisk GK, Malhotra A. Treatment of ARDS with prone positioning. Chest. (2017) 151:215–24. doi: 10.1016/j.chest.2016.06.032
28. Guérin C. Prone positioning acute respiratory distress syndrome patients. Ann Transl Med. (2017) 5:289. doi: 10.21037/atm.2017.06.63
29. Girard R, Baboi L, Ayzac L, Richard J-C, Guérin C, Proseva trial group. The impact of patient positioning on pressure ulcers in patients with severe ARDS: results from a multicentre randomised controlled trial on prone positioning. Intens Care Med. (2014) 40:397–403. doi: 10.1007/s00134-013-3188-1
30. Cox J. Pressure injury risk factors in adult critical care patients: a review of the literature. Ostomy Wound Manag. (2017) 63:30–43.
31. Rondinelli J, Zuniga S, Kipnis P, Kawar LN, Liu V, Escobar GJ. Hospital-acquired pressure injury: risk-adjusted comparisons in an integrated healthcare delivery system. Nurs Res. (2018) 67:16–25. doi: 10.1097/NNR.0000000000000258
32. Zingarelli EM, Ghiglione M, Pesce M, Orejuela I, Scarrone S, Panizza R. Facial pressure ulcers in a COVID-19 50-year-old female intubated patient. Indian J Plastic Surg. (2020) 53:144–6. doi: 10.1055/s-0040-1710403
33. Lin L, Jiang X, Zhang Z, Huang S, Zhang Z, Fang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. (2020) 69:997–1001. doi: 10.1136/gutjnl-2020-321013
34. Jin X, Lian J-S, Hu J-H, Gao J, Zheng L, Zhang Y-M, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. (2020) 69:1002–9. doi: 10.1136/gutjnl-2020-320926
35. Tang J, Li B, Gong J, Li W, Yang J. Challenges in the management of critical ill COVID-19 patients with pressure ulcer. Int Wound J. (2020) 17:1523–4. doi: 10.1111/iwj.13399
36. Garnier-Crussard A, Forestier E, Gilbert T, Krolak-Salmon P. Novel coronavirus (COVID-19) epidemic: what are the risks for older patients? J Am Geriatr Soc. (2020) 68:939–40. doi: 10.1111/jgs.16407
37. European Pressure Ulcer Advisory Panel (EPUAP), National Pressure Injury Advisory Panel (NPIAP), Pan Pacific Pressure Injury Alliance (PPPIA). Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline. 3d ed. EPUAP, NPIAP and PPPIA (2019). Available online at: http://www.internationalguideline.com/static/pdfs/Quick_Reference_Guide-10Mar2019.pdf
38. Cheung JC-H, Ho LT, Cheng JV, Cham EYK, Lam KN. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med. (2020) 8:e19. doi: 10.1016/S2213-2600(20)30084-9
39. Khojastehfar S, Najafi Ghezeljeh T, Haghani S. Knowledge and attitude of intensive care nurses regarding the prevention of pressure ulcer. Iran J Nurs. (2019) 31:5–17. doi: 10.29252/ijn.31.116.5
40. Dalvand S, Ebadi A, Gheshlagh RG. Nurses' knowledge on pressure injury prevention: a systematic review and meta-analysis based on the Pressure Ulcer Knowledge Assessment Tool. Clin Cosmet Investig Dermatol. (2018) 11:613–20. doi: 10.2147/CCID.S186381
41. De Meyer D, Verhaeghe S, Van Hecke A, Beeckman D. Knowledge of nurses and nursing assistants about pressure ulcer prevention: A survey in 16 Belgian hospitals using the PUKAT 2.0 tool. J Tissue Viabil. (2019) 28:59–69. doi: 10.1016/j.jtv.2019.03.002
42. Fulbrook P, Lawrence P, Miles S. Australian nurses' knowledge of pressure injury prevention and management: a cross-sectional survey. J Wound Ostomy Continence Nurs. (2019) 46:106–12. doi: 10.1097/WON.0000000000000508
43. Miller DM, Neelon L, Kish-Smith K, Whitney L, Burant CJ. Pressure injury knowledge in critical care nurses. J Wound Ostomy Continence Nurs. (2017) 44:455–7. doi: 10.1097/WON.0000000000000350
44. Charalambous C, Koulouri A, Roupa Z, Vasilopoulos A, Kyriakou M, Vasiliou M. Knowledge and attitudes of nurses in a major public hospital in Cyprus towards pressure ulcer prevention. J Tissue Viabil. (2019) 28:40–5. doi: 10.1016/j.jtv.2018.10.005
45. Ebi WE, Hirko GF, Mijena DA. Nurses' knowledge to pressure ulcer prevention in public hospitals in Wollega: a cross-sectional study design. BMC Nurs. (2019) 18:20. doi: 10.1186/s12912-019-0346-y
46. Hoviattalab K, Hashemizadeh H, D'Cruz G, Halfens RJ, Dassen T. Nursing practice in the prevention of pressure ulcers: an observational study of G erman H ospitals. J Clin Nurs. (2015) 24:1513–24. doi: 10.1111/jocn.12723
47. Law AC, Forbath N, O'Donoghue S, Stevens JP, Walkey AJ. Hospital-level availability of prone positioning in Massachusetts ICUs. Am J Respir Crit Care Med. (2020) 201:1006–8. doi: 10.1164/rccm.201910-2097LE
48. Grisell M, Place HM. Face tissue pressure in prone positioning: a comparison of three face pillows while in the prone position for spinal surgery. Spine. (2008) 33:2938–41. doi: 10.1097/BRS.0b013e31818b9029
49. Romero CM, Cornejo RA, Gálvez LR, Llanos OP, Tobar EA, Berasaín MA, et al. Extended prone position ventilation in severe acute respiratory distress syndrome: a pilot feasibility study. J Crit Care. (2009) 24:81–8. doi: 10.1016/j.jcrc.2008.02.005
50. Wu T, Wang S-T, Lin P-C, Liu C-L, Chao Y-FC. Effects of using a high-density foam pad versus a viscoelastic polymer pad on the incidence of pressure ulcer development during spinal surgery. Biol Res Nurs. (2010) 13:419–24. doi: 10.1177/1099800410392772
51. Moore Z, Patton D, Avsar P, McEvoy NL, Curley G, Budri A, et al. Prevention of pressure ulcers among individuals cared for in the prone position: lessons for the COVID-19 emergency. J Wound Care. (2020) 29:312–20. doi: 10.12968/jowc.2020.29.6.312
52. Black J. COVID-19 and Tips for Safe Skin and Proning: What Should Skin Care Involve for Patients in the Prone Position? Wounds International TV. Available online at: https://woundsinternationaltv.com/editors-chioce/covid-19-and-tips-for-safe-skin-and-proning/?_cldee=Y2Fyb2xpbmEud2VsbGVyQG1vbmFzaC5lZHU%3d&recipientid=contact-02554ddf6fd8e911a812000d3a7ed483-61c7c45c041942b98c48dc9b35475faa&esid=f125779b-b4ac-ea11-a812-000d3a7ed30d (2020).
53. Schub E, Pilgrim J. Patient Positioning (Critical Care Patients): Prone. Nursing Practice and Skill. Glendale, CA: Cinahl Information Systems (2018).
54. Lazzeri M, Lanza A, Bellini R, Bellofiore A, Cecchetto S, Colombo A, et al. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR). Monaldi Arch Chest Dis. (2020) 90:163–8. doi: 10.4081/monaldi.2020.1285
55. World Health Organization. Health Workers Exposure Risk Assessment and manAgement in the Context of COVID-19 Virus. Interim Guidance March 4, 2020. WHO/2019-nCov/HCW_risk_assessment/2020.1 (2020). Available online at: https://apps.who.int/iris/handle/10665/331340. WHO
56. World Health Organization. Infection Prevention and Control During Health Care When COVID-19 Is Suspected Interim Guidance 19 March, 2020. WHO/2019-nCoV/IPC/2020.3 (2020). Available online at: https://www.who.int/publications/i/item/10665-331495
57. Weller CD, Gershenzon ER, Evans SM, Team V, McNeil JJ. Pressure injury identification, measurement, coding, and reporting: key challenges and opportunities. Int Wound J. (2018) 15:417–23. doi: 10.1111/iwj.12879
58. Espejo E, Andrés M, Borrallo R-M, Padilla E, Garcia-Restoy E, Bella F, et al. Bacteremia associated with pressure ulcers: a prospective cohort study. Eur J Clin Microbiol Infect Dis. (2018) 37:969–75. doi: 10.1007/s10096-018-3216-8
59. Gurusamy KS, Koti R, Toon CD, Wilson P, Davidson BR. Antibiotic therapy for the treatment of methicillin-resistant Staphylococcus aureus (MRSA) in non surgical wounds. Cochrane Database Syst Rev. (2013) 2013:Cd010427. doi: 10.1002/14651858.CD009726.pub2
60. Braga IA, Brito CS, Filho AD, Filho PPG, Ribas RM. Pressure ulcer as a reservoir of multiresistant Gram-negative bacilli: risk factors for colonization and development of bacteremia. Braz J Infect Dis. (2017) 21:171–5. doi: 10.1016/j.bjid.2016.11.007
61. Ortwine JK, Bhavan K. Morbidity, mortality, and management of methicillin-resistant S. aureus bacteremia in the USA: update on antibacterial choices and understanding. Hosp Pract. (2018) 46:64–72. doi: 10.1080/21548331.2018.1435128
62. Padula WV, Delarmente BA. The national cost of hospital-acquired pressure injuries in the United States. Int Wound J. (2019) 16:634–40. doi: 10.1111/iwj.13071
63. Dreyfus J, Gayle J, Trueman P, Delhougne G, Siddiqui A. Assessment of risk factors associated with hospital-acquired pressure injuries and impact on health care utilization and cost outcomes in US hospitals. Am J Med Qual. (2017) 33:348–58. doi: 10.1177/1062860617746741
64. Nguyen K-H, Chaboyer W, Whitty JA. Pressure injury in Australian public hospitals: a cost-of-illness study. Aust Health Rev. (2015) 39:329–36. doi: 10.1071/AH14088
65. Nussbaum SR, Carter MJ, Fife CE, DaVanzo J, Haught R, Nusgart M, et al. An economic evaluation of the impact, cost, and medicare policy implications of chronic nonhealing wounds. Value Health. (2018) 21:27–32. doi: 10.1016/j.jval.2017.07.007
66. Olsson M, Järbrink K, Divakar U, Bajpai R, Upton Z, Schmidtchen A, et al. The humanistic and economic burden of chronic wounds: a systematic review. Wound Repair Regener. (2019) 27:114–25. doi: 10.1111/wrr.12683
67. Zarei E, Madarshahian E, Nikkhah A, Khodakarim S. Incidence of pressure ulcers in intensive care units and direct costs of treatment: evidence from Iran. J Tissue Viabil. (2019) 28:70–4. doi: 10.1016/j.jtv.2019.02.001
68. Padula WV, Pronovost PJ, Makic MBF, Wald HL, Moran D, Mishra MK, et al. Value of hospital resources for effective pressure injury prevention: a cost-effectiveness analysis. BMJ Qual Saf. (2019) 28:132. doi: 10.1136/bmjqs-2017-007505
69. Bartsch SM, Ferguson MC, McKinnell JA, O'Shea KJ, Wedlock PT, Siegmund SS, et al. The potential health care costs and resource use associated with COVID-19 in the United States. Health Affairs. (2020) 39:927–35. doi: 10.1377/hlthaff.2020.00426
70. Colenda CC, Applegate WB, Reifler BV, Blazer DG II. COVID-19: financial stress test for academic medical centers. Acad Med. (2020) 95:1143–5. doi: 10.1097/ACM.0000000000003418
71. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. (2020) 395:1225–28. doi: 10.1016/S0140-6736(20)30627-9
72. McKibbin WJ, Fernando R. The global macroeconomic impacts of COVID-19: seven scenarios. In: CAMA Working Paper No. 19/2020 (2020). Available online at: https://ssrn.com/abstract=3547729
73. Jean WC, Ironside NT, Sack KD, Felbaum DR, Syed HR. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir. (2020) 162:1229–40. doi: 10.1007/s00701-020-04342-5
74. Topf MC, Shenson JA, Holsinger FC, Wald SH, Cianfichi LJ, Rosenthal EL, et al. A framework for prioritizing head and neck surgery during the COVID-19 pandemic. Head Neck. (2020) 42:1159–67. doi: 10.1002/hed.26184
75. Zoia C, Bongetta D, Veiceschi P, Cenzato M, Di Meco F, Locatelli D, et al. Neurosurgery during the COVID-19 pandemic: update from Lombardy, northern Italy. Acta Neurochir. (2020) 162:1221–2. doi: 10.1007/s00701-020-04305-w
76. Zaman S, MacIsaac AI, Jennings GLR, Schlaich M, Inglis SC, Arnold R, et al. Cardiovascular disease and COVID-19: Australian/New Zealand consensus statement. Med J Aust. (2020) 1. doi: 10.5694/mja2.50714
77. Tuech JJ, Gangloff A, Di Fiore F, Michel P, Brigand C, Slim K, et al. Strategy for the practice of digestive and oncological surgery during the Covid-19 epidemic. J Visceral Surg. (2020) 157:S7–12. doi: 10.1016/j.jviscsurg.2020.03.008
78. Xu S, Li Y. Beware of the second wave of COVID-19. Lancet. (2020) 395:1321–2. doi: 10.1016/S0140-6736(20)30845-X
79. World Health Organization. “Immunity Passports” in the Context of COVID-19. Scientific Brief 24 April, 2020 (2020). Available online at: https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19
Keywords: acute respiratory distress syndrome, COVID-19, guidelines, intensive care, pressure injury, pressure points, prone positioning, ventilation
Citation: Team V, Team L, Jones A, Teede H and Weller CD (2021) Pressure Injury Prevention in COVID-19 Patients With Acute Respiratory Distress Syndrome. Front. Med. 7:558696. doi: 10.3389/fmed.2020.558696
Received: 03 May 2020; Accepted: 02 December 2020;
Published: 22 January 2021.
Edited by:
Ata Murat Kaynar, University of Pittsburgh, United StatesReviewed by:
Eizo Watanabe, Chiba University, JapanReed F. Johnson, National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIH), United States
Copyright © 2021 Team, Team, Jones, Teede and Weller. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Victoria Team, dmljdG9yaWEudGVhbUBtb25hc2guZWR1
 Victoria Team
Victoria Team Lydia Team
Lydia Team Angela Jones
Angela Jones Helena Teede
Helena Teede Carolina D. Weller
Carolina D. Weller