- 1Department of Rheumatology, University College London Hospital, London, United Kingdom
- 2Division of Medicine, Department of Rheumatology, University College London, London, United Kingdom
- 3Department of Respiratory Medicine, University College London Hospital, London, United Kingdom
- 4Leukocyte Trafficking Laboratory, Centre for Inflammation and Tissue Repair, UCL Respiratory, University College London, London, United Kingdom
Pulmonary manifestations of systemic lupus erythematosus (SLE) are wide-ranging and debilitating in nature. Previous studies suggest that anywhere between 20 and 90% of patients with SLE will be troubled by some form of respiratory involvement throughout the course of their disease. This can include disorders of the lung parenchyma (such as interstitial lung disease and acute pneumonitis), pleura (resulting in pleurisy and pleural effusion), and pulmonary vasculature [including pulmonary arterial hypertension (PAH), pulmonary embolic disease, and pulmonary vasculitis], whilst shrinking lung syndrome is a rare complication of the disease. Furthermore, the risks of respiratory infection (which often mimic acute pulmonary manifestations of SLE) are increased by the immunosuppressive treatment that is routinely used in the management of lupus. Although these conditions commonly present with a combination of dyspnea, cough and chest pain, it is important to consider that some patients may be asymptomatic with the only suggestion of the respiratory disorder being found incidentally on thoracic imaging or pulmonary function tests. Treatment decisions are often based upon evidence from case reports or small cases series given the paucity of clinical trial data specifically focused on pulmonary manifestations of SLE. Many therapeutic options are often initiated based on studies in severe manifestations of SLE affecting other organ systems or from experience drawn from the use of these therapeutics in the pulmonary manifestations of other systemic autoimmune rheumatic diseases. In this review, we describe the key features of the pulmonary manifestations of SLE and approaches to investigation and management in clinical practice.
Introduction
Systemic lupus erythematosus (SLE) is a chronic, autoimmune disorder that can present with a wide array of clinical and immunological abnormalities (1). Pulmonary manifestations of the disease include disorders of the lung parenchyma, pleura, and pulmonary vasculature. Furthermore, some SLE therapies predispose to an increased risk of respiratory infections (2).
Clinical assessment of patients with SLE should routinely consider careful evaluation for respiratory involvement. Symptoms including dyspnea, pleuritic chest pain, reduced exercise tolerance, cough, and hemoptysis should prompt investigation for potential underlying lung disease (3, 4). However, it is important to consider that some asymptomatic patients may also present with incidental findings of abnormal chest imaging or lung function tests in the absence of overt respiratory symptoms (5). It is also important to consider whether these symptoms are occurring in the context of active SLE involving other organ systems. Serological evidence of increased disease activity including elevated erythrocyte sedimentation rate (ESR), low complement, and increased double-stranded DNA (dsDNA) antibody titers should also prompt the clinician to consider whether new respiratory symptoms are directly attributed to lupus.
The exact prevalence of SLE-related lung disease is unknown and previous studies have varied widely in their estimates. Most report that between 20 and 90% of SLE patients will experience some form of lung involvement during the course of their disease (6, 7). However, more recently it has been suggested that this figure lies between the range of 50–70% (8). Predictors for progression to earlier permanent lung damage, include older age and those positive for anti-RNP antibodies (9). Pulmonary manifestations of SLE are associated with a higher mortality rate (10) and this varies depending upon the exact type and extent of lung involvement seen. More chronic forms of lung disease relating to SLE can have a significant negative affect on patient wellbeing, physical performance status, and are detrimental to quality of life (11).
In this review, we discuss the latest understanding on the ways in which lupus can affect the respiratory system, highlight how these patients may present clinically, and outline current approaches for investigation and management.
Diseases of the Lung Parenchyma
Interstitial Lung Disease (ILD)
The estimated prevalence of SLE-associated interstitial lung diseases (ILD) is suggested to be between 3 and 9% (12, 13). Although ILD is highly prevalent in rheumatoid arthritis and other systemic autoimmune rheumatic diseases (such as scleroderma and anti-synthetase syndrome), it is relatively uncommon in SLE (8). A small study previously reported that clinical progression of ILD in SLE is slow and often stabilizes over time (12). Risk factors for developing SLE-associated ILD include longstanding disease, older age and overlapping clinical features with scleroderma such as Raynaud's phenomenon and sclerodactyly (14–17). Various forms of ILD have been described in SLE including non-specific interstitial pneumonia (NSIP), organizing pneumonia, lymphocytic interstitial pneumonia, follicular bronchitis, and usual interstitial pneumonia (18–21). Bronchiolitis obliterans has also been reported as an initial manifestation of SLE (19).
Patients present similarly in most types of ILD with symptoms such as cough and dyspnea although it is important to consider that some may be asymptomatic (22). Diagnosis of SLE-associated ILD can be made with high resolution computed tomography (HRCT) and excluding other potential causes of ILD (such as screening for overlap disorders by measuring rheumatoid factor, serum muscle enzymes, an extended myositis panel and anti-centromere autoantibodies) (23). Checking extractable nuclear antigens (ENA) should also be considered as previous studies have demonstrated that patients with anti-La, anti-Scl-70 and anti-U1RNP antibodies were more likely to develop ILD. Interestingly, anti-dsDNA antibody titer do no associate with the development of ILD (24). Lung function tests may show a restrictive pattern of disease and a decrease in diffusing capacity for carbon monoxide (DLCO) (8). Histological studies have reported the presence of lymphocytic and mononuclear interstitial and peribronchiolar infiltrates in biopsies taken from those with SLE-related NSIP (25).
There are a lack of clinical trials assessing the treatment of SLE-related ILD and in particular there are no head-to-head studies. Therefore, recommendations are predominantly based on case reports, small case series, physician expertise, and by applying findings from studies of ILD in other autoimmune rheumatic diseases. Intravenous cyclophosphamide was reported to show significant improvement vital capacity in two SLE patients with ILD in which both patients presented with pleuritic chest pain in the context of active SLE (26). Another case report noted that oral methotrexate resulted in a marked improvement in lung function in a patient with SLE-related ILD (27). An observational study of 14 patients with SLE-associated ILD reported that three patients showed significant improvement with high dose oral steroids (60 mg prednisolone daily for a minimum of 4 weeks). Six of the 14 patients had an improvement in respiratory symptoms and all were treated with systemic steroids (18). Three patients within the cohort died, two of pulmonary fibrosis, and one from infection thus highlighting the clinical challenge posed by immunosuppressive therapy in the context of SLE-related ILD. It is important to consider that this study was published in 1990 and thus predates a number of the newer treatments available for the management of SLE, such as mycophenolate mofetil (MMF), rituximab and belimumab.
Current treatment often includes the use of high dose corticosteroids along with agents such as cyclophosphamide and rituximab in severe cases (28, 29) to induce remission. Steroid-sparing agents such as MMF and azathioprine may be used in milder cases or in maintaining long-term control of the disease (30, 31).
Acute Lupus Pneumonitis
In some cases, chronic ILD may be the long-term sequelae of an acute process, for example acute lupus pneumonitis. This is a rare manifestation of SLE that has been reported to occur in 1–4% of patients (32). Clinically, acute lupus pneumonitis presents in the context of a systemic flare of SLE in addition to dyspnea, cough (including hemoptysis) and pleuritic chest pain. Fever is commonly associated with the acute presentation, thus making it a clinical challenge to differentiate from infection. There is limited data on lung histology in acute lupus pneumonitis, although reports of lymphocytic infiltrates and alveolar damage with associated interstitial edema have been reported in both lung biopsy samples and at post-mortem assessment (24).
Acute lupus pneumonitis may also be the initial presenting symptom of SLE. A case series of five patients in which acute lupus pneumonitis was the first feature of SLE reported that all five were female, aged 14–26 years old. They were all ANA positive, whilst three were also positive for anti-dsDNA antibodies. Fever was present in all cases with cough as a presenting symptom in four of the five patients, with hypoxia noted in three. All patients received corticosteroids and four patients were treated with cyclophosphamide either as monotherapy or in combination with intravenous immunoglobulins (IVIg). The one patient who did not receive cyclophosphamide was treated with azathioprine. Three patients survived but two died as a result of infection (33). Others have also reported the use of IVIg in acute lupus pneumonitis (34, 35). Given that the differential diagnosis in this presentation often includes bacterial pneumonia, and as infection can commonly co-exist with acute lupus pneumonitis, IVIg represents a useful option as it does not convey the high risk of immunosuppression associated with other agents. It is also important to consider using broad spectrum antibiotics (in particular directed against encapsulated organisms) if there are concerns about intercurrent infection. Further, prompt initiation of systemic glucocorticoid therapy has been reported to be of benefit in reducing mortality rates. Additional treatments that have been used in the management of acute lupus pneumonitis are similar to those used in SLE-related ILD, such as high dose glucocorticoids in combination with either MMF, azathioprine, rituximab, or cyclophosphamide. However, in spite of this the outcomes are often poor with associated high mortality rates (33, 36).
Pleural Disease
Pleural involvement is the most common SLE-related lung disease (37). Clinically, patients often present with pleuritic chest pain, cough and dyspnea due to inflammation of the pleura (38). Patients may have an associated pleural effusion which is often bilateral and exudative in nature (39, 40). Estimates suggest that between 30 and 50% of SLE patients will develop a pleural effusion at some point during their disease course, although often these are small and may not result in obvious symptoms (39, 41).
Diagnosis of pleural involvement in SLE is usually clinical with typical features in the patient history. It is however important to exclude other causes of pleural inflammation that can occur in SLE including infection, pulmonary embolism, malignancy, congestive cardiac failure (37), or pericarditis, which may present in a similar manner. Drug-induced pleuritis from agents such as hydralazine, procainamide and anti-tumor necrosis factor-alpha medications should also be considered (42–44). In such cases, drug cessation is often sufficient to resolve symptoms.
Although not necessary for diagnosis, if there is clinical uncertainty as to the cause of a pleural effusion, aspiration can be performed. Pleural fluid in patients with SLE classically show elevated levels of protein, lactate dehydrogenase (LDH), leukocytes, and in some cases ANA positivity (37, 39).
The mainstay treatment of pleurisy in SLE has traditionally been non-steroidal anti-inflammatory drugs (NSAIDs) with some patients requiring corticosteroids (38). Rarely, other steroid-sparing agents such as azathioprine, methotrexate, cyclosporine, and cyclophosphamide may be indicated (37). In refractory disease, there have been cases showing effective use of pleurodesis (45, 46).
Disorders of the Pulmonary Vasculature
Pulmonary Arterial Hypertension (PAH)
Pulmonary arterial hypertension (PAH) is a progressive disorder characterized by a resting mean pulmonary artery pressure above 25 mmHg and a pulmonary wedge pressure below 15 mmHg (47). There are a number of possible underlying causes that may result in PAH in SLE, including left ventricular dysfunction or congestive cardiac failure that may be a result of the increased risk of atherosclerosis associated with SLE. It may also be a manifestation of the long-term sequelae of parenchymal lung diseases (such as ILD) or chronic thromboembolic disease (48). Studies estimate the prevalence of PAH in SLE to be in the range of 1–43% depending on the cohort (49–54). A recent comprehensive meta-analysis assessing the prevalence of PAH found an estimated pooled prevalence of 8% (55). Despite this, severe PAH is thought to be a rare manifestation in SLE and is not included in the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) disease activity score (56).
Clinical symptoms of PAH in SLE are often non-specific and range from generalized fatigue and weakness to chest pain and dyspnea at rest (48). Initial investigations often include an electrocardiogram that may show right ventricular hypertrophy and right axis deviation. Radiographic imaging with computerized tomography may be used to exclude other diseases such as ILD and will often show enlarged pulmonary vessels (57). Echocardiography can estimate systolic pulmonary artery pressure and is therefore a vital non-invasive tool to assist in making a diagnosis. However, even with a suggestive echocardiogram result and high clinical suspicion, right heart catheterization remains the “gold standard” test to confirm the diagnosis (58).
Management of PAH in SLE is similar to that of idiopathic PAH. However, most randomized controlled trials that have specifically analyzed the management of PAH associated with connective tissue diseases often have not included a subgroup analysis of SLE patients (48). Drugs such as phosphodiesterase-5 inhibitors, endothelin receptor antagonists and prostacyclin pathway agonists have all shown to be effective in SLE associated PAH to varying degrees (59–64). More recently, the guanylate cyclase stimulator riociguat has shown to be effective in a small number of SLE-associated PAH cases (65, 66).
Numerous observational cohort studies have also noted benefit with corticosteroids and immunosuppressive therapy including cyclophosphamide, cyclosporine and MMF (67–70). One case report has also described effective use of rituximab in refractory SLE-associated PAH (71). Overall, it is generally thought that a combination of both immunosuppression and traditional PAH treatment should be used together to enhance long-term outcomes (68).
Pulmonary Embolic Disease
Pulmonary embolism (PE) also needs to be considered in the acute setting in any patient with SLE who presents with pleuritic chest pain (especially if associated with acute hypoxia). In the more chronic setting, chronic pulmonary embolic disease can also lead to pulmonary hypertension (chronic thromboembolic pulmonary hypertension). It is particularly important to consider embolic disease in those patients who have secondary anti-phospholipid syndrome (APS), given the obvious increased risk of thrombosis associated with the disease. Previous studies have reported that one-third of patients with SLE will have positive anti-phospholipid antibodies and those with a positive lupus anticoagulant have previously been shown to have a six-fold increased risk of venous thrombosis. In comparison, a positive anti-cardiolipin antibody carried twice the risk when compared with SLE patients without positive anti-cardiolipin antibodies (72). Previous studies have also reported that patients with SLE, even in the absence of APS, are at an increased risk of unprovoked PE when compared with the general population and therefore the absence of positive anti-phospholipid serology should not be falsely reassuring.
The “gold standard” investigation for PE is computed topography pulmonary angiogram (CTPA), which can identify the presence of thrombosis within the pulmonary vasculature. However, it is important to consider that SLE patients presenting with pleuritic chest pain and hypoxia may instead be suffering from pleurisy (as described above). Results from the Michigan Lupus Cohort assessed the outcomes of 182 patients with SLE who had previously undergone a total of 357 CTPA scans. The authors found a significant decrease in the likelihood of confirming PE in patients who had previously had three or more scans, thus suggesting that repeated scanning of patients without a previously proven PE is unlikely to confirm a new diagnosis (73).
In the context of PE associated with APS, lifelong anticoagulation is likely to be recommended. Recent studies investigating direct oral anticoagulants have recommended against their use in arterial thrombosis, such as PE (74).
Pulmonary Vasculitis and Pulmonary Hemorrhage
Pulmonary vasculitis, or diffuse alveolar hemorrhage (DAH), is a rare but severe manifestation of SLE that is associated with a high mortality rate of up to 90% (75). This has been reported to affect <5% of patients with SLE and is more commonly seen concurrently in the context of active lupus nephritis (76). In addition, this manifestation has been reported to be the initial presentation of SLE in ~20% of all cases, which means that it is important to consider lupus in any new case of pulmonary hemorrhage in which an alternate underlying cause is not present (77). It has also been reported that patients with secondary APS may be at increased risk of DAH and that this may also occur de novo in patients with SLE who are have anti-phospholipid antibodies without previous thrombotic events. This suggests that this is not entirely the result of anticoagulant therapy and may represent an as yet unclassified mechanism for pulmonary vasculitis (78). As with other acute pulmonary manifestations of SLE, the symptoms can often mimic infection thus making the diagnosis a challenge.
Findings from small cases series and cohort studies have highlighted that dyspnea and pulmonary infiltrates on thoracic imaging are almost universally in seen. Fever is reported in the majority of cases although occult hemoptysis is only seen in just over half of patients at presentation (79). Many patients will also present with extrapulmonary manifestations of SLE to suggest a generalized systemic flare of the disease. More subtle signs that suggest DAH include pleural effusions and anemia is seen in nearly all cases, and may be present before signs such as hemoptysis are observed (75, 80). Imaging studies often describe classical bilateral alveolar interstitial infiltrates. Many patients are deemed clinically unstable for further dedicated investigation however those that proceed to bronchoscopy are usually found to have high neutrophil count, low lymphocyte count and hemosiderin-laden macrophages within the lavage and occult blood often seen (79, 81). If the patient is able to tolerate pulmonary function tests then an elevated DLCO is usually indicative of alveolar hemorrhage.
Given a lack of clinical trial data from DAH in SLE, treatment recommendations are usually based upon other autoimmune conditions associated with pulmonary hemorrhage (such as ANCA-associated vasculitis) and often include pulsed intravenous steroids in combination with cyclophosphamide (79), rituximab, plasmapheresis, and IVIg (81, 82).
Shrinking Lung Syndrome (SLS)
Shrinking lung syndrome (SLS) is an uncommon manifestation of SLE with an estimated prevalence of ~1–2% (9, 83, 84). The exact cause of SLS is unclear, however it is believed to involve abnormal diaphragmatic strength and may be related to due to impaired phrenic nerve signaling (85).
Patients with SLS often present with symptoms of pleuritic chest pain and progressive dyspnea (86). Due to its rarity, there is no diagnostic criteria for SLS. Lung function tests often show a restrictive defect with a reduction in lung volume and DLCO (84). Radiographic imaging in SLS is often non-specific with occasional elevation of the diaphragm and basal atelectasis with usually no evidence of interstitial lung or pleural disease (87). It is also important to consider other conditions before a diagnosis of SLS is made including central nervous system disorders and diaphragmatic palsies (88).
Evidence for the optimal management of SLS is limited. Corticosteroids and immunosuppressive agents including azathioprine, MMF and rituximab have been used to varying degrees of efficacy (86, 89–92). Some have suggested the use of hematopoietic cell transplantation (93) and beta agonist therapy (94) in SLS. Others have reported some benefit in the use of theophylline thought to be helpful by improving diaphragmatic strength (87, 95). Comprehensive studies have generally shown a good prognosis with treatment in most SLS patients (87, 88).
Conclusions
Pulmonary manifestations of SLE can present with a wide array of symptoms and can often be difficult to differentiate from other conditions, most notably infection. The key differences between these disorders are summarized in Table 1.
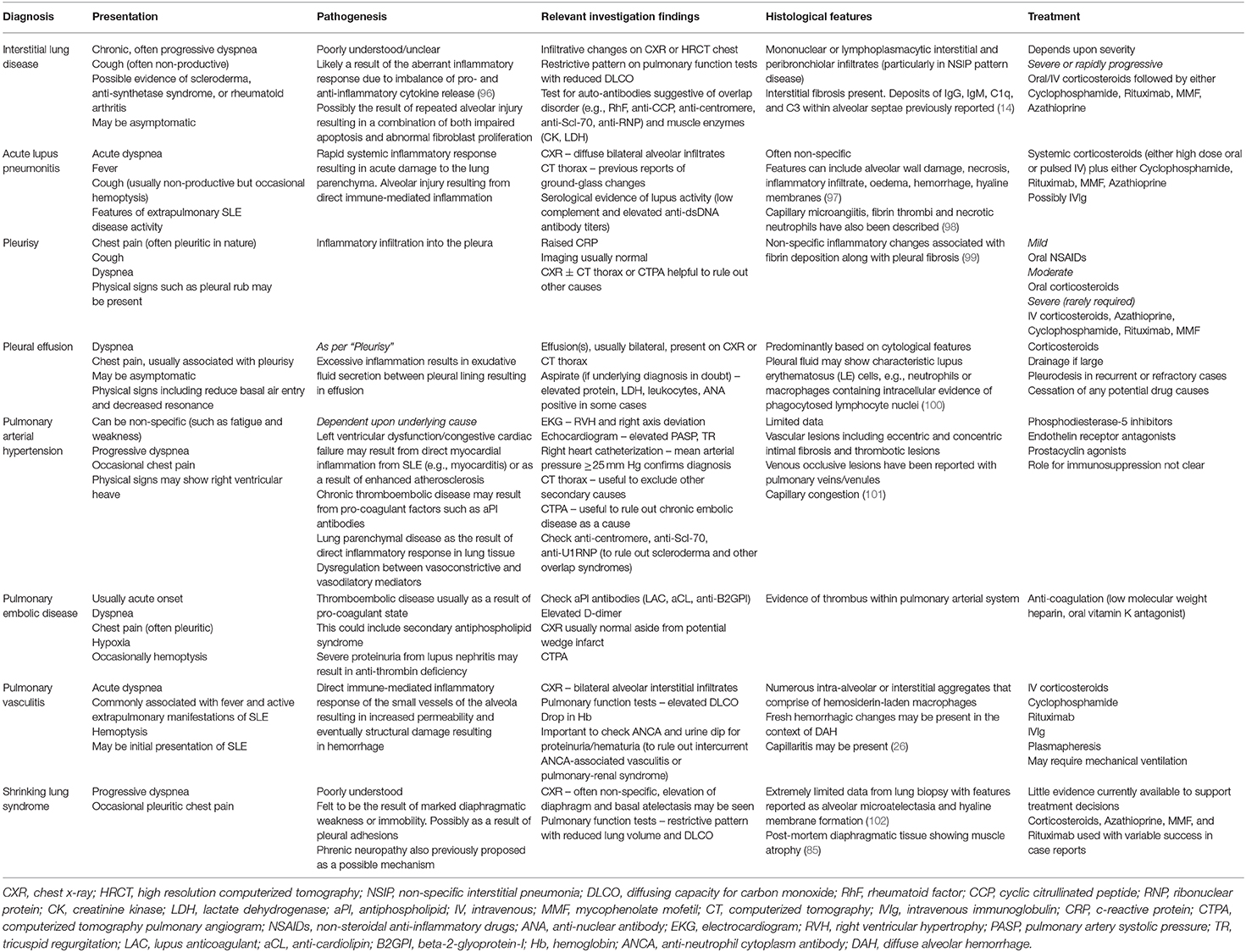
Table 1. A summary of the way in which pulmonary manifestations of systemic lupus erythematosus (SLE) may present in clinical practice, the underlying pathogenesis and relevant treatment options.
It is important to consider that SLE-related lung disorders are likely to be under-represented due to the fact that respiratory involvement may be asymptomatic. Furthermore, serositis (pleurisy/pleural effusion) is the only respiratory symptom included in the revised 1997 American College of Rheumatology (ACR) criteria for SLE (103) and no additional respiratory manifestations were included in the 2019 combined ACR/EULAR criteria (104). In terms of measuring disease activity from pulmonary manifestations of SLE, the British Isles Lupus Assessment Group (BILAG) index includes a subsection on (cardio)respiratory features of the disease, which considers pleurisy, pleural effusion, pulmonary hemorrhage/vasculitis, interstitial lung disease, and shrinking lung syndrome as possible pulmonary manifestations of the disease (105). In comparison, the SLEDAI-2K only accounts for pleurisy as a scorable item of lupus activity involving the lungs (106). In turn, this may result in a number of patients with respiratory complications of SLE (particularly those symptoms considered more mild) to be falsely considered as either in remission or a low disease activity state (107). In comparison, the Systemic Lupus International Collaborating Clinics (SLICC)/ACR Damage Index for SLE does include a wide array of pulmonary manifestations although these are typically irreversible and thus may not be a useful measure in preventative studies (108). This has important implications for clinical trial design, which may exclude patients who have predominantly respiratory symptoms. As a result, evidence supporting therapeutic options in SLE-related lung disease are often extrapolated from other severe manifestations of the disease. Dedicated studies in the management of pulmonary disorders in SLE are greatly needed and represent a major unmet need.
Author Contributions
RA conducted a literature review of relevant respiratory disorders. SAY, EKD, and CW expanded upon this. All authors agreed to the finalized version of this manuscript prior to submission.
Funding
SAY was funded by the Royal College of Physicians, Rosetrees Trust, NIHR University College London Hospitals Biomedical Research Centre and UCLH Charities. EKD was funded by the Breathing Matters Charity and the NIHR University College London Hospital Biomedical Research Centre. CW was funded by Versus Arthritis (ref 21992).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
CW would like to acknowledge the support he receives from Versus Arthritis and LUPUS UK.
References
1. Bakshi J, Segura BT, Wincup C, Rahman A. Unmet needs in the pathogenesis and treatment of systemic lupus erythematosus. Clin Rev Allergy Immunol. (2018) 55:352–67. doi: 10.1007/s12016-017-8640-5
2. Cuchacovich R, Gedalia A. Pathophysiology and clinical spectrum of infections in systemic lupus erythematosus. Rheum Dis Clin North Am. (2009) 35:75–93. doi: 10.1016/j.rdc.2009.03.003
3. Alamoudi OSB, Attar SM. Pulmonary manifestations in systemic lupus erythematosus: association with disease activity. Respirology. (2015) 20:474–80. doi: 10.1111/resp.12473
4. Hellman DB, Kirsch CM, Whiting-O'Keefe Q, Simonson J, Schiller NB, Petri M, et al. Dyspnea in ambulatory patients with SLE: prevalence, severity, and correlation with incremental exercise testing. J Rheumatol. (1995) 22:455–61.
5. Nakano M, Hasegawa H, Takada T, Ito S, Muramatsu Y, Satoh M, et al. Pulmonary diffusion capacity in patients with systemic lupus erythematosus. Respirology. (2002) 7:45–9. doi: 10.1046/j.1440-1843.2002.00361.x
6. Aguilera-Pickens G, Abud-Mendoza C. Pulmonary manifestations in systemic lupus erythematosus: pleural involvement, acute pneumonitis, chronic interstitial lung disease and diffuse alveolar hemorrhage. Reumatol Clin. (2018) 14:294–300. doi: 10.1016/j.reuma.2018.03.012
7. Tselios K, Urowitz MB. Cardiovascular and pulmonary manifestations of systemic lupus erythematosus. Curr Rheumatol Rev. (2017) 13:206–18. doi: 10.2174/1573397113666170704102444
8. Hannah JR, D'Cruz DP. Pulmonary complications of systemic lupus erythematosus. Semin Respir Crit Care Med. (2019) 40:227–34. doi: 10.1055/s-0039-1685537
9. Bertoli AM, Vila LM, Apte M, Fessler BJ, Bastian HM, Reveille JD, et al. Systemic lupus erythematosus in a multiethnic US Cohort LUMINA XLVIII: factors predictive of pulmonary damage. Lupus. (2007) 16:410–7. doi: 10.1177/0961203307079042
10. Kamen DL, Strange C. Pulmonary manifestations of systemic lupus erythematosus. Clin Chest Med. (2010) 31:479–88. doi: 10.1016/j.ccm.2010.05.001
11. Fidler L, Keen KJ, Touma Z, Mittoo S. Impact of pulmonary disease on patient-reported outcomes and patient-performed functional testing in systemic lupus erythematosus. Lupus. (2016) 25:1004–11. doi: 10.1177/0961203316630818
12. Weinrib L, Sharma OP, Quismorio FP Jr. A long-term study of interstitial lung disease in systemic lupus erythematosus. Semin Arthritis Rheum. (1990) 20:48–56. doi: 10.1016/0049-0172(90)90094-V
13. Wiedemann HP, Matthay RA. Pulmonary manifestations of systemic lupus erythematosus. J Thorac Imaging. (1992) 7:1–18. doi: 10.1097/00005382-199203000-00003
14. Eisenberg H, Dubois EL, Sherwin RP, Balchum OJ. Diffuse interstitial lung disease in systemic lupus erythematosus. Ann Intern Med. (1973) 79:37–45. doi: 10.7326/0003-4819-79-1-37
15. Mathai SC, Danoff SK. Management of interstitial lung disease associated with connective tissue disease. BMJ. (2016) 352:h6819. doi: 10.1136/bmj.h6819
16. ter Borg EJ, Groen H, Horst G, Limburg PC, Wouda AA, Kallenberg CG. Clinical associations of antiribonucleoprotein antibodies in patients with systemic lupus erythematosus. Semin Arthritis Rheum. (1990) 20:164–73. doi: 10.1016/0049-0172(90)90057-M
17. Ward MM, Polisson RP. A meta-analysis of the clinical manifestations of older-onset systemic lupus erythematosus. Arthritis Rheum. (1989) 32:1226–32. doi: 10.1002/anr.1780321007
18. Frankel SK, Brown KK. Collagen vascular diseases of the lung. Clin Pulm Med. (2006) 13:25–36. doi: 10.1097/01.cpm.0000197403.64631.de
19. Min JK, Hong YS, Park SH, Park JH, Lee SH, Lee YS, et al. Bronchiolitis obliterans organizing pneumonia as an initial manifestation in patients with systemic lupus erythematosus. J Rheumatol. (1997) 24:2254–7.
20. Tansey D, Wells AU, Colby TV, Ip S, Nikolakoupolou A, du Bois RM, et al. Variations in histological patterns of interstitial pneumonia between connective tissue disorders and their relationship to prognosis. Histopathology. (2004) 44:585–96. doi: 10.1111/j.1365-2559.2004.01896.x
21. Yood RA, Steigman DM, Gill LR. Lymphocytic interstitial pneumonitis in a patient with systemic lupus erythematosus. Lupus. (1995) 4:161–3. doi: 10.1177/096120339500400217
22. Cheema GS, Quismorio FP, Jr. Interstitial lung disease in systemic lupus erythematosus. Curr Opin Pulm Med. (2000) 6:424–9. doi: 10.1097/00063198-200009000-00007
23. Fenlon HM, Doran M, Sant SM, Breatnach E. High-resolution chest CT in systemic lupus erythematosus. AJR Am J Roentgenol. (1996) 166:301–7. doi: 10.2214/ajr.166.2.8553934
24. Lian FZJ, Wang Y, Cui W, Chen D, Li H, Qiu Q, et al. Clinical features and independent predictors of interstitial lung disease in systemic lupus erythematosus. Int J Clin Exp Med. (2016) 9:4233–42.
25. Vivero M, Padera RF. Histopathology of lung disease in the connective tissue diseases. Rheum Dis Clin North Am. (2015) 41:197–211. doi: 10.1016/j.rdc.2014.12.002
26. Eiser AR, Shanies HM. Treatment of lupus interstitial lung disease with intravenous cyclophosphamide. Arthritis Rheum. (1994) 37:428–31. doi: 10.1002/art.1780370318
27. Fink SD, Kremer JM. Successful treatment of interstitial lung disease in systemic lupus erythematosus with methotrexate. J Rheumatol. (1995) 22:967–9.
28. Lim SW, Gillis D, Smith W, Hissaria P, Greville H, Peh CA. Rituximab use in systemic lupus erythematosus pneumonitis and a review of current reports. Intern Med J. (2006) 36:260–2. doi: 10.1111/j.1445-5994.2006.01055.x
29. Okada M, Suzuki K, Matsumoto M, Nakashima M, Nakanishi T, Takada K, et al. Intermittent intravenous cyclophosphamide pulse therapy for the treatment of active interstitial lung disease associated with collagen vascular diseases. Mod Rheumatol. (2007) 17:131–6. doi: 10.3109/s10165-007-0554-2
30. Koo S-M, Uh S-T. Treatment of connective tissue disease-associated interstitial lung disease: the pulmonologist's point of view. Korean J Intern Med. (2017) 32:600–10. doi: 10.3904/kjim.2016.212
31. Swigris JJ, Olson AL, Fischer A, Lynch DA, Cosgrove GP, Frankel SK, et al. Mycophenolate mofetil is safe, well tolerated, and preserves lung function in patients with connective tissue disease-related interstitial lung disease. Chest. (2006) 130:30–6. doi: 10.1016/S0012-3692(15)50949-5
32. Keane MP, Lynch JP, III. Pleuropulmonary manifestations of systemic lupus erythematosus. Thorax. (2000) 55:159–66. doi: 10.1136/thorax.55.2.159
33. Wan SA, Teh CL, Jobli AT. Lupus pneumonitis as the initial presentation of systemic lupus erythematosus: case series from a single institution. Lupus. (2016) 25:1485–90. doi: 10.1177/0961203316646461
34. Winder A, Molad Y, Ostfeld I, Kenet G, Pinkhas J, Sidi Y. Treatment of systemic lupus erythematosus by prolonged administration of high dose intravenous immunoglobulin: report of 2 cases. J Rheumatol. (1993) 20:495–8.
35. Chen YJ, Tseng JJ, Yang MJ, Tsao YP, Lin HY. Acute respiratory distress syndrome in a pregnant woman with systemic lupus erythematosus: a case report. Lupus. (2014) 23:1528–32. doi: 10.1177/0961203314548713
36. Boulware DW, Hedgpeth MT. Lupus pneumonitis and anti-SSA(Ro) antibodies. J Rheumatol. (1989) 16:479–81.
37. Pego-Reigosa JM, Medeiros DA, Isenberg DA. Respiratory manifestations of systemic lupus erythematosus: old and new concepts. Best Pract Res Clin Rheumatol. (2009) 23:469–80. doi: 10.1016/j.berh.2009.01.002
38. Wang D-Y. Diagnosis and management of lupus pleuritis. Curr Opin Pulm Med. (2002) 8:312–6. doi: 10.1097/00063198-200207000-00012
39. Good JT Jr, King TE, Antony VB, Sahn SA. Lupus pleuritis. Clinical features and pleural fluid characteristics with special reference to pleural fluid antinuclear antibodies. Chest. (1983) 84:714–8. doi: 10.1378/chest.84.6.714
40. Hunninghake GW, Fauci AS. Pulmonary involvement in the collagen vascular diseases. Am Rev Respir Dis. (1979) 119:471–503.
41. Pines A, Kaplinsky N, Olchovsky D, Rozenman J, Frankl O. Pleuro-pulmonary manifestations of systemic lupus erythematosus: clinical features of its subgroups. Prognostic and therapeutic implications. Chest. (1985) 88:129–35. doi: 10.1378/chest.88.1.129
42. Ajakumar Menon A, Kirshenbaum D, Burke G. Drug induced lupus presenting as isolated pleural effusion. Chest. (2015) 148:884A. doi: 10.1378/chest.2236839
43. Costa MF, Said NR, Zimmermann B. Drug-induced lupus due to anti-tumor necrosis factor alpha agents. Semin Arthritis Rheum. (2008) 37:381–7. doi: 10.1016/j.semarthrit.2007.08.003
44. Smith PR, Nacht RI. Drug-induced lupus pleuritis mimicking pleural space infection. Chest. (1992) 101:268–9. doi: 10.1378/chest.101.1.268
45. Glazer M, Berkman N, Lafair JS, Kramer MR. Successful talc slurry pleurodesis in patients with nonmalignant pleural effusion. Chest. (2000) 117:1404–9. doi: 10.1378/chest.117.5.1404
46. McKnight KM, Adair NE, Agudelo CA. Successful use of tetracycline pleurodesis to treat massive pleural effusion secondary to systemic lupus erythematosus. Arthritis Rheum. (1991) 34:1483–4. doi: 10.1002/art.1780341121
47. Hoeper MM, Ghofrani H-A, Grünig E, Klose H, Olschewski H, Rosenkranz S. Pulmonary hypertension. Dtsch Arztebl Int. (2017) 114:73–84. doi: 10.3238/arztebl.2016.0073
48. Tselios K, Gladman DD, Urowitz MB. Systemic lupus erythematosus and pulmonary arterial hypertension: links, risks, and management strategies. Open Access Rheumatol. (2016) 9:1–9. doi: 10.2147/OARRR.S123549
49. Johnson SR, Gladman DD, Urowitz MB, Ibañez D, Granton JT. Pulmonary hypertension in systemic lupus. Lupus. (2004) 13:506–9. doi: 10.1191/0961203303lu1051oa
50. Pan TL, Thumboo J, Boey ML. Primary and secondary pulmonary hypertension in systemic lupus erythematosus. Lupus. (2000) 9:338–42. doi: 10.1191/096120300678828361
51. Quismorio FP Jr, Sharma O, Koss M, Boylen T, Edmiston AW, Thornton PJ, et al. Immunopathologic and clinical studies in pulmonary hypertension associated with systemic lupus erythematosus. Semin Arthritis Rheum. (1984) 13:349–59. doi: 10.1016/0049-0172(84)90015-5
52. Shen JY, Chen SL, Wu YX, Tao RQ, Gu YY, Bao CD, et al. Pulmonary hypertension in systemic lupus erythematosus. Rheumatol Int. (1999) 18:147–51. doi: 10.1007/s002960050074
53. Simonson JS, Schiller NB, Petri M, Hellmann DB. Pulmonary hypertension in systemic lupus erythematosus. J Rheumatol. (1989) 16:918–25.
54. Winslow TM, Ossipov MA, Fazio GP, Simonson JS, Redberg RF, Schiller NB. Five-year follow-up study of the prevalence and progression of pulmonary hypertension in systemic lupus erythematosus. Am Heart J. (1995) 129:510–5. doi: 10.1016/0002-8703(95)90278-3
55. Lv T-T, Wang P, Guan S-Y, Li H-M, Li X-M, Wang B, et al. Prevalence of pulmonary hypertension in systemic lupus erythematosus: a meta-analysis. Ir J Med Sci. (2018) 187:723–30. doi: 10.1007/s11845-017-1727-4
56. Pope J. An update in pulmonary hypertension in systemic lupus erythematosus - do we need to know about it? Lupus. (2008) 17:274–7. doi: 10.1177/0961203307087188
57. Dhala A. Pulmonary arterial hypertension in systemic lupus erythematosus: current status and future direction. Clin Dev Immunol. (2012) 2012:854941. doi: 10.1155/2012/854941
58. Hoeper MM, Bogaard HJ, Condliffe R, Frantz R, Khanna D, Kurzyna M, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol. (2013) 62(25 Suppl.):D42–50. doi: 10.1016/j.jacc.2013.10.032
59. Badesch DB, Hill NS, Burgess G, Rubin LJ, Barst RJ, Galiè N, et al. Sildenafil for pulmonary arterial hypertension associated with connective tissue disease. J Rheumatol. (2007) 34:2417–22.
60. Mok MY, Tsang PL, Lam YM, Lo Y, Wong WS, Lau CS. Bosentan use in systemic lupus erythematosus patients with pulmonary arterial hypertension. Lupus. (2007) 16:279–85. doi: 10.1177/0961203307076509
61. Oudiz RJ, Schilz RJ, Barst RJ, Galié N, Rich S, Rubin LJ, et al. Treprostinil, a prostacyclin analogue, in pulmonary arterial hypertension associated with connective tissue disease. Chest. (2004) 126:420–7. doi: 10.1378/chest.126.2.420
62. Robbins IM, Gaine SP, Schilz R, Tapson VF, Rubin LJ, Loyd JE. Epoprostenol for treatment of pulmonary hypertension in patients with systemic lupus erythematosus. Chest. (2000) 117:14–8. doi: 10.1378/chest.117.1.14
63. Rubin LJ, Badesch DB, Barst RJ, Galie N, Black CM, Keogh A, et al. Bosentan therapy for pulmonary arterial hypertension. N Engl J Med. (2002) 346:896–903. doi: 10.1056/NEJMoa012212
64. Shirai Y, Yasuoka H, Takeuchi T, Satoh T, Kuwana M. Intravenous epoprostenol treatment of patients with connective tissue disease and pulmonary arterial hypertension at a single center. Mod Rheumatol. (2013) 23:1211–20. doi: 10.3109/s10165-012-0828-1
65. Humbert M, Coghlan JG, Ghofrani H-A, Grimminger F, He J-G, Riemekasten G, et al. Riociguat for the treatment of pulmonary arterial hypertension associated with connective tissue disease: results from PATENT-1 and PATENT-2. Ann Rheum Dis. (2017) 76:422–6. doi: 10.1136/annrheumdis-2015-209087
66. Kuzuya K, Tsuji S, Matsushita M, Ohshima S, Saeki Y. Systemic sclerosis and systemic lupus erythematosus overlap syndrome with pulmonary arterial hypertension successfully treated with immunosuppressive therapy and riociguat. Cureus. (2019) 11:e4327. doi: 10.7759/cureus.4327
67. Gonzalez-Lopez L, Cardona-Muñoz EG, Celis A, García-de la Torre I, Orozco-Barocio G, Salazar-Paramo M, et al. Therapy with intermittent pulse cyclophosphamide for pulmonary hypertension associated with systemic lupus erythematosus. Lupus. (2004) 13:105–12. doi: 10.1191/0961203304lu509oa
68. Kommireddy S, Bhyravavajhala S, Kurimeti K, Chennareddy S, Kanchinadham S, Rajendra Vara Prasad I, et al. Pulmonary arterial hypertension in systemic lupus erythematosus may benefit by addition of immunosuppression to vasodilator therapy: an observational study. Rheumatology. (2015) 54:1673–9. doi: 10.1093/rheumatology/kev097
69. Prete M, Fatone MC, Vacca A, Racanelli V, Perosa F. Severe pulmonary hypertension as the initial manifestation of systemic lupus erythematosus: a case report and review of the literature. Clin Exp Rheumatol. (2014) 32:267–74.
70. Tanaka E, Harigai M, Tanaka M, Kawaguchi Y, Hara M, Kamatani N. Pulmonary hypertension in systemic lupus erythematosus: evaluation of clinical characteristics and response to immunosuppressive treatment. J Rheumatol. (2002) 29:282–7.
71. Hennigan S, Channick RN, Silverman GJ. Rituximab treatment of pulmonary arterial hypertension associated with systemic lupus erythematosus: a case report. Lupus. (2008) 17:754–6. doi: 10.1177/0961203307087610
72. Wahl DG, Guillemin F, de Maistre E, Perret C, Lecompte T, Thibaut G. Risk for venous thrombosis related to antiphospholipid antibodies in systemic lupus erythematosus—a meta-analysis. Lupus. (1997) 6:467–73. doi: 10.1177/096120339700600510
73. Kado R, Siegwald E, Lewis E, Goodsitt MM, Christodoulou E, Kazerooni E, et al. Utility and associated risk of pulmonary embolism computed tomography scans in the michigan lupus cohort. Arthritis Care Res. (2016) 68:406–11. doi: 10.1002/acr.22684
74. Pengo V, Denas G, Zoppellaro G, Jose SP, Hoxha A, Ruffatti A, et al. Rivaroxaban vs. warfarin in high-risk patients with antiphospholipid syndrome. Blood. (2018) 132:1365–71. doi: 10.1182/blood-2018-04-848333
75. Abud-Mendoza C, Diaz-Jouanen E, Alarcón-Segovia D. Fatal pulmonary hemorrhage in systemic lupus erythematosus. Occurrence without hemoptysis. J Rheumatol. (1985) 12:558–61.
76. Zamora MR, Warner ML, Tuder R, Schwarz MI. Diffuse alveolar hemorrhage and systemic lupus erythematosus. Clinical presentation, histology, survival, and outcome. Medicine. (1997) 76:192–202. doi: 10.1097/00005792-199705000-00005
77. Cordier JF, Cottin V. Alveolar hemorrhage in vasculitis: primary and secondary. Semin Respir Crit Care Med. (2011) 32:310–21. doi: 10.1055/s-0031-1279827
78. Yachoui R, Sehgal R, Amlani B, Goldberg JW. Antiphospholipid antibodies-associated diffuse alveolar hemorrhage. Semin Arthritis Rheum. (2015) 44:652–7. doi: 10.1016/j.semarthrit.2014.10.013
79. Santos-Ocampo AS, Mandell BF, Fessler BJ. Alveolar hemorrhage in systemic lupus erythematosus: presentation and management. Chest. (2000) 118:1083–90. doi: 10.1378/chest.118.4.1083
80. Koh WH, Thumboo J, Boey ML. Pulmonary haemorrhage in Oriental patients with systemic lupus erythematosus. Lupus. (1997) 6:713–6. doi: 10.1177/096120339700600906
81. Masoodi I, Sirwal IA, Anwar SK, Alzaidi A, Balbaid KA. Predictors of mortality in pulmonary haemorrhage during SLE: a single centre study over eleven years. Open Access Maced J Med Sci. (2019) 7:92–6. doi: 10.3889/oamjms.2019.038
82. Martínez-Martínez MU, Oostdam DAH, Abud-Mendoza C. Diffuse alveolar hemorrhage in autoimmune diseases. Curr Rheumatol Rep. (2017) 19:27. doi: 10.1007/s11926-017-0651-y
83. Borrell H, Narváez J, Alegre JJ, Castellví I, Mitjavila F, Aparicio M, et al. Shrinking lung syndrome in systemic lupus erythematosus: a case series and review of the literature. Medicine. (2016) 95:e4626. doi: 10.1097/MD.0000000000004626
84. Deeb M, Tselios K, Gladman DD, Su J, Urowitz MB. Shrinking lung syndrome in systemic lupus erythematosus: a single-centre experience. Lupus. (2018) 27:365–71. doi: 10.1177/0961203317722411
85. Laroche CM, Mulvey DA, Hawkins PN, Walport MJ, Strickland B, Moxham J, et al. Diaphragm strength in the shrinking lung syndrome of systemic lupus erythematosus. Q J Med. (1989) 71:429–39.
86. Toya SP, Tzelepis GE. Association of the shrinking lung syndrome in systemic lupus erythematosus with pleurisy: a systematic review. Semin Arthritis Rheum. (2009) 39:30–7. doi: 10.1016/j.semarthrit.2008.04.003
87. Karim MY, Miranda LC, Tench CM, Gordon PA, D'Cruz DP, Khamashta MA, et al. Presentation and prognosis of the shrinking lung syndrome in systemic lupus erythematosus. Semin Arthritis Rheum. (2002) 31:289–98. doi: 10.1053/sarh.2002.32555
88. Duron L, Cohen-Aubart F, Diot E, Borie R, Abad S, Richez C, et al. Shrinking lung syndrome associated with systemic lupus erythematosus: a multicenter collaborative study of 15 new cases and a review of the 155 cases in the literature focusing on treatment response and long-term outcomes. Autoimmun Rev. (2016) 15:994–1000. doi: 10.1016/j.autrev.2016.07.021
89. Benham H, Garske L, Vecchio P, Eckert BW. Successful treatment of shrinking lung syndrome with rituximab in a patient with systemic lupus erythematosus. J Clin Rheumatol. (2010) 16:68–70. doi: 10.1097/RHU.0b013e3181d0757f
90. Langenskiöld E, Bonetti A, Fitting JW, Heinzer R, Dudler J, Spertini F, et al. Shrinking lung syndrome successfully treated with rituximab and cyclophosphamide. Respiration. (2012) 84:144–9. doi: 10.1159/000334947
91. Peñacoba Toribio P, Córica Albani ME, Mayos Pérez M, Rodríguez de la Serna A. Rituximab in the treatment of shrinking lung syndrome in systemic lupus erythematosus. Reumatol Clin. (2014) 10:325–7. doi: 10.1016/j.reuma.2013.09.003
92. Walz-Leblanc BA, Urowitz MB, Gladman DD, Hanly PJ. The “shrinking lungs syndrome” in systemic lupus erythematosus–improvement with corticosteroid therapy. J Rheumatol. (1992) 19:1970–2.
93. Traynor AE, Corbridge TC, Eagan AE, Barr WG, Liu Q, Oyama Y, et al. Prevalence and reversibility of pulmonary dysfunction in refractory systemic lupus: improvement correlates with disease remission following hematopoietic stem cell transplantation. Chest. (2005) 127:1680–9. doi: 10.1378/chest.127.5.1680
94. Muñoz-Rodríguez FJ, Font J, Badia JR, Miret C, Barberà JA, Cervera R, et al. Shrinking lungs syndrome in systemic lupus erythematosus: improvement with inhaled beta-agonist therapy. Lupus. (1997) 6:412–4. doi: 10.1177/096120339700600413
95. Van Veen S, Peeters AJ, Sterk PJ, Breedveld FC. The “shrinking lung syndrome” in SLE, treatment with theophylline. Clin Rheumatol. (1993) 12:462–5. doi: 10.1007/BF02231771
96. Jindal SK, Agarwal R. Autoimmunity and interstitial lung disease. Curr Opin Pulm Med. (2005) 11:438–46. doi: 10.1097/01.mcp.0000170522.71497.61
97. Orens JB, Martinez FJ, Lynch JP III. Pleuropulmonary manifestations of systemic lupus erythematosus. Rheum Dis Clin North Am. (1994) 20:159–93.
98. Myers JL, Katzenstein AA. Microangiitis in lupus-induced pulmonary hemorrhage. Am J Clin Pathol. (1986) 85:552–6. doi: 10.1093/ajcp/85.5.552
99. Turner-Stokes L, Haslam P, Jones M, Dudeney C, Le Page S, Isenberg D. Autoantibody and idiotype profile of lung involvement in autoimmune rheumatic disease. Ann Rheum Dis. (1990) 49:160–2. doi: 10.1136/ard.49.3.160
100. Pandya MR, Agus B, Grady RF. Letter: In vivo LE phenomenon in pleural fluid. Arthritis Rheum. (1976) 19:962–3. doi: 10.1002/art.1780190526
101. Dorfmüller P, Humbert M, Perros F, Sanchez O, Simonneau G, Müller KM, et al. Fibrous remodeling of the pulmonary venous system in pulmonary arterial hypertension associated with connective tissue diseases. Hum Pathol. (2007) 38:893–902. doi: 10.1016/j.humpath.2006.11.022
102. Carmier D, Diot E, Diot P. Shrinking lung syndrome: recognition, pathophysiology and therapeutic strategy. Expert Rev Respir Med. (2011) 5:33–9. doi: 10.1586/ers.10.84
103. Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. (1997) 40:1725. doi: 10.1002/art.1780400928
104. Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R, et al. 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheumatol. (2019) 71:1400–12. doi: 10.1002/art.40930
105. Yee CS, Farewell V, Isenberg DA, Griffiths B, Teh LS, Bruce IN, et al. The BILAG-2004 index is sensitive to change for assessment of SLE disease activity. Rheumatology. (2009) 48:691–5. doi: 10.1093/rheumatology/kep064
106. Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol. (2002) 29:288–91.
107. Franklyn K, Lau CS, Navarra SV, Louthrenoo W, Lateef A, Hamijoyo L, et al. Definition and initial validation of a Lupus Low Disease Activity State (LLDAS). Ann Rheum Dis. (2016) 75:1615–21. doi: 10.1136/annrheumdis-2015-207726
108. Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M, et al. The development and initial validation of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum. (1996) 39:363–9. doi: 10.1002/art.1780390303
Keywords: systemic lupus erythematosus (SLE), interstitial lung disease (ILD), pleurisy, pleural effusion, shrinking lung syndrome, pulmonary arterial hypertension, acute lupus pneumonitis, pulmonary vasculitis
Citation: Amarnani R, Yeoh SA, Denneny EK and Wincup C (2021) Lupus and the Lungs: The Assessment and Management of Pulmonary Manifestations of Systemic Lupus Erythematosus. Front. Med. 7:610257. doi: 10.3389/fmed.2020.610257
Received: 25 September 2020; Accepted: 07 December 2020;
Published: 18 January 2021.
Edited by:
Peter Korsten, University Medical Center Göttingen, GermanyReviewed by:
Javier Merayo-Chalico, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ), MexicoSilvia Piantoni, University of Brescia, Italy
Copyright © 2021 Amarnani, Yeoh, Denneny and Wincup. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chris Wincup, Yy53aW5jdXBAdWNsLmFjLnVr
 Raj Amarnani
Raj Amarnani Su-Ann Yeoh
Su-Ann Yeoh Emma K. Denneny
Emma K. Denneny Chris Wincup
Chris Wincup