- Key Laboratory of Respiratory Disease of Zhejiang Province, Department of Respiratory and Critical Care Medicine, Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, China
Background: Chronic cough is a common complaint that in rare cases can be caused by premature ventricular beats (PVCs).
Materials and Methods: In this report, we present the case of a healthy 44-year-old female who presented persistent cough and cough syncope that was attributed to PVCs.
Results: The cough disappeared after radiofrequency ablation, and no recurrence of arrhythmia or cough was observed.
Conclusion: PVCs should be considered a probable cause of chronic cough and cough syncope in differential diagnosis.
Introduction
Chronic cough, which is defined as a cough lasting for more than 8 weeks, is the most common symptom that accompanies a diverse range of respiratory diseases, non-respiratory conditions, and rarer conditions (1, 2). Various causes of chronic cough have been found, including upper airway cough syndrome, gastroesophageal reflux disease (GERD)/laryngopharyngeal reflux disease, asthma, and non-asthmatic eosinophilic bronchitis (NAEB); however, almost 7% of all chronic coughs are unexplained (3–5). This case report describes a patient with premature ventricular beats (PVCs) presenting with chronic cough and cough syncope.
Case Presentation
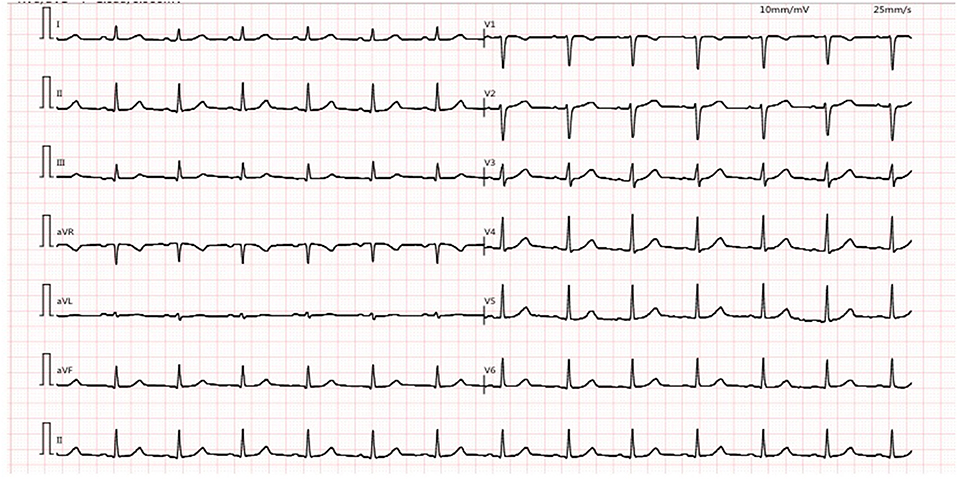
This 44-year-old female presented with daily productive cough and expectoration for 4 years and experienced recurrence for more than half a year. The respiratory symptoms were predominantly nocturnal and more severe in the winter. She was diagnosed with chronic cough and was treated with cough medications for cough symptoms, which did not prevent the disease from worsening. Seven months prior, the chest film and spirometry test were almost normal; however, 4 months prior, the cough returned and the patient suffered from cough-related syncope for 3 h. She denied chest pain, chest distress, shortness of breath, heartburn, or acid regurgitation. She had no known allergies and denied smoking. The patient presented no abnormality on physical examination. White blood cell count, eosinophil count, and serum immunoglobulin E (39.1 IU/mL, normal value <100 IU/mL) were normal. Chest high-resolution CT (HRCT) (Figure 1A), pulmonary ventilation and single-breath diffusing capacity of the lung for carbon monoxide were normal. The methacholine challenge test for bronchial hyperreactivity was negative (Figure 1B). In pulmonary function testing, the forced vital capacity (FVC) was 2.99 L (100.9% of predicted value), the forced expiratory volume in 1 s (FEV1) was 2.45 L (96.5% of predicted value), and the FEV1/FVC ratio was 81.99% (Figure 1C). The patient's electrocardiogram (ECG) showed normal sinus rhythm with frequent premature ventricular beats (PVCs) (Figure 2). The 24 h-Holter ECG monitor showed normal sinus rhythm with 27553 PVCs (Figure 3). The frequent occurrence of PVCs was associated with repetitive coughing. Two-dimensional color echocardiography was normal except for trivial regurgitant flow (Figure 4). Subsequent treatment with oral antiarrhythmic drugs was ineffective. Therefore, radiofrequency ablation of the arrhythmogenic focus was proposed. Surprisingly, cough disappeared after radiofrequency ablation, and no recurrence of arrhythmia or cough was observed (Figure 5).
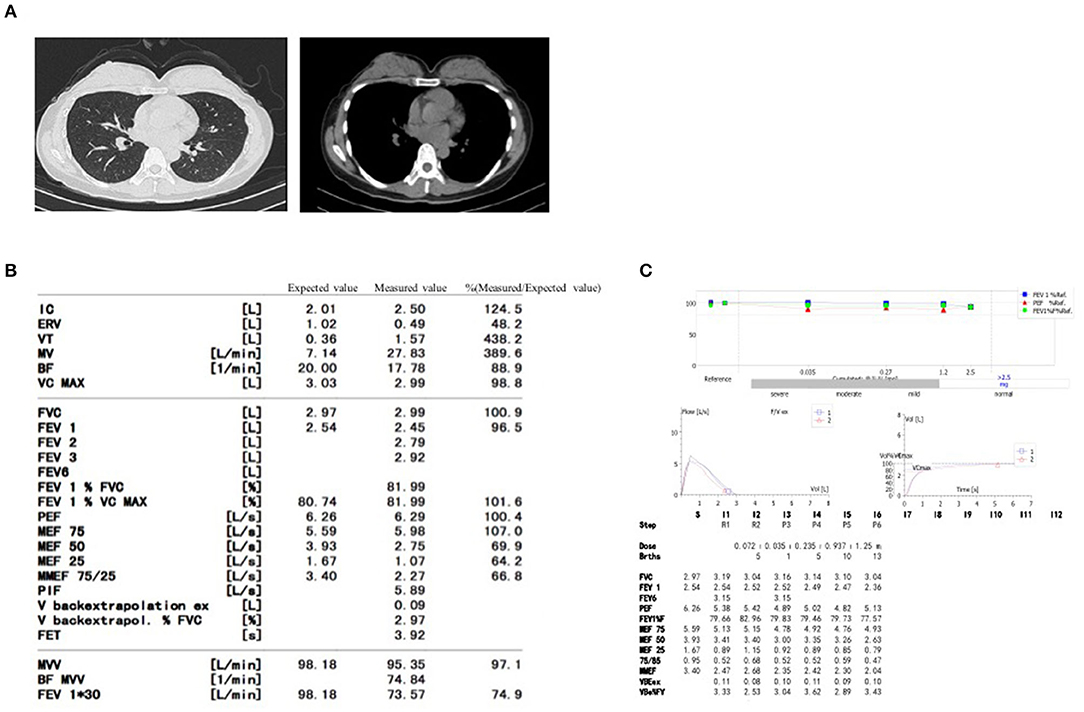
Figure 1. The examination of Chest high-resolution CT (A), pulmonary function (B) and methacholine challenge test (C) in the patient.
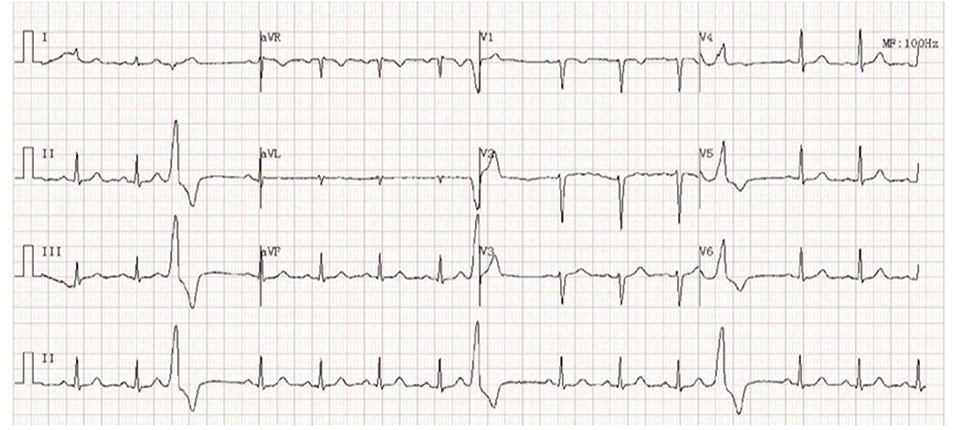
Figure 2. Electrocardiogram (ECG) showing normal sinus rhythm with premature ventricular complexes (PVCs).

Figure 3. 24 h-Holter monitoring showing normal sinus rhythm with premature ventricular complexes (PVCs) during coughing.
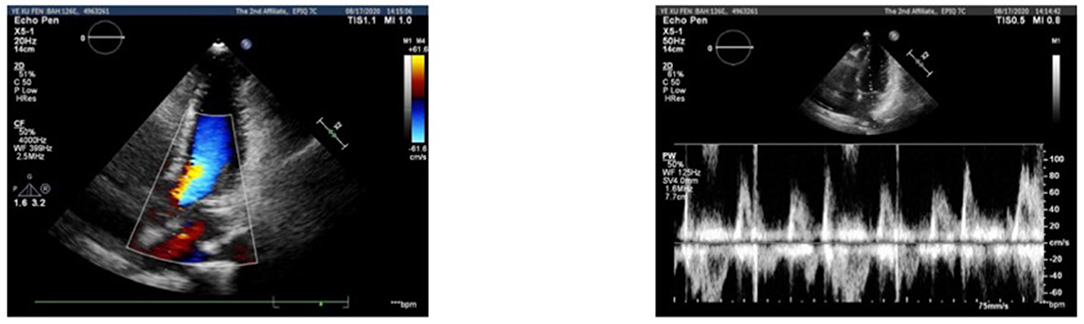
Figure 4. Doppler echocardiogram recordings of blood flow during sinus rhythm and premature ventricular complexes (PVCs).
Discussion
We report the case of a 44-year-old female who presented to our hospital for PVCs with chronic cough and cough syncope. Symptoms were resolved immediately with the suppression of the PVCs, supporting the causal relationship. The mechanism is uncertain. It has been proposed that PVC-induced cough happens due to the cardiopulmonary reflex (6). Sebastian and his colleagues reported that a patient had premature ventricular complex-induced chronic cough and cough syncope and speculated that the cough reflex was triggered by stimulating sympathetic innervation in the right ventricular outflow tract or pulmonary artery (6). Nimii et al. suggested PVC- induced haemodynamic changes in the pulmonary circulation as factors inducing chronic cough (7). Another mechanism is the cough reflex, which either directly activates C-fibers in the left ventricular wall or distends the pulmonary artery and activates cough receptors as a result of augmented pulmonary blood flow following PVCs (8).
At present, many mechanisms have been reported to be associated with cough syncope (9–12). We suspect that pronounced hypotension and an inappropriate cough-triggered blood pressure-heart rate relationship during PVCs could contribute to syncope and reduce cerebral flow due to vagal modulation (5, 13–15).
Approximately 5% of patients with PVCs present with chronic cough (6). In addition, some less common conditions also occur with chronic cough, such as idiopathic pulmonary fibrosis, eosinophilic bronchitis, and sarcoidosis. These were concluded to be the cause for chronic cough.
Conclusion
Our patient's case demonstrated PVC-induced cough and cough syncope in a single healthy patient. We suspect that the PVCs might be responsible for coughing in our patient. Even though cough is a rare symptom, it is necessary to explain potential mechanisms between cough and PVC or other arrhythmias. PVCs should be considered a probable cause of chronic cough in the clinical setting.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board for Human Studies of Second Affiliated Hospital of Zhejiang University School of Medicine (Hangzhou, China). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
YH examined the patient, ordered the needed tests, interpreted the data, and was a major contributor in finalizing the manuscript. WH interpreted the data and analyzed the results. NL and HH collected the needed data, analyzed and interpreted the results, and was a major contributor in finalizing the manuscript, and submitting it for publication. All authors read and approved the final manuscript.
Funding
This work was supported in part by the General Project (grant nos. 81800074, 81901454) from the National Natural Science Foundation of China and the Youth Foundation Project of Zhejiang Province of China (grant no. LQ18H010002).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the patient for allowing us to publish this report.
References
1. Irwin RS. Introduction to the diagnosis and management of cough: ACCP evidence-based clinical practice guidelines. Chest. (2006) 129:25S–27S. doi: 10.1378/chest.129.1_suppl.25S
2. Smith JA, Woodcock A. Chronic cough. N Engl J Med. (2016) 375:1544–51. doi: 10.1056/NEJMcp1414215
3. Pratter MR. Overview of common causes of chronic cough: ACCP evidence-based clinical practice guidelines. Chest. (2006) 129:59S–62S. doi: 10.1378/chest.129.1_suppl.59S
4. Morice AH, Fontana GA, Sovijarvi AR, Pistolesi M, Chung KF, Widdicombe J, et al. The diagnosis and management of chronic cough. Eur Respir J. (2004) 24:481–92. doi: 10.1183/09031936.04.00027804
5. Stec S, Dabrowska M, Zaborska B, Bielicki P, Maskey-Warzechowska M, Tarnowski W, et al. Premature ventricular complex-induced chronic cough and cough syncope. Eur Respir J. (2007) 30:391–4. doi: 10.1183/09031936.00062606
6. Stec SM, Grabczak EM, Bielicki P, Zaborska B, Krenke R, Krynski T, et al. Diagnosis and management of premature ventricular complexes-associated chronic cough. Chest. (2009) 135:1535–41. doi: 10.1378/chest.08-1814
7. Nimii AKY, Sumita Y, Okano Y, Tambara K, Fujita M. Cough reflex by ventricular premature contractions. Int Heart J. (2005) 46:923–6. doi: 10.1536/ihj.46.923
8. Hasdemir C, Musayev O, Kehribar DY, Kartal Y, Can LH. Chronic cough and tachycardia-induced cardiomyopathy in a patient with idiopathic frequent, monomorphic premature ventricular contractions. Pacing Clin Electrophysiol. (2013) 36:e156–8. doi: 10.1111/j.1540-8159.2011.03236.x
9. Avramov K, Sztriha L, Makai A, Jambrik Z, Rudas L, Vecsei L. [Mechanism of cough syncope]. Orv Hetil. (2004) 145:1625–1627.
11. Krediet CT, Wieling W, Edward P. Sharpey-Schafer was right: evidence for systemic vasodilatation as a mechanism of hypotension in cough syncope. Europace. (2008) 10:486–8. doi: 10.1093/europace/eun022
12. McIntosh HD, Estes EH, Warren JV. The mechanism of cough syncope. Am Heart J. (1956) 52:70–82. doi: 10.1016/0002-8703(56)90119-3
13. Benditt DG, Samniah N, Pham S, Sakaguchi S, Lu F, Lurie KG, et al. Effect of cough on heart rate and blood pressure in patients with “cough syncope”. Heart Rhythm. (2005) 2:807–13. doi: 10.1016/j.hrthm.2005.04.022
14. Malkoff MD, Gomez CR, Myles G, Cruz-Flores S. Cerebrovascular hemodynamic inefficiency of premature ventricular contractions. Angiology. (1996) 47:51–6. doi: 10.1177/000331979604700107
Keywords: chronic cough, syncope, premature ventricular beats, radiofrequency ablation, arrhythmia
Citation: Hu Y, Hua W, Li N and Huang H (2021) Case Report: Premature Ventricular Beats-Induced Chronic Cough and Cough Syncope. Front. Med. 8:641948. doi: 10.3389/fmed.2021.641948
Received: 15 December 2020; Accepted: 15 February 2021;
Published: 10 March 2021.
Edited by:
Piero Valentini, Università Cattolica del Sacro Cuore, ItalyReviewed by:
Gunnar N. Hillerdal, Karolinska University Hospital, SwedenDanilo Buonsenso, Catholic University of the Sacred Heart, Italy
Copyright © 2021 Hu, Hua, Li and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Na Li, bGluYXpqdUB6anUuZWR1LmNu; Huaqiong Huang, enJfaGhxQHpqdS5lZHUuY24=
†These authors have contributed equally to this work
 Yue Hu
Yue Hu Wen Hua
Wen Hua