- 1Department of Massage, Hangzhou TCM Hospital Affiliated to Zhejiang Chinese Medical University, Hangzhou, China
- 2Third Clinical Medical College, Zhejiang Chinese Medical University, Hangzhou, China
Objective: Several studies suggested that Qigong exercise (QE) can relieve fatigue in patients diagnosed with various diseases. Our review aimed to evaluate the efficacy of QE for alleviating fatigue.
Methods: A related literature search was performed in the PubMed, Web of Science, Embase, Cochrane Library, China Biology Medicine disc (CBM), China National Knowledge Infrastructure (CNKI), Wanfang, and VIP data bases from inception to November 2020. Information on fatigue, malaise, tiredness, and Qigong research data was collected.
Results: Sixteen randomized controlled trials (RCTs) were reported in patients with cancer (n = 4), chronic fatigue syndrome (n = 2), and other diseases (n = 10). The QE groups showed significant improvements in total fatigue intensity [15 RCTs, p < 0.00001; standard mean difference (SMD) −0.69 (−0.95 to −0.44)]. The QE groups did not show significant improvement in quality of life [4 RCTs, p = 0.08; SMD 0.53 (−0.07 to 1.14)]. The statistically significant difference of the subgroup analyses (different primary diseases, QE types, and study quality) also remained unchanged.
Conclusion: The findings of this meta-analysis indicate that QE may be beneficial for improving fatigue in patients diagnosed with various diseases. Considering the limitations of the study, we draw a very cautious conclusion regarding the resulting estimate of the effect. Further studies are warranted to better understand the benefits of QE in primary medical care.
Introduction
Fatigue, a subjective symptom, is the embodiment of complex physiological, psychological, and pathological phenomena, wherein the body's physical strength or energy is weakened or lost (1). With the rapid industrialization of society, chronic fatigue is prevalent in 15–20% of the general population (2, 3). In some occupations or specific environments, the incidence rate of fatigue symptoms is even >70% (4, 5). Fatigue is also one of the most common symptoms in primary medical care. Approximately 10–20% of patients complain of fatigue (6, 7), and 10–30% of patients consider fatigue an important accompanying symptom (8, 9). Several drugs, such as anti-neoplastic agents (10) and antidepressants (11), may be associated with secondary fatigue, which is produced by the adverse effects of the administered treatment. For the general population, fatigue is an alarm signal given by the body when it attains its physical limits. Without effective treatment, the symptoms of physical illness and common psychological disorders may lead patients into a vicious cycle associated strongly with fatigue, depression, anxiety, chronic pain, and sleep disturbances (12). However, clinically, patients describe fatigue in varying ways, such as sleepiness, weakness, lethargy, pain, and heaviness, and physicians may overlook or underestimate its severity (13).
The treatment options for fatigue should address the etiology and mechanism of the primary diseases, if possible. However, the multidimensionality and subjective nature of fatigue, and the lack of consensus on its pathophysiology make effective treatment difficult (14). As a result, a standardized and specific treatment that may improve or prevent fatigue in population groups that are considered “patients at risk” has not been established (15, 16). Methods for improving fatigue in patients are divided into pharmacological and non-pharmacological categories. However, some drugs used for treating fatigue possess insufficient evidence of efficacy and should be further investigated (17, 18); the adverse effects of other medications could cause more complications in patients (19, 20). Aerobic exercise has been recommended as a non-pharmacological alternative for treating fatigue (21, 22). It is a practical option and can easily be adhered to by patients in the long-term. Unfortunately, the efficacy of aerobic exercise in improving fatigue has also been questioned in some systematic reviews (23, 24).
Qigong exercise (QE), a distinctive traditional technique that has amassed a large following in China, is a form of low-intensity exercise (25, 26). Numerous clinical guidelines related to the use of QE for the rehabilitation of fatigue in patients with cardiopulmonary diseases and Parkinson's disease are available, with positive recommendations (27, 28). Other systematic reviews either evaluated QE as a component of aerobic exercise or aimed to summarize the potential of QE to address the multifaceted needs of cancer survivors (21, 22). In this study, we aimed to comprehensively evaluate the therapeutic benefits of QE on fatigue. We investigated a broader scope of primary diseases and patient clinical outcomes by summarizing and analyzing the existing literature.
Methods
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline (Supplementary Appendix 1). The study had been registered on INPLASY (https://inplasy.com) and the registration number is INPLASY2020110133. There was no direct patient or public involvement in this review.
Data Sources and Searches
We searched the related studies from PubMed, Web of Science, Embase, Cochrane Library, China Biology Medicine disc, China National Knowledge Infrastructure, Wanfang, and VIP Data Knowledge Service Platform published from inception until November 2020.
Exhaustive search strategies for each electronic database were developed by the review team members. The English-language search strategy containing relevant terms was based on the concepts: (1) “Fatigue” or “Malaise” or “Tiredness,” (2) “Qigong,” and (3) “Randomized Clinical Trial.” In the Chinese databases, we used equivalent search terms. Search tactics for PubMed are shown in Supplementary Appendix 2.
Inclusion and Exclusion Criteria
Studies considered in this meta-analysis were required to meet the following inclusion criteria. First, studies published in English or Chinese up to November 30, 2020 with a randomized controlled trial (RCT) design investigating the use of QE interventions for fatigue symptoms were considered for inclusion. Studies were included if appropriate data were available for the calculation of effect sizes in each treatment arm. Second, studies involving patients with primary disease-related symptoms of fatigue were included, regardless of the underlying disease, age, sex, education, ethnicity, and occupation of the studied patients. If the patients experienced serious complications, such as cognitive communication disorders, the study was excluded. Third, studies were included if QE alone (any form of Qigong category, including Baduanjin, Yijinjing, and Wuqinxi) or QE combined with other treatments was the main intervention in the observation group. No limit was set on the duration and frequency of treatment. Moreover, in the control group, the patients were treated with any type of intervention, including exercise, stretching, or sham Qigong; studies with observation groups were also included. Finally, the primary outcome defined to be compared was the severity, duration, frequency, or improvement of fatigue, evaluated through the following scales: Functional Assessment Chronic Illness Therapy–Fatigue, Chalder's Fatigue Scale, Multidimensional Fatigue Inventory-20, Fatigue Scale-14, Visual Analog Scales for fatigue, Fatigue Severity Scale, or Revised Piper fatigue Scale, and medical scales for some specific diseases including Functional Assessment of Cancer Therapy-General, 16-item Parkinson Fatigue Scale, or Fatigue scale in the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire - Core 30. Other secondary outcomes were quality of life (QOL), assessed through the MOS item short-form health survey-36 and Medical Outcomes Study 12-Item Short-Form Health Survey.
Study Selection and Data Extraction
When the results of one study were presented in several publications, only the most recent publication and complete data were considered. The eligibility of trials was assessed by two authors independently (WR and W-YQ). The following information was extracted by two authors (WR and H-XY) based on a fixed protocol: geographical location, primary disease, number of QE group and control participants, interventions of QE type, duration, and outcomes results. Discrepancies were settled by agreement, and a third author (SD) was consulted if necessary.
Risk of Bias Assessment
Two researchers (WR and H-XY) independently assessed the quality of the selected studies according to the Cochrane Collaboration's tool for randomized controlled trials (29). Items were evaluated in three categories: low risk of bias, unclear bias, and high risk of bias. The following characteristics were evaluated: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other biases resulting from these questions were graphed and assessed using Review Manager 5.4. Any disagreements were resolved by discussion or with the help of a third author (SD).
Data Synthesis and Statistical Analysis
The traditional pair-wise efficacy data in populations were synthesized and statistically analyzed using Review Manager 5.4 by random effects modeling (weighted by the inverse of the variance). For continuous data including the total fatigue intensity and QOL scale score, which were measured using different tools, the standard mean difference (SMD) and 95% confidence intervals were used for effective evaluation. To ensure uniformity of the included data, all of them were used in the intention-to-treat analysis. P-values <0.05 were considered statistically significant unless otherwise specified.
Between-study heterogeneity was assessed using the χ2 and I2 tests. According to the Cochrane handbook, an I2 value > 60% was considered substantial, 30 −60% moderate, and <30% non-important heterogeneity (30). An I2 statistics of 50% or higher indicated the presence of heterogeneity. To further assess the influence of heterogeneity on the meta-analyses' conclusions, meta-regression and subgroup analysis were performed to assess the primary outcome data according to the primary diseases, QE type, sample size, year of publication, intervention length, and study quality (depending on whether random sequence generation and allocation concealment are used to determine the high or low quality of the studies). Visual inspection of asymmetry in funnel plots was conducted. Egger-weighted regression method using STATA 15.0 (Stata-Corp) was also used to statistically assess the publication bias.
Results
Studies Included in the Meta-Analysis
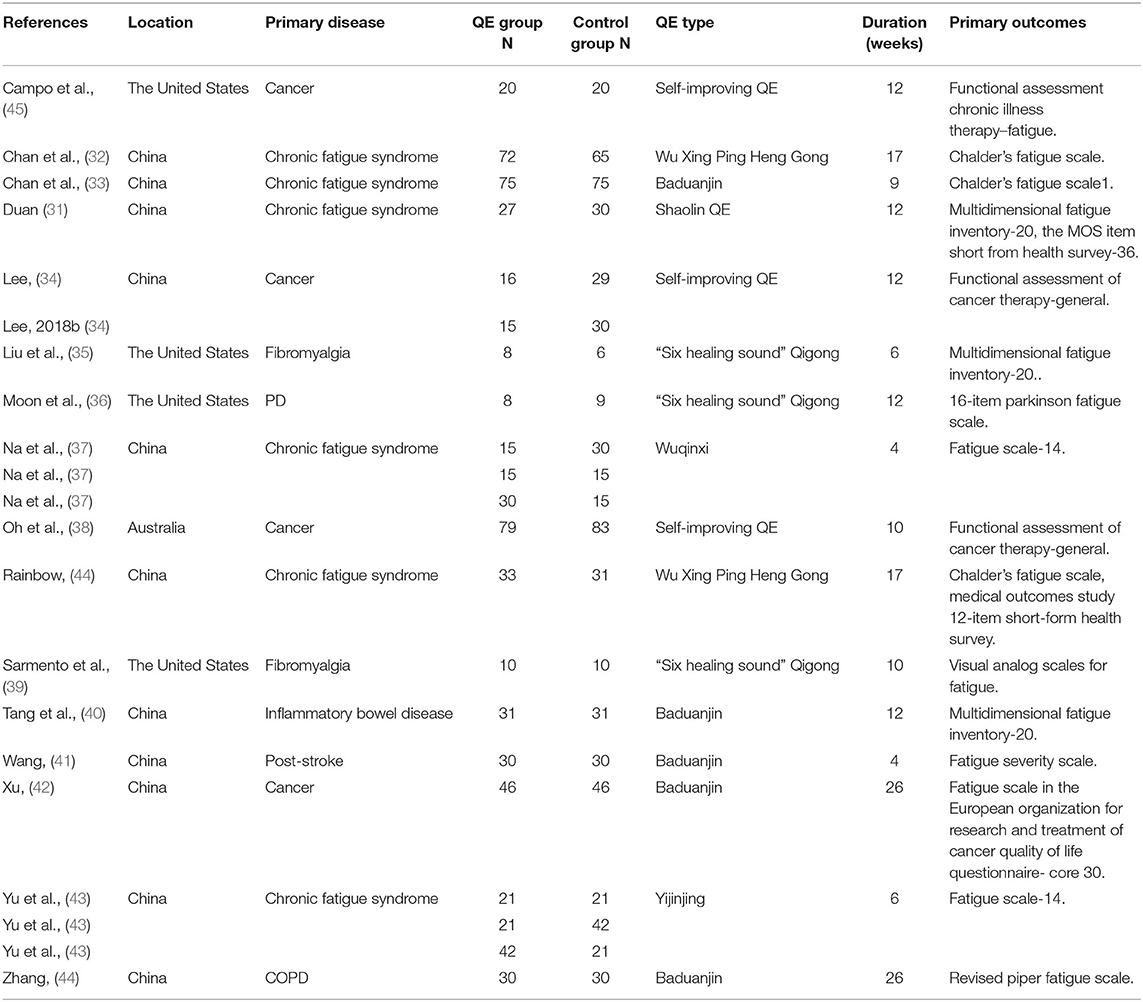
Figure 1 presents a flow chart of the study selection process. Following the initial literature review, a total of 1,836 studies were found. Of these, 1,820 were excluded as only 16 studies met the inclusion criteria (Table 1) (31–46). The total number of participants included was 1,313, and the concise summary characteristics of each study are presented in Table 1. Of the 16 published studies, 11 were conducted in China, 4 in the United States, and 1 in Australia. Among these studies, the primary disease was cancer in 4 studies, chronic fatigue syndrome in 6, fibromyalgia in 2, post-stroke in 1, chronic obstructive lung disease in the stable phase in 1, inflammatory bowel disease in 1, and Parkinson's disease in 1. Sample sizes ranged from 14 to 162, and drop-out rates ranged from 0 to 33.33%.
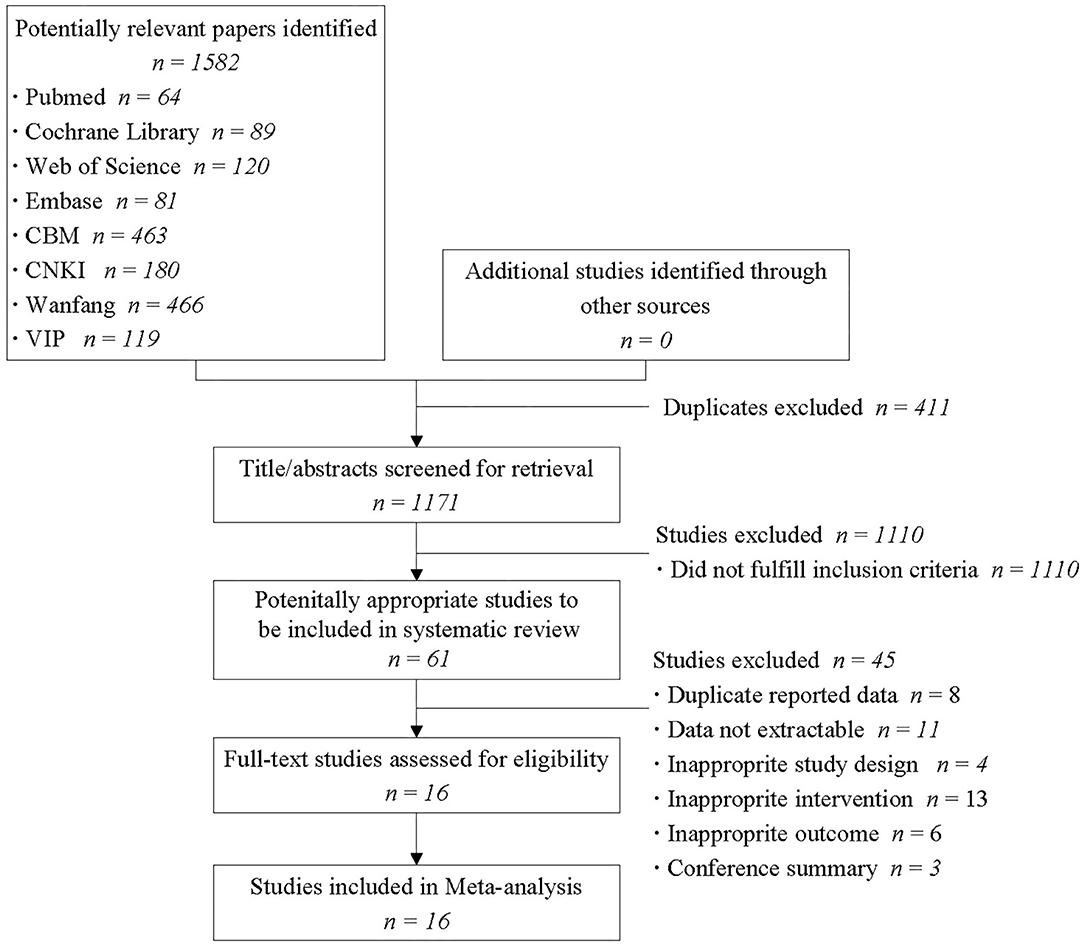
Figure 1. Flow diagram of the study selection process. CBM, Chinese biomedical literature database; CNKI, China national knowledge infrastructure.
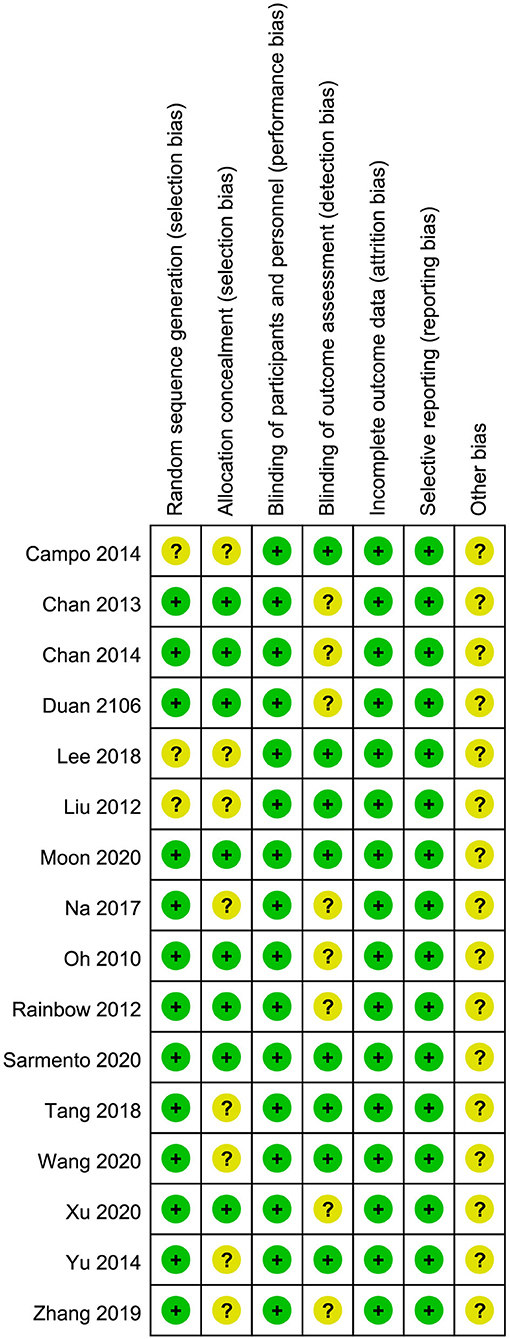
Quality of Studies
The quality of each study was evaluated considering certain methodological aspects by two authors (WR and H-XY) and is summarized in Figure 2. The generation of random sequences was adequate in 13 trials and unclear in the remaining trials. Allocation concealment was judged to be sufficient to minimize the selection bias in 8 trials; however, it was unclear in other trials. In particular, as blinding could not be applied to both participants and researchers owing to the nature of QE, blinding was judged adequate to prevent performance bias in all trials. Blinding of the outcome assessment was considered sufficient to prevent detection bias in eight trials and was unclear in eight trials. In all the trials, the quality of incomplete outcome data was adequate. No selective reporting of outcomes was observed, and other biases were classified as unclear.
Evidence From Randomized Trials
Primary Outcomes
Total Fatigue Intensity
Fifteen RCTs involving 1,253 participants reported changes in fatigue intensity. In this cohort, 614 patients performed QE; and 639 patients received other treatments in the control groups. Heterogeneity was evident (I2 = 76%, p < 0.00001). Analysis of data in the random effect method showed that QE could improve the symptoms of fatigue (SMD −0.69, 95% CI −0.95 to −0.44, p < 0.00001; Figure 3A).
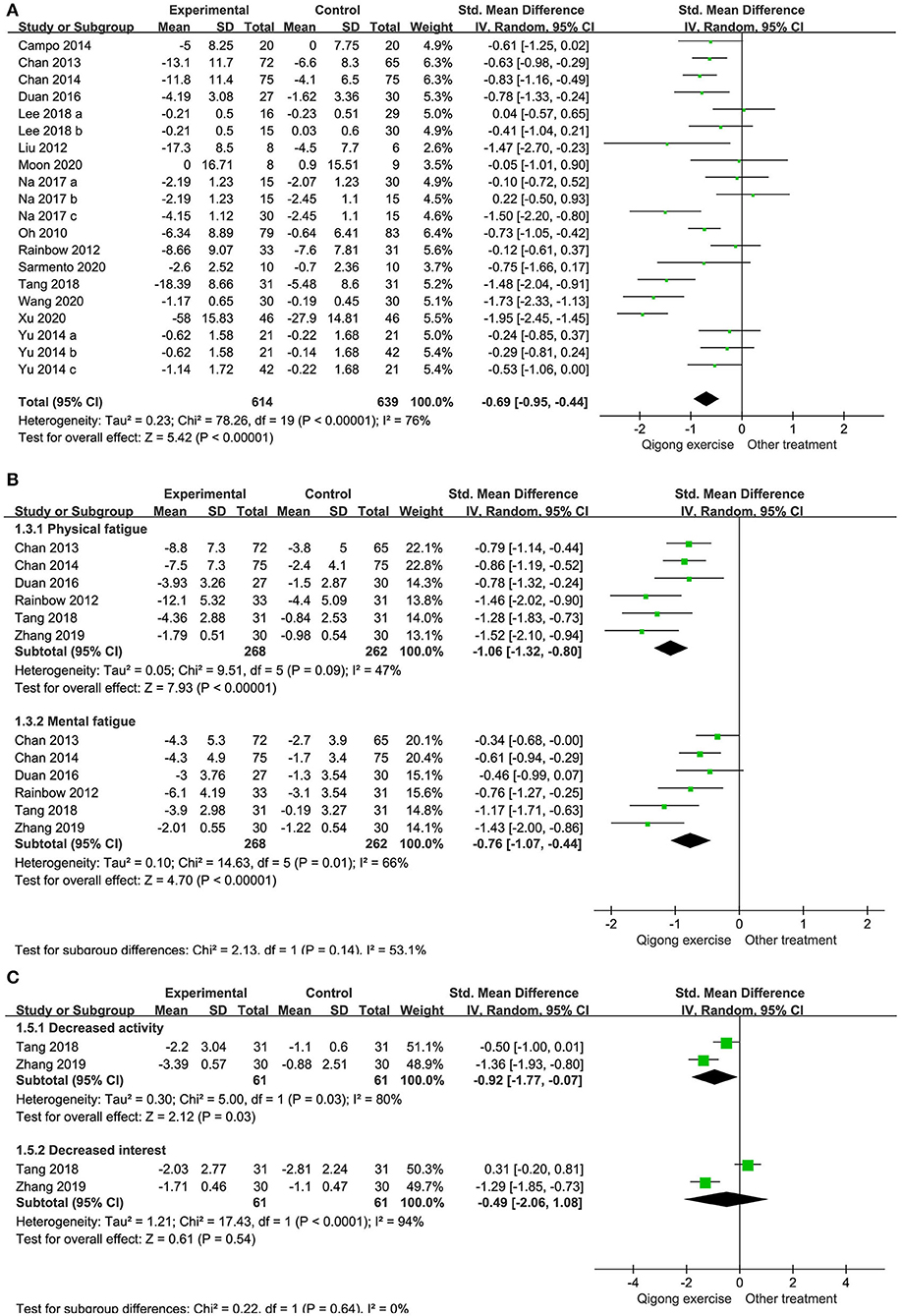
Figure 3. Forest plots illustrating the meta-analysis of outcomes with Qigong exercise (QE) vs. other treatments for fatigue symptoms. The outcomes analyzed were (A) total fatigue intensity, (B) physical and mental fatigue intensity, and (C) decreased activity and interest scale.
Physical and Mental Fatigue Intensity
Six studies involving 530 patients were included in our meta-analysis on the efficacy of QE in lowering physical and mental fatigue intensity. The intensity in all the studies was significantly lower with an overall SMD of −1.06 for physical fatigue intensity (95% CI −1.32 to −0.80) and −0.76 for mental fatigue intensity (95% CI −1.07 to −0.44; Figure 3B).
Decreased Activity and Interest Scales
Two studies involving 122 patients reported the change in activity and interest levels between baseline and endpoint. In these studies, 61 patients performed QE and 61 served as controls. The results showed that QE could improve the decreased activity levels but not the decreased interest levels. The SMDs were −0.92 and −0.49 for the decreased activity levels (95% CI −1.77 to −0.07, p = 0.03) and decreased interest levels (95% CI −2.06 to 1.08, p = 0.54; Figure 3C), respectively.
Secondary outcomes
QOL
Four RCTs reported comparisons of QOL scale scores between patients who performed QE and those who received other treatments. Significant heterogeneity was noted in the enrolled 364 patients (166 in the QE groups and 198 in the control groups) (I2 = 84%, p < 0.0001). QE could not improve the QOL scale scores (SMD 0.53, 95% CI −0.07 to 1.14; Figure 4A).
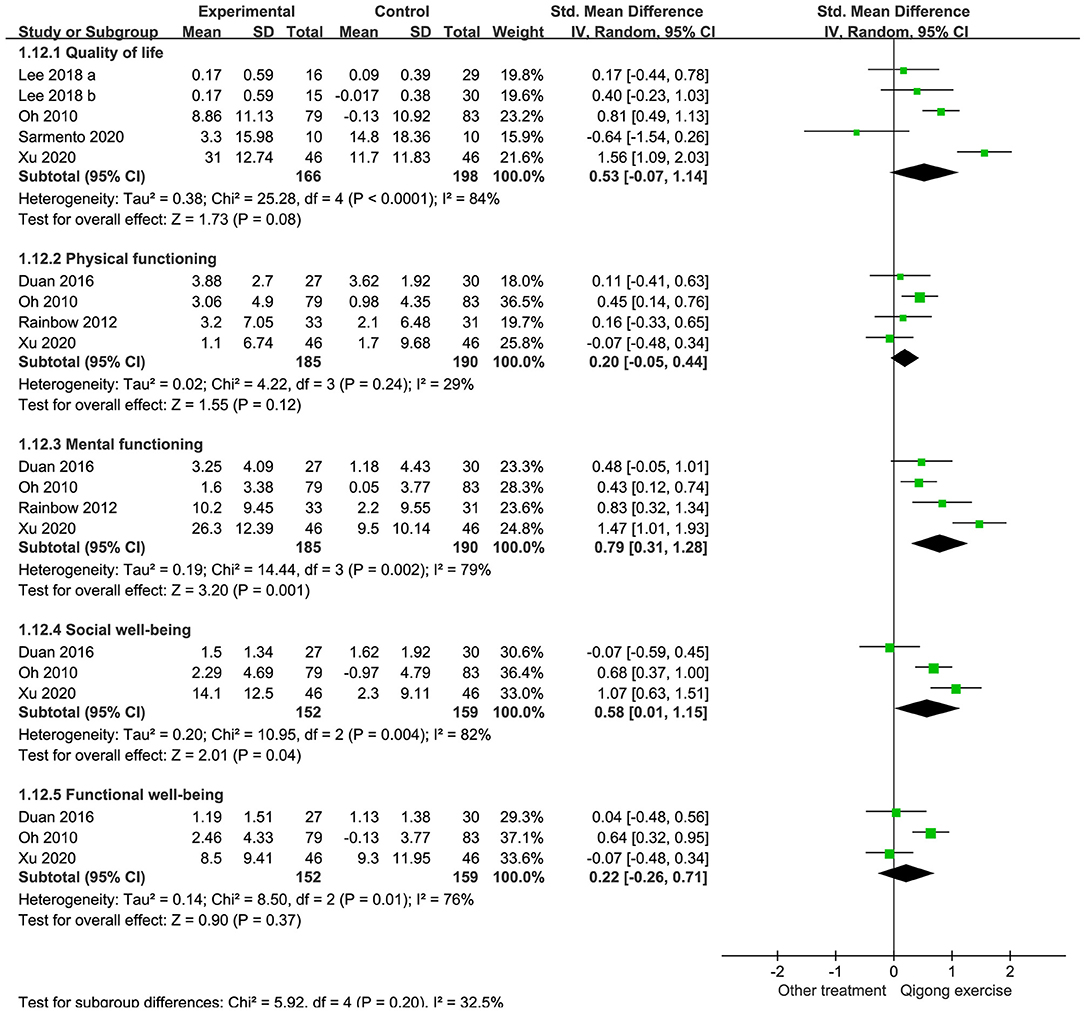
Figure 4. Forest plots illustrating the meta-analysis of outcomes with Qigong exercise (QE) vs. other treatments for quality of life (QOL). The outcomes analyzed were (A) QOL scales, (B) physical and mental functioning scales, and (C) social and functional well-being scales.
Four RCTs reported data on physical and mental functioning scale scores. Heterogeneity was not significant in studies comparing the physical functioning scale scores (I2 = 29%, p = 0.24) but was significant in those assessing mental functioning (I2 = 79%, p < 0.001). Data analyses showed that QE could not improve the physical functioning scale scores (SMD 0.20, 95% CI −0.05 to 0.44, p = 0.12) but improved the mental functioning scale scores (SMD 0.79, 95% CI 0.31 to 1.28, p = 0.001; Figures 4B,C).
Three RCTs compared the social and functional well-being scale scores between the QE and control groups. A combined analysis of 311 patients revealed that QE could improve social well-being (SMD 0.58, 95% CI 0.01 to 1.15, p = 0.04) but not functional well-being (SMD 0.22, 95% CI −0.26 to 0.71, p = 0.37). Heterogeneities were significant in these two comparisons (I2 = 82%, p = 0.04 and I2 = 76%, p = 0.01, respectively; Figures 4D,E).
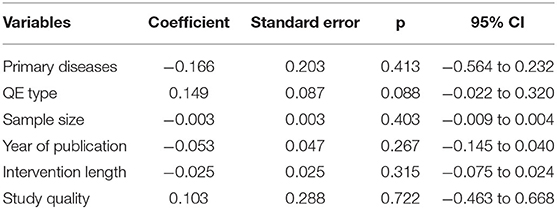
Meta-Regression
Factors examined individually in the meta-regression model of total fatigue intensity included primary diseases (cancer-related fatigue, chronic fatigue syndrome, or other diseases related fatigue), QE type (Baduanjin, other traditional Chinese QE, Wu Xing Ping Heng Gong, “Six healing sound” Qigong, or other self-improving QE), sample size, year of publication, intervention length, or study quality (high or low quality). No significant associations were found between fatigue intensity and the factors (Table 2).
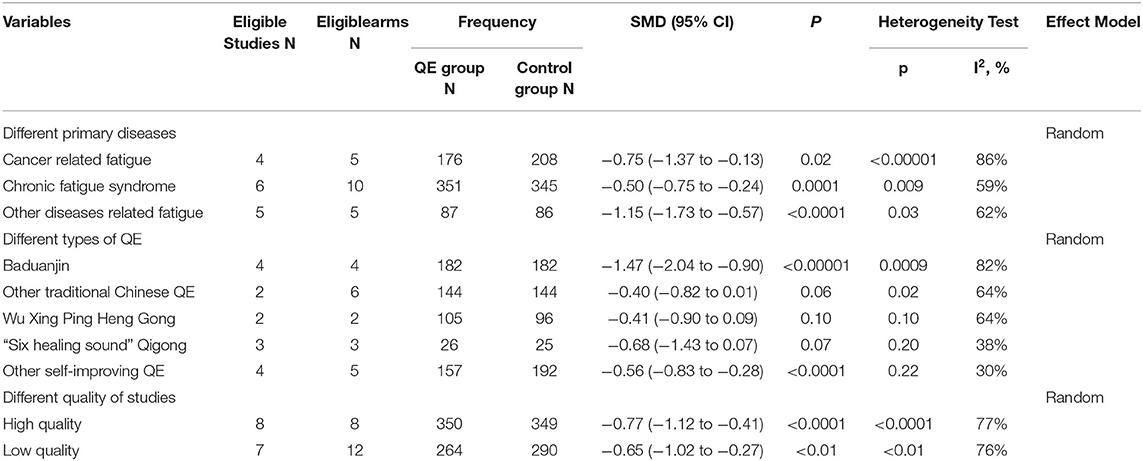
Subgroup Analysis
Although meta-regression did not detect significant factors responsible for heterogeneity, we selected different primary disease, QE type, and study quality for subgroup analysis based on the clinical characteristics of the included studies. The results suggested that the QE group with other primary disease-related fatigue showed superior total fatigue intensity improvement compared with that seen in patients with chronic fatigue syndrome and cancer-related fatigue. The Baduanjin QE group presented a trend toward better score improvement when compared with the various types of QE groups. We also found that high-quality studies were better than low-quality studies in demonstrating the benefits of QE for fatigue improvement (Table 3, Supplementary Appendix 3).
Sensitivity Analysis
Sensitivity analysis was performed in each domain of the primary outcomes to assess the stability of the meta-analysis. When any single study was deleted, the corresponding pooled SMD changed only slightly. The statistical results before and after the deletion were similar, indicating that the stability of the performed meta-analysis was good (Supplementary Appendix 4).
Publication Bias
Publication bias of the literature was tested using the Egger test. A potential publication bias in the meta-analysis on QE intervention was not detected using the funnel plot on total fatigue intensity. The graphical funnel plots of the 15 studies seemed to be symmetrical (Figure 5). We found no evidence of publication bias in the Egger regression test (t = 0.27, 95% CI −2.71 to 3.50, p = 0.79; Supplementary Appendix 5).
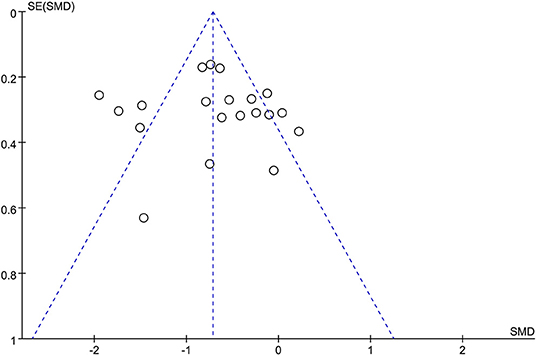
Figure 5. Funnel plot on total fatigue intensity to evaluate the publication bias of the literature. SMD, standardized mean difference.
Discussion
Whether QE is effective in alleviate fatigue is currently unknown. This meta-analysis demonstrated that QE could result in total fatigue intensity improvement in patients with symptoms of fatigue due to various diseases. Moreover, similar results were shown in both physical and mental fatigue intensity and decreased activity levels; however, the change in decreased interest levels was not significant. Moreover, the mental functioning and social well-being scale scores and the pooled data of QOL scale, physical functioning scale, and functional well-being scale scores suggest that QE was not effective.
The marked heterogeneity is a constraint of the analysis of the RCTs included in this study. An important possible reason for the observed heterogeneity is that fatigue symptoms caused by various primary diseases cannot be standardized in the baseline analysis, and differences exist in the individualized assessment scales. The effect of QE on the total fatigue intensity did not vary with the subgroup analysis of the primary diseases. Different types of QE interventions included in this study may also have led to heterogeneity. However, we found that distinguishing between different QE types had little effect on the results of fatigue improvement. In this study, the possible influence of research quality on heterogeneity was also considered, but the results of the subgroup analysis remained unchanged considering the QE effects.
We found that QE did not lead to an improved QOL in patients with fatigue. We hypothesize that this may be due to the overly complex factors that could affect the changes in indicators of QOL. Notably, QE has been effectively used in the rehabilitation of a wide range of diseases (47); it was found to improve the risk factors associated with metabolic syndrome, enhance the QOL of community-dwelling older adults with chronic disease (48), and maintain the health of patients with stable chronic obstructive lung disease (49). The mechanisms by which QE improves fatigue may include positive modulation of immune function (50), balancing the frequency of α1 and α2 waves in different brain regions (51), and increasing serum nitric oxide levels and superoxide dismutase activity to reduce the harmful effects of free radicals in patients (52). However, the mechanism underlying the therapeutic effects requires further studies. The current study revealed certain new negative findings on QE.
Reports on the effects of low-intensity exercise are conflicting. Gendron et al. considered active mind-body movement therapies as an adjunct to, or in comparison with, pulmonary rehabilitation for people with chronic obstructive pulmonary disease; however, the results remain inconclusive (53). Kelley et al. also expressed that a lack of certainty exists with regard to the benefits of exercise on chronic fatigue syndrome in adults (54). The reasons for this contrast could be attributed to the flawed trial protocol design and the poor quality of evidence, which limits their confidence in the observed effects.
We believe that the fatigue in patients may be caused by an intertwining of various diseases and varies in degree depending on age, sex, marital status, occupation, and education, which complicate the analysis of the fatigue symptoms (12). Many hypotheses regarding the pathogenesis of fatigue have been developed; however, no substantial understanding has been garnered so far, which in turn further complicates the treatment (55, 56).
Aerobic exercise, including but not limited to QE, tai chi, walking, and yoga, has been applied as rehabilitation modalities for people with fatigue in primary care, but the abovementioned recent studies did not support these treatments. However, the results of our meta-analysis were mainly positive and the quality of clinical studies in China is also improving. Previous studies often unconsciously ignored the Chinese literature, which was included in our study, since aerobic exercise itself is very popular in China. When we performed data synthesis, we did not eliminate studies based on primary disease, as a result of which we were able to assess a larger number of studies than that done by previous studies. As we sought for an intervention program with a broad clinical effect, our results differ from studies focusing on aerobic exercise.
This study had several limitations. First, the inclusion of multiple different diseases in our study, despite the statistically significant results, is likely to have produced biological bias and is one of the main reasons for the large heterogeneity. Although we performed a meta-regression analysis, it was not successful in identifying the source of heterogeneity in the correlates. The fact that fatigue, as a common symptom in primary care, occurs in different diseases is the reason for the inevitable heterogeneity of this study. We therefore performed subgroup analysis according to different primary diseases, which still showed positive results. Second, the determination of fatigue is very subjective and this has led to differences in the evaluation criteria across the included literatures. Finally, the lack of uniform QE types and intervention length may have contributed to the bias in the overall results of this study. Moreover, if individual patient data are accurate and detailed, subgroup analyses can be adjusted for age, race, and geographic location. Therefore, the statistical power of the relevant sections was influenced to a certain extent. These limitations can be overcome by conducting larger and higher quality clinical trials so that we can standardize the details of the specific diseases and QE intervention conditions.
Conclusion
Our meta-analysis demonstrated that QE was able to improve fatigue symptoms, including total fatigue intensity and physical and mental fatigue intensity. QE for fatigue in patients or the general population has not been well investigated, with only a few publications regarding this common but under-diagnosed clinical problem. Future well-designed, high-quality studies with larger sample sizes are warranted.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
DS: conceptualization, supervision, writing — review, and editing. RW: data curation, funding acquisition, validation, and writing — original draft. RW and XH: methodology. XH and YW: software. All authors contributed to the article and approved the submitted version.
Funding
This study is supported by the China Qigong Management Center (grant NO.QG2018031).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.684058/full#supplementary-material
References
1. Bansal RA, Tadros S, Bansal AS. The presence of overlapping quality of life symptoms in primary antibody deficiency (PAD) and chronic fatigue syndrome (CFS). Allergy Asthma Clin Immunol. (2020) 16:21. doi: 10.1186/s13223-020-0417-3
2. Galland-Decker C, Marques-Vidal P, Vollenweider P. Prevalence and factors associated with fatigue in the Lausanne middle-aged population: a population-based, cross-sectional survey. BMJ Open. (2019) 9:e027070. doi: 10.1136/bmjopen-2018-027070
3. Baek Y, Jung K, Kim H, Lee S. Association between fatigue, pain, digestive problems, and sleep disturbances and individuals' health-related quality of life: a nationwide survey in South Korea. Health Qual Life Outcomes. (2020) 18:159. doi: 10.1186/s12955-020-01408-x
4. Tang C, Liu C, Fang P, Xiang Y, Min R. Work-related accumulated fatigue among doctors in tertiary hospitals: a cross-sectional survey in six provinces of China. Int J Environ Res Public Health. (2019) 16:3049. doi: 10.3390/ijerph16173049
5. Sagherian K, Steege LM, Cobb SJ, Cho H. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: a cross-sectional survey of hospital nursing staff in the United States. J Clin Nurs. (2020) 20:1–38. doi: 10.1111/jocn.15566
6. Donnachie E, Schneider A, Mehring M, Enck P. Incidence of irritable bowel syndrome and chronic fatigue following GI infection: a population-level study using routinely collected claims data. Gut. (2017) 0:1–9. doi: 10.1136/gutjnl-2017-313713
7. Hinz A, Weis J, Brahler E, Mehnert A. Fatigue in the general population: German normative values of the EORTC QLQ-FA12. Qual Life Res. (2018) 27:2681–9. doi: 10.1007/s11136-018-1918-0
8. Zengarini E, Ruggiero C, Perez-Zepeda MU, Hoogendijk EO, Vellas B, Mecocci P, et al. Fatigue: relevance and implications in the aging population. Exp Gerontol. (2015) 70:78–83. doi: 10.1016/j.exger.2015.07.011
9. Thomas K, Hjalmarsson C, Mullis R, Mant J. Conceptualising post-stroke fatigue: a cross-sectional survey of UK-based physiotherapists and occupational therapists. BMJ Open. (2019) 9:e033066. doi: 10.1136/bmjopen-2019-033066
10. Ferro M, Di Lorenzo G, de Cobelli O, Bruzzese D, Pignataro P, Borghesi M, et al. Incidence of fatigue and low-dose corticosteroid use in prostate cancer patients receiving systemic treatment: a meta-analysis of randomized controlled trials. World J Urol. (2019) 37:1049–59. doi: 10.1007/s00345-018-2579-x
11. Ghanean H, Ceniti AK, Kennedy SH. Fatigue in patients with major depressive disorder: prevalence, burden and pharmacological approaches to management. CNS Drugs. (2018) 32:65–74. doi: 10.1007/s40263-018-0490-z
12. Montan I, Lowe B, Cella D, Mehnert A, Hinz A. General population norms for the functional assessment of chronic illness therapy (FACIT)-fatigue scale. Value Health. (2018) 21:1313–21. doi: 10.1016/j.jval.2018.03.013
13. Engberg I, Segerstedt J, Waller G, Wennberg P, Eliasson M. Fatigue in the general population- associations to age, sex, socioeconomic status, physical activity, sitting time and self-rated health: the northern Sweden MONICA study 2014. BMC Public Health. (2017) 17:654. doi: 10.1186/s12889-017-4623-y
14. Komaroff AL. Advances in understanding the pathophysiology of chronic fatigue syndrome. JAMA. (2019) 13:322. doi: 10.1001/jama.2019.8312
15. Ripamonti CI, Antonuzzo A, Bossi P, Cavalieri S, Roila F, Fatigoni S. Fatigue, a major still underestimated issue. Curr Opin Oncol. (2018) 30:219–25. doi: 10.1097/CCO.0000000000000451
16. Zielinski MR, Systrom DM, Rose NR. Fatigue, sleep, and autoimmune and related disorders. Front Immunol. (2019) 10:1827. doi: 10.3389/fimmu.2019.01827
17. Minton O, Richardson A, Sharpe M, Hotopf M, Stone P. A systematic review and meta-analysis of the pharmacological treatment of cancer-related fatigue. J Natl Cancer Inst. (2008) 100:1155–66. doi: 10.1093/jnci/djn250
18. Kreijkamp-Kaspers S, Brenu EW, Marshall S, Staines D, Van Driel ML. Treating chronic fatigue syndrome: a study into the scientific evidence for pharmacological treatments. Australian Family Physician. (2011) 40:907–12. doi: 10.1620/tjem.225.221
19. Yang TT, Wang L, Deng XY, Yu G. Pharmacological treatments for fatigue in patients with multiple sclerosis: a systematic review and meta-analysis. J Neurol Sci. (2017) 380:256–61. doi: 10.1016/j.jns.2017.07.042
20. Mucke M, Mochamat Cuhls H, Peuckmann-Post V, Minton O, Stone P, Radbruch L. Pharmacological treatments for fatigue associated with palliative care. Cochrane Database Syst Rev. (2015) 30:CD006788. doi: 10.1002/14651858.CD006788.pub3
21. Knips L, Bergenthal N, Streckmann F, Monsef I, Elter T, Skoetz N. Aerobic physical exercise for adult patients with haematological malignancies. Cochrane Database Syst Rev. (2019) 1:CD009075. doi: 10.1002/14651858.CD009075.pub3
22. Wu CX, Zheng Y, Duan YT, Lai X, Cui SY, Xu NG, et al. Nonpharmacological interventions for cancer-related fatigue: a systematic review and bayesian network meta-analysis. Worldviews Evid Based Nurs. (2019) 116:102–110. doi: 10.1111/wvn.12352
23. Cramp F. The role of non-pharmacological interventions in the management of rheumatoid-arthritis-related fatigue. Rheumatology. (2019) 58:v22–8. doi: 10.1093/rheumatology/kez310
24. Song YY, Hu RJ, Diao YS, Chen L, Jiang XL. Effects of exercise training on restless legs syndrome, depression, sleep quality, and fatigue among hemodialysis patients: a systematic review and meta-analysis. J Pain Symptom Manage. (2018) 55:1184–95. doi: 10.1016/j.jpainsymman.2017.12.472
25. Chen CH, Hung KS, Chung YC, Yeh ML. Mind-body interactive qigong improves physical and mental aspects of quality of life in inpatients with stroke: a randomized control study. Eur J Cardiovasc Nurs. (2019) 18:658–66. doi: 10.1177/1474515119860232
26. Zeng ZP, Liu YB, Fang J, Liu Y, Luo J, Yang M. Effects of Baduanjin exercise for knee osteoarthritis: a systematic review and meta-analysis. Complement Ther Med. (2020) 48:102279. doi: 10.1016/j.ctim.2019.102279
27. Liu XH, Li XX, Bi HY, Wang XL, Zheng X, Yang YR, et al. Working group of clinical practice guidelines of traditional chinese medicine rehabitation for cardiopulmonary.clinical practice guidelines of traditional chinese medicine rehabitation for cardiopulmonary. Rehabil Med. (2020) 30:259–65. doi: 10.3724/SP.J.1329.2020.04003
28. Cho KH, Kim TH, Kwon S, Jung WS, Moon SK, Ko CN, et al. Complementary and alternative medicine for idiopathic parkinson's disease: an evidence-based clinical practice guideline. Front Aging Neurosci. (2018) 10:323. doi: 10.3389/fnagi.2018.00323
29. Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. Cochrane statistical methods, G. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
30. Higgins JP, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta-analyses. Educ Debate. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
31. Duan X. Effect of shaolin neigong on chronic fatigue syndrome (CFS) and study about the resting-state fMRI in CFS patients. (2016).
32. Chan JS, Ho RT, Wang CW, Yuen LP, Sham JS, Chan CL. Effects of qigong exercise on fatigue, anxiety, and depressive symptoms of patients with chronic fatigue syndrome-like illness: a randomized controlled trial. Evid Based Complement Alternat Med. (2013) 2013:485341. doi: 10.1155/2013/485341
33. Chan JS; Ho RT, Chung KF, Wang CW, Yao TJ, Ng SM, et al. Qigong exercise alleviates fatigue, anxiety, and depressive symptoms, improves sleep quality, and shortens sleep latency in persons with chronic fatigue syndrome-like illness. Evid Based Complement Alternat Med. (2014) 2014:106048. doi: 10.1155/2014/106048
34. Lee YH, Lai GM, Lee DC, Tsai Lai LJ, Chang YP. Promoting physical and psychological rehabilitation activities and evaluating potential links among cancer-related fatigue, fear of recurrence, quality of life, and physiological indicators in cancer survivors. Integr Cancer Ther. (2018) 17:1183–94. doi: 10.1177/1534735418805149
35. Liu W, Zahner L, Cornell M, Le T, Ratner J, Wang Y, et al. Benefit of Qigong exercise in patients with fibromyalgia: a pilot study. Int J Neurosci. (2012) 122:657–64. doi: 10.3109/00207454.2012.707713
36. Moon S, Sarmento CVM, Steinbacher M, Smirnova IV, Colgrove Y, Lai SM, et al. Can Qigong improve non-motor symptoms in people with Parkinson's disease - a pilot randomized controlled trial? Complement Ther Clin Pract. (2020) 39:101169. doi: 10.1016/j.ctcp.2020.101169
37. Na K, Zhao DYHL, Li Y, He JG, Wu L, Sun J, et al. Clinical research on the treatment of chronic fatigue syndrome by thunder fire moxibustion combined with Wuqinxi. J Basic Chin Med. (2017) 23: 995–998. doi: 10.1006-3250(2017)07-0995-04
38. Oh B, Butow P, Mullan B, Clarke S, Beale P, Pavlakis N, et al. Impact of medical Qigong on quality of life, fatigue, mood and inflammation in cancer patients: a randomized controlled trial. Ann Oncol. (2010) 21:608–14. doi: 10.1093/annonc/mdp479
39. Sarmento CVM, Moon S, Pfeifer T, Smirnova IV, Colgrove Y, Lai SM, et al. The therapeutic efficacy of Qigong exercise on the main symptoms of fibromyalgia: a pilot randomized clinical trial. Integr Med Res. (2020) 9:100416. doi: 10.1016/j.imr.2020.100416
40. Tang C, Zhang SM, Fang J, Huang SC, Lu ST, Zhang, et al. Effects of Baduanjin exercise in traditional Chinese medicine on fatigue and quality of life in patients with moderate inflammatory bowel disease. Chin J Mod Nurs. (2018) 24:3280–84. doi: 10.3760/cma.j.issn.1674-2907.2018.27.014
41. Wang JP, Gui PJ, Xie Y. Rehabilitation effect of Baduanjin group therapy on post - stroke fatigue. J Clin Exp Med. (2020) 19:399–403. doi: 10.1016/CNKI:SUN:SYLC.0.2020-04-019
42. Xu T, Chen L, Jin CH, Zhang XQ. Effects of baduanjin on 42 cases of cancer-related fatigue and quality of life in the patients with postoperative rehabilitation of gastrointestinal malignant tumors. J Tradit Chin Med. (2020) 61:881–5. doi: 10.1016/CNKI:SUN:ZZYZ.0.2020-10-018
43. Yu XT, Hu WM, Yang WJ, Xie C, Zhu J, Zhang CY, et al. Combination of acupoint application and daoyin techniques on biomechanical properties of knee in patients with chronic fatigue syndrome. Shang J Trad Chin Med. (2014) 48:61–5. doi: 10.1016/CNKI:SUN:SHZZ.0.2014-06-028
44. Zhang TT, Ma XQ, Chen RH, Yang Y. Effects of the baduanjin exercise on the pulmonary function, fatigue status and activity tolerance in the patients with stable COPD. World J Int Trad Western Med. (2019) 14:415–8. doi: 10.1016/CNKI:SUN:SJZX.0.2019-03-035
45. Campo RA, Agarwal N, LaStayo PC, O'Connor K, Pappas L, Boucher KM, et al. Levels of fatigue and distress in senior prostate cancer survivors enrolled in a 12-week randomized controlled trial of Qigong. J Cancer Surviv. (2014) 8:60–9. doi: 10.1007/s11764-013-0315-5
46. Ho RT, Chan JS, Wang CW, Lau BW, So KF, Yuen LP, et al. A randomized controlled trial of qigong exercise on fatigue symptoms, functioning, and telomerase activity in persons with chronic fatigue or chronic fatigue syndrome. Ann Behav Med. (2012) 44:160–70. doi: 10.1007/s12160-012-9381-6
47. Zou L, Zhang Y, Sasaki JE, Yeung AS, Yang L, Loprinzi PD, et al. Wuqinxi Qigong as an alternative exercise for improving risk factors associated with metabolic syndrome: a meta-analysis of randomized controlled trials. Int J Environ Res Public Health. (2019) 16:1396. doi: 10.3390/ijerph16081396
48. Gouw VXH, Jiang Y, Seah B, He H, Hong J, Wang W. Effectiveness of internal Qigong on quality of life, depressive symptoms and self-efficacy among community-dwelling older adults with chronic disease: a systematic review and meta-analysis. Int J Nurs Stud. (2019) 99:103378. doi: 10.1016/j.ijnurstu.2019.06.009
49. Tong H, Liu Y, Zhu Y, Zhang B, Hu J. The therapeutic effects of qigong in patients with chronic obstructive pulmonary disease in the stable stage: a meta-analysis. BMC Compl Altern Med. (2019) 19:239. doi: 10.1186/s12906-019-2639-9
50. Wang CW, Ng SM, Ho RT, Ziea ET, Wong VC, Chan CL. The effect of qigong exercise on immunity and infections: a systematic review of controlled trials. Am J Chin Med. (2012) 40:1143–56. doi: 10.1142/S0192415X1250084X
51. Guo Y, Xu M, Ji M, Wei Z, Zhang J, Hu Q, et al. Gender-specific analysis of psychological adjustment of Baduanjin based on alpha band electroencephalogram power. China J Trad Chin Med Pharmacy. (2018) 33:2377–82. doi: 10.3969/j.issn.1006-2157.2017.08.007
52. Huang T, Chang JD. Influences of body building Qigong and eight-sectioned brocade on the metablisms of nitric oxide, malondialdehyde and superoxide dismutase in middle-aged and elderly people of different gender. Chin J Clin Rehabil. (2005) 9:162–4. doi: 10.1671-5926(2005)16-0162-03
53. Gendron LM, Nyberg A, Saey D, Maltais F, Lacasse Y. Active mind-body movement therapies as an adjunct to or in comparison with pulmonary rehabilitation for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. (2018) 10:CD012290. doi: 10.1002/14651858.CD012290.pub2
54. Kelley GA, Kelley KS. Exercise and cancer-related fatigue in adults: a systematic review of previous systematic reviews with meta-analyses. BMC Can. (2017) 17:693. doi: 10.1186/s12885-017-3687-5
55. Hu H, Baines C. Recent insights into 3 underrecognized conditions: Myalgic encephalomyelitis-chronic fatigue syndrome, fibromyalgia, and environmental sensitivities-multiple chemical sensitivity. Can Family Physician. (2018) 64:413–5.
Keywords: qigong exercise, fatigue, quality of life, systematic review, meta-analysis
Citation: Wang R, Huang X, Wu Y and Sun D (2021) Efficacy of Qigong Exercise for Treatment of Fatigue: A Systematic Review and Meta-Analysis. Front. Med. 8:684058. doi: 10.3389/fmed.2021.684058
Received: 22 March 2021; Accepted: 25 May 2021;
Published: 22 June 2021.
Edited by:
Kevin Lu, University of South Carolina, United StatesReviewed by:
Eron Grant Manusov, The University of Texas Rio Grande Valley, United StatesDongming Jiang, Tongji University, China
Byeongsang Oh, The University of Sydney, Australia
Copyright © 2021 Wang, Huang, Wu and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dai Sun, aHpzenl5c2RAMTI2LmNvbQ==
 Rui Wang
Rui Wang Xueyan Huang
Xueyan Huang Yeqi Wu
Yeqi Wu Dai Sun
Dai Sun